Professional Documents
Culture Documents
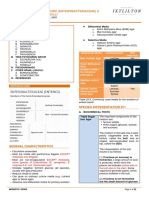
SURG (15.1) Inguinal Hernias Part 1 - Anatomy and Physiology, Diagnostics (Dr. Refuerzo - DR Capungcol)
Uploaded by
Cindy Mae Macamay0 ratings0% found this document useful (0 votes)
6 views5 pagesThe document discusses the anatomy of inguinal hernias. It describes the boundaries of the inguinal canal, including the external oblique aponeurosis anteriorly. It also discusses important structures like Hesselbach's triangle, bounded by the inferior epigastric vessels, rectus sheath, and inguinal ligament. Several important nerves that pass through the inguinal canal are also outlined, including the ilioinguinal and iliohypogastric nerves which provide sensation to the upper thigh and genitals.
Original Description:
Original Title
SURG (15.1) Inguinal Hernias Part 1_ Anatomy and Physiology, Diagnostics (Dr. Refuerzo_Dr Capungcol).Docx
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses the anatomy of inguinal hernias. It describes the boundaries of the inguinal canal, including the external oblique aponeurosis anteriorly. It also discusses important structures like Hesselbach's triangle, bounded by the inferior epigastric vessels, rectus sheath, and inguinal ligament. Several important nerves that pass through the inguinal canal are also outlined, including the ilioinguinal and iliohypogastric nerves which provide sensation to the upper thigh and genitals.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views5 pagesSURG (15.1) Inguinal Hernias Part 1 - Anatomy and Physiology, Diagnostics (Dr. Refuerzo - DR Capungcol)
Uploaded by
Cindy Mae MacamayThe document discusses the anatomy of inguinal hernias. It describes the boundaries of the inguinal canal, including the external oblique aponeurosis anteriorly. It also discusses important structures like Hesselbach's triangle, bounded by the inferior epigastric vessels, rectus sheath, and inguinal ligament. Several important nerves that pass through the inguinal canal are also outlined, including the ilioinguinal and iliohypogastric nerves which provide sensation to the upper thigh and genitals.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
INGUINAL HERNIAS PART 1: Anatomy and
Physiology, Diagnostics 3rd BIMO
Surgery 2 | Dr. Refuerzo LEC 15.1
February 7, 2023
OUTLINE spermatic cord crosses a defect in the external
I. Introduction oblique aponeurosis
II. Anatomy ● The spermatic cord traverses the inguinal canal,
A. Boundaries of Inguinal Canal and it contains three arteries, three veins, two nerves,
B. Hesselbach’s triangle the pampiniform venous plexus and the vas deferens
C. Femoral Ring
D. Blood Supply ● Additional important structures surrounding the
E. Nerve Supply inguinal canal include the iliopubic tract, the lacunar
F. Triangle of Doom ligament, Cooper’s ligament, and the conjoined
G. Triangle of Pain tendon
H. Circle of Death
III. Pathophysiology ● The iliopubic tract is an aponeurotic band that begins
IV. Types of Inguinal Hernia at the anterior superior iliac spine and inserts into
A. Indirect Inguinal Hernia Cooper’s ligament from above
B. Direct Inguinal Hernia ● The iliopubic tract helps from the inferior margin of
C. Femoral Inguinal Hernia
V. Nyhus Classification System the internal inguinal ring as it courses medially, where
