Professional Documents
Culture Documents
2021 - Neuromuscular Disorders in The Intensive Care Unit
Uploaded by
Olga Manco GuzmánOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2021 - Neuromuscular Disorders in The Intensive Care Unit
Uploaded by
Olga Manco GuzmánCopyright:
Available Formats
REVIEW ARTICLE
Neuromuscular Disorders
C O N T I N UU M A UD I O
I NT E R V I E W A V AI L A B L E
ONLINE
in the Intensive Care Unit
By Torrey Boland Birch, MD
ABSTRACT
PURPOSE OF REVIEW: Thisarticle discusses the pathophysiology, presentation,
diagnosis, treatment, and prognosis of common neuromuscular disorders
seen in the intensive care unit, including Guillain-Barré syndrome,
myasthenia gravis, and intensive care unit–acquired weakness.
RECENT FINDINGS: Guillain-Barré syndrome can have an excellent prognosis if
patients are diagnosed early, appropriately treated, and monitored for
complications, including respiratory failure and dysautonomia. Intensive
care unit–acquired weakness increases overall mortality in patients who
are critically ill, and distinguishing between critical illness myopathy and
critical illness polyneuropathy may have important prognostic
implications.
SUMMARY: Neuromuscular disorders are not rare in the intensive care unit
setting, and precise identification and treatment of these conditions can
greatly impact long-term outcomes.
INTRODUCTION
P
atients with neuromuscular disorders are at high risk for respiratory
failure and other complications, including infection and
CITE AS:
CONTINUUM (MINNEAP MINN)
dysautonomia, that require aggressive treatment in the intensive care
2021;27(5, NEUROCRITICAL CARE): unit (ICU). Myasthenia gravis (MG) and Guillain-Barré syndrome
1344–1364.
(GBS) are two of the most common causes of neuromuscular
respiratory failure seen in the ICU; in one study, MG accounted for up to 32% of
Address correspondence to
Dr Torrey Boland Birch, 1725 W patients presenting with respiratory failure and GBS accounted for just under
Harrison St, Ste 1106, Chicago, 15%.1 Early identification and awareness of potential complications can
IL 60026, Torrey_birch@rush.edu.
significantly mitigate morbidity and mortality,1 and with aggressive treatment,
RELATIONSHIP DISCLOSURE: many patients can experience a significant recovery. Neurologists should be
Dr Birch serves on an advisory familiar with the diagnosis, treatment, and prognosis of GBS and MG and can
board for Gift of Hope Organ &
Tissue Donor Network and has help the ICU team, the patient, and family members anticipate both
served as a consultant for the complications and the overall course of the disease. In addition, as improvements
legal firm Rhoades McKee PC. in critical care are leading to an increasing number of survivors of prolonged
UNLABELED USE OF hospitalizations, neurologists should be familiar with the complications of critical
PRODUCTS/INVESTIGATIONAL illness, including ICU-acquired weakness.
USE DISCLOSURE:
Dr Birch reports no disclosure.
GUILLAIN-BARRÉ SYNDROME
© 2021 American Academy
GBS is an acute monophasic polyradiculoneuropathy that is immune mediated
of Neurology. and characterized by ascending flaccid paralysis and areflexia accompanied by
1344 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
CSF findings of albuminocytologic dissociation, which is the finding of an KEY POINTS
elevated protein level in the absence of an elevated cell count. The eponym
● Guillain-Barré syndrome
Guillain-Barré has persisted since the description in 1916 by Guillain, Barré, and (GBS) has three
Strohl2 of patients with an ascending flaccid paralysis. Landry had previously phenotypical variants:
described a similar disease over 50 years earlier, and in recognition of this, the purely demyelinating (acute
disease is occasionally referred to as Landry-Guillain-Barré syndrome. inflammatory demyelinating
polyradiculoneuropathy),
purely axonal (acute motor
Pathophysiology axonal neuropathy), and
The term GBS has come to encompass several variants of an immune-mediated demyelinating with an
polyradiculoneuropathy. The primary phenotypical variants are a purely axonal component.
demyelinating variant, a purely axonal variant, and a variant that is
● The primary targets in the
demyelinating with an axonal component.3 The demyelinating variant is referred acute motor axonal
to as acute inflammatory demyelinating polyradiculoneuropathy (AIDP), neuropathy phenotype of
whereas the axonal variant is referred to as acute motor axonal neuropathy GBS are the neuronal
(AMAN). Patients may also have involvement of the sensory nerves in the acute membrane gangliosides,
including GM1, GD1a, and
motor-sensory axonal neuropathy (AMSAN) subtype. Although all the subtypes GQ1b.
of GBS are antibody mediated, AIDP does not have identified antigens or
antibodies. Inflammation, activation of complement, and destruction of myelin, ● GBS begins with
however, support the hypothesis that the process is immune mediated. In ascending weakness,
typically initially involving
AMAN, the primary antigen targets are neuronal membrane gangliosides,
the proximal leg muscles,
particularly GM1, GD1a, and GQ1b on the axon itself. This leads to direct damage with diminished or absent
of the axon, the regeneration of which is slow and often incomplete. In contrast, reflexes.
the process of remyelination may occur more efficiently. For this reason, the
AMAN phenotype is associated with worse outcomes and longer recovery times
than the AIDP phenotype.
Significant molecular mimicry exists between the glycan present on
lipooligosaccharides of Campylobacter jejuni and the neuronal membrane
gangliosides GM1 and GD1a, which is the reason infection with C. jejuni can
trigger GBS, particularly the AMAN variant.3 Other infections can similarly
precede the onset of GBS, including cytomegalovirus, Epstein-Barr virus,
influenza A, Mycoplasma pneumoniae, Haemophilus influenzae, severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2), and Zika virus. GBS has
been reported after administration of the Semple rabies vaccine and several types
of influenza A virus vaccines, most notably the 1976 H1N1 influenza A vaccine.
More recent studies suggest a possible minimal increase in GBS cases with
influenza A vaccination, although this risk may be offset by the possibility of
GBS developing after infection with influenza A.4 The specific neuronal
membrane ganglioside GQ1b is the target in the Miller Fisher variant of GBS. An
association also appears to exist between recent surgery and GBS, although the
mechanism is unclear.5
Presentation
The classic presentation of GBS is one of ascending weakness and areflexia, often
following an infection or other immune stimulus. More than two-thirds of
patients with GBS will report respiratory or gastrointestinal symptoms in the
4 weeks before symptom onset (CASE 7-1).6 Pain may precede the development
of weakness and is commonly described in the back, buttocks, and thighs. The
pain is often described as aching or throbbing and may also be described as a
tight, crampy sensation. Patients frequently report paresthesia, particularly in
the fingers and toes, although objectively their sensation is often preserved.
CONTINUUMJOURNAL.COM 1345
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
CASE 7-1 A 43-year-old previously healthy woman presented to the emergency
department for evaluation of lower extremity weakness. She reported an
acute onset of diarrhea 7 days earlier. Several days later, she developed
worsening fatigue, back pain, and painful paresthesia of the legs, which
progressed to difficulty climbing stairs. The following day, she was
unable to rise from a chair and noted mild weakness in her arms.
On arrival, the patient was afebrile, with mild tachycardia and
tachypnea. Blood pressure and oxygen saturation were within normal
limits. General medical examination was unremarkable. On neurologic
examination, mentation and cranial nerve examination were normal. The
patient was noted to have symmetric weakness of the legs, proximally
more so than distally. She had mild symmetric proximal weakness in the
arms. Sensation was normal. Reflexes were absent.
The patient was admitted to the intensive care unit (ICU) for close
monitoring of her respiratory status. Given concern for Guillain-Barré
syndrome (GBS), a lumbar puncture was performed, which revealed only
elevated protein. Bedside pulmonary function testing showed a
borderline low forced vital capacity of 45 mL/kg, maximal inspiratory
pressure of -40 cm H2O, and a maximal expiratory pressure of 50 cm H2O.
Several hours later, the patient developed a paradoxical breathing
pattern. Repeat pulmonary function testing showed a decline in values,
with a forced vital capacity of 20 mL/kg, maximal inspiratory pressure of
-25 cm H2O, and a maximal expiratory pressure of 40 cm H2O. Arterial
blood gas was normal. At that time, the patient was intubated.
Over the next 24 hours, the patient progressed to a flaccid
quadriparesis. IV immunoglobulin (IVIg) 0.4 g/kg/d was started, with a
planned 5-day course. EMG was performed, which showed diffusely
absent motor responses consistent with acute motor axonal neuropathy
(AMAN). Blood work showed the presence of GD1a antibodies, although
this test did not result until day 5 of admission.
The patient was noted to have several episodes of labile blood
pressure and heart rate, which slowly improved during her hospitalization
and were treated supportively. She continued to require full respiratory
support at 7 days, and tracheostomy was performed. She remained in the
ICU for an additional 2 weeks because of autonomic instability.
Ultimately, the patient’s blood pressure stabilized, and she was
discharged to a neurorehabilitation and ventilator weaning facility. One
year later, she returned to clinic ambulating, with her tracheostomy
decannulated. She had returned to work part-time.
COMMENT This patient presented with the AMAN variant of GBS, with positive GD1a
antibodies. Given her rapid progression, respiratory failure, and axonal
phenotype, early tracheostomy was required. Despite the severity of the
disease, many survivors of GBS can ultimately have a nearly full recovery.
