Professional Documents
Culture Documents
Lyann 2019
Uploaded by
valperlunCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lyann 2019
Uploaded by
valperlunCopyright:
Available Formats
Efficacy of Various Surface Treatments on the Bonding
Performance of Saliva-contaminated Lithium-Disilicate
Ceramics
Sai Kham Lyanna / Tomohiro Takagakib / Toru Nikaidoc / Takahiro Wadad / Motohiro Uoe /
Masaomi Ikedaf / Alireza Sadrg / Junji Tagamih
Purpose: To investigate the efficacy of different ceramic surface cleaning methods after saliva contamination on
the resin bond strength to lithium disilicate ceramics.
Materials and Methods: 300 e.max CAD blocks (Ivoclar Vivadent) were polished with 600-grit silicon carbide paper
and divided into five groups with or without human saliva contamination and according to the surface treatment
performed (n = 10); control: no pretreatment; MP: Monobond Plus; PA+MP: 37% phosphoric acid (PA) followed by
MP; HF+MP: 5% hydrofluoric acid (HF) followed by MP; MEP: Monobond Etch & Prime. The specimens were bonded
with one of three resin cements: Variolink Esthetic DC (VE), Multilink Automix (MA) and Speed CEM (SC). After 24-h
water storage, tensile bond strength (TBS) was measured. The ceramic surfaces after pretreatment were analyzed
using x-ray photoelectron spectroscopy (XPS).
Results: XPS analysis showed similar elemental distributions between saliva contamination vs no saliva in PA, HF,
and MEP. The TBSs were significantly influenced by surface treatments (p < 0.05). HF+MP and MEP showed statisti-
cally non-significantly different bond strengths to saliva-contaminated HF+MP and MEP, but were different from MP
and saliva-contaminated MP. The TBSs after 24 h were significantly higher in HF+MP and MEP groups with VE. HF+MP
and MEP did not show statistically significant differences among any groups with or without saliva contamination.
Conclusion: Surface treatments with PA or HF followed by silane or by MEP alone were effective in removing saliva
contamination and enhancing the resin bond strength.
Keywords: lithium disilicate ceramics, saliva-contaminated, tensile bond strength.
J Adhes Dent 2019; 21: 51–58. Submitted for publication: 01.06.18; accepted for publication: 25.11.18
doi: 10.3290/j.jad.a41918
T he demands for esthetic restorations have increased
substantially in recent years, and the popularity of all-
ceramic materials as an alternative to metal-ceramic for in-
microscopic surface flaws, but the resistance to crack prop-
agation of ceramics has been improved by leucite, fluor-
mica, or alumina reinforcement of the glass matrix.23 Many
direct restorations has therefore grown. A weak point for all studies have documented the success of glass-ceramic
ceramics is considered to be the extension and growth of restorations bonded with resin-based cements. However, to
a Student, Cariology and Operative Dentistry, Graduate School of Medical and f Junior Assistant Professor, Oral Prosthetic Engineering, Graduate School,
Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. Participated Tokyo, Japan. Performed a statistical analysis, contributed substantially to dis-
in experimental design, performed the experiments, wrote the manuscript. cussion.
b Assistant Professor, Cariology and Operative Dentistry, Graduate School of Med- g Associate Professor, Department of Restorative Dentistry, University of Wash-
ical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. ington School of Dentistry, Seattle, WA, USA. Contributed substantially to dis-
Idea, hypothesis, experimental design, proofread the manuscript. cussion, proofread the manuscript.
c Lecturer, Department of Operative Dentistry, Division of Oral Functional Sci- h Professor, Cariology and Operative Dentistry, Graduate School of Medical and
ence and Rehabilitation, School of Dentistry, Asahi University, Gifu, Japan. Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan. Sup-
d ported the experiments, contributed substantially to discussion.
Assistant Professor, Advanced Biomaterials, Graduate School, Tokyo Medical
and Dental University, Tokyo, Japan. Contributed substantially to discussion,
proofread the manuscript.
Correspondence: Tomohiro Takagaki, Cariology and Operative Dentistry, Gradu-
e Professor, Advanced Biomaterials, Graduate School, Tokyo Medical and Dental ate School of Medical and Dental Sciences, Tokyo Medical and Dental University,
University, Tokyo, Japan. Contributed substantially to discussion, proofread the 1-5-45, Yushima, Bunkyo-ku, Tokyo 113-8510, Japan. Tel: +813-5803-5483;
manuscript. e-mail address: takagaki.ope@tmd.ac.jp
Vol 21, No 1, 2019 51
Lyann et al
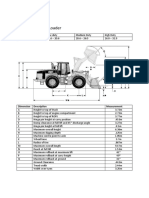
Ultrasonic cleaning
(deionized water 5 min, immersed in human saliva (1 min.)
ethanol 2 min) and washed with water and air dried
air drying
IPS e.max CAD (5 mm x 15 mm)
•sintering Surface treatment
•polishing with #600 SiC paper
1. Control (no treatment)
2. No treatment + Monobond Plus (60 s)
3. Phosphoric acid (20 s) + Monobond Plus (60 s)
4. Hydrofluoric acid (20 s) + Monobond Plus (60 s)
5. Monobond Etch & Prime (scrub for 20 s, leave to
react for 40 s)
metal rod
The specimens were
resin cement Failure mode
stored in deionized water Tensile bond
aluminium tape at 37°C for 24 h strength test analysis by SEM
e.max CAD block
Filled with resin cement
and light cured for 40 s
Fig 1 Schematic representation of specimen preparation design.
optimally create a resin-ceramic bond, glass-ceramic resto- surface.1,16,29 In fact, due to the hazardous potential of HF,
rations should be pretreated with hydrofluoric acid (HF) and its chairside application should be performed with cau-
a silane coupling agent.22 HF creates porosities in the tion.24 As a result, alternative cleaning methods without the
glass ceramic, and the coupling agent serves the dual pur- use of HF have been sought, including rinsing with water,25
pose of binding to the silica of the ceramic and to the meth- etching with phosphoric acid, and cleaning with alcohol.34
acrylate group of the adhesive resin.4,22 Despite the fact that these methods are easy to apply, they
Ceramic etching with HF can be performed either at did not seem to recover the bonding capacity of ceramic
chairside by the dentist or in the dental laboratory by the restorations compared to non-contaminated surfaces.25,34
dental technician. As a series of surveys on clinically used Ammonium fluorides, especially ammonium bifluoride in
adhesive ceramic bonding methods in Northern Germany combination with other acids, have been investigated as a
showed, there is still a considerable lack of understanding possible etching media for dental ceramics for many
about the principles of reliable ceramic bonding among den- years.3,12,20 Recently, a single bottle ceramic self-etching
tal practitioners.15 When performed by the dental techni- silane primer Monobond Etch & Prime (MEP, Ivoclar Viva-
cian, the subsequent try-in procedure leads to surface con- dent; Schaan, Liechtenstein) was introduced. It has been
tamination with saliva.22 Saliva contains organic materials claimed that effects of MEP are comparable to those of HF
such as salivary proteins, enzymatic molecules, bacteria and silane treatment.19,26,30,33 However, details regarding
and food debris, and inorganic compounds such as mineral bonding efficacy, surface analysis, and detailed comparison
ions in water.18 Adsorption of salivary proteins to dental with existing cleaning materials after human saliva contam-
materials and tooth surfaces results in a pellicle consisting ination remain unclear.
