Professional Documents
Culture Documents
Pulmonary Embolism
Uploaded by
MaNiaaa LoxOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pulmonary Embolism
Uploaded by
MaNiaaa LoxOCopyright:
Available Formats
AUGUST 2023 | VOLUME 25 | ISSUE 8
Emergency Medicine Practice Evidence-Based Education • Practical Application
CLINICAL CHALLENGES:
• What are the clinical risk factors
for pulmonary embolism?
• How are patients assessed
for probability of pulmonary
embolism?
• What are the highest-value
diagnostic tests for detecting a
pulmonary embolism?
Authors
Alfred Sacchetti, MD, FACEP
Director of Clinical Services, Emergency
Department, Virtua Our Lady of Lourdes
Hospital, Camden, NJ; Assistant Clinical
Professor of Emergency Medicine, Thomas
Jefferson University, Philadelphia, PA
Michael Driscoll, DO, FACOI, FCCP
Attending Physician, Department of Medicine, Evidence-Based
Section of Pulmonary and Critical Care, Virtua
Our Lady of Lourdes Medical Center, Camden, Management of
Pulmonary Embolism in
NJ
Peer Reviewers the Emergency Department
Mark Andreae, MD
Assistant Professor of Surgery and Emergency
Medicine, Institute for Critical Care Medicine, n Abstract
Icahn School of Medicine at Mount Sinai, New Patients with pulmonary emboli present both diagnostic and
York, NY therapeutic challenges to the emergency clinician, because
Christopher Willoughby, MD, initial symptoms can be variable and overlap with other medical
FAAEM conditions. This issue reviews treatment options for patients
Assistant Professor of Clinical Medicine, with pulmonary emboli based on risk stratification scores of low,
Department of Emergency Medicine, Louisiana intermediate-low, intermediate-high, and high risk classifications.
State University Health Sciences Center New
The evidence on laboratory testing and imaging is presented,
Orleans, New Orleans, LA
as well as treatment strategies that include anticoagulation,
thrombolytics, and mechanical or surgical thrombectomy.
Management decisions regarding pregnancy and COVID-19 are
Prior to beginning this activity, see “CME discussed, as well as considerations for outpatient treatment of
Information” on page 2. low-risk patients.
For online For mobile
access: app access:
This issue is eligible for CME credit. See page 2. EBMEDICINE.NET
CME Information
Date of Original Release: August 1, 2023. Date of most recent review: July 10, 2023. Termination date: August 1, 2026.
Accreditation: EB Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide
continuing medical education for physicians.
Credit Designation: EB Medicine designates this enduring material for a maximum of 4 AMA PRA Category 1 CreditsTM. Physi-
cians should claim only the credit commensurate with the extent of their participation in the activity.
Specialty CME: Not applicable. For more information, contact Customer Service at 678-366-7933.
ACEP Accreditation: Emergency Medicine Practice is approved by the American College of Emergency Physicians for 48 hours of ACEP Cat-
egory I credit per annual subscription.
AAFP Accreditation: The AAFP has reviewed Emergency Medicine Practice, and deemed it acceptable for AAFP credit. Term of approval is from
07/01/2023 to 06/30/2024. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This session,
Evidence-Based Management of Pulmonary Embolism in the Emergency Department is approved for 4.0 enduring material AAFP Prescribed
credits.
AOA Accreditation: Emergency Medicine Practice is eligible for 4 Category 2-B credit hours per issue by the American Osteopathic Association.
Needs Assessment: The need for this educational activity was determined by a practice gap analysis; a survey of medical staff, including the
editorial board of this publication; review of morbidity and mortality data from the CDC, AHA, NCHS, and ACEP; and evaluation responses from
prior educational activities for emergency physicians.
Target Audience: This enduring material is designed for emergency medicine physicians, physician assistants, nurse practitioners, and residents.
Goals: Upon completion of this activity, you should be able to: (1) identify areas in practice that require modification to be consistent with current
evidence in order to improve competence and performance; (2) develop strategies to accurately diagnose and treat both common and critical ED
presentations; and (3) demonstrate informed medical decision-making based on the strongest clinical evidence.
CME Objectives: Upon completion of this activity readers will be able to: (1) identify the risks of a pulmonary embolism based on a patient's
clinical presentation; (2) select appropriate diagnostic studies to identify the presence of a pulmonary embolism; (3) select appropriate diagnostic
studies to determine the severity of the patient’s condition; and (4) develop a management approach based on the clinical and diagnostic charac-
teristics of the patient.
Discussion of Investigational Information: As part of the activity, faculty may be presenting investigational information about pharmaceutical
products that is outside Food and Drug Administration approved labeling. Information presented as part of this activity is intended solely as
continuing medical education and is not intended to promote off-label use of any pharmaceutical product.
Disclosure: It is the policy of EB Medicine to ensure objectivity, balance, independence, transparency, and scientific rigor in all CME activities.
All individuals in a position to control content have disclosed all financial relationships with ACCME-defined ineligible companies. EB Medicine
has assessed all relationships with ineligible companies disclosed, identified those financial relationships deemed relevant, and appropriately
mitigated all relevant financial relationships based on each individual’s role(s). Please find disclosure information for this activity below:
Planners Faculty
• Daniel J. Egan, MD (Course Director): Nothing to Disclose • Alfred Sacchetti, MD (Author): Nothing to Disclose
• Andy Jagoda, MD (Editor-in-Chief): • Michael Driscoll, DO (Author): Nothing to Disclose
l Pfizer (Consultant/Advisor) • Mark Andreae, MD (Peer Reviewer): Nothing to Disclose
l Janssen (Consultant/Advisor) • Christopher Willoughby, MD (Peer Reviewer): Nothing to Disclose
l Abbott Laboratories (Consultant/Advisor) • Aimee Mishler, PharmD (Pharmacology Editor): Nothing to Disclose
• Kaushal Shah, MD (Associate Editor-in-Chief): Nothing to Disclose • Joseph D. Toscano, MD (Research Editor): Nothing to Disclose
• Dorothy Whisenhunt, MS (Content Editor): Nothing to Disclose
• Cheryl Belton, PhD (Content Editor): Nothing to Disclose
Commercial Support: This issue of Emergency Medicine Practice did not receive any commercial support.
Earning CME Credit: Go online to https://www.ebmedicine.net/CME and click on the title of the test you wish to take. When completed, a CME
certificate will be emailed to you.
Additional Policies: For additional policies, including our statement of conflict of interest, source of funding, statement of informed consent, and
statement of human and animal rights, visit https://www.ebmedicine.net/policies
CEO: Stephanie Williford
Director of Finance & Analytics: Robin Wilkinson
Publisher: Suzanne Verity
Director of Editorial Quality: Dorothy Whisenhunt, MS
Senior Content Editor: Cheryl Belton, PhD, ELS
Direct all inquiries to: Managing Editor: Angie Wallace
Phone: 678-366-7933 CME & Content Coordinator: Kristen Raynor, MEd
Fax: 770-500-1316 Education Coordinator: Kandis Slater
5600 Spalding Drive, Unit 921697 Customer Service Representative: Katie Resumovic
Norcross, GA 30010-1697 Account Executive: Dana Stenzel
Director of Marketing: Anna Motuz, MBA
E-mail: ebm@ebmedicine.net Email Marketing Specialist: Joshua Devou, MBA
Website: www.ebmedicine.net Marketing Specialist: Valerie Yuhouse
Database Administrator: Jose Porras
ISSN info and disclaimer:
Emergency Medicine Practice (ISSN Print: 1524-1971, ISSN Online: 1559-3908, ACID-FREE) is published monthly (12 times per year) by EB Medicine
(5600 Spalding Drive, Unit 921697, Norcross, GA 30010-1697). Opinions expressed are not necessarily those of this publication. Mention of products
or services does not constitute endorsement. This publication is intended as a general guide and is intended to supplement, rather than substitute,
professional judgment. It covers a highly technical and complex subject and should not be used for making specific medical decisions. The materials
contained herein are not intended to establish policy, procedure, or standard of care. Copyright © 2023 EB Medicine. All rights reserved. No part of
this publication may be reproduced in any format without written consent of EB Medicine. This publication is intended for the use of the individual
subscriber only and may not be copied in whole or part or redistributed in any way without the publisher’s prior written permission.
AUGUST 2023 • www.ebmedicine.net 2 ©2023 EB MEDICINE
Case Presentations
An obese 55-year-old man reports exertional dyspnea that began 2 days prior…
• The man says he is generally active, despite being obese, and says that he walks extensively for his job.
CASE 1
• His ECG is normal sinus rhythm at 95 beats/min and his resting pulse oximetry is at 94%. There are no
other abnormalities. Chest x-ray, natriuretic peptide, and high-sensitivity troponin are normal.
• All of his symptoms can be explained by his weight, but you wonder whether you should start down a
diagnostic pulmonary embolism algorithm...
A 65-year-old woman presents with a complaint of shortness of breath she developed that morning…
• She says she recently recovered from COVID-19 disease and was doing well prior.
CASE 2
• On examination, her lungs have a few residual ronchi from her illness, but are otherwise clear. Vital signs
are normal, and her pulse oximetry is 97% on room air. As part of her workup, a D-dimer is ordered and
returns incalculably high. She has a well-documented IV contrast allergy. A pulmonary perfusion scan
was ordered, which shows a clear perfusion defect consistent with a pulmonary embolism.
• You consider whether this patient is a candidate for outpatient treatment and which medications to use...
A 60-year-old woman presents in extremis via basic EMS…
• She was recently released from the hospital following a 1-week hospitalization for COVID-19 disease,
during which she was placed on low-molecular-weight heparin (LMWH). She stopped the LMWH 4 days
CASE 3
prior. She said she developed severe shortness of breath about 1 hour ago when she stood up from a
recliner she had been resting in.
• On arrival to the ED, she was cyanotic, tachypneic, tachycardic, and verbalizing “I can’t breathe”
repeatedly. Initial pulse oximetry was 70%, with a sinus tachycardia of 130 beats/min and a blood
pressure of 84/40 mm Hg.
• Does this patient require endotracheal intubation, and should thrombolytics be started immediately?
n Introduction n Critical Appraisal of the Literature
The presentation of patients with pulmonary emboli A literature search was performed using multiple
ranges from the patently obvious to the extremely databases including PubMed, Google Scholar,
subtle. Clinical outcomes may seem, at times, to defy Emergency Medical Abstracts, MEDLINE®, and the
any physiologic management. Patients with massive Cochrane Database of Systematic Reviews, with
clot burden may survive with no complications follow- no time criteria. Search terms included pulmonary
ing minimal interventions while others with relatively embolism with the following subtitles: diagnosis,
minor emboli may die despite aggressive care. laboratory, radiography, ultrasound, physical
Venous thromboembolism (VTE) is among the examination, risk factors, stratification, thrombolysis,
most lethal of all acute medical conditions. Un- anticoagulation, and invasive, with no restrictions on
treated VTE has an acute mortality of 25%, which can the type of article. Over 500 articles were identified,
decrease to 5% with timely medical management. of which 141 were selected. A large number of
Nonetheless, even with appropriate care, approxi- descriptive studies were identified, along with
mately 15% to 30% of patients who are treated for a anecdotal therapeutic reports. High-quality subject
pulmonary embolism will die within 90 days.1-3 The reviews with evidence-based recommendations on
cause of death may not be the pulmonary embolism diagnostic and therapeutic approaches to pulmonary
itself, but the underlying medical pathology that led embolism, along with specialty society guidelines and
to the offending clot. Misdiagnosis of patients who policy and procedures were also reviewed, and 99
were discharged from the ED but were ultimately were identified for inclusion in this manuscript.
diagnosed with pulmonary emboli occurs in 11.9% to
19% of cases,4 and pulmonary embolism remains the
third most common cause of death from cardiovascu- n Etiology and Pathophysiology
lar causes. This issue of Emergency Medicine Practice Clot formation occurs continuously in the venous sys-
presents an emergency medicine approach to the tems of the body. These clots tend to be very small,
diagnosis, treatment, and disposition of patients with and they are broken down by the action of circulat-
pulmonary emboli. ing enzymes, most prominently, plasmin. Pathologic
AUGUST 2023 • www.ebmedicine.net 3 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
deep vein thrombi may be described as venous clots latory system, pulmonary emboli activate the clot-
that do not resolve spontaneously but instead propa- ting cascade, damage the endothelium, and lead to
gate, resulting in obstruction or migration. The most localized blood stagnation. The presence of a fresh
common conditions leading to venous thrombus clot in the pulmonary arteries leads to the release of
formation were described by Virchow, in which he a number of vasoactive chemicals that contribute to
listed in his triad of (1) vessel wall injury, (2) venous pulmonary hypertension. Most prominent of these are
stasis, and (3) hypercoagulability. Vessel wall injuries the endothelins: serotonin, thromboxane A2, adenos-
denude the endothelium, leading to exposure of the ine, and multiple prostaglandins, along with other
underlying thrombogenic media layers of the vessel. small molecules. The presence of these agents leads
Venous stasis leads to thrombus formation in the cusp to competing actions of vasoconstriction and vasodi-
of the venous valves, where prolonged contact with lation in the pulmonary arteries; however, the overall
platelets allows for activation of other components of effect is strongly weighted toward vasoconstric-
the clotting cascade. Hypercoagulability may result tion. Because of the soluble nature of these agents,
from inborn errors in the coagulation cascade, the vasoactive effects occur in both the embolized and
presence of mucus-secreting tumors, or iatrogenic nonembolized portions of the lungs.1,3,6 Pulmonary
thrombotic medications or devices.3,5 infarctions may occur in 16% to 31% of patients with
Once formed, venous clots can follow 1 of 3 pulmonary emboli.2,7
pathways. First, they may be lysed by the body’s Pulmonary emboli do not occur as isolated
normal thrombolytic processes. Second, they may events. Frequently, more than one embolism will
propagate and become larger, leading to further occur in any given patient. It is often said that it is
clot formation and obstruction in the affected vessel. not the pulmonary embolism you diagnose that kills
Finally, they may break free and migrate to a more the patient, but the subsequent ones that originate
proximal portion of the venous tree, including the from the offending clot source. Although not proven,
lungs. By definition, any material migrating to the it may be that the pulmonary vasculature has been
pulmonary arterial system is termed a pulmonary primed by the initial clot and the second offending
embolism, including air, amniotic fluid, and foreign clot is able to exert a larger vasoactive effect, which
bodies, although blood clots are, by far, the most leads to the cardiovascular collapse.
common source of pulmonary emboli and will be the
focus of this discussion. Risk Factors for Pulmonary Emboli
When an embolism lodges in the pulmonary Most of the risk factors for pulmonary emboli are
vascular tree, it produces a cascade of mechanical similar to risk factors for the formation of deep
and chemical reactions. Prominent among the venous thrombi, although they are not identical.8 Any
mechanical reactions is obstruction of flow to the circumstances that lead to venous stasis, particularly
portions of the lung distal to where the embolus is in the lower extremities, are considered risk factors
embedded. A decrease in the available surface area for a pulmonary emboli. Extended bed rest of any
for exchange of oxygen and carbon dioxide occurs duration places patients at risk for development of
in alveoli supplied by that portion of the pulmonary deep vein thrombosis (DVT). With limited activity,
arterial circulation. If the clot is large enough, even young patients can develop clots in the
pulmonary hypertension may result. The right lower extremities. Compression devices, as well as
ventricle is anatomically and physiologically designed anticoagulants, can limit the formation of thrombi.
to pump blood into a low-pressure system, and acute However, clinicians should still consider the possibility
pulmonary hypertension leads to right ventricular of a blood clot in patients despite the use of DVT
dilation and pulmonary vascular congestion. This prophylaxis or treatments.
