Professional Documents
Culture Documents
296 - Renal Pathology) Respiratory Acidosis
Uploaded by
MuhammadR1Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
296 - Renal Pathology) Respiratory Acidosis
Uploaded by
MuhammadR1Copyright:
Available Formats
Last edited: 8/31/2021
2. RESPIRATORY ACIDOSIS
Respiratory Acidosis Medical Editor: Jan Camille Santico
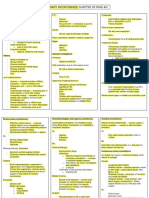
OUTLINE III) PATHOPHYSIOLOGY OF RESPIRATORY ACIDOSIS
I) INTERPRETING THE ABG In respiratory acidosis, the carbon dioxide level in the
II) PHYSIOLOGY OF RESPIRATORY ACIDOSIS blood is increased/increasing
III) PATHOPHYSIOLOGY OF RESPIRATORY o Recall: CO2 + H2O ↔ H2CO3 ↔ H+ + HCO2
ACIDOSIS o According to Le Chatelier’s principle, when a
IV) DIFFERENTIALS reactant/substrate is in excess, the reaction will shift
V) EFFECT OF HYPOXIA to the opposite side to maintain equilibrium
VI) TREATMENT o When there is excess CO2, the reaction will shift to
VII) REVIEW QUESTIONS the right, causing an increase in protons (H+), which
VIII) REFRENCES consequently lowers the pH and leads to acidosis
Thus, in respiratory acidosis, there is deficient clearance
of carbon dioxide and deficient oxygen intake/exchange
I) INTERPRETING THE ABG Summary
Table 1. Sample ABG Case The respiratory centers send signals via the phrenic nerve
ABG Result Normal Values and intercostal nerves to stimulate the diaphragm and
pH 7.29 7.35 – 7.45 external intercostals to contract, respectively
The contraction of these muscles will help take in oxygen
pCO2 58 mmHg 35 – 45 during inhalation; during exhalation, healthy lungs will
HCO3 22 mEq/L 22 – 26 collapse and recoil to expel carbon dioxide
pO2 50 mmHg >90 A patient with respiratory acidosis must have a problem with
Note: Please refer to the lecture video on “Acid Base Disorders and ABG
carbon dioxide clearance, oxygen intake, or gas exchange.
Interpretation” to understand this section better.
The pH is acidic, meaning there is acidemia and IV) DIFFERENTIALS
underlying acidosis.
To determine if it is a metabolic or respiratory acidosis, This section gives an overview of the possible
check the HCO3 and pCO2 causes/differentials of respiratory acidosis, arranged
o If the HCO3 is going in the same direction as the pH= anatomically.
Metabolic
(A) RESPIRATORY CENTER
o If the pCO2 is going in the opposite direction as the
pH= Respiratory (1) Lesions in the Respiratory Center
Since the pCO2 is going in the opposite direction, the Possible causes
patient has respiratory acidosis. o Tumor
o In respiratory acidosis, the bicarbonate is expected to o Infection (e.g. encephalitis)
increase to compensate and to make the environment o Traumatic brain injury
more alkalotic; however, in this case, since the
Diagnosis/Work-up
bicarbonate falls within the normal range, this is
o Order cranial imaging (e.g. CT, MRI) to check for lesions
uncompensated respiratory acidosis
o Order a lumbar puncture to check for a CNS infection
The oxygen saturation is low, so there is hypoxia
(2) Drugs
Table 2. Oxygen Saturation Values There are drugs which can depress the medulla and thus
Oxygen Saturation Interpretation the respiratory centers
80 - 100 Normal o Opioids
o Benzodiazepines
60 - 80 Mild Hypoxia
o Barbiturates
40 - 60 Moderate Hypoxia
Diagnosis/Work-up
<40 Severe Hypoxia
o Order a tox screen
o Order a urine drug screen
• For subheading use style “Heading 5”
II) PHYSIOLOGY OF RESPIRATORY ACIDOSIS
(3) Decreased metabolic activity
In the medulla, there is a ventral and dorsal respiratory
group, which function as respiratory centers that There are certain conditions which decrease the
