Professional Documents
Culture Documents
Competence To Consent and Its Relationship With Cognitive Function in Patients With Schizophrenia
Uploaded by
Julio DelgadoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Competence To Consent and Its Relationship With Cognitive Function in Patients With Schizophrenia
Uploaded by
Julio DelgadoCopyright:
Available Formats
MINI REVIEW
published: 12 April 2019
doi: 10.3389/fpsyt.2019.00195
Competence to Consent and Its
Relationship With Cognitive Function
in Patients With Schizophrenia
Norio Sugawara 1*, Norio Yasui-Furukori 2 and Tomiki Sumiyoshi 1
1
Department of Clinical Epidemiology, Translational Medical Center, National Center of Neurology and Psychiatry, Kodaira,
Japan, 2 Department of Neuropsychiatry, Hirosaki University School of Medicine, Hirosaki, Japan
Decisional capacity to consent is an emerging ethical and legal concept, and is closely
related to self-determination of patients facing important medical decisions or research
participations. Recently, the MacArthur Competence Assessment Tool (MacCAT), a
semi-structured interview consisting of four dimensions (Understanding, Appreciation,
Reasoning, and Expression of a Choice), was developed to assess the decisional
capacity. Decision-making capacity in a group of patients with schizophrenia, as
measured by the MacCAT, has been shown to be impaired in comparison with healthy
control people. However, this does not necessarily mean the presence of impaired
decisional capacity in all cases. Considering the real-world practice of obtaining informed
consent from patients with schizophrenia, it is important to evaluate the relationship
Edited by: between psychopathological features and decisional capacity of the illness. Negative
Renzo Bianchi,
University of Neuchâtel, Switzerland
symptoms of schizophrenia have been demonstrated to be related to the ability to
Reviewed by:
understand information relevant to the decision, reason rationally, and appreciate a
Julio Eduardo Armijo, situation and its consequences. On the other hand, positive symptoms, such as
Diego Portales University, Chile
delusions and hallucinations have been an inconsistent correlate of poor capacity.
Christopher James Ryan,
University of Sydney, Australia Furthermore, some studies indicate that impairment of cognitive function, a core
*Correspondence: symptom of schizophrenia, could be more largely associated with decisional capacity
Norio Sugawara than positive and negative symptoms. Therefore, it is reasonable to assume cognitive
nsnga@ncnp.go.jp
enhancement would enlarge the capacity to consent and promote autonomy in medical
Specialty section: treatment and research participation in patients with schizophrenia. Further studies are
This article was submitted to warranted to elucidate this and related issues.
Psychopathology,
a section of the journal Keywords: competence to consent, cognitive function, schizophrenia, MacArthur Competence Assessment Tools,
Frontiers in Psychiatry decisional capacity
Received: 30 November 2017
Accepted: 18 March 2019
Published: 12 April 2019
INTRODUCTION
Citation: Competence to consent for individuals with psychiatric symptoms or impaired cognitive
Sugawara N, Yasui-Furukori N and
functioning has become central to the debate on the informed consent in clinical care and research
Sumiyoshi T (2019) Competence to
Consent and Its Relationship With
settings. Clinicians and researchers bear the responsibilities to protect two aspects of human
Cognitive Function in Patients With rights; the right of competent patients to make choices about their medical care and the right of
Schizophrenia. incompetent patients to be protected from the potential harm of their decisions (1). However,
Front. Psychiatry 10:195. in real-world clinical settings, some patients with capacity were detained in hospital by law, or
doi: 10.3389/fpsyt.2019.00195 other patients with incapacity were admitted to hospital on a voluntary basis (2). In terms of
Frontiers in Psychiatry | www.frontiersin.org 1 April 2019 | Volume 10 | Article 195
Sugawara et al. Decisional Capacity in Schizophrenic Patients
clinical research, some patients with incapacity might have been a more consistent correlate of poor cognitive functioning
participated in clinical trials with their own consent. than have other subscales. However, all of above mentioned
Although several decision-making tasks specifically assess studies employed MacCAT-Clinical Research (MacCAT-CR)
decisional capacities (3, 4), the medical/psychiatric literature has for assessing participants’ decision-making abilities for clinical
commonly cited the following abilities as relevant to capacity research. So, the potential range of understanding subscales being
for informed consent: (1) understanding information relevant at least three times those of the other subscales might affect
to treatment decision making; (2) appreciating the personal inconsistent results of other subscales.
significance of treatment information, especially concerning one’s A longitudinal assessment for capacity, in terms of
own illness and the probable consequences of one’s treatment understanding, was conducted among participants in the
options; (3) reasoning with relevant information to engage in a Clinical Antipsychotic Trials of Intervention Effectiveness
logical process of weighting treatment options; and (4) expressing (CATIE) schizophrenia study (20). Over 18 months treatment,
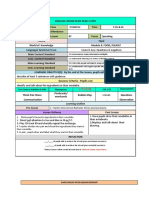
a choice (5). These are also the key elements of the MacArthur poorer baseline neurocognitive composite scores consisting
Competence Assessment Tool (MacCAT) (6) (Figure 1), which of processing speed, verbal memory, vigilance, reasoning, and
has been widely used for competence assessment (7). However, working memory, predicted falling below the critical decision-
the MacCAT is not clearly designed to provide a total score for making capacity threshold. In the same analysis, lower baseline
the assessment of decision-making capacity. Furthermore, the scores of understanding subscale also were associated with falling
abilities assessed in the MacCAT do not necessarily equate to the below the threshold during follow-up period.
abilities relevant to the assessment of decision-making capacity
in many jurisdictions.
