Professional Documents
Culture Documents
CNS Micro Impulse
Uploaded by
dineshvd75Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CNS Micro Impulse
Uploaded by
dineshvd75Copyright:
Available Formats
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Section 9: Central Nervous System Infections
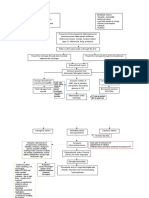
Infective Syndromes of Central Nervous System
ESSAY
(Nil)
SHORT ESSAYS
(Nil)
CNS
SHORT ANSWERS
(Nil)
OBJECTIVE TYPE QUESTIONS
(July 2022)
1. A CSF sample, collected in the ward by lumbar puncture, does not reach the laboratory
for processing for bacterial culture. Discuss the correct decision and the appropriate
action to be taken.
Ans:
CSF should never be refrigerated as delicate pathogens such as H. influenzae, pneumococci or
meningococci may die
If a delay is expected, it may be kept in an incubator at 37°C
(July 2023)
2. A CSF sample was received in microbiology lab for culture. The label in the specimen
container was not matching with the specimen referral form. How will you manage the
situation
Ans: Ask to Resend the sample properly.
01 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Bacterial Meningitis
Bacterial Meningi�s
ESSAY
ESSAY
(February 2020)
1. A 4 years old child presented with history of fever, neck rigidity and altered sensorium for the
last 48 hours. He was admi�ed in the hospital for evalua�on. CSF was collected and examined for
cell morphology, protein, and sugar. Answer the following.
a) What is the probable diagnosis ?
b) Name the bacterial e�ologic agents causing this condi�on
CNS
c) How will you proceed with lab diagnosis?
d) What are the virulence factors associated with this and describe the pathogenesis ?
e) What measures can you take to preven�on this condi�on?
Ans:
a) What is the probable diagnosis?
Acute Meningi�s can be due to bacterial, viral, tubercular in origin
b) Name the bacterial e�ologic agents causing this condi�on
Streptococcus pneumoniae
Neisseria meningi�dis
Streptococcus agalac�ae
Haemophilus influenzae
Listeria monocytogenes
Escherichia coli
Klebsiella
Pseudomonas
Acinetobacter
c) How will you proceed with lab diagnosis?
Laboratory diagnosis
CSF collec�on:
CSF is obtained by lumbar puncture under strict asep�c precau�ons.
Divided into 3 sterile containers :
Cell count.
Biochemical analysis
Bacteriological examina�on
Transport : for culture, the sample should never be refrigerated.
CSF analysis
Characteris�cs Normal Individual Pyogenic Tuberculous Viral meningi�s
meningi�s/bacterial meningi�s
meningi�s
CSF pressure Normal (50 - 150) Highly elevated Moderately Slightly
elevated elevated/Normal
Total WBC 0-5 100-1000 10-500 25-500
count (/mm3)
Predominant Lymphocytes Neutrophils Lymphocytes Lymphocytes
cell type
Glucose (%mg) 40-70 < 40 20-40 Normal
Protein 15-45 >45 100-500 20-80
02 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
*In suspected acute pyogenic meningi�s, CSF shows leukocytosis (except in listeria, where
lymphocytes increase predominantly), total protein content is elevated pressure is highly elevated.
CSF microscopy
Gram staining of heaped smear is done to appreciate the morphology of bacteria causing
meningi�s.
Streptococcus pneumoniae – gram posi�ve, flame shaped diplococci.
Neisseria menigni�dis – gram nega�ve diplococci, capsulated with adjacent sides fla�ened.
CNS
Haemophilus influenzae - Pleomorphic gram-nega�ve capsulated coccobacilli
Escherichia Coli- gram nega�ve bacilli arranged singly.
Listeria monocytogenes – Gram posi�ve short bacilli, o�en confused with diptheroids.
Direct an�gen detec�on
From CSF – a�er centrifuga�on of CSF, supernatant can be used for an�gen detec�on. Latex
agglu�na�on test is performed using latex beads coated with an�-capsular an�bodies.
From urine – an�gen detec�on in urine is useful for pneumococcal an�gens.
Culture
Blood culture - blood agar, chocolate agar , MacConkey agar,
Use BHI broth or automated blood culture bo�les
Iden�fica�on
Biochemical reac�ons, MALDI-TOF,VITEK
An�microbial suscep�bility test
Disk diffusion method / MIC based methods – VITEK
d) What are the virulence factors associated with this and describe the pathogenesis
Virulence factors
Capsular Polysaccharide-
Outer membrane proteins - porin proteins
LPS and endotoxin - induces the release of various inflammatory mediators
IgA proteases
Transferrin binding proteins
Adhesins
03 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Pathogenesis
Nasopharyngeal carriers
Droplet inhala�on
Entry through the nasopharynx
CNS
Reach the meninges via i)Hematogenous route
ii)Cribriform
iii)Plate conjunc�va.
Release of various inflammatory mediators
Damage the vascular endothelium
Fever
Vomi�ng
Headache
Neck s�ffness
Non-blanching rash
Loss of fluid and shock
Intravascular thrombosis
DIC
Myocardial dysfunc�on
e) What measures can you take to preven�on this condi�on?
Chemoprophylaxis Vaccine Prophylaxis
Ce�riaxone (single dose, IM) Meningococcal polysaccharide vaccines
Rifampicin - Bivalent(A,C)/ quadrivalent
Ciprofloxacin (A,C,Y,W135)
Close contacts of primary cases, regardless of Two doses, 3 months apart to children of 3–
their vaccina�on status 18 months of age
Single dose to older children or adult
for high-risk people
MenB Vaccine
Two doses - IM route 1 month apart
For 16–25 years age
(February 2022)
2. A 5-year-old girl was brought in by her mother with the symptoms of fever, vomi�ng (7-8
episodes) and altered sensorium for the last 24 h. Central nervous system examina�on
showed that she was drowsy, had signs of meningeal irrita�on, neck rigidity.
Examina�on of CSF showed neutrophilic predominance.
(a) What is the clinical diagnosis?
(b) Name SIX common probable causes of this clinical condi�on.
(c) Name two rapid tests to detect these causes.
(d) What are the confirmatory tests that can be done in the laboratory?
04 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(e) Name the an�microbial given empirically for this condi�on
(f) Give details of vaccines available for these microbial agents
(g) Name two other drugs which can be used for trea�ng this condi�on
Ans:
(a) What is the clinical diagnosis?
Acute bacterial meningi�s
CNS
(b) Name SIX common probable causes of this clinical condi�on.
Streptococcus pneumoniae
Neisseria meningi�dis
Streptococcus agalac�ae
Haemophilus influenzae
Listeria monocytogenes
Escherichia coli
Klebsiella
Pseudomonas
Acinetobacter
(c) Name two rapid tests to detect these causes.
Direct An�gen Detec�on
Molecular methods
(d) What are the confirmatory tests that can be done in the laboratory?
Laboratory diagnosis
CSF collec�on:
CSF is obtained by lumbar puncture under strict asep�c precau�ons.
Divided into 3 sterile containers : Cell count
Biochemical analysis
Bacteriological examina�on
Transport : for culture, the sample should never be refrigerated.
CSF analysis
Characteris�cs Normal Individual Pyogenic Tuberculous Viral meningi�s
meningi�s/bacterial meningi�s
meningi�s
CSF pressure Normal (50 - 150) Highly elevated Moderately Slightly
elevated elevated/Normal
Total WBC count 0-5 100-1000 10-500 25-500
(/mm3)
Predominant Lymphocytes Neutrophils Lymphocytes Lymphocytes
cell type
Glucose (%mg) 40-70 < 40 20-40 Normal
Protein 15-45 >45 100-500 20-80
*In suspected acute pyogenic meningi�s, CSF shows leukocytosis (except in listeria, where
lymphocytes increase predominantly), total protein content is elevated pressure is highly elevated.
05 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
CSF microscopy
Gram staining of heaped smear is done to appreciate the morphology of bacteria causing
meningi�s.
Streptococcus pneumoniae – gram posi�ve, flame shaped diplococci.
Neisseria menigni�dis – gram nega�ve diplococci, capsulated with adjacent sides fla�ened.
Haemophilus influenzae - Pleomorphic gram-nega�ve capsulated coccobacilli
Escherichia Coli- gram nega�ve bacilli arranged singly.
Listeria monocytogenes – Gram posi�ve short bacilli, o�en confused with diptheroids.
CNS
Direct an�gen detec�on
From CSF – a�er centrifuga�on of CSF, supernatant can be used for an�gen detec�on. Latex
agglu�na�on test is performed using latex beads coated with an�-capsular an�bodies.
From urine – an�gen detec�on in urine is useful for pneumococcal an�gens.
