Professional Documents
Culture Documents
Pharmacoeconomics in Healthcare
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacoeconomics in Healthcare
Copyright:
Available Formats
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
Pharmacoeconomics in Healthcare
Apoorva Mahendrakar 1*; Hrithik Ajja1; Aashutosh Sinwal2; Ishu2; Nisha2; Priyanshi Jain 2
1
Malla Reddy College of Pharmacy, Maisammaguda, Hyderabad, Telangana, India- 500100
2
Pharm D, School of Pharmaceutical Sciences, Jaipur National University, Jaipur, Rajasthan, India,302017
Corresponding Author: Apoorva Mahendrakar *
Malla Reddy College of Pharmacy, Maisammaguda,
Hyderabad, Telangana, India- 500100
Abstract:- Pharmacoeconomics is the study of the cost- sufficient reimbursement and payment for services is
effectiveness and accessibility of pharmaceutical increasingly dependent on conducting cost-effectiveness
treatments from the perspective of both individuals and studies of pharmacological choices. Additionally,
the healthcare system as a whole. This field can help pharmacoeconomic methods aid in validating the costs and
policymakers and healthcare providers make more advantages of different pharmaceutical services and
informed decisions about patient care. The field of health therapies, which may aid in determining the relevance of
economics saw its inaugural publication in 1973, while those options and aiding in the proper allocation of
the idea of cost-benefit and cost-effectiveness analysis resources in dynamic healthcare systems.[2]
was originally put forth by University of Minnesota
researchers McGhan, Rowland, and Bootman in 1978. In II. GENESIS OF PHARMACOECONOMICS
pharmacoeconomics, four main categories exist cost-
utility analysis, cost-minimization analysis, cost-benefit In the early 1960s, the field of pharmacy was officially
analysis, and cost-effectiveness analysis. acknowledged as a clinical profession inside the healthcare
Pharmacoeconomics was originally an applied discipline. system. Clinical pharmacy, drug information, and
Because of their relative youth, health economics, and pharmacokinetics are three areas of the pharmaceutical
pharmacoeconomics are still in the process of refining sciences that emerged during this period and are integral to
and evaluating their methods. Health economics has a lot pharmacy science and education. Rooted in the 1970s,
of issues that make it hard to use in real life. The field of pharmacoeconomics emerged in the 1980s.[3] The field of
pharmacoeconomics offers valuable insights that health economics saw its inaugural publication in 1973,
healthcare practitioners can use in their practice. Drug while the idea of cost-benefit and cost-effectiveness analysis
policy and clinical decision-making are both aided by was originally put forth by University of Minnesota
pharmacoeconomics. researchers McGhan, Rowland, and Bootman in 1978. The
results of tailoring aminoglycoside doses to critically burned
Keywords:- Pharmacoeconomics, Cost-Minimization patients with gram-negative septicemia were evaluated in a
Analysis, Cost-Utility Analysis, Cost-Effectiveness Analysis, 1979 early research publication in the field of pharmacy that
Cost-Benefit Analysis, Quality-Adjusted Life Years. included complex pharmacokinetic protocols and cost-
benefit analysis.[4] A specialist pharmacy academic program
I. INTRODUCTION was established in 1983 at Ohio State University College of
Pharmacy to offer a general introduction to cost-benefit and
A subfield of health economics known as cost-effective analysis in healthcare, particularly as it
"pharmacoeconomics" studies the effects and costs of pertains to the provision of pharmaceutical treatment. With
pharmaceutical goods and services. Research into drugs, its original definition as "analysis of the costs of drug
their manufacturing, delivery, storage, price, and finally, therapy to healthcare systems and society," the term
their consumption, are all interconnected in this economic "pharmacoeconomics" didn't make it into print until
model. When it comes to pharmaceutical goods, services, Townsend's 1986 publication brought attention to the need
and programs, pharmacoeconomics is the study of how they to establish research initiatives in this emerging field. The
affect people, businesses, and markets. To put it simply, first issue of the journal "Pharmacoeconomics" appeared in
pharmacoeconomics is the study of the cost-effectiveness 1992.[5]
and accessibility of pharmaceutical treatments from the
perspective of both individuals and the healthcare system as Pharmacoeconomics Evaluations: Key Components
a whole. [1] This field can help policymakers and healthcare To provide a decision-making framework, economic
providers make more informed decisions about patient care. evaluations compare and contrast at least two health
For healthcare decision-makers, pharmacoeconomic interventions to determine the costs and outcomes of various
methods include cost-minimization, cost-effectiveness, cost- technologies in a certain population. In this study, "costs"
utility, cost-benefit, cost-of-illness, cost-consequence, and and "outcomes" play crucial roles. Those individuals or
other useful economic analytic approaches. Achieving groups that are most likely to gain from a health intervention
IJISRT24MAR1293 www.ijisrt.com 1102
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
are called the target population. In the economic evaluation, categorized as either medical or non-medical based on
interventions (such as medications, vaccines, medical whether they pertain to specific medical procedures or other
procedures, or services) were used as comparators. One way related expenses. Costs can be categorized as either fixed or
to look at the costs and benefits of health care is from a variable based on changes in the amount of services
variety of perspectives. During an economic analysis, the supplied, due to the flexibility in medical care delivery. [9]
temporal horizon is used to compute the costs and outcomes, Indirect expenses include things like patients', families', and
which are also known as benefits and consequences. A society's lost wages or production as a result of patients'
decision's opportunity cost is the value of a benefit that illnesses. The amount of pain and suffering caused by a
could have been achieved had a different choice been medical condition or treatment is an example of an
selected.[6] In economic analysis, "costs" mean the monetary intangible cost. These are typically hard to pin down and put
part. Intangible costs, as well as direct and indirect medical a price on. Nonetheless, these details were more and more
and non-medical expenditures, are a part of it. Healthcare or incorporated into evaluations by researchers undertaking
humanistic outcomes are the anticipated results of an investigations from a social viewpoint.[10]
intervention; they are also known as benefits or
consequences. The term "willingness to pay" refers to a The second part of any economic analysis is the
method of gathering information on people's financial anticipated advantages of an intervention or the outcome to
