Professional Documents
Culture Documents
DR Ahmed
DR Ahmed
Uploaded by
Hasnaa MahmoudOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DR Ahmed
DR Ahmed
Uploaded by
Hasnaa MahmoudCopyright:
Available Formats
Introduction to Quality
Quality in general is a term that is widely used in relation to products
and services that are being traded daily between people. A product or
service of good quality is that which will result in brand recognition and will
increase customer loyalty and trust making them willing to but this product
or service again. Quality product and service will also reduce rework,
defects and unnecessary loss of resources. All of this will eventually lead to
an increase in revenue and overall profit for the organization.
Dr. Ahmed Refat 2
Introduction to Quality
Service quality is considered the measure of how the organization delivers
its services in comparison to the expectations of its customers ,who either
consciously or unconsciously have set certain standards for how this service
will fulfill the needs making them ask for this service in the first place. The
healthcare service sector is of critical nature and because of that multiple
organizations have suggested different methodologies for establishing
frameworks that show the way into providing quality healthcare services.
Dr. Ahmed Refat 3
Introduction to Quality
Quality management systems will provide the organizations with the way to
do the right thing, the first time and every time, a famous quote by Phil
Crosby one of the management and quality gurus who was an advisor to
several “Fortune 500” companies. Crosby also introduced the concept of
“Quality is free” which projected the fact about faulty systems allow things
to go wrong. Crosby based his quality management systems upon four
absolutes: quality means adherence to requirements, quality comes from
prevention, performance standard is zero defects and quality is measured
by nonconformance.
Dr. Ahmed Refat 4
Absolutes of Quality
✓Quality means adherence to requirements
✓Quality comes from prevention
✓Performance standard is “ZERO” defects
✓Quality is measured by non-conformance
Dr. Ahmed Refat 5
Introduction to Quality
1. Conformance must be to standards, limit or specifications
2. Secret of prevention is to look at processes and identify opportunities
for errors
3. Management system made by leaders and tells employees what is
expected from them
4. All expenses involved in doing things wrong, then costs of fixing
problems, correcting orders & correcting products.
Dr. Ahmed Refat 6
Introduction to Quality
Quality is maintained and improved when leaders, managers and the
workforce understand and commit to constant customer satisfaction
through continuous quality improvement. So leaders’ policies and actions
should reflect their commitment to quality. In order to plan a service of a
recognized quality, we should be always looking for what the customer
needs and design all the aspects of the system to meet these needs reliably.
Dr. Ahmed Refat 7
Introduction to Quality
Leaders should then be always looking for the compliance of these
processes and the system overall with the standards they put in order to
meet the expectations of the customer. Improvement projects are used to
get the aspects of the system that fall behind the target expectations back
on track moving towards achieving the targeted level of quality.
Dr. Ahmed Refat 8
Introduction to Quality
ISO’s 7 quality management principles form a framework of fundamental
beliefs, rules and norms that are accepted to be a basis for quality
management. They come as follows – as stated in ISO’s publication - in 2015
with no intended order; customer focus, leadership, engagement of people,
process approach, improvement, evidence-based decision making and
relationship management.
Dr. Ahmed Refat 9
Dr. Ahmed Refat
10
Introduction to Quality
1. Customer focus: The primary focus of quality management is to meet customer
requirements and to strive to exceed customer expectations.
2. Leadership: Leaders at all levels establish unity of purpose and direction and create
conditions in which people are engaged in achieving the organization’s quality
objectives.
3. Engagement of people: Competent, empowered and engaged people at all levels
throughout the organization are essential to enhance its capability to create and
deliver value.
Dr. Ahmed Refat 11
Introduction to Quality
4. Process approach: Consistent and predictable results are achieved more effectively and
efficiently when activities are understood and managed as interrelated processes that
function as a coherent system.
5. Improvement: Successful organizations have an ongoing focus on improvement.
6. Evidence-based decision-making: Decisions based on the analysis and evaluation of
data and information are more likely to produce desired results
7. Relationship management: For sustained success, an organization manages its
relationships
Dr. Ahmed Refat 12
Introduction to Quality
For an organization to claim that it’s applying quality standards in its process
build up, it should be able to differentiate between the different
perspectives of quality. Actual quality can be measured by different
methods according to which part of the organization’s performance we
want to gauge.