Culture
Blood culture - blood agar, chocolate agar, MacConkey agar,
Use BHI broth or automated blood culture bo�les
Iden�fica�on
Biochemical reac�ons, MALDI-TOF,VITEK
An�microbial suscep�bility test
Disk diffusion method / MIC based methods – VITEK
(e) Name the an�microbial given empirically for this condi�on
IV cefotaxime / ce�riaxone + vancomycin
If Listeria is suspected - IV ampicillin
+ IV dexamethasone
(f) Give details of vaccines available for these microbial agents
Polysaccharide Quadrivalent conjugate MenB Vaccine
0.5 mL 0.5 mL Recombinant vaccine
subcutaneous or IM IM Anterolateral thigh or Group B meningococcus
Anterolateral thigh or upper upper arm Adhesin A, heparin binding
arm IAP schedule :- an�gen, factor H binding
IAP schedule :- High-risk categories; >2 years protein and outer membrane
High-risk categories; >2-year- old: One dose 9-23 months old vesicles (OMV)
old (>3 months old in (in USA, not licensed in India: Two doses, given IM route 1
outbreaks): One dose; repeat Two doses 3 months apart) month apart
a�er 3-5 years, A/E:- 16–25 years age.
if required Local pain, swelling or redness;
A/E:- Guillain-Barre syndrome (rare)
Fever, local pain or redness C/I :-
C/I :- May interfere with
Anaphylaxis a�er previous pneumococcal vaccine;
dose separate administra�on by 4
Usage :- 2-8°C - protect from weeks
light Usage :-2 - 8° C - not freeze
Use within 30 minutes of NIS :- Not included
recons�tu�on
NIS :- Not included
06 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(g) Name two other drugs which can be used for trea�ng this condi�on
Rifampicin , Ciprofloxacin
Penicillin , Ampicillin , Amoxicillin
CNS
07 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT ESSAYS
SHORT ESSAYS
(May 2021)
1. Laboratory diagnosis of bacterial meningi�s
Ans:
Laboratory diagnosis
CSF collec�on:
CSF is obtained by lumbar puncture under strict asep�c precau�ons.
Divided into 3 sterile containers: Cell count.
CNS
Biochemical analysis
Bacteriological examina�on
Transport: for culture, the sample should never be refrigerated.
CSF analysis
Characteris�cs Normal Individual Pyogenic Tuberculous Viral meningi�s
meningi�s/bacterial meningi�s
meningi�s
CSF pressure Normal (50 - 150) Highly elevated Moderately Slightly
elevated elevated/Normal
Total WBC 0-5 100-1000 10-500 25-500
count (/mm3)
Predominant Lymphocytes Neutrophils Lymphocytes Lymphocytes
cell type
Glucose (%mg) 40-70 < 40 20-40 Normal
Protein 15-45 >45 100-500 20-80
*In suspected acute pyogenic meningi�s, CSF shows leukocytosis (except in listeria, where
lymphocytes increase predominantly), total protein content is elevated pressure is highly elevated.
CSF Microscopy
Gram staining of heaped smear is done to appreciate the morphology of bacteria causing
meningi�s.
Streptococcus pneumoniae – gram posi�ve, flame shaped diplococci.
Neisseria menigni�dis – gram nega�ve diplococci, capsulated with adjacent sides fla�ened.
Haemophilus influenzae - Pleomorphic gram-nega�ve capsulated coccobacilli
Escherichia Coli- gram nega�ve bacilli arranged singly.
Listeria monocytogenes – Gram posi�ve short bacilli, o�en confused with diptheroids.
Direct an�gen detec�on
From CSF – a�er centrifuga�on of CSF, supernatant can be used for an�gen detec�on. Latex
agglu�na�on test is performed using latex beads coated with an�-capsular an�bodies.
From urine – an�gen detec�on in urine is useful for pneumococcal an�gens.
Culture
Blood culture - blood agar, chocolate agar, MacConkey agar,
Use BHI broth or automated blood culture bo�les
Iden�fica�on
Biochemical reac�ons, MALDI-TOF,VITEK
An�microbial suscep�bility test
Disk diffusion method / MIC based methods – VITEK
08 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORTANSWERS
SHORT ANSWERS
(September 2013)
1. Listeria monocytogenes
Food borne pathogen.
Serious infec�ons par�cularly in neonates, pregnant women, and elderly people
Due to its ability to survive refrigera�on, it is commonly found in stored foods.
CNS
Macrophage phagocytosis causing host cell polymeriza�on and further migrates to the adjacent
epithelial cells by direct cell to cell spread.
It mainly causes meningi�s in extremes of ages, febrile gastroenteri�s, Immunosuppression.
Neonates, Elderly, and pregnant women are prone to develop listeriosis.
Mo�lity: tumbling mo�lity - 25°C nonmo�le - 37°C differen�al mo�lity - temperature
dependent flagella expression
Culture: It grows on blood agar (β-haemoly�c colonies), and chocolate agar.
Selec�ve media such as PALCAM agar (containing mixture of an�bio�cs) - for isola�on
(May 2022)
2. Name four causa�ve agents of neonatal meningi�s
Escherichia Coli
Streptococcus agalac�ae
Klebsiella
Listeria monocytogenes
OBJECTIVE TYPE QUESTIONS
(July 2022)
1. Enumerate two bacteria causing neonatal meningi�s
Streptococcus agalac�ae
Escherichia coli
Klebsiella
Listeria monocytogenes
09 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
TETANUS
TETANUS
ESSAY
ESSAY
(Nil)
SHORT
SHORTESSAYS
ESSAYS
(Nil)
SHORT
SHORTANSWERS
ANSWERS
(April 2013)
1. Prophylaxis of tetanus
CNS
Most effec�ve method is Ac�ve immuniza�on/Tetanus Vaccina�on
Tetanus Toxoid: prepared by incuba�ng toxin with formalin to become toxoid and then
adsorbed onto alum.
DPT vaccine consists of diphtheria toxoid, pertussis whole cell killed prepara�on and tetanus
toxoid.
Td vaccine: tetanus toxoid and adult diphtheria toxoid
Pentavalent vaccine: DPT, Hepa��s B and Hib
NIS of India - Total 7 doses are given.3 doses of pentavalent vaccine at 6,10,14 weeks
following birth.2 booster doses of DPT at 16-24 months and 5 years then 2 addi�onal doses
of Td at 10 years and 16 years.
10 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
VIRAL MENINGITIS AND MYELITIS
VIRAL MENINGITIS AND MYELITIS
ESSAY
ESSAY
(March 2014)
1. A one year old child presented with history of inability to move limbs associated with neck
s�ffness following a bout of fever Immuniza�on history was not available. O/E the child has flaccid
paralysis.
a) What is the probable clinical diagnosis and name the ae�ological agent?
CNS
b) Describe the pathogenesis of the disease?
c) How is it diagnosed in the lab and men�on the prophylaxis available?
Ans:
a) What is the probable clinical diagnosis and name the ae�ological agent?
Poliomyeli�s ; Ae�ological agent: Poliovirus
b) Describe the pathogenesis of the disease?
Pathogenesis:
Virus enters body via Faeco-oral route, respiratory droplets, conjunc�val contact
Virus enters the host cells by binding to CD155 receptors present on the host cell
Mul�plies locally in the intes�nal epithelial cells, submucosal lymphoid �ssue, tonsils, and other
lymphoid �ssue
Virus then spreads to CNS/Spinal cord through hematogenous or neural routes
Final target site for poliovirus – anterior horn cells of spinal cord
This leads to muscle weakening and paralysis
Virus infected neurons undergo degenera�on
c) How is it diagnosed in the lab and men�on the prophylaxis available?
1. Virus isola�on
Specimen:
Poliovirus may be recovered from throat swabs ( up to 3 weeks of illness )
From rectal swabs or stool samples ( up to 12 weeks of illness )
Transport :
Specimens should be kept frozen during transport to laboratory
Cell line:
Primary monkey kidney cell lines: most recommended cell lines
Iden�fica�on of growth of polio virus
Cytopathological effects – Crena�on and degenera�on of en�re cell sheet
An�gen detec�on – Neutraliza�on with the specific an�serum / by immunofluorescence test
2. An�body detec�on - Neutraliza�on test
3. Molecular method – Real-�me mul�plex reverse-transcriptase PCR
11 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Prophylaxis:
CNS
12 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT ESSAYS
SHORT ESSAYS
(September 2015, February 2016)
1. Prophylaxis of poliomyeli�s
Oral Polio Vaccine (OPV) : The primary method for prophylaxis against poliomyeli�s is the
administra�on of the oral polio vaccine. This vaccine contains weakened (a�enuated) forms of
the three types of polioviruses (type 1, type 2, and type 3). It is typically given to children in
mul�ple doses, star�ng at an early age, to provide immunity. The OPV is easy to administer,
CNS
cost-effec�ve, and highly effec�ve in preven�ng polio.
Rou�ne Immuniza�on : Rou�ne immuniza�on schedules in many countries include several
doses of the oral polio vaccine, o�en given at 2, 4, and 6 months of age, with booster doses at
later ages. This ensures that children develop strong immunity to polio.
Inac�vated Polio Vaccine (IPV) : In some regions, the inac�vated polio vaccine is used in
addi�on to or in place of OPV. IPV contains inac�vated (killed) poliovirus and is administered
via injec�on. It is commonly used in countries where there is a low risk of wild poliovirus
transmission or in post-eradica�on phases.