Schizophrenia is a severe mental disorder that generally COGNITIVE MEASURES OF EACH DOMAIN
appears in late adolescence or early adulthood. Epidemiological AND COMPETENCE TO CONSENT
data indicates that prevalence of schizophrenia is approximately
1% in the worldwide population. Symptoms of schizophrenia Verbal communication plays an important role in informed
are clinically divided into three main categories of positive consent (21). Two studies demonstrated the relationship between
symptoms (delusions, disordered thoughts, and hallucinations), understanding subscales and verbal cognitive functioning based
negative symptoms (restricted affect and drive), and impairments on the Wechsler Adult Intelligence Scale (WAIS)-Revised
in cognitive function (8, 9). When schizophrenia was first (WAIS-R) (22, 23). In addition, other studies showed that
identified by Kraepelin, he noted the fundamental role of appreciation and reasoning subscales are associated with
cognitive impairment in this disorder, and called this dementia verbal comprehension composed of vocabulary, similarities, and
praecox (10). Although patients with schizophrenia are more information subtests from the WAIS–Third Edition (WAIS-III)
likely to lack the competence to consent than control groups (17, 24). Although previous studies indicated that verbal abilities
(6, 11), the diagnosis of schizophrenia cannot be equated with may predict competence to consent, the relationship between
decisional incapacity (12). Many researchers have investigated specific dimensions of decisional capacity and individual verbal
the associations of competence to consent with positive ability areas is still obscure.
and negative symptoms of schizophrenia (13–15). Although Memory is a complex process, consisting of registration,
poor capacity has correlated with negative symptoms more storage, retainment, and retrieval of information (25). Previous
consistently than positive symptoms, high levels of positive studies from US revealed that the RBANS memory index
symptoms, including disorganization, may affect competence had significant relationships to understanding, appreciation
to consent. Furthermore, recent empirical data suggest that (13) and reasoning subscales (16). Another study from Hong
neurocognitive functioning could explain a larger proportion of Kong indicated an association of understanding subscales
the variance in competence to consent than positive and negative with immediate and delayed logical memory from the
symptoms of schizophrenia (14, 16, 17). Wechsler Memory Scale (WMS) (5). Furthermore, some
Therefore, the aim of this narrative review is to elucidate (1) studies implicated that memory also underlies an aspect of
the relationships between cognitive function and competence to learning outcome (17, 24). Palmer et al. showed the relationship
consent, and (2) the interventions to compensate the decision- of learning composite scores with three subscales of MacCAT
making capacity in patients with schizophrenia. (understanding, appreciation, and reasoning) (24). They also
demonstrated that auditory and visual learning abilities could
affect the competence to consent (17).
COGNITIVE MEASURES OF MULTIPLE Working memory is a complex and multifaced construct
DOMAINS AND COMPETENCE to store and simultaneously manipulate a limited amount of
TO CONSENT information during short intervals. This capacity facilitates
further cognitive processing, such as response selection relevant
Several studies investigated the association of competence to for a specific context. Working memory comprises two short-
consent and cognitive measures such as the Mini-Mental State term information storage systems, the visuospatial network
Examination (MMSE) (15, 17–19) and the Repeatable Battery for for visual material and the phonologic loop for verbal-acoustic
the Assessment of Neuropsychological Status (RBANS) (13, 16). material (25). In the CATIE schizophrenia trial (14), this
On the whole, poor understanding subscales of MacCAT have cognitive domain was assessed by a computerized test of
Frontiers in Psychiatry | www.frontiersin.org 2 April 2019 | Volume 10 | Article 195
Sugawara et al. Decisional Capacity in Schizophrenic Patients
FIGURE 1 | Key elements of the MacArthur Competence Assessment Tool.
visuospatial working memory and letter number sequencing One intriguing study (31) showed that performance on a
test of auditory working memory. Specifically, working memory metacognition test was more closely related to decisional capacity
performance showed considerable bivariate relationships compared to executive function. Metacognition focuses on the
with the understanding, appreciation, and reasoning subscale level of self-confidence of patients in comparison with actual
scores from the MacCAT-CR. Furthermore, similar results performance, and predicts performance on the MacCAT-T (31).