Dr. Ahmed Refat 13
Introduction to Quality
• Expected Quality: It is the true needs and expectations of the customer and it’s what the
customer assumes he will receive from the product.
• Actual Quality: It is the outcome of the system’s processes and it’s what is finally
delivered to the patient.
• Perceived Quality: It’s what is developed by the customer after receiving the service or
product and comparing it to what he expected.
Perceived quality vs Expected Quality
Dr. Ahmed Refat 14
Healthcare Quality
Healthcare is a unique service as it dealing solely with the wellbeing of
people, and this makes it more important to notice that this service requires
greater interest and consideration towards the presence of a quality
management system that ensures this service will always be at hand in a
way that fulfills the ambitions of both the service provider and benefactor.
Dr. Ahmed Refat 15
Healthcare Quality
Being a service business, the healthcare business , as we referred to earlier,
requires a specific approach when dealing with quality systems. Services are
intangible, uncountable and can’t be verified in advance. It’s a combination
of expertise, experiences and skills. It shows higher variation depending on
its provider, the environment of provision and interaction between the
provider and the benefactor. Healthcare quality is related to 4 main aspects;
what, who, how and result of care.
Dr. Ahmed Refat 16
Healthcare Quality
• What of care is looking for the doing the right service for the patient at
the right time and place.
• Who of care is related to the competency of the caregiver and whether
he can provide the service in the right way.
• How of care looks for policies, procedures and processes that lead to the
provision of this service.
• Finally, the result of care is linked to the outcome of this healthcare
service on the patient’s health.
Dr. Ahmed Refat 17
Healthcare Quality
Then comes a debate to decide whether the value of this healthcare service
will meet that of the business sector. The proof that shows that the quality
of care received, and the dollars spent on this care best meet can be
ensured by implementing a healthcare quality management system and
continuous performance audits to check if this system actually works at it
was planned to.
Dr. Ahmed Refat 18
Healthcare Quality
The value of the services introduced to the customer depends on the results
that the customer perceives. The concept of quality is best defined by the
recipient of product\service. If you need to calculate the value out of any
service you will have to add the quality of the provided care + the outcome
of this care and divide all of this by the cost, all the cost that the
organization had to bear in order to deliver this service.
𝑄𝑢𝑎𝑙𝑖𝑡𝑦 𝑜𝑓 𝑐𝑎𝑟𝑒 + 𝑜𝑢𝑡𝑐𝑜𝑚𝑒
𝑉𝑎𝑙𝑢𝑒 =
𝐶𝑜𝑠𝑡
Dr. Ahmed Refat 19
Healthcare Quality
This “value” must be agreed upon by all the stakeholders related to the
service provision and reception, because the integration of all stakeholders’
contributions and the balance and integration of cost, quality and risk is
crucial for the coordination of all services delivery processes.
The total quality management in healthcare is built over the
commitment of leadership and an established philosophy in the
organization in order to deliver value to the customer. The implementation
of total quality management in healthcare began in 1990 with 10 basic
principles that somewhat relate to those of ISO.
Dr. Ahmed Refat 20
Healthcare Quality
They include:
• Productive work is accomplished through processes
• Main source of quality defects is problems in the processes
• Understanding the variability of processes is key to improving quality
• Quality control must focus on the most vital processes
• Sound customer-supplier relationship is absolutely necessary for sound
quality management
Dr. Ahmed Refat 21
Healthcare Quality
They include:
• Poor quality is costly
• The modern approach to quality is thoroughly grounded in scientific and
statistical thinking
• Total employee involvement is critical
• New organizational structures can help achieve quality improvement
• Quality management employs three basic, closely interrelated activities:
Quality planning, quality control, and quality improvement
Dr. Ahmed Refat 22
Healthcare Quality
CQI continuous quality improvement – also known as Kaizen – is a
philosophy that focuses on continuous improvement throughout the daily
activities depending on successive cycles of assessment of the current
practice processes and utilizing tools that enables team members to assess
and improve healthcare delivery in order to achieve a desired outcome.