may translate to depressed blood flow from both Direct trauma to an extremity, even without
the superior and inferior vena cavas through the creation of a fracture, produces soft-tissue edema and
tricuspid valve. As right ventricular pressures increase, micro-clots. If severe enough, such clotting can lead
displacement of the intraventricular septum into the to propagation and DVT.8
left ventricle occurs, affecting left ventricular function Proximal obstruction to blood flow through a
as well. The mechanical obstruction of the pulmonary vein can lead to stasis and clot formation. Pathologic
circulation will decrease pulmonary venous return to masses such as tumors, excessive adipose tissue, and
the left side of the heart. If significant enough, this indwelling foreign bodies such as vascular devices
leads to physiologic hypovolemia and shock. Right can all serve as a nidus for clot formation. The clots
ventricular dysfunction secondary to clot mass does distal to the offending source of obstruction generally
not occur until approximately 50% of the pulmonary do not migrate to the lungs, as they are blocked by
vascular tree is embolized.3,6 the obstruction. However, these clots can serve as the
Compounding these problems is the ability of nidus that allows propagation of a clot more proxi-
fresh emboli to propagate within the pulmonary mally, which can then embolize to the lungs.1,2
circulation itself. As with clots anywhere in the circu- Hypercoagulable states are independent risk
AUGUST 2023 • www.ebmedicine.net 4 ©2023 EB MEDICINE
factors for thromboembolic events. Cancer of any emboli are helpful in excluding other diagnoses in
type is a risk factor for pulmonary embolism, account- their differential.
ing for up to 66.7% of deaths in oncology patients.9 Patients with primary cardiovascular presenta-
All tumors place patients at risk for thromboembolic tions including chest pain, shortness of breath, and
events, but those that contain mucinous secreting hemoptysis will commonly be considered for the
cells are the most common.8,10,11 Pancreatic, colonic, possibility of pulmonary emboli. Patients with non-
and lung are the most common of these types of can- pulmonary presentations including syncope, weak-
cers. Cancer patients with pulmonary emboli can also ness, malaise, and other nonspecific complaints may
present differently from those without cancer. Overall, also be considered for pulmonary emboli, depending
they are older, with an average age 64 years versus on the clinical circumstances involved. Underlying
58 years of age, and they are less likely to present conditions such as COPD, congestive heart failure,
with chest pain, 18% versus 37%.12 and other chronic conditions should increase the clini-
Hypercoagulable states related to genetic fac- cians’ suspicion for this disease. Syncope in conjunc-
tors can occur in up to 30% of VTE patients. The vast tion with other risk factors may lead to the consider-
majority of these abnormalities are related to factor V ation of pulmonary emboli, although isolated syn-
Leiden and prothrombin G2021A mutations. Patients cope with no other associated symptoms suggestive
may be heterozygous or homozygous for the abnor- of a pulmonary embolism is not an indication for an
mal enzymes and vary in their severity for the forma- evaluation for thromboembolic disease. A prospec-
tion of pathologic clots.10 tive study of 1380 syncope patients found a pulmo-
General anesthesia is an independent risk factor nary embolism at presentation in only 19 patients.15
for thrombus formation. Patients with a history A retrospective cohort study of 224 patients found a
of recent surgery, even procedures not involving pulmonary embolism in 22 patients; however, all had
the lower extremities, have a lower threshold for classic signs and symptoms of the disease.16
abnormal clotting.1 Misdiagnosis of patients discharged from the
In the Prospective Investigation of Pulmonary ED but ultimately diagnosed with pulmonary emboli
Embolism Diagnosis II (PIOPED II) study, the most occurs in 11.9% to 19% of pulmonary embolism
common risk factors found included: female sex (58% patients. A delayed diagnosis in patients admitted to
of patients), followed by immobilization (25%), recent the hospital can be as high as 21.5%.4 Patients with
surgery (21%), malignancy (19%), and travel >4 hours pulmonary emboli missed on their initial ED visits
in the previous month (12%).13,14 Table 1 lists com- tended to be older, 77.5 years of age versus 67 years
mon risk factors for pulmonary emboli. of age; have less dyspnea, 45.5% versus 59.9%; less
chest pain, 18% versus 49.5%; and more nonspecific
symptoms, 29.5% versus 8.8%. Morbidity and
n Differential Diagnosis mortality can be as high as 30% to 43% in patients
Based on the clinical presentation of patients with with a missed pulmonary embolism diagnosis,
pulmonary emboli, the differential diagnosis is quite compared to 1.6% in those diagnosed initially.17
extensive. Certainly, myocardial ischemia should be
considered in patients with chest pain. In addition,
primary pulmonary pathology including chronic n Prehospital Care
obstructive pulmonary disease (COPD), asthma, For patients who have complaints suggestive of pul-
pneumonia, pneumothorax, and pleuritis all need to monary embolism and are transported by an emergen-
be considered. Fortunately, many of the diagnostic cy medical services (EMS) system, standard prehospital
studies used to evaluate patients for pulmonary chest pain or shortness of breath protocols are ap-
propriate. There is little that traditional prehospital
intervention has to offer pulmonary embolism patients
aside from supplemental oxygen and cardiac monitor-
Table 1. Clinical Risk Factors for ing. Airway interventions and positive-pressure ventila-
Pulmonary Embolism1,13,14 tion have significant physiologic effects on patients
• Female sex/estrogen therapy with large pulmonary emboli and should be used
• Prolonged immobility (≥3 days) according to prevailing EMS protocols for patients with
• General anesthesia/recent surgery
• Cancer
hypoxia and/or respiratory distress.
• Travel ≥4 hours
• Major trauma/fracture
• Pacemaker placement n Emergency Department Evaluation
• Venous catheterization History
• Obesity
• Antiphospholipid syndrome
Most patients with pulmonary emboli will present
• Chronic inflammatory disorders with complaints of either dyspnea or chest pain. For
• Heparin-induced thrombocytopenia those presenting with dyspnea, the time of onset and
AUGUST 2023 • www.ebmedicine.net 5 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
duration of symptoms can help distinguish pulmonary characterized.13 Pleuritic chest pain was found in 35%
embolism-related dyspnea from that of congestive to 46% of these patients, while non–pleuritic pain was
heart failure, pneumonia, and COPD. present in 18% to 20%.13 Other studies found similar
Data from the PIOPED II study found that dyspnea results when signs, symptoms, and risk factors were
is the most common presenting symptom for patients examined.14,21
with a pulmonary embolism, occurring in 79% of indi- There is variability in presentations according
viduals. Dyspnea at rest occurred in 61% of patients, to patients’ age. Patients aged <65 and >85 years
while dyspnea only with exertion was found in 13% to presented with a similar frequency of dyspnea,
18%. In 41%, the onset of dyspnea was rapid; in most occurring in 77% and 74%, respectively. However,
cases occurring within seconds, and within minutes chest pain showed a significant age difference, being
in another 26%.13 Similarly, patients with chest pain present in 60% of those aged <65 years but in only
should be asked for a description of their symptom 31% of those aged >85 years. Tachycardia was found
characteristics. In the same PIOPED II study, pleuritic in 19% of those aged <65 years but in 11.4% in those
chest pain occurred in 47% of patients, with non–pleu- aged >85 years. Other clinical signs and symptoms
ritic chest pain in another 17%.13 were similar in both the younger and older patients.21
If pulmonary embolism is considered high on Visual cyanosis reinforces the impression of
the differential, ask specifically about lower extremity severe dyspnea, regardless of etiology. The presence
symptoms, as swelling or pain in the legs may be of 3 to 5 g/dL of deoxygenated hemoglobin is
present in 39% to 42% of patients.13 Asking specific generally enough to produce a bluish discoloration of
questions concerning the risk factors listed in Table 1 the skin.22 In a person with normal hemoglobin levels,
(page 5) can also help establish or refute a pulmonary cyanosis will appear at a pulse oximetry reading of
embolism as the source of a patient’s symptoms. approximately 85%.22 Pulse oximetry can indicate
unrecognized hypoxemia; however, the degree
Physical Examination of hypoxemia is extremely variable and does not
Vital Signs correlate with the clot load in the pulmonary vascular
From a clinical perspective, the most important tree. An oxygen saturation of <90% has only a 32%
point to remember regarding the ED presentation sensitivity for the diagnosis of pulmonary embolism.
of pulmonary embolism patients is that vital signs However, pulse oximetry does correlate with short-
are often normal. According to PIOPED II, the most term mortality, with a death rate of 16.7% for patients
common vital sign abnormalities in patients with with baseline pulse oximetry <88% compared to 4.8%
pulmonary embolism were tachypnea (52%-57%) and for those with pulse oximetry ≥88%.19 Part of this
tachycardia (21%-28%).13 A resting heart rate of >100 variability stems from the ability of even small clots
beats/min occurred in 26% of patients in the PIOPED to induce significant shunting and vasoconstriction. A
II study.13 A normal heart rate does not eliminate low pulse oximetry reading should raise concern for
the possibility of a thromboembolic event, nor does a possible pulmonary embolism; however, a normal
reversion of an elevated heart rate to normal, which reading should not reassure a clinician that the
may be seen in 18% of patients.18 disease does not exist.
Abnormal respiratory rates are less predictive Auscultation of the lungs is helpful in identifying
of pulmonary emboli, although at the extreme, it other pathology rather than confirming a pulmonary
is predictive of severe disease. Respiratory rates embolism. In the PIOPED II study, rales were found in
>30 breaths/min demonstrated a sensitivity of 43% 21% of patients, wheezing in 6%, and ronchi in 5%.13
and a specificity of 69% for pulmonary embolism- Splinting secondary to nontraumatic chest pain
related deaths. Tachypnea with a respiratory rate indicates some form of pleuritic or musculoskeletal
>20 breaths/min was found in 57% of patients in the irritation as the source of pain, but is not specific
PIOPED II study.13,19 to pulmonary emboli, occurring in only 17% of
Hypotension is the least specific vital sign, oc- patients.13,23 If the pleural inflammation is secondary
curring in 5% of pulmonary embolism patients. Intui- to an infarction of the lung, it will generally take
tively, it would seem that the size of the clot burden time to develop and will not be useful as an acute
would correlate with the presence of hypotension. screening finding.
However, because of the vasoactive actions of the Jugular venous distention can be seen in up to
clots in the pulmonary circulation, even small clots 11% of pulmonary embolism patients but can occur in
can produce hypotension. Conversely, large clots other disease states such as congestive heart failure,
may have no impact on blood pressure.20 primary pulmonary hypertension, and right-sided
valvular disease.13,23
Other Physical Examination Findings Lower extremity edema, swelling, or tenderness
In 22% of patients with pulmonary embolism, are common findings in DVT. Since lower extrem-
abnormalities in the cardiac examination can be ity veins are the most common source of pulmonary
found, but aside from tachycardia, they are not easily emboli, there is a strong association between physical
AUGUST 2023 • www.ebmedicine.net 6 ©2023 EB MEDICINE
findings of DVT and pulmonary embolism, and it may utilized to determine the need for further diagnostic
be seen in up to 39% to 56% of patients. However, testing. These clinical probability scoring systems
the absence of lower extremity clots does not exclude are not the same as the outcome and management
a pulmonary clot. Regardless, it is important to in- scoring systems discussed in ”Risk Stratification
clude a lower extremity examination in the evaluation Categorization“ section, on page 11.
of patients with suspected pulmonary embolism.24
Migration of venous thrombi from the upper
Online calculators for these scores are
extremities to the lungs is much less common,
available at www.MDCalc.com
occurring in <4.8% of cases. The diagnosis of upper
• Wells’ Criteria for Pulmonary
extremity DVT includes internal jugular and subclavian
Embolism: www.mdcalc.com/calc/115/
clots and is not restricted to just the arms.24
wells-criteria-pulmonary-embolism
• Geneva Score (Revised) for Pulmonary
Diagnostic Risk Scoring Systems
Embolism: www.mdcalc.com/calc/1750/
No single sign or symptom is completely reliable in
geneva-score-revised-pulmonary-embolism
confirming or excluding the diagnosis of pulmonary
• PERC Rule for Pulmonary Embolism: www.
embolism. Clinical gestalt alone demonstrates poor
mdcalc.com/calc/347/perc-rule-pulmonary-
performance in excluding the need for further testing
embolism
in potential pulmonary embolism patients, with a
• YEARS Algorithm for Pulmonary Embolism
kappa between clinicians examining the same patient
(including adaptation for pregnant patients):
as low as 0.33.25,26 To compensate for this problem,
www.mdcalc.com/calc/4067/years-algorithm-
different components of patient presentations and
for-pulmonary-embolism-pe
diagnostics have been combined into pulmonary
embolism scoring systems to generate clinical
pretest probabilities. Table 2 contains a summary
of different validated clinical pretest probabilities n Diagnostic Studies
scoring systems. Although there are minor variations Because of the variable clinical presentations in
among systems, in general, all of them divide patients with pulmonary emboli, diagnostic studies
the risk for pulmonary embolism into low (5%- play a major role in the diagnosis of this disease. Any
10%), intermediate (25%-30%) or high (60%-65%) diagnostic studies used to evaluate for a pulmonary
probabilities. The clinical risk categorization is then embolism must be interpreted in conjunction with
Table 2. Clinical Pretest Probability Scoring Systems
Criteria Scoring System
Wells rGeneva PERC YEARS
Age (years) >65: 1 ≥50: 1
Surgery or immobilization within the past 4 weeks 1.5 2 1
Cancer 1 2
Previously diagnosed PE or DVT 1.5 3 1
Hormonal estrogenic treatment 1
Hemoptysis 1 2 1 1
Clinical signs of DVT 3 1
Unilateral lower limb pain 3
Pain on lower limb deep vein palpation and unilateral edema 4 1
Heart rate (beats/min) >100: 1.5 75-94: 3 ≥100: 1
≥95: 5
Pulse oxygen saturation <95% 1
PE is #1 diagnosis or equally likely 3 1
Clinical Probability
Very low (exclusion threshold) 0
Low PE risk (5%-10%) 0-1 0-3 0
Intermediate PE risk (25%-30%) 2-6 4-10 ≥1
High PE risk (60%-65%) ≥7 ≥11 1
Abbreviations: DVT, deep vein thrombosis; PE, pulmonary embolism; PERC, pulmonary embolism rule-out criteria; VTE, venous thromboembolism.
www.ebmedicine.net
AUGUST 2023 • www.ebmedicine.net 7 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
the patient’s clinical pretest probability for having a pulmonary embolism patients.30
pulmonary thrombus. Because the normal value for a D-dimer varies
with age, an age-adjusted D-dimer should be used
Electrocardiogram in applying the assay results to any particular patient.
ECG may be useful, but it is not diagnostic, with When using D-dimers as part of any risk stratification
approximately 25% of patients having normal tool, the treating clinician must be aware of the spe-
tracings.27 A resting tachycardia is the most common cific D-dimer assay used by their laboratory. D-dimer
ECG finding in pulmonary embolism patients, seen is reported in 2 different units: FEU (fibrinogen equiv-
in 26% to 27% of cases. The triad of an S wave in alent units) or DDU (D-dimer units). Although specific
lead 1 in conjunction with Q waves and inverted formulas are used to define age-adjusted D-dimer
T wave in lead 3 (S1Q3T3) is neither sensitive nor results, a practical formula for calculating the FEU is
specific. Although historically described as diagnostic to set the threshold for a positive test in individuals
for pulmonary embolism, more rigorous studies aged >50 years to the patient’s age multiplied by 10.
have proven that only 3.7% of pulmonary embolism For example, a 65-year-old patient being tested in a
patients do have these findings.13,27 Other ECG laboratory with a baseline D-dimer assay threshold
abnormalities found in patients with acute pulmonary of 500 ng/mL would have a threshold of 650 ng/
embolism include right ventricular strain, as defined mL.29 Because the DDU threshold is half that of FEU,
by simultaneous T-wave inversions in the inferior and the age correction is 5 times the patient’s age, not
right precordial leads (11.1%), atrial dysrhythmias 10 times. In the above example, if the laboratory is
(10.1%), and right bundle branch block (9%). Atrial reporting in DDUs, the normal value would be 250
fibrillation is the most common arrhythmia found in ng/mL and the corrected normal for a patient aged
acute pulmonary embolism patients, but it is not an 65 years would be 325 ng/mL.
independent predictor of a pulmonary blood clot.27,28
Serum Troponin and Natriuretic Peptides
Laboratory Studies Cardiac troponin T and I isoforms (cTnT and cTnI)
D-dimer Assay are expressed in cardiac muscle tissue and are not
A D-dimer study analyzes the presence of fibrinogen specific for acute myocardial infarctions, but also may
split products that result from the fibrinolysis of a occur with other medical conditions.31 Elevations
blood clot. More specifically, these tests identify in serum troponin levels can be seen in up to 50%
the presence of the 2 bound fibrin D-domains of hypotensive pulmonary embolism patients, but
created by the action of factor XIII. The physiologic in very few asymptomatic patients. As a diagnostic
baseline for D-dimer levels varies with age, and is test, serum troponin has a sensitivity of 51% and a
up to 2.5 times higher in patients aged >70 years specificity of 81%.32 Serum troponin determinations
compared with those aged <50 years. Levels also are much more valuable as prognostic tests for
change with the duration of the clot, dropping severity of illness or mortality than as a tool in
significantly in patients with clots older than 7 days.29 diagnosing pulmonary emboli.