were reported in other studies employing the letter number
sequencing test (5) and WAIS-III (17). A previous study
indicated an association between language comprehension and INTERVENTIONS TO COMPENSATE THE
working memory for sentences (26). Impairment of working DECISION-MAKING CAPACITY
memory in patients with schizophrenia might be consequent
upon verbal comprehension deficits. Although antipsychotic medication may improve decisional
Information processing represents a cognitive process of capacities (32, 33), clinicians and researchers should improve
taking information and encoding it to be understood and the informed consent process to maximize the decision-
recalled when appropriately cued. Processing speed is the making capacities of patients with schizophrenia. Providing
rapidity by which information processing occurs (25). Several information repeatedly and discussing presented information
studies showed bivariate correlation between processing with participants may strengthen the competence to consent
speed composite scores and understanding, appreciation, (16, 34). Furthermore, consent procedures via multimedia may
and reasoning subscales of MacCAT (14, 17, 24), but only facilitate the understanding to decide on complex or high-risk
the relationship between processing speed composite scores protocols (35). Naughton et al. conducted a small uncontrolled
and understanding subscales was replicated in a multiple study to evaluate the effect of metacognitive training (MCT) to
regression model (14). In patients with schizophrenia, processing improve a person’s awareness of cognitive biases and thinking
speed performance is strongly associated with global cognitive styles on decision-making capacities (36). MCT was found
deficits (27). Thus, processing speed may contribute to the to elicit improvement in understanding and reasoning, but
relationship between competence to consent and general not appreciation abilities of patients. Furthermore, cognitive
cognitive performance. remediation may improve competence to consent (37), providing
Executive function involves the simultaneous use of ethically adequate care, as well as clinical improvement.
information rather than the basic cognitive process, and governs
goal-directed behaviors or adaptive responses to complex or LIMITATIONS
novel situations. Generally, executive function is characterized
by several complex mental abilities, including unique skills Several limitations of this review should be acknowledged.
used for expansion, modulation, and implementation of goal- The principal limitation is the relatively small sample sizes
directed activities (25). This domain of cognitive function has in most studies, mentioned here, on the relationship between
been thought to rely on frontal lobe functions (28). A positive cognitive function and competence to consent in patients of
correlation has been reported between performance on the schizophrenia. Secondly, for ethical and legal reasons, only
Frontal Assessment Battery and total scores of the MacCAT (29) subjects who consented to participate in studies were included.
in chronic schizophrenia patients. Specifically, scores on the Even among individuals who consented to participate, 10% were
understanding subscale were most consistently correlated with too agitated to complete the entire assessments (6), suggesting
executive function (5, 24). that generalization of previous findings should be considered
Cognitive underpinnings underlying the limited decisional with caution. Thirdly, the MacCAT does not have a specific
capacity in psychiatric patients remain to be explored (30). cutoff to dichotomize competence vs. incompetence. This
Frontiers in Psychiatry | www.frontiersin.org 3 April 2019 | Volume 10 | Article 195
Sugawara et al. Decisional Capacity in Schizophrenic Patients
may obscure the associations between cognitive functions and process. Further studies are warranted to elucidate competence
decisional capacities (38). Finally, the MacCAT, which is based to consent and related issues.
on not only medical literature but also existing case law and
statutes, does not assess the emotional aspect of decisional AUTHOR CONTRIBUTIONS
capacities. Further studies investigating the relationship
between cognitive function and decisional capacities, NS, NY-F, and TS were involved in the study concept,
including both comprehensive emotional and legal aspects, interpretation of manuscript, critical revision of manuscript
are needed. for intellectual content, literature review, and drafting of
the manuscript.
CONCLUSIONS
FUNDING
Neurocognitive functioning may explain competence to consent
more accurately than positive and negative symptoms. Previous Funding for this study was provided by a Grant-in-Aid for
results have not indicated differential relationships between Scientific Research (C) (17K10347). The Ministry of Education,
specific cognitive ability areas and decision-making capacity. Culture, Sports, Science and Technology, Japan.
Interventions with multimedia procedure, MCT, etc. likely
enhance competence to consent. Cognitive remediation might ACKNOWLEDGMENTS
provide ethically adequate care as well as clinical improvement.
Clinicians and researchers are responsible for maximizing This research was well supported by staffs of Translational
decision-making capacities of patients in the informed consent Medical Center.
REFERENCES 13. Moser DJ, Schultz SK, Arndt S, Benjamin ML, Fleming FW, Brems
CS, et al. Capacity to provide informed consent for participation in
1. Grisso T, Appelbaum P. Assessing Competence to Consent to Treatment. A schizophrenia and HIV research. Am J Psychiatry. (2002). 159:1201–7.
Guide for Physicians and Other Health Professionals. New York, NY: Oxford doi: 10.1176/appi.ajp.159.7.1201
University Press (1998). 14. Stroup S, Appelbaum P, Swartz M, Patel M, Davis S, Jeste D, et al.
2. Owen GS, Szmukler G, Richardson G, David AS, Hayward P, Rucker J, Decision-making capacity for research participation among individuals
et al. Mental capacity and psychiatric in-patients: implications for the new in the CATIE schizophrenia trial. Schizophr Res. (2005). 80:1–8.
mental health law in England and Wales. Br J Psychiatry. (2009). 195:257–63. doi: 10.1016/j.schres.2005.08.007
doi: 10.1192/bjp.bp.108.059782. 15. Lan TH, Wu BJ, Chen HK, Liao HY, Lee SM, Sun HJ. Validation
3. Toplak ME, Sorge GB, Benoit A, West RF, Stanovich KE. Decision-making of chinese version of the MacArthur competence assessment tool for
and cognitive abilities: a review of associations between Iowa Gambling Task clinical research (MacCAT-CR) in patients with schizophrenia spectrum
performance, executive functions, and intelligence. Clin Psychol Rev. (2010). disorders. Psychiatry Res. (2013). 210:634–40. doi: 10.1016/j.psychres.2013.