of free (ie, planktonic) bacteria which develops to a thick- Therefore, the purpose of this study was to investigate the
ness of 10-20 nm within a few minutes.9 The resulting per- efficacy of different ceramic surface cleaning methods after
sistent protein contamination from saliva in particular was saliva contamination on the resin bond strength to lithium
shown to hinder adhesion of the resin cements to ceram- disilicate ceramics. The null hypothesis was that the resin-
ics.7,21 Therefore, several cleaning methods have been pro- ceramic bond strength of the resin cements to the ceramics
posed to eliminate such contamination from the ceramic was not influenced by contamination and cleaning method.
52 The Journal of Adhesive Dentistry
Lyann et al
Table 1 Composition of the materials used in this study
Material Product Composition Batch No.
IPS e.max CAD Ivoclar Vivadent SiO2, Li2O, K2O, Al2O3, P2O5, ZrO2, ZnO, MgO, color oxides U37584
IPS Ceramic Etching Gel Ivoclar Vivadent < 5 % hydrofluoric acid T35311
Total Etch Ivoclar Vivadent Phosphoric acid (37 wt% in water), thickening agent and pigments V20970
Monobond Etch & Prime Ivoclar Vivadent Butanol, trimethoxypropyl methacrylate, tetrabutylammoniun dihydrogen
U20251
trifluoride, methacrylated phosphoric acid ester, colorant
Monobond Plus Ivoclar Vivadent Silane methacrylate, phosphoric acid methacrylate, ethanol and sulfide
T29123
methacrylate
Alloy primer Kuraray Noritake Dental Monomer MDP, triazine-based vinyl monomer, solvent (acetone) C80060
Urethane dimethacrylate and methacrylate monomers
Variolink Esthetic DC Ivoclar Vivadent Ytterbium trifluoride and spheroid mixed oxide V28271
Initiators, stabilizers and pigments
Mixed oxide
Multilink Automix Ivoclar Vivadent Dimethacrylate and HEMA U54978
Barium glass, ytterbium trifluoride and spheroid mixed oxide
Dimethacrylates and acidic monomers
Barium glass, ytterbium trifluoride, co-polymer and highly dispersed
SpeedCEM Ivoclar Vivadent V10538
silicon dioxide
Initiators, stabilizers and pigments (<1%)
Al2O3: aluminum oxide; HEMA, 2-hydroxyethyl methacrylate; K2O: potassium oxide; Li2O: lithium superoxide; MgO: magnesium oxide;
MDP: 10-methacryloyloxydecyl dihydrogen phosphate; P2O5: phosphorus pentoxide; SiO2: silicon dioxide; ZnO, zinc oxide; ZrO2: zirconium oxide.
MATERIALS AND METHODS Then excess saliva was removed by water spraying for 15 s,
followed by air drying for another 15 s.
The materials used in the bonding procedure are listed in Each group was further divided into five subgroups
Table 1. (n = 20, with and without contamination) according to the
surface treatment performed:
Experiment 1: Tensile bond test y Control: no pretreatment.
Specimen fabrication y MP: a thin coat of Monobond Plus (MP; Ivoclar Vivadent)
Lithium disilicate ceramics blocks (e.max CAD, Ivoclar Viva- was applied with a brush and the material allowed to
dent) were used in this study. Specimens (5 mm thick x react for 60 s. Subsequently, any remaining excess was
15 mm wide x 15 mm long) were retrieved from original blocks dispersed with a strong air stream.
using a low-speed diamond saw (IsoMet, Buehler; Lake Bluff, y PA+MP: surfaces were etched with 37% phosphoric acid
IL, USA) and sintered. One surface of each specimen was (PA; Total Etch, Ivoclar Vivadent) for 20 s and then
ground using 600-grit silicon carbide paper under water rinsing. rinsed and dried. After etching, MP was applied as in the
The specimens were ultrasonically cleaned in deionized water MP group.
for 5 min followed by ethanol for 2 min and then air dried. y HF+MP: surfaces were etched with < 5% HF (IPS Ceramic
Etcting Gel, Ivoclar Vivadent) for 20 s and then rinsed and
Surface preparation dried. After etching, MP was applied as in the MP group.
The specimens were left as is or were contaminated with y MEP: MEP was applied, rubbed for 20 s, and left on the
human saliva. To contaminate, the specimens were im- surface for a further 40 s for sufficient reaction. It was
mersed in saliva for 1 min. Saliva was collected from one of subsequently washed off with water and then dried with
the authors who had refrained from eating and drinking air for another 10 s.
1.5 h prior to the collection procedure under a protocol ap-
proved by the Ethics Committee at Tokyo Medical and Den- Tensile bond strength test
tal University (No. D2017-053). All experiments were per- After surface treatment, a 100-μm-thick piece of aluminum
formed using fresh saliva collected on the same occasion. masking tape with a 4-mm diameter hole was placed on
Vol 21, No 1, 2019 53
Lyann et al
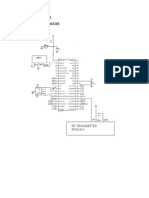
Fig 2 Schematic illustration of specimen
e.max CAD disks preparation methods for surface analysis.
