Professional Documents
Culture Documents
Anti-Infect Dis
Uploaded by
Muhammad Amin BozdarOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti-Infect Dis
Uploaded by
Muhammad Amin BozdarCopyright:
Available Formats
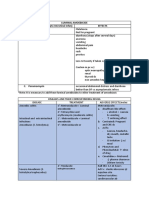
Dis Pathogen Emperic Th Adv Disadv
Acetaminophine (pain relief) for 48-72 hrs, most kids resolve, if not (only 1 out of 12) will
need AB. <2y-->10 days AB, >2y-->5 days, azithropmycin-->5 days for all ages
Serous Otitis media--> AB for 2w-3m
1) eff agnst 90% of bact of
Better abs than
New Episode &
AOM 2)most eff ag occ mild diarrhea, maculopapular
ampicillin
Serous OM:
pneumococci e' low suscp skin rash
Amoxicillin (TID),
to Pencef 3)Excll safety
Acute otitis Media AOM
Pivampicillin (BID), profile high cost, e' no improvement
S. pneumonia (+ve) Co trimoxazole (BID) Suitable for travelling bec liq 1) not eff agnst Strept gpA
H.influenza (-ve) formln has long shelf-life at RT 2) inc resist of pneumococci & H influ
Morhaxilla
catarrhalis (-ve) Recurrent: Amox/Clav: diarrhea occurs in 50%
Amoxicillin high dose or Amoxicillin /Clavu a' TID of pts
NB eff agnst amoxicillin resist strains of H 1) not eff ag S aureus or pneumococci
(1) ; pnuemococcal Cefixime (OD) influenza & M catarrhalis 2) Diarrhea in 10% of pts
vaccination is ineff in
AOM
NB (2) ; Oral anti Cefaclor (BID or TID) Serum sickness in 1% of children
eff agnst most bact of AOM
hist & decongestant
won't improve it av as sachets for 1) Bitter after taste of susp.'. Taken e'
Cefuroxime (BID)
travellers juice or food
Cefprozil (BID)
NB: Pneumoc are sometimes resistant to
good tasting liq formuln Azithro
Azithromycin OD HS
better tolerated than Bitter after taste to be taken e' food
Clarithromycin BID NB: Pneumoc are sometimes resist
eythro to it
Erythromycin/ Eryth--> 40% NV abd pain
Sulphaisoxazole Sulpha--> Rash
TID or QID
Penicillin V TID (all AB for full 10 days) or G
St Sore throat
Strept gp A od
(pharyngitis,
laryngitis)
NB: any if allergy; Erythromycin estolate, Erythromycin ethylsuccinate bid-qid, Clarithromycin
culture (acute or chronic BID, Azithromycin OD HS If not eff; Cephalexin
case) that yield Strpt
gpA-->AB for fear of Acetaminophine for pain and fever, Lozenges and gargle for symptomatic ttt
Rheumatoid fever If chronic carriage .'.addn of Rifampin in the last 4
days of Pen Or Clindamycin alone
a- hemolytic Amoxicillin (oral) or Ampicillin IV (before)
strept. or S
Prevention of
Endocarditis
viridans; for dental, Dental extractn; 3 g before & 1.5 after
Bacterial
oral, resp, oesoph If allergy: clinda, clarithro, azithro, cephadroxil, cephalexin allergy & Not oral;
proced (but not endos) Clinda, cephazolin
enterococcus If allergy & moderate risk; Vancomycin
fecalis; GI & Gu (but If high risk; (cardiac) Amp+genta before then Amp or Amox after if allergy;
not all types of delivery or
hyst) vanco+genta
Enfants:
H.