regulate our rate and depth of breathing. metabolic activity of neurons
When the neurons of these respiratory centers fire, they o Hypothyroidism
send signals to the lower motor neurons in the spinal Pathophysiology: decreased production of T3 and T4
cord decreased basal metabolic rate decreased firing of
The action potentials then travel through the peripheral neurons in the respiratory center
nerves that innervate the muscles for breathing Diagnosis: Check TSH and T3/T4 levels
o Diaphragm • In hypothyroidism, expect high TSH and low
o External intercostals T3/T4 levels
o Hypothermia
When these muscles contract, they help pull oxygen in Pathophysiology: increased body temperature
the lungs and blow carbon dioxide out Diagnosis: Check core temperature
Respiratory Acidosis RENAL PATHOLOGY: NOTE #2. . 1 of 4
(B) SPINAL CORD AND PERIPHERAL NERVES (D) LUNGS
(1) Anterior Grey Horn (1) Airway Obstruction
A lesion in the anterior grey horn of the spinal cord might Airway obstruction can interfere with proper oxygen
interfere with the transmission of action potentials from intake and carbon dioxide clearance
the respiratory centers to the muscles for breathing Possible causes of obstruction include:
Possible lesions include: o Mucus plugging
o Amyotrophic Lateral Sclerosis (ALS) o Collapsing of airway due to loss of elasticity
Diagnosis: signs of upper motor neuron (UMN) o Foreign body aspiration
and lower motor neuron (LMN) lesions Obstruction may occur in the lower or upper airways
o Poliomyelitis
Diagnosis: No polio vaccine, muscle weakness (i) Lower Airway
o Transverse myelitis
• Common cause: Chronic Obstructive
Diagnosis: History of fever, muscle pain
Pulmonary Disease (COPD)
Work-up: Order a lumbar puncture
• History: smoking
(2) Myelin Sheath • Diagnosis/Work-up
Demyelination of peripheral nerves can interfere with the o Abnormal pulmonary function test
transmission of action potentials and thus affect the o Hyperinflated lungs in chest X-ray
muscles for breathing o Barrel-chested appearance
Guillain-Barré Syndrome (GBS) o Cough with mucus
o Pathophysiology: presence of autoantibodies (ii) Upper Airway
attacking the myelin sheath
o Diagnosis: history of previous gastrointestinal (GI) or • Possible causes:
upper respiratory tract (URT) infections o Foreign body aspiration
o Classic sign: symmetric ascending paralysis Young children who choke on small
o Work-up: Order a lumbar puncture; look for albumin- objects
cytological dissociation Diagnosis: Laryngoscopy,
bronchoscopy
(3) Neuromuscular Junction (NMJ) o Laryngeal edema
Recall: Acetylcholine (Ach) is released by the peripheral Causes:
nerves (in the NMJ, and this neurotransmitter binds to • generalized angioedema due to
nicotinic receptors on the muscle cells medication
Myasthenia Gravis • mechanical ventilation
o Pathophysiology: autoantibodies attack the nicotinic
(2) Fluid in the Airway
receptors, interfering with muscle contraction
o Diagnosis The presence of fluid/pus/secretions in the airway
History/presence of thymoma interferes with proper gas exchange, leading to hypoxia
Bulbar weakness Possible causes:
• Double vision o Pneumonia
• Eyelid drooping o Acute Respiratory Distress Syndrome (ARDS)
• Facial weakness o Pulmonary edema
Muscle weakness that is worse as the day passes Fluid/secretions between the lung space (alveoli)
o Work-up: Check Ach receptor antibodies and capillaries
o Pulmonary embolism
(C) MUSCLES A blood clot enters and obstructs a pulmonary
Muscle exhaustion/fatigue is one of the most common vessel, causing failure of gas exchange
causes of respiratory acidosis
o Due to increased work of breathing from underlying
respiratory problems