willingness to pay for a specific intervention or service. A be examined. The goal of "benefit" measurement is to be as
person's time preferences can be taken into consideration all-encompassing as possible by including all of how the
through the application of discounting. A positive rate of health intervention affects the patient's life. The value
time preference dictates that most people would rather have gained from selecting option A instead of B is seen as the
advantages sooner rather than later and that they would defined benefits. Natural units (such as years of life gained
rather bear expenses later rather than sooner. Decision trees or events prevented like strokes, surgeries, or peptic ulcer
and simulation models are two examples of modeling healing) and utility units (which try to encompass as much
procedures that can operationalize decision analyses derived of the notion of 'value' as possible) are two ways these
from economic evaluations. Uncertainty in economic interventions can be measured. Utility units can take into
evaluation outcomes can be represented through sensitivity account things like the quality of a state of health rather than
analysis. Multiway sensitivity analysis, probabilistic just its quantity or the satisfaction that comes from going
sensitivity analysis, threshold sensitivity analysis, and one- from one state of health to another. A measure of 'quality of
way basic sensitivity analysis are the four significant life' in various illness stages is sometimes used to inform
varieties of sensitivity studies.[7] these utility estimations.[11]
When it comes to pharmacoeconomic studies, the rules III. METHODS OF PHARMACOECONOMIC
for how they should be conducted and reported are made by ANALYSIS
the Professional Society for Health Economics and
Outcomes Research (ISPOR). These components make up The goal of pharmacoeconomic studies is to compare
the CHEERS statement, which is a condensed version of the the financial, medical, and subjective results of various
original. Researchers in the field of pharmacy practice treatments. To gain more support from healthcare
should take into account the following two ideas, however, professionals, administrators, and the general public, it is
while conducting an economic evaluation.[6,7] helpful to show how novel therapies affect costs using the
evaluation methods outlined. In pharmacoeconomics, four
When one choice is made, additional benefits that may main categories exist:
have been had from other possibilities are lost. This is Cost-Utility Analysis
called opportunity cost. Players will allocate funds to one Cost-Minimization Analysis
healthcare activity at the expense of others due to Cost-Benefit Analysis
resource scarcity, according to this theory. So, to make Cost-Effectiveness Analysis
smarter decisions, it's helpful to know what opportunities
can be lost if one technology is chosen over another. When multiple treatment options provide almost the
A non-welfarist viewpoint on decision-making is known same results, the cheapest one should be considered using
as "willingness to pay" (WTP). According to this view, cost-minimization analysis (CMA). The goal of cost-benefit
the best health intervention is the one that, up to a certain analysis (CMA) in drug selection is to identify the treatment
point, reaps the greatest benefit for the greatest number option with the lowest total cost. The expense of both dosing
of patients. Using a WTP threshold, decision-makers can and preparation is also reflected in it.[12] When determining
determine the point at which it is worthwhile to pay how much a medicine will cost, this is the approach that is
more for additional value.[8] most commonly utilized. Only two drugs with similar
therapeutic effects and doses can be compared using this
Expenses, or monetary consequences, are typically method. Thus, when comparing therapeutic equivalents and
broken down into direct, indirect, medical, non-medical, and generic versions of medications, this strategy is at its best. If
intangible expenses. This is the initial stage in any cost therapeutic equivalent cannot be proven, then cost-
study. The term "direct costs" describes the money that goes minimization analysis is unacceptable because there is often
straight into healthcare services, meaning they are directly no verifiable equivalence between two products. [13] To back
related to how patients are treated. Direct costs can be up economic assessments, there are a lot of clinical evidence
IJISRT24MAR1293 www.ijisrt.com 1103
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
sources; but, the "gold standard" is usually the randomized because CEAs might use a wide range of health outcomes as
controlled trial (RCT), which keeps everything constant their effectiveness term.[15] An economic analysis known as
except the medicine being tested. It is not feasible to a cost-benefit analysis (CBA) takes monetary values for
conduct a CMA in conjunction with an RCT because of the both the costs and the outcomes. The investment in the
lack of certainty regarding the equivalence of the health therapy is defined by the denominator, while the benefit
outcomes being compared, which arises from the fact that from the treatment is stated in the numerator. To directly
clinical trial results cannot be predicted in advance. Thus, calculate the net monetary cost of reaching a health
CMAs are not the starting point for prospective economic outcome, cost-benefit analysis (CBA) is used to value both
evaluations; health economists will only use CMAs as a incremental costs and outcomes in monetary terms. [16] The
methodology if the produced health outcomes are shown to societal productive value of a life-year may be considered as
be "identical or similar" in an empirical setting. The CMA is a cost when calculating a gain in life-years. One approach to
often depicted as the "poor relation" of health economic evaluating improvements to quality of life is the willingness-
methodology; critics argue that it lacks the theoretical rigor to-pay method, which determines how much people are
to be seriously examined alongside other, more complex prepared to spend in exchange for a benefit to their quality
approaches. However, health economists should realize and of life.[17]
accept that CMA has robust theoretical foundations like any
other economic evaluation approach. [11,13] By comparing the incremental cost of a program from
a particular perspective to the incremental health gain
When there are multiple treatment options with varied indicated in quality-adjusted life years (QALYs), cost-utility
efficacies, cost-effectiveness analysis (CEA) comes into analysis (CUA) is a type of economic analysis. Utility costs,
play. The expenses of the condition's treatment, both measured in terms of things like quantity and quality of life,
directly and indirectly (via work impact), are stated in the are calculated using CUA. When comparing two treatments
numerator, while the benefit to the patient, measured in life- or procedures with potentially varying benefits, cost-utility
years saved or healthy days, is stated in the denominator. In analysis is more appropriate than cost-benefit analysis.