DOC < 1 m; Vancomycin + (Amp + genta or Cefotaxime)
influenza type b,
Bacterial meningitis
< 3 m or Elderly; Amp + Ceftriaxone or Cefotaxime. If S
S. Ceftriaxone or Cefotaxime pneum.'. > 3 m: Vancomycin + IV Cefotaxime (esp
pneumonia, Pen G if pneumococcal) or Ceftriaxone If allergy to B-
N. Pen G lactam or hypersensitivity: vancomycin + Rifampin Anti-inf Th: IV
meningitidis
Dexamethasone in child > 6w : 1) ttt & dec deafness caused by H influenza. 2)
Elderly; Amp considered for S pneumonia & N meningitidis but it dec penetration of AB to CSF
S. pneum, Ceftriaxone or Cefotaxime
Prophylaxis:
E coli, Amp
Pneumococcal conjugate vaccine & AB Th as Rifampin, Ceftriaxone or
Listeria Ciprofloxacin Response Monitoring: imprved brain func
monocytogene
Susc; Pen G, Amox, Macrolide
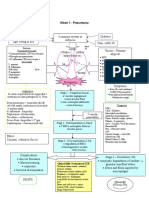
Community Acquired
Strept Resis; Pen G, Cefo, cef, levo
Sympt; cough, shortness of breath, plueritic chest pain, sputum,
fever, chilis, myalgia, arthalgia, headache severe; resp rate > 30
Mycoplasma Pneum
Doxycilline, macrolide
Clamydia If severity is < 90; ttt at home & Macrolide or Doxycycline
Pneumonia
H influenza Cephalosporin, or If hospitalized; Levofloxacin OR (2nd or 3rd Ceph + macrolide)
M. catarrhalis Amox/Clav
If ICU; IV Levofloxacin + B-lactam (imipenem or
Staph aureus Meth susc-->Cloxacilin meropenem) OR Macrolide + Aminoglycoside + IV B-
Legionella MRSA-->Vancomycin lactam
Fquinolone Or macrolide NB Vaccination ag Pneumo & influenza shd b considered
+ Rifampin (never used alone in CAP)
latent TB: INH for 9 m If resist: Rifampin 6m OR Rifampin+Pyrazinamide 8 w
Active TB: INH+Rifampin+Pyrazinamide+Ethambutol or Streptomycin (initial emp th)
Regimen; 6m; INH + Rifampin + Pyrazinamide (2 m) then INH + Rifampin (4m)
mycobacterium
9 m; INH + Rifampin
TB
Tuberclosis
Preg; INH + Rifampin + Ethambutol
(Mantoux Test)
Breast Feeding; Anti TB D' are safe as only
small conc in milk 2nd line Th; Cycloserine,
Ethionamide, Aminoglycoside
NB: BCG is not generally used In Canada
Lep
ros
Mycobact
Staph Leprae
aureus, g-ve Dapson + Rifampin
y
enterics,
Neonates; gp B strept,
Child; gpA strept,
Cloxacillin + Cefotaxime
Osteomyelitis
Adults; No
NB; Adults, Cloxacillin only
Acute
Diabetic Foot; Imipenem + Cilastatin or Cipro + Clindamycan
Staph aureus, Strept,
g-ve bacilli, anaerobes If DM + HT ; Clinda + Genta for 6w
Imidazole; (top) clotri,
hypersensitivity,
1 in preg used e' caution
eco, mico, tio
local
candida--> cheesy Triazoles;
not used in 1st trimeter
discharge+ pruritis+ terconazole (top)
VVC
inflam pH < 4.5
(all D' have no SE: NVD, abd pain, H, dizz, pruritis, DI: inc INR e' warfarin, inc phenytoin &
established Data in Fluconazole rash, thrombocytopenia, inc theophylline, dec BG e' sulfonylureas,
Lactation) transaminases, hypo K+ dec by Rifampin Preg: CI
PolyeneMacrolide
used in Preg until 6 wks preterm
Nystatin
2
Bacterial
Trichomoni Vaginosi
NVD, abd pain, constipation,
grey/milky dischrge e' heartburn, H diz Vertigo
Clindamycin Used in Preg & Lact
s
odour pH > 4.5 Oral: pseudomembranous colitis
topical; VVC
3 NVD, abd pain, H ataxia Vertigo
pseudomembranous colitis, DI: e' warfarin inc INR, e' alc Disulfuram like
Bact Vag +
Trichomonas-->
asis
purulent discharge e' reaction, e' Disulfuram confusion &
odour, pruritis & inflam Metronidazole VVC, transient leucopenia, mettalic
psychosis, dec e' barb & phenytoin
pH >4.5 partner shd b ttt taste , gynecomastia, dark urine, Preg: used e' caution in 2nd & 3rd tri