Na�onal and Global Immuniza�on Campaigns : Governments and interna�onal organiza�ons
conduct mass vaccina�on campaigns, known as Na�onal Immuniza�on Days (NIDs) or
Supplementary Immuniza�on Ac�vi�es (SIAs), to reach children who may have missed rou�ne
vaccina�ons. These campaigns are especially important in areas where polio is s�ll endemic or
where there is a risk of outbreaks.
Travel Vaccina�on : Individuals traveling to or from regions where polio is s�ll present should
ensure they are adequately vaccinated before travel.
Surveillance and Response : In addi�on to vaccina�on, an essen�al aspect of polio
prophylaxis is surveillance for poten�al cases. Rapid detec�on and response to any suspected
cases-ACUTE FLACCID PARALYSIS, are cri�cal for preven�ng the spread of the virus and
facilita�ng a coordinated public health response.(Acute flaccid paralysis)
Global Polio Eradica�on Ini�a�ve : The Global Polio Eradica�on Ini�a�ve (GPEI) is a
comprehensive effort led by organiza�ons like the World Health Organiza�on (WHO), UNICEF,
and Rotary Interna�onal to eradicate polio worldwide. This ini�a�ve involves mass vaccina�on
campaigns, surveillance, and research to ensure that the poliovirus is eliminated from every
corner of the globe.
13 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
CNS
(July 2022)
2. Pathogenesis and laboratory diagnosis of polio
Pathogenesis:
Virus enters body via Faeco-oral route, respiratory droplets, conjunc�val contact
Virus enters the host cells by binding to CD155 receptors present on the host cell
Mul�plies locally in the intes�nal epithelial cells, submucosal lymphoid �ssue, tonsils, and other
lymphoid �ssue
Virus then spreads to CNS/Spinal cord through hematogenous or neural routes
Final target site for poliovirus – anterior horn cells of spinal cord
This leads to muscle weakening and paralysis
Virus infected neurons undergo degenera�on
Laboratory diagnosis:
1. Virus isola�on
Specimen:
Poliovirus may be recovered from throat swabs ( up to 3 weeks of illness )
From rectal swabs or stool samples ( up to 12 weeks of illness )
Transport :
Specimens should be kept frozen during transport to laboratory
Cell line:
Primary monkey kidney cell lines: most recommended cell lines
14 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Iden�fica�on of growth of polio virus
Cytopathological effects – Crena�on and degenera�on of en�re cell sheet
An�gen detec�on – Neutraliza�on with the specific an�serum / by immunofluorescence test
2. An�body detec�on - Neutraliza�on test
3. Molecular method – Real-�me mul�plex reverse-transcriptase PCR
(July 2023)
3. Describe the pathogenesis, laboratory diagnosis and prophylaxis of Polio myeli�s
CNS
Ans:
Pathogenesis
Virus enters body via Faeco-oral route, respiratory droplets, conjunc�val contact
Virus enters the host cells by binding to CD155 receptors present on the host cell
Mul�plies locally in the intes�nal epithelial cells, submucosal lymphoid �ssue, tonsils, and other
lymphoid �ssue
Virus then spreads to CNS/Spinal cord through hematogenous or neural routes
Final target site for poliovirus – anterior horn cells of spinal cord
This leads to muscle weakening and paralysis
Virus infected neurons undergo degenera�on
Laboratory diagnosis
1. Virus isola�on
Specimen:
Poliovirus may be recovered from throat swabs ( up to 3 weeks of illness )
From rectal swabs or stool samples ( up to 12 weeks of illness )
Transport :
Specimens should be kept frozen during transport to laboratory
Cell line:
Primary monkey kidney cell lines: most recommended cell lines
Iden�fica�on of growth of polio virus
Cytopathological effects – Crena�on and degenera�on of en�re cell sheet
An�gen detec�on – Neutraliza�on with the specific an�serum / by immunofluorescence test
2. An�body detec�on - Neutraliza�on test
3. Molecular method – Real-�me mul�plex reverse-transcriptase PCR
15 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Prophylaxis of Poliomyeli�s
CNS
16 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT ANSWERS
SHORT ANSWERS
(February 2017)
1. Asep�c meningi�s
Viral meningi�s
Inflamma�on of the meninges
Generally, less severe
E�ology
CNS
Enteroviruses – Coxsackieviruses, echoviruses, parechoviruses and Enterovirus 71.
Herpesviruses - HSV , VZV , EBV
Arboviruses - West Nile virus, Saint Louis encephali�s virus, Powassan virus, California
encephali�s virus , Colorado �ck fever virus
LCM virus - Lymphocy�c choriomeningi�s virus
Mumps virus
Measles virus
Influenza virus
Human immunodeficiency virus
Clinical Features
Fever
Headache
S�ff neck
Photophobia,
Sleepiness or
Trouble in waking up from sleep,
Nausea
Irritability,
Vomi�ng,
Lack of appe�te
Lethargy
Laboratory Diagnosis
CSF Analysis (Cytological and Biochemical)
Molecular Methods - Mul�plex PCR , mul�plex real-�me PCR , BioFire Film Array
Viral Culture
An�body Detec�on
Oligoclonal Gamma Globulin Bands
Treatment
Primarily symptoma�c - analgesics, an�pyre�cs, an�eme�cs and fluid and electrolyte
replacement
Oral or intravenous acyclovir
highly ac�ve an�retroviral therapy – if HIV
17 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(February 2019)
2. List 2 important differences between live and killed polio virus vaccines
LIVE POLIO VIRUS VACCINE KILLED POLIO VIRUS VACCINE
Oral Sabin Injectable Salk (intradermal route)
Total 5 doses, zero dose at birth,1st, 2nd, and 3rd Total 2 frac�onal doses
dose given at 6th,10th and 14th weeks of age, Given at 6th and 14th weeks
booster given at 16-24 months
CNS
Economical Expensive
Paralysis and intes�nal re infec�on, more chance Zero chance of VAPP
of VAPP and VDPV
(July 2019)
3. Vaccines used to prevent poliomyeli�s with immuniza�on schedule
Ans:
Vaccine When to give Maximum age Dose Dilu�on Route Site
OPV – 0 At birth or as Within first 15 2 drops No Oral Oral
(Sabin) early as days
possible
OPV 1,2,3 At 6 weeks, 10 5 years of age 2 drops No Oral Oral
(Sabin) weeks, and 14
weeks
IPV Two frac�onal 1 year of age 0.1 mL No Intradermal Right
(Salk) doses at 6 and upper arm
14 weeks of age
(February 2020)
4. Pulse polio programme
Ans:
The Pulse Polio Programme is a vital public health campaign in the fight against polio, as it helps
maintain immunity levels in the popula�on and contributes to the eventual eradica�on of the
disease.
Immuniza�on Drive: A na�onwide or region-specific immuniza�on campaign aimed at
vaccina�ng children under the age of five against polio virus.
Intensive Vaccina�on Rounds: The program conducts periodic vaccina�on rounds, o�en
referred to as "pulse" rounds, during which health workers visit communi�es, schools, and
public spaces to administer the oral polio vaccine (OPV).
Polio Eradica�on Goal: The primary objec�ve of the Pulse Polio Programme is to achieve the
complete eradica�on of wild poliovirus, which has been largely successful in India.
Public Awareness: The ini�a�ve involves extensive public awareness and mobiliza�on efforts to
ensure that all eligible children receive the polio vaccine, thereby contribu�ng to the global
effort to eradicate polio.
OBJECTIVE TYPE QUESTIONS
(Nil)
18 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
VIRAL ENCEPHALITIS & ENCEPHALOPATHY
VIRAL ENCEPHALITIS & ENCEPHALOPATHY
ESSAY
ESSAY
(February 2016)
1. A 27 year old male was admi�ed in the intensive medical care unit with drooling of saliva and
fear of intake of liquids since morning. There was history of dog bite on his right leg for 10 days
back.
a) What is the provisional diagnosis?
b) Discuss briefly about the pathogenesis of the above clinical condi�on?
CNS
c) Describe the laboratory inves�ga�ons to confirm the diagnosis.
d) Explain the prophylaxis of the condi�on
Ans:
a) What is the provisional diagnosis?
Rabies
b) Discuss briefly about the pathogenesis of the above clinical condi�on?
Mul�ply locally at the site of inocula�on Enters into peripheral neurons Spreads centripetally
and reaches up to CNS Infects the CNS (most common sites are hippocampus and cerebellum)
From CNS, virus spreads along sensory and autonomic nerves to various �ssues Shed in saliva
Average incuba�on period – 20-90 days
Clinical spectrum consists of 3 phases:
Prodromal phase, Acute neurologic phase and Coma and death.
19 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
c) Describe the laboratory inves�ga�ons to confirm the diagnosis.