There are over 30 different assays and 20 different Elevations in serum B-type natriuretic peptide
monoclonal antibodies used in D-dimers. Each assay (BNP) or N-terminal-pro BNP levels can also occur in
has a threshold above which a test is considered patients with pulmonary emboli. These findings result
positive. The most sensitive and reliable tests are from stretching of the right ventricle secondary to
the enzyme-linked immunosorbent assays (ELISAs) elevated right ventricular pressures and are more use-
and the enzyme-inked immunofluorescent assays ful for prognostic scoring than for diagnostic testing.
(ELIFAs), both of which have sensitivities around 95% Patients with elevated pro-BNP have a 10% risk for
but specificities in the 46% to 53% range. One point early death and a 23% risk for an adverse outcome.33
that must be stressed when using D-dimer assays to
evaluate for thromboembolic diseases is that these Imaging Studies
tests cannot be considered in isolation. They must Chest Radiograph
be combined with the clinical pretest probability for A chest radiograph is useful in identifying alternative
a pulmonary embolism or DVT. A patient with a low pathology to account for a patient’s presentation, but
clinical pretest probability can be effectively ruled out it is of little value in confirming or excluding a pulmo-
with a negative D-dimer study; however, a patient nary embolism. In a double-blind study, experienced
with a high clinical pretest probability may not be radiologists demonstrated, on plain chest x-ray, a
ruled out with a negative D-dimer and must have sensitivity of 33% and a specificity of 59%, for an
additional diagnostic studies.29 overall accuracy of 40% for the diagnosis of pulmo-
A meta-analysis that included more than 47,000 nary emboli on a plain chest x-ray.34 Plain chest x-rays
patients found that the use of age-adjusted D-dimer were 70% accurate in diagnosing pulmonary infarc-
assays was as sensitive as conventional thresholds tions through identification of a combination of dia-
in making management decisions for suspected phragm elevation, atelectasis, and pleural effusions,
AUGUST 2023 • www.ebmedicine.net 8 ©2023 EB MEDICINE
but they were unable to diagnose pulmonary em- area of a chest x-ray for signs of free air, radio-opaque
boli.35,36 Chest radiograph reports describe a paucity gallstones, or intestinal dilations.
of vascular markings in pulmonary embolism patients
(the Westermark sign), or central pulmonary artery di- Computed Tomography
lation, but these can be very subjective and are rarely Computed tomographic pulmonary arteriography
found.37 The Hampton hump is a peripheral, wedge- (CTPA) is both sensitive and specific for the pres-
shaped opacification adjacent to the pleural surface, ence of clots in the pulmonary vascular tree.39,40 (See
representing a pulmonary infarction distal to a pulmo- Figure 1.) For the identification of clinically significant
nary embolus. This sign is also neither sensitive nor blood clots, the sensitivity of CTPA varies between
specific.34 Congestive heart failure on a chest x-ray 96% and 100%, with a specificity of 89% to 98%.41
is an independent risk factor for pulmonary emboli, Multiple variations of CT angiography now exist for
with an odds ratio (OR) of 2.34.38 Upper abdominal the diagnosis of pulmonary emboli, including triple-
pathology can produce chest pain symptoms that can rule-out protocols to evaluate for aortic dissections
be consistent with pulmonary embolism. For this rea- and coronary stenosis, dual-energy pulmonary CT
son, clinicians should examine the subdiaphragmatic angiography, perfusion imaging, virtual monoen-
Figure 1. Computed Tomography Pulmonary Angiography Scans Showing Pulmonary
Embolisms
The pulmonary arteries are enhanced by contrast, but PEs appear as filling defects, as indicated by the yellow arrows.
Abbreviation: PE, pulmonary embolism.
Reprinted from Rosen's Emergency Medicine Concepts and Clinical Practice. 10th edition. Ron M. Walls, ed. Pulmonary embolism and deep vein
thrombosis. Christopher Kabrhel. Pages 1022-1041 Copyright 2023, with permission from Elsevier.
AUGUST 2023 • www.ebmedicine.net 9 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
ergetic imaging, and low-tube-voltage scanning. studies should have a dialysis session within 48 hours
Despite subtle protocol differences, all of these of receiving diagnostic contrast. Patients managed
approaches use intravenous (IV) iodinated contrast with peritoneal dialysis, regardless of format, should
material timed to demonstrate blood flow through undergo some form of dialysis within 24 hours, so this
the pulmonary circulation. More importantly for the is not a problem for these individuals.47 However, cli-
clinician, all of these approaches provide the same nicians should be familiar with the preferences of their
95%-plus sensitivity for the detection of blood clots particular institution in how IV contrast is managed in
in the lungs. The significance of the detection of end-stage renal disease patients.
subsegmental pulmonary emboli remains controver-
sial, with such clots being identified in up to 9.4% of Point-of-Care Ultrasonography
cases.41 Even more concerning is that fact that up to Another study that may be readily available to the
75% of identified subsegmental pulmonary emboli emergency clinician is point-of-care ultrasound
are thought to be false positives.42 (POCUS). The utility of this test is very provider-spe-
Radiation exposure from CTPA varies with the pro- cific. The most useful POCUS finding indicative of a
tocols used, ranging from 1.1 mSv to 10 mSv.43 The pulmonary embolism is the identification of a throm-
generally accepted threshold for biological exposure bus in lower extremity veins. A meta-analysis found
to produce genetic mutations is considered to be >50 that a pulmonary embolus can be seen in up to 6.9%
mSv, well above that of a typical CTPA study. of patients with superficial venous thrombosis.48 Con-
CT pulmonary angiograms also provide informa- comitant pulmonary embolisms and DVTs can occur
tion for other thoracic organs, including the heart in between 40% and 70% of patients.49 The presence
and aorta. As such, some centers will perform what of a DVT is an independent risk factor for a pulmo-
is frequently termed a triple-rule-out, in which the nary embolism, with an OR of 2.1 for a pulmonary
radiology technicians time their studies to identify embolism.38 Interestingly, in patients with a unilateral
pathology in the coronary vessels and the aorta. If DVT, right-sided clots appeared more commonly than
performed correctly, there is no decrease in the sen- left-sided clots; 26.7% versus 17.7%. A presumptive
sitivity of the study in identifying pulmonary emboli.44 diagnosis of pulmonary embolism can be made in a
The use of the triple-rule-out is particularly well-suited patient with the appropriate clinical symptoms and a
to patients whose clinical presentation is consistent lower extremity DVT on ultrasound examination.
with multiple possible etiologies. Chest POCUS can also support the diagnosis of
a pulmonary embolism. Identification of subpleural
Risks of Iodinated Contrast infarcts on a lung ultrasound scan was 60% sensitive
Because a CTPA study uses iodinated contrast, it has and 95.6% specific for the diagnosis of pulmonary
a risk for producing acute kidney injury. Variability in emboli, while identification of right ventricular dilation
the severity of illness, the degree of hydration, and was 32.7% sensitive and 90.6% specific.50
underlying renal function in ED patients undergoing Sophisticated echocardiographic criteria exist
iodinated contrast studies makes resulting contrast- for the diagnosis of pulmonary emboli, including an
induced nephropathy difficult to predict. Reports of increased right-ventricle-to-left-ventricle size ratio;
contrast-induced nephropathy range from 1.9% to abnormal septal motion; tricuspid regurgitation;
23% of patients following a diagnostic procedure decreased tricuspid annular plane systolic excursion;
involving contrast.45 One recommended risk pulmonary artery midsystolic notching; speckle
stratification tool for contrast-induced nephropathy tracking demonstrating decreased right ventricular
is based on the patient’s estimated glomerular free wall strain; and the general appearance of a
filtration rate (eGFR)46: dilated right ventricle and recognition of hypokinesis
• eGFR ≥45 mL/min/1.73m2: negligible risk or akinesis of the right ventricular free wall with
• eGFR 30-44 mL/min/1.73m2: intermediate risk preservation of the apex (the McConnell sign).51-54
• eGFR <30 mL/min/1.73m2: higher risk More practically, recognition of the McConnell sign is
within the skill set of ED clinicians and it can be seen
The presence of other risk factors (eg, diabetes in 68% of pulmonary embolism patients.53 Abnormal
mellitus) will elevate any of these risks.46 If a CTPA bowing of the intraventricular septum from the right
is the best diagnostic study in a critical patient, then ventricle to the left (“D” sign) is another POCUS
it needs to be performed and the possible renal finding that may be seen by emergency clinicians.
complications addressed as they occur. Although such septal motion is only 25% sensitive
Patients who are already on renal dialysis pres- for pulmonary embolism, its 95% specificity is useful
ent another challenge when undergoing pulmonary for confirming right ventricular overload.52 Using
angiography. Because of the lack of renal clear- a multiorgan protocol of examination of the heart,
ance for the study’s contrast load, these patients will lungs, and leg, POCUS had a sensitivity of 90% and a
require dialysis to eliminate the excess iodine. As a specificity of 86% for pulmonary embolism.50
general rule, hemodialysis patients undergoing these
AUGUST 2023 • www.ebmedicine.net 10 ©2023 EB MEDICINE
Pulmonary Perfusion Study the Diagnostic Approach to Suspected Pulmonary
The other primary diagnostic study for patients at risk Embolism (page 19) summarizes how a clinical risk
for pulmonary emboli is the ventilation/perfusion (V/Q) classification system might be combined with diagnostic
scan.55 Since the introduction of CT angiography, the studies to diagnose a pulmonary embolism.
use of the V/Q scan to diagnose pulmonary emboli In contrast, prognostic risk classifications com-
has decreased markedly, and is now being used as bine physiologic and diagnostic studies to determine
the sole study in as few as 7.1% of suspected patients, the severity of the pulmonary embolism in a patient.
despite having noninferior accuracy in the diagnosis A number of scoring systems are in current use to
of this disease.55 A systematic review of diagnostic describe patients for prognostic risk stratification. In
accuracy and outcome studies utilizing the Quality one scoring system, the term massive pulmonary em-
Assessment of Diagnostic Accuracy Studies tool found boli is applied to patients with abnormal vital signs,
that single-photon emission CT (SPECT) V/Q studies including: systolic blood pressure <90 mm Hg for >15
demonstrated a mean sensitivity of 96% and a specific- minutes; a need for vasopressors; clinical shock; or
ity of 94%.56 The migration to CT over V/Q scanning bradycardia. The term submassive pulmonary emboli
for the diagnosis of suspect pulmonary embolism likely is applied to patients with an abnormal or dilated
stems from the rapidity of the CT study as well as the right ventricle on echocardiogram or CT scan or ab-
ability of CT to detect other lung pathology. normal troponin levels or natriuretic peptides (either
BNP or pro-BNP).
Pulmonary Angiography A scoring system developed by the European
Dedicated pulmonary angiography is a standard Society of Cardiology uses sustained hypotension,
angiography procedure in which a formal digital bradycardia, need for vasopressors, and clinical
angiogram is performed though a catheter placed shock to define the high-risk group. (See Table 3.)
into the pulmonary artery. Although extremely Intermediate-high risk is defined as both the presence
accurate, the procedure requires an interventional of right ventricle abnormality and either an elevated
radiologist or cardiologist and a dedicated troponin or natriuretic peptide. Intermediate-low risk
angiography facility. is defined by only an abnormal right ventricle or an
abnormal laboratory study, troponin, or BNP. Other
Magnetic Resonance Angiography scoring systems include the simplified Pulmonary Em-
Magnetic resonance angiography is a more recent bolism Index (sPESI) (Table 4, page 12) and the Bova
addition to the diagnostic studies used to identify Score for Pulmonary Embolism Complications (Table
pulmonary emboli. Because of the time required to 5, page 12). The advantage of these scoring systems
acquire an image with this technique, at present, up is that they can be used not only to predict morbidity
to 30% of tests are technically unreadable. Of those and mortality but also direct treatments.
that are interpretable, the sensitivity is only 78%
but the specificity is 99%.57 At present, magnetic
resonance angiography is not regarded as a first- Online calculators for these scores are
line diagnostic study for patients with suspected available at www.MDCalc.com
pulmonary embolism. • Simplified PESI (Pulmonary Embolism
Severity Index): https://www.mdcalc.
Risk Stratification Categorization com/calc/1247/simplified-pesi-pulmonary-
A number of risk stratification scores based on the embolism-severity-index
physiologic characteristics of pulmonary embolism • Bova Score for Pulmonary Embolism Compli-
patients have been developed.58,59 Clinical risk cations: https://www.mdcalc.com/calc/4004/
classification tools are used to create a pretest bova-score-pulmonary-embolism-complica-
probability score to determine the need for further tions
diagnostic studies to rule in or rule out the presence
of a pulmonary embolism. The Clinical Pathway for
Table 3. European Society of Cardiology Prognostic Classification of Pulmonary Embolism33
Risk Hemodynamic Instability Right Ventricular Dysfunction on CT or Elevated Biomarkers
Echocardiogram Troponin, BNP, or Pro-BNP
Low risk Negative Negative Negative
Intermediate-low risk Negative CT positive or echocardiogram positive Negative
Intermediate-high risk Negative CT positive and echocardiogram positive Negative
High risk Sustained hypotension or bradycardia or shock or inotropic support
Abbreviations: BNP, B-type natriuretic peptide; CT, computed tomography.
AUGUST 2023 • www.ebmedicine.net 11 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
n Treatment intrathoracic pressure, ventilation by endotracheal
Treatment is dictated by the clinical stability of the intubation results in only passive blood flow into the
patient. Unconscious patients, those with altered right side of the heart. In addition, positive-pressure
mental status, or those with profound lethargy may ventilation increases right ventricular afterload, plac-
require stabilization of their airway with endotracheal ing further stress on a distended right ventricle. If
intubation before initiation of any diagnostics. endotracheal intubation is necessary, the minimum
For more stable patients, supportive care begins amount of positive end-expiratory pressure should be
with assurance of patient oxygenation. In animal used, along with lung protective ventilator settings.
models of acute pulmonary embolism, oxygen ther- Induction agents for rapid sequence intubation
apy reduced right ventricle afterload and decreased should take into account the fragile cardiovascular
right ventricle mechanical work.60 Maintaining a pulse status of these patients. Medications that produce
oximetry level >95% should be the treatment goal. hypotension (eg, propofol, remifentanil, barbiturates)
For minimally symptomatic patients, delivery of sup- should be avoided, while drugs such as ketamine and
plemental oxygen can be via nasal cannula or simple etomidate may be preferred. Providing additional
face mask. If the oxygen deficit requires >6 L/min of intravascular fluid to augment this blood flow may
nasal oxygen to maintain an adequate pulse oximetry help create greater right ventricular preload but has
level, then a more advanced delivery system should additional detrimental effects in a distended right
be considered. Noninvasive respiratory support can ventricle.65 In cases of severe hypoxia, endotracheal
be provided by either high-flow nasal cannula (HFNC) intubation may be the best option despite its
or noninvasive positive-pressure ventilation (NIPPV). detrimental effects on right ventricular function.
