Professional Documents
Culture Documents
Burns Guideline
Uploaded by
Roi LevinzonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Burns Guideline
Uploaded by
Roi LevinzonCopyright:
Available Formats
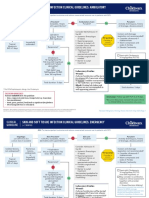
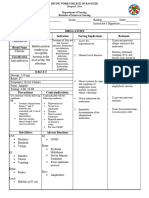
Clinical Guideline
Burns (Adult and Pediatric)
Severe Criteria Patient presents with a burn injury. Signs of Impending Airway
Compromise
• Circumferential burns
• Burns across joints • History of enclosed space fire
• Burns of face, neck, or groin Assess VS, circulation, airway, and breathing. (including house fire)
• Electrical/chemical burns • Burn injury or soot in oropharynx
• Inhalation injuries/respiratory distress • Stridor or wheezing
• Trauma (refer to ATLS) • Circumferential burn of neck
• Any full-thickness (3rd degree) burns Are there signs of impending Consider early
airway compromise? Yes endotracheal
See Box. intubation. Village Management
Disposition Considerations/Criteria
For any burn that warrants travel to
No
Village: wound care by health aides over RMT, Bethel, instruct health aides to apply
consider PT by telehealth. bacitracin and NOT silvadene to avoid
• Pain controlled on PO regimen. Assess total body surface area (TBSA) painful cleaning of wounds in Bethel.
• No sign of wound infection. affected by partial or full thickness burns.
• Unlikely to require further debridement.
• Patient/caregiver/health aide able to perform • IV access
dressing changes. Adult TBSA > 10%? • Analgesia
Child TBSA > 5%? Yes • Labs: CBC with diff, CMP, UDS, EtOH, CK, coags.
Outpatient (ED/Outpatient Clinic/PT): daily follow-up Severe criteria? See Box. • If inhalation injury, add ABG, carboxyhemoglobin.
for wound management and ROM exercises. • If TBSA >15%, give IVF per Consensus Formula in box.
• Wound infection improving on PO antibiotic regimen.
• Debridement not more than once/day. No
• Dressing changes not more than twice/day. Findings Concerning for Abuse
• Need for PT assessment not more than twice/week. Wound Care
• Delay in seeking care
Inpatient YKHC: • Debridement as appropriate. Debride clear • Variations in history
• Pain uncontrolled on oral medications. blisters >2 cm. Consider sedation. Consult • Injuries inconsistent with history
• Dressing changes more than twice/day. • Cleanse in dilute chlorhexidine solution. General • Immersion injuries
• Wound infection requiring IV antibiotics. • Apply bacitracin or mupirocin and cover Surgeon. • Uniform depth
• Nonambulatory (including wounds on both feet). with Adaptic. • Well-demarcated burn margins
• Wrap with dry gauze. • Geometric pattern/object imprint
Inpatient ANMC: • Elevate/compress affected extremities.
• Critical illness. If any concern for abuse, send a
• Wound requiring operative debridement or grafting. message to Child Abuse on Call
• Surgeon recommends higher level of care. Determine disposition. See Box. by Tiger Connect.
• Child with severe criteria.
• If expected wound care exceeds currently available
resources at YKHC. Consensus Formula (Brooke/Parkland)
Only used if TBSA >15%.
Lund and Browder Chart to Estimate TBSA in Adults and Children
(weight in kg) x 2-4 mL x %TBSA = total fluid to be given over 24 hours
Do not convert %TBSA to a decimal. For example, 15% TBSA would be 15.
Give half in first eight hours from time of burn. Give other half over the next sixteen hours.
If delayed presentation, begin at initial calculated 8 hour rate; do not “catch up” with fluid boluses.
Goal UOP 0.5-1 mL/kg/hour.
Use LR used for adults unless mitigating circumstances. For pediatric patients <30 kg, add D5.
Classification of Burns by Depth
Burns evolve over time; initial TBSA and depth classification can change and often the difference
between deep partial thickness and full thickness can only be determined operatively.
• Superficial (1st degree): epidermis only, dry, red, blanches with pressure, no blisters, painful.
• Superficial partial-thickness (2nd degree): epidermis and part of dermis, blisters, moist, red,
weeping, blanches with pressure, painful.
• Deep partial-thickness (2nd degree): epidermis and deep dermis, blisters, wet or waxy dry,
patchy white to red, does not blanch, pressure sensation only.