1346 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Weakness tends to start in the proximal legs and ultimately can progress to KEY POINTS
involve the arms, diaphragm, and cranial nerves. Patients often describe
● Symptoms in GBS
difficulty climbing stairs or rising from chairs. Reflexes are absent or diminished, typically reach maximal
although early on they may be preserved. The disease is monophasic, and severity within 2 weeks, and
typically the maximal weakness is reached within 2 weeks of the initial progression beyond 4 weeks
neurologic symptoms. Symptoms are unlikely to progress after 4 weeks; should raise concern for an
alternative diagnosis.
additional progression at that point should raise concern for an alternative
diagnosis, such as chronic inflammatory demyelinating polyradiculoneuropathy ● Autonomic dysfunction
(CIDP). In 20% to 30% of cases, progression of weakness leads to respiratory occurs in more than
failure requiring mechanical ventilation.7 one-third of patients with
Autonomic dysfunction is common in GBS as well, occurring in 38% of GBS and is related to
demyelination of
patients in one large study, with an increased incidence in patients requiring sympathetic nerves and
mechanical ventilation (odds ratio 6.93 [3.39-14.15]).8 This is likely caused by disruption of the baroceptor
demyelination of sympathetic nerves and disruption of the baroreceptor reflexes.
reflexes.9 The most common symptoms are ileus, hypertension, hypotension,
● The Miller Fisher variant
fever, tachycardia, and bradycardia. Patients with more severe disease, including of GBS presents with cranial
those with quadriparesis, bulbar and neck flexor weakness, and respiratory nerve dysfunction, ocular
failure, are more likely to manifest dysautonomia. motor weakness, and bulbar
Aside from the classic presentation, several clinical variants of GBS are well symptoms. It is associated
with antibodies against GQ1b
described. The most common is Miller Fisher syndrome (also referred to as
and is less likely to progress
Fisher syndrome), with cranial nerve dysfunction including facial weakness, to respiratory failure than
ocular motor weakness, and bulbar symptoms. Patients may also have ataxia, more classic forms of GBS.
sensory signs, and dysautonomia. This variant can progress to involve the limbs
as well, which can be referred to as an overlap syndrome and may have a course ● The diagnosis of GBS is
clinical, with progressive
more typical of the classic forms of GBS. Patients with pure Miller Fisher weakness and decreased
syndrome are less likely to need mechanical ventilation; however, those with the reflexes as key features.
overlap syndrome may require mechanical ventilation earlier than patients with Supportive features include
a more typical form of GBS.10 Miller Fisher syndrome is associated with albuminocytologic
dissociation in the CSF and
anti-GQ1b antibodies, which are located on the ocular motor nerves and in the electrophysiologic testing
brainstem, which accounts for the presentation of symptoms. Pharyngeal- consistent with either
brachial and paraparetic variants of GBS also exist, for which the target antigens demyelination or axonal
are not yet known. injury.
Diagnosis
The diagnosis of GBS is primarily clinical, based on the patient’s history,
clinical presentation, and physical examination. Supportive studies include
CSF analysis, electrophysiologic studies including nerve conduction studies
and EMG, and antibody testing. Standardized diagnostic criteria were
proposed by the National Institute of Neurological Disorders and Stroke
(NINDS) and have been modified since their introduction in 1978; however,
these criteria may miss variants such as Miller Fisher syndrome (TABLE 7-1).11
The two required features for diagnosis include progressive weakness of the
legs and arms (occasionally only in legs initially) and areflexia or decreased
tendon reflexes in the affected limbs. Additional supportive features include a
progressive phase lasting up to 4 weeks, relative symmetry, mild sensory
symptoms, cranial nerve involvement, autonomic dysfunction, and pain. The
Brighton Collaboration criteria are more stringent diagnostic criteria used for
research purposes that include the NINDS criteria as well as albuminocytologic
dissociation in the CSF in addition to electrophysiologic findings consistent with
GBS for diagnostic certainty.7
CONTINUUMJOURNAL.COM 1347
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
EMG is not required for diagnosis but can be helpful in determining the
phenotype (AIDP or AMAN), which may be helpful for prognosis. Appropriate
workup should be done to exclude alternative causes based on the clinical
examination. Other conditions that may present similarly include MG, botulism,
West Nile virus, organophosphate poisoning, tick paralysis, porphyria,
transverse myelitis and other causes of myelopathy, and vasculitic neuropathies
(TABLE 7-2). A leukocytosis in the CSF, fever at onset, sensory level, asymmetry,
persistent bowel and bladder dysfunction, respiratory failure in the absence of
limb weakness, and prolonged progression of symptoms should raise concern for
an alternative diagnosis. Spinal imaging should be done in the setting of acute
TABLE 7-1 Diagnostic Criteria for Guillain-Barré Syndromea
Features required for diagnosis
◆ Progressive bilateral weakness of arms and legs (initially only legs may be involved)
◆ Absent or decreased tendon reflexes in affected limbs (at some point in clinical course)
Features that strongly support diagnosis
◆ Progressive phase lasts from days to 4 weeks (usually <2 weeks)
◆ Relative symmetry of symptoms and signs
◆ Relative mild sensory symptoms and signs (absent in pure motor variant)
◆ Cranial nerve involvement, especially bilateral facial palsy
◆ Autonomic dysfunction
◆ Muscular or radicular back or limb pain
◆ Increased protein level in CSF; normal protein levels do not rule out the diagnosis
◆ Electrodiagnostic features of motor or sensorimotor neuropathy
Features that cast doubt on diagnosis
◆ Increased numbers of mononuclear or polymorphonuclear cells in CSF
◆ Marked persistent asymmetry of weakness
◆ Bladder or bowel dysfunction at onset or persistent during disease course
◆ Severe respiratory dysfunction with limited limb weakness at onset
◆ Sensory signs with limited weakness at onset
◆ Fever at onset
◆ Nadir <24 hours
◆ Sharp sensory level indicating spinal cord injury
◆ Hyperreflexia or clonus
◆ Extensor plantar responses
◆ Abdominal pain
◆ Slow progression with limited weakness without respiratory involvement
◆ Alteration of consciousness
CSF = cerebrospinal fluid.
a
Modified from Leonhard SE, et al, Nat Rev Neurol.11 © 2019 The Authors.
1348 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Differential Diagnosis of Rapidly Progressive Weaknessa TABLE 7-2
Central nervous system
◆ Encephalitis
◆ Acute disseminated encephalomyelitis (ADEM)
◆ Transverse myelitis and other causes of myelopathy
◆ Brainstem compression
◆ Leptomeningeal malignancy
Motor neuron
◆ Poliomyelitis
◆ West Nile virus anterior myelitis
◆ Rabies
◆ Amyotrophic lateral sclerosis
◆ Progressive spinal muscular atrophy
Peripheral nerve
◆ Guillain-Barré syndrome
◆ Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP)
◆ Critical illness neuropathy
◆ Vasculitis
◆ Diphtheria
◆ Porphyria
◆ Tick paralysis
◆ Heavy metal toxicity
Neuromuscular junction
◆ Myasthenia gravis
◆ Lambert-Eaton myasthenic syndrome
◆ Botulism
◆ Organophosphate intoxication
Muscles
◆ Critical illness myopathy
◆ Mitochondrial disease
◆ Acute rhabdomyolysis
◆ Polymyositis
◆ Dermatomyositis
◆ Medication-induced myopathy
◆ Metabolic/electrolyte disorders
a
Data from Willison HJ, et al, Lancet4 and Leonhard SE, et al, Nat Rev Neurol.11
CONTINUUMJOURNAL.COM 1349
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
onset of symptoms, a sensory level, or hyperreflexia, or when the weakness is
asymmetric. In some cases, brain imaging may be helpful to exclude brainstem
pathology as the cause of the weakness. MRI of the spine with gadolinium can be
helpful but is not required in the diagnosis of GBS, as enhancement of the nerve
roots is a sensitive but nonspecific finding in GBS.11 The presence of
antiganglioside antibodies or evidence of recent infection, such as C. jejuni, may
increase the diagnostic certainty but is not required for diagnosis.
West Nile virus, which emerged in North America in 1999, can result in an
acute flaccid paralysis syndrome termed West Nile poliomyelitis that may mimic
GBS. This results from infection of the anterior horn cells of the spinal cord. This
may or may not be accompanied by an encephalitis. The weakness is typically
asymmetric and may cause weakness of one limb, although in more severe cases,
patients can develop quadriplegia and acute neuromuscular respiratory failure.
As compared to GBS, patients with West Nile poliomyelitis more often have
fever, absent sensory symptoms, and a pleocytosis along with elevated protein in
the CSF.12
Porphyric neuropathy can also mimic GBS by causing both progressive
weakness and autonomic dysfunction. The acute hepatic porphyrias are most
likely to cause neurologic manifestations and are inherited or acquired disorders
of heme synthesis. Acute intermittent porphyria, an autosomal dominant
condition with low penetrance, is the most common of the acute hepatic
porphyrias. Patients are often healthy young women presenting with fatigue,
abdominal pain, nausea, and subtle neurologic signs that could include
weakness.13 Seizures and psychosis are common. During an acute attack, a
combined sensory and motor neuropathy can develop, and the autonomic
nervous system can be affected as well. Weakness often begins in the proximal
muscles, and the severity is highly variable, ranging from mild sensory
symptoms to involvement of the cranial nerves or progression to
quadriparesis and respiratory failure. The diagnosis can be confirmed by
measuring porphobilinogen in the urine. For additional mimics of GBS,
refer to TABLE 7-2.
Treatment
Although supportive treatment of patients with GBS is critical, particularly in the
setting of acute respiratory failure, both plasma exchange and IV
immunoglobulin (IVIg) have been proven to be effective at reducing the length
of time patients require mechanical ventilation and to lead to faster recovery.14,15
The American Academy of Neurology’s quality measurement set on inpatient
and emergency care for patients with neurologic illnesses aims to improve timely
treatment of patients with GBS and states that patients admitted to an inpatient
facility with GBS who are nonambulatory should be treated with
immunosuppressive therapy using plasma exchange or IVIg and not prescribed
corticosteroids.16 Combination therapy, such as plasma exchange followed by
IVIg, is not more effective than monotherapy.17 In addition, no clear evidence
indicates that a second course of IVIg is helpful, although further study may be
needed. An observational study of 237 patients did not show better outcome with
a second course of IVIg in patients with a predicted poor prognosis; however, the
study was limited by small numbers and by the fact that the patients receiving a
second course were more disabled than those receiving only a single course.18 No
role exists for administration of corticosteroids.
1350 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Intensive Care Unit Management KEY POINTS
Patients with GBS should be managed in the ICU when they have rapidly
● Plasma exchange and IV
progressive weakness, evidence of bulbar weakness, autonomic dysfunction, or immunoglobulin are equally
concern for impending respiratory failure. As many patients with GBS may effective in the treatment of
present to the medical ICU setting, a consulting neurologist can help guide the GBS. No evidence suggests
ICU team through the expected time course of respiratory failure and educate the that the combination of the
two treatments is more
team to anticipate autonomic dysfunction. As discussed later in this article, the
effective than monotherapy.
neurologist may also assist with goals-of-care discussions and help to advise on Steroids are not
the need for early tracheostomy in patients with severe weakness who are not recommended.
expected to regain enough strength to successfully wean from mechanical
ventilation in the short term. The Erasmus GBS Respiratory Insufficiency Score ● The 20/30/40 rule guides
intubation in GBS; forced
(EGRIS) is a tool that calculates the probability that a patient will require vital capacity less than
mechanical ventilation within 1 week of assessment (gbstools.erasmusmc. 20 mL/kg, maximal
nl/prognosis-tool). The main predictors are length of time between onset of inspiratory pressure less
weakness and hospital admission, facial and/or bulbar weakness at hospital than 30 cm H2O, or maximal
expiratory pressure less
admission, and Medical Research Council (MRC) sum score at hospital than 40 cm H2O suggests the
admission.19 If the patient is in clear respiratory failure, they should be need for mechanical
immediately intubated; however, even well-appearing patients should be ventilation.
monitored with objective respiratory measurements, including forced vital
capacity, maximal inspiratory pressure (MIP), and maximal expiratory
pressure (MEP). Alternatively, clinicians can ask patients to count during the
expiration of one full inspiratory effort breath to provide a measurement to
follow, although this value may vary from patient to patient depending on the
speed by which the individual counts. It may be more useful to track trends in
an individual patient. A forced vital capacity less than 20 mL/kg, MIP less than
30 cm H2O, or MEP less than 40 cm H2O should be used as cutoffs to guide
intubation. This is often referred to as the 20/30/40 rule. Although arterial blood
gases may be trended, hypercarbia and hypoxemia are late findings in the
respiratory failure associated with GBS. Patients may also exhibit a paradoxical
breathing pattern in which the abdominal wall moves inward on inspiration.