The PDCA (plan-do-check-act) approach is one example that enables the
implementation of CQI. Continuous quality improvement enables
professionals to master and perfect the systems and processes in care
delivery, provided that there is a learning and improving culture within the
organization.
Dr. Ahmed Refat 23
STEEEP Quality Dimensions
From the moment you enter the health system, you depend on the
people providing care to correctly diagnose your problems, provide effective
treatment, and ensure your safety. This is basically linked to the system
which operates the healthcare institution where you are being serviced. The
culture, policies, procedures, equipment, qualifications and regulations
established within the facility will be adding to the healthcare service you
receive.
Dr. Ahmed Refat 24
STEEEP Quality Dimensions
Organizational theorist James Reason described safety as a “dynamic non-
event”: Safety is dynamic because it requires “timely human adjustments”
and a non-event because “successful outcomes rarely call attention to
themselves” so if you need to ensure that nothing bad happens, a lot of
good things must happen.
When nothing happens, something is happening
Dr. Ahmed Refat 25
STEEEP Quality Dimensions
In 1999, the Institute of Medicine (IOM) released its landmark report,
“To Err Is Human”, which revealed that between 44,000 and 98,000 died
each year in United States hospitals due to medical errors and adverse
events. The report didn’t point fingers at a single cause to the only or even
the main cause for these deaths. It didn’t even relate these deaths to
recklessness or incompetence. But it stated that “ Faulty systems, processes,
and conditions that lead people to make mistakes or fail to prevent them”
were to be blamed for these harms.
Dr. Ahmed Refat 26
STEEEP Quality Dimensions
Then in 2001 IOM published “Crossing the quality chasm”, another
report related to the quality of healthcare services that included the 6
dimensions of quality known in abbreviation as “STEEEP”. STEEEP
represents; Safety, Timeliness, Effectiveness, Efficiency, Equity and Patient-
Centeredness. We will discuss each one of them in some details in order to
get to know it well.
6 Dimensions of Qulaity
Dr. Ahmed Refat 27
STEEEP Quality Dimensions
• Safety:
First, do no harm. Ensuring the healthcare services are safe and doesn’t
harm patients. This can be related to every perspective of the process. It
aims at reducing the risks and impacts of incidents that can harm the
patient. Incidents are defined as unplanned events that can result in injury,
damage or loss. Safety may also be related to non-clinical incidents like
wrong personal data, improper diet planning or discharge procedures.
Dr. Ahmed Refat 28
STEEEP Quality Dimensions
• Timeliness:
This is about how quickly the patient receives the healthcare service he
needs. No barriers will face patients preventing them from receiving the
care they need. It includes access to care and system responsiveness which
is represented in reducing waiting times and delays in elective surgery,
emergency department, patient discharge, bed availability or even room
cleaning. Adherence to timely healthcare requires reducing geographical,
financial, social or medical issues that prevent right care at the right time.
Dr. Ahmed Refat 29
STEEEP Quality Dimensions
• Effectiveness:
Providing service based on scientific knowledge to all those who are in
need of it. This also includes not providing tests, medications or procedures
to those who will not benefit from them. Over treatment and under
treatment are both issues to be considered when planning and executing
the plan of care to patients. Over treatment is like not following blood
transfusion guidelines and giving blood to a patient who doesn’t need it
while under treatment is like not doing proper assessment for pressure
ulcers in ICU patients.
Dr. Ahmed Refat 30
STEEEP Quality Dimensions
• Efficiency:
This is about getting the most out of available resources and it looks into
reducing waste of these resources. This waste can be equipment, supplies,
energy, time and money. Sometimes we can manage the things we need for
the patient in a different way yet get the same results or even better. For
example, the comparison between hospitalizing the patient and performing
a day-case surgery or even at outpatient setting.
Dr. Ahmed Refat 31
STEEEP Quality Dimensions
• Equity:
Care is delivered regardless of the socio-economic, ethnic, gender or any
other personal characteristics. All patients must have access to the same
appropriate health services regardless of any characteristics.