Polymyositis and dermatomyositis are less likely causes
o Diagnosis: muscle biopsy
2 of 4 RENAL PATHOLOGY: NOTE #2. Respiratory Acidosis
Figure 1. Differentials for Respiratory Acidosis
V) EFFECT OF HYPOXIA IV immunoglobulin
GBS Plasma exchange
When there is less oxygen in the bloodstream, there is (PLEX)
hypoxia NERVES
Chemoreceptors detect the increased carbon dioxide in Myasthenia IV immunoglobulin
the body, sending signals to the respiratory centers gravis PLEX
The respiratory centers will then direct your body to Steroids
increase respiratory rate and depth Non-invasive positive
o Breathing faster and deeper pressure ventilation
Respiratory (NPPV)
The increased breathing rate will expel more carbon MUSCLES
muscle fatigue Mechanical ventilation
dioxide, which initially leads to respiratory alkalosis
(e.g. endotracheal
However, if the increased respiratory rate is sustained
tube)
over a long time, the respiratory muscles will eventually
fatigue, leading to decreased respiratory rate and depth Inhaled
The decreased respiratory rate and depth leads to the corticosteroids
reduced clearance of carbon dioxide and acidic pH COPD Duoneb
Oral/IV steroids (in
acute exacerbations)
NPPV
LUNGS
Laryngeal Steroids
edema Benadryl
VI) TREATMENT (antihistamines)
The approach to treating respiratory acidosis is to treat Foreign body Remove foreign body
the underlying cause aspiration
Pneumonia Antibiotics
Support respiratory
Table 3. Treatments for Respiratory Acidosis
ARDS system via positive
Organ Differential Treatment pressure ventilation
Resect the tumor Pulmonary Diuretics to decrease
Tumor Steroids to decrease edema (due to fluid
vasogenic edema heart failure)
Infection Antibiotics or antivirals Heparin drip
Dependent on nature of Pulmonary Tissue plasminogen
Trauma activator
trauma embolism
Opioid Naloxone Embolectomy to
MEDULLA remove the clot
overdose
Benzodiazepine Flumazenil While treating the underlying cause, it is also important to
overdose support the airway of the patient. The empirical
Barbiturate Sodium bicarbonate approaches for this are:
overdose o NIPPV
High flow nasal cannula
Hypothyroidism Levothyroxine
Bilevel Positive Airway Pressure (BiPAP)
Hypothermia Warm the patient o Mechanical Ventilation (invasive)
Respiratory Acidosis RENAL PATHOLOGY: NOTE #2. . 3 of 4
VII) REVIEW QUESTIONS
Given the following ABG results, determine if the
acidosis is respiratory or metabolic.
ABG Result
pH 7.31
pCO2 35 mmHg
HCO3 14 mEq/L
pO2 75 mmHg
a. Respiratory
b. Metabolic
Given the following ABG results, determine if the
acidosis is respiratory or metabolic.
ABG Result
pH 7.31
pCO2 50 mmHg
HCO3 28 mEq/L
pO2 75 mmHg
a. Respiratory
b. Metabolic
In a patient with opioid overdose, which is the most
likely culprit for respiratory acidosis?
a. Lesion in the medulla
b. Depressed respiratory center
c. Demyelination of peripheral nerves
d. Generation of autoantibodies
Which of the following pathophysiologic
mechanisms lead to respiratory acidosis?
a. Impaired clearance of carbon dioxide
b. Impaired gas exchange
c. Both A and B
d. None of the above
Which of the following is supportive treatment for
patients with respiratory acidosis?
a. Ice packs
b. Antihistamines
c. BiPAP
d. None of the above
CHECK YOUR ANSWERS
VIII) REFRENCES
4 of 4 RENAL PATHOLOGY: NOTE #2. Respiratory Acidosis
You might also like
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- 297 - Renal Pathology) Respiratory AlkalosisDocument3 pages297 - Renal Pathology) Respiratory AlkalosisMuhammadR1No ratings yet
- Nutri Diet 6Document6 pagesNutri Diet 6jellybeandumpppNo ratings yet
