Professional Documents
Culture Documents
US Liver Doppler Only
Uploaded by
micropocketfilmsCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
US Liver Doppler Only
Uploaded by
micropocketfilmsCopyright:
Available Formats
UT Southwestern Department of Radiology
Ultrasound – Liver Doppler Protocol
PURPOSE:
To evaluate the hepatic vasculature for patency, directional flow, and evidence of portal hypertension.
SCOPE:
Applies to all ultrasound abdominal Doppler studies performed in Imaging Services / Radiology
ORDERABLE:
• US Doppler Liver (perform this protocol only)
• May be combined with US Liver and/or US Liver Elastography—please see separate Protocol for
details
• For order US Liver Transplant and Doppler, see dedicated US Liver Transplant protocol
INDICATIONS:
• Signs or symptoms of vascular insufficiency or venous thrombosis attributable to the liver
(examples: ascites, varices, splenomegaly, acute liver failure)
• Known liver disease (cirrhosis or other) with suspected portal hypertension
• Known hepatic artery stenosis; follow up to angioplasty and/or stent
• Abnormal findings on other imaging studies
• Follow up known hepatic vascular issue and/or portal hypertension
• For Liver Transplant, see dedicated US Liver Transplant protocol
CONTRAINDICATIONS:
• No absolute contraindications
• Exam may be compromised by bandages, fresh surgical incisions, bowel gas, obesity.
EQUIPMENT:
• Curvilinear transducer with a frequency range of 1-9 MHz that allows for appropriate
penetration and resolution depending on patient’s body habitus
PATIENT PREPARATION:
• None
EXAMINATION:
GENERAL GUIDELINES:
A complete examination includes evaluation of the hepatic veins, portal veins, splenic vein,
superior mesenteric vein, hepatic artery, inferior vena cava (IVC), TIPS (if present), and
additional image acquisition protocols based on orderable (above)
May be combined with US Liver and/or US Liver Elastography—please see separate Protocol for
details
EXAM INITIATION:
• Introduce yourself to the patient and explain test
• Verify patient identity using patient name and DOB
• Obtain patient history including symptoms. Enter and store data page
• Place patient in supine or left lateral decubitus (LLD) position
US Liver Doppler 04-23-2023 1| P a g e Revision date: 04/23/2023
TECHNICAL CONSIDERATIONS:
• Always review any prior imaging, making note of abnormalities or other findings requiring
further evaluation.
• Review clinical and surgical history, making note of relevant findings
• Note any variations in technique or technical limitations
• In LLD position, the liver shifts towards the midline improving accessibility for scanning
• Optimize gain and display setting with respect to depth, dynamic range, and focal zones on
grey scale imaging first
• Optimize color Doppler setting to show optimal flow
o Adjust scale and gain to maximally fill the vessel of interest without artifact
Light color in the middle of the vessel lumen, darker toward periphery,
showing laminar flow
o Use Power Doppler if suspect absent flow with color Doppler
• Optimize spectral Doppler
o Place time-gate centrally within the vessel of interest
o Adjust scale to extend spectral waveform (amplitude adequate for interpretation)
o Reduce aliasing for high flow evaluation
• As much as possible, utilize angle correction of ≤ 60⁰ to measure velocities
o Angle correction should always be parallel to the vessel wall
o For certain anatomy, may need to try from different approaches to optimize angle
• Evaluate hepatic artery and main portal vein using angle corrected spectral Doppler
• Evaluate hepatic vein phasicity during suspended respiration or shallow breathing
o Deep inspiration may dampen hepatic venous flow
• Evaluate the area around the ligamentum teres for a dilated patent paraumbilical vein
o If present, document image including flow direction
• Evaluate for other upper abdominal varices particularly along the gastrohepatic ligament,
near the splenic hilum, and near the renal hilum
o If present, document image
• Assess the perihepatic area for fluid collections; if a fluid collection is visualized, document
and measure; evaluate with and without color.