• Full-thickness (3rd degree): epidermis and entire dermis, waxy white to leathery gray to
charred/black, dry and inelastic, does not blanch, sensation to deep pressure only, may be
defined as 4th degree with extension into underlying fascia, muscle, or bone.
This gu ideline is designed for the gen eral use o f most patients but may need to b e a dapted
to mee t th e special nee ds of a specifi c patient a s determined by the medical practitio ner.
Approved by Clinical Guideline Committee 4/28/23. Click here to see the supplemental resources for this guideline.
If comm ents about this guide line, plea se contac t Travis_Nelson@yk hc .org.
You might also like
- 1 Burns and Grafts Dr. Gio Santos September 3 2021Document7 pages1 Burns and Grafts Dr. Gio Santos September 3 2021L4 CLERK - UY, Rhea Andrea F.No ratings yet
- 12b. Burns Injury (Russells Hall Hospital, UPDATED Mar 2012)Document11 pages12b. Burns Injury (Russells Hall Hospital, UPDATED Mar 2012)akshayNo ratings yet
- BurnsDocument4 pagesBurnsjuliusNo ratings yet
- Corneal Disease and Dystrophy Management PDFDocument53 pagesCorneal Disease and Dystrophy Management PDFScerbatiuc CristinaNo ratings yet
- Fever Measles Ear ProblemsDocument10 pagesFever Measles Ear ProblemsEBNo ratings yet
- L3-SURG-Burns (Aug3021)Document5 pagesL3-SURG-Burns (Aug3021)Marc Lyndon CafinoNo ratings yet
- 2014 Burn Patient Management - Clinical Practice GuidelinesDocument70 pages2014 Burn Patient Management - Clinical Practice Guidelinesd dNo ratings yet
- NCP AccDocument19 pagesNCP AccAthyrah KadirNo ratings yet
- LSEBN Initial Management of SEVERE BurnsDocument1 pageLSEBN Initial Management of SEVERE Burnskareem186No ratings yet
- Arizona Burncenter Guidelines PDFDocument20 pagesArizona Burncenter Guidelines PDFBuyungNo ratings yet
- Mod 7 & 8 Study GuidesDocument11 pagesMod 7 & 8 Study GuidesFerd RuizNo ratings yet
- Burns (NCM 112 - Medsurg)Document5 pagesBurns (NCM 112 - Medsurg)mblanco.dchNo ratings yet
- Burn Education Module 2.14.22Document22 pagesBurn Education Module 2.14.22Ashraf HusseinNo ratings yet
- Drug Study NicoleDocument6 pagesDrug Study NicoleFrancheska Nicole Delos SantosNo ratings yet
- Burns: by Victoria S. Brioso-AngDocument33 pagesBurns: by Victoria S. Brioso-AngAmanda OsbornNo ratings yet
- Symptom Management Guidelines: Radiation Dermatitis: Type of Radiation and EnergyDocument11 pagesSymptom Management Guidelines: Radiation Dermatitis: Type of Radiation and EnergyAdonanNo ratings yet
- Concept Map 4 AnsiiDocument1 pageConcept Map 4 Ansiiapi-523409624No ratings yet
- Burn Injury ABCDocument96 pagesBurn Injury ABCSheryl Ann Barit PedinesNo ratings yet
- Pleural Effusion Case PresentationDocument16 pagesPleural Effusion Case PresentationDhindee OmahoyNo ratings yet
- Drugn Study 2 0Document15 pagesDrugn Study 2 0Ken ChavezNo ratings yet
- 2nd Rotation Drug StudyDocument10 pages2nd Rotation Drug StudyKarolien Faye DongaNo ratings yet
- NCP Mandibular)Document5 pagesNCP Mandibular)yellarfNo ratings yet
- Bu VonnyDocument41 pagesBu VonnyZola IsmuNo ratings yet
- Cefuroxime Drug Study Rosemarie Llanillo BSN Ii eDocument3 pagesCefuroxime Drug Study Rosemarie Llanillo BSN Ii eFernandez, Florence NicoleNo ratings yet
- DrugStudy - 01 02 24Document3 pagesDrugStudy - 01 02 24Laurente, Patrizja Ysabel B. BSN-2DNo ratings yet
- Peri OpDocument9 pagesPeri OpggukNo ratings yet
- Burns: Alhad Naragude Final Year M.B.B.S (BJMC Pune) Dr. Pawan Chumbale M.S, MCH Plastic Surgery (Sassoon Hospital, Pune)Document93 pagesBurns: Alhad Naragude Final Year M.B.B.S (BJMC Pune) Dr. Pawan Chumbale M.S, MCH Plastic Surgery (Sassoon Hospital, Pune)EuniceGeraldineNo ratings yet