addition, the incremental cost-effectiveness studies compare Using a single health outcome category, CUA expresses the
the two treatments.[13] value for money. It is common practice to express the ICER
Cost-effectiveness ratio = Cost/Outcome in this context as the incremental cost to achieve an
additional QALY.[17,18] This method takes a holistic view,
A more holistic view of medication expenses is measuring improvements in quality of life alongside
required for cost-effectiveness analysis (CEA). The advances in survival time. On a scale from 0 (death) to 1
monetary cost and the clinical outcome (such as the number (ideal quality of life), an improvement in QoL is represented
of lives saved, complications avoided, or diseases cured) are as a utility value. Using incremental cost-utility ratios, we
two separate but related metrics. Thus, CEA is a measure of can compare the expense of a drug's therapy to that of
the additional cost of achieving a specific health outcome alternative health therapies that provide the same or
that differs for each medication indication. CEA is a method equivalent benefits.[19]
for comparing many choices by calculating the relative
importance of each option's cost and health efficacy. The Impact of Pharmacoeconomics on Healthcare
overarching purpose of CEA is to develop a unified Pharmacoeconomics was originally an applied
metric—the ICER—that connects the value of a treatment discipline. In the years leading up to the new millennium, a
option to its differential cost. The ICER is determined using plethora of new products—mostly pharmaceuticals—came
the following formula when comparing two options: The to market at a dizzying rate, prompting the widespread belief
health resource costs, which are expressed in monetary that healthcare budgets were under pressure due to the
terms and represent the difference in costs between outsized spending on pharmaceuticals compared to other
treatment 1 and treatment 2, are the numerator in medical or areas of healthcare. Suddenly, payers wanted manufacturers
pharmacoeconomic cost-effectiveness analyses.[12,14] The to explain their products' high prices, so they turned to
non-monetary changes in health effectiveness values implied economics, clinical experts, and decision analysts for
by selecting treatment 1 over treatment 2 constitute the guidance. At first, theory did not serve as a compass for the
differential benefits of the various options (the denominator) majority of these reasons.[20] Most of these efforts focused
in cost-effectiveness analysis. Lives saved, years lived, on trying to put a price tag on the anticipated benefits and
disease episodes prevented, and other clinical or health recording the clinical results but in broader, patient-centered
outcomes are common ways to assess these results. The language. Pharmacoeconomics can be a great asset when it
cost-benefit analysis takes into account the monetary worth comes to making decisions about things like making sure the
of both the costs and benefits of interventions, in contrast to right medication is affordable and accessible to the right
CEA. The incremental cost-effectiveness ratio (ICER) is a patients at the right time, comparing drugs in the same class
metric for comparing medical intervention techniques that or with similar mechanisms of action, and holding drug
CEA uses. Data from clinical trials can be used for these manufacturers accountable for their claims. [21] By using
kinds of studies if there is information about the trials' costs pharmacoeconomics correctly, pharmacists and pharmacy
and their efficacy. Another typical way is to utilize decision administrators will be able to make better, more educated
analysis models to combine data from various sources. decisions about the services and goods they offer. In the
Interpreting their findings can be difficult because there isn't past, pharmacotherapy decisions were based only on clinical
a universally accepted definition of "cost-effectiveness" and outcomes, such as safety and efficacy. However,
IJISRT24MAR1293 www.ijisrt.com 1104
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
pharmacoeconomics has taught us that drug therapy should actual thresholds for societal assessment of health outcomes
take into account three primary outcomes: clinical, are inconsistent, arbitrary, and at odds with exploratory
economic, and humanistic. Everyone agrees that acquisition research.[21,22,23]
costs alone cannot be used to make good drug selection
decisions today.[22] In conclusion, decision-making, Handling the Results of Economic Evaluations
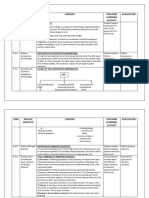
evaluating patient affordability, ensuring timely Think about the four outcomes that could occur in a
pharmaceutical access, and comparing goods for illness CEA. In the first triangle, we have "dominance" and the
treatment are all areas where applied pharmacoeconomics preferred treatment option, which is the medication with the
can be useful. In doing so, it will give evidence that runs lowest cost and higher health benefits. Secondly, in triangle
counter to the marketing of some very expensive medical IV, it is recommended that you not use the new drug
treatments. According to one school of thought, healthcare because it is more expensive and has less of an effect. In the
systems should aim to improve the health of the population third and most typical scenario, the new medicine
as a whole while staying within a certain financial outperforms the standard (quadrant I) but is also more
constraint, and the value of a new intervention can be costly. In this circumstance, ICERs are used to determine if
determined by calculating the amount of money needed to the greater benefits of the treatment are worth the extra