30:562–81. doi: 10.1016/j.cpr.2010.04.002. 07.002
4. Manes F, Torralva T, Ibáñez A, Roca M, Bekinschtein T, Gleichgerrcht 16. Carpenter WT Jr., Gold JM, Lahti AC, Queern CA, Conley RR, Bartko JJ, et al.
E. Decision-making in frontotemporal dementia: clinical, theoretical Decisional capacity for informed consent in schizophrenia research. Arch Gen
and legal implications. Dement Geriatr Cogn Disord. (2011). 32:11–7. Psychiatry. (2000). 57:533–8. doi: 10.1001/archpsyc.57.6.533
doi: 10.1159/000329912 17. Palmer BW, Dunn LB, Appelbaum PS, Jeste DV. Correlates of
5. Wong JG, Cheung EP, Chen EY. Decision-making capacity of inpatients treatment-related decision-making capacity among middle-aged and
with schizophrenia in Hong Kong. J Nerv Ment Dis. (2005). 193:316–22. older patients with schizophrenia. Arch Gen Psychiatry. (2004). 61:230–6.
doi: 10.1097/01.nmd.0000161685.54077.e4 doi: 10.1001/archpsyc.61.3.230
6. Grisso T, Appelbaum PS, Hill-Fotouhi C. The MacCAT-T: a clinical tool to 18. Palmer BW, Dunn LB, Appelbaum PS, Mudaliar S, Thal L, Henry R, et al.
assess patients’ capacities to make treatment decisions. Psychiatr Serv. (1997). Assessment of capacity to consent to research among older persons with
48:1415–9. doi: 10.1176/ps.48.11.1415 schizophrenia, Alzheimer disease, or diabetes mellitus: comparison of a 3-item
7. Wang SB, Wang YY, Ungvari GS, Ng CH, Wu RR, Wang J, et al. The questionnaire with a comprehensive standardized capacity instrument. Arch
MacArthur competence assessment tools for assessing decision-making Gen Psychiatry. (2005). 62:726–33. doi: 10.1001/archpsyc.62.7.726
capacity in schizophrenia: a meta-analysis. Schizophr Res. (2017). 183:56–63. 19. Wu BJ, Liao HY, Chen HK, Lan TH. Psychopathology, psychopharmacological
doi: 10.1016/j.schres.2016.11.020 properties, decision-making capacity to consent to clinical research
8. van Os J, Kapur S. Schizophrenia. Lancet. (2009). 374:635–45. and the willingness to participate among long-term hospitalized
doi: 10.1016/S0140-6736(09)60995-8 patients with schizophrenia. Psychiatry Res. (2016). 237:323–30.
9. Freedman R Schizophrenia. N Engl J Med. (2003). 349:1738–49. doi: 10.1016/j.psychres.2016.01.020
doi: 10.1056/NEJMra035458 20. Stroup TS, Appelbaum PS, Gu H, Hays S, Swartz MS, Keefe RS, et al.
10. McGlashan TH. Eugen Bleuler: centennial anniversary of his 1911 publication Longitudinal consent-related abilities among research participants with
of Dementia Praecox or the group of schizophrenias. Schizophr Bull. (2011). schizophrenia: results from the CATIE study. Schizophr Res. (2011). 130:47–
37:1101–3. doi: 10.1093/schbul/sbr130 52. doi: 10.1016/j.schres.2011.04.012.
11. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional 21. Merz JF, Druzdzel MJ, Mazur DJ. Verbal expressions of probability
capacity in people with schizophrenia compared to normal subjects: an in informed consent litigation. Med Decis Making. (1991). 11:273–81.
overview. Schizophr Bull. (2006). 32:121–8. doi: 10.1093/schbul/sbj001 doi: 10.1177/0272989X9101100405
12. Okai D, Owen G, McGuire H, Singh S, Churchill R, Hotopf M. Mental capacity 22. Grisso T, Appelbaum PS. The MacArthur treatment competence study. III:
in psychiatric patients: Systematic review. Br J Psychiatry. (2007). 191:291–7. abilities of patients to consent to psychiatric and medical treatments. Law
doi: 10.1192/bjp.bp.106.035162 Hum Behav. (1995). 19:149–74.
Frontiers in Psychiatry | www.frontiersin.org 4 April 2019 | Volume 10 | Article 195
Sugawara et al. Decisional Capacity in Schizophrenic Patients
23. Kovnick JA, Appelbaum PS, Hoge SK, Leadbetter RA. Competence to consent 33. Owen GS, Ster IC, David AS, Szmukler G, Hayward P, Richardson G,
to research among long-stay inpatients with chronic schizophrenia. Psychiatr Hotopf M. Regaining mental capacity for treatment decisions following
Serv. (2003). 54:1247–52. doi: 10.1176/appi.ps.54.9.1247 psychiatric admission: a clinico-ethical study. Psychol Med. (2011). 41:119–28.