In typical respiration patterns, the abdomen moves outward on inspiration as
the diaphragm contracts and moves downward, displacing the abdominal
contents outward. When patients have weakness of the diaphragm, the
abdominal muscles may contract on inspiration to assist the expansion of the
chest (FIGURE 7-120). Patients who are not intubated should be carefully
screened for bulbar weakness and should have their ability to swallow assessed
before allowing them to take food or medications orally. Some early predictors of
respiratory failure include a short (<7 days) time course from symptom onset to
admission, inability to cough, inability to stand, inability to lift the elbows or
head, or elevated liver enzymes.21 Patients with these findings should be
monitored in the ICU for the development of respiratory failure.
Patients showing signs of respiratory failure should be intubated rather
than treated with noninvasive ventilation, as the respiratory failure is unlikely
to quickly reverse. Noninvasive ventilation also poses a high risk for aspiration
in those with bulbar weakness. Although the optimal timing of intubation in
GBS remains unclear, it is reasonable to intubate patients early and in a
controlled setting to avoid complications such as anoxic injury from sudden
respiratory or cardiac arrest.22 However, a randomized trial showed no
significant difference in the incidence of pneumonia, length of stay, neurologic
scores, need for tracheostomy, in-hospital death, or any serious adverse
CONTINUUMJOURNAL.COM 1351
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
FIGURE 7-1
Graphic illustration of paradoxical breathing pattern. A, Diaphragm at rest. B, Normal
diaphragm movement during inspiration resulting in expansion of the chest and abdomen. C,
Paradoxical breathing pattern (inward abdominal movement during inspiration) because of
diaphragmatic weakness.
Reprinted with permission from Wijdicks EFM, Oxford University Press.20 © 2012 Mayo Foundation for
Medical Education and Research.
events between patients randomly assigned to early intubation compared to
conventional care.23
Because of the prolonged nature of respiratory failure in patients with GBS,
tracheostomy is often necessary. The decision to proceed with tracheostomy in a
patient with severe GBS may occur early, particularly in patients with the AMAN
variant as they have a protracted recovery. Some predictors of prolonged
mechanical ventilation include the inability to lift the arms at 1 week and
evidence of axonal degeneration.24
Autonomic dysfunction associated with GBS often requires close attention in
the ICU. Severe hypertension can lead to cardiac complications and additional
neurologic complications, such as posterior reversible encephalopathy
syndrome (PRES).8 Patients may also develop the syndrome of inappropriate
secretion of antidiuretic hormone (SIADH), likely related to fluctuating
catecholamines.8 Although dysautonomia is common, clinicians should continue
to monitor for alternative causes of symptoms, such as fever, hypotension, and
hypertension, as secondary infection, pain, and other causes can all occur in
patients in the ICU. Clinicians should avoid long-acting blood pressure
medications and rapid fluctuations in blood pressure in patients with
dysautonomia.
Given the prolonged nature of severe GBS with respiratory failure,
high-level ICU care, including frequent turning and repositioning to prevent
skin breakdown, chemoprophylaxis for deep vein thrombosis, sequential
compression devices, adequate nutrition, stress ulcer prophylaxis, and early
mobilization with physical therapy are crucial. Patients with GBS have a 3% to
7% risk of pulmonary embolism, and prophylaxis against deep vein
1352 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
thrombosis is key to preventing this complication. The Neurocritical Care KEY POINTS
Society suggests combining pharmacologic and mechanical venous
● Patients with GBS have
thromboembolism prophylaxis in patients with neuromuscular disease and preserved consciousness
continuing venous thromboembolism prophylaxis until the ability to and should be assessed and
ambulate returns.25 For patients with prolonged immobilization, hand splints treated for pain, anxiety,
and pressure relief ankle-foot orthotics may be used to prevent contractures. and depression.
Ileus is the most common manifestation of dysautonomia8; patients should be
● Most survivors of GBS will
prophylactically treated with a bowel regimen, and their abdominal regain the ability to walk,
examination should be monitored closely. It should be emphasized that although recovery can take
patients with GBS have preserved consciousness despite their inability to more than a year.
respond to commands because of profound weakness. Appropriate pain
management for procedures should always be implemented, and patients
should be spoken to and updated regarding their condition. Most patients with
GBS do recover, and this should be emphasized to them. Antidepressant
medications may be appropriate, and, as patients are able to communicate,
they should be screened for depression as well as pain.
Prognosis
More than 80% of patients with GBS will recover to the point of regaining the
ability to ambulate at 6 months.7 Patients with axonal involvement,
dysautonomia, and respiratory failure requiring mechanical ventilation are
more likely to have a poor outcome. The rate of mortality in GBS has been
described in the range of 2% to 12%, most often from pulmonary
complications or autonomic dysfunction in the acute phase of the illness4;
however, as ICU care has improved, mortality has decreased. Recent studies
have described a mortality rate of 6% in patients with dysautonomia
compared to a 2% mortality overall,8 although an older study found a
mortality rate as high as 20% in patients requiring mechanical ventilation.26
Of the survivors, nearly 80% of patients requiring mechanical ventilation
went on to walk independently at 1 year. Recovery may be lengthy, with
progress continuing 12 months after the disease onset. Patients requiring
mechanical ventilation are more likely to have a prolonged recovery course.
Because of the significant recovery most patients see, clinicians should
treat GBS aggressively and ensure that all patients receive high-level ICU
care to avoid preventable complications that may increase morbidity
and mortality.
Future Trends
The International Guillain-Barré Syndrome Outcome Study, which was started
in 2012, should provide a valuable data set to help to further characterize
epidemiology, antecedent events, and long-term outcomes in GBS.27 As new
infections emerge across the globe, additional triggers of GBS may be identified
that require further investigation. Recent descriptions of GBS occurring after
infection with SARS-CoV-2 and the Zika virus indicate that the incidence of cases
could vary as new infection patterns emerge.28
MYASTHENIA GRAVIS
MG is an autoimmune disorder affecting the postsynaptic membrane of the
neuromuscular junction. Patients may present with fluctuating weakness of the
ocular, bulbar, limb, and respiratory muscles. In more severe cases, respiratory
CONTINUUMJOURNAL.COM 1353
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
function can be compromised because of weakness of either the muscles of
respiration or the bulbar muscles that work to protect the airway.
Pathophysiology
In MG, autoantibodies bind to the acetylcholine receptor (AChR) or related
proteins, which leads to weakness of skeletal muscles. Antibodies most
commonly bind directly to the AChR, although variants of MG exist in which
antibodies to muscle-specific tyrosine kinase (MuSK) or lipoprotein
receptor-related protein 4 (LRP4) are found.29 Treatment of MG is directed at
improving the availability of acetylcholine at the synapse through the use of
acetylcholinesterase inhibitors and immunosuppressive drug therapy.
MG can occur at any age; however, it appears to have a bimodal distribution.29
The age of 50 years is used as a cutoff to describe early-onset MG as compared to
late-onset MG. Early-onset MG is more likely to affect women, whereas
late-onset MG is slightly more common in men. Patients with early-onset MG are
more likely to have thymic hyperplasia, and many patients have additional
autoimmune conditions, including thyroiditis, systemic lupus erythematosus, or
rheumatoid arthritis. One-third of patients with a thymoma will develop MG. In
addition, an association exists between MG and neuromyelitis optica (NMO) as
well as between MG and amyotrophic lateral sclerosis.29
Diagnosis
For patients without a prior diagnosis of MG, a careful history may increase
suspicion for the disease. Significant delays often occur in the diagnosis of MG.
One study reported that although 57% of patients were diagnosed within 1 year of
onset of symptoms, 13% of patients had a delay of greater than 5 years.30 A detailed
neurologic examination often reveals some degree of ocular or facial weakness.
In this setting, confirmation of the diagnosis with additional testing should be
pursued. Immunologic testing for AChR, MuSK, and LRP4 should be obtained.
Of patients with MG, 10% to 15% will be antibody negative. The ice pack test can
be performed at the bedside in patients with ptosis. In this test, after ptosis is
observed, an ice pack is laid on the closed lid for 2 minutes. The patient is
reexamined immediately after removal to assess for improvement in the ptosis.
Improvement suggests a disorder of neuromuscular transmission, as the activity
of acetylcholinesterases is decreased at lower temperatures. Electrodiagnostic
testing can also aid in diagnosis. The presence of decremental responses on
repetitive nerve stimulation can provide physiologic support for the diagnosis
when moderate or greater generalized weakness is present (FIGURE 7-2). Single-
fiber EMG is more sensitive than repetitive nerve stimulation but is less specific
(can be abnormal in disorders such as botulism, amyotrophic lateral sclerosis,
and rapidly progressive polyneuropathies). It is a technically challenging
procedure and is rarely achievable in the critical care setting.
All patients with newly diagnosed MG should undergo CT examination of the
chest. MG has a strong association with thymoma, and this should be treated with
thymectomy. Guidelines for the indications for elective thymectomy in MG have
been published.31,32
The biggest threat to patients with MG is the development of a life-threatening
crisis that compromises respiratory function because of weakness of the muscles
of respiration or the bulbar muscles. A 2016 consensus statement defined the
terms impending myasthenic crisis and manifest myasthenic crisis.33 Impending
1354 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
● Myasthenia gravis is an
autoimmune disorder with
antibodies targeting the
postsynaptic membrane of
the neuromuscular junction,
including the acetylcholine
receptor, muscle-specific
tyrosine kinase, and
lipoprotein receptor-
related protein 4.
● Twenty percent of
patients present in
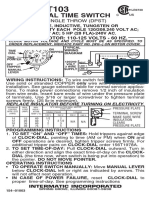
FIGURE 7-2
myasthenic crisis as the first
Repetitive nerve stimulation of the spinal accessory nerve in a patient with myasthenia gravis.
manifestation of their
This nerve conduction study shows a decremental compound muscle action potential
disease.