achieve one more healthy person. In addition, the costs, and the drug is then considered cost-effective. A
practitioners advocated for the use of quality-adjusted life predetermined ICER threshold value might serve as a
years (QALYs) as a metric for health, a unit that combines defining factor in this case. In the fourth scenario, which is
life expectancy with the anticipated quality of that life in quite similar to the third, but with the new therapy and the
comparison to an unspecified ideal of health. The idea, standard in opposite positions (triangle III), the question
however, was unsupported by evidence. It was noted that the becomes whether the additional benefits of the standard
real decision-makers were occupied with dealing with outweigh the additional costs of keeping it as the preferred
disease and its effects, rather than aiming to maximize treatment when a new, less effective but cheaper drug is
collective health. A cost-effectiveness criteria was available.[24]
subsequently necessary as a result of this. The proposed and
Fig 1.Dealing with the Outcomes of Economic Evaluations is Illustrated
IV. LIMITS OF PHARMACOECONOMIC As a result, health economics is occasionally exploited for
EVALUATION promotional purposes. To improve the efficacy and
efficiency of prescribing, clinical pharmacologists should
Because of their relative youth, health economics, and embrace pharmacoeconomic evaluation. [20,25]
pharmacoeconomics are still in the process of refining and
evaluating their methods. Health economics has a lot of Applications of Pharmacoeconomics
issues that make it hard to use in real life. From the The field of pharmacoeconomics offers valuable
assumptions taken, the selection of the comparator insights that healthcare practitioners can use in their
medicine, to the selective presentation of results, the entire practice. Drug policy and clinical decision-making are both
process could be skewed. Because pharmaceutical aided by pharmacoeconomics. Once upon a time, most drug
corporations have an interest in the outcomes of the research therapy decisions were based entirely on the clinical
they perform or fund, there is a bias in the publication of outcomes (such as safety and efficacy) linked with a
studies that are advantageous to the sponsoring companies. treatment option. However, modern pharmacotherapy
IJISRT24MAR1293 www.ijisrt.com 1105
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
includes evaluations of three fundamental outcome areas: [9]. De Rijdt, T., Willems, L., & Simoens, S. (2008).
economic, humanistic, and clinical. It has been common Economic effects of clinical pharmacy interventions: A
practice to calculate the potential financial benefits of a literature review. American Journal of Health-System
treatment option in the last fifteen to twenty years. These Pharmacy: AJHP: Official Journal of the American
days, it's all about re-involving the patient in the decision- Society of Health-System Pharmacists, 65(12), 1161–
making process by factoring in the humanistic outcomes 1172. https://doi.org/10.2146/ajhp070506
linked to treatment alternatives. Making medication [10]. Kosari, S., Deeks, L. S., Naunton, M., Dawda, P.,
selection decisions based on purchase prices alone is Postma, M. J., Tay, G. H., & Peterson, G. M. (2021).
inappropriate in today's healthcare system.[26] Funding pharmacists in general practice: A feasibility
study to inform the design of future economic
V. CONCLUSION evaluations. Research in Social & Administrative
Pharmacy: RSAP, 17(5), 1012–1016.
In conclusion, pharmacoeconomics is a vital field that [11]. Walley, T., & Haycox, A. (1997).
studies the cost-effectiveness and accessibility of Pharmacoeconomics: basic concepts and
pharmaceutical treatments, aiding policymakers and terminology. British Journal of Clinical
healthcare providers in making informed decisions about Pharmacology, 43(4), 343–348.
patient care. Economic evaluations compare health [12]. Pontinha, V. M., Wagner, T. D., & Holdford, D. A.
interventions to determine costs and outcomes, with (2021). Point-of-care testing in pharmacies—An
methods like cost-utility, cost-minimization, cost-benefit, evaluation of the service from the lens of resource-
and cost-effectiveness analyses playing key roles in based theory of competitive advantage. Journal of the
assessing the financial, medical, and subjective impacts of American Pharmacists Association: JAPhA, 61(2),
treatments. e45–e54.
[13]. Rai, M., & Goyal, R. (2018). Pharmacoeconomics in
REFERENCES Healthcare. In Pharmaceutical Medicine and
Translational Clinical Research (pp. 465–472).
[1]. Ahmad, A., Chang, J., Chung, H., Mohanta, G., Elsevier.
Parimilakrishnan, S., & Patel, I. (2013). The role of [14]. Eandi, M., Zara, G. P., & Pepa, C. D. (2000).
pharmacoeconomics in current Indian healthcare Application of pharmacoeconomics to the use of
system. Journal of Research in Pharmacy antibiotics. Clinical Microbiology and Infection: The
Practice, 2(1), 3. Official Publication of the European Society of
[2]. Drummond, M. F., Sculpher, M. J., & Torrance, G. W. Clinical Microbiology and Infectious Diseases, 6, 90–
(2005). Methods for the Economic Evaluation of 92.
Health Care Programmes. Critical Assessment of [15]. Aberidoost, M., Nikfar, S., Abdollahiasl, A., &
Economic Evaluation. Dinarvand, R. (2013). Pharmaceutical supply chain
[3]. Bootman, J. L., Townsend, R. J., & Mcghan, W. F. risks: a systematic review. Daru, 21(1).
(1996). Principles of Pharmacoeconomics. Harvey [16]. Biswkarma, V. K., & Wadhawan, S. (2020). Emerging
Whitney Books Co. role of pharmacoeconomics into clinical trials and its
[4]. International Society for Pharmacoeconomics and outcomes: An overview. Indian Journal of Pharmacy
Outcomes Research (ISPOR). Brief definition. (n.d.). and Pharmacology, 7(2), 66–72.