24. Palmer BW, Jeste DV. Relationship of individual cognitive abilities doi: 10.1017/S0033291710000383
to specific components of decisional capacity among middle-aged and 34. Palmer BW, Nayak GV, Dunn LB, Appelbaum PS, Jeste DV. Treatment-related
older patients with schizophrenia. Schizophr Bull. (2006). 32:98–106. decision-making capacity in middle-aged and older patients with psychosis: a
doi: 10.1093/schbul/sbj002 preliminary study using the MacCAT-T and HCAT. Am J Geriatr Psychiatry.
25. Kar SK, Jain M. Current understandings about cognition and the (2002). 10:207–11. doi: 10.1097/00019442-200203000-00012
neurobiological correlates in schizophrenia. J Neurosci Rural Pract. (2016). 35. Jeste DV, Palmer BW, Golshan S, Eyler LT, Dunn LB, Meeks T, et al.
7:412–8. doi: 10.4103/0976-3147.176185 Multimedia consent for research in people with schizophrenia and normal
26. Condray R, Steinhauer SR, van Kammen DP, Kasparek A. Working subjects: a randomized controlled trial. Schizophr Bull. (2009). 35:719–29.
memory capacity predicts language comprehension in schizophrenic doi: 10.1093/schbul/sbm148
patients. Schizophr Res. (1996). 20:1–13. doi: 10.1016/0920-9964(95)0 36. Naughton M, Nulty A, Abidin Z, Davoren M, O’Dwyer S, Kennedy HG.
0061-5 Effects of group metacognitive training (MCT) on mental capacity and
27. Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The functioning in patients with psychosis in a secure forensic psychiatric hospital:
brief assessment of cognition in schizophrenia: reliability, sensitivity, and a prospective-cohort waiting list controlled study. BMC Res Notes. (2012).
comparison with a standard neurocognitive battery. Schizophr Res. (2004). 5:302. doi: 10.1186/1756-0500-5-302
68:283–97. doi: 10.1016/j.schres.2003.09.011 37. Vingerhoets WA, Bloemen OJ, Bakker G, van Amelsvoort TA.
28. Eisenberg DP, Berman KF. Executive function, neural circuitry, and genetic Pharmacological interventions for the MATRICS cognitive domains
mechanisms in schizophrenia. Neuropsychopharmacology. (2010). 35:258–77. in schizophrenia: what’s the evidence? Front Psychiatry. (2013). 4:157.
doi: 10.1038/npp.2009.111 doi: 10.3389/fpsyt.2013.00157
29. Linder M, Lev-Ari L, Kurs R, Melamed Y. Evaluation of the capacity 38. Dunn LB, Palmer BW, Appelbaum PS, Saks ER, Aarons GA, Jeste DV.
of inpatients with chronic schizophrenia to provide informed consent for Prevalence and correlates of adequate performance on a measure of abilities
participation in clinical trials; use of the Hebrew version of the MacArthur related to decisional capacity: differences among three standards for the
competence assessment tool for clinical research (MacCAT-CR). Isr Med Assoc MacCAT-CR in patients with schizophrenia. Schizophr Res. (2007). 89:110–8.
J. (2012). 14:470–4. doi: 10.1016/j.schres.2006.08.005
30. Palmer BW, Savla GN. The association of specific neuropsychological
deficits with capacity to consent to research or treatment. J Int Conflict of Interest Statement: The authors declare that the research was
Neuropsychol Soc. (2007). 13:1047–59. doi: 10.1017/S13556177070 conducted in the absence of any commercial or financial relationships that could
71299 be construed as a potential conflict of interest.
31. Koren D, Poyurovsky M, Seidman LJ, Goldsmith M, Wenger S, Klein EM.
The neuropsychological basis of competence to consent in first-episode Copyright © 2019 Sugawara, Yasui-Furukori and Sumiyoshi. This is an open-access
schizophrenia: a pilot metacognitive study. Biol Psychiatry. (2005). 57:609–16. article distributed under the terms of the Creative Commons Attribution License (CC
doi: 10.1016/j.biopsych.2004.11.029 BY). The use, distribution or reproduction in other forums is permitted, provided
32. Dornan J, Kennedy M, Garland J, Rutledge E, Kennedy HG. Functional the original author(s) and the copyright owner(s) are credited and that the original
mental capacity, treatment as usual and time: magnitude of change in secure publication in this journal is cited, in accordance with accepted academic practice.
hospital patients with major mental illness. BMC Res Notes. (2015). 8:566. No use, distribution or reproduction is permitted which does not comply with these
doi: 10.1186/s13104-015-1547-4 terms.