HFNC systems are simple to initiate, well toler-
ated, and provide fraction of inspired oxygen (FiO2) Fluid Management
levels up to 100%. HFNC systems function through Patients with stable vital signs will generally have
the use of elevated gas flows to wash out the upper no additional fluid requirements as long as they are
airway dead spaces of exhaled high CO2 and low O2 permitted ad lib access to liquids. For those who are
gases and replace them with low CO2 high O2 gas.60 hypotensive, some degree of fluid therapy may be re-
Successful use of HFNC systems for pulmonary em- quired. Intuitively, it would seem that increasing right
bolism patients has been described only in some case ventricular preload would augment blood flow to the
reports and observational studies.61-63 lungs to help bypass the obstructing clots.65 However,
NIPPV systems are either continuous positive air- physiologically, the exact opposite seems to occur.
way pressure systems (CPAP) or bilevel positive airway The added fluid further dilates the right ventricle and
pressure systems (BiPAP). In both of these systems, leads to right ventricular failure. As the right ventricle
positive pressure is maintained through all phases of fails, less blood is pumped across the pulmonary
the respiratory cycle. One disadvantage of NIPPV sys- vascular bed and less blood is presented to the left
tems is that this positive pressure is also transmitted ventricle. This produces a functional hypovolemic
to the intrathoracic cavity, decreasing venous return state, which then leads to systemic hypotension.66,67
to the heart. This is advantageous in cases of pulmo- Further cardiovascular compromise can result as the
nary overload, such as in congestive heart failure, but distended right ventricle displaces the intraventricular
may be detrimental in pulmonary embolus patients.64 septum into the left ventricle, disrupting systemic
Endotracheal intubation provides 100% oxygen- cardiac output.
ation but has the same limitations as NIPPV. Be- The right ventricle evolved to contract against
cause there is no native breath to generate negative a low pressure afterload, and it struggles when it
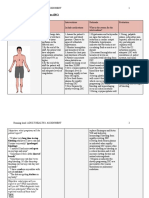
Table 4. Simplified Pulmonary Embolism Table 5. Bova Score for Pulmonary
Index (sPESI) Embolism Complications
Variable Points Variable Points
Age >80 years 1 Systolic blood pressure 90-100 mm Hg 2
History of cancer 1 Elevated cardiac troponin 2
History of chronic cardiopulmonary disease 1 Right ventricular dysfunction on computed 2
Pulse ≥110 beats/min 1 tomography or echocardiogram
Systolic blood pressure <100 mm Hg 1 Heart rate ≥110 beats/min 1
Arterial blood saturation <90% 1 Total Points ______
Total Points ______ Stage I, low risk 0-2 points
Low risk 0 Stage II, intermediate risk 3-4 points
High risk ≥1 Stage III, high risk >4 points
AUGUST 2023 • www.ebmedicine.net 12 ©2023 EB MEDICINE
encounters the sudden onset of pulmonary hy- Anticoagulation
pertension. Though counterintuitive, decreasing Anticoagulation is the mainstay of pulmonary embo-
intravascular volume could improve right ventricular lism management to prevent further clot propaga-
function. In an observational study, normotensive tion and to facilitate dissolution of any existing clot.
patients receiving furosemide demonstrated improve- Table 6 summarizes initial anticoagulation options for
ments in shock index 0.82 versus 0.63 and simplified pulmonary embolus patients. In the ED, the choice
pulmonary embolism severity (sPESI) index ≥1: 45% of anticoagulant is guided by the individual patient’s
versus 55%.68 In a study of intermediate-risk pulmo- clinical scenario. For pulmonary embolism, there are
nary embolism patients, 80 mg of furosemide re- currently 3 direct oral anticoagulant (DOAC) fac-
duced sPESI characteristics in 51.5% of diuretic-treat- tor Xa inhibitors commonly used in clinical practice:
ed patients compared to 37.1% of placebo patients.69 apixaban, rivaroxaban, and edoxaban. Major ad-
Improvements in peak tricuspid annular systolic vantages of these agents are that they can be orally
velocity and heart rate were observed in the diuretic loaded at the time of the patient’s initial encounter,
group of a third study comparing furosemide and and they generally produce anticoagulation within a
fluid expansion in pulmonary embolism patients.70 few hours of administration. These DOACs have pre-
dictable therapeutic profiles, with no need for blood
Vasoactive Agents sample monitoring. These characteristics make them
As with ventricular dysfunction involving the left appropriate for patients with stable vital signs and
ventricle, the use of vasopressors can be considered normal oxygen saturation levels.73-75
for patients with right ventricular failure. Agents More clinically compromised patients will require
such as norepinephrine or dobutamine can be used initial parenteral therapy. Infusions of unfractionated
to maintain systemic blood pressure in patients in heparin have relatively predictable pharmacokinetics,
shock.33 Any vasoactive agent will be limited by although it does require periodic measurements of
filling pressures in the left ventricle. A medication the activated partial thromboplastin time (aPTT). A
such as milrinone with both inotropy and vascular major advantage of heparin is its ability to be phar-
relaxant effects may be more effective but needs to macologically reversed with protamine should the
be added cautiously in hypotensive patients. There patient require a surgical procedure.75 Low-molecular-
is evidence that milrinone will produce pulmonary weight heparins (LMWHs), given subcutaneously,
artery dilation, which can then augment blood have a rapid onset and achieve therapeutic levels
flow and decrease right ventricular afterload.33 All within hours, making them potentially more beneficial
vasodilators are nonspecific and although they may for the initial treatment of symptomatic pulmonary
dilate the pulmonary circulation, they may also dilate emboli for patients without renal impairment.33,75
the systemic circulation, leading to hypotension.66,67 Warfarin was the oral anticoagulant traditionally
Specific pulmonary artery vasodilators (eg, inhaled used for outpatient management of pulmonary em-
nitric oxide) have shown mixed results in the ability boli. Although effective, it has an erratic therapeutic
to improve right ventricular function in pulmonary profile and requires periodic blood samplings to mea-
embolism patients. Newer experimental agents such sure the patient’s international normalized ratio (INR).
as terlipressin have shown promise in animal models, Patients on warfarin will require a bridge of heparin or
but definitive human studies are pending.71,72 LMWH until a therapeutic INR level is achieved.75
Table 6. Initial Anticoagulant Therapy for Pulmonary Embolism
Medication Route Initial Dose Maintenance Dose Comments
Apixaban (DOAC) Oral 10 mg twice daily × 1 wk 5 mg twice daily Requires renal adjustment
Rivaroxaban (DOAC) Oral 15 mg twice daily × 3 wk 20 mg once daily Requires renal adjustment
Edoxaban (DOAC) Oral Weight-based dosing: Weight-based dosing: Requires renal adjustment
>60 kg: 60 mg once daily >60 kg: 60 mg once daily
≤60 kg: 30 mg once daily with ≤60 kg: 30 mg once daily
parenteral bridge for at least 5 days
Unfractionated heparin IV 80 units/kg bolus followed by 18 units/hr Titrated every 6 hr based on aPTT No renal adjustment
Enoxaparin (LMWH) SubQ 1 mg/kg twice daily or 1.5 mg/kg/day 1 mg/kg twice daily or 1.5 mg/kg/day Requires renal adjustment
Warfarin Oral 2.5-5 mg with parenteral bridge Dose adjustments based on INR, Several factors affect therapeutic
with INR goal of 2-3 efficacy
Abbreviations: aPTT, activated partial thromboplastin time; DOAC, direct oral anticoagulant; INR, international normalized ratio; IV, intravenous; LMWH,
low-molecular-weight heparin; subQ, subcutaneously.
www.ebmedicine.net
AUGUST 2023 • www.ebmedicine.net 13 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
Thrombolytics Thrombectomy
Although anticoagulants help prevent additional As with emboli in other areas of the body, mechani-
clot propagation, active dissolution is obtained cal removal of a clot in the pulmonary circulation is
only through the use of thrombolytics, which a therapeutic option. Various retrieval devices have
include alteplase, urokinase, and streptokinase. been developed to mechanically remove clots in the
Alteplase (tissue plasminogen activator, tPA) is the pulmonary circulation. Some mechanically disrupt
primary means of lysing clots. These agents must the clot; others suction it back into a catheter; while
be administered systemically or through pulmonary other use pressure jets to break the clot into small
artery catheters. Systemic thrombolytics are reserved fragments. All of these devices require the services
for use in unstable patients. Compared to heparin, of an intravascular interventional physician to direct
systemic thrombolytics show a reduction in overall the thrombectomy device into the pulmonary circula-
mortality, particularly among high-risk patients (OR, tion. Technical success rates in removing clots from
0.59), and a lower need for treatment escalation the pulmonary circulation range as high as 97.1%,
(OR, 0.34) but at the cost of increased major adverse with clinical success rates of 90.7%.81 The impact on
hemorrhage (OR, 2.91).76 clinical outcome of clot removal is less well defined,
Alteplase is effective for decreasing CT-docu- however, and the clinical indications for these proce-
mented right ventricular abnormalities;76 however, dures are controversial.82
there is no consensus on dosing of alteplase in this
scenario. Some dosing strategies that have been Operative Thoracotomy
described in the literature and have been used in Extraction of clots through a formal thoracotomy
patients with differing degrees of symptom severity remains an option for patients refractory to any other
include the following: therapy. This approach is the most invasive and is re-
• 0.6 mg/kg IV bolus followed by the remainder of served for extremely large clot loads in patients in ex-
100 mg over 2 hours tremis or those failing other less-invasive approaches.
• 50-100 mg IV over 2 hours This is also the preferred approach for patients with
• 50-100 mg IV push a clot in transit, generally a clot straddling a patent
• 50 mg IV push followed by 50 mg IV over 2 hours foramen ovale. Mortality among patients undergoing
this procedure is understandably high, ranging from
Tenecteplase is a modified tPA that is also used 11% to 75%, with the highest death rates occurring in
in patients with pulmonary embolism. It has the patients suffering preprocedure cardiac arrest.83
advantage of delivery as a single bolus injection and
does not require follow-up infusion. Nonetheless, the
evidence in support of tenecteplase over alteplase is
currently lacking.77
Because of the risk for major hemorrhage as-
sociated with the use of any systemic thrombolytic,
care must be taken to avoid administering them Table 7. Contraindications to Systemic
to patients who have contraindications to these Thrombolytic Treatment of Pulmonary
agents. Table 7 lists the contraindications to systemic
Embolism78
thrombolysis of pulmonary emboli.
Absolute Contraindications
• Prior intracranial hemorrhage
Catheter-Directed Thrombolysis • Structural intracranial cerebrovascular disease
In addition to systemic administration of thrombo- • Malignant intracranial neoplasm
lytics, these medications can be delivered directly to • Ischemic stroke within prior 3 months
the clot via catheter-directed thrombolysis via a pul- • Suspected aortic dissection
• Active bleeding or bleeding diathesis
monary artery catheter. In these catheters, ports for
• Recent surgery near spinal canal or brain
thrombolytic delivery are coupled with an ultrasonic • Recent significant closed-head or facial trauma with bony fracture or
agitator to help disperse the medication into and brain injury
around the clot. This invasive approach will require
the services of an interventional clinician as well as Relative Contraindications
• Age >75 years
a fluoroscopic suite.79 This approach is generally ap-
• Current use of anticoagulants
plied to patients who are at intermediate-high risk, • Pregnancy
high risk with cardiovascular instability, or who have • Noncompressible vascular punctures
contraindications for systemic thrombolysis. In a study • Traumatic or prolonged cardiopulmonary resuscitation
of intermediate-risk patients, the placement of the • Internal bleeding in past 2-4 weeks
• History of chronic, severe, poorly controlled hypertension
catheter-directed thrombolysis catheter took only 15
• Dementia
minutes and resulted in a reduction of the pulmonary • Ischemic stroke >3 months prior
artery obstruction by 35.9%.80 • Major surgery within prior 3 weeks
AUGUST 2023 • www.ebmedicine.net 14 ©2023 EB MEDICINE
Extracorporeal Membrane Oxygenation n Special Populations
Extracorporeal membrane oxygenation (ECMO) is Pulmonary Embolism in Pregnant Patients
a final option for patients unable to be adequately Pregnancy is an independent risk factor for the
stabilized through other means. ECMO may be development of pulmonary emboli, including the
delivered as either a venous-to-venous (VV) route prepartum and postpartum periods, and is a leading
or a venous-to-arterial (VA) route. In VV ECMO, the cause of maternal mortality, causing 1.13 deaths per
procedure assumes the gas exchange responsibility 100,000 maternities.89 Pregnant patients also present
of the lungs, providing oxygenation while removing a diagnostic challenge in that many of the signs and
carbon dioxide. In these patients, the left ventricle symptoms of pulmonary emboli are present as normal
still provides the systemic cardiac output. In VA characteristics of pregnancy. The YEARS criteria for
ECMO, the procedure also assumes the responsibility clinical pretest probability categorization is the only
for providing the systemic circulation. ECMO is most algorithm with dedicated pregnancy evaluation.89
commonly used as a bridge to a more definitive Pulmonary embolism diagnosis is further compli-
therapeutic procedure to remove the offending clot, cated by the risks to the mother and fetus with the
though high-quality data are lacking.83,84 use of diagnostic CTPA or pulmonary perfusion stud-
ies;90,91 however, both studies present a radiation risk
Patient Management that is well below the 50 mSv threshold for biologic
Patient management for an acute pulmonary injury. CTPA may present an exposure of 3 to 10 mSV
embolism must be individualized. Clinical decisions to the mother’s breast tissue and a 0.05 to 0.5 mSV
can be extremely complex and often require the dose to the fetus, while a V/Q scan will present a fetal
input of multiple consultants. The development of exposure of 0.2 to 0.6 mSV.92
institution-specific pulmonary embolism response Magnetic resonance testing may be considered
teams (PERTs) has helped to facilitate real-time for pregnant patients, particularly if the iron supple-
decisions for these patients. The PERT composition ment ferumoxytol is used for contrast. At present
can vary, but frequently will include members from though, this has limited usefulness in most clinical
emergency medicine, pulmonology, interventional sites.93 The use of D-dimer values is also limited as
radiology, interventional cardiology, and critical a screening test because the thresholds for positive
care, plus others, depending on the institution. PERT values vary through the trimesters of the pregnancy.
notification criteria vary, but, in general, become In one report in which 500 ng/mL was considered the
active for patients determined to be at intermediate- normal threshold in nonpregnant patients, D-dimer
high risk and high risk.79,85 intervals were determined to be 110 to 400 ng/mL
The specific management approach to the patient in the first trimester; 140 to 750 ng/mL in the sec-
with a pulmonary embolism is controversial, at best. ond trimester, and 160 to 1300 ng/mL in the third.94
Multiple organizations have developed treatment The Clinical Pathway for Emergency Department
algorithms based on clinical risk assessments for Management of Pulmonary Embolism in Pregnant
the treatment of pulmonary emboli. Stable patients Patients (page 21) presents an approach to suspect-
with no hypoxia, tachycardia, or dyspnea who ed pulmonary embolism in pregnancy.90
meet low-risk criteria can be safely managed with Treatment of pulmonary embolism in pregnancy
anticoagulation only. These patients may also be in low-risk patients is with LMWHs.95 However, once
candidates for outpatient care. a patient’s risk rises to the intermediate-risk or high-
All intermediate-risk and high-risk patients will risk category, more difficult management decisions
require hospitalization, preferably with continuous must be made. The use of thrombolytics (regardless
cardiac monitoring. Supplemental oxygen in the form of delivery method), catheter interventions, ECMO,
of nasal cannula may be required to maintain an oxy- and surgical embolectomy all come into play in these
gen saturation >95%. The specific therapy to address patients and are best decided upon with a PERT team
the pulmonary embolism remains controversial. These or with input from multiple consultants. None of these
patients may be managed with initial anticoagulation options is clearly superior to any others or present
with a LMWH or heparin.45 superior risk-benefit ratios.33
With the introduction of catheter-directed
procedures for thrombolysis and thrombectomy, the Pulmonary Embolism and COVID-19 Patients
treatment of patients who are intermediate-high risk Infection with the SARS-CoV-2 virus, COVID-19
and high risk is changing. However, to date, there disease, can lead to elevated pulmonary thrombo-
are no definitive data to identify which patients embolic risks. Two mechanisms have been proposed
can benefit from these interventions.81,86-88 The for this increase. The first is a hypercoagulable state,
Clinical Pathway for Risk-Directed Management leading to large-vessel thrombi. The second is a
of Pulmonary Embolism (page 20) presents a risk- direct endovascular injury secondary to viral infection
assessment therapeutic approach to the management of endothelial cells. Pulmonary embolism rates vary
of pulmonary embolism patients. depending on the reporting source,96-98 but one
AUGUST 2023 • www.ebmedicine.net 15 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
systematic review places the incidence at 17.5% for limited, if any, evidence to identify which patients
emergency department patients, 23.9% for general may benefit from these new therapies. Intermediate-
wards, and 48.6% for intensive care unit patients.98 high and high-risk individuals appear to be the group
Diagnosis of pulmonary embolism in patients most likely to require some form of more aggressive
either with or following infection with the SARS-CoV-2 therapy including catheter-directed thrombolysis,
virus is hampered due to the overlapping symptoms mechanical thrombectomy, and even ECMO or surgi-
of the 2 diseases, undermining the accuracy of clinical cal thrombectomy. Unfortunately, the role of more
decision rules. D-dimer analysis encounters the same aggressive treatment beyond systemic thrombolysis
problem, although raising the threshold to 1000 ng/mL remains undefined. The mortality rate for conserva-
may improve the specificity of the test, as COVID-19 tively managed patients in the intermediate-high–risk
patients with pulmonary emboli, in general, have a group or those with an sPESI score of 0 can be as
higher D-dimer level than non-COVID patients.97 low as 1% to 3%, making objective proof of outcome
Unfortunately, there is no good clinical practice ad- improvements for these procedures difficult to obtain.
justment to help distinguish patients with pulmonary Multiple studies have used normalization of the right-
emboli and no infection from patients with shortness of ventricle-to-left ventricle ratio to ≤0.9 as a surrogate
breath and hypoxia secondary to their viral infection. marker in single-arm studies on invasive management
Once diagnosed, the management of SARS- techniques. However, at this time there is no random-
COV-2 patients with pulmonary emboli is essentially ized study comparing aggressive and conservative
the same as for noninfected individuals.98,99 treatments in the management of intermediate-high-
risk patients. Comparisons of systemic thrombolytics
with mechanical thrombectomy have shown advan-
n Controversies and Cutting Edge tages and disadvantages to both approaches but no
5 Recommendations
Catheter-directed thrombolysis
To Apply and mechanical
in Practice clear-cut optimal management approach. The input
thrombectomy have introduced new treatment of a PERT team can be extremely valuable in sorting
options for the management of higher-risk pulmo- through the options in the care of these patients.
nary embolism 5patients. At present though, there is
Recommendations
To Apply in Practice
n Disposition
Despite the potential severity of pulmonary emboli
5 Things That Will Change and the risk for significant morbidity and mortality,
5 Recommendations
the disposition of these patients ranges from inten-
Your Practice
To Apply in Practice
sive care unit admission to outpatient home care.