• If a TIPS is present, survey the entire TIPS – see US Liver TIPS protocol
• If applicable, please see separate US Liver Doppler and US Liver Elastography if also
ordered/performed
US Liver Doppler 04-23-2023 2| P a g e Revision date: 04/23/2023
IMAGE DOCUMENTATION:
Anatomy Grey Scale Color Waveform *PV RI SAT
Doppler
Splenic vein: hilum x x x
Splenic vein: mid x x x
Splenic vein: confluence x x x
Superior mesenteric vein: x x x
central
Hepatic artery: proper x x x x x
Portal vein: main x x x x
Portal vein: main (diameter x
measurement)
Portal vein: right x x x
Portal vein: left x x x
Hepatic vein: right x x x
Hepatic vein: middle x x x
Hepatic vein: left x x x
IVC x x x
^TIPS: portal vein end x x x x
^TIPS: mid x x x x
^TIPS: hepatic vein/IVC end x x x x
Data page with
measurements
* If there is no phasic waveform, then measure peak velocity
^ If present or if visible (review US Liver TIPS Protocol for details)
For Liver Transplant, see dedicated US Liver Transplant protocol.
PROCESSING:
• Review examination data
• Export and review all images in PACS
• Confirm data transmission in Imorgon (where available)
• Note any study limitations (in Tech Study Note or paper communication, per local workflow)
REFERENCES:
• ACR-AIUM Practice Guideline (Revised 2007)
• ICAVL Guidelines (Updated 8/2012)
• Radiology (2011) 260(3): 884-891
• Radiographics (2011) 31(1): 161-189
US Liver Doppler 04-23-2023 3| P a g e Revision date: 04/23/2023
APPENDIX:
• Hepatic artery
o RI 0.55-0.70 normal range; abnormal elevation > 0.80
Elevated (nonspecific) = postprandial, elderly, diffuse peripheral microvascular
compression or disease (chronic hepatocellular disease or cirrhosis), hepatic venous
congestion
Low = proximal stenosis, distal vascular shunt, cirrhosis with portal HTN and shunts,
Osler-Weber-Rendu with AV fistulas
o PSV ~100 cm/sec
• Portal hypertension
o Reversal of flow (hepatofugal)
o Barcelona Criteria
Main portal vein diameter >13 mm
Monophasic waveform velocity <16 cm/sec
Phasic waveform mean velocity <13 cm/sec
• Normal TIPS velocity is 90-190 cm/sec
o Suspect stenosis if
Portal vein velocity change from baseline ↓ >40 cm/sec ↑ >60 cm/sec
TIPS velocity (if no baseline) <90 cm/sec >190 cm/sec
Portal vein velocity (if no baseline) <30 cm/sec
US Liver Doppler 04-23-2023 4| P a g e Revision date: 04/23/2023
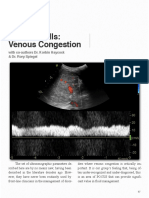
Normal Arterial Waveforms:
Spectrum of increasing hepatic arterial resistance (right to left).
Causes of Elevated Hepatic Arterial Resistance (RI > 0.7)
Causes of Decreased Hepatic Arterial Resistance (RI < 0.55)
US Liver Doppler 04-23-2023 5| P a g e Revision date: 04/23/2023
Normal Hepatic Waveforms:
Causes of Pulsatile Hepatic Venous Waveform
Causes of Decreased Hepatic Venous Phasicity
US Liver Doppler 04-23-2023 6| P a g e Revision date: 04/23/2023
Normal Portal Veins:
Assessment of portal vein pulsatility
Causes of Pulsatile Portal Waveform
US Liver Doppler 04-23-2023 7| P a g e Revision date: 04/23/2023
Transplant liver
o Relevant anastomosis for each vessel should be specifically interrogated, if evident
sonographically
o Determine if the patient underwent a caval interposition technique, in which case both
proximal and distal anastomoses should be interrogated, or a piggy back, in which case
there will be a blind-ending oversewn end of the donor vena cava—thrombus may form in
this structure. A velocity gradient > 3 and turbulent flow may indicate a significant stenosis.
o The portal vein anastomosis can frequently be identified as an area of subtle narrowing. A
velocity gradient > 3 and turbulent flow may indicate a significant stenosis.
o Hepatic artery:
RI 0.55-0.70 normal range; abnormal elevation > 0.80
In the immediate post-transplant period, transient elevation in RIs is not unexpected
and should resolve over the subsequent 48-72 hours.