- Blood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIDocument39 pagesBlood Gases and Acid-Base Disorders: Dr. Wan Nedra Sp. A Pediatricts Departement University of YARSIIQBAL HAKKIKINo ratings yet
- Hypercapnia: Bernie Y. Sunwoo, - Babak MokhlesiDocument12 pagesHypercapnia: Bernie Y. Sunwoo, - Babak MokhlesiSaraNo ratings yet
- Hypoxia BAC 2020Document21 pagesHypoxia BAC 2020ss8d6vm5znNo ratings yet
- Internal Medicine - Phase 3: Important Legal InformationDocument19 pagesInternal Medicine - Phase 3: Important Legal InformationClaire YabaNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation IndependentDocument3 pagesAssessment Nursing Diagnosis Planning Intervention Rationale Evaluation IndependentSHEILA MAE SACLOTNo ratings yet
- Mindanao State University College of Health Sciences Marawi CityDocument17 pagesMindanao State University College of Health Sciences Marawi CityBella DonnaNo ratings yet
- Veterinary Clinics: Respiratory Acidosis: A Quick ReferenceDocument4 pagesVeterinary Clinics: Respiratory Acidosis: A Quick ReferenceAndersonValentimOliveiradaSilvaNo ratings yet
- 3.05 PHYSIOLOGY-Control of RespirationDocument2 pages3.05 PHYSIOLOGY-Control of RespirationDi CanNo ratings yet
- 5.06b Ventilation & Sleep Apnea: I. Disorders of VentilationDocument9 pages5.06b Ventilation & Sleep Apnea: I. Disorders of VentilationvcNo ratings yet
- Critical Care Emergency Medicine 01Document7 pagesCritical Care Emergency Medicine 01AstridNo ratings yet
- CO2 NarcoseDocument5 pagesCO2 NarcoseHasan NyambeNo ratings yet
- Arterial Blood Gas Analysis OUTLINEDocument3 pagesArterial Blood Gas Analysis OUTLINEPaula TapilNo ratings yet
- Abg InterpretationDocument5 pagesAbg InterpretationGeoffrey Panjeton100% (1)
- Respiratory FailureDocument7 pagesRespiratory FailuremuhammadridhwanNo ratings yet
- ABG InterpretationDocument11 pagesABG InterpretationertrggerNo ratings yet
- Control of Respiration PhysiologyDocument9 pagesControl of Respiration PhysiologypuchioNo ratings yet
- PH - Log (H+) H+ Is Really A Proton Range Is From 0 - 14 If (H+) Is High, The Solution Is Acidic PH 7Document3 pagesPH - Log (H+) H+ Is Really A Proton Range Is From 0 - 14 If (H+) Is High, The Solution Is Acidic PH 7ahsanNo ratings yet
- Assessment Nursing Diagnosis Planning Nsg. Intervention Rationale Evaluation SubjectiveDocument6 pagesAssessment Nursing Diagnosis Planning Nsg. Intervention Rationale Evaluation SubjectiveIngrid Eunice ConcordiaNo ratings yet
- 295 - Renal Pathology) Acid Base Disorders and ABG Interpretation - IntroductionDocument6 pages295 - Renal Pathology) Acid Base Disorders and ABG Interpretation - IntroductionMuhammadR1No ratings yet
- JAPS Review Article LatestDocument5 pagesJAPS Review Article LatestSumit BediNo ratings yet
- Fluid and Electrolyte Imbalance - Test2Document7 pagesFluid and Electrolyte Imbalance - Test2M SanchezNo ratings yet
- Fluid Electrolytes Acid Base BalanceDocument18 pagesFluid Electrolytes Acid Base BalanceVin Lorenzo Campbell100% (1)
- Hypoxia (缺氧) : Rutao Long Professor Department of Pathophysiology Hainan Medical College 2016/3/31Document72 pagesHypoxia (缺氧) : Rutao Long Professor Department of Pathophysiology Hainan Medical College 2016/3/31Kwadwo Sarpong JnrNo ratings yet
- NullDocument159 pagesNullvishnuNo ratings yet
- ABG GeekymedicsDocument13 pagesABG Geekymedicscharlyn206No ratings yet
- Abg SakshiDocument59 pagesAbg SakshiSakshi GuptaNo ratings yet
- NCP 1 N 2Document5 pagesNCP 1 N 2Cuttie Anne GalangNo ratings yet
- MS Respi (NLE)Document3 pagesMS Respi (NLE)Maginalyn CangasNo ratings yet
- L4 PDFDocument12 pagesL4 PDFMiles HuiNo ratings yet
- The Physiology of VentilationDocument14 pagesThe Physiology of VentilationEva SánchezNo ratings yet