1. Recognize high-risk factors for pulmonary Low-risk patients meeting the Hestia criteria (See Ta-
emboli, and consider pulmonary embolism ble 8) may be candidates for outpatient management
as a cause of a patient’s symptoms when pre- of their pulmonary emboli. Anticoagulation must be
senting to the emergency department. initiated for these patients in the emergency depart-
2. Consider outpatient management. Applica- ment and may include either a DOAC or a LMWH.
tion of tools such as the Hestia criteria allow Patients managed with warfarin are best admitted to
clinicians to identify patients at low risk for the hospital for bridging therapy until anticoagulation
complications who may safely be discharged is achieved. Low-risk patients not meeting the Hestia
from the ED. criteria should be admitted to the hospital, preferably
3. Use clinical classifications to guide inpatient in a unit with cardiovascular monitoring capabilities.
management. Application of clinical risk
scores can help direct the clinician toward the
most appropriate treatment. This will limit the
overuse of invasive procedures that do not
Table 8. Hestia Criteria for Outpatient
impact patient outcomes. Treatment of Pulmonary Embolism3
4. Interpret D-dimer studies appropriately. All Criteria Must be Answered “No” to Qualify for Outpatient
Pulmonary Embolism Therapy:
Understanding the concept of age-adjusted
• Hemodynamic instability
D-dimer studies will prevent diagnosis based • Thrombolysis or embolectomy required
on false-positive results. • Active bleeding or high risk for bleed
5. Use pretest probability risk stratification tools • Oxygen required to maintain pulse oxygen >90%
to limit diagnostic studies. The use of algo- • Pulmonary embolism diagnosed during anticoagulant treatment
• Recent intravenous pain medication
rithms to create risk categories for patients
• Other medical or social issue requiring hospitalization
with potential pulmonary emboli can direct • Creatine clearance <30 mL/min* (Cockcroft-Gault formula)
emergency clinicians on the most effective • Severe liver disease
use of radiographic studies. • Pregnancy
• History of heparin-induced thrombocytopenia
AUGUST 2023 • www.ebmedicine.net 16 ©2023 EB MEDICINE
Case Conclusions
For the obese 55-year-old man with 2 days of exertional dyspnea…
Because all previous studies did not explain his dyspnea and mild tachycardia, you obtained a D-dimer,
which returned at 1250 ng/mL. You obtained a chest CT angiogram that revealed the presence of a large
CASE 1
pulmonary embolism. You began anticoagulation with LMWH. A Doppler study also revealed a DVT in
his left leg, and an echocardiogram depicted right ventricular strain. His troponin I returned normal. You
contacted your PERT team. This patient was intermediate-high risk, which now opened the debate for the
best management. Ultimately, because of the patient’s size, it was determined that a catheter embolectomy
was the best course. The procedure was performed, the patient did well, and was discharged to home.
For the 65-year-old woman with dyspnea…
CASE 2
The patient required anticoagulation, but the question arose as to which agent to use and the ideal
disposition. She met low-risk criteria by sPESI and she met the Hestia criteria for outpatient management.
You discussed the case with the PERT team, and with shared decision-making with the patient, she was
started on a DOAC and scheduled to follow up with the pulmonologist from the PERT team in 2 days.
For the 60-year-old woman who arrived via EMS cyanotic, tachypneic, and tachycardic…
This patient was clearly a high-risk pulmonary embolism patient, even without any diagnostic studies. A
right humeral intraosseous access was obtained. She became lethargic, with a progressively dropping
respiratory rate. She underwent rapid sequence intubation with ketamine and rocuronium, and her
oxygenation improved to a pulse oximetry of 85% on 100% bag-valve mask ventilation, with an end-tidal
CASE 3
carbon dioxide level of 60 mm Hg. A right internal jugular catheter was placed and she was administered
alteplase 50 mg IV over 2 hours. A portable chest x-ray was negative. Bedside echocardiography
demonstrated a dilated right ventricle. The patient’s oxygen saturation gradually improved to 95%, and CO2
level decreased to 40 mm Hg. She was transferred to the CT scanner, where a pulmonary saddle embolism
was identified. Her blood pressure stabilized at 100/70 mm Hg, and her heart rate decreased to 110 beats/
min. Her oxygen continued to improve over the next 3 hours and she was transferred to the intensive
care unit. Following a rocky 1 month hospitalization, the patient was discharged home with a return to
premorbid baseline health status.
High-risk patients, by definition, have unstable n Time- and Cost-Effective Strategies
vital signs and should be cared for in a critical care- • Invasive management techniques for pulmo-
level unit that can provide close monitoring of all vital nary emboli are impressive, particularly when a
signs. Intermediate-risk patients (whether intermedi- thrombectomy is performed and multiple large
ate-low or intermediate-high) will also require cardio- collections of clots are removed. However, there
vascular monitoring but may be cared for in another is no evidence that such procedures change pa-
monitored unit in the hospital, depending on the tient outcomes, especially when it comes to mor-
logistics of that particular facility. A hospital-specific tality. Considering the costs and risks of catheter
PERT consult may be useful in directing the admission thrombectomies, more research will be required
location for admitted patients. before these procedures become the norm for
intermediate-risk patients.
• The use of clinical risk diagnosis scores such as
n Summary PERC, Wells, and YEARS can limit the excessive
Acute pulmonary embolism patients present a unique use of high-cost tests such as CTPAs and V/Q
challenge to emergency clinicians. Fortunately, the scans.
creation of risk stratification criteria help with both the • Use the Hestia criteria to discharge low-risk
diagnostic workup of potential pulmonary embolism patients, as it is very cost effective and safe.
patients as well as their therapeutic management. • Use the YEARS criteria in pregnant patients at risk
Having an understanding of how and when to apply for pulmonary embolism to eliminate unnecessary
these criteria allows emergency clinicians to deliver radiation studies.
well-supported, evidence-based care across the entire • Use the age-adjusted D-dimer criteria to reduce
spectrum of acute pulmonary embolism patients. the number of elderly patients requiring further
studies for pulmonary embolism.
AUGUST 2023 • www.ebmedicine.net 17 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
Risk Management Pitfalls for Pulmonary Embolism
in the Emergency Department
1. “The patient had normal vital signs, they could 6. “The patient met most of the Hestia criteria
not have a pulmonary embolism.” Abnormal vi- for outpatient management, isn’t that good
tal signs are of value in alerting a clinician to look enough?” For outpatient management of
for a pulmonary embolism, but the reverse is not pulmonary embolus patients, it is prudent to be
true. Patients with pulmonary emboli can have certain that discharged patients meet all of the
normal vital signs. Hestia criteria or some other outpatient scoring
system. This diagnosis has the potential to take
2. “She had no pleuritic chest pain, so a pulmo- a downward turn very quickly, so it is best to
nary embolism should not be on the differen- be conservative regarding which patients are
tial.” Pleuritic chest pain occurs in less than 50% admitted and which are sent home.
of patients, while nonpleuritic chest pain can
occur in 17% of cases. 7. “I started the patient on warfarin, so he was
anticoagulated.” Warfarin is a vitamin K antago-
3. “The onset of shortness of breath was over nist, and it takes time to become effective. If it is
days. That is not how a pulmonary embolism to be used for pulmonary embolism patients, a
presents.” It is true that approximately 67% of bridge with a rapid-acting anticoagulant must be
patients with a pulmonary embolism will describe used until the warfarin becomes therapeutic.
their dyspnea as “sudden” in onset, occurring
within minutes, but this still leaves a gradual 8. “The patient’s rGeneva score was 4. That is
onset occurring in about one-third of cases. almost low-risk.” Low-risk is ≤3. You can state in
your note that the patient was intermediate-risk
4. “It doesn't matter what the patient’s blood but you decided that the entire clinical picture
pressure showed, or her normal troponin and did not warrant further workup, but do not state
BNP. There was a large clot on the CTPA and the patient was “almost” low-risk.
a dilated right ventricle. She needed tPA.” In
patients who are stable, low-risk, or intermediate- 9. “The patient’s chest pain was clearly cardiac,
low risk, the value of tPA is not well established. and I ruled them out with a negative troponin
There is real risk for bleeding with tPA, as well. At test and an ECG.” The pain from a pulmonary
present, tPA should be used only in high-risk pa- embolism can mimic that from an acute myocar-
tients and should be considered in intermediate- dial infarction. Just because you have ruled out
high risk patients. one does not mean you do not need to consider
the other.
5. “I am an emergency physician. I can manage
my patients without a PERT team.” It may not 10. “I didn’t think the recent surgery was an is-
be the standard of care to consult a PERT team sue. The patient needed tPA.” If the patient is
for every pulmonary embolism patient; however, high risk and has an absolute contraindication to
getting expert consultants involved in the care tPA, then the clinician should attempt to arrange
of a patient, especially one who is not low-risk, is another approach, which might include catheter-
always a good idea. directed tPA or a thrombectomy.
AUGUST 2023 • www.ebmedicine.net 18 ©2023 EB MEDICINE
Clinical Pathway for the Diagnostic Approach
to Pulmonary Embolism Management
Patient presents with suspected pulmonary embolism
Apply clinical probability assessment
(determined by prediction rule) (Class I)
Low or intermediate probability High probability
Perform D-dimer test (Class I) Perform CTPA or V/Q scan (Class I)
Positive? Positive?
NO YES YES NO
Perform CTPA or V/Q
No treatment scan (Class I) YES Treat Pursue other diagnoses
Positive?
Abbreviations: CTPA, computed tomographic pulmonary arteriography; V/Q, ventilation/perfusion.
Class of Evidence Definitions
Each action in the clinical pathways section of Emergency Medicine Practice receives a score based on the following definitions.
Class I Class II
• Always acceptable, safe • Safe, acceptable Class III Indeterminate
• Definitely useful • Probably useful • May be acceptable • Continuing area of research
• Proven in both efficacy and effectiveness • Possibly useful • No recommendations until further
Level of Evidence: • Considered optional or alternative research
Level of Evidence: • Generally higher levels of evidence treatments
• One or more large prospective studies • Nonrandomized or retrospective stud- Level of Evidence:
are present (with rare exceptions) ies: historic, cohort, or case control Level of Evidence: • Evidence not available
• High-quality meta-analyses studies • Generally lower or intermediate levels • Higher studies in progress
• Study results consistently positive and • Less robust randomized controlled trials of evidence • Results inconsistent, contradictory
compelling • Results consistently positive • Case series, animal studies, • Results not compelling
consensus panels
• Occasionally positive results
This clinical pathway is intended to supplement, rather than substitute for, professional judgment and may be changed depending upon a patient’s individual
needs. Failure to comply with this pathway does not represent a breach of the standard of care.
Copyright © 2023 EB Medicine. www.ebmedicine.net. No part of this publication may be reproduced in any format without written consent of EB Medicine.
AUGUST 2023 • www.ebmedicine.net 19 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
Clinical Pathway for Risk-Directed Management
of Pulmonary Embolism
Patient has confirmed pulmonary embolism
Initiate anticoagulation (see Table 6) (Class I)
Risk-stratify patient (Class I)
Low risk Intermediate-low risk Intermediate-high risk High risk
Continue anticoagulation Are there
NO Is there clinical deterioration to high risk? YES
(Class I) contraindications to
thrombolysis?
(see Table 7)
YES YES NO
Consider reduced-dose thrombolysis or mechanical thrombectomy
YES, relative
(Class III)
Consider mechanical thrombectomy (Class III) YES, absolute
Systemic thrombolysis,
full or reduced dose
(Class III)
For Class of Evidence definitions, see page 19.
AUGUST 2023 • www.ebmedicine.net 20 ©2023 EB MEDICINE
Clinical Pathway for Emergency Department Management
of Pulmonary Embolism in Pregnant Patients
Pregnant patient presents with
suspicion for pulmonary embolism
• Perform D-dimer study (Class I)
• Assess YEARS criteria* (Class II)
YES Clinical signs of deep vein thrombosis? NO
Perform compression ultrasound of Any YEARS criteria positive?
lower extremities (Class I) (Class III)
YES NO
D-dimer <1000
Positive for deep vein thrombosis? NO D-dimer <500 ng/mL?
ng/mL?
YES YES YES NO
No pulmonary Perform CTPA; if
Initiate anticoagulation (see Table 6)
embolism positive, initiate
anticoagulation
*YEARS criteria:
• Clinical signs of deep vein thrombosis
• Hemoptysis
• Pulmonary embolism is the most likely diagnosis
MDCalc online tool for YEARS:
https://www.mdcalc.com/calc/4067/years-algorithm-for-pulmonary-embolism-pe
Abbreviation: CTPA, computed tomography pulmonary angiography.
For Class of Evidence definitions, see page 19.
AUGUST 2023 • www.ebmedicine.net 21 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
n References 16. Richmond C, Jolly H, Isles C. Syncope in pulmonary em-
bolism: a retrospective cohort study. Postgrad Med J.
Evidence-based medicine requires a critical appraisal 2021;97(1154):789-791. (Retrospective cohort study; 224
of the literature based upon study methodology and patients)
number of subjects. Not all references are equally 17. Kline JA, Hernandez-Nino J, Jones AE, et al. Prospective study
robust. The findings of a large, prospective, random of the clinical features and outcomes of emergency department
patients with delayed diagnosis of pulmonary embolism. Acad
ized, and blinded trial should carry more weight than
Emerg Med. 2007;14(7):592-598. (Prospective observational
a case report. study; 161 patients)
To help the reader judge the strength of each 18.* Kline JA, Corredor DM, Hogg MM, et al. Normalization of vital
reference, pertinent information about the study will signs does not reduce the probability of acute pulmonary em-
be included in bold type following the reference, bolism in symptomatic emergency department patients. Acad
where available. In addition, the most informative Emerg Med. 2012;19(1):11-17. (Prospective observational
study; 192 patients)
references cited in this paper, as determined by
DOI: 10.1111/j.1553-2712.2011.01253.x
the authors, are noted by an asterisk (*) next to the
19. Becattini C, Vedovati MC, Pruszczyk P, et al. Oxygen satu-
number of the reference. ration or respiratory rate to improve risk stratification in
hemodynamically stable patients with acute pulmonary embo-
1. Khan F, Tritschler T, Kahn SR, et al. Venous thromboembolism. lism. J Thromb Haemost. 2018;16(12):2397-2402. (Prospective
Lancet. 2021;398(10294):64-77. (Review) cohort study; 946 patients)
2. Kahn SR, de Wit K. Pulmonary embolism. N Engl J Med. 20. Bowers T, Goldstein JA. Hemodynamic compromise in pulmo-
2022;387(1):45-57. (Review) nary embolism: “a tale of two ventricles”. Catheter Cardiovasc
3.* Westafer LM, Long B, Gottlieb M. Managing pulmonary embo- Interv. 2021;97(2):299-300. (Pathophysiology presentation)
lism. Ann of Emerg Med. 2023:1-9. (Review) 21. Chan TF, Ngian VJJ, Hsu K, et al. Pulmonary embolism: clinical
DOI: 10.1016/j.annemergmed.2023.01.019 presentation and diagnosis in the oldest old. Intern Med J.