Frontiers in Psychiatry | www.frontiersin.org 5 April 2019 | Volume 10 | Article 195
You might also like
- Dimensional PsychopathologyFrom EverandDimensional PsychopathologyMassimo BiondiNo ratings yet
- ndt-18-891Document7 pagesndt-18-891Julio DelgadoNo ratings yet
- Neuroimaging of Schizophrenia and Other Primary Psychotic Disorders: Achievements and PerspectivesFrom EverandNeuroimaging of Schizophrenia and Other Primary Psychotic Disorders: Achievements and PerspectivesNo ratings yet
- HSR 2179Document13 pagesHSR 2179Lisa SariNo ratings yet
- Cognitive Insight As An Indicator of Competence To Consent To Treatment in SchizophreniaDocument4 pagesCognitive Insight As An Indicator of Competence To Consent To Treatment in SchizophreniaJulio DelgadoNo ratings yet
- Paper Croskerry Medical Science Educator 2018Document6 pagesPaper Croskerry Medical Science Educator 2018Alyatur MardaNo ratings yet
- Cognitive Enhancement in SchizophreniaDocument20 pagesCognitive Enhancement in SchizophreniaPsikiatri 76 UndipNo ratings yet
- Coghill Sonuga Barke 2012. Category Vs Dimension in PsychopathologyDocument21 pagesCoghill Sonuga Barke 2012. Category Vs Dimension in PsychopathologyAlexandru NaeNo ratings yet
- Jurnal 3Document19 pagesJurnal 3Belajar KedokteranNo ratings yet
- 1 s2.0 S0140673612612689 MainDocument3 pages1 s2.0 S0140673612612689 MainOana OrosNo ratings yet
- Schizophrenia Case StudyDocument10 pagesSchizophrenia Case StudyAnanya GulatiNo ratings yet
- The Relationship of Cognitive Functions and Psychopathology On The Level of Insight in Patients With SchizophreniaDocument6 pagesThe Relationship of Cognitive Functions and Psychopathology On The Level of Insight in Patients With SchizophrenianandhaNo ratings yet
- Cognitive Assessment For CliniciansDocument10 pagesCognitive Assessment For CliniciansFernando AtenciaNo ratings yet
- Blen Now 2016Document7 pagesBlen Now 2016AmandaNo ratings yet
- PSYCH 001 Psychiatric Interview of The Medically Ill PDFDocument10 pagesPSYCH 001 Psychiatric Interview of The Medically Ill PDFKaye Nee100% (1)
- 2470 PDFDocument8 pages2470 PDFPreetha Kumar AJKKNo ratings yet
- Esquizo ITP 2011Document4 pagesEsquizo ITP 2011DrMartens AGNo ratings yet
- SBJ 053Document6 pagesSBJ 053filipamaltezNo ratings yet
- Diagnostic Brain Imaging in PsychiatryDocument8 pagesDiagnostic Brain Imaging in PsychiatryalexNo ratings yet
- Toward Recovery in SchizophreniaDocument10 pagesToward Recovery in SchizophreniaAlondra CastilloNo ratings yet
- Jurnal Inggris 1Document28 pagesJurnal Inggris 1ErinaTandirerungNo ratings yet
- Decisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockDocument4 pagesDecisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockJulio DelgadoNo ratings yet
- Insight in Social Behavioral Dysfunction in Schizophrenia: Preliminary StudyDocument8 pagesInsight in Social Behavioral Dysfunction in Schizophrenia: Preliminary StudyDanielaNo ratings yet
- Mandel 2019Document3 pagesMandel 2019Instituto Colombiano de PsicometriaNo ratings yet
- A Universal Model of Diagnostic Reasoning.14Document7 pagesA Universal Model of Diagnostic Reasoning.14Emília SantocheNo ratings yet
- Seminar: Jonathan Posner, Guilherme V Polanczyk, Edmund Sonuga-BarkeDocument13 pagesSeminar: Jonathan Posner, Guilherme V Polanczyk, Edmund Sonuga-BarkeCristinaNo ratings yet
- FocusDocument49 pagesFocusElizabeth AhnNo ratings yet
- The Mental Status ExaminationDocument7 pagesThe Mental Status Examinationdra.hadleyNo ratings yet
- Caspi Et Al The P Factor One General Psychopathology Factor in The Structure of PsychiatricDocument19 pagesCaspi Et Al The P Factor One General Psychopathology Factor in The Structure of PsychiatricAlejandro CaraveraNo ratings yet
- Neural Substrates of Decision Making As Measured WDocument11 pagesNeural Substrates of Decision Making As Measured Wzeinebabd20No ratings yet
- 2019 - NATURE - Clinical-Learning Versus Machine-Learning For Transdiagnostic Prediction of Psychosis Onset in Individuals At-RiskDocument11 pages2019 - NATURE - Clinical-Learning Versus Machine-Learning For Transdiagnostic Prediction of Psychosis Onset in Individuals At-RiskPriya KumariNo ratings yet
- Delhom Et Al., 2022Document13 pagesDelhom Et Al., 2022Administrador ContaNo ratings yet
- Executive Dysfunctions in Schizophrenia: A Critical Review of Traditional, Ecological, and Virtual Reality AssessmentsDocument26 pagesExecutive Dysfunctions in Schizophrenia: A Critical Review of Traditional, Ecological, and Virtual Reality Assessmentslolocy LNo ratings yet