- Electrical Burn: Xantipphy Mae IbrahimDocument32 pagesElectrical Burn: Xantipphy Mae IbrahimMinette EmmanuelNo ratings yet
- CPG Bite StingsDocument10 pagesCPG Bite StingsMarvin M PulaoNo ratings yet
- Symptom Management Guidelines: Care of Malignant WoundsDocument7 pagesSymptom Management Guidelines: Care of Malignant WoundsPatrico Rillah Setiawan100% (1)
- BEC Conflict Primary Survey Module1 ENDocument16 pagesBEC Conflict Primary Survey Module1 ENOsamaNo ratings yet
- WHO-ICRC Basic Emergency Care CourseDocument74 pagesWHO-ICRC Basic Emergency Care CoursevverasanczNo ratings yet
- Clinical Practice Guidelines Cellulitis and AbscessDocument7 pagesClinical Practice Guidelines Cellulitis and AbscessAhmad Rafi Satrio PrayogoNo ratings yet
- 03 Perioperative NursingDocument3 pages03 Perioperative NursingAngeli IdrisNo ratings yet
- Burn CareDocument3 pagesBurn CareRafaela LennyNo ratings yet
- Referat Bedah Plastik RosDocument43 pagesReferat Bedah Plastik RosRisna AnnisaNo ratings yet
- Burn Injuries FdneDocument25 pagesBurn Injuries FdneRonit ChandNo ratings yet
- AMPUTATIONDocument6 pagesAMPUTATIONapi-3822433No ratings yet
- Bactericidal Inhibits Cell Wall Mucopeptide Synthesis: CeftriaxonDocument4 pagesBactericidal Inhibits Cell Wall Mucopeptide Synthesis: Ceftriaxonzesty-merr-l-akut-9424No ratings yet
- 2A - Pasay - Module 8 - ElaborateDocument23 pages2A - Pasay - Module 8 - ElaborateTrishaNo ratings yet
- Delantar 3bsna Parotidectomy Pleomorophic AdenomaDocument26 pagesDelantar 3bsna Parotidectomy Pleomorophic AdenomasharedNo ratings yet
- Healthcare 5.5 Session1Document3 pagesHealthcare 5.5 Session1JAY JR. APONNo ratings yet
- Protocolos Minnesota Piel ATBDocument8 pagesProtocolos Minnesota Piel ATBDaniel Alejandro CastrilloNo ratings yet
- Nursing Care PlansDocument16 pagesNursing Care PlansJobelle AcenaNo ratings yet
- LSEBN Burns Referral CriteriaDocument1 pageLSEBN Burns Referral CriteriaAna TataranuNo ratings yet
- Pneumonia AdultDocument1 pagePneumonia AdultRoi LevinzonNo ratings yet
- Consult Training 1Document9 pagesConsult Training 1Lumos MaximaNo ratings yet
- CaftriaxonedrugstudyDocument1 pageCaftriaxonedrugstudyAdrianne Khyle OngNo ratings yet
- NCP and Fdar.Document4 pagesNCP and Fdar.Ralph Laurent De DiosNo ratings yet
- ClindamycinDocument2 pagesClindamycinCrissah LacernaNo ratings yet
- Problem 2 ErwinDocument26 pagesProblem 2 ErwinZhy YouichiNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanIrish Paping TucyapaoNo ratings yet
- Surgery PDFDocument163 pagesSurgery PDFjoedeegan_100% (1)
- Skin and Soft Tissue Infections (Sstis) Clinical Guideline CellulitisDocument4 pagesSkin and Soft Tissue Infections (Sstis) Clinical Guideline Cellulitisཛཉཀབས0% (1)
- Nursing Care Plan: MDH Ob/GyneDocument10 pagesNursing Care Plan: MDH Ob/GyneTrisha Dianne RaquenioNo ratings yet
- Approach To A Patient of Bullous DisorderDocument50 pagesApproach To A Patient of Bullous DisorderAbhirut ThakurNo ratings yet
- DRUG STUDY - DobutamineDocument3 pagesDRUG STUDY - DobutamineAjon Veloso75% (4)
- Tatalaksana Luka Bakar Pada Layanan Primer - FBBDocument31 pagesTatalaksana Luka Bakar Pada Layanan Primer - FBBfebiola sihiteNo ratings yet
- Management of Burns ReadingDocument28 pagesManagement of Burns Readinghimanshugupta811997No ratings yet
- Clinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3From EverandClinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3No ratings yet