[5]. Rajesh, B., Isha, B. P., & Chang, J. (2010). The [17]. Taylor, D., Knapp, M., & Kerwin, R.
Emerging role of pharmacoeconomics in the Indian (2002). Pharmacoeconomics in psychiatry.
scenario. Indian J. Pharm. Pract, 2, 1–5. [18]. Henderson, L. W. (2000). Future developments in the
[6]. Jana, S., & Mondal, P. (2005). Pharmacoeconomics: treatment of end-stage renal disease: a North American
The need to sensitize undergraduate medical perspective. American Journal of Kidney Diseases:
students. Indian J Pharmacol, 37, 277–278. The Official Journal of the National Kidney
[7]. Steed, L., Sohanpal, R., Todd, A., Madurasinghe, V. Foundation, 35(4 Suppl 1), S106-16.
W., Rivas, C., Edwards, E. A., Summerbell, C. D., [19]. Lyles, A. (2008). L13 Recent trends in
Taylor, S. J. C., & Walton, R. T. (2019). Community pharmacoeconomics: Needs and unmet
pharmacy interventions for health promotion: effects needs. European Journal of Pharmaceutical Sciences:
on professional practice and health outcomes. The Official Journal of the European Federation for
Cochrane Library. Pharmaceutical Sciences, 34(1), S12.
[8]. Touchette, D. R., Doloresco, F., Suda, K. J., Perez, A., [20]. Trude, S., Au, M., & Christianson, J. B. (2006). Health
Turner, S., Jalundhwala, Y., Tangonan, M. C., & plan pay-for-performance strategies. The American
Hoffman, J. M. (2014). Economic evaluations of Journal of Managed Care, 12(9), 537–542.
clinical pharmacy services: 2006–
2010. Pharmacotherapy, 34(8), 771–793.
IJISRT24MAR1293 www.ijisrt.com 1106
Volume 9, Issue 3, March – 2024 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165 https://doi.org/10.38124/ijisrt/IJISRT24MAR1293
[21]. Chisholm-Burns, M. A., Graff Zivin, J. S., Lee, J. K.,
Spivey, C. A., Slack, M., Herrier, R. N., Hall-Lipsy, E.,
Abraham, I., & Palmer, J. (2010). Economic effects of
pharmacists on health outcomes in the United States: A
systematic review. American Journal of Health-System
Pharmacy: AJHP: Official Journal of the American
Society of Health-System Pharmacists, 67(19), 1624–
1634.
[22]. Saokaew, S., Maphanta, S., & Thangsomboon, P.
(2009). Impact of pharmacist’s interventions on cost of
drug therapy in intensive care unit. Pharmacy
Practice, 7(2).
[23]. McIntosh E, Luengo-Fernandez R. Economic
evaluation. Part 1: Introduction to the concepts of
economic evaluation in health care. J Fam Plann
Reprod Health Care. 2006;32(2):107–112.
[24]. Gyrd-Hansen, D. (2005). Willingness to pay for a
QALY: Theoretical and methodological
issues. PharmacoEconomics, 23(5), 423–432.
[25]. Torrance, G. W., & Feeny, D. (1989). Utilities and
quality-adjusted life years. International Journal of
Technology Assessment in Health Care, 5(4), 559–575.
[26]. Clement, F. M., Harris, A., Li, J. J., Yong, K., Lee, K.
M., & Manns, B. J. (2009). Using effectiveness and
cost-effectiveness to make drug coverage decisions: A
comparison of Britain, Australia, and Canada. JAMA:
The Journal of the American Medical
Association, 302(13), 1437.
IJISRT24MAR1293 www.ijisrt.com 1107
You might also like
- PACU Monitoring Sheet - RR Record - SCT-CONDocument4 pagesPACU Monitoring Sheet - RR Record - SCT-CONFitz JaminitNo ratings yet
- Mother's Class BFDocument55 pagesMother's Class BFriz04_fortitudessa5178100% (1)
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyFrom EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyRating: 4.5 out of 5 stars4.5/5 (3)
- Burning Mouth SyndromeDocument40 pagesBurning Mouth SyndromeSuci Sylvana HrpNo ratings yet
- Chapter 01Document14 pagesChapter 01flaviamarottaNo ratings yet
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- TriageDocument40 pagesTriagerizka50% (2)
- Clinical Examination Techniques in OtologyDocument44 pagesClinical Examination Techniques in OtologyDr. T. Balasubramanian100% (2)
- PhaaaaDocument101 pagesPhaaaaWesam MazenNo ratings yet
- Social and Administrative PharmacyDocument18 pagesSocial and Administrative PharmacyMarianne Cruz100% (1)
- Foundation Issues: Pharmacoeconomics: Principles, Methods, and ApplicationsDocument16 pagesFoundation Issues: Pharmacoeconomics: Principles, Methods, and ApplicationsbencleeseNo ratings yet
- Antepartum HemorrhageDocument21 pagesAntepartum HemorrhageNidhi SharmaNo ratings yet
- Pharmacoeconomicskeytoaffordablemedicines2012 130905064144Document24 pagesPharmacoeconomicskeytoaffordablemedicines2012 130905064144Tarachand Lalwani100% (1)
- PharmacoeconomicsDocument10 pagesPharmacoeconomicsKarl Ian Maliwat100% (1)
- Health Economics 1Document4 pagesHealth Economics 1Rira Fauziah INo ratings yet
- Introduction PharmacoeconomicDocument16 pagesIntroduction Pharmacoeconomic2013SecB100% (2)
- Operating Manual and Sop For Private Medical ClinicsDocument31 pagesOperating Manual and Sop For Private Medical ClinicsKlinik Rakyat LangkapNo ratings yet
- Pharmaco EconomicsDocument7 pagesPharmaco Economicsss86smkhbhNo ratings yet
- FarmacoeconomicsDocument52 pagesFarmacoeconomicsAlina-Maria CojanNo ratings yet
- Pharmacoeconomics-A Review: April 2014Document5 pagesPharmacoeconomics-A Review: April 2014chichi ramadhaniNo ratings yet
- Pharmacoeconomics in HealthcareDocument8 pagesPharmacoeconomics in HealthcareDyah Ayuwati WaluyoNo ratings yet