VI. Clinical Classification of Hernia it continues as the anteromedial border of the femoral
VII. Diagnosis canal
A. History ● The lacunar ligament, or ligament of Gimberat, is the
B. Physical Examination
C. Imaging triangular fanning of the inguinal ligament as it joins
the pubic tubercle
● Cooper’s (pectineal) ligament is the lateral portion of
Must Know Book Lecturer
the lacunar ligament that is fused to the periosteum
of the pubic tubercle
I. INTRODUCTION ● The conjoined tendon is commonly described as the
fusion of the inferior fibers of the internal oblique and
● Approximately 75% of abdominal wall hernias occur transversus abdominis aponeurosis at the point
in the groin where they insert on the pubic tubercle
● Lifetime risk of inguinal hernia is 27% in men and 3% ● Laparoscopic inguinal hernia repair requires a
in women thorough knowledge of inguinal anatomy from a
● The incidence of inguinal hernias in males has a posterior perspective
bimodal distribution, with peaks before the first year ● Intraperitoneal points of reference are the five
of age and after the age 40 peritoneal folds, bladder, inferior epigastric vessels,
● The most common subtype of groin hernia in men and psoas muscle
and women is the indirect inguinal hernia ● Between the peritoneum and the posterior lamina of
● Inguinal hernia is a defect in the groin and the transversalis fascia is Bogros’s (preperitoneal)
intra-abdominal wall and organs that protrudes in the space. this are contains preperitoneal fat and areolar
inguinal area tissue
● ENDOABDOMINAL FASCIA (Transversalis ● The most medial aspect of the preperitoneal space,
Fascia)--layer in the abdominal wall that will prevent that which lies superior to the bladder, is known as
the protrusion of organs through the abdominal tract the space of Retzius
○ defect will result to hernia
● Most common predisposing factor is increased in
A. BOUNDARIES OF INGUINAL CANAL
abdominal pressure
● Femoral hernias occur more commonly in women
but not the most common type ● Anteriorly: External oblique aponeurosis
● Laterally: Internal oblique muscle
II. ANATOMY ● Posteriorly: Transvesalis fascia and Transversus
abdominis
● The inguinal canal is an approximately 4 to 6 cm ● Superiorly: Internal oblique and Tranvesus abdominis
long, cone shaped region situated in the anterior ● Inferiorly: Inguinal (Poupart’s) Ligament
portion of the pelvic basin
● The canal begins on the posterior abdominal wall,
where the spermatic cord passes through a hiatus in
the transversalis fascia also known as the deep
(internal) inguinal ring
● the canal concludes medially at the superficial
(external) inguinal ring, the point at which the
TG (19): Mercado, Poche, Salurio 1 of 5
D. BLOOD SUPPLY
● The vascular space is situated between the posterior
and anterior laminae of the tranvesalis fascia, and it
houses the inferior epigastric vessels which are
supplied by external iliac artery and anastomoses
with superior epigastric a continuation of the internal
thoracic artery
● Epigastric veins course parallel to the arteries in the
rectus sheath
E. NERVE SUPPLY
● Nerves of interest in the inguinal region
o Ilioinguinal
o iliohypogastric
o Genitofemoral
o Lateral femoral cutaneous
● The ilioinguinal and iliohypogastric nerves arise