photosensitivity
4 Gonococcal by Cephalosporin: Ceftriaxone (inj), Cefixime (oral) Ceftriaxone: Preg e' caution
Cervicitis & Urethritis
Neisseria Quinolones: Cipro, ofloxacin Quinolones: not used in Preg
gonorrhea Spectinomycin (not eff in pharyngeal gonococcal inf) Spect:Preg e' caution (alt for Ceftriaxon)
Doxycycline (bid x 7d) Tetracycline (qid x 7d) CI in Preg
Chlamydial:
Chlamydia Macrolides: Azithro (1gx 1 dose), Preg e' caution, alt for tetracycline
Trachomatis --> erythro (test of cure after 3 wks) used in Preg, L e' caution,
mucopurulent disch Quinolones: Ofloxacin CI in Preg
(opaque/yellow) e'
frequent urination --> Amoxicillin (test of cure after 3 wks)
sterility recent partner ttt used in Preg & L (alt for erythro in 3rd tri)
5 Cephalosporin or Quinolones + Doxycycline or metronidazole
PI
"Shunker dis" D
6 Treponema safe in Preg & Lact
Benzathine Penicillin G: 1ry, 2ry & early latent: once/
Syphilis
Pallidium SE: may cause Jarisch Herxheimer dis in
Late latent x3
2ry Syphilis
recent partner ttt
Tetracycline or Doxycycline or Ceftriaxone
alt in allergy CI in Preg
Erythromycin
Uncomplicated: Co-trimoxazole (if 1st inf--> 3d, Recurrent-->7d,
E coli CI in Renal Failure (not as eff as
complicated 10-14d), Nirofurantoin , Cephalosporins
3d Cotrimoxazole)
Complicated; Ecoli,
10-14d
UTI
Paerogenosa, P flouroquinolones 2nd line due to cost
mirabilis, E. fecalis NB: ttt can be by single dose if cystitis
Pyelonephritis Aminoglycosides Parentral 14d
Acute cystitis;
Amoxicillin / Clav, or Pivmecillinam (Ampicillin)
(urethritis) / Preg
Enterobacteriaceae,
Prostati
Bact Staph aureus,
Cotrimoxazole, floroquinolone, Doxycycline 6 weeks
tis
P
aerogenosa
Enterotoxigenic Ecoli SE: black stool and tongue
Prevention:
CI: e' anticoag, salicylates, allergy
Bi subsalicylate
Traveller's Diarrhea
Campylobacter, to salicylates
salmonella, Shigella
Proph AB as cotrimoxazole & Doxycycline r
Floroquinolone (cipro-nor) used proph in Diplomatic missi not recomm->clstridium difficile assoc diarr
mild: BSS+Antimotility ttt; SE: Toxic megacolon CI: e'
Moderate Loperamide dysentry--> risk of bloody stool & fever
or severe:
Fluids+AB+Antimotility AB: 1. Fquinolones (cipro-nor) eff & safe
2. Doxycycline or Cotrimoxazole
Rehydran (esp infants &
useful if Diar>14hrs & wt loss, steatorrhea, or
preg) or 3. Metronidazole Giardia Lamblia inf
less pref 1tsp salt+ 8tsp
sugar + 1 L h2o
4. Azithromycin not for prophy
Safe in Preg & children
SE; Retinopathy, pigmentation, hearing
Chloroquin & Hydroxychloroquin (alt) loss, seizures, severe
neuropsychological SE
Safe in 2nd half of Preg & children
Mephloquin less severe
neuropsychological SE
Malaria
Anopheline CI in Preg & children (discolor teeth)
No need for dose adj in renal failure
Mosquito Doxycycline 100mg to be taken e' food & avoid sun
bet dusk & dawn exposure (photosensitivity)
CI in Preg
Primaquin (for terminal prophy & radicle cure, for GI upset (to be taken e' food), potent
dormant liver forms; hypnozoids) v eff prophy oxidising agent, induce hemolytic anemia in
No vaccine for malaria those e G-6PD def (shd take enz before ttt)
Malarone (ttt & prophy of chloroquin resist) CI in Preg & children
Fansidar Self ttt regimen when medical care is not av
j
You might also like
- Overlooked 150 Year Old Household Cleaner A Remedy For Swine Flu?Document4 pagesOverlooked 150 Year Old Household Cleaner A Remedy For Swine Flu?nsmith7100% (2)