600# SiC paper polishing
Without saliva With saliva contamination
Saliva immersion for
1 min, rinsing with water
spray for 15 s, air drying
Water HF PA ME Water HF PA ME
cleaning cleaning
XPS Analysis
each ceramic surface. A metal rod treated with a metal ad- by the t-test with Bonferroni correction for pairwise compari-
hesive primer (Alloy Primer, Kuraray Noritake; Tokyo, Japan) sons. The two factors analyzed were surface treatments and
was attached to each ceramic block using one of the 3 storage conditions. For all analyses, a confidence level of
resin cements (Ivoclar Vivadent): Variolink Esthetic DC (VE), 95% was assumed. All statistical procedures were performed
Multilink Automix (MA), and SpeedCEM (SC). The resin ce- using SPSS software (SPSS 22, IBM; Chicago, IL, USA).
ment was light cured for 40 s with a curing unit at a light
intensity of 600 mW/cm2 (Optilux 501, Demetron-Kerr; Dan- Experiment 2: Surface Analysis
bury, CT, USA). The cemented specimens were left to com- The surfaces of e.max CAD disks were prepared following
plete polymerization at room temperature for 30 min, then the same procedure as the tensile bond strength test. Each
stored in distilled water at 37°C for 24 h. A total of 300 group was divided into four subgroups (n = 2, with and with-
specimens were produced in 5 surface treatment groups out contamination) according to the surface treatment per-
with 3 resin cements and tested under two conditions: with formed: control, 5% HF, 37% PA, and MEP in Fig 2.
or without saliva contamination (n = 10). Tensile bond X-ray photoelectron spectroscopy (XPS) was used to ana-
strength (TBS) was measured in a universal testing appara- lyze the surfaces of the e.max CAD samples. XPS (JPC-
tus (Autograph-J, Shimadzu; Kyoto, Japan) at a crosshead 9010MC, JEOL; Tokyo, Japan) analyses were performed
speed of 2 mm/min.16 using a Mg Kα x-ray source under the following conditions:
operating pressure, 10−7 Pa; emission current, 10 mA; ac-
Failure mode analysis celerating voltage, 10 kV. Wide scans were measured at
The fractured interfaces of the debonded specimens were pass energies of 100 eV.
examined using a light microscope (OCS 912042, Olympus;
Tokyo, Japan) to calculate the debonded area and assign
failure modes. The failure modes were classified into the RESULTS
following three types: type I: adhesive failure, no resin ce-
ment remnant on the ceramic block; type II: mixed failure, Experiment 1: Tensile Bond Strength Test
fracture comprises both the ceramic block and resin ce- Tables 2 to 4 show tensile bond strength results as well as
ment (some ceramic and some resin cement visible); type failure modes, with or without saliva contamination. The two
III: cohesive failure, fracture within resin cement, fracture surface treatment factors (with or without saliva contamina-
surface consists of only resin cement. Representative sam- tion and surface treatment) and their interactions were sta-
ples were examined in a scanning electron microscope tistically significant for all the cements (p < 0.05). The typi-
(SEM, JSM-5310LV, JEOL; Tokyo, Japan) with an accelera- cal failure modes as observed with SEM are shown in (Fig 3).
tion voltage of 15 KV after sputtering using a conductive
layer of gold to determine the pattern of debonding. Variolink esthetic DC (VE)
In both conditions, HF+MP and MEP resulted in statistically
Statistical analysis significantly higher mean TBS than did the control, MP, and
According to the Shapiro-Wilk test, the data were normally PA+MP (p < 0.05) (Table 2). After saliva contamination,
distributed (p > 0.05). Therefore, TBS data in MPa were ana- there were no statistically significantly differences vs
lyzed separately for each cement by two-way ANOVA, followed groups without saliva. Regarding failure analysis, almost all
54 The Journal of Adhesive Dentistry
Lyann et al
Table 2 Tensile bond strength means and standard deviations in MPa to Variolink Esthetic DC (VE)
Surface treatment Control MP PA+MP HF+MP ME
3.5 ± 1.4abcd 25.6 ± 5.4aef 27.6 ± 4.4bgh 40.6 ± 6.3ceg 37.0 ± 6.6dfh
Without saliva
(10/0/0) (0/0/10) (0/0/10) (0/0/10) (0/0/10)
0.6 ± 0.2abcd 26.5 ± 5.1ae 26.2 ± 6.3bfg 36.7 ± 9.8cef 33.9 ± 5.9dg
Saliva contamination
(10/0/0) (0/2/8) (0/0/10) (0/0/10) (0/0/10)
All groups n = 10. Failure modes: adhesive failure/ mixed failure/ cohesive failure. Same lowercase superscript letters indicate significant differences
between the rows (p < 0.05).
Table 3 Tensile bond strength means and standard deviations in MPa to to Multilink Automix (MA)
Surface treatment Control MP PA+MP HF+MP ME
7.1 ± 0.9abcd 25.1 ± 5.8aA 31.2 ± 6.5b 29.1 ± 5.2c 26.1 ± 3.9d
Without saliva
(10/0/0) (10/0/0) (0/0/10) (4/4/2) (0/0/10)
6.9 ± 2.8abcd 16.8 ± 2.8aefgA 31.5 ± 9.7be 31.4 ± 5.1cf 26.3 ± 7.1dg
Saliva Contamination
(10/0/0) (10/0/0) (0/0/10) (9/0/1) (0/0/10)
All groups n = 10. Failure modes: adhesive failure/ mixed failure/ cohesive failure. Same lowercase superscript letters indicate significant differences
between the rows (p < 0.05). Same uppercase superscript letters indicate significant differences between the columns (p < 0.05).
Table 4 Tensile bond strength means and standard deviations in MPa to SpeedCEM (SC)
Surface treatment Control MP PA+MP HF+MP ME
5.8 ± 1.3abcd 28.2 ± 5.0aA 32.9 ± 8.7b 31.1 ± 5.5c 31.0 ± 4.7d
Without saliva
(10/0/0) (0/0/10) (0/0/10) (0/4/6) (0/0/10)
6.6 ± 3.4abc 13.2 ± 3.6defA 28.7 ± 4.2ad 27.1 ± 7.3be 31.4 ± 6.9cf
Saliva contamination
(10/0/0) (10/0/0) (0/0/10) (7/0/3) (0/0/10)
All groups n = 10. Failure modes: adhesive failure/ mixed failure/ cohesive failure. Same lowercase superscript letters indicate significant differences
between the rows (p < 0.05). Same uppercase superscript letters indicate significant differences between the columns (p < 0.05).
specimens showed cohesive failure, except the control contamination, no significant decrease was observed in
group, both with and without saliva contamination. PA+MP, HF+MP, and MEP (p > 0.05). However, bond
strength in the MP group decreased significantly after saliva
Multilink Automix (MA) contamination (Table 4). Regarding failure mode, MEP and
The control group presented lower bond strength at base- PA+MP resulted in 100% cohesive failure, while more adhe-
line in both conditions (Table 3). Without contamination, sive failures were observed in MP and HF+MP after saliva
MP, PA+MP, HF+MP and MEP showed the highest bond contamination.