4. Mansella G, Keil C, Nickel CH, et al. Delayed diagnosis in 2020;50(5):627-631. (Retrospective cohort study; 302 pa-
pulmonary embolism: frequency, patient characteristics, and tients)
outcome. Respiration. 2020;99(7):589-597. (Retrospective case 22. Adeyinka A, Kondamudi NP. Cyanosis. StatPearls [Internet].
comparison; 1119 patients) Treasure Island (FL): StatPearls Publishing; 2022. (Review)
5. Stone J, Hangge P, Albadawi H, et al. Deep vein thrombosis: 23. Busse LW, Vourlekis JS. Submassive pulmonary embolism. Crit
pathogenesis, diagnosis, and medical management. Cardiovasc Care Clin. 2014;30(3):447-473. (Review)
Diagn Ther. 2017;7(Suppl 3):S276-S284. (Review) 24. Vyas V, Goyal A. Acute pulmonary embolism. StatPearls [Inter-
6. Rali PM, Criner GJ. Submassive pulmonary embolism. Am J net]. Treasure Island (FL): StatPearls Publishing; 2022. (Review)
Respir Crit Care Med. 2018;198(5):588-598. (Review) 25. Kline JA, Garrett JS, Sarmiento EJ, et al. Over-testing for
7. Kaptein FHJ, Kroft LJM, Hammerschlag G, et al. Pulmo- suspected pulmonary embolism in American emergency
nary infarction in acute pulmonary embolism. Thromb Res. departments: the continuing epidemic. Circ Cardiovasc Qual
2021;202:162-169. (Review) Outcomes. 2020;13(1):E005753. (Database analysis)
8. Wenger N, Sebastian T, Engelberger RP, et al. Pulmonary em- 26. Rodger MA, Maser E, Stiell I, et al. The interobserver reliability
bolism and deep vein thrombosis: similar but different. Thromb of pretest probability assessment in patients with suspected
Res. 2021;206:88-98. (Review) pulmonary embolism. Thromb Res. 2005;116(2):101-107. (Pro-
9. Wang H, Huang Y, Xu CW, et al. Clinical analysis of tumor and spective cohort; 110 patients)
non-tumor patients complicated with pulmonary embolism. Int 27. Thomson D, Kourounis G, Trenear R, et al. ECG in suspected
J Clin Exp Med. 2015;8(10):18729-18736. pulmonary embolism. Postgrad Med J. 2019;95(1119):12-17.
10. Senst B, Tadi P, Basit H, et al. Hypercoagulability. StatPearls (Retrospective case control; 1397 patients)
[Internet]. Treasure Island (FL): StatPearls Publishing; 2022. 28. Friberg L, Svennberg E. A diagnosis of atrial fibrillation is not a
(Review) predictor for pulmonary embolism. Thromb Res. 2020;195:238-
11. Gimbel IA, Mulder FI, Bosch FTM, et al. Pulmonary em- 242. (Retrospective registry study; 1.5 million patients)
bolism at autopsy in cancer patients. J Thromb Haemost. 29. Freund Y, Chauvin A, Jimenez S, et al. Effect of a diagnostic
2021;19(5):1228-1235. (Retrospective cohort study; 9571 strategy using an elevated and age-adjusted D-dimer threshold
patients) on thromboembolic events in emergency department patients
12. Au C, Gupta E, Khaing P, et al. Clinical presentations and out- with suspected pulmonary embolism: a randomized clinical
comes in pulmonary embolism patients with cancer. J Thromb trial. JAMA. 2021;326(21):2141-2149. (Prospective random-
Thrombolysis. 2021;51(2):430-436. (Retrospective case series; ized trial; 726 patients)
581 patients) 30.* Iwuji K, Almekdash H, Nugent KM, et al. Age-adjusted D-dimer
13.* Stein PD, Beemath A, Matta F, et al. Clinical characteristics of in the prediction of pulmonary embolism: systematic review
patients with acute pulmonary embolism: data from PIOPED and meta-analysis. J Prim Care Community Health. 2021;12:1-
II. Am J Med. 2007;120(10):871-879. (Analysis of prospective 8. (Systematic review) DOI: 10.1177/21501327211054996
data base; 824 patients) 31. Chauin A. The main causes and mechanisms of increase in
DOI: 10.1016/j.amjmed.2007.03.024 cardiac troponin concentrations other than acute myocardial
14. Kline JA, Kabrhel C. Emergency evaluation for pulmonary em- infarction (part 1): physical exertion, inflammatory heart disease,
bolism, part 1: clinical factors that increase risk. J Emerg Med. pulmonary embolism, renal failure, sepsis. Vasc Health Risk
2015;48(6):771-780. (Review) Manag. 2021;17:601-617. (Review)
15.* Badertscher P, du Fay de Lavallaz J, Hammerer-Lercher A, et al. 32. Kilinc G, Dogan OT, Berk S, et al. Significance of serum car-
Prevalence of pulmonary embolism in patients with syncope. diac troponin I levels in pulmonary embolism. J Thorac Dis.
J Am Coll Cardiol. 2019;74(6):744-754. (Prospective observa- 2012;4(6):588-593. (Prospective observational study; 106
tional study; 1380 patients) DOI: 10.1016/j.jacc.2019.06.020 patients)
AUGUST 2023 • www.ebmedicine.net 22 ©2023 EB MEDICINE
33.* Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC extremity deep vein thrombosis in patients with pulmonary
guidelines for the diagnosis and management of acute pulmo- embolism undergoing catheter-directed therapy. J Invasive
nary embolism developed in collaboration with the European Cardiol. 2021;33(11):e910-e915. (Retrospective case series;
Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603. 137 patients)
(Guidelines) DOI: 10.1093/eurheartj/ehz405 50. Nazerian P, Vanni S, Volpicelli G, et al. Accuracy of point-of-care
34. Greenspan RH, Ravin CE, Polansky SM, et al. Accuracy of the multiorgan ultrasonography for the diagnosis of pulmonary em-
chest radiograph in diagnosis of pulmonary embolism. Invest bolism. Chest. 2014;145(5):950-957. (Prospective case series;
Radiol. 1982;17(6):539-543. (Prospective case series; 152 357 patients)
patients) 51. Alerhand S, Sundaram T, Gottlieb M. What are the
35. Talbot S, Worthington BS, Roebuck EJ. Radiographic signs echocardiographic findings of acute right ventricular strain that
of pulmonary embolism and pulmonary infarction. Thorax. suggest pulmonary embolism? Anaesth Crit Care Pain Med.
1973;28(2):198-203. (Autopsy study; 123 patients) 2021;40(2):100852. (Descriptive review article)
36. Coche E, Verschuren F, Hainaut P, et al. Pulmonary embolism 52. Alerhand S, Hickey SM. Tricuspid Annular Plane Systolic Excur-
findings on chest radiographs and multislice spiral CT. Eur sion (TAPSE) for risk stratification and prognostication of pa-
Radiol. 2004;14(7):1241-1248. (Matched control series) tients with pulmonary embolism. J Emerg Med. 2020;58(3):449-
37. Buckner CB, Walker CW, Purnell GL. Pulmonary embo- 456. (Review)
lism: chest radiographic abnormalities. J Thorac Imaging. 53. Mediratta A, Addetia K, Medvedofsky D, et al.
1989;4(4):23-27. (Descriptive review) Echocardiographic diagnosis of acute pulmonary embo-
38. Hou J, Wang W, Cai H, et al. Patients with right lower extrem- lism in patients with McConnell’s sign. Echocardiography.
ity deep vein thrombosis have a higher risk of symptomatic 2016;33(5):696-702. (Retrospective case series; 167 patients)
pulmonary embolism: a retrospective study of 1585 patients. 54. Daley JI, Dwyer KH, Grunwald Z, et al. Increased sensitivity of
Ann Vasc Surg. 2022;81:240-248. (Retrospective study; 1585 focused cardiac ultrasound for pulmonary embolism in emer-
patients) gency department patients with abnormal vital signs. Acad
39. Knollmann F, Chu L, Lang JA. CT angiography for the detection Emerg Med. 2019;26(11):1211-1220. (Prospective case series;
of pulmonary embolism: role of tube voltage and contrast injec- 1432 patients)
tion rate on diagnostic confidence. Acad Radiol. 2022;29:S91- 55. Bonnefoy PB, Prevot N, Mehdipoor G, et al. Ventilation/
S97. (Retrospective comparison; 401 patients) perfusion (V/Q) scanning in contemporary patients with
40. Leithner D, Gruber-Rouh T, Beeres M, et al. 90-kVp low- pulmonary embolism: utilization rates and predictors of use in
tube-voltage CT pulmonary angiography in combination a multinational study. J Thromb Thrombolysis. 2022;53(4):829-
with advanced modeled iterative reconstruction algorithm: 840. (Database analysis; 26,540 patients)
effects on radiation dose, image quality and diagnostic ac- 56. Le Roux PY, Robin P, Tromeur C, et al. Ventilation/perfusion
curacy for the detection of pulmonary embolism. Br J Radiol. SPECT for the diagnosis of pulmonary embolism: a systematic
2018;91(1088):1-6. (Retrospective case series; 40 patients) review. J Thromb Haemost. 2020;18(11):2910-2920.
41. Wiener RS, Schwartz LM, Woloshin S. When a test is too good: (Systematic review)
how CT pulmonary angiograms find pulmonary emboli that do 57. Benson DG, Schiebler ML, Repplinger MD, et al. Contrast-en-
not need to be found. BMJ. 2013;347:F3368. (Opinion) hanced pulmonary MRA for the primary diagnosis of pulmonary
42. Keeling D, Klok FA, Le Gal G. Controversies in venous throm- embolism: current state of the art and future directions. Br J
boembolism--2015. Blood Rev. 2016;30(1):27-33. (Review) Radiol. 2017;90(1074):20160901. (Review)
43. Takahashi EA, Yoon HC. Four-year cumulative radiation 58. Maraziti G, Cimini LA, Becattini C. Risk stratification to optimize
exposure in patients undergoing computed tomography the management of acute pulmonary embolism. Expert Rev
angiography for suspected pulmonary embolism. Radiol Res Cardiovasc Ther. 2022;20(5):377-387. (Review)
Pract. 2013;2013:482403. (Retrospective case series; 300 59. Triantafyllou GA, O’Corragain O, Rivera-Lebron B, et al. Risk
patients) stratification in acute pulmonary embolism: the latest algo-
44. Russo V, Sportoletti C, Scalas G, et al. The triple rule out CT rithms. Semin Respir Crit Care Med. 2021;42(2):183-198.
in acute chest pain: a challenge for emergency radiologists? (Review)
Emerg Radiol. 2021;28(4):735-742. (Prospective observational 60. Lyhne MD, Hansen JV, Dragsbæk SJ, et al. Oxygen therapy
study; 350 patients) lowers right ventricular afterload in experimental acute pulmo-
45. Ong MY, Koh JJ, Kothan S, et al. The incidence and associated nary embolism. Crit Care Med. 2021;49(9):e891-e901. (Animal
risk factors of contrast-induced nephropathy after contrast- model)
enhanced computed tomography in the emergency setting: 61. Sharma S, Danckers M, Sanghavi D, et al. High flow nasal
a systematic review. Life (Basel). 2022;12(6):826. (Systematic cannula. StatPearls [Internet]. Treasure Island (FL): StatPearls
review) Publishing; 2022. (Review)
46. Rudnick MR, Leonberg-Yoo AK, Litt HI, et al. The controversy of 62. Messika J, Goutorbe P, Hajage D, et al. Severe pulmonary em-
contrast-induced nephropathy with intravenous contrast: what bolism managed with high-flow nasal cannula oxygen therapy.
is the risk? Am J Kidney Dis. 2020;75(1):105-113. (Review) Eur J Emerg Med. 2017;24(3):230-232. (Case report)
47. Younathan CM, Kaude JV, Cook MD, et al. Dialysis is not 63. Aksakal A, Saglam L, Kerget B, et al. Comparison of the ef-
indicated immediately after administration of nonionic contrast fectiveness of high-flow and conventional nasal cannula oxygen
agents in patients with end-stage renal disease treated by therapy in pulmonary embolism patients with acute hypoxemic
maintenance dialysis. AJR Am J Roentgenol. 1994;163(4):969- respiratory failure. Tuberk Toraks. 2021;69(4):469-476. (Prospec-
971. (Review) tive randomized controlled trial; 58 patients)
48. Di Minno MN, Ambrosino P, Ambrosini F, et al. Prevalence 64. Johnson KG. APAP, BPAP, CPAP, and new modes of positive air-
of deep vein thrombosis and pulmonary embolism in pa- way pressure therapy. Adv Exp Med Biol. 2022;1384:297-330.
tients with superficial vein thrombosis: a systematic review (Review)
and meta-analysis. J Thromb Haemost. 2016;14(5):964-972. 65. Pinsky MR. The right ventricle: interaction with the pulmonary
(Meta-analysis; 9326 patients) circulation. Crit Care. 2016;20(1):266. (Review)
49. Shirkhodaie C, Lattell J, Paul J, et al. Concomitant lower- 66. Crager SE, Humphreys C. Right ventricular failure and pulmo-
AUGUST 2023 • www.ebmedicine.net 23 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
nary hypertension. Emerg Med Clin North Am. 2022;40(3):519- Opin Pulm Med. 2022;28(5):384-390. (Opinion)
537. (Review) 84. Goldhaber SZ. ECMO and surgical embolectomy: two potent
67. Cassady SJ, Ramani GV. Right heart failure in pulmonary hyper- tools to manage high-risk pulmonary embolism. J Am Coll
tension. Cardiol Clin. 2020;38(2):243-255. (Review) Cardiol. 2020;76(8):912-915. (Opinion)
68. Lim P, Delmas C, Sanchez O, et al. Diuretic vs. placebo in 85.* Rivera-Lebron BN, Rali PM, Tapson VF. The PERT concept: a
intermediate-risk acute pulmonary embolism: a randomized step-by-step approach to managing pulmonary embolism.
clinical trial. Eur Heart J Acute Cardiovasc Care. 2022;11(1):2-9. Chest. 2021;159(1):347-355. (Review)
(Prospective randomized controlled trial; 276 patients) DOI: 10.1016/j.chest.2020.07.065
69. Ternacle J, Gallet R, Mekontso-Dessap A, et al. Diuretics in 86. Jolly M, Phillips J. Pulmonary embolism: current role of catheter
normotensive patients with acute pulmonary embolism and treatment options and operative thrombectomy. Surg Clin
right ventricular dilatation. Circ J. 2013;77(10):2612-2618. (Ret- North Am. 2018;98(2):279-292. (Review)
rospective case series; 70 patients) 87. Al-Khadra Y, Missula V, Al-Bast B, et al. Outcomes of mechani-
70. Schouver ED, Chiche O, Bouvier P, et al. Diuretics versus vol- cal thrombectomy compared with systemic thrombolysis in
ume expansion in acute submassive pulmonary embolism. Arch pulmonary embolism: a comprehensive evaluation from the
Cardiovasc Dis. 2017;110(11):616-625. (Prospective random- National Inpatient Sample Database. J Endovasc Ther. 2022.
ized controlled trial; 46 patients) (Database review; 16,890 patients)
71. Schultz J, Andersen A, Lyhne MD, et al. Terlipressin increases 88. Rivera-Lebron B, McDaniel M, Ahrar K, et al. Diagnosis, treat-
systemic and lowers pulmonary arterial pressure in experimen- ment and follow up of acute pulmonary embolism: consensus
tal acute pulmonary embolism. Crit Care Med. 2020;48(4):e308- practice from the PERT consortium. Clin Appl Thromb Hemost.
e315. (Animal study) 2019;25:1-16. (Review)
72. Kline JA, Puskarich MA, Jones AE, et al. Inhaled nitric oxide 89. Hobohm L, Farmakis IT, Munzel T, et al. Pulmonary embo-
to treat intermediate risk pulmonary embolism: a multicenter lism and pregnancy-challenges in diagnostic and therapeu-
randomized controlled trial. Nitric Oxide. 2019;84:60-68. (Ran- tic decisions in high-risk patients. Front Cardiovasc Med.
domized controlled trial; 38 patients) 2022;9:856594. (Review)
73. Palmirotta R. Direct oral anticoagulants (DOAC): are we ready 90. van der Pol LM, Tromeur C, Bistervels IM, et al. Pregnancy-
for a pharmacogenetic approach? J Pers Med. 2021;12(1):17. adapted YEARS algorithm for diagnosis of suspected pul-
(Review) monary embolism. N Engl J Med. 2019;380(12):1139-1149.