together from the first lumbar nerve (L1)
B. HESSELBACH’S TRIANGLE
Ilioinguinal Nerve
● Superolaterally: Inferior Epigastric Vessels ● emerges from the lateral border of the psoas major
● Medially: Rectus Sheath and passes obliquely across the quadratus lumborum
● Inferiorly: Inguinal Ligament ● it pierces the transversus and internal oblique
muscles to enter the inguinal canal and exits through
the superficial inguinal ring
● it supplies somatic sensation to the skin of the upper
and medial thigh
● In males, it also innervates the base of the penis and
upper scrotum
● in females, it innervates the mons pubis and labia
majora
F. TRIANGLE OF DOOM
● Medial: Vas deferens
● Lateral: Vessels of the spermatic cord
● Contents:
C. FEMORAL RING o External iliac vessels
o Deep circumflex iliac vein
● Anteriorly: Iliopubic tract and inguinal ligament o Femoral nerve
● Posteriorly: Cooper’s ligament o Genital branch of the genitofemoral nerve
● Medially: Lacunar ligament
● Laterally: Femoral vein
SURG INGUINAL HERNIAS PART 1: Anatomy and Physiology, Diagnostics 2 of 5
G. TRIANGLE OF PAIN ● Several studies have documented strenuous physical
activity as a risk factor for acquired inguinal hernia
● bordered by the iliopubic tract and gonadal vessels, ● Microscopic examination of skin of inguinal hernia
and it encompasses the lateral femoral cutaneous, patients demonstrated significantly decreased ratios
femoral branch of genitofemoral and femoral nerves of type I to type III collagen
H. CIRCLE OF DEATH
● A vascular continuation formed by:
o common iliac
o internal iliac
o obturator
o inferior epigastric
o external iliac
III. PATHOPHYSIOLOGY
● Inguinal hernias may be congenital or acquired
● Most adult inguinal hernias are considered acquired
defects in the abdominal wall
● The most likely risk factor for inguinal hernia is
weakness in the abdominal wall musculature
● Congenital hernias, which make up the majority of
pediatric hernias, can be considered a developmental
defect rater that an acquired weakness
● Failure of the peritoneum to close results in a patent
processus vaginalis (PPV)
SURG INGUINAL HERNIAS PART 1: Anatomy and Physiology, Diagnostics 3 of 5
IV. TYPES OF INGUINAL HERNIA V. NYHUS CLASSIFICATION SYSTEM
A. INDIRECT INGUINAL HERNIA Nyhus Classification categorizes hernia defects by
location, size and type.
● congenital
● Children (1st decade of life)
● Patent Processus Vaginalis
● Lateral to the inferior epigastric vessels
● enter inguinal canal at the deep inguinal ring
● cass pass into the scrotum
● more common (⅔ of hernia)
B. DIRECT INGUINAL HERNIA VI. CLINICAL CLASSIFICATION OF HERNIA
● Acquired REDUCIBLE HERNIA
● Adults (4th decade of life) ● is one which can be pushed back into the abdomen
● Weakness of the abdominal wall by putting manual pressure to it
● Directly behind the superficial inguinal ring
● Medial to the inferior epigastric vessels, within IRREDUCIBLE/INCARCERATED HERNIA
Hesselbach’s triangle ● is one which cannot be pushed back into the
● Cannot descend into the scrotum abdomen by applying manual pressure
● Obstructed Hernia - one in which the lumen of the
C. FEMORAL INGUINAL HERNIA herniated part of intestine is obstructed
● Strangulated hernia - in one in which the blood