Dr. Ahmed Refat 32
STEEEP Quality Dimensions
• Patient-Centered:
It’s about putting the patient in the center of the care system. in some
cases, the treatment plan allow for options and selecting the options for
treatment must be based upon the patient’s preferences, needs and values.
Honoring the patient and his family choices, experiences and values is
essential in planning the treatment plan. This requires proper
communication with patients and relatives, understanding of cultural
traditions and proper education made to the patient about the different
options regarding the plan of care.
Dr. Ahmed Refat 33
Quality Dimensions
• https://youtu.be/erei6SZjcck?si=OmaTE7QZg6QGeAJN
• https://youtu.be/pj-AvTOdk2Q?si=8ob5a8MJ45NCQU9q
Dr. Ahmed Refat 34
Quality Dimensions
The equation changed. Value is now reconsidered and the elements that
contribute to value of service expanded to include safety and patient
experience. Patient safety became a major concern to healthcare
institutions, both service providers and regulation bodies.
𝑄𝑢𝑙𝑎𝑖𝑡𝑦 𝑜𝑓 𝑐𝑎𝑟𝑒 + 𝑠𝑎𝑓𝑒𝑡𝑦 + 𝑝𝑎𝑡𝑖𝑒𝑛𝑡 𝑒𝑥𝑝𝑒𝑟𝑖𝑒𝑛𝑐𝑒
𝑉𝑎𝑙𝑢𝑒 =
𝐶𝑜𝑠𝑡
Dr. Ahmed Refat 35
Licensure, certification and accreditation
A lot of confusion goes around the differences between licensure,
certification and accreditation. Those three terms are all related to
healthcare facilities’ systems, processes and infrastructure used in
healthcare provision.
Dr. Ahmed Refat 36
Licensure, certification and accreditation
Licensure:
A non-voluntary legal document granted by a governmental body that provides
permission to engage in an activity such as the practice of medicine. So, any private
healthcare facility in Egypt can’t practice medicine in any form with patients without this
license. A governmental body, Ministry of Health, issues this license according to some
basic requirements that it issue according to law and some regulations. Licensing allows
governmental bodies to ensure that healthcare organizations meet the minimum standards
pursuing the primary objective of protecting the public’s health and safety.
Dr. Ahmed Refat 37
Licensure, certification and accreditation
Certification:
A voluntary process that is designed to ensure competence of an organization based
upon completion of certain requirements and after certain evaluation procedures. It may
be issued through a governmental or non-governmental organization, and it’s usually used
to demonstrate specialized service, so although it’s voluntary, healthcare facilities can’t
perform or offer certain services without gaining the required certifications. Certification is
often non-recurring and typically involves fewer standards than accreditation but a larger
number than licensing.
Dr. Ahmed Refat 38
Licensure, certification and accreditation
So, licensure and certification resemble in that both of them are required
to initiate the service. One is required to initiate the service at the first place
and the other is required to add some specialized service within the facility.
They also resemble each other in that they are granted once and for life and
mostly don’t require further follow-up and continuous improvement.
Dr. Ahmed Refat 39
Licensure, certification and accreditation
Accreditation:
WHO defines accreditation as “An external assessment against predefined, evidence-based
requirements or standards, and the use of standardized quantitative and qualitative
metrics to evaluate, recommend improvements to and report on levels of quality, from
clinical and organizational perspectives, in health facilities or organizations.”
Dr. Ahmed Refat 40
Licensure, certification and accreditation
Accreditation:
This is pure voluntary action that healthcare facilities go through in order to establish
confidence in the operating system within the facility. Accreditation is done through non-
governmental organizations that have certain standards and guidelines through which
they help healthcare facilities implement organizational structures and processes of care
to achieve better results in all areas. It’s repeated every 2-4 years depending on the
policies of the accreditation body.
Dr. Ahmed Refat 41
Licensure, certification and accreditation
Accreditation:
Here are other definitions for accreditation:
- ISQua: A self-assessment and external peer review process used by health and social
care organisations to accurately assess their level of performance in relation to
established standards and to implement ways to continuously improve the health or
social care system.