- Pharmacoeconomics Principles Methodsand Economic Evaluationof Drug Therapies 1Document9 pagesPharmacoeconomics Principles Methodsand Economic Evaluationof Drug Therapies 1WIKA ADMAJA KediriNo ratings yet
- Pharmaco Economic Evaluation in Polypharmacy of Elder Population: A Prospective Observational StudyDocument12 pagesPharmaco Economic Evaluation in Polypharmacy of Elder Population: A Prospective Observational StudyManeesha KodipelliNo ratings yet
- Pharmacoeconomic Research: January 2004Document3 pagesPharmacoeconomic Research: January 2004chichi ramadhaniNo ratings yet
- Pharmacoeconomics Principles Methodsand Economic Evaluationof Drug Therapies 1Document9 pagesPharmacoeconomics Principles Methodsand Economic Evaluationof Drug Therapies 1liaNo ratings yet
- Introduction To PE - chp1Document18 pagesIntroduction To PE - chp1Catalina DumitruNo ratings yet
- Pharmacoeconomics: Basic Concepts and Terminology: T. Walley & A. HaycoxDocument6 pagesPharmacoeconomics: Basic Concepts and Terminology: T. Walley & A. HaycoxIndra PratamaNo ratings yet
- Pharmacoecononics: An OverviewDocument5 pagesPharmacoecononics: An OverviewNunik Dewi KumalasariNo ratings yet
- Pharmacoeconomics An Emerging Branch in Health SciDocument7 pagesPharmacoeconomics An Emerging Branch in Health Scichichi ramadhaniNo ratings yet
- Article 4Document7 pagesArticle 4nindafathiaNo ratings yet
- Economic Effects of Clinical Pharmacy Interventions: A Literature ReviewDocument12 pagesEconomic Effects of Clinical Pharmacy Interventions: A Literature ReviewIndra PratamaNo ratings yet
- The Value of Self Medication Summary of Existing Evidence PDFDocument12 pagesThe Value of Self Medication Summary of Existing Evidence PDFRoberto GarceteNo ratings yet
- Eview F Herapeutics: Economic Evaluations of Clinical Pharmacy Services: 2006 - 2010Document23 pagesEview F Herapeutics: Economic Evaluations of Clinical Pharmacy Services: 2006 - 2010Igor SilvaNo ratings yet
- Economic Impact of Antimicrobial Resistance: Special IssueDocument7 pagesEconomic Impact of Antimicrobial Resistance: Special IssueTiexinNo ratings yet
- Digital Drugs An Anatomy of New Medicines PDFDocument27 pagesDigital Drugs An Anatomy of New Medicines PDFshraddha5jNo ratings yet
- Pharmacoepidemiology: Pinar Yalcin Balcik, Gulcan KahramanDocument6 pagesPharmacoepidemiology: Pinar Yalcin Balcik, Gulcan KahramandebbyirmaNo ratings yet
- Mr. Hariom Rajput Mr. Ramsingh Ji Gmail-ID International Association of Oncology (IAO) Government of IndiaDocument6 pagesMr. Hariom Rajput Mr. Ramsingh Ji Gmail-ID International Association of Oncology (IAO) Government of IndiaHariom RajputNo ratings yet
- Fundamental Understanding of Pharmacoeconomics As An Innovative Concept Within The Modern Clinical Pharmacy in Today's Healthcare SystemDocument17 pagesFundamental Understanding of Pharmacoeconomics As An Innovative Concept Within The Modern Clinical Pharmacy in Today's Healthcare SystemKemal Surji PhD RRTNo ratings yet
- PharmacoepidemiologyDocument2 pagesPharmacoepidemiologyFyrrNo ratings yet
- Pharmacoeconomics NewDocument62 pagesPharmacoeconomics NewgowthamNo ratings yet
- 3.outcome AnalyzeDocument29 pages3.outcome AnalyzeMunawar ReyhanNo ratings yet
- Pharmacoeconomics As Applied To Hospital Pharmacy HandoutDocument20 pagesPharmacoeconomics As Applied To Hospital Pharmacy HandoutLeylu RepatoNo ratings yet
- Social Pharmacy Assignment 2Document9 pagesSocial Pharmacy Assignment 2mdsahilkusugal17No ratings yet
- 2017 MethodologicalApproachHealthEconEv IJPHCSDocument13 pages2017 MethodologicalApproachHealthEconEv IJPHCSyanti ikmNo ratings yet
- AYU NOVITA-dikonversiDocument17 pagesAYU NOVITA-dikonversiRita AnggrainiNo ratings yet
- The Pharmaceutical Industry Analysis REVISED 2Document5 pagesThe Pharmaceutical Industry Analysis REVISED 2Even a smallest lie can break a biggestNo ratings yet
- Consumers Views On Generic Medicines A Reiew of TDocument11 pagesConsumers Views On Generic Medicines A Reiew of TlabiaernestoNo ratings yet
- Pharmacopolitics, Implications and Implementation in Clinical StudiesDocument3 pagesPharmacopolitics, Implications and Implementation in Clinical StudiesNantarat KengkeatchaiNo ratings yet
- ADocument6 pagesANeharika MahajanNo ratings yet
- Pharmaceutical MarketingDocument6 pagesPharmaceutical MarketingFazal MalikNo ratings yet
- Pharmacoeconomics FinalDocument62 pagesPharmacoeconomics FinalYash SoniNo ratings yet
- Artikel Bing 2Document5 pagesArtikel Bing 2Putri FebrianaNo ratings yet
- A Clinician's Guide To Cost-Effectiveness Analysis: Annals of Internal Medicine. 1990 113:147-154Document8 pagesA Clinician's Guide To Cost-Effectiveness Analysis: Annals of Internal Medicine. 1990 113:147-154dsjervisNo ratings yet
- Medicine Shortages: Impact Behind Numbers: Research Open AccessDocument12 pagesMedicine Shortages: Impact Behind Numbers: Research Open Accesscnmoar97No ratings yet
- Administration of Medicine Policy (Final)Document15 pagesAdministration of Medicine Policy (Final)onesmusnzomo20No ratings yet
- Post Marketing Surveillance and PharmacoepidemiologyDocument7 pagesPost Marketing Surveillance and PharmacoepidemiologyEditor IJTSRDNo ratings yet