- Respiration at High Altitudes AtfDocument5 pagesRespiration at High Altitudes Atfpnsscsny29No ratings yet
- Arterial Blood Gases (ABG) : Shaza AlyDocument56 pagesArterial Blood Gases (ABG) : Shaza AlyaymenNo ratings yet
- Translate Part 1Document22 pagesTranslate Part 1TiaRa JuraidNo ratings yet
- Respiratory DisordersDocument15 pagesRespiratory Disordersmnlstr100% (5)
- CLINICAL CHEMISTRY 2 LecDocument14 pagesCLINICAL CHEMISTRY 2 LecMACOB, ETHELHYN JHANENo ratings yet
- 16 Respiratory AlkalosisDocument28 pages16 Respiratory AlkalosisJoel Topf100% (2)
- Arterial Blood Gas (Abg) Analysis: Submitted ToDocument5 pagesArterial Blood Gas (Abg) Analysis: Submitted ToRumela ChakrabortyNo ratings yet
- BLOODBUFFERSDocument2 pagesBLOODBUFFERSkulangkatunNo ratings yet
- Clinical Chemistry II ELECTROLYTESDocument2 pagesClinical Chemistry II ELECTROLYTESEden MaeNo ratings yet
- Long-Term Oxygen TherapyDocument11 pagesLong-Term Oxygen TherapyFontecha AnaNo ratings yet
- Respiratory Acidosis: Dr. Ann Valerie F. Habana Critical Care MedicineDocument21 pagesRespiratory Acidosis: Dr. Ann Valerie F. Habana Critical Care Medicineannv748687No ratings yet
- Arterial Blood Gases Made EasyDocument1 pageArterial Blood Gases Made EasyAkanksha RawatNo ratings yet
- HW1Document2 pagesHW1Bug AphidNo ratings yet
- Indian Pediatrics - Abg DisordersDocument10 pagesIndian Pediatrics - Abg Disordersdr.gladyvargheseNo ratings yet
- Blood Gases and Acid-Base BalanceDocument11 pagesBlood Gases and Acid-Base BalanceREMAN ALINGASANo ratings yet
- Regulation of RespirationDocument46 pagesRegulation of Respirationnirilib89% (9)
- ABG Interpretation: Normal Ranges 2. PHDocument2 pagesABG Interpretation: Normal Ranges 2. PHAlexander EnnesNo ratings yet
- ANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Document7 pagesANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNo ratings yet
- 3 Interpretation of Arterial Blood Gases Seminar 4 yDocument18 pages3 Interpretation of Arterial Blood Gases Seminar 4 yPrasenjit SarkarNo ratings yet
- FRCEM ExamPrep RespiratoryDocument26 pagesFRCEM ExamPrep RespiratoryskNo ratings yet
- Acid BaseDocument6 pagesAcid BaseCarol Solanyi Gacha QuinteroNo ratings yet
- ABG InterpretationDocument13 pagesABG InterpretationAbid KhanNo ratings yet
- First Shift Case Discussion (September 22, 2020) : 1CMED C6 - Dra. Roasa Leader: SecretaryDocument6 pagesFirst Shift Case Discussion (September 22, 2020) : 1CMED C6 - Dra. Roasa Leader: SecretaryjetNo ratings yet
- ABG QuizDocument13 pagesABG QuizSSNo ratings yet
- Common Causes of HypoxemiaDocument6 pagesCommon Causes of HypoxemiaSamantha LuiNo ratings yet
- The Concept of Syed Muhammad Naquib Al-Attas On deDocument21 pagesThe Concept of Syed Muhammad Naquib Al-Attas On deMuhammadR1No ratings yet
- Bab Iii PDFDocument29 pagesBab Iii PDFHabral El-AttasNo ratings yet
- Notice For Dip PEC (SA) - FS 2023 13 1 2024Document1 pageNotice For Dip PEC (SA) - FS 2023 13 1 2024MuhammadR1No ratings yet
- EndometriosisDocument8 pagesEndometriosisMuhammadR1No ratings yet
- Carcinoma of The CervixDocument5 pagesCarcinoma of The CervixMuhammadR1100% (1)
- InfertilityDocument10 pagesInfertilityMuhammadR1No ratings yet
- Disorders of Lower Urinary TractDocument5 pagesDisorders of Lower Urinary TractMuhammadR1No ratings yet
- Msds Bopp Packing TapeDocument3 pagesMsds Bopp Packing TapeTran Tuan anhNo ratings yet
- Lived Experiences of Grade 11 StudentsDocument3 pagesLived Experiences of Grade 11 StudentsLeand Majin SahipNo ratings yet
- Chapter1 To 3Document26 pagesChapter1 To 3Gerard Adrian Bautista AnonuevoNo ratings yet