Tardus parvus waveform:
• SAT >0.07 msec AND PSV >48 cm/sec (69% sensitive, 99.1% specific)
• Absence of tardus parvus waveform has a high NPV for stricture,
dissection, or thrombosis
REVISION HISTORY:
SUBMITTED BY: David T. Fetzer, MD Title Medical Director
APPROVED BY: David T. Fetzer, MD Title Medical Director
APPROVAL DATE: 11-09-2015
REVIEW DATE(S): 09-24-2018 Abhinav Vij, MD
REVISION DATE(S): 04-24-2016 Brief Summary Updates to protocol
name, corresponding to
new templates
04-17-2017 Brief Summary Included details for liver
transplant
06-19-2017 Brief Summary Changes to list of relevant
orders to reflect
consolidation of EPIC
orderables
04-11-2018 Brief Summary Removed references to
Liver Transplant, directing
reader to dedicated US
Liver Transplant protocol
09-24-2018 Brief Summary Minor Language Edits
12-11-2019 Brief Summary Routine formatting
updates
02-12-2020 Brief Summary Removed SAT from HA
09-09-2020 Brief Summary Clarified combining with
other liver exams
04-23-2023 Added MPV Diameter to
Documentation section
US Liver Doppler 04-23-2023 8| P a g e Revision date: 04/23/2023
You might also like
- US Renal Doppler CompleteDocument5 pagesUS Renal Doppler CompletePakde RiNo ratings yet
- Renal Doppler Study: DR Subash Pathak 2nd Year Resident Radiodiagnosis NamsDocument98 pagesRenal Doppler Study: DR Subash Pathak 2nd Year Resident Radiodiagnosis NamsNam Đàm PhươngNo ratings yet
- Liver ImagingDocument7 pagesLiver ImagingBenn BerriganNo ratings yet
- Abdomen Complete ProtocolDocument7 pagesAbdomen Complete Protocolrdfj.muganhu1No ratings yet
- Vexus ScoreDocument28 pagesVexus Scorerev nashrulezNo ratings yet
- Carotid Doppler Study: Dr.I.Gurubharath MD PHD DR - Pooja MDDocument116 pagesCarotid Doppler Study: Dr.I.Gurubharath MD PHD DR - Pooja MDJing CruzNo ratings yet
- The Role of Color Doppler Ultrasound in Living Donor Liver Transplantation 2008 Journal of Medical UltrasoundDocument11 pagesThe Role of Color Doppler Ultrasound in Living Donor Liver Transplantation 2008 Journal of Medical UltrasoundIman Ru-ancaNo ratings yet
- Aortic Stenosis:: Updates in Diagnosis & ManagementDocument48 pagesAortic Stenosis:: Updates in Diagnosis & ManagementCuca PcelaNo ratings yet
- Doppler of The Portal SystemDocument59 pagesDoppler of The Portal SystemivoklarinNo ratings yet
- Liver RebeDocument81 pagesLiver RebeOded YanaNo ratings yet
- Hemodialysis Access: Ultrasound Evaluation Before & After CreationDocument40 pagesHemodialysis Access: Ultrasound Evaluation Before & After CreationobdeeNo ratings yet
- Renal Artery StenosisDocument80 pagesRenal Artery StenosisAnn FloydNo ratings yet
- Imaging in Abdominal Trauma: S ThiyagarajanDocument133 pagesImaging in Abdominal Trauma: S ThiyagarajanEdward Arthur IskandarNo ratings yet
- Venous Congestion ChapterDocument8 pagesVenous Congestion ChapterpcarrascoeNo ratings yet
- Extended Focused Assessment With Sonography in Trauma (eFAST)Document45 pagesExtended Focused Assessment With Sonography in Trauma (eFAST)vimal rajNo ratings yet
- Hepatoportal DopplerDocument15 pagesHepatoportal DopplerRaj Koticha100% (1)
- Renal Ultrasound ProtocolDocument4 pagesRenal Ultrasound Protocolfouad tabetNo ratings yet
- Life Saving Pocket - GuideDocument10 pagesLife Saving Pocket - GuideNur FarhanaNo ratings yet
- Guidelines of Arterial Duplex ScanDocument23 pagesGuidelines of Arterial Duplex ScanMohamed Omar Elfarok100% (1)
- CMR Guide CHD 2014 PDFDocument105 pagesCMR Guide CHD 2014 PDFBasemAlharbiNo ratings yet
- ABG and Oximetry StudentDocument86 pagesABG and Oximetry StudentAlexander Santiago ParelNo ratings yet
- Right Heart Catheterization, NicvdDocument17 pagesRight Heart Catheterization, NicvdNavojit ChowdhuryNo ratings yet