- Differentiate Between Antimortem and Postmortem Asphyxial DeathDocument9 pagesDifferentiate Between Antimortem and Postmortem Asphyxial DeathMahnoor AyeshaNo ratings yet
- Kavitt Robert T Diagnosis and Treatment of Peptic 2019Document10 pagesKavitt Robert T Diagnosis and Treatment of Peptic 2019Nix Santos100% (1)
- Afeccion Ocular y Blefaroconjuntivitis Por Leishmania de HumanosDocument4 pagesAfeccion Ocular y Blefaroconjuntivitis Por Leishmania de HumanosPilar Sanchez GuiraoNo ratings yet
- Department of Education: Republic of The PhilippinesDocument2 pagesDepartment of Education: Republic of The PhilippinesJonelyn MercadoNo ratings yet
- New BookDocument2 pagesNew BookKaren Raskin KleimanNo ratings yet
- PhysioEx Exercise 7 Activity 1Document3 pagesPhysioEx Exercise 7 Activity 1CLAUDIA ELISABET BECERRA GONZALESNo ratings yet
- NURS FPX 5003 Assessment 4 Executive Summary - Community Health AssessmentDocument6 pagesNURS FPX 5003 Assessment 4 Executive Summary - Community Health AssessmentCarolyn HarkerNo ratings yet
- Pharmaceutics 3Document30 pagesPharmaceutics 3Shahid Manzoor50% (2)
- Head & Neck TumoursDocument15 pagesHead & Neck TumoursMalueth AnguiNo ratings yet
- Yang2015 Pili TortiDocument3 pagesYang2015 Pili TortiErnawati HidayatNo ratings yet
- Squash Seeds FinalDocument19 pagesSquash Seeds FinalMae TomeldenNo ratings yet
- The Safe & Effective Care EnvironmentDocument140 pagesThe Safe & Effective Care EnvironmentMoreiyamNo ratings yet
- 9.cancer of The Female Genital Tract.Document58 pages9.cancer of The Female Genital Tract.vichramNo ratings yet
- Community Based Assessment Checklist (CBAC) FormDocument3 pagesCommunity Based Assessment Checklist (CBAC) FormShubhaDavalgiNo ratings yet
- MAN 32025 Forpdf Rev0Document16 pagesMAN 32025 Forpdf Rev0alejandra ojeda anayaNo ratings yet
- 1581 PDF PDFDocument7 pages1581 PDF PDFNyinyizaw ZawNo ratings yet
- First Aid Booklet: Transition Passport / Daily Living / HealthDocument11 pagesFirst Aid Booklet: Transition Passport / Daily Living / Healthmaggie HurleyNo ratings yet
- IVT FORM 09 S 09Document1 pageIVT FORM 09 S 09lamuraoNo ratings yet
- ASHP COVID 19 Evidence TableDocument138 pagesASHP COVID 19 Evidence TableOrchid Limoso LozanoNo ratings yet
- Paraphrase DDocument62 pagesParaphrase DVignesh GNo ratings yet
- 13 - Universal Precautions: Safety Training: Eh&S - MgaDocument2 pages13 - Universal Precautions: Safety Training: Eh&S - MgaPradnya ParamitaNo ratings yet
- Hypovolemic Shock PathophysiologyDocument8 pagesHypovolemic Shock PathophysiologyKAYCEENo ratings yet
- Clinical Uses of Diode Lasers in Orthodontics PDFDocument8 pagesClinical Uses of Diode Lasers in Orthodontics PDFmonwarul azizNo ratings yet
- Curriculum For One Year Fellowship in Pain ManagementDocument8 pagesCurriculum For One Year Fellowship in Pain ManagementDr. Pankaj N SurangeNo ratings yet
- 10 Reasons Why Friendship Is ImportantDocument12 pages10 Reasons Why Friendship Is ImportantVlad CheaburuNo ratings yet
- Identification Death Dying Declaration AGE: Presented byDocument82 pagesIdentification Death Dying Declaration AGE: Presented bySaveeza Kabsha AbbasiNo ratings yet
- Ziad Abdeen PDFDocument46 pagesZiad Abdeen PDFIron Man-tcpNo ratings yet
- Internet of Nano, Bio-Nano, Biodegradable And-3-4Document2 pagesInternet of Nano, Bio-Nano, Biodegradable And-3-47d96d1b6a8No ratings yet
- CV McafeeDocument8 pagesCV Mcafeeapi-510952416No ratings yet
- Baltimore County Resource Guide December 2023Document13 pagesBaltimore County Resource Guide December 2023api-516741446No ratings yet