- LEC 1 Basic Concepts of Pharmacoeconomics 2023Document13 pagesLEC 1 Basic Concepts of Pharmacoeconomics 2023ouribin1989No ratings yet
- Role of The Pharmacist in Antimicrobial Stewardship: Rachel Fortin, Pharmd, BcpsDocument2 pagesRole of The Pharmacist in Antimicrobial Stewardship: Rachel Fortin, Pharmd, BcpsSih AtiiNo ratings yet
- qt5j15k0nf NosplashDocument2 pagesqt5j15k0nf NosplashsinayaphetNo ratings yet
- Chapter 9. Pharmacoeconomics and Economic Evaluation of Drug TherapiesDocument9 pagesChapter 9. Pharmacoeconomics and Economic Evaluation of Drug TherapiesJuan AntonioNo ratings yet
- Tinpus FarmakoekonomiDocument6 pagesTinpus FarmakoekonomiYesi Widya IswariNo ratings yet
- Practice Standard Safety & QualityDocument2 pagesPractice Standard Safety & Qualityssreya80No ratings yet
- Article 7yCODocument11 pagesArticle 7yCOAychluhm TatekNo ratings yet
- Literature Review On Medication Errors in HospitalsDocument7 pagesLiterature Review On Medication Errors in Hospitalsfvgjcq6aNo ratings yet
- Cheers Statement IsporDocument5 pagesCheers Statement IsporKatherine CuéllarNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Study Assessing Viability of Installing 20kw Solar Power For The Electrical & Electronic Engineering Department Rufus Giwa Polytechnic OwoDocument6 pagesStudy Assessing Viability of Installing 20kw Solar Power For The Electrical & Electronic Engineering Department Rufus Giwa Polytechnic OwoInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Blockchain Based Decentralized ApplicationDocument7 pagesBlockchain Based Decentralized ApplicationInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Unmasking Phishing Threats Through Cutting-Edge Machine LearningDocument8 pagesUnmasking Phishing Threats Through Cutting-Edge Machine LearningInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cyber Security Awareness and Educational Outcomes of Grade 4 LearnersDocument33 pagesCyber Security Awareness and Educational Outcomes of Grade 4 LearnersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- An Industry That Capitalizes Off of Women's Insecurities?Document8 pagesAn Industry That Capitalizes Off of Women's Insecurities?International Journal of Innovative Science and Research TechnologyNo ratings yet
- Factors Influencing The Use of Improved Maize Seed and Participation in The Seed Demonstration Program by Smallholder Farmers in Kwali Area Council Abuja, NigeriaDocument6 pagesFactors Influencing The Use of Improved Maize Seed and Participation in The Seed Demonstration Program by Smallholder Farmers in Kwali Area Council Abuja, NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smart Health Care SystemDocument8 pagesSmart Health Care SystemInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Insights Into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesDocument8 pagesInsights Into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Parastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueDocument2 pagesParastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Visual Water: An Integration of App and Web To Understand Chemical ElementsDocument5 pagesVisual Water: An Integration of App and Web To Understand Chemical ElementsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smart Cities: Boosting Economic Growth Through Innovation and EfficiencyDocument19 pagesSmart Cities: Boosting Economic Growth Through Innovation and EfficiencyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Compact and Wearable Ventilator System For Enhanced Patient CareDocument4 pagesCompact and Wearable Ventilator System For Enhanced Patient CareInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Impact of Silver Nanoparticles Infused in Blood in A Stenosed Artery Under The Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in A Sten. Art. Under The Eff. of Mag. FieldDocument6 pagesImpact of Silver Nanoparticles Infused in Blood in A Stenosed Artery Under The Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in A Sten. Art. Under The Eff. of Mag. FieldInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Predict The Heart Attack Possibilities Using Machine LearningDocument2 pagesPredict The Heart Attack Possibilities Using Machine LearningInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Air Quality Index Prediction Using Bi-LSTMDocument8 pagesAir Quality Index Prediction Using Bi-LSTMInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Relationship Between Teacher Reflective Practice and Students Engagement in The Public Elementary SchoolDocument31 pagesThe Relationship Between Teacher Reflective Practice and Students Engagement in The Public Elementary SchoolInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Parkinson's Detection Using Voice Features and Spiral DrawingsDocument5 pagesParkinson's Detection Using Voice Features and Spiral DrawingsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Investigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatDocument16 pagesInvestigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Implications of Adnexal Invasions in Primary