● Femoral hernias protrude through the small and supply of the hernia contents is cut off, thus, leading
inflexible femoral ring to ischemia. The lumen of the intestine may be patent
● They traverse the empty space between the femoral or notc
vein and the lymphatic channels Clinical Parameters of Strangulation:
● Fever
● Tachycardia
● Exquisite tenderness
● Erythema tenderness
● Erythema of underlying skin
● leukocytosis
● Obstructive symptoms
VII. DIAGNOSIS
A. HISTORY
● The most common symptom of inguinal hernia is a
groin mass that protrudes while standing, coughing,
or straining
● Symptoms that are extrainguinal such as change in
bowel habits or urinary symptoms are far less
SURG INGUINAL HERNIAS PART 1: Anatomy and Physiology, Diagnostics 4 of 5
common but should be recognized as having the C. IMAGING
potential to be ominous
● The pain is thought to be due to compression of the ● In the case of an ambiguous diagnosis, radiologic
nerves by the sac, causing generalized pressure, investigations may be used as an adjunct to history
localized sharp pain, or referred pain and physical examination. Imaging in obvious cases
● Patients will often reduce the hernia by pushing the is unnecessary
contents back into the abdomen, thereby providing
temporary relief. As the defect size increases and ULTRASOUND
more intra-abdominal contents fill the hernia sac, the
hernia may become harder to reduce and ● Least invasive technique and does not impart any
incarcerate, prompting urgents surgical intervention radiation to the patient
● Certain elements of the review of systems such as ● Anatomic structures can be more easily identified by
chronic constipation, cough, or urinary retention the presence of bony landmarks; however, because
should prompt the surgeon to perform a thorough there are few bones in the inguinal canal, other
workup to rule out any underlying malignancy structures such as the inferior epigastric vessels are
used to define groin anatomy
● Positive intra-abdominal pressure is used to elicit the
B. PHYSICAL EXAMINATION herniation of abdominal contents
● Sensitivity of 86%, specificity of 77%
● Essential for diagnosis
● The patient should be examined in a standing CT-SCAN
position ● Provide static images that are able to delineate groin
● Ideally, the patient should be examined in a standing anatomy, to detect groin hernias, and to exclude
position to increase intra-abdominal pressure, with potentially confounding diagnoses
the groin and scrotum fully exposed ● Sensitivity of 80%, specificity of 65%
● Inspection is performed first, with the goal of
identifying an abnormal bulge along the groin or MRI
within the scrotum. if an obvious bulge is not
detected, palpation is performed to confirm the ● Most commonly utilized in cases where physical
presence of the hernia examination detects a groin bulge, but where
● Palpation is performed by advancing the index finger ultrasonography is inconclusive
through the scrotum towards the external inguinal ● The expense of MRI precludes its routine use to
ring (Digital exam) diagnose inguinal hernias
● The patient is then asked to perform a Valsalva
maneuver to increase intraabdominal pressure REFERENCES
● Examination of the contralateral side affords the
clinician the opportunity to compare the presence and Dr. Refuerzo’s ppt