Specimen – saliva, serum, CSF, skin biopsies from hair follicles at nape of neck
Rabies an�gen detec�on Direct immunofluorescence test/Direct
florescent an�body test
Viral isola�on Mouse inocula�on, Cell lines like mouse
neuroblastoma cell line, baby hamster kidney
cell lines
An�body detec�on Mouse neutraliza�on test, Rapid fluorescent
CNS
focus inhibi�on test, fluorescent an�body virus
neutraliza�on test, Indirect fluorescence assay
Viral RNA detec�on RTPCR
Negri body detec�on – brain biopsy Postmortem diagnosis
d) Explain the prophylaxis of the condi�on
Local treatment of wound – Cleansing by soap and water, Chemical treatment,
Suturing only if necessary and an�bio�c and an� – tetanus measure.
IMMUNIZATION
1. Intramuscular
Essen regimen: The 5-dose regimen prescribes 1 dose on each of days 0,3,7,14 and 28.
Zareb regimen: 4 dose abbreviated mul�site regimen – 2 doses on day 0,1 dose on each day 7
and 21.
2. Intradermal
2 site intradermal regimen prescribes injec�on of 0.1 ml at 2 sites (deltoid or thigh) on days
0,3,7 and 28.
(February 2021)
2. A 20-year-old male pa�ent was admi�ed in hospital with the complaints of difficulty in
swallowing liquids, loss of appe�te and restlessness. He gave history of dog bite by a street dog
one month back
a) What is the diagnosis of this condi�on?
b) Discuss the pathogenesis?
c) Describe the laboratory diagnosis of the condi�on?
d) What is the post exposure prophylac�c measures of his condi�on?
Ans:
Refer previous ques�ons
(January 2023)
3. A four-year-old child was brought to paediatric casualty with fever, altered behaviour and
difficulty to swallow liquids. Mother gives a history of dog bite two months back and not
taking vaccine as per schedule.
(a) What is your clinical diagnosis?
(b) Name the causa�ve agent.
(c) Describe the pathogenesis of this condi�on.
(d) List the samples collected and the methods of antemortem diagnosis of this condi�on.
(e) Name cell culture vaccines for this disease.
(f) What is IDRV. Discuss the post exposure vaccina�on schedule
20 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Ans:
(a) What is your clinical diagnosis?
Rabies
(b) Name the causa�ve agent.
Rabies virus belongs to Rhabdoviridae family
(c) Describe the pathogenesis of this condi�on.
CNS
(d) List the samples collected and the methods of antemortem diagnosis of this condi�on.
Specimen – saliva, serum, CSF, skin biopsies from hair follicles at nape of neck
Rabies an�gen detec�on Direct immunofluorescence test/Direct
florescent an�body test
Viral isola�on Mouse inocula�on, Cell lines like mouse
neuroblastoma cell line, baby hamster kidney
cell lines
An�body detec�on Mouse neutraliza�on test, Rapid fluorescent
focus inhibi�on test, fluorescent an�body virus
neutraliza�on test, Indirect fluorescence assay
Viral RNA detec�on RTPCR
Negri body detec�on – brain biopsy Postmortem diagnosis
21 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(e) Name cell culture vaccines for this disease.
Cell culture vaccines
Purified chick embryo cell (PCEC) vaccine - chicken fibroblast cell line
Purified Vero cell (PVC) vaccine - Vero cell line
Human diploid cell (HDC) vaccine - WI-38 (human embryonic lung fibroblast cell line)
CNS
(f) What is IDRV? Discuss the post exposure vaccina�on schedule
IDRV – Intra Dermal Rabies Vaccine
Local treatment of wound – Cleansing by soap and water, Chemical treatment, Suturing only if
necessary and an�bio�c and an� – tetanus measure
Risk categoriza�on and recommended an�-rabies prophylaxis
Category of risk Type of exposure Recommended prophylaxis
(WHO)
Category I (No risk) • Touching, or feeding of • No treatment needed if
animal history is reliable
• Licks on intact skin
Category II (Minor risk) Minor scratches or abrasions • Wound management
without bleeding or nibbling of • Rabies vaccine
uncovered skin • Observe the dog for 10 days
Category III (Major risk) • Single or mul�ple • Wound management
transdermal bites with oozing • Rabies immunoglobulin
of blood • Rabies vaccine
• Licks on broken skin (fresh • Observe the dog for 10 days
wounds) or mucous
membrane
• Direct contact with bats or
wild animals
1. Post exposure prophylaxis [PEP]
a. Previously not received PEP/PrEp
ID PEP regimen (2-2-2): 2-site ID vaccine is given on days 0, 3 and 7
1-site IM vaccine given on days 0, 3, 7 and the fourth dose between days 14 to 28
2-site IM vaccine given on day 0 and 1-site IM on days 7 and 21.
b. Previously received PEP/PrEp
1-site ID vaccine given on days 0 and 3 or
1-site IM vaccine given on days 0 and 3 or
4-site ID vaccine given on day 0 only
22 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT ESSAYS
SHORT ESSAYS
(October 2016)
1. Japanese encephali�s
Most common cause of epidemic encephali�s.
Enveloped ssRNA virus.
Transmi�ed - bite of Culex mosquito.
Ardeid birds - natural reservoirs
Pigs - amplifier hosts
CNS
Ca�les and buffaloes act as mosquito a�ractants
Man is the dead-end host
Ardeid birds Culex Ardeid birds
Pigs Culex Pigs (amplifier)
Clinical Features
Incuba�on period: 5-15 days
Clinical course: - consists of 3 stages-prodromal, acute encephali�c, late stage and sequelae
PRODROMAL ACUTE ENCEPHALITIC STAGE LATE STAGE AND SEQUELAE
Febrile illness, onset of which Acute onset of fever, mental Convalescent stage in which
may be abrupt, acute, or confusion, disorienta�on, the pa�ent may recover
subacute delirium, seizures completely or retain certain
permanent neurological
deficit.
Lab Diagnosis
IgM capture - MAC ELISA
Molecular methods - RT-PCR
Prophylaxis
Live a�enuated cell Inac�vated cell Inac�vated Vero cell
culture derived SA-14- culture derived SA-14- culture derived Kolar
14-2 14-2 (Jeev) (Jenvac)
Dose , route 0.5 mL; 1 – 3 yr : 0.25 0.5 mL ; intramuscular
subcutaneous mL; > 3 yr :0.5 mL ;
intramuscular
site Anterolateral thigh , Anterolateral Anterolateral thigh ,
upper arm thigh , upper arm upper arm
Schedule Only endemic areas ; Not used Not used
na�onal programme two doses at 9 and 16-
18 months
IAP 2016 Recommended in Recommended in Recommended in
endemic areas endemic areas endemic areas
Not available in ≥ 1 yr old ;two doses 4 ≥ 1 yr old ;two doses 4
private sector weeks apart weeks apart
Catch up Up to 18 years ; one Up to 18 years Up to 18 years
23 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
dose to non-immune
adults
Adverse reac�ons Fever , malaise , Less common : fever , Uncommon
hypersensi�vity is rare pain , malaise
Chimeric Vaccine
Live a�enuated YFV-17D/JEV vaccine
CNS
Under development
Phase 3 studies is ongoing
Premembrane and envelop (prME) gene of SA-14-14-2 strain is inserted between core and
non-structural genes of YFV-17D strain.
(July 2022)
2. What are prions? Name human prion diseases. Discuss in detail any one of them.
Ans :
Prions are infec�ous protein par�cles that lack any nucleic acid
They are filterable like viruses
But are resistant to wide range of chemical and physical agents of steriliza�on.
There are several prion diseases of humans and animals
Human prion diseases
Kuru
Gerstmann- Sträussler - Scheinker syndrome
Fatal familial insomnia
Creutzfeldt-Jakob disease (CJD)
Creutzfeldt-Jakob Disease (CJD)
Most common prion disease
Rare disorder
Rapidly progressive demen�a
Sporadic form of CJD is about 85% of cases
Familial forms are caused by muta�ons in PRNP.
Peak incidence in the seventh decade
Types
Classical or sporadic (sCJD) Familial (fCJD) Iatrogenic (iCJD): Variant (vCJD)
Spontaneous misfolding fCJD and its variants Blood transfusion Consump�on of
of prion-protein in an Gerstmann Sträussler- Use of human-derived contaminated
individual Scheinker syndrome and pituitary growth beef with BSE
85% of cases fatal familial insomnia hormones, prions
are hereditary gonadotropin hormone
Majority of the other therapy
15% of cases of CJD Corneal and
meningeal transplants
Risk factors
Corneal transplanta�on,
Deep implanta�on of electrodes in the brain
24 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Contaminated prepara�ons of naturally derived human growth hormone
Clinical Features
Subtle changes in memory and behaviour
Rapidly progressive demen�a
Startle myoclonus
Ataxia
Uniformly fatal
CNS
The average survival -7 months a�er the onset of symptoms
Pathogenesis
Prions enters in the body
Infec�ous protein par�cles are carried to brain
Induce misfolding of normal cellular prion proteins (PrPc)
Disease-causing isoform (PrPsc)
PrPsc are aggregated as amyloid-like plaques
internalized by neurons
get accumulated inside the cytoplasmic vacuoles
spongiform appearance
Laboratory Diagnosis
Measurement of PrPsc by conforma�on dependent immunoassay
Brain biopsies: spongiform degenera�on with lack of inflammatory response
Sequencing the PRNP gene - familial forms of prion diseases
Abnormal EEG - high-voltage, triphasic sharp discharges are observed
Treatment
No known effec�ve therapy for preven�ng or trea�ng prion diseases
25 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(July 2023)
3. Discuss the pathogenesis, antemortem lab diagnosis and post exposure prophylaxis of
Rabies.