- WHO, World Bank & OECD: the public recognition, by an external body (public sector,
non-profit or for-profit), of an organization’s level of performance across a core set of
prespecified standards.
Dr. Ahmed Refat 42
Licensure, certification and accreditation
As an ongoing process with periodic renewals, accreditation offers the
pathway that healthcare institutions can implement to produce continuous
improvements in the healthcare quality they serve, and this is the main
difference between accreditation and any other external evaluations. When
we talk about accreditation, we skip talking about minimum standards and
requirements and we skip talking about once in a lifetime evaluations.
Instead, we are talking about culture, attitude and system changes that will
drive the facility into a continuous cycle of internal and external evaluations
to ensure targeting the optimal levels of quality healthcare.
Dr. Ahmed Refat 43
Licensure, certification and accreditation
So, to summarize,
• Accreditation is a form of voluntary external evaluation for healthcare facilities by a
independent agency
• It results in recognition of the facility’s compliance with certain pre-established
standards that allow for quality improvement.
• The quality improvement cycles initiated by accreditation, recommendations and re-
accreditation is not present in licensing and certification which are granted for life.
• Some time accreditation become the trigger for adjustments in the provision of care to
patients in healthcare facilities if it identifies deficiencies in this care through the
assessment process.
Dr. Ahmed Refat 44
Does accreditation work?
What is in it for all of us?
The major question everyone asks when you start talking about
accreditation programs is “ Why should we go this mile?” “What is the
benefit of all this extra work?”. And frankly speaking, it’s a very logical
question. So, we need to discuss it on various levels.
Dr. Ahmed Refat 45
Does accreditation work?
What is in it for all of us?
Hospital\Facility level:
Major organizational structural changes had been reported in healthcare
facilities that have undergone accreditation or being prepared for it. These
changes were mostly evident in regard to the quality of care and the safety
of healthcare providers and receivers when care is delivered. Safer care
results from adherence to standard and regulatory measures governing
each step of care provision, and this safer care is more likely to reduce the
risks and adverse events.
Dr. Ahmed Refat 46
Does accreditation work?
What is in it for all of us?
Hospital\Facility level:
Another aspect of relevance to the facility is the cost reduction, as more
efficient and higher quality processes result in fewer medical diagnostics,
procedures and complications. Relating the provision of services to
standards and regulations reduces variations between different providers
and eventually moves the service provision into somewhat a unified pattern
that is based upon widely or internationally accepted standards.
Dr. Ahmed Refat 47
Does accreditation work?
What is in it for all of us?
Hospital\Facility level:
The variation that quality and standardization aims to reduce is in most
of cases the gap between the ideal outcome that you aim for and the actual
outcome. Eventually, one of these variations (fewer cases) may end up into
unacceptable behavior\performance\service\procedure that may harm the
hospital\facility legally, financially or on the market share level.
Dr. Ahmed Refat 48
Does accreditation work?
What is in it for all of us?
Healthcare professionals' level:
Accreditation programs always stress on the communication between
team members included in the provision of healthcare services. This
communication fosters the culture of teamwork and allows each one to
understand his duties and contributions to the facility’s mission. Better
communication allows for best practices to be shared amongst
practitioners.
Dr. Ahmed Refat 49
Does accreditation work?
What is in it for all of us?
Healthcare professionals' level:
Another advantage you get when you go for accreditation is that culture
of safety you plant inside the organization. The cooperation between team
members of healthcare practitioners to provide the best possible service,
according to the standards and guidelines provided by the accreditation
system you are working through, provides them with a feeling that they are
in one team and they can perform better together.
Dr. Ahmed Refat 50
Does accreditation work?
What is in it for all of us?
Patients and Community:
Patients usually see the accredited healthcare facility as one that have a
very strict system that governs all the phases of healthcare delivery and
they trust the healthcare professionals working in such facilities as being
qualified, trained and organized enough to put their lives in their hands.
Adherence to standardization of healthcare practices results in better
clinical outcomes and this is the main aim, if not the only aim, of patients
admitted into hospitals.
Dr. Ahmed Refat 51
Does accreditation work?