(CMAP) response of greater than 10% of the trapezius muscle while stimulating the spinal
accessory nerve on repetitive stimulation at 3 Hz, consistent with a disorder of
neuromuscular transmission such as myasthenia gravis. ● Myasthenic crisis can be
Figure courtesy of Ryan Jacobson, MD. triggered by infection;
medications such
aminoglycosides,
fluoroquinolones, and
beta-blockers; and surgery.
myasthenic crisis is defined as “rapid clinical worsening that, in the opinion of
the treating physician, could lead to crisis in the short term (days to weeks).”33 ● Immune checkpoint
Manifest myasthenic crisis is defined as “worsening of myasthenic weakness inhibitors may induce an
requiring intubation or noninvasive ventilation to avoid intubation, except when immune-related myasthenia
gravis in patients without a
these measures are employed during routine postoperative management.”33 Both history of myasthenia gravis.
conditions should be treated in the inpatient setting, typically in the ICU.
Presentation
Most patients who present with myasthenic crisis have a known diagnosis of MG,
although up to 20% of patients will present to medical attention for the first time
in crisis (CASE 7-2).34,35 Patients with a known diagnosis of MG may give a history
of worsening systemic and/or bulbar weakness, although, rarely, respiratory
failure can be the only symptom. Because of generalized weakness, patients may
not manifest typical signs of respiratory distress, including use of accessory
muscles. Of concern, the clinical picture can also be muddled by the escalation of
dosing of anticholinesterase medications, which may precipitate a cholinergic
crisis, with increased salivation, gastrointestinal symptoms, and, ultimately,
worsening muscle weakness.
Myasthenic crises can be triggered by several factors, including infection,
medications, and surgery. The most common cause is a simultaneous infection,
and a workup should be initiated to exclude an underlying infection in patients
presenting in crisis.36 Numerous medications can worsen weakness in patients
with MG (TABLE 7-3), and a comprehensive list can be found on the website of
the Myasthenia Gravis Foundation of America (myasthenia.org/what-is-mg/
MG-management/cautionary-drugs).37 Aminoglycosides, fluoroquinolones, and
beta-blockers are common offenders. The US Food and Drug Administration
(FDA) has issued boxed warnings against the use of fluoroquinolones and for the
antibiotic telithromycin (no longer available in the United States) in MG. In
addition, reports exist of immune checkpoint inhibitors triggering an
immune-related MG.38 These drugs are used in the treatment of melanoma,
CONTINUUMJOURNAL.COM 1355
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
non–small cell lung carcinoma, and other malignancies. They can worsen
symptoms of individuals with existing MG as well as lead to a new diagnosis of
MG in patients who did not previously have the disorder. As soon as a crisis is
identified, medication lists should be reviewed and offending agents should be
discontinued. In addition, patients with a known history of MG who are
receiving cautionary drugs should be monitored closely or switched to an
alternative agent, if possible.
Once concern exists for impending or manifest myasthenic crisis, the patient’s
respiratory status should be monitored closely. As in patients with GBS, forced
vital capacity, MIP, and MEP should be monitored closely, and it is reasonable to
use the same cutoffs as described earlier to guide intubation, although evidence
for these cutoffs is limited. However, given the fluctuating nature of the
weakness, clinicians should use caution in relying solely on those parameters to
CASE 7-2 A 54-year-old man presented to the emergency department with fever,
shortness of breath, and poor appetite. A chest x-ray showed an infiltrate
in the left lower lobe consistent with pneumonia, and the patient was
started on levofloxacin. He developed worsening respiratory failure and
was intubated and admitted to the medical intensive care unit. Despite
treatment of the pneumonia, the patient was unable to pass his
spontaneous breathing trials because of low lung volumes. The internal
medicine resident noted a left ptosis that seemed to vary in severity
throughout the day and consulted the neurology team.
A detailed history from the family revealed that the patient had been
intubated 4 times in the past 2 years in the setting of minor infections,
each time with difficulty weaning from the ventilator. The family reported
that over the past 2 years, the patient appeared fatigued throughout the
day, worse in the evening. They reported that they occasionally noted
ptosis, but it typically resolved within a day. At the bedside, the
neurology resident placed a cold ice pack on the left eye and waited for
2 minutes. After lifting the pack, the patient’s ptosis had resolved.
Repetitive nerve stimulation was performed, showing a decremental
response of greater than 10%, consistent with myasthenia gravis (MG).
Serum antibodies were sent, and the patient was positive for antibodies
against the acetylcholine receptor. He was started on plasma exchange
and steroids, and his antibiotic was changed to ceftriaxone. Ultimately,
he did well and was extubated 10 days later.
COMMENT This case demonstrates the difficulty in making a diagnosis of MG. This
patient had been intubated 4 times in the recent past, but each time the
diagnosis was missed as his symptoms improved with treatment of the
underlying infection. Only when a detailed history and examination was
performed was MG considered in the differential diagnosis. In this case,
the patient’s pulmonary infection in combination with the administration of
a fluoroquinolone triggered a myasthenic crisis.
1356 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
guide respiratory management. In addition, prominent bulbar symptoms leading
to inability to manage secretions are an indication for intubation. Noninvasive
ventilation may be used in patients with minimal bulbar symptoms who are able
to manage their secretions. This strategy may prevent intubation, particularly in
those with less severe symptoms.35,39
Treatment
In an exacerbation of myasthenic symptoms, early initiation of rapid short-acting
immunotherapy should occur with either IVIg or plasma exchange. No clear
evidence supports one treatment over the other40; however, several studies have
suggested that plasma exchange may have a more rapid effect, leading to fewer
intubations35 and earlier extubation.41 In a consensus statement, the Myasthenia
Gravis Foundation of America suggests that although the two treatments are
likely equally effective based on available evidence and should be chosen based
on clinical patient characteristics, plasma exchange may be more effective and
has a faster effect.33 This statement is based on consensus expert opinion. Patients
with high risk of a hypercoagulable state or renal failure should avoid IVIg, as
Cautionary Drugs in Myasthenia Gravisa TABLE 7-3
Drugs with US Food and Drug Administration (FDA) boxed warnings for use in myasthenia
gravis
◆ Telithromycin (no longer available in the United States)
◆ Fluoroquinolones (ciprofloxacin, moxifloxacin, levofloxacin)
Drugs to use with caution, if at all, in myasthenia gravis
◆ Botulinum toxin
◆ D-penicillamine
◆ Chloroquine
◆ Hydroxychloroquine
◆ Quinine
◆ Magnesium
◆ Macrolide antibiotics (erythromycin, azithromycin, clarithromycin)
◆ Aminoglycoside antibiotics (gentamicin, neomycin, tobramycin)
◆ Corticosteroidsb
◆ Procainamide
◆ Desferrioxamine
◆ Beta-blockers
◆ Statins
◆ Immune checkpoint inhibitors (pembrolizumab, nivolumab, atezolizumab, avelumab,
durvalumab, ipilimumab)
a
Data from Myasthenia Gravis Foundation of America.37
b
Corticosteroids may cause transient worsening of symptoms in the first 2 weeks but are part of the
standard treatment for myasthenia gravis. Close monitoring should be in place when initiating steroids.
CONTINUUMJOURNAL.COM 1357
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
IVIg may precipitate thromboembolic events and can lead to acute kidney injury.
Patients with a history of multiple cardiovascular risk factors have an increased
risk for thromboembolic events, as do those with malignancy, hyperviscosity,
hereditary hypercoagulable states, and prior thromboembolic events. Acute
kidney injury following IVIg is more common in patients with preexisting
chronic kidney disease. Those with high risk for hemodynamic instability, such
as sepsis, recent hemorrhage, or hypotension, should avoid plasma exchange as
the procedure could precipitate further hypotension and may lead to coagulation
factor depletion, increasing the risk of bleeding. The administration of plasma
exchange often requires placement of a central venous catheter, which may
increase the risk of the procedure as well. IVIg is administered peripherally. The
American Academy of Neurology’s quality measurement standards advocate for
the administration of immunosuppressive therapies for patients admitted with
myasthenic crisis, stating that the decision between IVIg and plasma exchange
should be made based on availability, adverse effects, costs, and the patient’s
profile.16
Corticosteroids are an important part of the treatment of a myasthenic
crisis and should be used in most patients. Although high-dose steroids may
precipitate worsening weakness, administering them concurrently or several
days following plasma exchange or IVIg likely counteracts this effect. If a
patient is already intubated, the risks of beginning high-dose steroids are
lessened and they should be started immediately. Prednisone and
prednisolone are considered equally effective, and doses of 60 mg/d to
80 mg/d are recommended. On an outpatient basis, steroids are generally
given on alternate days to minimize side effects, but while patients are in the
ICU, daily administration is preferred. Once out of the crisis, steroids should
be tapered to the lowest effective dose. Consideration for steroid-sparing
immunosuppressant therapy will be needed. If patients in myasthenic crisis
are on baseline anticholinesterase therapy, it should be discontinued once the
patient is placed on mechanical ventilation to avoid complications. Although
no guidelines exist regarding the optimal timing to restart the medication, it is
reasonable to resume anticholinesterase therapy via nasogastric tube once the
patient’s respiratory status is improving and mechanical ventilation is being
weaned for potential extubation.42
As with GBS, high-level supportive ICU care is critical to ensuring good
outcomes, including early physical therapy, frequent turning, and appropriate
prophylaxis for deep vein thrombosis and gastric ulcers.
Prognosis
The mortality among patients with myasthenic crisis is estimated at 5% to 19%.35,43
In one large study of patients requiring mechanical ventilation for a myasthenic
crisis, the primary cause of death was multiorgan failure secondary to sepsis.35 In
this study, an estimated 20% of patients requiring mechanical ventilation still
required ventilatory support at the time of discharge. Risk factors for prolonged
mechanical ventilation include age, comorbidities such as pneumonia, high
disease burden, and late-onset MG.35,41 Higher preintubation CO2 was associated
with disability and death in another study.43 Extubation success can be difficult
to predict because of fluctuating symptoms, and failure can be as high as 40%.39
However, cough strength and MEP greater than 40 cm H2O may help to predict a
good outcome.39 Noninvasive ventilation may be helpful in supporting patients
1358 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
with a preserved cough following extubation, although the role of noninvasive KEY POINTS
ventilation is not clearly defined in this patient population.39 Patients who
● Fluctuations in the degree
successfully tolerated noninvasive ventilation early in their course and had of weakness in myasthenia
early-onset MG and thymic hyperplasia were more likely to require less than gravis make respiratory
15 days of mechanical ventilation.35 Of those who survive hospitalization, up to monitoring less helpful in
80% will have a good functional outcome at 12 months.43 predicting intubation.
● Noninvasive ventilation
Future Trends may be helpful in preventing
As the use of immunomodulatory drugs such as immune checkpoint inhibitors intubation in patients with
increases in other fields, it remains to be seen what effect they may have on respiratory failure and
autoimmune diseases, which may be triggered by these medications. preserved cough and bulbar
strength.