extent of herniation between sides Schwartz’s Principles of Surgery, 10th Ed.
● In addition to inguinal hernia, a number of other
diagnoses may be considered in the differential of a FREEDOM WALL
groin bulge
SURG INGUINAL HERNIAS PART 1: Anatomy and Physiology, Diagnostics 5 of 5
You might also like
- SURGERY 4.4 Inguinal HerniaDocument17 pagesSURGERY 4.4 Inguinal HerniaMaikka IlaganNo ratings yet
- Sahitya Snigdha (Hernia Module)Document159 pagesSahitya Snigdha (Hernia Module)h9pkyd9dg9No ratings yet
- Groin AnatomyDocument7 pagesGroin AnatomyLorenzo Daniel AntonioNo ratings yet
- Hernia Refarat Khansa 2Document31 pagesHernia Refarat Khansa 2Khansa Hanifah Mutia100% (1)
- (Lib-Ebooks Com) 020320211902Document6 pages(Lib-Ebooks Com) 0203202119029423352601No ratings yet
- HerniaDocument5 pagesHerniasarguss14100% (5)
- Inguinal CanalDocument48 pagesInguinal CanalMahi100% (1)
- Anatomy of Inguinal Canal: DR Vishnu Mohan 29/11/2014Document51 pagesAnatomy of Inguinal Canal: DR Vishnu Mohan 29/11/2014abbasNo ratings yet
- Hernia FTDDocument71 pagesHernia FTDEmmanuel Papa AcquahNo ratings yet
- Visual 2. Auditory 3. EroticDocument10 pagesVisual 2. Auditory 3. EroticChristyl JoNo ratings yet
- Inguinal Canal and ScrotumDocument55 pagesInguinal Canal and ScrotumAuza Moses IbrahimNo ratings yet
- Inguinal Hernias Lecture by Wilfredo Tayag, M.D, FPCS Schwartz Principle of Surgery 10 EditionDocument9 pagesInguinal Hernias Lecture by Wilfredo Tayag, M.D, FPCS Schwartz Principle of Surgery 10 EditionMarlon molano100% (9)
- Triangle of Doom and Pain 1Document7 pagesTriangle of Doom and Pain 1AnantaSiddhiPrawaraNo ratings yet
- Inguinoscrotal Swellings and Undescended TestisDocument115 pagesInguinoscrotal Swellings and Undescended Testissyirah99No ratings yet
- Saint Louis University School of Medicine Mmxxii: Dr. Laygo - October 22, 2020Document37 pagesSaint Louis University School of Medicine Mmxxii: Dr. Laygo - October 22, 2020Djan Kurvie ValencerinaNo ratings yet
- EMRCS Abdomin AnatomyDocument54 pagesEMRCS Abdomin AnatomyShakirNo ratings yet
- Anatomy For Groin Hernia RepairDocument69 pagesAnatomy For Groin Hernia RepairROUNAK MEHROTRANo ratings yet
- OB Williams Chap 2 Maternal AnatomyDocument7 pagesOB Williams Chap 2 Maternal AnatomyRem Alfelor0% (1)
- Dinding Abdomen PSIKDocument79 pagesDinding Abdomen PSIKSondang DamanikNo ratings yet
- Anatomy of GIT For PCII Students..Document106 pagesAnatomy of GIT For PCII Students..AMANUEL HABTEWOLDNo ratings yet
- Perineal TearsDocument49 pagesPerineal TearsvisakhaNo ratings yet
- Chapter 2 Maternal AnatomyDocument9 pagesChapter 2 Maternal AnatomyRem Alfelor100% (2)
- Inguinalcanalanatomy DR 170104140951Document51 pagesInguinalcanalanatomy DR 170104140951srinathbadugu0777No ratings yet
- Anatomy of Female Reproductive Organs: Dr.M.Mahalakshmi Assistant Professor Government Chengalpattu Medical CollegeDocument20 pagesAnatomy of Female Reproductive Organs: Dr.M.Mahalakshmi Assistant Professor Government Chengalpattu Medical Collegepranu6789No ratings yet
- Anatomy of Inguinal CanalDocument10 pagesAnatomy of Inguinal CanalsaisoniaNo ratings yet
- Abdominal Wall and HerniaDocument35 pagesAbdominal Wall and HerniaMohammad BanisalmanNo ratings yet