- Nursing PharmacologyDocument13 pagesNursing PharmacologyRikka Calnea Tabuzo100% (3)
- Lehne Flash CardsDocument73 pagesLehne Flash Cardssarah_stover_1100% (11)
- Moonlighting GuideDocument14 pagesMoonlighting GuideJulienneNo ratings yet
- Pharmacology Reviewer 001Document7 pagesPharmacology Reviewer 001Kath MartinezNo ratings yet
- Muscarine & Nicotinic: ReceptorDocument26 pagesMuscarine & Nicotinic: ReceptorCess Lagera Ybanez88% (16)
- Lymphedema and Lipedema Nutrition Guide: Foods, Vitamins, Minerals, and Supplements - Chuck EhrlichDocument6 pagesLymphedema and Lipedema Nutrition Guide: Foods, Vitamins, Minerals, and Supplements - Chuck EhrlichmafawepyNo ratings yet
- 7 Best Natural Antibiotics - Uses, Evidence, and EffectivenessDocument10 pages7 Best Natural Antibiotics - Uses, Evidence, and Effectivenessbaek2mo340No ratings yet
- AntibioticsDocument9 pagesAntibioticsAudrey Beatrice ReyesNo ratings yet
- PharmacologyDocument93 pagesPharmacologyPh SamerNo ratings yet
- Classification of Antibiotics For PrintingDocument4 pagesClassification of Antibiotics For PrintingMuthu Kumar100% (2)
- (PHA6129 LAB) Terms, Abbreviations, and DefinitionsDocument7 pages(PHA6129 LAB) Terms, Abbreviations, and DefinitionsNotfor TaoNo ratings yet
- Triage, Communucation & Stabilization TLS 2014Document39 pagesTriage, Communucation & Stabilization TLS 2014Makan Budak100% (1)
- Drug of ChoiceDocument16 pagesDrug of ChoiceVicky Vidhata100% (1)
- 2.epidemiology and Diseases TransmissionDocument28 pages2.epidemiology and Diseases TransmissionAnonymous XGE6XwHZNo ratings yet
- Ankylosing SpondylitisDocument21 pagesAnkylosing SpondylitisPaul Kelner100% (2)
- (QUIZ) NEMATODES (2nd Year BS Medical Technology)Document2 pages(QUIZ) NEMATODES (2nd Year BS Medical Technology)avery aerNo ratings yet
- Pathophysiology of Hepatitis BDocument9 pagesPathophysiology of Hepatitis BDianne G Ignacio100% (4)
- Flash Notes Tumor MarkersDocument22 pagesFlash Notes Tumor MarkersschxzerrydawnNo ratings yet
- antiNEOPLASTICmanPrinterFriendly PDFDocument1 pageantiNEOPLASTICmanPrinterFriendly PDFdarla ryanNo ratings yet
- ASTHMA - SemisDocument4 pagesASTHMA - SemisInday BertaNo ratings yet
- AsthmaDocument2 pagesAsthmaNurliyana GhazaliNo ratings yet
- Pharmacology Assignment 2Document3 pagesPharmacology Assignment 2Shamantha Santhana KrishnanNo ratings yet
- Acute Otitis Media Children and AdolescentsDocument1 pageAcute Otitis Media Children and AdolescentsSreya SanilNo ratings yet
- QA Pneumonia Adult For CheckingDocument4 pagesQA Pneumonia Adult For CheckingFatima Kasim MacarongonNo ratings yet
- OPAT Anti-Infective Administration MethodsDocument6 pagesOPAT Anti-Infective Administration MethodsNikki TranNo ratings yet
- Antibiotics: Lecture 6: Antibiotics For Anaerobic InfectionsDocument12 pagesAntibiotics: Lecture 6: Antibiotics For Anaerobic InfectionsMuath AlqarniNo ratings yet
- AGs Lect 09072007Document28 pagesAGs Lect 09072007api-3705123No ratings yet
- Chemotherapy 1Document7 pagesChemotherapy 1VitaliNo ratings yet
- Defibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasDocument4 pagesDefibrillation Is The Definitive Treatment For The Life-Threatening Cardiac ArrhythmiasErika RiceNo ratings yet
- PcolDocument17 pagesPcolThea JulianaNo ratings yet
- Cell Wall SynthesisDocument7 pagesCell Wall SynthesisKC PalattaoNo ratings yet