strengths. After saliva contamination, MP showed signifi-
cantly lower bond strength than did the other groups Experiment 2: Surface Analysis
(p < 0.05). A higher ratio of cohesive failures was observed The typical wide-scan spectra from XPS analysis are shown
in groups with higher bond strengths. After saliva contami- in Fig 3. Clear N-1s and C-1s peaks were identified by XPS
nation, 100% adhesive failures were noticed after no sur- analysis. After saliva contamination, the intensities of N-1s
face treatment (control), MP, and HF+MP. and C-1s peaks increased. In HF, Zn-2p peaks were de-
tected under both conditions. In HF and PA, there were no
SpeedCEM (SC) N-1s peaks and small C-1s peaks. In MEP, C-1s and F-1s
The control group presented the lowest bond strength at peaks were the specific peaks under both conditions, but
baseline with or without saliva contamination. After saliva there was no N-1s peak after saliva contamination.
Vol 21, No 1, 2019 55
Lyann et al
a b c
LD RC
LD
RC
Fig 3 Representative SEM images (35X) of typical failure modes. A clean ceramic surface was indicative of adhesive failure between
ceramic and cement. Mixed failure showed surfaces with both ceramic and resin cement. Cohesive failure in resin cement was indicated by
resin cement particles attached to the ceramic surface. RC: resin cement; LD: lithium disilicate.
DISCUSSION The specimens bonded without silane primer in the con-
trol group had statistically significantly low TBS compared
Intraoral seating of pre-etched glass ceramics during a try-in to the other groups with or without saliva contamination.
procedure frequently results in salivary contamination, and The use of silane primer, alone or in combination with the
if this contamination is not removed, it may result in de- etchant, is clinically essential for the adhesive bonding of
creased bond strength between the resin cement and the lithium disilicate ceramic. The use of silane without acid
glass-ceramic surface. The null hypothesis was rejected, as etching (MP group) resulted in lower bond strengths in com-
statistically significant differences in the tensile bond parison with the PA+MP or HF+MP or MEP.
strength of resin cement to lithium disilicate ceramic were To avoid the detrimental effect of saliva contamination
found based on the type of surface and cleaning proce- on resin-to-ceramic bond strength, ceramic restorations
dures. Etching or rinsing of the pre-etched glass-ceramic should be etched and silanized after the try-in procedure.27
surface after contamination is necessary to dislodge the Several studies reported that phosphoric acid cleaning was
saliva and allow more effective bonding. The use of surface effective for saliva decontamination,21,35 whereas others
treatments according to the manufacturer’s instructions on reported it to be ineffective.11,31 Acid cleaning requires
an etched, saliva-contaminated lithium disilicate surface be- water rinsing, and the remaining water may inhibit bonding
fore silanization resulted in bond strengths similar to that of efficacy.13 In this study, phosphoric acid cleaning did not
the uncontaminated control group. For those clinicians work as well as HF in VE resin cement; HF resulted in sta-
whose laboratories do not pre-etch the ceramics or who mill tistically significantly higher bond strength (40.6 ± 6.3 MPa)
their lithium disilicate restorations chairside, rinsing the sa- than PA (27.6 ± 4.4 MPa) in VE.
liva-contaminated ceramic after try-in and then etching with Interestingly, in the present study, TBS was comparable
hydrofluoric acid in the operatory is adequate, as it provides when resin cement was bonded to lithium disilicate ceramic
bond strengths similar to the uncontaminated control. using MEP or HF+MP with all resin cements. MEP contains
Saliva consists of organic materials such as salivary pro- trimethoxypropyl methacrylate for silanizarion and polyfluor-
teins, bacteria, and food debris in an aqueous solution. ide for etching. It has been indicated that the bond between
After saliva immersion, salivary protein adsorption occurs silica and fluoride is extremely strong.17 Therefore, a pos-
not only on the tooth surface,2 but also on the restorative sible explanation for the effective bonding of MEP to lithium
materials.5,10 Non-covalent adsorption of salivary proteins disilicate ceramic may be attributed to the chemical affinity
occurred on this surface after the immersion of ceramic between silica in lithium disilicate ceramic and ammonium
into saliva for 60 s. This organic coating could not be re- tri-fluoride in MEP.28
moved by rinsing with tap water for 15 s, as shown by XPS, The bond quality of ceramic restorations should not only
revealing a considerable increase in C and N after saliva be assessed by bond strength measurements. Another im-
immersion and rinsing. portant quality indicator is provided by the analysis of frac-
Cleaning the glass-ceramic surface with only water spray ture modes.6,14,16,25 The failure modes of the experimental
after saliva contamination resulted in significantly lower groups were investigated using a light microscope and
bond strength to lithium disilicate glass ceramic compared SEM. If adhesive failure modes occur more frequently, it
to the uncontaminated control group. All specimens showed can be an indication of lower bond quality. In this study,
low initial bond strengths and debonded spontaneously with adhesive failure modes were observed in specimens which
100% adhesive failure at the ceramic surface. Other clean- were not silanized or only silanized after contamination. Co-
ing procedures led to bond strength that did not differ sta- hesive failures (fractures within the composite resin) fre-
tistically significantly from the uncontaminated groups. quently occurred in MEP. In these cases, the bond strength
56 The Journal of Adhesive Dentistry
Lyann et al
Fig 4 Typical spectra of wide-scan using XPS.