- Perineum: Dr. Edi Patmini SS, Spog/Dr. M. Nurhadi Rahman, SpogDocument16 pagesPerineum: Dr. Edi Patmini SS, Spog/Dr. M. Nurhadi Rahman, Spogpuskesmas gebangNo ratings yet
- AbdWall, Hernia Atbp - AnnoDocument34 pagesAbdWall, Hernia Atbp - AnnoJuan Lorenzo RequironNo ratings yet
- 2 - Female PerineumDocument30 pages2 - Female PerineumAndrew AldrichNo ratings yet
- Hernia Seminar 2 Aug 2014 FinalDocument20 pagesHernia Seminar 2 Aug 2014 FinalKishan NaiduNo ratings yet
- Peretul AbdominalDocument9 pagesPeretul AbdominalBotond LukacsNo ratings yet
- Inguinal Region AnatomyDocument6 pagesInguinal Region AnatomysimonaNo ratings yet
- Inguinal HerniaDocument19 pagesInguinal HerniaArdham ChesukoruNo ratings yet
- Anterior Abdominal Wall and Inguinal CanalDocument35 pagesAnterior Abdominal Wall and Inguinal Canalapi-3698357100% (3)
- Abdominal HerniasDocument33 pagesAbdominal Herniastianally100% (2)
- Hernias SabistonDocument27 pagesHernias SabistonAdip Grimaldis MirandaNo ratings yet
- Anterior Abdominal Wall& Inguinal Canal 2023Document26 pagesAnterior Abdominal Wall& Inguinal Canal 2023GanapathyGaneshNo ratings yet
- The Perineum: Dr:Ahmed Ibrahim Abdi (Nawawi) AnatomistDocument21 pagesThe Perineum: Dr:Ahmed Ibrahim Abdi (Nawawi) AnatomistSAKARIYE MAXAMEDNo ratings yet
- Organ Anatomy Notes 2Document11 pagesOrgan Anatomy Notes 2ELIANA CARIS CABILDONo ratings yet
- Abdomen MCQDocument24 pagesAbdomen MCQTatyanna Rammouz100% (1)
- 1 - OB 1 (Maternal Anatomy)Document13 pages1 - OB 1 (Maternal Anatomy)Gen XNo ratings yet
- Abdomen (Inguinal Hernia) : Anatomy II Block 3 NotesDocument39 pagesAbdomen (Inguinal Hernia) : Anatomy II Block 3 NotesJoseph KimNo ratings yet
- HerniaDocument106 pagesHerniaDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Yyyyycrash Course Anatomy - AbdomenDocument31 pagesYyyyycrash Course Anatomy - Abdomen黃芳昌No ratings yet
- Anatomical Considerations During G-Laparoscopic SurgeryDocument28 pagesAnatomical Considerations During G-Laparoscopic SurgeryMahia RahmanNo ratings yet
- ABDOMINAL WALL Reviewer For AnatomyDocument3 pagesABDOMINAL WALL Reviewer For AnatomyLeira LeeNo ratings yet
- Key PointsDocument34 pagesKey PointsSe YunNo ratings yet
- Inguinal Hernias: Trix M. Asuncion M.D. General SurgeryDocument55 pagesInguinal Hernias: Trix M. Asuncion M.D. General Surgeryjitendra magarNo ratings yet
- Antaomy of GITDocument5 pagesAntaomy of GITMike GNo ratings yet
- PerineumDocument41 pagesPerineumDr chaitra brNo ratings yet
- LG 3 (Abdominal Wall Muscles and Inguinal Canal)Document33 pagesLG 3 (Abdominal Wall Muscles and Inguinal Canal)allanNo ratings yet
- Surgical Anatomy-Anal Canal: Dr. Belal MansoorDocument79 pagesSurgical Anatomy-Anal Canal: Dr. Belal MansoorYogi drNo ratings yet
- U Michigan Written Quiz - Inguinal RegionDocument14 pagesU Michigan Written Quiz - Inguinal Regiontheintrepiddodger0% (1)
- Types of Hernias: AnatomyDocument3 pagesTypes of Hernias: Anatomyhrg79qzwc2No ratings yet
- Perineal Tear: Presented by - Mayuri Zanwar Guided By-Dr. Sheetal Ma'AmDocument20 pagesPerineal Tear: Presented by - Mayuri Zanwar Guided By-Dr. Sheetal Ma'Ammayuri zanwarNo ratings yet
- 3-Inguinal Canal PDFDocument58 pages3-Inguinal Canal PDFN A0% (1)
- Epidural AnaesthesiaDocument99 pagesEpidural AnaesthesiaabhinavguttikondaNo ratings yet