- PRONE Position Wheezing Chest Retractions Grunt: - Chocking - Hacking/Barking Cough-Worse at NightDocument3 pagesPRONE Position Wheezing Chest Retractions Grunt: - Chocking - Hacking/Barking Cough-Worse at NightEben Ezar Dela CruzNo ratings yet
- MedimapDocument2 pagesMedimapKristian Dave DivaNo ratings yet
- Laboratory Animal Compilation Mid TermDocument6 pagesLaboratory Animal Compilation Mid TermWenn Marc Catuiran DuceNo ratings yet
- Drugs For AsthmaDocument1 pageDrugs For Asthmakamil malikNo ratings yet
- Comprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference TipsDocument3 pagesComprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference Tipshyukkie minnieNo ratings yet
- Antibiotics NoWatermarkpdfDocument2 pagesAntibiotics NoWatermarkpdfduy luuNo ratings yet
- Bronchial Asthma (1) SKDocument24 pagesBronchial Asthma (1) SKSafoora RafeeqNo ratings yet
- Aminoglycoside & Macrolide Antibiotics Classification:: Systemic AminoglycosidesDocument5 pagesAminoglycoside & Macrolide Antibiotics Classification:: Systemic AminoglycosidesSai VamshiNo ratings yet
- Salicylates Propionic Acid Derivatives Indole Acetic Acid Phenylacet Ic Acid Derivatives Oxicam Acetaminoph enDocument4 pagesSalicylates Propionic Acid Derivatives Indole Acetic Acid Phenylacet Ic Acid Derivatives Oxicam Acetaminoph enLana AmerieNo ratings yet
- Name of Drug Classificatio N Mechanism of Action Indications Contraindication S Adverse Effects Side EffectsDocument7 pagesName of Drug Classificatio N Mechanism of Action Indications Contraindication S Adverse Effects Side EffectsHilario. Hayascent.Reign.M.No ratings yet
- Emergency DrugsDocument2 pagesEmergency DrugssapphiresamNo ratings yet
- Pulmonary Edema: Mycobacterium Tuberculosis Patient BackgroundDocument1 pagePulmonary Edema: Mycobacterium Tuberculosis Patient BackgroundAubrey RecierdoNo ratings yet
- Antibiotic/Antiviral Policy - Paediatric PCF (EWMSCDocument9 pagesAntibiotic/Antiviral Policy - Paediatric PCF (EWMSCLizbet parrondoNo ratings yet
- Revision Tables - 270820162807Document105 pagesRevision Tables - 270820162807flickers xxxNo ratings yet
- Oncology Cheat Sheets - 1Document5 pagesOncology Cheat Sheets - 1abdallahmaurice94No ratings yet
- Compare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDocument2 pagesCompare and Contrast Atropine and Glycopyrulate, and Discuss The Clinical ImplicationsDonkeyManNo ratings yet
- RespDisord (PART B & C)Document4 pagesRespDisord (PART B & C)GraceNo ratings yet
- WK 01 - PneumoniaDocument1 pageWK 01 - PneumoniablackswallowNo ratings yet
- FECAVA Recommendations For Appropriate Antimicrobial TherapyDocument1 pageFECAVA Recommendations For Appropriate Antimicrobial Therapyমুহাম্মাদ রিদুয়ান পাশাNo ratings yet
- CPAMSDocument7 pagesCPAMSDominic chuaNo ratings yet
- Summary of Pharmacology1 by 3alam El Teb DR - MahmoudDocument41 pagesSummary of Pharmacology1 by 3alam El Teb DR - MahmoudaamirNo ratings yet
- AcetylcysteineDocument2 pagesAcetylcysteineTINAYNo ratings yet
- Ascp AceDocument67 pagesAscp AceJohn Dale DuranoNo ratings yet
- Friday, March 3 2023: 1 PatientDocument15 pagesFriday, March 3 2023: 1 PatientbobbyNo ratings yet
- Ponr 2Document18 pagesPonr 2PAUL MICHAEL G. BAGUHINNo ratings yet
- HSB Pneumonia Antibiotic AlgorithmDocument4 pagesHSB Pneumonia Antibiotic AlgorithmDr.Senthil KumarNo ratings yet
- Standard Luminal AmoebicidesDocument2 pagesStandard Luminal AmoebicidesPrince Kevin AdinaNo ratings yet
- Bacteria Summary TableDocument10 pagesBacteria Summary TableNur Alia YasminNo ratings yet