Counts
Counts
1000 800 600 400 200 0 1000 800 600 400 200 0
Binding energy (eV) Binding energy (eV)
between the glass-ceramic surface and the composite resin saliva contamination during the intraoral try-in procedures
could exceed the internal strength of the composite resin. may impair bond strengths, demonstrating the clinical sig-
Consequently, MEP self-etching silane primer of glass ce- nificance of this investigation particularly for minimally inva-
ramic surface after saliva contamination is a simple and sive preparations which rely on retention from adhesive
useful method to increase the quality of the bond. bonding. Adhesive cementation protocols should consider
XPS was performed to identify the contamination and the removal of contamination media as a critical step to im-
efficacy of cleaning methods.32 According to XPS analysis, prove the longevity of bonded restorations. More in vitro
there were no N-1s and small C-1s peaks in the control studies are needed to obtain further information under long-
group. However, after saliva contamination, both N and C term water storage and thermalcycling conditions after sa-
peaks derived from salivary proteins on the lithium disili- liva contamination.
cate surface were detected. In HF group, Zn-2p peaks were
detected both with and without saliva contamination. HF
formed microporosities as the glass matrices were dis- CONCLUSION
solved, leaving ZnO exposed on that treated surface. In HF
and PA groups, N-1s was not detected and the C-1s peak Saliva contamination on the bonded surface of the lithium
was small even with saliva contamination. This shows that disilicate glass ceramics before its cementation should be
these acids were able to remove the contaminated saliva avoided. Treating the surface with phosphoric or hydro-
protein on the lithium disilicate surface. MEP is partly com- fluoric acid in combination with silane coupling agent or the
posed of trimethoxypropyl methacrylate, which leaves a thin use of Monobond Etch & Prime were effective methods for
silane layer to chemically bond to the ceramic after water removing saliva contamination and ensuring proper bonding
rinsing and drying of the treated surface. Although the of the resin cement to the lithium disilicate glass-ceramic
mechanism of action of MEP is not fully clear, EL-Daman- bonding surface.
houry and Gaintantzopoulou8 found fluorine residue on the
treated ceramic surface using energy dispersive x-ray analy-
sis. In this study, C-1s and F-1s were the characteristic ACKNOWLEDGMENTS
peaks in both conditions. However, there was no N-1s peak We would like to thank Ivoclar Vivadent for supplying lithium disilicate
after saliva contamination. The F-1s and C-1s peaks in the disks. This work was supported by the JPSP Grant-in-Aid for Scientific
MEP group were higher than those in the other groups. A Research (C) 17K11701 and the Cooperative Research Program of
small F-1s peak might be the results of remaining ammo- the Institute for Catalysis, Hokkaido University (Grants #16B1004
nium polyfluoride, which mildly etched the lithium disilicate and #17B1007).
surface to achieve the etching pattern. A C-1s peak was
also detected in the saliva contaminated group. However,
these peaks are always accompanied by an N-1s peak. C REFERENCES
peaks in the MEP group, however, lack corresponding N-1s 1. Aboush YE. Removing saliva contamination from porcelain veneers before
bonding. J Prosthet Dent 1998;80:649–653.
peaks both with and without saliva contamination. From 2. Baier RE, Glantz PO. Characterization of oral in vivo films formed on dif-
this point of view, the C-1s peak in the MEP group could be ferent types of solid surfaces. Acta Odontol Scand 1978;36:289–301.
coming from the silane coupling agent on the lithium disili- 3. Bailey LF, Bennett RJ. DICOR® surface treatments for enhanced bonding.
J Dent Res 1988;67:925–931.
cate surface.
4. Borges GA, Sophr AM, De Goes MF, Sobrinho LC, Chan DC. Effect of
Although adhesion between resin cement and etched etching and airborne particle abrasion on the microstructure of different
and silanized glass ceramics is well established, possible dental ceramics. J Prosthet Dent 2003;89:479–488.
Vol 21, No 1, 2019 57
Lyann et al
5. Carlén A, Nikdel K, Wennerberg A, Holmberg K, Olsson J. Surface charac- 24. Özcan M, Allahbeickaraghi A, Dündar M. Possible hazardous effects of
teristics and in vitro biofilm formation on glass ionomer and composite hydrofluoric acid and recommendations for treatment approach: A review.
resin. Biomaterials 2001;22:481–487. Clin Oral Investig 2012;16:15–23.
6. Della Bona A, Anusavice KJ, Mecholsky JJ. Failure analysis of resin com- 25. Quaas AC, Yang B, Kern M. Panavia F 2.0 bonding to contaminated zirco-
posite bonded to ceramic. Dent Mater 2003;19:693–699. nia ceramic after different cleaning procedures. Dent Mater 2007;23:
7. Della Bona A, Northeast SE. Shear bond strength of resin bonded ce- 506–512.
ramic after different try-in procedures. J Dent 1994;22:103–107. 26. Roman-Rodriguez JL, Perez-Barquero JA, Gonzalez-Angulo E, Fons-Font A,
8. El-Damanhoury HM, Gaintantzopoulou MD. Self-etching ceramic primer Bustos-Salvador JL. Bonding to silicate ceramics: Conventional technique
versus hydrofluoric acid etching: Etching efficacy and bonding perfor- compared with a simplified technique. J Clin Exp Dent 2017;9:e384–e386.
mance. J Prosthodont Res 2018;62:75–83. 27. Roulet JF, Söderholm KJ, Longmate J. Effects of treatment and storage
9. Hannig M. Ultrastructural investigation of pellicle morphogenesis at two conditions on ceramic/composite bond strength. J Dent Res 1995;74:
different intraoral sites during a 24-h period. Clin Oral Investig 381–387.
1999;3:88–95. 28. Schaan L, Vivadent® I. Monobond Etch & Prime. Self-etching glass-ce-
10. Hannig M. Transmission electron microscopic study of in vivo pellicle for- ramic primer. Scientific documentation, 2016. http://www.ivoclarviva-
mation on dental restorative materials. Eur J Oral Sci 1997;105:422–433. dent.com/en/bonding-agents-l.
11. Ishii R, Tsujimoto A, Takamizawa T, Tsubota K, Suzuki T, Shimamura Y, Mi- 29. Sfondrini MF, Fraticelli D, Gandini P, Scribante A. Shear bond strength of
yazaki M. Influence of surface treatment of contaminated zirconia on sur- orthodontic brackets and disinclusion buttons: Effect of water and saliva
face free energy and resin cement bonding. Dent Mater J 2015;34:91–97. contamination. Biomed Res Int 2013;2013:180137.
12. Kato H, Matsumura H, Atsuta M. Effect of etching and sandblasting on 30. Siqueira FS, Alessi RS, Cardenas AF, Kose C, Souza Pinto SC, Bandeca
bond strength to sintered porcelain of unfilled resin. J Oral Rehabil 2000; MC, Loguercio AD, Gomes JC. New single-bottle ceramic primer: 6-month
27:103–110. case report and laboratory performance. J Contemp Dent Pract 2016;17:
1033–1039.
13. Kawaguchi A, Matsumoto M, Higashi M, Miura J, Minamino T, Kabetani T,
Takeshige F, Mine A, Yatani H. Bonding effectiveness of self-adhesive and 31. Stawarczyk B, Krawczuk A, Ilie N. Tensile bond strength of resin compos-
conventional-type adhesive resin cements to CAD/CAM resin blocks. Part ite repair in vitro using different surface preparation conditionings to an
2: Effect of ultrasonic and acid cleaning. Dent Mater J 2016;35:29–36. aged CAD/CAM resin nanoceramic. Clin Oral Investig 2015;19:299–308.