Extramammary Paget's Disease: A Systematic ReviewDocument6 pagesImplications of Adnexal Invasions in Primary Extramammary Paget's Disease: A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Keywords:-Ibadhy Chooranam, Cataract, Kann Kasam,: Siddha Medicine, Kann NoigalDocument7 pagesKeywords:-Ibadhy Chooranam, Cataract, Kann Kasam,: Siddha Medicine, Kann NoigalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- An Analysis On Mental Health Issues Among IndividualsDocument6 pagesAn Analysis On Mental Health Issues Among IndividualsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Harnessing Open Innovation For Translating Global Languages Into Indian LanuagesDocument7 pagesHarnessing Open Innovation For Translating Global Languages Into Indian LanuagesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Utilization of Date Palm (Phoenix Dactylifera) Leaf Fiber As A Main Component in Making An Improvised Water FilterDocument11 pagesThe Utilization of Date Palm (Phoenix Dactylifera) Leaf Fiber As A Main Component in Making An Improvised Water FilterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Making of Object Recognition Eyeglasses For The Visually Impaired Using Image AIDocument6 pagesThe Making of Object Recognition Eyeglasses For The Visually Impaired Using Image AIInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Advancing Healthcare Predictions: Harnessing Machine Learning For Accurate Health Index PrognosisDocument8 pagesAdvancing Healthcare Predictions: Harnessing Machine Learning For Accurate Health Index PrognosisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diabetic Retinopathy Stage Detection Using CNN and Inception V3Document9 pagesDiabetic Retinopathy Stage Detection Using CNN and Inception V3International Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Digital Marketing Dimensions On Customer SatisfactionDocument6 pagesThe Impact of Digital Marketing Dimensions On Customer SatisfactionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Terracing As An Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains - CameroonDocument14 pagesTerracing As An Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains - CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Dense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)Document2 pagesDense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Formulation and Evaluation of Poly Herbal Body ScrubDocument6 pagesFormulation and Evaluation of Poly Herbal Body ScrubInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Rle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNDocument33 pagesRle Lectures Medications: Arturo G. Garcia JR RN, MSN, U.S RNMaria Paula Amor GeronimoNo ratings yet
- SepsisDocument43 pagesSepsisHamza Shaikh100% (1)
- Mackenzie TortorichDocument2 pagesMackenzie Tortorichapi-509402148No ratings yet
- Student'S Copy Please Do Not DuplicateDocument134 pagesStudent'S Copy Please Do Not DuplicateChn ypNo ratings yet
- Physical Activities Toward Health and Fitness 2Document15 pagesPhysical Activities Toward Health and Fitness 2Danilo CuntapayNo ratings yet
- 10 3889@oamjms 2019 300Document6 pages10 3889@oamjms 2019 300Rudi WsNo ratings yet
- Learning PlanDocument7 pagesLearning Planapi-283070240No ratings yet
- 5 Storyboard (Contoh 1)Document1 page5 Storyboard (Contoh 1)RaniCianTarNo ratings yet
- The Five Senses: A Patient Preference-Based Comparative AnalysisDocument8 pagesThe Five Senses: A Patient Preference-Based Comparative AnalysisasclepiuspdfsNo ratings yet
- The Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliDocument3 pagesThe Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliImran TarmiziNo ratings yet
- Lecture 4. Patient Counseling ComplianceDocument8 pagesLecture 4. Patient Counseling Compliancedaniya nadeemNo ratings yet
- Child Health Problems GlobalDocument86 pagesChild Health Problems GlobalBagus P Agen SuplierNo ratings yet
- Triclosan 0410Document1 pageTriclosan 0410TeenahNo ratings yet
- Neglected Tropical Disease - Review Article DraftDocument31 pagesNeglected Tropical Disease - Review Article DraftpriyalkudavNo ratings yet
- Epidemiology Course OutlineDocument6 pagesEpidemiology Course OutlineFYMNo ratings yet
- First Aid Quiz IDocument32 pagesFirst Aid Quiz Ianon_617170800No ratings yet
- 2018 Management of Multiply Injured Pediatric Trauma Patients in The Emergency Department PDFDocument20 pages2018 Management of Multiply Injured Pediatric Trauma Patients in The Emergency Department PDFVladimir Basurto100% (1)
- The Complete Guide To Weight Loss and FitnessDocument4 pagesThe Complete Guide To Weight Loss and FitnessOnika BoteroNo ratings yet
- Vehling Annika ResumeDocument1 pageVehling Annika Resumeapi-733364471No ratings yet
- Kasus 1 RKG 5 Euginia YosephineDocument5 pagesKasus 1 RKG 5 Euginia YosephineEuginia YosephineNo ratings yet
- Artikel No. 5 PCX - ReportDocument13 pagesArtikel No. 5 PCX - ReportAnonymous Q6Ih0AfJNo ratings yet
- Dental Management of The Cardiovascular Compromised Patient: A Clinical ApproachDocument4 pagesDental Management of The Cardiovascular Compromised Patient: A Clinical ApproachMiftahul JannahNo ratings yet