Immune-related MG carries a high mortality rate and may be more difficult to
treat than classic MG.44 Future studies should assess whether the treatment for ● Corticosteroids should be
MG caused by immune checkpoint inhibitors should be different than the administered either with or
current protocols used for classic MG. shortly after plasma
exchange or IV
immunoglobulin to prevent
INTENSIVE CARE UNIT–ACQUIRED WEAKNESS worsening of muscle
ICU-acquired weakness is a broad term used to describe weakness in patients weakness in myasthenic
who are critically ill that is not caused by an alternative etiology other than the crisis.
critical illness itself.45 This weakness can frequently manifest as inability to wean
● Intensive care
from the ventilator, may persist for many months after the acute illness has unit–acquired weakness
resolved, and is associated with worse outcomes.46 ICU-acquired weakness is includes the diagnoses of
generally classified into three groups: critical illness polyneuropathy, critical critical illness myopathy,
illness myopathy, and a combination of the two called critical illness critical illness
polyneuropathy, and critical
neuromyopathy. This phenomenon has been described since the early 1900s but illness neuromyopathy.
came into prominence in the 1970s and 1980s.47-49
Pathophysiology
The pathophysiology of ICU-acquired weakness is multifactorial. Sepsis,
prolonged mechanical ventilation, multiorgan failure, systemic inflammatory
response syndrome, hyperglycemia, hyperosmolarity, parenteral nutrition, use
of norepinephrine, elevated lactate, and female sex are all associated with
ICU-acquired weakness.50 The role of steroids in the pathophysiology of
ICU-acquired weakness is uncertain, as data are conflicting.47 Proposed
mechanisms include microcirculatory failure, inactivation of sodium channels, a
catabolic state, mitochondrial dysfunction, oxidative stress, and disuse atrophy.
Critical illness polyneuropathy is an axonal polyneuropathy without
demyelination, possibly secondary to microcirculatory failure of the axon,
although the exact mechanism is unknown.47 Critical illness myopathy is
associated with loss of thick filaments in the muscle along with muscle necrosis.47
The two conditions may coexist, as they share risk factors and likely a common
mechanism.
Presentation
Clinically, ICU-acquired weakness may be difficult to detect and diagnose.
Patients who are critically ill are often heavily sedated, although ICU practices in
recent years have shifted toward a reduction in sedation. ICU-acquired weakness
is often first considered when patients are unable to wean from the ventilator.
Both critical illness myopathy and critical illness polyneuropathy lead to a
symmetric proximal weakness. Tone is decreased, and reflexes are frequently
CONTINUUMJOURNAL.COM 1359
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
reduced, although they are more likely to be preserved in critical illness
myopathy. In critical illness polyneuropathy, all cranial nerves are typically
preserved. Critical illness myopathy can occasionally lead to facial weakness but
rarely affects the extraocular muscles. Involvement of the extraocular muscles
should suggest an alternative diagnosis. Serum creatinine kinase is normal in
critical illness polyneuropathy and may be normal or increased in critical illness
myopathy. In both processes, the muscles of respiration can be involved,
particularly the diaphragm. It is difficult to distinguish critical illness
polyneuropathy from critical illness myopathy clinically without the assistance of
electrophysiologic studies. This challenge is enhanced by the frequent
coexistence of the two pathologies.
Diagnosis
When making the diagnosis of ICU-acquired weakness, the clinician must
exclude alternative causes of weakness based on clinical suspicion, including a
central process such as a cervical myelopathy or other neuromuscular disorders
such as MG, GBS, botulism, and vasculitic neuropathy. Electrodiagnostic studies
are helpful in making the diagnosis, but performing them in the inpatient ICU
setting may present logistic challenges. Electrical interference may create
artifacts, and patient conditions such as anasarca, peripheral edema, and
hypothermia can create challenges. In addition, patients with poor mentation
will not be able to participate in the examination, which may limit the
ability to perform a complete evaluation. To limit technical factors, limbs
should be kept warm during the study and unnecessary machines should be
powered off.51
In critical illness polyneuropathy, CMAP and sensory nerve action potential
(SNAP) amplitudes are reduced or absent. In critical illness myopathy, CMAP
waveforms may show reduced amplitude and increased duration. Muscle
biopsy can be performed if uncertainty exists about the diagnosis or if an
alternative myopathy is being considered, with selective loss of thick
filaments and muscle necrosis being consistent with the diagnosis of critical
illness myopathy. The primary benefit of differentiating between critical
illness polyneuropathy and critical illness myopathy is to better prognosticate
the recovery of patients, as discussed below. Patients with critical illness
myopathy have a greater chance of recovery than do patients with critical
illness polyneuropathy.
Treatment
Treatment of ICU-acquired weakness is currently focused on prevention. A
large randomized controlled trial showed that aggressive control of blood
sugar decreased the rate of ICU-acquired weakness,52 although other trials
have shown similar intensive control of blood glucose to result in an increase
in mortality.53 Based on these trials, moderate, rather than intensive, glucose
control is recommended in the ICU. Avoiding early parenteral nutrition,
minimizing sedation, and promoting early mobilization are also strategies
used to prevent the development of ICU-acquired weakness. Early physical
and occupational therapy starting at the time of respiratory failure has been
shown to be beneficial in improving outcomes from decreasing time on
mechanical ventilation to increasing the percentage of patients discharged
directly to home.46 Animal studies suggest that circulating ketones may have a
1360 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
protective effect, although further research is required before translating this KEY POINTS
into a clinical strategy.54
● Critical illness
polyneuropathy typically
Prognosis spares the cranial nerves,
The risk of death is higher in patients who are critically ill with ICU-acquired and although critical illness
weakness than in those without ICU-acquired weakness.55 One study of patients myopathy may involve facial
muscles, extraocular
in the ICU receiving more than 7 days of mechanical ventilation reported a
muscles are spared.
doubling of inpatient mortality in patients with ICU-acquired weakness as Involvement of the cranial
compared with patients who were mechanically ventilated for similar amounts of nerves should prompt
time and did not develop weakness.56 In a review of survivors of critical illness assessment for an
alternative cause of
with ICU-acquired weakness, nearly 30% had long-term disability.57 However,
weakness.
all ICU-acquired weakness types are not equal. Several studies have shown a
significantly better prognosis in critical illness myopathy than in critical illness ● Primary treatment
polyneuropathy and critical illness neuromyopathy. More than 80% of patients strategies for intensive care
with critical illness myopathy may experience a complete recovery within 6 to unit–acquired weakness
focus on prevention, with
12 months following their ICU stay.58,59 Although the treatments of critical illness minimization of sedation,
myopathy and critical illness polyneuropathy/critical illness neuromyopathy do avoidance of
not differ, differentiating between the two pathologies may have important hyperglycemia, and use of
prognostic value. early mobilization
strategies.
Future Trends ● Critical illness myopathy
Although the focus of this section is on critical illness myopathy, critical illness carries a significantly better
polyneuropathy, and critical illness neuromyopathy, an additional type of prognosis than critical
illness polyneuropathy, with
ICU-acquired weakness that clinicians should be aware of is peripheral nerve
most patients with critical
injury due to compression or traction of the nerves in the ICU setting. In illness myopathy seeing a
particular, the use of the prone position for patients with acute respiratory complete recovery.
distress syndrome (ARDS) can lead to acquired peripheral nerve injury,
particularly of the brachial plexus.60 As proning has become one of the mainstays
of treatment for COVID-19, neurologists should be aware of this condition and
work toward preventive methods in the positioning of patients in the ICU. One
study of patients with injuries following hospitalization for COVID-19 showed
injuries to the ulnar nerve, radial nerve, sciatic nerve, brachial plexus, and
median nerve.61 Although proning is likely a contributing factor to these
neuropathies, further studies will need to continue to determine whether other
factors contribute to the nerve injuries seen after this disease, including direct
inflammation from the virus, vascular involvement, or demyelination. In
addition, femoral neuropathy has been described as a complication following
extracorporeal membrane oxygenation (ECMO) and may become more
prevalent as patients are treated with ECMO for COVID-19.62
Chronic Neurologic Conditions
Patients with chronic progressive neuromuscular disorders may have weakness
that becomes unmasked during a hospitalization for another reason, leading to
neuromuscular respiratory failure. These patients require a thorough workup
with consideration for more chronic conditions. They often come to the attention
of neurologists late in their course, commonly for failure to wean from the
ventilator. In one study of 85 patients admitted for neuromuscular respiratory
failure, 55% of those patients did not have a known diagnosis of a neuromuscular
condition at the time of admission.1 Of those patients, the majority were
diagnosed with a neurologic condition. Final diagnoses included amyotrophic
CONTINUUMJOURNAL.COM 1361
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
lateral sclerosis, CIDP, postpolio syndrome, Kennedy disease, botulism,
amyloidosis, myopathy, myasthenia, and GBS. Other conditions such as
myotonic dystrophy, muscular dystrophy, multiple sclerosis, and mitochondrial
disease may also be considered. Keeping chronic neurologic conditions in the
differential when working up neuromuscular respiratory failure is important to
ensure accurate diagnosis and prognosis.
CONCLUSION
Neuromuscular diseases frequently lead to respiratory failure in the ICU, and
prompt and accurate recognition of distinct conditions such as GBS and MG can
lead to early targeted treatment and improved outcomes. Patients with GBS can
go on to have significant recovery if they can avoid the complications associated
with the respiratory failure and severe dysautonomia that often accompany the
disease. Patients with MG may be able to avoid intubation with the use of
noninvasive ventilation, and rapid initiation of therapy with plasma exchange or
IVIg along with steroids improves outcomes. Much is still to be learned about the
treatment of ICU-acquired weakness; however, awareness of the disease and a
focus on prevention is important until further treatment options can be elicited.
REFERENCES
1 Serrano MC, Rabinstein AA. Causes and 8 Chakraborty T, Kramer CL, Wijdicks EFM,
outcomes of acute neuromuscular respiratory Rabinstein AA. Dysautonomia in Guillain-Barré
failure. Arch Neurol 2010;67(9):1089-1094. doi: syndrome: prevalence, clinical spectrum, and
10.1001/archneurol.2010.207 outcomes. Neurocrit Care 2020;32(1):113-120. doi:
10.1007/s12028-019-00781-w
2 Guillain G, Barré JA, Strohl A. Sur un syndrome de
radiculonevrite avec hyperalbuminose du liquid 9 Asbury AK, Arnason BG, Adams RD. The
cephalon-rachidien sans reaction cellulaire: inflammatory lesion in idiopathic polyneuritis. Its
remarques sur les caracteres cliniques et role in pathogenesis. Medicine (Baltimore) 1969;
graphiques des reflexes tendineux. Bull 48(3):173-215. doi:10.1097/00005792-196905000-
Memoires Soc Med Hopitaux Paris 1916;40: 00001
1462-1470.