Ans:
CNS
Antemortem diagnosis
An�gen detec�on from hair follicles at nape and from corneal smear—by direct IF test
Viral Isola�on by: Mouse inocula�on Cell lines inocula�on—Mouse neuroblastoma and BHK
cell lines.
An�body detec�on from serum and CSF—by MNT, RFFIT, FAVN, and IFA
Viral RNA detec�on—by RT-PCR
Post exposure prophylaxis
Local treatment of wound – Cleansing by soap and water, Chemical treatment, Suturing only if
necessary and an�bio�c and an� – tetanus measure
Risk categoriza�on and recommended an�-rabies prophylaxis
Category of risk Type of exposure Recommended prophylaxis
(WHO)
Category I (No risk) • Touching, or feeding of • No treatment needed if
animal history is reliable
• Licks on intact skin
Category II (Minor risk) Minor scratches or abrasions • Wound management
26 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
without bleeding or nibbling of • Rabies vaccine
uncovered skin • Observe the dog for 10 days
Category III (Major risk) • Single or mul�ple • Wound management
transdermal bites with oozing • Rabies immunoglobulin
of blood • Rabies vaccine
• Licks on broken skin (fresh • Observe the dog for 10 days
wounds) or mucous
membrane
CNS
• Direct contact with bats or
wild animals
Post exposure prophylaxis [PEP]
a. Previously not received PEP/PrEp
ID PEP regimen (2-2-2): 2-site ID vaccine is given on days 0, 3 and 7
1-site IM vaccine given on days 0, 3, 7 and the fourth dose between days 14 to 28
2-site IM vaccine given on day 0 and 1-site IM on days 7 and 21.
b. Previously received PEP/PrEp
1-site ID vaccine given on days 0 and 3 or
1-site IM vaccine given on days 0 and 3 or
4-site ID vaccine given on day 0 only
27 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORTANSWERS
SHORT ANSWERS
(April 2013, October 2016)
1. Prophylaxis of rabies
Local treatment of wound – Cleansing by soap and water, Chemical treatment, Suturing only if
necessary and an�bio�c and an� – tetanus measure
Risk categoriza�on and recommended an�-rabies prophylaxis
Category of risk Type of exposure Recommended prophylaxis
CNS
(WHO)
Category I (No risk) • Touching, or feeding of • No treatment needed if
animal history is reliable
• Licks on intact skin
Category II (Minor risk) Minor scratches or abrasions • Wound management
without bleeding or nibbling of • Rabies vaccine
uncovered skin • Observe the dog for 10 days
Category III (Major risk) • Single or mul�ple • Wound management
transdermal bites with oozing • Rabies immunoglobulin
of blood • Rabies vaccine
• Licks on broken skin (fresh • Observe the dog for 10 days
wounds) or mucous
membrane
• Direct contact with bats or
wild animals
1. Post exposure prophylaxis [PEP]
a. Previously not received PEP/PrEp
ID PEP regimen (2-2-2): 2-site ID vaccine is given on days 0, 3 and 7
1-site IM vaccine given on days 0, 3, 7 and the fourth dose between days 14 to 28
2-site IM vaccine given on day 0 and 1-site IM on days 7 and 21.
b. Previously received PEP/PrEp
1-site ID vaccine given on days 0 and 3 or
1-site IM vaccine given on days 0 and 3 or
4-site ID vaccine given on day 0 only
2. Pre exposure prophylaxis [PrEP]
For individuals at higher occupa�onal risk
For sub-popula�ons in remote endemic areas
provide life�me protec�on
no need to take PrEP booster periodically
Regimen- 2-site ID vaccine given on days 0 and 7
1-site IM vaccine given on days 0 and 7
28 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Summarised
Type of Route of Dose of Day of No of Total No. Site of
Prophylaxis Administra�on Vaccine Dose Injec�ons Per Visit Injec�on
Pre Intra Dermal 0.1ml per Day 0,3, 7 2 4 Adults:
Exposure dose and 28 Deltoid
CNS
Prophylaxis Muscle
Intramuscular 1 en�re Day 0,3, 1 5
vaccine vial 7,14 and Infants and
28 Small
Children:
Pre Intra Dermal 0.1ml per Day 0,7, 1 3 Anterolateral
Exposure dose and Thigh
prophylaxis booster on
either day
21 or 28
Intramuscular 1 en�re Day 0,7, 1 3
vaccine vial and
booster on
either day
21 or 28
Re- Intra Dermal 0.1ml per Day 0&3 1 2
exposure dose
Intramuscular 1 en�re Day 0&3 1 2
vaccine vial
(September 2013, July 2023)
2. Prions
Ans:
Prions are infec�ous protein par�cles that lack any nucleic acid
They are filterable like viruses
But are resistant to wide range of chemical and physical agents of steriliza�on.
There are several prion diseases of humans and animals
Human prion diseases:
Kuru
Gerstmann-Straussler- Scheinker syndrome
Fatal familial insomnia
Creutzfeldt-Jakob disease (CJD)
29 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Pathogenesis
Prions enters in the body
Infec�ous protein par�cles are carried to brain
Induce misfolding of normal cellular prion proteins (PrPc)
Disease-causing isoform (PrPsc)
CNS
PrPsc are aggregated as amyloid-like plaques
Internalized by neurons
Get accumulated inside the cytoplasmic vacuoles
Spongiform appearance
Laboratory Diagnosis
Measurement of PrPsc by conforma�on dependent immunoassay
Brain biopsies: spongiform degenera�on with lack of inflammatory response
Sequencing the PRNP gene - familial forms of prion diseases
Abnormal EEG - high-voltage, triphasic sharp discharges are observed
Treatment
No known effec�ve therapy for preven�ng or trea�ng prion diseases
(September 2013, July 2019)
3. Negri bodies
Intracytoplasmic inclusion bodies - inner basophilic granules
Composed of viral RNA and proteins.
Stains used - H and E , Sellers stains
IHC - Peroxidase labelled & formalin-fixed �ssues
They are most observed in Purkinje cells of cerebellum and in pyramidal neurons of
hippocampus.
Confirm the postmortem diagnosis of rabies.
Absence of Negri bodies does not rule out the diagnosis of rabies - may not be detected in
20%
H and E staining of brain biopsy
30 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(February 2017)
4. Slow virus disease
Neurodegenera�ve condi�ons affec�ng both humans and animals.
It is characterized by :
Long incuba�on period.
Predilec�on for CNS
High fatality
Strong gene�c predisposi�on
CNS
Absence of an�genicity
Resistant to normal steriliza�on methods
Examples:
Progressive mul�focal leukoencephalopathy – JC virus
Polyoma virus / John Cunningham Virus
Subacute sclerosing panencephali�s – Measles
Progressive rubella encephali�s
Visna and Maedi
Maedi virus encephali�s
(February 2015, February 2018)
5. Name the non-neural vaccines for preven�ng rabies?
Ans:
Purified chick embryo cell vaccine
Purified Vero cell vaccine
Human diploid cell vaccine
(July 2018)
6. Rabies vaccine and latest schedule for immuniza�on
1. Intramuscular
Essen regimen: The 5-dose regimen prescribes 1 dose on each of days 0,3,7,14 and 28.
Zareb regimen: 4 dose abbreviated mul�site regimen – 2 doses on day 0,1 dose on each day 7
and 21.
2. Intradermal
2 site intradermal regimen prescribes injec�on of 0.1 ml at 2 sites (deltoid or thigh) on days
0,3,7 and 28.
OBJECTIVE TYPE QUESTIONS
(July 2023)
1. Write the mode of transmission of Japanese encephali�s
Ans:-Vector borne disease transmi�ed by culex tritaeniorhynchus and culex vishnuii
31 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Parasitic and Fungal Infections
Parasi�c and Fungal Infec�ons
ESSAY
ESSAY
(February 2022)
1. A 21-year-old female presented with recurrent episodes of seizures, headache and
vomi�ng and ver�go. MRI of the brain showed mul�ple ring-enhancing lesions in the
brain parenchyma. The causa�ve agent was thought to be a cestode.
(a) What is the probable causa�ve agent?
(b) Which is the infec�ve stage of the parasite responsible for the above-men�oned
CNS
condi�on?
(c) What is the mode of transmission?
(d) Name other four cestodes with their defini�ve hosts.
(e) Name two stool concentra�on methods.
(f) How do you treat the pa�ent?