- Craddock 2014 World PsychiatryDocument2 pagesCraddock 2014 World PsychiatryPrateekGandhiNo ratings yet
- Van Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)Document17 pagesVan Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)susanvanscoyoc9870No ratings yet
- Diff Erences in Cognitive Function and Daily Living Skills Between Early-And Late-Stage SchizophreniaDocument8 pagesDiff Erences in Cognitive Function and Daily Living Skills Between Early-And Late-Stage SchizophreniaRenny TjahjaNo ratings yet
- 2019 - Conners 3 ADHD SymptomsDocument18 pages2019 - Conners 3 ADHD Symptomsblanca_dhNo ratings yet
- Best Practice Guidelines For COGNITIVE REHABILITATDocument23 pagesBest Practice Guidelines For COGNITIVE REHABILITATSamantha Colle100% (1)
- Cognitive Remediation Therapy (CRT) : Improving Neurocognition and Functioning in SchizophreniaDocument19 pagesCognitive Remediation Therapy (CRT) : Improving Neurocognition and Functioning in SchizophreniaKaterina ChatzNo ratings yet
- Psychotherapy For Borderline Personality FocusingDocument3 pagesPsychotherapy For Borderline Personality FocusingjoannaNo ratings yet
- Effectiveness of Empathy in General Practice:: ResearchDocument9 pagesEffectiveness of Empathy in General Practice:: ResearchAndrés Ricardo Horta JaraNo ratings yet
- Schizophrenia Research: Alice M. Saperstein David A. Lynch Min Qian Alice MedaliaDocument6 pagesSchizophrenia Research: Alice M. Saperstein David A. Lynch Min Qian Alice Medaliaresearch managementNo ratings yet
- Best PracticeDocument10 pagesBest Practice123maidenNo ratings yet
- Cognitive Emotional and Social Processes in PsychosisDocument8 pagesCognitive Emotional and Social Processes in Psychosishelen.ashton5No ratings yet
- Insight On Insights - David 2017Document2 pagesInsight On Insights - David 2017gerard sansNo ratings yet
- Cognitive DebiasingDocument7 pagesCognitive DebiasingJefferson ChavesNo ratings yet
- Caz 7Document19 pagesCaz 7Marinela MeliszekNo ratings yet
- Forensic Psychiatry PDFDocument8 pagesForensic Psychiatry PDFleoqfb688gmail.com HernandezNo ratings yet
- 2019 - NATURE - Recommendations and Future Directions For Supervised Machine Learning in PsychiatryDocument12 pages2019 - NATURE - Recommendations and Future Directions For Supervised Machine Learning in PsychiatryPriya KumariNo ratings yet
- CBT Cancer1Document11 pagesCBT Cancer1Rizka Hadian PermanaNo ratings yet
- A Brief Cognitive Assessment Tool For SchizophreniaDocument8 pagesA Brief Cognitive Assessment Tool For SchizophreniaRatriningdyah DewiNo ratings yet
- PICO: Model For Clinical Questions: Evidence-Based Medicine August 2018Document3 pagesPICO: Model For Clinical Questions: Evidence-Based Medicine August 2018ShervieNo ratings yet
- Irritability in Youth - An UpdateDocument3 pagesIrritability in Youth - An Updatelors93No ratings yet
- (10920684 - Neurosurgical Focus) Informed Consent in Neurosurgery - A Systematic ReviewDocument10 pages(10920684 - Neurosurgical Focus) Informed Consent in Neurosurgery - A Systematic ReviewOnilis RiveraNo ratings yet
- StampedDocument13 pagesStampedjessicatleiteNo ratings yet
- Psychedelic Medicine - Safety and Ethical ConsiderationsDocument2 pagesPsychedelic Medicine - Safety and Ethical ConsiderationsKayla GreenstienNo ratings yet
- Good For QualitativeDocument9 pagesGood For QualitativeWassie TsehayNo ratings yet
- Levels of Distress Tolerance in Schizophrenia Appear Equivalent To Those Found in Borderline Personality Disorder.Document9 pagesLevels of Distress Tolerance in Schizophrenia Appear Equivalent To Those Found in Borderline Personality Disorder.danielaNo ratings yet
- General Hospital Psychiatry: Review ArticleDocument10 pagesGeneral Hospital Psychiatry: Review Articlehevi_tarsumNo ratings yet
- 1 Clinical InterviewDocument14 pages1 Clinical InterviewClara Del Castillo ParísNo ratings yet
- Treatment Decision-Making Capacity in Nonconsensual Psychiatric Treatment A Multicentre StudyDocument8 pagesTreatment Decision-Making Capacity in Nonconsensual Psychiatric Treatment A Multicentre StudyJulio DelgadoNo ratings yet
- Decisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockDocument4 pagesDecisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockJulio DelgadoNo ratings yet
- 1.1.capacity To Consent For Treatment in Patients With Psychotic Disorder A Cross-Sectional Study From North KarnatakaDocument6 pages1.1.capacity To Consent For Treatment in Patients With Psychotic Disorder A Cross-Sectional Study From North KarnatakaJulio DelgadoNo ratings yet