10 Funakoshi K, Kuwabara S, Odaka M, et al. Clinical
3 Wijdicks EF, Klein CJ. Guillain-Barré syndrome. predictors of mechanical ventilation in Fisher/
Mayo Clin Proc 2017;92(3):467-479. doi:10.1016/j. Guillain-Barré overlap syndrome. J Neurol
mayocp.2016.12.002 Neurosurg Psychiatry 2009;80(1):60-64. doi:
10.1136/jnnp.2008.154351
4 Willison HJ, Jacobs BC, van Doorn PA. Guillain-
Barré syndrome. Lancet 2016;388(10045):717-727. 11 Leonhard SE, Mandarakas MR, Gondim FAA, et al.
doi:10.1016/S0140-6736(16)00339-1 Diagnosis and management of Guillain-Barré
syndrome in ten steps. Nat Rev Neurol 2019;15(11):
5 Rudant J, Dupont A, Mikaeloff Y, et al. Surgery
671-683. doi:10.1038/s41582-019-0250-9
and risk of Guillain-Barré syndrome: a French
nationwide epidemiologic study. Neurology 2018; 12 Sejvar JJ. Clinical manifestations and outcomes
91(13):e1220-e1227. doi:10.1212/ of West Nile virus infection. Viruses 2014;6(2):
WNL.0000000000006246 606-623. doi:10.3390/v6020606
6 Jacobs BC, Rothbarth PH, van der Meche FG, 13 Bissell DM, Anderson KE, Bonkovsky HL.
et al. The spectrum of antecedent infections in Porphyia. N Engl J Med 2017;377(9):862-872. doi:
Guillain-Barré syndrome: a case-control study. 10.1056/NEJMra1608634
Neurology 1998;51(4):1110-1115. doi:10.1212/
14 The Guillain-Barré Study Group. Plasmapheresis
wnl.51.4.1110
and acute Guillain-Barré syndrome. Neurology
7 Fokke C, van den Berg B, Drenthen J, et al. 1985;35(8):1096-1104. doi:10.1212/WNL.35.8.1096
Diagnosis of Guillain-Barré syndrome and
validation of Brighton criteria. Brain 2014;137(pt 1):
33-43. doi:10.1093/brain/awt285
1362 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
15 van der Meché FGA, Schmitz PIM. A randomized 27 Jacobs BC, van den Berg B, Verboon C, et al.
trial comparing intravenous immune globulin and International Guillain-Barré Syndrome Outcome
plasma exchange in Guillain-Barré syndrome. Study: protocol of a prospective observational
Dutch Guillain-Barré Study Group. N Engl J Med cohort study on clinical and biological predictors
1992;326(17):1123-1129. doi:10.1056/ of disease course and outcome in Guillain-Barré
NEJM199204233261705 syndrome. J Peripher Nerv Syst 2017;22(2):68-76.
doi:10.1111/jns.12209
16 Josephson SA, Ferro J, Cohen A, et al. Quality
improvement in neurology: inpatient and 28 Toscano G, Palmerini F, Ravaglia S, et al. Guillain-
emergency care quality measure set: executive Barré syndrome associated with SARS-CoV-2.
summary. Neurology 2017;89(7):730-735. doi: N Engl J Med 2020;382(26):2574-2576. doi:
10.1212/WNL.0000000000004230 10.1056/NEJMc2009191
17 Randomised trial of plasma exchange, 29 Gilhaus NE. Myasthenia gravis. N Engl J Med 2016;
intravenous immunoglobulin, and combined 375(26):2570-2581. doi:10.1056/NEJMra1602678
treatments in Guillain-Barré syndrome. Plasma
30 Beekman R, Kuks JB, Oosterhuis HJ. Myasthenia
Exchange/Sandoglobulin Guillain-Barré
gravis: diagnosis and follow-up of 100
Syndrome Trial Group. Lancet 1997;349(9047):
consecutive patients. J Neurol 1997;244(2):112-118.
225-230.
doi:10.1007/s004150050059
18 Verboon C, van den Berg B, Cornblath DR, et al.
31 Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized
Original research: second IVIg course in Guillain-
trial of thymectomy in myasthenia gravis. N Engl J
Barré syndrome with poor prognosis: the
Med 2016;375(6):511-522. doi:10.1056/
non-randomised ISID study. J Neurol Neurosurg
NEJMoa1602489
Psychiatry 2020;91(2):113-121. doi:10.1136/jnnp-
2019-321496 32 Gronseth GS, Barohn R, Marayanaswami P.
Practice advisory: thymectomy for myasthenia
19 Walgaard C, Lingsma HF, Ruts L, et al. Prediction
gravis (practice parameter update): Report of the
of respiratory insufficiency in Guillain-Barré
Guideline Development, Dissemination, and
syndrome. Ann Neurol 2010;67(6):781-787. doi:
Implementation Subcommittee of the American
10.1002/ana.21976
Academy of Neurology. Neurology 2020;94(16):
20 Wijdicks EFM. Core principles of acute 705-709. doi:10.1212/WNL.0000000000009294
neurology: handling difficult situations. Oxford
33 Sanders DB, Wolfe GI, Benatar M, et al.
University Press; 2014.
International consensus guidance for
21 Sharshar T, Chevret S, Bourdain F, et al. Early management of myasthenia gravis: executive
predictors of mechanical ventilation in Guillain- summary. Neurology 2016;87(4):419-425. doi:
Barré syndrome. Crit Care Med 2003;31(1): 10.1212/WNL.0000000000002790
278-283. doi:10.1097/00003246-200301000-
34 O'Riordan JI, Miller DH, Mottershead JP, et al. The
00044
management and outcome of patients with
22 Wijdicks EFM, Henderson RD, McClelland RL. myasthenia gravis treated acutely in a
Emergency intubation for respiratory failure in neurological intensive care unit. Eur J Neurol 1998;
Guillain-Barré syndrome. Arch Neurol 2003;60(7): 5(2):137-142. doi:10.1046/j.1468-1331.1998.520137.x
947-948. doi:10.1001/archneur.60.7.947
35 Neumann B, Angstwurm K, Mergenthaler P, et al.
23 Melone MA, Heming N, Meng P, et al. Early Myasthenic crisis demanding mechanical
mechanical ventilation in patients with Guillain- ventilation: a multicenter analysis of 250 cases.
Barré syndrome at high risk of respiratory failure: Neurology 2020;94(3):e299-e313. doi:10.1212/
a randomized trial. Ann Intensive Care 2020;10: WNL.0000000000008688
128. doi:10.1186/s13613-020-00742-z
36 Gummi RR, Kukulka NA, Deroche CB,
24 Walgaard C, Lingsma HF, van Doorn PA, et al. Govindarajan R. Factors associated with acute
Tracheostomy or not: prediction of prolonged exacerbations of myasthenia gravis. Muscle
mechanical ventilation in Guillain-Barré Nerve 2019;60(6):693-699. doi:10.1002/
syndrome. Neurocrit Care 2017;26(1):6-13. doi: mus.26689
10.1007/s12028-016-0311-5
37 Myasthenia Gravis Foundation of America.
25 Nyquist P, Bautista C, Jichici D, et al. Prophylaxis Cautionary drugs. Accessed August 6, 2020.
of venous thrombosis in neurocritical care myasthenia.org/what-is-mg/MG-management/
patients: an evidence-based guideline: a cautionary-drugs
statement for healthcare professionals from the
38 Huang Y-T, Chen Y-P, Lin W-C, et al. Immune
Neurocritical Care Society. Neurocrit Care 2016;
checkpoint inhibitor-induced myasthenia gravis.
24(1):47-60. doi:10.1007/s12028-015-0221-y
Front Neurol 2020;11:634. doi:10.3389/
26 Fletcher DD, Lawn ND, Wolter TD, Wijdicks EFM. fneur.2020.00634
Long-term outcome in patients with Guillain-
39 Wu J-Y, Kuo P-H, Fan P-C, et al. The role of
Barré syndrome requiring mechanical ventilation.
non-invasive ventilation and factors predicting
Neurology 2000;54(12):2311-2315. doi:10.1212/
extubation outcome in myasthenic crisis.
wnl.54.12.2311
Neurocrit Care 2009;10(1):35-42. doi:10.1007/
s12028-008-9139-y
CONTINUUMJOURNAL.COM 1363
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
NEUROMUSCULAR DISORDERS IN THE INTENSIVE CARE UNIT
40 Gajdos P, Chevret S, Clair B, et al. Clinical trial of 52 Van den Berghe G, Wouters P, Weekers F, et al.
plasma exchange and high-dose intravenous Intensive insulin therapy in critically ill patients.
immunoglobulin in myasthenia gravis. N Engl J Med 2001;345(19):1359-1367. doi:10.1056/
Myasthenia Gravis Clinical Study Group. NEJMoa011300
Ann Neurol 1997;41(6):789-796. doi:10.1002/
53 NICE-SUGAR Study Investigators, Finfer S,
ana.410410615
Chittock DR, et al. Intensive versus conventional
41 Liu Z, Yao S, Zhou Q, et al. Predictors of glucose control in critically ill patients. N Engl
extubation outcomes following myasthenic Med 2009;360(13):1283-1297. doi:10.1056/
crisis. J Int Med Res 2016;44(6):1524-1533. doi: NEJMoa0810625
10.1177/0300060516669893
54 Goossens C, Weckx R, Derde S, et al. Adipose
42 Godoy DA, de Mello LJV, Masotti L, Di Napoli M. tissue protects against sepsis-induced muscle
The myasthenic patient in crisis: an update of the weakness in mice: from lipolysis to ketones. Crit
management in neurointensive care unit. Care 2019;23(1):236. doi:10.1186/s13054-019-
Arq Neuropsiquiatr 2013;71(9A):627-639. doi: 2506-6
10.1590/0004-282X20130108
55 Hermans G, Van Mechelen H, Clerckx B, et al.
43 Liu F, Wang Q, Chan X. Myasthenic crisis treated Acute outcomes and 1-year mortality of intensive
in a Chinese neurological intensive care unit: care unit-acquired weakness. A cohort study and
clinical features, mortality, outcomes, and propensity-matched analysis. Am J Respir Crit
predictors of survival. BMC Neurol 2019;19(1):172. Care Med 2014;190(4):410-420. doi:10.1164/
doi:10.1186/s12883-019-1384-5 rccm.201312-2257OC
44 Becquart O, Lacotte J, Malissart P, et al. 56 Sharshar T, Bastuji-Garin S, Stevens R, et al.
Myasthenia gravis induced by immune Presence and severity of intensive care
checkpoint inhibitors. J Immunother 2019;42(8): unit-acquired paresis at time of awakening are
309-312. doi:10.1097/CJI.0000000000000278 associated with increased intensive care unit and
hospital mortality. Crit Care Med 2009;37(12):
45 Stevens RD, Marshall SA, Cornblath DR, et al. A
3047-3053. doi:10.1097/CCM.0b013e3181b027e9
framework for diagnosing and classifying
intensive care unit-acquired weakness. Crit Care 57 Latronico N, Shenu I, Seghelini E. Neuromuscular
Med 2009;37(10 suppl):S299-S308. doi:10.1097/ sequelae of critical illness. Curr Opin Crit Care
CCM.0b013e3181b6ef67 2005;11(4):381-390. doi:10.1097/01.