(g) How to prevent this infec�on?
Ans:
(a) What is the probable causa�ve agent?
Taenia solium
(b) Which is the infec�ve stage of the parasite responsible for the above-men�oned
condi�on?
Eggs of T. solium
(c) What is the mode of transmission?
Inges�on of contaminated food or water containing eggs of T. solium
Autoinfec�on External/Internal
(d) Name other four cestodes with their defini�ve hosts.
Cestodes Defini�ve host
Taenia saginata Man
Taenia solium Man
Echinococcus granulosus Dog
Hymenolepis nana Man
Diphyllobothrium latum Man
(e) Name two stool concentra�on methods.
Indica�ons
Parasite output is low in feces
Direct examina�on may not be able to detect the parasites
Methods
Sedimenta�on techniques - formalin-ether
Flota�on techniques - Zinc sulphate flota�on concentra�on technique
Sheather’s sugar flota�on technique
32 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(f) How do you treat the pa�ent?
Treatment
An�parasi�c agents Symptoma�c treatment Surgery
Albendazole (15 mg/kg per Seizures - an�epilep�c drugs Open craniotomy is rare
day for 8–28 days) High-dose glucocor�coids Surgery is indicated for
Praziquantel (50–100 mg/kg should be used to reduce the ocular
CNS
daily in three divided doses for inflamma�on spinal
15–30 days) Hydrocephalus: A�empts ventricular lesions because
should be made to reduce an�parasi�c drugs can provoke
intracranial pressure irreversible inflammatory
obstruc�ve hydrocephalus - damage
cys�cerci can be removed by
endoscopic surgery or
ventriculoperitoneal shun�ng.
(g) How to prevent this infec�on?
Good personal hygiene to prevent autoinfec�on with eggs
Effec�ve fecal disposal to prevent contamina�on of food and water with eggs
Treatment and preven�on of human intes�nal taeniasis
Vaccines to prevent porcine cys�cercosis
33 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT
SHORTESSAYS
ESSAYS
(July 2018, February 2020, May 2021)
1. Cryptococcosis
Caused by Cryptococcus neoformans
Capsulated yeast
Cryptococcal meningi�s mainly immunocompromised individuals.
Pathogenesis
CNS
By inhala�on of aerosolized forms
Pulmonary cryptococcosis
Cutaneous
Pulmonary vasculature manifesta�ons &
osteoly�c bone disease
Disseminates into the CNS
Cryptococcus neoformans
Clinical features
Chronic meningi�s
C/O – headache
Neck s�ffness,
34 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
And disorienta�on
Lesions in skin, lungs, or other organs
Diagnosis
Specimens - cerebrospinal fluid (CSF), �ssue, exudates, sputum, blood, cutaneous scrapings, and
urine
Detected by nega�ve staining microscopy – staining by Modified India ink or nigrosine stains.
Gram staining – gram posi�ve round budding yeast cells
CNS
Culture in SDA – mucoid creamy white and yeast like colonies
Niger seed agar and bird seed agar :- brown coloured colonies
Tests for GXM, capsular an�gen
Latex slide agglu�na�on test or enzyme immunoassay (EIA)- Cryptococcal an�gen
Lateral flow assay – GXM detec�on
CSF analysis:
CSF pressure and protein may be increased
Cell counts elevated
Glucose is normal or low
2. Cryptococcal meningi�s – risk factors, pathogenesis, and laboratory diagnosis
Ans:
Risk factors
Pa�ents with advanced HIV infec�on
Pa�ents with hematologic malignancies
Transplant recipients
Pa�ents on immunosuppressive or steroid therapy
Pathogenesis & Lab diagnosis: Refer previous questions.
(July 2022)
3. Primary amoebic meningoencephali�s – e�ology, mode of transmission, laboratory
diagnosis
Ans:
Caused by naegleria fowleri - a free living amoeba found in warm fresh water.
35 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Pathogenesis
CNS
Tissue destruc�on:
Amoebostome into which the cytopathic enzymes are liberated
Contact dependent cytolysis mediated by hemoly�c proteins, cytolysins and phospholipase
enzymes.
Mode of transmission
Nasal contamina�on during swimming in fresh hot water
Rarely, if the flagellated or cyst form enters, soon it reverts into amoeboid form
Diagnosis
CSF analysis – mimic bacterial meningi�s
CSF microscopy: 1. Wet mount
2. Phase contrast microscope
3. Direct fluorescent an�body staining
Histopathology - Brain biopsy – H&E/Giemsa - trophozoites having sky blue cytoplasm with a
pink nucleus
Culture - non-nutrient agar (Page’s saline and 1.5% agar) with bacterial supplement like E. coli
– Trail sign
Enflagella�on test
Isoenzyme analysis
Molecular methods - Mul�plex real-�me PCR of 18S rRNA
Imaging methods- CT scan and MRI
36 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
SHORT ANSWERS
SHORT ANSWERS
(September 2014)
1. Naegleria fowleri
Ans:
Free living amoeba
Seen in warm fresh water
Cyst and trophozoite forms
Acute suppura�ve fulminant infec�on of CNS
CNS
Pathogenesis
Tissue destruc�on:
Amoebostome into which the cytopathic enzymes are liberated
Contact dependent cytolysis mediated by hemoly�c proteins, cytolysins and phospholipase
enzymes.
Mode of transmission
Nasal contamina�on during swimming in fresh hot water
Rarely, if the flagellated or cyst form enters, soon it reverts into amoeboid form
Clinical Features
Incuba�on period: 1–2 days to 2 weeks
Changes in the taste and smell
Headache
Anorexia
Nausea
Vomi�ng
37 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
High fever
Signs of meningeal involvement - s�ff neck and a posi�ve Kernig’s sign
Confusion
Hallucina�ons
Lack of a�en�on
Ataxia
Seizures
CNS
Diagnosis
CSF analysis – mimic bacterial meningi�s
CSF microscopy: 1. Wet mount
2. Phase contrast microscope
3. Direct fluorescent an�body staining
Histopathology - Brain biopsy – H&E/Giemsa - trophozoites having sky blue cytoplasm with a
pink nucleus
Culture - non-nutrient agar (Page’s saline and 1.5% agar) with bacterial supplement like E. coli
– Trail sign
Enflagella�on test
Isoenzyme analysis
Molecular methods - Mul�plex real-�me PCR of 18S rRNA
Imaging methods- CT scan and MRI
Treatment
No effec�ve treatment is available for PAM
Amphotericin B
Rifampicin
Sulfisoxazole Found to be useful
Miconazole
Fluconazole
Miltefosine
(February 2016, October 2016, July 2022)
2. Cryptococcosis
Refer Short Essays
(February 2017)
3. Free living amoebae
Small
Freely living,
Widely distributed in soil and water and
Can cause opportunis�c infec�ons in humans.
The main 4 parasites belonging to this group
Free living amoebae Infec�on by it
Acanthamoeba species Primary amoebic meningoencephali�s (PAM)
Balamuthia mandrillaris Granulomatous amoebic encephali�s (GAE)
amoebic kera��s in contact lens wearers
Sappinia species Granulomatous amoebic encephali�s (GAE)
Encephali�s
38 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
(August 2017)
4. Lab diagnosis of cryptococcosis
Detected by nega�ve staining microscopy – staining by Modified India ink or nigrosine stains.
Gram staining of culture isolate – gram posi�ve round budding yeast cells
Culture in SDA – mucoid creamy white and yeast like colonies
Niger seed agar and bird seed agar: - brown coloured colonies
(February 2018)
CNS
5. Name the causa�ve agent, infec�ve form, and complica�ons of neurocys�cercosis
Ans:
Causa�ve agent: Tenia solium
Infec�ve form- Cyst ,Cys�cercus cellulosae
Complica�ons : -seizure, hydrocephalus, chronic meningi�s, cerebral arteri�s, demen�a, focal
neurological deficits
(May 2022)
6. Primary amoebic meningoencephali�s
Ans:
Acute suppura�ve fulminant infec�on of CNS
Caused by naegleria fowleri ; a free living amoeba found in warm fresh water.
Pathogenesis
Tissue destruc�on
Amoebostome into which the cytopathic enzymes are liberated
Contact dependent cytolysis mediated by hemoly�c proteins, cytolysins and phospholipase
enzymes.