- Baltarowich ABD pt1 Hepatobiliary US PDFDocument22 pagesBaltarowich ABD pt1 Hepatobiliary US PDFEka KusumaningatiNo ratings yet
- Portal HypertensionDocument22 pagesPortal Hypertensionsara.sherif099No ratings yet
- Hemodialysis AccessDocument90 pagesHemodialysis AccessSumit Singh GautamNo ratings yet
- Focused Assessment With Sonography For Trauma (Fast) and Extended-FastDocument49 pagesFocused Assessment With Sonography For Trauma (Fast) and Extended-FastajNo ratings yet
- Jeac 239Document4 pagesJeac 239Spam MailerNo ratings yet
- SSS, BCS, Avf, MalDocument42 pagesSSS, BCS, Avf, MalchintamaniNo ratings yet
- Hemodaynamic Monitoring KHDocument91 pagesHemodaynamic Monitoring KHomar kmr97No ratings yet
- 2 POCUS in Emergency FAST IVC LUNGresidents December 2022Document92 pages2 POCUS in Emergency FAST IVC LUNGresidents December 2022dr mohd abdul basithNo ratings yet
- Sat 1315-1415 Cardiac AngiogDocument47 pagesSat 1315-1415 Cardiac AngiogbenypermadiNo ratings yet
- Liver: Presented by Dr. Tahmina Islam MD Third PartDocument121 pagesLiver: Presented by Dr. Tahmina Islam MD Third PartNajib JamilNo ratings yet
- Dr. Yash Kumar AchantaniDocument65 pagesDr. Yash Kumar AchantaniJenniffer FNo ratings yet
- LiverultrasoundDocument62 pagesLiverultrasoundiuliia94No ratings yet
- Abdominal AortaDocument41 pagesAbdominal AortaMichael IdowuNo ratings yet
- Sample Protocol For Performing Lower Extremity Arterial Duplex ExaminationsDocument2 pagesSample Protocol For Performing Lower Extremity Arterial Duplex ExaminationsMohamed Omar ElfarokNo ratings yet
- Thoracic AngiographyDocument78 pagesThoracic Angiographyskjdef kjsebfNo ratings yet
- Echo With KosmosDocument57 pagesEcho With Kosmossamirmohamed900No ratings yet
- Lecture 21 - Doppler Applications 15 JULY 2020Document33 pagesLecture 21 - Doppler Applications 15 JULY 2020Waqas SaeedNo ratings yet
- VASCULAR - Abdominal Aorta Duplex ScanDocument24 pagesVASCULAR - Abdominal Aorta Duplex ScanSophia Elinor MenesesNo ratings yet
- Normal Sizes and Other Aids (Radiology)Document16 pagesNormal Sizes and Other Aids (Radiology)nmb1986No ratings yet
- 10 Upper Extremity Mapping For Creation of Dialysis Access or Bypass Graft Updated 2019Document7 pages10 Upper Extremity Mapping For Creation of Dialysis Access or Bypass Graft Updated 2019Marisol MorenoNo ratings yet
- Natalya Master CardioDocument71 pagesNatalya Master CardioTaman Hoang100% (1)
- Renal Artery Doppler NsDocument15 pagesRenal Artery Doppler Nss0800841739No ratings yet
- Jo Boy With SOB 04202016Document25 pagesJo Boy With SOB 04202016sirrfsNo ratings yet
- Kuliah Blok GI Tract - USG Abd - September 2010Document65 pagesKuliah Blok GI Tract - USG Abd - September 2010Natallia BatuwaelNo ratings yet
- Portal Hypertension: Dr. Ravi Gadani MS, FmasDocument57 pagesPortal Hypertension: Dr. Ravi Gadani MS, FmasRaviNo ratings yet
- RV InfarctionDocument52 pagesRV InfarctionpraasdwianggaNo ratings yet
- Gi Bleed RadiologyDocument60 pagesGi Bleed RadiologyDINESHNo ratings yet
- CCPACatheter Basics 07 MedicineDocument44 pagesCCPACatheter Basics 07 MedicinerinbijoyNo ratings yet
- Imaging of The Porta HepatisDocument71 pagesImaging of The Porta Hepatisjskmkabongo100% (1)
- Cardiovascular Pathology: Professor Mircea BuruianDocument174 pagesCardiovascular Pathology: Professor Mircea BuruianDiana PopoviciNo ratings yet
- Liver: What Is TheDocument37 pagesLiver: What Is TheAnkur MandeliaNo ratings yet
- Cardiovascular Physiology DR AnjilaDocument167 pagesCardiovascular Physiology DR AnjilaJacob MasikaNo ratings yet
- 1001130 - 急診基礎超音波 (CV+Chest+MSK) @羅東博愛Document78 pages1001130 - 急診基礎超音波 (CV+Chest+MSK) @羅東博愛juice119No ratings yet
- Upper GI BleedingDocument15 pagesUpper GI BleedingShishir ShresthaNo ratings yet