- Practices of Anorectal SurgeryFrom EverandPractices of Anorectal SurgeryDong Keun LeeNo ratings yet
- A New Order of Fishlike Amphibia From the Pennsylvanian of KansasFrom EverandA New Order of Fishlike Amphibia From the Pennsylvanian of KansasNo ratings yet
- PEDIA Quiz 1Document3 pagesPEDIA Quiz 1Cindy Mae MacamayNo ratings yet
- (UST-FMS) Guide For History Taking, Physical Examination, - Diagnosis of Pediatric Patients 3eDocument206 pages(UST-FMS) Guide For History Taking, Physical Examination, - Diagnosis of Pediatric Patients 3eCindy Mae MacamayNo ratings yet
- MED (6) Chills and Fever (Dr. Latoja)Document57 pagesMED (6) Chills and Fever (Dr. Latoja)Cindy Mae MacamayNo ratings yet
- PHARMA 02. PharmacodynamicsDocument11 pagesPHARMA 02. PharmacodynamicsCindy Mae MacamayNo ratings yet
- MICRO 11. EnterobacteriaceaeDocument22 pagesMICRO 11. EnterobacteriaceaeCindy Mae MacamayNo ratings yet
- Pharmacology Samplex (1 Bimonthly) : 1 QuizDocument15 pagesPharmacology Samplex (1 Bimonthly) : 1 QuizCindy Mae MacamayNo ratings yet
- Measures That Use COD PhilDocument52 pagesMeasures That Use COD PhilCindy Mae MacamayNo ratings yet
- PHARMA 06. Introduction To Autonomic PharmacologyDocument6 pagesPHARMA 06. Introduction To Autonomic PharmacologyCindy Mae MacamayNo ratings yet
- Revision of Pharmacokinetic TermsDocument40 pagesRevision of Pharmacokinetic TermsCindy Mae MacamayNo ratings yet
- Group 3 RESEARCH PROPOSALDocument41 pagesGroup 3 RESEARCH PROPOSALCindy Mae Macamay100% (5)
- PCM (1) Introduction To Biostatistics (Dr. Tante)Document20 pagesPCM (1) Introduction To Biostatistics (Dr. Tante)Cindy Mae MacamayNo ratings yet
- Case Study On Biopsychosocial ApproachDocument19 pagesCase Study On Biopsychosocial ApproachCindy Mae MacamayNo ratings yet
- PCM (2) Indices of Biostatistics (Dr. Tante)Document44 pagesPCM (2) Indices of Biostatistics (Dr. Tante)Cindy Mae MacamayNo ratings yet
- PHYSIO (38) Motor Functions of The Spinal Cord (Dr. Mambulao)Document7 pagesPHYSIO (38) Motor Functions of The Spinal Cord (Dr. Mambulao)Cindy Mae MacamayNo ratings yet
- MICRO (1) Fundamentals of Microbiology - Dra - AbuevaDocument16 pagesMICRO (1) Fundamentals of Microbiology - Dra - AbuevaCindy Mae Macamay100% (1)
- 3rdbimo NeuroPhysioDocument10 pages3rdbimo NeuroPhysioCindy Mae MacamayNo ratings yet
- Forms and Sources of EnergyDocument60 pagesForms and Sources of EnergyCindy Mae MacamayNo ratings yet
- What Are All These Pictures Representing?Document74 pagesWhat Are All These Pictures Representing?Cindy Mae MacamayNo ratings yet
- Energy Transformation: Prepared By: Ms. Cindy Mae V. MacamayDocument21 pagesEnergy Transformation: Prepared By: Ms. Cindy Mae V. MacamayCindy Mae MacamayNo ratings yet
- Skeletal System Summative Test (Grade 6)Document5 pagesSkeletal System Summative Test (Grade 6)Cindy Mae Macamay50% (2)
- SUMMATIVE TEST IN SCIENCE 6 (Fourth Quarter)Document3 pagesSUMMATIVE TEST IN SCIENCE 6 (Fourth Quarter)Cindy Mae Macamay100% (2)
- Harmful Effects of MixturesDocument34 pagesHarmful Effects of MixturesCindy Mae MacamayNo ratings yet
- 24 - Metor 6E DatasheetDocument2 pages24 - Metor 6E DatasheetCharles LiNo ratings yet
- 06 The Technical Framework of Truffle CultivationDocument19 pages06 The Technical Framework of Truffle CultivationMate CroNo ratings yet