74. Wells PS, Kovacs MJ, Bormanis J, et al. Expanding eligibility for (Prospective observational study; 510 patients)
outpatient treatment of deep venous thrombosis and pulmo- 91. Righini M, Robert-Ebadi H, Elias A, et al. Diagnosis of pul-
nary embolism with low-molecular-weight heparin: a compari- monary embolism during pregnancy: a multicenter pro-
son of patient self-injection with homecare injection. Arch Intern spective management outcome study. Ann Intern Med.
Med. 1998;158(16):1809-1812. (Prospective observational 2018;169(11):766-773. (Prospective observational study; 441
study; 194 patients) patients)
75. Leentjens J, Peters M, Esselink AC, et al. Initial anticoagulation 92. Bates SM. Pulmonary embolism in pregnancy. Semin Respir Crit
in patients with pulmonary embolism: thrombolysis, Care Med. 2021;42(2):284-298. (Review)
unfractionated heparin, LMWH, fondaparinux, or DOACs? Br J 93. Starekova J, Nagle SK, Schiebler ML, et al. Pulmonary MRA
Clin Pharmacol. 2017;83(11):2356-2366. (Review) during pregnancy: early experience with ferumoxytol. J Magn
76. Marti C, John G, Konstantinides S, et al. Systemic thrombolytic Reson Imaging. 2022. (Observational review; 98 patients)
therapy for acute pulmonary embolism: a systematic review and 94. Ercan S, Ozkan S, Yucel N, et al. Establishing reference intervals
meta-analysis. Eur Heart J. 2015;36(10):605-614. (Review) for D-dimer to trimesters. J Matern Fetal Neonatal Med.
77. Igneri LA, Hammer JM. Systemic thrombolytic therapy for 2015;28(8):983-987. (Retrospective review; 1448 patients)
massive and submassive pulmonary embolism. J Pharm Pract. 95. Wiegers HMG, Middeldorp S. Contemporary best practice in
2020;33(1):74-89. (Review) the management of pulmonary embolism during pregnancy.
78. Jaff MR, McMurtry MS, Archer SL, et al. Management of mas- Ther Adv Respir Dis. 2020;14:1-20. (Review)
sive and submassive pulmonary embolism, iliofemoral deep 96. Poor HD. Pulmonary thrombosis and thromboembolism in
vein thrombosis, and chronic thromboembolic pulmonary COVID-19. Chest. 2021;160(4):1471-1480. (Review)
hypertension: a scientific statement from the American Heart
97. Kwee RM, Adams HJA, Kwee TC. Pulmonary embolism in
Association. Circulation. 2011;123(16):1788-1830. (Scientific
patients with COVID-19 and value of D-dimer assessment: a
statement)
meta-analysis. Eur Radiol. 2021;31(11):8168-8186. (Meta analy-
79. Brown K, Devarapally S, Lee L, et al. Catheter directed sis)
thrombolysis of pulmonary embolism. StatPearls [Internet].
98. Cui LY, Cheng WW, Mou ZW, et al. Risk factors for pulmonary
Treasure Island (FL): StatPearls Publishing; 2022. (Review)
embolism in patients with COVID-19: a systemic review and
80. Bashir R, Foster M, Iskander A, et al. Pharmacomechanical meta-analysis. Int J Infect Dis. 2021;111:154-163. (Meta analy-
catheter-directed thrombolysis with the bashir endovascular sis)
catheter for acute pulmonary embolism: the RESCUE study.
99. Adams E, Broce M, Mousa A. Proposed algorithm for treatment
JACC Cardiovasc Interv. 2022;15(23):2427-2436. (Prospective
of pulmonary embolism in COVID-19 patients. Ann Vasc Surg.
observational study; 109 patients)
2021;70:282-285. (Opinion)
81. Chandra VM, Khaja MS, Kryger MC, et al. Mechanical aspira-
tion thrombectomy for the treatment of pulmonary embolism: a
systematic review and meta-analysis. Vasc Med. 2022;27(6):574-
584. (Review)
82.* Desai KR. Mechanical thrombectomy in pulmonary embolism:
ready for prime time? JACC Cardiovasc Interv. 2021;14(3):330-
332. (Opinion) DOI: 10.1016/j.jcin.2020.11.002
83. de Perrot M. Role of extracorporeal membrane oxygenation
and surgical embolectomy in acute pulmonary embolism. Curr
AUGUST 2023 • www.ebmedicine.net 24 ©2023 EB MEDICINE
n CME Questions 6. If the normal threshold for a D-dimer test
Current subscribers receive CME credit is 500 ng/mL, then the accepted D-dimer
absolutely free by completing the threshold for a 75-year-old woman would be:
following test. Each issue includes 4 AMA a. 75 ng/mL
PRA Category 1 CreditsTM, 4 ACEP b. 500 ng/mL
Category I credits, 4 AAFP Prescribed c. 750 ng/mL
credits, and 4 AOA Category 2-B credits. d. 1000 ng/mL
Online testing is available for current and archived
issues. To receive your free CME credits for this 7. The Hampton hump on a chest x-ray of
issue, scan the QR code below with your a person with a pulmonary embolism is
smartphone or visit www.ebmedicine.net/0823 described as:
a. A peripheral wedge-shaped opacification
b. An elevation of the right hemidiaphragm
c. A right-sided mediastinal bulge
d. An irregularly shaped aortic silhouette
8. When comparing computed tomography
pulmonary angiography (CTPA) and
1. Which is included in the Virchow triad as a ventilation/perfusion (V/Q) studies for the
cause of venous thrombus formation? diagnosis of pulmonary embolism, which of the
a. Thrombocytopenia following is an accurate statement?
b. Hypoxia a. V/Q scans are more sensitive than CTPA
c. Hyperventilation b. CTPA has a sensitivity approximately 10%
d. Venous stasis greater than V/Q scanning
c. Both exhibit an approximate 95% sensitivity
2. What is the most common genetic factor d. Neither test is >85% sensitive
leading to a hypercoagulable state?
a. Factor V Leiden 9. A person with a pulmonary embolism, no
b. Thalassemia major hemodynamic instability, right ventricular
c. Trisomy 21 dilation, and normal troponin and natriuretic
d. Congenital adrenal hyperplasia peptide levels would be classified by the
European Cardiology Society as:
3. In the PIOPED II study, what was the most a. Low risk
common risk factor found for pulmonary b. Intermediate-low risk
embolism? c. Intermediate-high risk
a. Recent trauma d. High risk
b. Body mass index <25
c. Hypertension 10. A pregnant patient in her third trimester has a
d. Female sex YEARS score of 0 and a D-dimer >1000 ng/mL.
What would be the next step in her care?
4. In what percentage of patients with pulmonary a. CTPA
embolism are abnormalities found in the b. Immediate administration of tissue
cardiac examination? plasminogen activator
a. 1% c. Compression ultrasonography
b. 10% d. Discharge to home
c. 22%
d. 78%
5. Visual cyanosis requires what degree of
hemoglobin desaturation?
a. 1 g/dL
b. 3-5 g/dL
c. 10 g/dL
d. There is no specific value
AUGUST 2023 • www.ebmedicine.net 25 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
Stay up-to-date on the most relevant
topics in emergency medicine with EMplify
at www.ebmedicine.net/podcast
The Emergency Medicine Practice Editorial Board
EDITOR-IN-CHIEF Daniel J. Egan, MD Charles V. Pollack Jr., MA, MD, CRITICAL CARE EDITORS
Andy Jagoda, MD, FACEP Harvard Affiliated Emergency FACEP, FAAEM, FAHA, FACC, William A. Knight IV, MD,
Professor and Chair Emeritus, Medicine Residency, FESC FACEP, FNCS
Department of Emergency Massachusetts General Hospital/ Clinician-Scientist, Department Associate Professor of
Medicine; Director, Center for Brigham and Women's Hospital, of Emergency Medicine, Emergency Medicine and
Emergency Medicine Education Boston, MA University of Mississippi School Neurosurgery, Medical Director,
and Research, Icahn School of of Medicine, Jackson MS EM Advanced Practice Provider
Marie-Carmelle Elie, MD
Medicine at Mount Sinai, New Professor and Chair, Department Ali S. Raja, MD, MBA, MPH Program; Associate Medical
York, NY of Emergency Medicine Executive Vice Chair, Emergency Director, Neuroscience ICU,
ASSOCIATE EDITOR-IN-CHIEF University of Alabama at Medicine, Massachusetts General University of Cincinnati,
Birmingham, Birmingham, AL Hospital; Professor of Emergency Cincinnati, OH
Kaushal Shah, MD, FACEP Medicine and Radiology, Harvard
Assistant Dean of Academic Nicholas Genes, MD, PhD Scott D. Weingart, MD, FCCM
Medical School, Boston, MA Editor-in-Chief, emCrit.org
Advising, Vice Chair of Clinical Assistant Professor,
Education, Professor of Ronald O. Perelman Department Robert L. Rogers, MD, FACEP, PHARMACOLOGY EDITOR
Clinical Emergency Medicine, of Emergency Medicine, NYU FAAEM, FACP
Grossman School of Medicine, Assistant Professor of Emergency Aimee Mishler, PharmD, BCPS
Department of Emergency
New York, NY Medicine, The University of Emergency Medicine Pharmacist,
Medicine, Weill Cornell School of
Maryland School of Medicine, St. Luke's Health System,
Medicine, New York, NY Michael A. Gibbs, MD, FACEP
Baltimore, MD Boise, ID
EDITORIAL BOARD Professor and Chair, Department
RESEARCH EDITOR
of Emergency Medicine, Alfred Sacchetti, MD, FACEP
Saadia Akhtar, MD, FACEP Carolinas Medical Center, Assistant Clinical Professor, Joseph D. Toscano, MD
Associate Professor, Department University of North Carolina Department of Emergency Chief, Department of Emergency
of Emergency Medicine, School of Medicine, Medicine, Thomas Jefferson Medicine, San Ramon Regional
Associate Dean for Graduate Chapel Hill, NC University, Philadelphia, PA Medical Center, San Ramon, CA
Medical Education, Program
Director, Emergency Medicine Steven A. Godwin, MD, FACEP Robert Schiller, MD INTERNATIONAL EDITORS
Residency, Mount Sinai Beth Professor and Chair, Department Chair, Department of Family
Peter Cameron, MD
Israel, New York, NY of Emergency Medicine, Medicine, Beth Israel Medical
Academic Director, The Alfred
Assistant Dean, Simulation Center; Senior Faculty, Family
William J. Brady, MD, FACEP, Emergency and Trauma Centre,
Education, University of Medicine and Community
FAAEM Monash University, Melbourne,
Florida COM-Jacksonville, Health, Icahn School of Medicine
Professor of Emergency Medicine Australia
Jacksonville, FL at Mount Sinai, New York, NY
and Medicine; Medical Director, Andrea Duca, MD
Emergency Management, Joseph Habboushe, MD MBA Scott Silvers, MD, FACEP
Attending Emergency Physician,
UVA Medical Center; Medical Assistant Professor of Clinical Associate Professor of
Ospedale Papa Giovanni XXIII,
Director, Albemarle County Fire Emergency Medicine, Emergency Medicine, Chair of
Bergamo, Italy
Rescue, Charlottesville, VA Department of Emergency Facilities and Planning, Mayo
Medicine, Weill Cornell School Clinic, Jacksonville, FL Suzanne Y.G. Peeters, MD
Calvin A. Brown III, MD of Medicine, New York, NY; Co- Attending Emergency Physician,
Director of Physician Corey M. Slovis, MD, FACP,
founder and CEO, MDCalc Flevo Teaching Hospital, Almere,
Compliance, Credentialing FACEP
The Netherlands
and Urgent Care Services, Eric Legome, MD Professor and Chair Emeritus,
Department of Emergency Chair, Emergency Medicine, Department of Emergency Edgardo Menendez, MD,
Medicine, Brigham and Women's Mount Sinai West & Mount Sinai Medicine, Vanderbilt University FIFEM
Hospital, Boston, MA St. Luke's; Vice Chair, Academic Medical Center, Nashville, TN Professor in Medicine and
Affairs for Emergency Medicine, Emergency Medicine; Director of
Peter DeBlieux, MD Stephen H. Thomas, MD, MPH
Mount Sinai Health System, Icahn EM, Churruca Hospital of Buenos
Professor of Clinical Medicine, Department of Emergency
School of Medicine at Mount Aires University, Buenos Aires,
Louisiana State University School Medicine, Beth Israel Deaconess
Sinai, New York, NY Argentina
of Medicine; Chief Experience Medical Center and Harvard
Officer, University Medical Keith A. Marill, MD, MS Medical School, Boston, MA Dhanadol Rojanasarntikul, MD
Center, New Orleans, LA Associate Professor, Department Attending Physician, Emergency
Ron M. Walls, MD
of Emergency Medicine, Harvard Medicine, King Chulalongkorn
Deborah Diercks, MD, MS, Professor and COO, Department
Medical School, Massachusetts Memorial Hospital; Faculty
FACEP, FACC of Emergency Medicine, Brigham
General Hospital, Boston, MA of Medicine, Chulalongkorn
Professor and Chair, Department and Women's Hospital, Harvard
University, Thailand
of Emergency Medicine, Angela M. Mills, MD, FACEP Medical School, Boston, MA
University of Texas Southwestern Professor and Chair, Department Edin Zelihic, MD
Medical Center, Dallas, TX of Emergency Medicine, Head, Department of Emergency
Columbia University Vagelos Medicine, Leopoldina Hospital,
College of Physicians & Schweinfurt, Germany
Surgeons, New York, NY
AUGUST 2023 • www.ebmedicine.net 27 © 2023 EB MEDICINE. ALL RIGHTS RESERVED.