14. Kern M, Wegner SM. Bonding to zirconia ceramic: Adhesion methods and 32. Takahashi A, Takagaki T, Wada T, Uo M, Nikaido T, Tagami J. The effect
their durability. Dent Mater 1998;14:64–71. of different cleaning agents on saliva contamination for bonding perfor-
mance of zirconia ceramics. Dent Mater J 2018;37:734–739.
15. Klosa K, Meyer G, Kern M. Clinically used adhesive ceramic bonding meth-
ods: a survey in 2007, 2011, and in 2015. Clin Oral Investig 2016;20: 33. Wille S, Lehmann F, Kern M. Durability of resin bonding to lithium disilicate
1691–1698. and zirconia ceramic using a self-etching primer. J Adhes Dent 2017;19:
491–496.
16. Klosa K, Wolfart S, Lehmann F, Wenz H-J, Kern M. The effect of storage con-
ditions, contamination modes and cleaning procedures on the resin bond 34. Yang B, Lange-Jansen HC, Scharnberg M, Wolfart S, Ludwig K, Adelung
strength to lithium disilicate ceramic. J Adhes Dent 2009;11:127–135. R, Kern M. Influence of saliva contamination on zirconia ceramic bonding.
Dent Mater 2008;24:508–513.
17. Kolasinski KW. Etching of silicon in fluoride solutions. Surf Sci 2009;
603:1904–1911. 35. Yang B, Scharnberg M, Wolfart S, Quaas AC, Ludwig K, Adelung R, Kern
M. Influence of contamination on bonding to zirconia ceramic. J Biomed
18. Lendenmann U, Grogan J, Oppenheim FG. Saliva and dental pellicle-a re-
Mater Res - Part B Appl Biomater 2007;81:283–290.
view. Adv Dent Res 2000;14:22–28.
19. Lyann SK, Takagaki T, Nikaido T, Uo M, Ikeda M, Sadr A, Tagami J. Effect
of different surface treatments on the tensile bond strength to lithium di-
silicate glass ceramics. J Adhes Dent 2018;20:261-268.
20. Morikawa T, Matsumura H, Atsuta M. Bonding of a mica-based castable
ceramic material with a tri-n-butylborane-initiated adhesive resin. J Oral
Rehabil 1996;23:450–455.
21. Nicholls JI. Tensile bond of resin cements to porcelain veneers. J Pros- Clinical relevance: For adhesive cementation of lithium
thet Dent 1988;60:443–447.
22. Nikolaus F, Wolkewitz M, Hahn P. Bond strength of composite resin to
disilicate glass ceramics, the newly developed Mono-
glass ceramic after saliva contamination. Clin Oral Investig 2013;17: bond Etch & Prime can effectively remove saliva contam-
751–755. ination and provide bond strengths comparable to the
23. Oh SC, Dong JK, Lüthy H, Schärer P. Strength and microstructure of IPS
Empress 2 glass-ceramic after different treatments. Int J Prosthodont
combination of hydrofluoric acid with Monobond Plus.
2000;13:468–472.
58 The Journal of Adhesive Dentistry
You might also like
- NonRinse Conditioning-BisharaDocument5 pagesNonRinse Conditioning-Bisharaavanthika krishnarajNo ratings yet
- Ceramic Surface Treatment With A Single-Component Primer: Resin Adhesion To Glass CeramicsDocument7 pagesCeramic Surface Treatment With A Single-Component Primer: Resin Adhesion To Glass CeramicsTatiana ChambaNo ratings yet
- In Uence of Contamination and Cleaning On Bond Strength To Modified ZirconiaDocument10 pagesIn Uence of Contamination and Cleaning On Bond Strength To Modified ZirconiaPradeepa PmNo ratings yet
- Acido Fluorhidrico 2017Document10 pagesAcido Fluorhidrico 2017angienayibeNo ratings yet
- Bond Strength Durability of Self-Adhesive Resin Cements To Zirconia Ceramic: An in Vitro StudyDocument8 pagesBond Strength Durability of Self-Adhesive Resin Cements To Zirconia Ceramic: An in Vitro Studygerson fabian arangoNo ratings yet
- Poulon Quintin2021Document8 pagesPoulon Quintin2021NICOLENo ratings yet
- Active and Passive Application of The Phosphoric Acid On The Bond Strength of Lithium DisilicateDocument5 pagesActive and Passive Application of The Phosphoric Acid On The Bond Strength of Lithium DisilicateluciojordanNo ratings yet
- Chenweravanich 2022 - Bond Durability of A Repaired Resin Composite Using A Universal Adhesive and Different Surface TreatmentsDocument10 pagesChenweravanich 2022 - Bond Durability of A Repaired Resin Composite Using A Universal Adhesive and Different Surface Treatmentsdr.gonzalezcalvinoNo ratings yet
- Kim HJ 2020 - Effects of Silane Treatment On Salivary Protein Contamination During The Bonding of Lithium Disilicate CeramicDocument14 pagesKim HJ 2020 - Effects of Silane Treatment On Salivary Protein Contamination During The Bonding of Lithium Disilicate CeramicPatsawat YodhongNo ratings yet
- Surface Roughness of Orthodontic Band Cements With Different CompositionsDocument5 pagesSurface Roughness of Orthodontic Band Cements With Different CompositionsDha Dina SevofrationNo ratings yet
- Influence of Ambient Air and Different Surface Treatments On The Bonding Performance of A CAD CAM Composite Block. Alghamdi Ali. 2018. J Adhes DentDocument8 pagesInfluence of Ambient Air and Different Surface Treatments On The Bonding Performance of A CAD CAM Composite Block. Alghamdi Ali. 2018. J Adhes DentValeria CrespoNo ratings yet
- Maccoll 1998Document6 pagesMaccoll 1998Andres CarvajalNo ratings yet
- Ultrastructure of The Dentin Adhesive Interface After Acidbase Challenge 2004Document8 pagesUltrastructure of The Dentin Adhesive Interface After Acidbase Challenge 2004Mohamed OudaNo ratings yet
- Joseph 1994Document7 pagesJoseph 1994Setthapong WisarnjarusornNo ratings yet