39 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Clinical features
Incuba�on period: 1–2 days to 2 weeks
Changes in the taste and smell
Headache
Anorexia
Nausea
Vomi�ng
High fever
CNS
Signs of meningeal involvement - s�ff neck and a posi�ve Kernig’s sign
Confusion
Hallucina�ons
Lack of a�en�on
Ataxia
Seizures
Diagnosis
CSF analysis – mimic bacterial meningi�s
CSF microscopy-
1. Wet mount
2. Phase contrast microscope
3. Direct fluorescent an�body staining
Histopathology - Brain biopsy – H&E/Giemsa - trophozoites having sky blue cytoplasm with a
pink nucleus
Culture - non-nutrient agar (Page’s saline and 1.5% agar) with bacterial supplement like E. coli -
Trail sign
Enflagella�on test
Isoenzyme analysis
Molecular methods - Mul�plex real-�me PCR of 18S rRNA
Imaging methods- CT scan and MRI
Treatment
No effec�ve treatment is available for PAM
Amphotericin B
rifampicin
sulfisoxazole found to be useful
miconazole
fluconazole
miltefosine
(May 2022)
7. Neurocys�cercosis
Ans:
Parasi�c infec�on of the CNS
By larvae of the pork tapeworm, Taenia solium
Defini�ve and intermediate host – Man
Infec�ve stage: Eggs of T. solium
Mode of transmission: inges�on of contaminated food or water containing eggs of T. solium
autoinfec�on External/Internal
40 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
Pathogenesis
Embryo or oncosphere is released from the eggs
penetrates the intes�ne
Portal circula�on or mesenteric lympha�cs
CNS
Reaches to various organs like subcutaneous �ssue, muscle, eye and brain
Larval stage
Cys�cercus cellulosae in 7–9 weeks and deposited as cyst
Full development to mature cysts takes 2–3 months of �me
Clinical features
Asymptoma�c NCC
Seizure
Hydrocephalus
Increased intracranial pressure - headache, vomi�ng and ver�go
Chronic meningi�s
Focal neurological deficits
Psychological disorders and demen�a
Cerebral arteri�s
Basal and ventricular involvement
Based on involvement :- 1. Parenchymal - brain parenchyma
2. Extra parenchymal - meninges, ventricles, spinal cord, and subarachnoid
space
Morphological stages
Vesicular
Necro�c
Nodular
Calcified stage
Laboratory diagnosis
Radiodiagnosis—CT scan and MRI
An�body detec�on in serum or CSF— ELISA &Western blot
An�gen detec�on in serum or CSF—ELISA
Lymphocyte transforma�on test
Histopathology of muscles, eyes, subcutaneous �ssues, or brain biopsies—can detect cys�cerci
FNAC of the cyst and then staining with Giemsa
Fundoscopy of eye—detects larvae
Modified Del Bru�o diagnos�c criteria
41 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
CNS
Cys�cercus cellulosae Ring enhanced lesions in CT brain
(March 2014)
8. Intermediate and defini�ve host for toxoplasma gondii
Ans: Intermediate host - cats and other felines (sexual cycle)
defini�ve host - other mammals like rodents (asexual cycle)
(March 2014)
9. Acanthamoeba
Free-living amoebae
Infect CNS, skin, and eye
They are ubiquitous and present worldwide
Acanthamoeba astronyxis, A. castellanii, A. culbertsoni and A. polyphaga - cause human
infec�on
Reservoir for bacteria: Legionella and may serve as a poten�al reservoir
Trojan horse of the microbial world
Granulomatous Amoebic Encephali�s (GAE)
Insidious onset
Incuba�on period varies from several weeks to months.
Subacute to chronic course: Lasts for months to years
Pathology: It produces focal granulomatous lesions in brain
Lymphocytosis of CSF can be seen
In pa�ents with AIDS, no cells are seen in CSF
Symptoms
Confusion
Dizziness
Nausea
Headache
S�ff neck
Seizure
Hemiplegia
In HIV pa�ents: nasal ulcers, cutaneous ulcers and musculoskeletal abscesses also
42 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
CNS
30 μm (25–40 µm) 10–25 μm
thorn or spine like pseudopodia double walled
acanthopodia outer wrinkled cyst wall
Nucleus is single with central karyosome
no peripheral chroma�n
43 Kerala University of Health Sciences
UNIVERSITY S O L V E D
Q U E S T I O N
MANUAL B A N K
OBJECTIVE TYPEQUESTIONS
OBJECTIVE TYPE QUESTIONS
(July 2023)
1. Write two iden�fying features of Cryptococcus neoformans
Ans:
Nega�ve staining - refrac�le delineated clear space surrounding the budding round yeast cells
against black background
Gram staining - gram-posi�ve round budding yeast cells
Mucicarmine stain - stains the carminophilic cell wall of C. neoformans „
CNS
Masson-Fontana stain - produc�on of melanin
Alcian blue stain - demonstrate the capsule.
Niger seed agar and bird seed agar - demonstrate melanin produc�on (brown colored colonies)
Growth at 37°C
Urease test is posi�ve
Assimila�on of inositol and nitrate
Mouse pathogenicity test
Automated iden�fica�on system such as MALDI-TOF
(July 2023)
2. Name one free living amoebae and the infec�on caused by it
Ans:
Free living amoebae Infec�on by it
Naegleria fowleri primary amoebic meningoencephali�s (PAM)
Acanthamoeba species granulomatous amoebic encephali�s (GAE)
amoebic kera��s in contact lens wearers
Balamuthia mandrillaris granulomatous amoebic encephali�s (GAE)
Sappinia species encephali�s
44 Kerala University of Health Sciences
You might also like
- Enumerate The Aetiological Agents of Meningeal Involvement in ChildrenDocument21 pagesEnumerate The Aetiological Agents of Meningeal Involvement in ChildrenAbhirup BoseNo ratings yet
- Meningitis: Review ArticleDocument19 pagesMeningitis: Review ArticleYo Me100% (1)
- Centralnervoussystem Lesionsin Immunocompromisedpatients: Robert Y. Shih,, Kelly K. KoellerDocument15 pagesCentralnervoussystem Lesionsin Immunocompromisedpatients: Robert Y. Shih,, Kelly K. Koelleralejandro echeverriNo ratings yet
- Centralnervoussystem Lesionsin Immunocompromisedpatients: Robert Y. Shih,, Kelly K. KoellerDocument15 pagesCentralnervoussystem Lesionsin Immunocompromisedpatients: Robert Y. Shih,, Kelly K. Koelleralejandro echeverriNo ratings yet
- Infectious Diseases Pharmacotherapy: Lesson 5 Central Nervous System InfectionDocument63 pagesInfectious Diseases Pharmacotherapy: Lesson 5 Central Nervous System Infectionbest batiNo ratings yet
- Diagnosing Meningitis Through Laboratory TestsDocument4 pagesDiagnosing Meningitis Through Laboratory TestsAlfrien Ivanovich LarchsonNo ratings yet
- CNS InfectionDocument10 pagesCNS InfectionShunqing ZhangNo ratings yet
- Formulation and Evaluation of Fast Dissolving Oral Films of Cetirizine HydrochlorideDocument25 pagesFormulation and Evaluation of Fast Dissolving Oral Films of Cetirizine HydrochlorideGaurav AdhikariNo ratings yet
- Neisse RiaDocument49 pagesNeisse RiaSubhada GosaviNo ratings yet
- CNS InfectionsDocument3 pagesCNS InfectionsStefy BarranoNo ratings yet
- Meningitis 2005Document87 pagesMeningitis 2005nafisyarifahNo ratings yet
- Meningitis PDFDocument10 pagesMeningitis PDFAlfatahadi SNo ratings yet
- Diagnosis and Treatment of Bacterial Meningitis: Archives of Disease in Childhood August 2003Document7 pagesDiagnosis and Treatment of Bacterial Meningitis: Archives of Disease in Childhood August 2003Jayalakshmi PreethaNo ratings yet
- Gram Negative Cocci Causing Meningitis, Septicaemia and Respiratory InfectionsDocument22 pagesGram Negative Cocci Causing Meningitis, Septicaemia and Respiratory InfectionsSalih TahsinNo ratings yet
- Fever With Rash SeminarDocument98 pagesFever With Rash SeminarSYAZRIANA SUHAIMINo ratings yet
- Treatment: Tensive Care Unit Is Often NecessaryDocument12 pagesTreatment: Tensive Care Unit Is Often NecessaryCocosul Cocosului CocosaruluiNo ratings yet
- Comparison of Culture and PCR Methods in The Diagnosis of Bacterial MeningitisDocument5 pagesComparison of Culture and PCR Methods in The Diagnosis of Bacterial Meningitisrais123No ratings yet
- Pathology BrainDocument4 pagesPathology BrainAshuNo ratings yet
- MENINGITISDocument44 pagesMENINGITIStummalapalli venkateswara rao100% (5)
- تَـلـخـيـص شَـابـتـر ٢٢?Document14 pagesتَـلـخـيـص شَـابـتـر ٢٢?سلطان محمد فوزي سلمانNo ratings yet