- Air Conditioning Drain Pan Treatments: DescriptionDocument3 pagesAir Conditioning Drain Pan Treatments: DescriptionCrescent MoonNo ratings yet
- KCALCDocument12 pagesKCALCPaty ParedsNo ratings yet
- Wika Thermowell DS PDFDocument4 pagesWika Thermowell DS PDFaspdNo ratings yet
- Corrosion Prevention During Acid Cleaning of Pulping EquipmentDocument22 pagesCorrosion Prevention During Acid Cleaning of Pulping EquipmentlyoufNo ratings yet
- House Sitting AgreementDocument16 pagesHouse Sitting AgreementjamesNo ratings yet
- Search For Childcare CentreDocument2 pagesSearch For Childcare CentrefalanksNo ratings yet
- Patho Ch. 10-12Document13 pagesPatho Ch. 10-12JoyyNo ratings yet
- Sped and AlsDocument20 pagesSped and Alsrose dianne reyesNo ratings yet
- Lectura Del U5Document6 pagesLectura Del U5Valeria RamosNo ratings yet
- Hatchery MNGT PresentationDocument16 pagesHatchery MNGT PresentationKarl KiwisNo ratings yet
- Urea EPC ScheduleDocument45 pagesUrea EPC Schedulevishal_madhukar100% (1)
- When I Say No, I Feel Guilty - Notes/Cheat SheetDocument3 pagesWhen I Say No, I Feel Guilty - Notes/Cheat Sheet914radio100% (9)
- Month Wise Checklist For Submission of Various ReturnsDocument3 pagesMonth Wise Checklist For Submission of Various Returnsadith24No ratings yet
- A005A120020-Basic Equipment (L0L) From April 2010Document1,105 pagesA005A120020-Basic Equipment (L0L) From April 2010Carlos Garcia GodoyNo ratings yet
- TAX 06 Preweek LectureDocument16 pagesTAX 06 Preweek LectureJohn DoeNo ratings yet
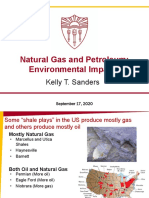
- FA2020 - ENE505 - L4.5 - Fossil Fuels - Oil & Gas Env ImpactsDocument43 pagesFA2020 - ENE505 - L4.5 - Fossil Fuels - Oil & Gas Env ImpactsTommy TrojanNo ratings yet
- Jeannerod (2001) Neural Simulation of Action. A Unifying Mechanism For Motor CognitionDocument7 pagesJeannerod (2001) Neural Simulation of Action. A Unifying Mechanism For Motor CognitionPaul Wood100% (2)
- E Locking Cessna 172Document3 pagesE Locking Cessna 172RAJ MOHANNo ratings yet
- MSDS Capilene G 86 EDocument4 pagesMSDS Capilene G 86 Ezubair1951No ratings yet
- Acei and ArbDocument6 pagesAcei and ArbNurulrezki AtikaNo ratings yet
- Lesson 3 The Ideal Gasq PDFDocument4 pagesLesson 3 The Ideal Gasq PDFireneNo ratings yet
- Lancet BFseriespaper1Document17 pagesLancet BFseriespaper1nosh.rose95No ratings yet
- DDA Housing Scheme 2020 - Previous DDA Flats Price List, Location, ApplicationDocument9 pagesDDA Housing Scheme 2020 - Previous DDA Flats Price List, Location, Applicationraj RajNo ratings yet
- Experiment 2 - Enzyme ActivityDocument7 pagesExperiment 2 - Enzyme ActivityFatimatuzzahra' Binti Hardiyono FISNo ratings yet
- Task Antropology of Law (Paper Bahasa Inggris Antropologi Hukum)Document7 pagesTask Antropology of Law (Paper Bahasa Inggris Antropologi Hukum)Ratri NugraheniNo ratings yet
- DRF 4343 Product Data enDocument8 pagesDRF 4343 Product Data enSami MoqbelNo ratings yet
- Adjectives - ED or - ING Exercise: A Fill The Gaps With The Adjectives in BracketsDocument2 pagesAdjectives - ED or - ING Exercise: A Fill The Gaps With The Adjectives in BracketsYoNo ratings yet
- Wheat Crop Development in Central Punjab (Faisalabad, 2020 - 21)Document32 pagesWheat Crop Development in Central Punjab (Faisalabad, 2020 - 21)Fuzail KhanNo ratings yet