- Articulo Surface TreatmentrDocument7 pagesArticulo Surface TreatmentrDaniela OliverosNo ratings yet
- 1757 899x2F1/012040Document8 pages1757 899x2F1/012040SahasraNo ratings yet
- OperativeDentistry JuliaPuppinRontaniDocument11 pagesOperativeDentistry JuliaPuppinRontaniAbdo SerboutiNo ratings yet
- 5 JAD Vol. 22 (2) Pp. 175-182 2020Document9 pages5 JAD Vol. 22 (2) Pp. 175-182 2020LucianoNo ratings yet
- Patcas 2015Document12 pagesPatcas 2015antonio dlNo ratings yet
- Clinical Trials With Crystal Growth Conditioning As An Alternative To Acid-Etch Enamel PretreatmentDocument8 pagesClinical Trials With Crystal Growth Conditioning As An Alternative To Acid-Etch Enamel PretreatmentJegan KumarNo ratings yet
- Self-Etch Vs Etch-And - RinseDocument16 pagesSelf-Etch Vs Etch-And - RinseKarla AlanisNo ratings yet
- Cuspal Deflection of Bulk Fill Versus LaDocument7 pagesCuspal Deflection of Bulk Fill Versus LaComarzzoNo ratings yet
- Influence of Etching Protocol and Silane Treatment With A Universal Adhesive On Lithium Disilicate Bond StrengthDocument7 pagesInfluence of Etching Protocol and Silane Treatment With A Universal Adhesive On Lithium Disilicate Bond StrengthCatalina GómezNo ratings yet
- Acta Odontol. Latinoam. Vol.28 No.1 Buenos Aires Abr. 2015Document10 pagesActa Odontol. Latinoam. Vol.28 No.1 Buenos Aires Abr. 2015NolcitoRomeroNo ratings yet
- Surface Properties and Color Stability of Resin-Infiltrated Enamel LesionsDocument10 pagesSurface Properties and Color Stability of Resin-Infiltrated Enamel LesionsElena Pleșca MunteanuNo ratings yet
- Effect of Denture Cleansers On Cobalt-Chromium Alloy Surface: A Simulated Period of 5 Years' UseDocument9 pagesEffect of Denture Cleansers On Cobalt-Chromium Alloy Surface: A Simulated Period of 5 Years' UseAmina Sakly BoussaidNo ratings yet
- Li 2014Document9 pagesLi 2014Omar MorteoNo ratings yet
- 10.1111@jerd.12615Document9 pages10.1111@jerd.12615Mairen RamirezNo ratings yet
- E!ect of Mechanical Surface Pretreatment On Metal Ion ReleaseDocument8 pagesE!ect of Mechanical Surface Pretreatment On Metal Ion Releasehayet debbichNo ratings yet
- Adhesion of Multimode Adhesives To Enamel and Dentin 2017Document9 pagesAdhesion of Multimode Adhesives To Enamel and Dentin 2017Paul AlvarezNo ratings yet
- Xu2009 PDFDocument9 pagesXu2009 PDFMariana Carolayne Almeida ResendeNo ratings yet
- Research ArticleDocument8 pagesResearch ArticleCarlos Rafael Vargas HuaylasNo ratings yet
- Contaminacion Zirconio Con SalivaDocument6 pagesContaminacion Zirconio Con SalivaangienayibeNo ratings yet
- Effect of Hydrofluoric Acid Concentration and Etching Duration On Select Surface Roughness Parameters For ZirconiaDocument7 pagesEffect of Hydrofluoric Acid Concentration and Etching Duration On Select Surface Roughness Parameters For ZirconiaJulio Torres OrtodonciaNo ratings yet
- 6 A03v9n2Document4 pages6 A03v9n2Yayis LondoñoNo ratings yet
- Effect of Different Surface Treatments of Titanium Surfaces On The Shear Bond Strength Between Titanium and Zirconia SurfacesDocument7 pagesEffect of Different Surface Treatments of Titanium Surfaces On The Shear Bond Strength Between Titanium and Zirconia SurfacesRanj KhaznadarNo ratings yet
- 10 3290@j Jad A42929Document9 pages10 3290@j Jad A42929ptoeNo ratings yet
- Evolution of Dentin Bonding Agents: AbstractDocument11 pagesEvolution of Dentin Bonding Agents: AbstractSamuel YeohNo ratings yet
- Cleaning Zirconia Surface Prior To Bonding. A Comparative Study of Different Methods and SolutionsDocument7 pagesCleaning Zirconia Surface Prior To Bonding. A Comparative Study of Different Methods and SolutionsMohamed KhaledNo ratings yet
- Comparison of Finishing and Polishing Systems For Residual Resin Removal After DebondingDocument7 pagesComparison of Finishing and Polishing Systems For Residual Resin Removal After DebondingYayis LondoñoNo ratings yet
- Effects of Thermocycling On The Tensile Bond Strength Between Resin Cement and Dentin Surfaces After Temporary Cement ApplicationDocument7 pagesEffects of Thermocycling On The Tensile Bond Strength Between Resin Cement and Dentin Surfaces After Temporary Cement Applicationjinny1_0No ratings yet
- In Vitro Evaluation of Push-Out Bond Strengths of Various Luting Agents To Tooth-Colored PostsDocument9 pagesIn Vitro Evaluation of Push-Out Bond Strengths of Various Luting Agents To Tooth-Colored PostsDidar Sadiq KwekhaNo ratings yet
- Effect of Resin Coating and Chlorhexidine On Microleakage of Two Resin Cements After StorageDocument10 pagesEffect of Resin Coating and Chlorhexidine On Microleakage of Two Resin Cements After StorageHisham HameedNo ratings yet
- Pineda Vasquez2019Document6 pagesPineda Vasquez2019Andres CarvajalNo ratings yet
- ABRZ Sato 2011Document9 pagesABRZ Sato 2011Carlos VivasNo ratings yet
- Mahmoodi 2015Document7 pagesMahmoodi 2015Pokemon Do GuetoNo ratings yet
- Remineralization Across The Resin-Dentin Interface: in Vivo Evaiuation Witli Nanoindentation Measurements, EDS, and SEMDocument11 pagesRemineralization Across The Resin-Dentin Interface: in Vivo Evaiuation Witli Nanoindentation Measurements, EDS, and SEMBAHAMON TRUJILLO MAYRA ALEJANDRANo ratings yet