- PyomeningitisDocument54 pagesPyomeningitisRiya BagdiNo ratings yet
- Microbiology Case Study on Viral MeningitisDocument5 pagesMicrobiology Case Study on Viral MeningitisSimran MgrNo ratings yet
- Bacterial Meningitis Causes, Symptoms & TreatmentDocument40 pagesBacterial Meningitis Causes, Symptoms & TreatmentDinesh ReddyNo ratings yet
- Cerebro Spinal Fluid Analysis KpbiDocument5 pagesCerebro Spinal Fluid Analysis KpbiHoopmen Silaen100% (1)
- CSF and CNS InfectionsDocument9 pagesCSF and CNS InfectionsJorelyn Frias100% (1)
- MeningitisDocument18 pagesMeningitisMBBS AspirantNo ratings yet
- DiseaseDocument5 pagesDiseasemartha rogersNo ratings yet
- Invasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportDocument5 pagesInvasive Cryptococcal Meningitis Presenting As A Skull Base Mass in An Immunocompetent Host: A Case ReportAsep RiswandiNo ratings yet
- Acute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorDocument28 pagesAcute Meningitis: DR K. Saroj Novel Jr-1 General Medicine Moderator:Dr - Sushanth MD Assistant ProfessorSaikiran GundaboynaNo ratings yet
- Meningococcemia GuideDocument5 pagesMeningococcemia GuidezzoOeeNo ratings yet
- What Is Meningitis?Document7 pagesWhat Is Meningitis?laujeroNo ratings yet
- Alterations in Ventilation Part V - Respiratory PandemicsDocument84 pagesAlterations in Ventilation Part V - Respiratory Pandemicsirish felixNo ratings yet
- Examination of CSF: Dr. Md. Razib HasanDocument33 pagesExamination of CSF: Dr. Md. Razib HasanRazib HasanNo ratings yet
- Microbiology - Inicet Nov 2022Document19 pagesMicrobiology - Inicet Nov 2022Kuldeep SinghNo ratings yet
- Intracranial SepsisDocument60 pagesIntracranial SepsisHarun MohamedNo ratings yet
- Pathogenesis of MENINGITISDocument30 pagesPathogenesis of MENINGITISPrachi TeteNo ratings yet
- Meningitis: Carlos J. Pech Lugo R2MiDocument55 pagesMeningitis: Carlos J. Pech Lugo R2MiGABY DORIS RAMOSNo ratings yet
- Meningitis Risk Factors and TreatmentDocument2 pagesMeningitis Risk Factors and Treatmentedrian02No ratings yet
- Pathogenesis of Central Nervous System InfectionsDocument44 pagesPathogenesis of Central Nervous System InfectionsMira ApriliaNo ratings yet
- Cryptococcosis: The Fungal Infection of Lungs and BrainDocument17 pagesCryptococcosis: The Fungal Infection of Lungs and BrainKarthick AnbuNo ratings yet
- Lecture CSF 1Document7 pagesLecture CSF 1وسيم جمال مياسNo ratings yet
- Meningitis (Completed)Document26 pagesMeningitis (Completed)seema83% (6)
- L - 2 - GR (-) CocciDocument82 pagesL - 2 - GR (-) CocciFahim NadvyNo ratings yet
- Acute GlomerulonephritisDocument47 pagesAcute Glomerulonephritissurbhib268No ratings yet
- Acute Bacterial Meningitis and Antimicrobials in NeurosurgeryDocument35 pagesAcute Bacterial Meningitis and Antimicrobials in NeurosurgeryCalicut NeurosurgeryNo ratings yet
- Central Nervous System (CNS) InfectionsDocument42 pagesCentral Nervous System (CNS) Infectionsapi-3699361100% (3)
- Lumbar Puncture: Videos in Clinical MedicineDocument4 pagesLumbar Puncture: Videos in Clinical MedicineAbo AmgadNo ratings yet
- Bacterial Meningitis Diagnosis and TreatmentDocument13 pagesBacterial Meningitis Diagnosis and TreatmentJubee FelicianoNo ratings yet
- CSF PDFDocument58 pagesCSF PDFVas KannanNo ratings yet
- LP After Correct.Document32 pagesLP After Correct.Academic Nurse. M.M AbbasNo ratings yet
- Clinical Microscopy - Other Body FluidsDocument93 pagesClinical Microscopy - Other Body FluidsTherese Ann Eve FlorenososNo ratings yet
- Bacterial Meningitis 13Document6 pagesBacterial Meningitis 13caliptra36No ratings yet
- 2midterm 8 - Diagnostic Virology TRANSDocument2 pages2midterm 8 - Diagnostic Virology TRANSRobee Camille Desabelle-SumatraNo ratings yet
- Meningitis TopicDocument9 pagesMeningitis Topicapi-668691030No ratings yet
- Case Report Paracoccidioidomycosis in A Liver Transplant RecipientDocument3 pagesCase Report Paracoccidioidomycosis in A Liver Transplant RecipientCarlos AlbertoNo ratings yet
- Molecular Biology Lab FinalsDocument2 pagesMolecular Biology Lab FinalsdokutahNo ratings yet
- 2018 COMPARATIVE MICRO MeningoencephalitisDocument6 pages2018 COMPARATIVE MICRO MeningoencephalitisMarianneTee-ruhNo ratings yet
- Pathobiology of the Endothelial CellFrom EverandPathobiology of the Endothelial CellHymie L. NosselNo ratings yet
- Common Communicable DiseasesDocument13 pagesCommon Communicable DiseasesSanthosh.S.U100% (1)
- Kode Simpus PTT EMIDocument18 pagesKode Simpus PTT EMIfauziahNo ratings yet
- Model Paper 9Document6 pagesModel Paper 9Dr-Sanjay SinghaniaNo ratings yet
- Practical Applications of Immunology Written ReportDocument9 pagesPractical Applications of Immunology Written ReportVincent Drystan AdronNo ratings yet
- Polio: Clinical Case DefinitionDocument6 pagesPolio: Clinical Case DefinitionRohit kumar patelNo ratings yet
- Puskesmas Kecamatan Kelapa Gading Provides Immunization ServicesDocument1,322 pagesPuskesmas Kecamatan Kelapa Gading Provides Immunization ServicesIRMA BUDI LESTARINo ratings yet
- Viral Infections: Measles, Rubella and MumpsDocument67 pagesViral Infections: Measles, Rubella and MumpsNicolle PanchoNo ratings yet
- Communicable Diseases of the Nervous SystemDocument11 pagesCommunicable Diseases of the Nervous SystemMilcah NuylesNo ratings yet
- Microbial Diseases of The Nervous System: DR Sonnie P. Talavera 08162009 OlfuDocument162 pagesMicrobial Diseases of The Nervous System: DR Sonnie P. Talavera 08162009 Olfuone_nd_onlyu0% (1)
- Electromyography 3Document16 pagesElectromyography 3Izabella MihályNo ratings yet
- SIA GuidelinesDocument18 pagesSIA Guidelinestamtam06100% (1)
- ROTARACT 101 - For New ClubsDocument47 pagesROTARACT 101 - For New ClubsRenan Joseph Jr. Ortua100% (1)
- Health Promotion&Problem of The Preschool 2Document31 pagesHealth Promotion&Problem of The Preschool 2Hadeer HamdyNo ratings yet
- Better Health Dot Point (HSC Biology)Document10 pagesBetter Health Dot Point (HSC Biology)KinzNo ratings yet
- ACT Crack BiologyDocument250 pagesACT Crack BiologyabdogamreNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
- NOVA Vaccines Calling The ShotsDocument7 pagesNOVA Vaccines Calling The Shotslu naeNo ratings yet
- Polio OutbreakDocument3 pagesPolio OutbreakAyn Jel MayNo ratings yet
- Raj Malhotra'S Ias Academy, ChandigarhDocument7 pagesRaj Malhotra'S Ias Academy, ChandigarhBhargavaNandaNo ratings yet
- ASM 345 Study Guide For Quiz 5 Module 5 - 2014-1Document2 pagesASM 345 Study Guide For Quiz 5 Module 5 - 2014-1Martín CastilloNo ratings yet
- Important Monthly Current Affairs Capsule - October 2022Document382 pagesImportant Monthly Current Affairs Capsule - October 2022FebzNo ratings yet
- St. Paul College of Ilocos SurDocument6 pagesSt. Paul College of Ilocos SurMarie Kelsey Acena Macaraig100% (1)
- Concepts of Health, Disease and EpidemiologyDocument9 pagesConcepts of Health, Disease and EpidemiologysohamNo ratings yet
- VIII Science Sampel PaperDocument4 pagesVIII Science Sampel PaperTaranjeet SinghNo ratings yet
- National EPI 2021 PDFDocument40 pagesNational EPI 2021 PDFyeabsira gashawNo ratings yet
- Global Polio Survilance Action Plan 2022-2024Document90 pagesGlobal Polio Survilance Action Plan 2022-2024monoluNo ratings yet
- Review of Common Pathologies Requiring Ankle-Foot OrthosesDocument32 pagesReview of Common Pathologies Requiring Ankle-Foot OrthosesnovitaNo ratings yet
- W.H.O. Murdered Africa by Dr. William Campbell DouglasDocument20 pagesW.H.O. Murdered Africa by Dr. William Campbell DouglasJohn Burns100% (4)
- Pediatrics Case Studies and Management GuidelinesDocument103 pagesPediatrics Case Studies and Management GuidelinesJulius Matthew LuzanaNo ratings yet
- Intensified Pulse Polio ImmunisationDocument30 pagesIntensified Pulse Polio ImmunisationAdrishyaNo ratings yet