- Lange Qampa Psychiatry 11th Edition CompressDocument69 pagesLange Qampa Psychiatry 11th Edition CompressJulio DelgadoNo ratings yet
- Kinds of Degree of ComparisonDocument21 pagesKinds of Degree of ComparisonmuldhanNo ratings yet
- ATA Framework For Standardized Error MarkingDocument2 pagesATA Framework For Standardized Error MarkingHưng Nguyễn ĐạtNo ratings yet
- Activity Evaluation FormDocument1 pageActivity Evaluation Formmelvani deadio100% (1)
- Crafting Texts - Planning SheetDocument3 pagesCrafting Texts - Planning SheetlngocnguyenNo ratings yet
- Water Conservation Lesson Plan - Day 1Document4 pagesWater Conservation Lesson Plan - Day 1api-384521849No ratings yet
- Chapter 5 Network FundamentalsDocument7 pagesChapter 5 Network FundamentalsAD StarlightNo ratings yet
- Passive Voice and Narration ArticalDocument69 pagesPassive Voice and Narration ArticalSyed AlamNo ratings yet
- Sekar Putri - Artikel KonseptualDocument5 pagesSekar Putri - Artikel Konseptualdevy ridaNo ratings yet
- Lesson Plan ScienceDocument3 pagesLesson Plan ScienceValarmathi VeerasenanNo ratings yet
- Bavish Gummadi's PM Recruiting GuideDocument11 pagesBavish Gummadi's PM Recruiting GuideSohini DeyNo ratings yet
- Chapter 8 Training and Developing EmployeesDocument14 pagesChapter 8 Training and Developing EmployeesSuhail Ahmed50% (2)
- Quality Leadership and Management, Technology-Based Instruction, Work Attitude, and Teachers Performance in The New NormalDocument6 pagesQuality Leadership and Management, Technology-Based Instruction, Work Attitude, and Teachers Performance in The New NormalJiesrel JimenoNo ratings yet
- Hidayati's ArticleDocument17 pagesHidayati's ArticlePusat Bahasa UmadaNo ratings yet
- Metamophors in Hugo Chavez Political DiscourseDocument232 pagesMetamophors in Hugo Chavez Political DiscourseRenata Peixoto De OliveiraNo ratings yet
- Krathwohl Affective DomainDocument13 pagesKrathwohl Affective DomainSaymon Casilang SarmientoNo ratings yet
- Bisang 1 HO1 BuenosAires 2017Document18 pagesBisang 1 HO1 BuenosAires 2017Anahí Lopez FavilliNo ratings yet
- Answer For TMA 1 of Strategic ManagmentDocument5 pagesAnswer For TMA 1 of Strategic ManagmentmichaelNo ratings yet
- Effects of Having A Relationship in The Studies of High School StudentsDocument3 pagesEffects of Having A Relationship in The Studies of High School StudentsMizhar Gerardo100% (1)
- D. 6. The Collection Development ProsesDocument7 pagesD. 6. The Collection Development ProsesmaydiNo ratings yet
- Cambridge Introduction Scenogr Part1 ElementsDocument10 pagesCambridge Introduction Scenogr Part1 ElementsAndreea Dalimon100% (1)
- Unit 2 Step 2: BrainstormingDocument11 pagesUnit 2 Step 2: BrainstormingIbrahim AhmedNo ratings yet
- Tactical Periodization Training The Brain To Make Quick Decisions PDFDocument4 pagesTactical Periodization Training The Brain To Make Quick Decisions PDFHung100% (1)
- BPT1501 Assignment 3Document5 pagesBPT1501 Assignment 3Anime LoverNo ratings yet
- Success Criteria: Pupils Can: 21st Century Activities & SkillsDocument16 pagesSuccess Criteria: Pupils Can: 21st Century Activities & SkillsAisy EizharNo ratings yet
- Communication Between Men and WomenDocument7 pagesCommunication Between Men and WomenPreyashiNo ratings yet
- Design ProcessDocument20 pagesDesign ProcessHarshavardhan Virendra MallaNo ratings yet
- Behavioural ActivationDocument8 pagesBehavioural ActivationvasilismNo ratings yet
- Effective Workplace CommunicationDocument13 pagesEffective Workplace Communicationtrissymaharaj100% (2)
- Word StressDocument11 pagesWord StressKing Solomon CatralNo ratings yet
- 2-4 Illusions of Competence PowerpointDocument16 pages2-4 Illusions of Competence PowerpointLajos FazakasNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (36)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (2)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingFrom EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingRating: 1 out of 5 stars1/5 (2)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Make Him BEG for Your Attention: 75 Communication Secrets for Captivating Men to Get the Love and Commitment You DeserveFrom EverandMake Him BEG for Your Attention: 75 Communication Secrets for Captivating Men to Get the Love and Commitment You DeserveRating: 4.5 out of 5 stars4.5/5 (220)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Secret of the Golden Flower: A Chinese Book Of LifeFrom EverandThe Secret of the Golden Flower: A Chinese Book Of LifeRating: 5 out of 5 stars5/5 (4)