ccx.0000168530.30702.3e
46 Fan E, Cheek E, Chlan L, et al. An official American
Thoracic Society Clinical Practice Guideline: the 58 Guarneri B, Bertolini G, Latronico N. Long-term
diagnosis of intensive care unit-acquired outcome in patients with critical illness
weakness in adults. Am J Respir Crit Care Med myopathy or neuropathy: the Italian multicentre
2014;190(12):1437-1446. doi:10.1164/rccm.201411- CRIMYNE study. J Neurol Neurosurg Psychiatry
2011ST 2008;79(7):838-841. doi:10.1136/jnnp.2007.142430
47 Kress JP, Hall JB. ICU-acquired weakness and 59 Koch S, Wollersheim T, Bierbrauer J, et al.
recovery from critical illness. N Engl J Med 2014; Long-term recovery in critical illness myopathy is
370(17):1626-1635. doi:10.1056/NEJMra1209390 complete, contrary to polyneuropathy. Muscle
Nerve 2014;50(3):431-436. doi:10.1002/mus.24175
48 MacFarlane IA, Rosenthal FD. Severe myopathy
after status asthmaticus. Lancet 1977;2(8038):615. 60 Simpson AI, Vaghela KR, Brown H, et al. Reducing
doi:10.1016/s0140-6736(77)91471-4 the risk and impact of brachial plexus injury
sustained from prone positioning—a clinical
49 Bolton CF, Gilbert JJ, Hahn AF, Sibbald WJ.
commentary. J Intensive Care Med 2020;35(12):
Polyneuropathy in critically ill patients. J Neurol
1576-1582. doi:10.1177/0885066620954787
Neurosurg Psychiatry 1984;47(11):1223-1231. doi:
10.1136/jnnp.47.11.1223 61 Malik GR, Wolfe AR, Soriano R, et al. Injury-prone:
peripheral nerve injuries associated with prone
50 Yang T, Li Z, Jiang L, et al. Risk factors for
positioning for COVID-19-related acute
intensive care unit–acquired weakness: a
respiratory distress syndrome. Br J Anaesth
systematic review and meta-analysis. Acta
2020;125(6):E478-E480. doi:10.1016/j.
Neurol Scand 2018;138(2):104-114. doi:10.1111/
bja.2020.08.045
ane.12964
62 Jang AY, Oh YJ, Lee SI, et al. Femoral neuropathy
51 Lacomis D. Electrophysiology of neuromuscular
following venoarterial-extracorporeal membrane
disorders in critical illness. Muscle Nerve 2013;
oxygenation therapy: a case report.
47(3):452-463. doi:10.1002/mus.23615
BMC Cardiovasc Disord 2020;20(1):393. doi:
10.1186/s12872-020-01675-y
1364 OCTOBER 2021
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Chronic Fatigue Syndrome From Chronic Fatigue To More Specific SyndromesDocument5 pagesChronic Fatigue Syndrome From Chronic Fatigue To More Specific SyndromesArgenis SalinasNo ratings yet
- Babok Framework Overview: BA Planning & MonitoringDocument1 pageBabok Framework Overview: BA Planning & MonitoringJuan100% (1)
- Rehabilitation in Guillian Barre SyndromeDocument6 pagesRehabilitation in Guillian Barre Syndromeanon_681345291No ratings yet
- Ataxia Continuum Agosto 2016Document19 pagesAtaxia Continuum Agosto 2016Habib G. Moutran BarrosoNo ratings yet
- Employee Leave PolicyDocument3 pagesEmployee Leave Policyladdu30No ratings yet
- Clinical Review - FullDocument5 pagesClinical Review - FullsarandashoshiNo ratings yet
- Guillain Barre Syndrome A ReviewDocument7 pagesGuillain Barre Syndrome A ReviewEditor IJTSRDNo ratings yet
- Choke Manifold Procedures 3932324 01Document4 pagesChoke Manifold Procedures 3932324 01Saïd Ben Abdallah100% (1)
- ACLS Post Test (Copy) 낱말 카드 - QuizletDocument18 pagesACLS Post Test (Copy) 낱말 카드 - Quizlet김민길No ratings yet
- Tinh Toan Tang AP Cau Thang - CT Qui LongDocument20 pagesTinh Toan Tang AP Cau Thang - CT Qui Longntt_121987No ratings yet
- Eye Essentials Cataract Assessment Classification and ManagementDocument245 pagesEye Essentials Cataract Assessment Classification and ManagementKyros1972No ratings yet
- Management of Cerebral Edema, Brain Compression,.4Document29 pagesManagement of Cerebral Edema, Brain Compression,.4Jorge MontenegroNo ratings yet
- Module 5 The Teacher and The Community School Culture and Organizational LeadershipDocument6 pagesModule 5 The Teacher and The Community School Culture and Organizational LeadershipHazeldiazasenas100% (6)
- Vol 27.5 - Neurocritical Care.2021Document363 pagesVol 27.5 - Neurocritical Care.2021RafaelNo ratings yet
- Guillain-Barré Syndrome Pediatrico 2018Document4 pagesGuillain-Barré Syndrome Pediatrico 2018Mariam Plata100% (1)
- Altered Mental Status in "Guillain-Barre Syndrome" - A Noteworthy Clinical Clue. Eoin MulroyDocument19 pagesAltered Mental Status in "Guillain-Barre Syndrome" - A Noteworthy Clinical Clue. Eoin MulroyJeffery TaylorNo ratings yet
- Agrawal2007 GBSDocument9 pagesAgrawal2007 GBSSimón Fuentes (STAHLGREIFER)No ratings yet
- Intensive Care Management of Guillain Barre Syndrome: A Retrospective Outcome Study and Review of LiteratureDocument10 pagesIntensive Care Management of Guillain Barre Syndrome: A Retrospective Outcome Study and Review of LiteratureFakhrur RaziNo ratings yet
- The Efficacy of Intravenous Immunoglobulin in Guillain-Barré Syndrome: The Experience of A Tertiary Medical CenterDocument7 pagesThe Efficacy of Intravenous Immunoglobulin in Guillain-Barré Syndrome: The Experience of A Tertiary Medical CenterHadana RetnopratiwiNo ratings yet
- Guillain-Barre Syndrome: Practice EssentialsDocument18 pagesGuillain-Barre Syndrome: Practice EssentialsAna-Maria DuMiNo ratings yet
- Jurnal GBSDocument15 pagesJurnal GBSfajar sugandaNo ratings yet
- Guillain-Barré Syndrome - Literature: SciencedirectDocument4 pagesGuillain-Barré Syndrome - Literature: SciencedirectArlentinaNo ratings yet
- Guillain Barre SyndromeDocument13 pagesGuillain Barre SyndromeAdreiTheTripleANo ratings yet
- Guillain Barre SyndromeDocument2 pagesGuillain Barre SyndromeTheresia Avila KurniaNo ratings yet
- Guillian BarrettDocument12 pagesGuillian BarrettOmar MadrigalNo ratings yet
- Journal GBSDocument11 pagesJournal GBSWinda Haeriyoko100% (1)
- GbsDocument8 pagesGbszhoujNo ratings yet
- Pneumoniae), Vaccines (E.g., Rabies, Tetanus, and Influenza), Lymphoma, Surgery, and TraumaDocument7 pagesPneumoniae), Vaccines (E.g., Rabies, Tetanus, and Influenza), Lymphoma, Surgery, and TraumaKenn yahweexNo ratings yet
- Guillain-Barré Syndrome Med Student PresentationDocument16 pagesGuillain-Barré Syndrome Med Student PresentationRon ShenkarNo ratings yet
- Review of CimDocument8 pagesReview of CimMuhammad Imran MirzaNo ratings yet
- AstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFDocument5 pagesAstraZeneca COVID-19 Vaccine and Guillain - Barre Syndrome in Tasmania PDFMelissa GuerreroNo ratings yet
- GBS1Document20 pagesGBS1Yenza FaheraNo ratings yet
- GBS A ReviewDocument6 pagesGBS A ReviewNurul Kartika SariNo ratings yet
- 5 Malado Guillain Barre SyndromeDocument7 pages5 Malado Guillain Barre SyndromeAllan CastroNo ratings yet
- Referat GBSDocument12 pagesReferat GBSSoraya Dwi KhairunnisaNo ratings yet
- Guillain-Barré Syndrome in Adults - Pathogenesis, Clinical Features, and Diagnosis - UpToDateDocument49 pagesGuillain-Barré Syndrome in Adults - Pathogenesis, Clinical Features, and Diagnosis - UpToDateLuísa OliveiraNo ratings yet
- GBSReviewDocument6 pagesGBSReviewyogesh sNo ratings yet
- Guillain-Barre Syndrome (GBS) PDFDocument13 pagesGuillain-Barre Syndrome (GBS) PDFerikafebriyanarNo ratings yet
- Immunotherapy of Guillain-Barre Syndrome 2018Document12 pagesImmunotherapy of Guillain-Barre Syndrome 2018victorcdNo ratings yet
- Acquired NeuropathiesDocument106 pagesAcquired NeuropathiesDanny J. BrouillardNo ratings yet
- Migraine in Systemic Autoimmune Diseases Cavestro-Ferrero 2018Document11 pagesMigraine in Systemic Autoimmune Diseases Cavestro-Ferrero 2018Adrianah ValenchyNo ratings yet
- Manejo Del SGB 10 PasosDocument13 pagesManejo Del SGB 10 PasosRonald ReyesNo ratings yet
- Autoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityDocument16 pagesAutoimmune Myasthenia Gravis: Emerging Clinical and Biological HeterogeneityGiuseppeNo ratings yet
- Immunoglobulin and Monoclonal Antibodi Therapies in GbsDocument12 pagesImmunoglobulin and Monoclonal Antibodi Therapies in GbsSyafiraNo ratings yet
- Differentiatingfamilial Neuropathiesfrom Guillain-Barre SyndromeDocument22 pagesDifferentiatingfamilial Neuropathiesfrom Guillain-Barre SyndromeKartika IwangNo ratings yet
- 1.-Nature Review SGBDocument14 pages1.-Nature Review SGBTony Gomez Luna LeyvaNo ratings yet
- Guillain-Barre SyndromeDocument42 pagesGuillain-Barre Syndromesuraj rajpurohitNo ratings yet
- Overview of Guillain-Barré Syndrome: I. Literature ReviewDocument10 pagesOverview of Guillain-Barré Syndrome: I. Literature ReviewS Dian RNo ratings yet