- Antifungal Agents: EchinocandinsDocument2 pagesAntifungal Agents: EchinocandinsCourtney TownsendNo ratings yet
- Drugs Pharmacokinetics Indications Contraindicatio N Interaction Adverse Effects Generic NameDocument1 pageDrugs Pharmacokinetics Indications Contraindicatio N Interaction Adverse Effects Generic NameJR BetonioNo ratings yet
- Respirology Division, Department of Child Health, Udayana University Medical School/Sanglah Hospital, DenpasarDocument59 pagesRespirology Division, Department of Child Health, Udayana University Medical School/Sanglah Hospital, DenpasarWita FitriyaniNo ratings yet
- HelminthsDocument11 pagesHelminthsTienneNo ratings yet
- Dialog HIVDocument5 pagesDialog HIVVadiLa ZaLfaNo ratings yet
- Final Meq Ss OncoDocument10 pagesFinal Meq Ss OncoRoadtogot 2023No ratings yet
- Rhomboid Flap For Pilonidal Sinus - Our ExperienceDocument5 pagesRhomboid Flap For Pilonidal Sinus - Our ExperienceKhalidHussainNo ratings yet
- What Is ScabiesDocument7 pagesWhat Is ScabiesKenNo ratings yet
- Body Mass Index Percentiles For Boys and Girls From 5-17 YearsDocument1 pageBody Mass Index Percentiles For Boys and Girls From 5-17 YearsadadanNo ratings yet
- Consumer World Amr Awareness Week 2023 Power Point PresentationDocument29 pagesConsumer World Amr Awareness Week 2023 Power Point PresentationSoha GalalNo ratings yet
- Journal of Dentistry and Oral SciencesDocument19 pagesJournal of Dentistry and Oral SciencesNadya PuspitaNo ratings yet
- Kanker ParuDocument10 pagesKanker Parunovi hidayahNo ratings yet
- 8 Important Facts About The COVID-19 Vaccine BoosterDocument1 page8 Important Facts About The COVID-19 Vaccine BoosterMT DevoteeNo ratings yet
- Infectious and Non-Infectious DiseasesDocument2 pagesInfectious and Non-Infectious DiseasesJanice ChingNo ratings yet
- Systemic Lupus Erythematosus - Immunity PDFDocument7 pagesSystemic Lupus Erythematosus - Immunity PDFTõkå MøhámmêdNo ratings yet
- A Case Presentation On PneumoniaDocument74 pagesA Case Presentation On PneumoniaYengkhom YoshiNo ratings yet
- Renr Review Ras Practice Test 30Document23 pagesRenr Review Ras Practice Test 30arkelliaNo ratings yet
- YÖKDİL Sağlık Cümle Tamamlama Soru TipiDocument7 pagesYÖKDİL Sağlık Cümle Tamamlama Soru Tipi6z4fhrvq5kNo ratings yet
- Materi Dr. Vinod BuraDocument24 pagesMateri Dr. Vinod BuraDiah FitriahNo ratings yet
- Nursing Care Plan: Milagrosa Candida V. Caburnay, RN, MNDocument6 pagesNursing Care Plan: Milagrosa Candida V. Caburnay, RN, MNArvin LazarteNo ratings yet
- What Current Events Have Greatly Influenced Tourism in The PhilippinesDocument2 pagesWhat Current Events Have Greatly Influenced Tourism in The PhilippinesMiley HartHartNo ratings yet
- Tubal Ligation and Salpingectomy and The Risk of Epithelial Ovarian CancerDocument6 pagesTubal Ligation and Salpingectomy and The Risk of Epithelial Ovarian CancerAlyssa MarzanNo ratings yet
- Gingiva Diseases Of89Document3 pagesGingiva Diseases Of89محمد العراقيNo ratings yet
- RUNDOWN West Borneo Cardiovascular Annual Meeting (WeBCAM) 2023Document3 pagesRUNDOWN West Borneo Cardiovascular Annual Meeting (WeBCAM) 2023Bayu Zeva WirasaktiNo ratings yet
- Nurse Np1 Board CramsheetDocument8 pagesNurse Np1 Board CramsheetZero TwoNo ratings yet
- 03 Pengkajian LukaDocument30 pages03 Pengkajian LukaRajaRafianNo ratings yet
- 4.22 - Quiz LeprosyDocument32 pages4.22 - Quiz LeprosyEdo LiawandiNo ratings yet