- CTA For IMDocument46 pagesCTA For IMbsythaymdNo ratings yet
- Atlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosFrom EverandAtlas of 3D Transesophageal Echocardiography in Structural Heart Disease Interventions: Cases and VideosNo ratings yet
- MA 106: Linear Algebra Tutorial 1: Prof. B.V. Limaye IIT DharwadDocument4 pagesMA 106: Linear Algebra Tutorial 1: Prof. B.V. Limaye IIT Dharwadamar BaroniaNo ratings yet
- Practice For Mounting Buses & Joints-374561Document11 pagesPractice For Mounting Buses & Joints-374561a_sengar1No ratings yet
- BIF-V Medium With Preload: DN Value 130000Document2 pagesBIF-V Medium With Preload: DN Value 130000Robi FirdausNo ratings yet
- Skincare Routine Order Cheat SheetDocument10 pagesSkincare Routine Order Cheat SheetYel Salenga100% (3)
- End of Summer Course Test August 2021Document16 pagesEnd of Summer Course Test August 2021Thanh Nguyen vanNo ratings yet
- OPTCL-Fin-Bhw-12Document51 pagesOPTCL-Fin-Bhw-12Bimal Kumar DashNo ratings yet
- Solar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power GeneratorDocument4 pagesSolar Charge Controller: Solar Car Solar Home Solar Backpack Solar Boat Solar Street Light Solar Power Generatorluis fernandoNo ratings yet
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atDocument1 pageIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentNo ratings yet
- Integration ConceptDocument34 pagesIntegration ConceptJANELLA ALVAREZNo ratings yet
- Aquaculture Scoop May IssueDocument20 pagesAquaculture Scoop May IssueAquaculture ScoopNo ratings yet
- Principles Involved in Baking 1Document97 pagesPrinciples Involved in Baking 1Milky BoyNo ratings yet
- Tabla de Avances de AcesoriosDocument3 pagesTabla de Avances de AcesoriosPedro Diaz UzcateguiNo ratings yet
- GSD Puppy Training Essentials PDFDocument2 pagesGSD Puppy Training Essentials PDFseja saulNo ratings yet
- Raneem AlbazazDocument33 pagesRaneem AlbazazGordana PuzovicNo ratings yet
- DP November 2017 Examination Schedule en PDFDocument4 pagesDP November 2017 Examination Schedule en PDFSuperlucidoNo ratings yet
- 1F-Korean-Nami Mun - Miles From NowhereDocument4 pages1F-Korean-Nami Mun - Miles From NowhereNeil PatelNo ratings yet
- G10Mapeh Exam First QuaterDocument8 pagesG10Mapeh Exam First QuaterJonas LamcisNo ratings yet
- Water Filling MachineDocument15 pagesWater Filling Machinepallab D RozarioNo ratings yet
- Las Tech Drafting 3Q WKDocument13 pagesLas Tech Drafting 3Q WKClemenda TuscanoNo ratings yet
- Para Lec CombinedDocument83 pagesPara Lec CombinedClent Earl Jason O. BascoNo ratings yet
- ff2023 Web 0 0Document2 pagesff2023 Web 0 0khaing khantNo ratings yet
- Chapter 7: Protein Function Part I: Myoglobin and HemoglobinDocument27 pagesChapter 7: Protein Function Part I: Myoglobin and HemoglobineliNo ratings yet
- Colour FastnessDocument37 pagesColour FastnessSivakumar K100% (1)
- Chapter 7 Dopant Diffusion - IDocument32 pagesChapter 7 Dopant Diffusion - I강준호No ratings yet
- c270 KW NTA855G2 60 HZDocument31 pagesc270 KW NTA855G2 60 HZAhmad El KhatibNo ratings yet
- Optik: Original Research ArticleDocument6 pagesOptik: Original Research ArticlesimarpreetNo ratings yet
- Rectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Document4 pagesRectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Lintas LtiNo ratings yet
- List of Fatigue Standards and Fracture Standards Developed by ASTM & ISODocument3 pagesList of Fatigue Standards and Fracture Standards Developed by ASTM & ISOSatrio Aditomo100% (1)
- Quartile1 PDFDocument2 pagesQuartile1 PDFHanifah Edres DalumaNo ratings yet
- Wcdma Idle Mode (Ericsson)Document29 pagesWcdma Idle Mode (Ericsson)Hosein ShahbaziNo ratings yet