- Bond Streng Manuel ToledanoDocument8 pagesBond Streng Manuel ToledanoLaura LealNo ratings yet
- 23 PDFDocument6 pages23 PDFSanjeev AthiberanNo ratings yet
- Push-Out Bond Strength of CPP-ACP-modified Calcium Silicate-Based CementsDocument5 pagesPush-Out Bond Strength of CPP-ACP-modified Calcium Silicate-Based CementsHatra MulyonoNo ratings yet
- Influence of Etching Mode On Bonding Performance oDocument8 pagesInfluence of Etching Mode On Bonding Performance oJose Manuel Quintero RomeroNo ratings yet
- Self-Etching Ceramic Primer Versus Hydrofluoric Acid Etching Etching Efficacy and Bonding PerformanceDocument9 pagesSelf-Etching Ceramic Primer Versus Hydrofluoric Acid Etching Etching Efficacy and Bonding PerformanceTatiana ChambaNo ratings yet
- Wang 2011Document6 pagesWang 2011SelenaNo ratings yet
- Adhesion and Dentin Bonding AgentsDocument50 pagesAdhesion and Dentin Bonding AgentsFatema86100% (2)
- 10 1016@j Prosdent 2018 12 018Document8 pages10 1016@j Prosdent 2018 12 018anonimoNo ratings yet
- In Vitro Effect of Cavity Disinfectants On The Bond Strength ofDocument6 pagesIn Vitro Effect of Cavity Disinfectants On The Bond Strength ofJorge Alberto Hernández MenjívarNo ratings yet
- Comparison of The Shear Bond Strength of A Light-Cured Glass Ionomer and A Chemically Cured Glass Ionomer For Use As An Orthodontic Bonding AgentDocument7 pagesComparison of The Shear Bond Strength of A Light-Cured Glass Ionomer and A Chemically Cured Glass Ionomer For Use As An Orthodontic Bonding Agentyina montoyaNo ratings yet
- 10 3290@j Jad A41923Document10 pages10 3290@j Jad A41923Carmen AdamesNo ratings yet
- RetrieveDocument11 pagesRetrieveDracoNo ratings yet
- Bouillaguet 2003Document7 pagesBouillaguet 2003valperlunNo ratings yet
- He 2007Document6 pagesHe 2007valperlunNo ratings yet
- Tay 2005 Geometria Conducto y AdhesionDocument6 pagesTay 2005 Geometria Conducto y AdhesionvalperlunNo ratings yet
- Opdam 1998Document6 pagesOpdam 1998valperlunNo ratings yet
- Proenca 2007Document7 pagesProenca 2007valperlunNo ratings yet
- Cohen Rudo 2011Document5 pagesCohen Rudo 2011valperlunNo ratings yet
- DM 441b Tisch MultimeterDocument38 pagesDM 441b Tisch MultimeterFebriansyah IndratnoNo ratings yet
- Service Manual: DSC-S980Document15 pagesService Manual: DSC-S980pasantitoNo ratings yet
- The Diy Free Energy Generator Using DC MotorDocument21 pagesThe Diy Free Energy Generator Using DC MotorNizel vista100% (1)
- Mother Dairy FinalDocument21 pagesMother Dairy FinalVishal Vilas Shete100% (1)
- An Improved Canny Edge Detection Algorithm Based On Type-2 Fuzzy SetsDocument5 pagesAn Improved Canny Edge Detection Algorithm Based On Type-2 Fuzzy SetsAbrhamNo ratings yet
- TDS - KB4302 (May 2021)Document3 pagesTDS - KB4302 (May 2021)Atham MuhajirNo ratings yet
- Citroen EdcDocument155 pagesCitroen EdcMiguel Chacon100% (1)
- Cat 980H Wheel Loader: Fuel BurnDocument2 pagesCat 980H Wheel Loader: Fuel BurnMohamed Badian TraoreNo ratings yet
- 8D Template Hussey Schnaider FormatDocument37 pages8D Template Hussey Schnaider FormatJuan Carlos Lekuona-Muñoz CarrilloNo ratings yet
- Deduplication GuideDocument122 pagesDeduplication GuidejlvinasNo ratings yet
- Design Guide CompactorDocument24 pagesDesign Guide Compactormaverik29No ratings yet
- Tutorial 9 EMIIDocument1 pageTutorial 9 EMIIThangam MaheshNo ratings yet
- Fpga Implementation of Ofdm Transceiver For A 60Ghz Wireless Mobile Radio SystemDocument5 pagesFpga Implementation of Ofdm Transceiver For A 60Ghz Wireless Mobile Radio SystemBoualem ZouggariNo ratings yet
- Tutorial 5Document4 pagesTutorial 5Kumar ShivamNo ratings yet
- Design and Analysis Using AutocadDocument9 pagesDesign and Analysis Using AutocadsudhakarNo ratings yet
- Timber AssignDocument17 pagesTimber AssignRashid AliNo ratings yet
- Service Station Manual: SMT RCRDocument118 pagesService Station Manual: SMT RCRRudolf PaalNo ratings yet
- Metrology in Chemistry - A Public Task: Gunther DubeDocument5 pagesMetrology in Chemistry - A Public Task: Gunther DuberubenNo ratings yet
- 19xr 6ssDocument206 pages19xr 6ssLouie Dupaya100% (1)
- Hitachi Supria 16 or 32 SliceDocument16 pagesHitachi Supria 16 or 32 SliceVishnu00490% (1)
- C Language Interview QuestionsDocument38 pagesC Language Interview QuestionsMd Suhas100% (1)
- ManualDocument322 pagesManualLê Minh Nguyên TriềuNo ratings yet
- THE AND Office Companion: Reliable CompactDocument4 pagesTHE AND Office Companion: Reliable CompactYaser HamdyNo ratings yet
- Catalogue IN 1016 v3 Min PDFDocument282 pagesCatalogue IN 1016 v3 Min PDFRajendra ChoudhuryNo ratings yet
- BS 12385-1 Wire Rope SlingsDocument22 pagesBS 12385-1 Wire Rope SlingsWalid BdeirNo ratings yet
- 2016 Modelx LHD Sop3Document73 pages2016 Modelx LHD Sop3luisxdNo ratings yet
- Oil and Gas Field Development, Principles andDocument17 pagesOil and Gas Field Development, Principles andAnonymous p6pNOLu67067% (3)
- Circuit Diagram Wireless TransmitterDocument17 pagesCircuit Diagram Wireless Transmitterumaiya1990100% (2)
- Pavel BedrikovetskyDocument1 pagePavel BedrikovetskyMehdi AlizadehNo ratings yet
- Liebert PDX Technical Manual Eng PDFDocument150 pagesLiebert PDX Technical Manual Eng PDFJelena PerićNo ratings yet