- PDF Diseases of Tunas - CompressDocument20 pagesPDF Diseases of Tunas - CompressYen AduanaNo ratings yet
- Hopes For Speedy Rebound Dim: For Personal, Non-Commercial Use OnlyDocument32 pagesHopes For Speedy Rebound Dim: For Personal, Non-Commercial Use OnlyMiguel DiazNo ratings yet
- 2022 Benefits Enrollment GuideDocument28 pages2022 Benefits Enrollment GuideWyattNo ratings yet
- CombinepdfDocument214 pagesCombinepdfAl Ther JumadilNo ratings yet
- Diagnostic Test Battery For Different Age GroupsDocument14 pagesDiagnostic Test Battery For Different Age GroupsDhana KrishnaNo ratings yet
- QualifiedPhysio MSK Interview Preparation Pack PDFDocument48 pagesQualifiedPhysio MSK Interview Preparation Pack PDFUkpabi GinikachiNo ratings yet
- L3 Hematology Regulation of Iron MetabolismDocument3 pagesL3 Hematology Regulation of Iron MetabolismMurtadha AlrubayeNo ratings yet
- Phoenix. Software V9 Series. Programmer S Reference For Hypertherm Touchscreen Shape Cutting Controls Revision 7Document107 pagesPhoenix. Software V9 Series. Programmer S Reference For Hypertherm Touchscreen Shape Cutting Controls Revision 7David Barrientos RuizNo ratings yet
- Male Female PsychologyDocument38 pagesMale Female PsychologyParamjit SharmaNo ratings yet
- Personal Development: Quarter 2 - Module 6: Persons and Careers (Career Basic Concepts)Document3 pagesPersonal Development: Quarter 2 - Module 6: Persons and Careers (Career Basic Concepts)Lovely Joy ValdezNo ratings yet
- Neonatal and Pediatric Mechanical Ventilation - 2020Document88 pagesNeonatal and Pediatric Mechanical Ventilation - 2020Ahmed YasserNo ratings yet
- Datasheet PLD ComecDocument7 pagesDatasheet PLD Comecouss oussNo ratings yet
- Articles of PartnershipDocument3 pagesArticles of Partnershipjonel sembranaNo ratings yet
- Questions For OSCE Exam 2Document7 pagesQuestions For OSCE Exam 2Farah FarahNo ratings yet
- Staff Nurses, Lab-Technicians& Pharmacists: WWW - Vizianagaram.nic - inDocument6 pagesStaff Nurses, Lab-Technicians& Pharmacists: WWW - Vizianagaram.nic - inSATYAM NAIDUNo ratings yet
- Full Download Test Bank For Health Psychology 3rd Edition Sanderson PDF Full ChapterDocument13 pagesFull Download Test Bank For Health Psychology 3rd Edition Sanderson PDF Full Chapterrequinneologic8yzqgt100% (17)
- Fluid Therapy: Route Advantages DisadvantagesDocument3 pagesFluid Therapy: Route Advantages DisadvantagesAshref BelhajNo ratings yet
- Ulkus DiabetikumDocument8 pagesUlkus DiabetikumDwi Feri HariyantoNo ratings yet
- Conjunctions of PurposeDocument19 pagesConjunctions of PurposeHackerNo ratings yet
- Beyond Sexless Class and Classless Sex Towards FemDocument38 pagesBeyond Sexless Class and Classless Sex Towards FemAedermNo ratings yet
- Neonatal Resuscitation: Dr. (Col) C.G.Wilson Professor& H.O.D (Paed)Document38 pagesNeonatal Resuscitation: Dr. (Col) C.G.Wilson Professor& H.O.D (Paed)shaharuddin_yahayaNo ratings yet
- Household Services 7 Q4 - Week 3 4Document11 pagesHousehold Services 7 Q4 - Week 3 4Christian LastimosaNo ratings yet
- Shaukat Khanum Memorial Cancer Hospital & Research Centre: Coagulation ProfileDocument1 pageShaukat Khanum Memorial Cancer Hospital & Research Centre: Coagulation ProfileSyed Muhammad Zubair TariqNo ratings yet
- Tagalog Thesis Chapter 3Document7 pagesTagalog Thesis Chapter 3fjgmmmew100% (2)
- 5-Minute Exercises To Make Your Belly Fat Melt Like SnowDocument6 pages5-Minute Exercises To Make Your Belly Fat Melt Like Snowmelbe5jane5quiamcoNo ratings yet
- Personality Assessment TestsDocument5 pagesPersonality Assessment TestsDennis KimNo ratings yet
- Colisage ProduitsDocument6 pagesColisage ProduitsBerriche MohamedNo ratings yet