Points & Pearls
QUICK READ
Evidence-Based Management
of Pulmonary Embolism in
the Emergency Department
AUGUST 2023 | VOLUME 25 | ISSUE 8
Points
• Even with appropriate care, approximately 15%-
Pearls
30% of patients with pulmonary embolism (PE) • The most common risk factors for PE are fe-
will die within 90 days,1-3 potentially from the un- male sex, immobilization, recent surgery, ma-
derlying medical pathology that led to the clot. lignancy, and travel >4 hours in the previous
• Chest pain, dyspnea, and hemoptysis are com- month. Table 1 lists other clinical risk factors.
mon signs of PE; establishing the time of onset of • Primary pulmonary pathologies such as COPD,
symptoms can help determine the cause. asthma, pneumonia, pneumothorax, and
• Isolated syncope with no other symptoms sug- pleuritis should be on the differential for sus-
gestive for PE is not an indication for an evalua- pected PE.
tion for thromboembolic disease. • Vital signs in PE may be normal; hypotension is
• Other findings in PE include tachypnea, tachycar- the least specific vital sign (5%).20
dia, cyanosis, lower extremity edema, and deep • Clinical gestalt alone demonstrates poor
vein thrombosis. performance in excluding the need for further
• Scoring systems for determining clinical pretest testing.25,26
probability include the Wells, rGeneva, PERC, • D-dimer assays should be used in combination
and YEARS criteria. (See Table 2.) with a patient‘s clinical pretest probability to
• Electrocardiogram is useful, though not diagnos- determine whether PE can be ruled out or ad-
tic, with 25% of patients having normal tracings.27 ditional diagnostic studies are needed.29
• Age-adjusted D-dimer should be used. • CTPA is sensitive and specific for the presence
• D-dimer levels change with duration of the clot.29 of clots in the pulmonary vascular tree.39,40
• Serum troponin levels32 and elevations in serum Figure 1 shows PEs on CTPA.
natriuretic peptide levels are more valuable as • Maintaining pulse oximetry >95 is the treat-
prognostic for severity of illness and mortality ment goal, delivered via nasal cannula, high-
than in diagnosis of PE. flow nasal cannula, or noninvasive positive-
• Chest radiographs have little value in confirming pressure ventilation.
or excluding PE; however, they may be helpful in • Anticoagulation is the mainstay of treatment to
identifying alternative pathology.35-38 prevent further clot propagation. See Table 6
• The estimated glomerular filtration rate (eGFR) for recommendations for initial anticoagulant
can be used as a risk stratification tool to predict therapy.
contrast-induced nephropathy following comput-
ed tomographic pulmonary arteriography (CTPA).
• Concomitant lower extremity DVTs and PEs can interventionalist clinician to administer.
occur in 40%-70% of patients.49 • Thrombectomy, operative thoracotomy, and
• A multiorgan point-of-care ultrasound protocol of extracorporeal membrane oxygenation (ECMO)
examination of the heart, lungs, and leg has 90% may be options for some patients, as available.
sensitivity and 86% specificity for PE.50 • The pulmonary embolism response team (PERT) is
• Prognostic risk classifications use physiologic and a multidisciplinary team of clinicians that assists in
diagnostic criteria to determine severity of PE. coordination of care in institutions where available.
Tables 3, 4, and 5 present 3 classification systems. • PE in pregnant patients is a significant cause of
• Fluid management and vasoactive agents may be maternal mortality. Though low-molecular weight
appropriate in some circumstances. heparin can be given to low-risk patients, higher
• Systemic thrombolytics are reserved for use in un- risk patients require input from a PERT team or
stable patients. See Table 7 for contraindications. multiple consultants.
• Thrombolytics can be delivered via pulmo- • Patients meeting Hestia criteria (see Table 8) may
nary artery catheter, but this use requires an be candidates for outpatient management.
AUGUST 2023 • www.ebmedicine.net 28 ©2023 EB MEDICINE
You might also like
- 00130478-202105000-00006 Serial Neurologic Assessment in Pediatrics (SNAP) : A New Tool For Bedside Neurologic Assessment of Critically Ill ChildrenDocument13 pages00130478-202105000-00006 Serial Neurologic Assessment in Pediatrics (SNAP) : A New Tool For Bedside Neurologic Assessment of Critically Ill ChildrenYo MeNo ratings yet
- Case Files Emergency MedicineDocument480 pagesCase Files Emergency MedicinestarrnewmanpaNo ratings yet
- Case-Based Pace, ICDs, and CRT Volume 1Document234 pagesCase-Based Pace, ICDs, and CRT Volume 1oxequlalisNo ratings yet
- Omnibus Risk EstimatorDocument6 pagesOmnibus Risk EstimatorranaNo ratings yet
- The Last Bloodcarver by Vanessa LeDocument15 pagesThe Last Bloodcarver by Vanessa LeMacmillan KidsNo ratings yet
- Diabetic EmergenciesDocument24 pagesDiabetic EmergencieshabibfmNo ratings yet
- Toxic Ingestions Pediatric EmergencyDocument24 pagesToxic Ingestions Pediatric EmergencyXimenaEspinaNo ratings yet
- Surgical AirwaysDocument24 pagesSurgical AirwaysMed. TrackNo ratings yet
- Advances in Cardiac Resuscitation in The Emergency Department 1Document24 pagesAdvances in Cardiac Resuscitation in The Emergency Department 1Jhon Bayron Muñoz QuinteroNo ratings yet
- 0822 Cardiac Valve EmergenciesDocument23 pages0822 Cardiac Valve EmergenciessarahmacielNo ratings yet
- AngioedemaDocument24 pagesAngioedemaMed. TrackNo ratings yet
- Pediatric Septic ShockDocument24 pagesPediatric Septic ShockBRENDA AMARONo ratings yet
- Community Acquired Pneumonia 2Document22 pagesCommunity Acquired Pneumonia 2carosegurallNo ratings yet
- Hypertensive EmergenciesDocument28 pagesHypertensive EmergenciesluonganhsiNo ratings yet
- Neuro Trauma PICDocument19 pagesNeuro Trauma PICNadir MonteroNo ratings yet
- Clasificacion de Tumores Cerebreales de La OMS 2016 Articulo de RevisionDocument17 pagesClasificacion de Tumores Cerebreales de La OMS 2016 Articulo de RevisionSebastian SalvadorNo ratings yet
- Traumatic Spinal Cord Injury 2018Document16 pagesTraumatic Spinal Cord Injury 2018LEONARDO ANTONIO CASTILLO ZEGARRANo ratings yet
- HFNC Noninvasive VentilationDocument24 pagesHFNC Noninvasive VentilationAbody MenaNo ratings yet
- Gunshot Wounds - Ballistic Trauma in The Emergency DepartmentDocument30 pagesGunshot Wounds - Ballistic Trauma in The Emergency DepartmentMulugeta DagneNo ratings yet
- Procedural Sedation AnalgesiaDocument24 pagesProcedural Sedation Analgesiabenitez1228No ratings yet
- Disorders of The Cauda EquinaDocument19 pagesDisorders of The Cauda Equinanight.shadowNo ratings yet
- 0413 Massive Upper GI BleedingDocument12 pages0413 Massive Upper GI BleedingIsaura MendezNo ratings yet
- Obstetric Life Support ManualDocument71 pagesObstetric Life Support Manualtf.jorgeNo ratings yet
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 pagesDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahNo ratings yet
- Emergency Department Management of Acute Asthma ExacerbationsDocument32 pagesEmergency Department Management of Acute Asthma ExacerbationsFercho MedNo ratings yet
- Identifying Emergency Department Patients With Chest Pain Who Are at Low Risk For Acute Coronary SyndromesDocument24 pagesIdentifying Emergency Department Patients With Chest Pain Who Are at Low Risk For Acute Coronary SyndromesCarlos Alejandro Rojas CastellanosNo ratings yet
- Updates and Controversies in The Early Management of Sepsis and Septic ShockDocument34 pagesUpdates and Controversies in The Early Management of Sepsis and Septic Shockdogui0071No ratings yet
- Blunt Cardiac InjuryDocument23 pagesBlunt Cardiac InjuryDaniel Cárdenas RojasNo ratings yet
- Guia 2023 de Manejo de SdraDocument9 pagesGuia 2023 de Manejo de SdraBrian Antonio Veramatos LopezNo ratings yet
- 1115 Ocular Injuries PDFDocument24 pages1115 Ocular Injuries PDFAndrea Valentina Villarroel BarriosNo ratings yet
- HSA ContinuunDocument35 pagesHSA ContinuunJose DavidNo ratings yet
- Infective EndocarditisDocument24 pagesInfective EndocarditisNicolás HonoresNo ratings yet
- Topical Issues in Anesthesia 2016Document207 pagesTopical Issues in Anesthesia 2016Ketzalzin DmgNo ratings yet
- Supraglottic Airway DevicesDocument20 pagesSupraglottic Airway Devicesvaletg27No ratings yet
- Advances in Emergent Airway Management in PediatricsDocument19 pagesAdvances in Emergent Airway Management in PediatricsLuis Miguel VillanuevaNo ratings yet
- 0115 Seizures and SEDocument28 pages0115 Seizures and SEGavin TexeirraNo ratings yet
- MS4 Residency Survival GuideDocument202 pagesMS4 Residency Survival GuideShibb ShubbNo ratings yet
- Practical Emergency Resuscitation and Critical Care, 2nd Edition (Original PDF From Publisher)Document655 pagesPractical Emergency Resuscitation and Critical Care, 2nd Edition (Original PDF From Publisher)Duk Han KimNo ratings yet
- Jurnal FartokDocument195 pagesJurnal FartokMustafa RahmatillahNo ratings yet
- ABCDE. The Assessment of The Critically Ill PatientDocument4 pagesABCDE. The Assessment of The Critically Ill PatientGani mutiaraNo ratings yet
- Multiple Sclerosis and Other Cns in Ammatory Diseases: Guest Editor: Dean M. Wingerchuk, MD, MSC, FRCPC, FaanDocument318 pagesMultiple Sclerosis and Other Cns in Ammatory Diseases: Guest Editor: Dean M. Wingerchuk, MD, MSC, FRCPC, FaanabelNo ratings yet
- Review Course Vascular - AnaesthesiaDocument36 pagesReview Course Vascular - AnaesthesiazaidNo ratings yet
- 0221 Community-Acquired-PneumoniaDocument29 pages0221 Community-Acquired-PneumoniaDiego YanezNo ratings yet
- Intracranial Pressure: Current Perspectives On Physiology and MonitoringDocument11 pagesIntracranial Pressure: Current Perspectives On Physiology and MonitoringCristian Andres Arancibia GomezNo ratings yet
- Ventilator Management of Adult Patients in The Emergency DepartmentDocument20 pagesVentilator Management of Adult Patients in The Emergency DepartmentLeandro NogueiraNo ratings yet
- Splenic Trauma WSES Classification and GuidelinesDocument27 pagesSplenic Trauma WSES Classification and GuidelinespgmzNo ratings yet
- Emergency Department Management of Cellulitis and Other Skin andDocument24 pagesEmergency Department Management of Cellulitis and Other Skin andJesus CedeñoNo ratings yet
- Ebm Emergency Department Management of Patients With Thermal Burns Trauma Cme 1Document24 pagesEbm Emergency Department Management of Patients With Thermal Burns Trauma Cme 1Luis GuerraNo ratings yet
- Spinal Cord Anatomy and LocalizationDocument18 pagesSpinal Cord Anatomy and LocalizationJuanCarlosRiveraAristizabalNo ratings yet
- Practical: Invasive Mechanical VentilationDocument307 pagesPractical: Invasive Mechanical VentilationDayana CheriyanNo ratings yet
- Overview of Complications Occurring in The Post-Anesthesia Care UnitDocument14 pagesOverview of Complications Occurring in The Post-Anesthesia Care UnitShahabuddin ShaikhNo ratings yet
- Management of Deep Vein Thrombosis in The Emergency DepartmentDocument24 pagesManagement of Deep Vein Thrombosis in The Emergency Departmentmundode paisajes100% (1)
- Libro VM Obeso 2018 PDFDocument305 pagesLibro VM Obeso 2018 PDFNataly Osorio MarínNo ratings yet
- Anaesthesia For Trauma PatientsDocument5 pagesAnaesthesia For Trauma Patientscahya candraNo ratings yet
- Recruitment Maneuvers and PEEP TitrationDocument17 pagesRecruitment Maneuvers and PEEP TitrationDiego Cruces OrdoñezNo ratings yet
- AAP Emergencies Ped Drug Doses PDFDocument20 pagesAAP Emergencies Ped Drug Doses PDFUlvionaNo ratings yet
- Textbook of Echocardiography For Intensivists and Emergency PhysiciansDocument567 pagesTextbook of Echocardiography For Intensivists and Emergency PhysiciansYeseniaNo ratings yet
- AsfixiabuenoDocument24 pagesAsfixiabuenoAdrianaGallardoTapiaNo ratings yet
- 792Document527 pages792MarcNicaNo ratings yet
- CCCDocument487 pagesCCCSlaviša KovačevićNo ratings yet
- Major Incident Medical Management and Support: The Practical Approach at the SceneFrom EverandMajor Incident Medical Management and Support: The Practical Approach at the SceneNo ratings yet
- NCLEX CardiovascularDocument93 pagesNCLEX CardiovascularYaoling WenNo ratings yet
- Japanese Triple Peptide Breakthrough Regenerates CellsDocument6 pagesJapanese Triple Peptide Breakthrough Regenerates CellsHalter Michael KareniNo ratings yet
- Pathology-MCQs - PDF Copy CopyDocument130 pagesPathology-MCQs - PDF Copy CopyMhamad MamasenyNo ratings yet
- General Pathology - Topical Past Papers-1Document21 pagesGeneral Pathology - Topical Past Papers-1RazaNo ratings yet
- Soebandiri Dept of Medicine, Division of Hematology Airlangga University School of Medicine SurabayaDocument17 pagesSoebandiri Dept of Medicine, Division of Hematology Airlangga University School of Medicine SurabayaniluhayusumbawatiNo ratings yet
- THROMBOSISDocument18 pagesTHROMBOSISShruti Verma100% (1)
- NatokinaseDocument6 pagesNatokinasefabadioNo ratings yet
- Secondary HemostasisDocument9 pagesSecondary HemostasisMedicah Simon PeligrinoNo ratings yet
- Types, Causes, Symptoms of AnemiaDocument66 pagesTypes, Causes, Symptoms of AnemiaKristel AnneNo ratings yet
- Arterial Thrombosis by AbrarDocument20 pagesArterial Thrombosis by AbrarZain HadiNo ratings yet
- Clot Architecture Is Altered in Abdominal Aortic Aneurysms and Correlates With Aneurysm SizeDocument8 pagesClot Architecture Is Altered in Abdominal Aortic Aneurysms and Correlates With Aneurysm SizeOnur KNo ratings yet
- L-6C-Tranportation CBEDocument18 pagesL-6C-Tranportation CBEPratibhaNo ratings yet
- Aloe Vera Gel as an Anti-Blood CoagulantDocument8 pagesAloe Vera Gel as an Anti-Blood CoagulantDanica Bondoc50% (2)
- Acute Infectious Purpura FulminansDocument15 pagesAcute Infectious Purpura FulminansFranklin Aranda100% (2)
- Anatomy Physiology Exam QuestionsDocument160 pagesAnatomy Physiology Exam Questionssyafi zulNo ratings yet
- Anticoagulant, Fibrinolytic and Antiplatelet Drugs GuideDocument28 pagesAnticoagulant, Fibrinolytic and Antiplatelet Drugs GuideJagdesh SajnaniNo ratings yet
- Minutes) PRE TESTDocument13 pagesMinutes) PRE TESTRanes AndyNo ratings yet
- IJBM2023 - 244 - Chitosan-Based Hydrogel Wound Dressing From Mechanism To Applications, A ReviewDocument17 pagesIJBM2023 - 244 - Chitosan-Based Hydrogel Wound Dressing From Mechanism To Applications, A Reviewmaolei0101No ratings yet
- Module 3 ReviDocument35 pagesModule 3 ReviJohn Van Dave TaturoNo ratings yet
- Background + RefDocument40 pagesBackground + Refبشير حيدرNo ratings yet
- Hemostasis, Hemorrhagic Disorders and ThrombosisDocument114 pagesHemostasis, Hemorrhagic Disorders and ThrombosisZeeNo ratings yet
- Case Study About Ischemic StrokeDocument5 pagesCase Study About Ischemic StrokeMoath MahmoudNo ratings yet
- How To Succeed in Your Livestock Production by Understanding Animal Health?Document43 pagesHow To Succeed in Your Livestock Production by Understanding Animal Health?Valiant Dominic D. VelardeNo ratings yet
- DIC Case StudyDocument3 pagesDIC Case StudyJuliaNo ratings yet
- Antitrombotik, PPT 7Document66 pagesAntitrombotik, PPT 7Rizky Saraswati IndraputriNo ratings yet
- Case Study On Pulmonary EmbolismDocument12 pagesCase Study On Pulmonary EmbolismJobelle Acena100% (2)
- Cid en AdultosDocument38 pagesCid en AdultosJosephGabrielNo ratings yet
- PathologyDocument30 pagesPathologyTenorski baritonNo ratings yet
- 23 DC Acenocoumarol A Review PDFDocument6 pages23 DC Acenocoumarol A Review PDFnaga chaitanyaNo ratings yet