- Chronic Inflammatory Demyelinating PolyradiculopathyDocument8 pagesChronic Inflammatory Demyelinating PolyradiculopathyATIKA INDAH SARINo ratings yet
- Cronicon: Clinical Case Study Clinical Manifestation, Diagnosis, Treatment and Prevention of Leprosy: An UpdateDocument4 pagesCronicon: Clinical Case Study Clinical Manifestation, Diagnosis, Treatment and Prevention of Leprosy: An Updatetifa adaNo ratings yet
- Ann MS Id 000849Document8 pagesAnn MS Id 000849azucenadeoNo ratings yet
- Consensus: StatementDocument13 pagesConsensus: StatementElfrida FernandesNo ratings yet
- Síndrome de Guillain-Barré y Anticuerpos Anti-Gangliósidos El Viaje de Un Clínico-CientíficoDocument28 pagesSíndrome de Guillain-Barré y Anticuerpos Anti-Gangliósidos El Viaje de Un Clínico-Científicofrancisco bacaNo ratings yet
- Clinical Evaluation and Investigation of Neuropathy: Hugh J Willison, John B WinerDocument7 pagesClinical Evaluation and Investigation of Neuropathy: Hugh J Willison, John B WinerCindy Julia AmandaNo ratings yet
- 97ff PDFDocument10 pages97ff PDFElfrida FernandesNo ratings yet
- 1 s2.0 S1201971216310244 MainDocument2 pages1 s2.0 S1201971216310244 Mainnurahmi widyani ratriNo ratings yet
- Mimics and Chameleons in Guillain - Barré and Miller Fisher SyndromesDocument10 pagesMimics and Chameleons in Guillain - Barré and Miller Fisher SyndromesElfrida FernandesNo ratings yet
- How Great Thou ArtDocument8 pagesHow Great Thou ArtRenz Marion AlemaniaNo ratings yet
- Gullain-Barre SyndromeDocument7 pagesGullain-Barre Syndromejanellekate1224No ratings yet
- Out PDFDocument6 pagesOut PDFMaria RenjaanNo ratings yet
- Uillain Arré Yndrome: L A. M, MDDocument4 pagesUillain Arré Yndrome: L A. M, MDYuriko AndreNo ratings yet
- Chapter 23 Acquired Neuropathies PDFDocument106 pagesChapter 23 Acquired Neuropathies PDFzloncar3No ratings yet
- Clinical Evaluation and Investigation of Neuropathy: Hugh J Willison, John B WinerDocument7 pagesClinical Evaluation and Investigation of Neuropathy: Hugh J Willison, John B Winerdefri rahmanNo ratings yet
- Guillain Barre Syndrome As A Complication of Covid 19 A Systematic ReviewDocument11 pagesGuillain Barre Syndrome As A Complication of Covid 19 A Systematic ReviewKARLOS ALVARO ACURIO ORTIZNo ratings yet
- Dampd 5 Manual Del Jugador EspDocument24 pagesDampd 5 Manual Del Jugador EspClaudio ReichelNo ratings yet
- Pathophysiology and Therapy of Associated Features of MigraineDocument22 pagesPathophysiology and Therapy of Associated Features of MigraineNicki Pinzon NariñoNo ratings yet
- Guillain-Barré Syndrome in Children: Epidemiology, Clinical Features, and DiagnosisDocument21 pagesGuillain-Barré Syndrome in Children: Epidemiology, Clinical Features, and Diagnosisgocelij948No ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Neurometabolic Hereditary Diseases of AdultsFrom EverandNeurometabolic Hereditary Diseases of AdultsAlessandro P. BurlinaNo ratings yet
- Risk Factors Promoting External Ventricular Drain Infections in Adult Neurosurgical Patients at The Intensive Care Unit-A Retrospective StudyDocument13 pagesRisk Factors Promoting External Ventricular Drain Infections in Adult Neurosurgical Patients at The Intensive Care Unit-A Retrospective StudyOlga Manco GuzmánNo ratings yet
- Research Article: Hindawi Critical Care Research and Practice Volume 2022, Article ID 3834165, 8 PagesDocument8 pagesResearch Article: Hindawi Critical Care Research and Practice Volume 2022, Article ID 3834165, 8 PagesOlga Manco GuzmánNo ratings yet
- 2023 - Intraoperative Blood Pressure and Carbon Dioxide Values During Aneurysmal Repair and The Outcomes After Aneurysmal Subarachnoid HemorrhageDocument9 pages2023 - Intraoperative Blood Pressure and Carbon Dioxide Values During Aneurysmal Repair and The Outcomes After Aneurysmal Subarachnoid HemorrhageOlga Manco GuzmánNo ratings yet
- Palliative Care and Shared Decision Making in The.14Document14 pagesPalliative Care and Shared Decision Making in The.14AmitShettyNo ratings yet
- 2021 - Acute Neurologic Manifestations of Respiratory VirusesDocument17 pages2021 - Acute Neurologic Manifestations of Respiratory VirusesOlga Manco GuzmánNo ratings yet
- NEJMra 1602678Document12 pagesNEJMra 1602678Olga Manco GuzmánNo ratings yet
- J NCL 2006 11 003Document17 pagesJ NCL 2006 11 003Olga Manco GuzmánNo ratings yet
- 713full 221024 135448Document8 pages713full 221024 135448Olga Manco GuzmánNo ratings yet
- Encefalitis AutoinmunebznDocument11 pagesEncefalitis AutoinmunebznCarolina CrucesNo ratings yet
- Cryptococcose Neuro-MeningéDocument12 pagesCryptococcose Neuro-MeningéTongamanantsoa RazainjafyNo ratings yet
- Greene - 2019 - Progressive Supranuclear Palsy, Corticobasal Degeneration, and Multiple System Atrophy - RevisiónDocument17 pagesGreene - 2019 - Progressive Supranuclear Palsy, Corticobasal Degeneration, and Multiple System Atrophy - RevisiónEmmanuel Domínguez RosalesNo ratings yet
- Lancet Parkinson's DiseaseDocument17 pagesLancet Parkinson's DiseaseYong WaiNo ratings yet
- 1-Approach To The History and Evaluation of VertigoDocument24 pages1-Approach To The History and Evaluation of VertigoOlga Manco GuzmánNo ratings yet
- Sem3 - Pharmacotherapy Pearls For Emergency Neurological Life SupportDocument26 pagesSem3 - Pharmacotherapy Pearls For Emergency Neurological Life SupportOlga Manco GuzmánNo ratings yet
- Sem3 - Airway, Ventilation, and SedationDocument25 pagesSem3 - Airway, Ventilation, and SedationOlga Manco GuzmánNo ratings yet
- Sem3 Protocol AVSDocument15 pagesSem3 Protocol AVSOlga Manco GuzmánNo ratings yet
- Update On Antiseizure Medications 2022.13Document36 pagesUpdate On Antiseizure Medications 2022.13Ana Castro MondacaNo ratings yet
- NeuroinfecciónDocument19 pagesNeuroinfecciónfabio100% (1)
- Harvard Referencing GuideDocument6 pagesHarvard Referencing GuideKhánh Nguyên VõNo ratings yet
- Unit 5.4 - Incapacity As A Ground For DismissalDocument15 pagesUnit 5.4 - Incapacity As A Ground For DismissalDylan BanksNo ratings yet
- ListwarehouseDocument1 pageListwarehouseKautilya KalyanNo ratings yet
- Piaget Stages of Cognitive DevelopmentDocument2 pagesPiaget Stages of Cognitive DevelopmentSeph TorresNo ratings yet
- Gambaran Professional Quality of Life Proqol GuruDocument7 pagesGambaran Professional Quality of Life Proqol Gurufebrian rahmatNo ratings yet
- 2.3 & 2.5 Cell DivisionDocument14 pages2.3 & 2.5 Cell DivisionJhonnyNo ratings yet
- Ideal Discharge Elderly PatientDocument3 pagesIdeal Discharge Elderly PatientFelicia Risca RyandiniNo ratings yet
- VedasUktimAlA Sanskrit Hindi EnglishDocument47 pagesVedasUktimAlA Sanskrit Hindi EnglishAnantha Krishna K SNo ratings yet
- Hotel ClassificationDocument10 pagesHotel ClassificationRonelyn Boholst100% (1)
- Mental Health & TravelDocument18 pagesMental Health & TravelReyza HasnyNo ratings yet
- Tda12110h1 N300Document1 pageTda12110h1 N300rolandseNo ratings yet
- Concrete and Its PropertiesDocument24 pagesConcrete and Its PropertiesAmila LiyanaarachchiNo ratings yet
- Economics Half Yearly Question PaperDocument6 pagesEconomics Half Yearly Question PaperBhumika MiglaniNo ratings yet
- Strict and Absolute LiabilityDocument29 pagesStrict and Absolute LiabilityShejal SharmaNo ratings yet
- Final PR 2 CheckedDocument23 pagesFinal PR 2 CheckedCindy PalenNo ratings yet
- Rovers - CH - 2 - Drug TherapyDocument28 pagesRovers - CH - 2 - Drug TherapyKhalid Bin AliNo ratings yet
- Optimization Process of Biodiesel Production With Ultrasound Assisted by Using Central Composite Design MethodsDocument47 pagesOptimization Process of Biodiesel Production With Ultrasound Assisted by Using Central Composite Design MethodsMiftahFakhriansyahNo ratings yet
- IS 11255 - 7 - 2005 - Reff2022 Methods For Measurement of Emission From Stationary Sources Part 7 Oxides of NitrogenDocument10 pagesIS 11255 - 7 - 2005 - Reff2022 Methods For Measurement of Emission From Stationary Sources Part 7 Oxides of NitrogenPawan SharmaNo ratings yet
- This Study Resource WasDocument3 pagesThis Study Resource WasNayre JunmarNo ratings yet
- 2013 Casel GuideDocument80 pages2013 Casel GuideBobe MarinelaNo ratings yet
- Damasco - Cpi - Activity No. 10Document18 pagesDamasco - Cpi - Activity No. 10LDCU - Damasco, Erge Iris M.No ratings yet
- Period of Intuitive NursingDocument4 pagesPeriod of Intuitive NursingJhey-ar Toledo100% (1)
- T103 InstructionsDocument1 pageT103 Instructionsjtcool74No ratings yet