What is in it for all of us?
If you investigate the previous levels of benefits of accreditation on
hospitals and on healthcare professionals, you will understand that their
benefits are eventually the benefits for the patients and that all three levels
interact with each other and eventually building a safe environment for
healthcare service.
Dr. Ahmed Refat 52
Types of accreditation bodies
JCI (Joint Commission International)
An independent non-profit organization established in USA and have cooperation with
healthcare facilities in over 100 countries worldwide. Its aim is to improve the safety and
quality of care internationally and to enhance the commitment of healthcare facilities
worldwide to patient safety. The gold seal of JCI is the most famous icon in the field of
healthcare quality and accreditation.
Dr. Ahmed Refat 53
Types of accreditation bodies
JCI (Joint Commission International)
8 hospital programs, 3 ambulatory care programs and 1 laboratory in Egypt have JCI
accreditation. The first healthcare facility to acquire the gold seal in Egypt was Dar Al Fouad
Hospital in July 2005 and the last one was Sharm International Hospital in December 2022.
The only lab in Egypt to acquire the JCI accreditation was Acculab in July 2018 and
International Eye Hospital, Magrabi Eye hospital and Baheya Center have had their
ambulatory care programs accredited. KSA has 112 JCI accreditations while UAE has an
astonishing 217.
Dr. Ahmed Refat 54
Types of accreditation bodies
CBAHI
Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) was first
established in Makkah in 2001 as an independent council for ensuring the application of
total quality management principles in Makkah region. In 2005, its authorities and activities
included all of Saudi Arabia and they had their 1st set of standards set in 2006. It acquired
its own accreditation from ISQua in 2012 and by late 2013 it became an obligation for all
healthcare facilities operating in Saudi Arabia to be accredited by CBAHI.
Dr. Ahmed Refat 55
Types of accreditation bodies
CBAHI
They have 3 types of accreditation; one for hospitals, another is for primary healthcare
centers PHC and the other is for laboratories and blood banks. The accreditation is valid for
3 years and the hospital will undergo the same assessment again.
Dr. Ahmed Refat 56
Types of accreditation bodies
Accreditation Canada
This is the accreditation body from Canada and it’s not working only in Canada of
course. They are operating in over 38 countries worldwide in more than 15000 locations.
Out of these 38 countries, 10 are Arab countries spanning from Qatar (which have the
largest number of facilities accredited by AC), UAE and Bahrain in the east to Morocco in
the west. Egypt has only one hospital that is accredited by Accreditation Canada which
Saudi German Hospital.
Dr. Ahmed Refat 57
Types of accreditation bodies
GAHAR
General Authority for Healthcare Accreditation and Regulations GAHAR was established
in 2018 as an independent authority under a special Egyptian law that entitles it the right
to issue the standards for healthcare quality and to accredit the institutions that
successfully implement it in along with the launch of the Universal Health Insurance. We
now have 21 GAHAR-accredited hospitals in Egypt, 12 of these are related to Egypt’s
Healthcare authority, 3 are private sector hospitals and the rest are distributed among civil
associations, military, police, and university hospitals.
Dr. Ahmed Refat 58
Accreditation Process by GAHAR
Online applications are made on the website and required documents are uploaded
with a proposed date for the survey. The survey team will go back into the hospital’s
records and documentations to ensure its compliance with the required standard
throughout the look-back period. Registered hospitals seeking accreditation for the first
time will be reviewed for compliance with National Safety Requirements for all the period
of time since the registration till the survey date and will be assessed for the rest of GAHAR
requirements through the previous four months. Previously accredited hospitals will be
reviewed for compliance since the day of the previous accreditation.
Dr. Ahmed Refat 59
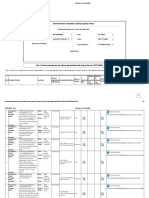
Accreditation Process by GAHAR
Scoring:
• Met: when the hospital shows 80% or more compliance with the requirements with
total score of 2
• Partially met: when the hospital shows less than 80% but more than or equal to 50%
• Not met: when the hospital shows less than 50% compliance with the requirements
• Not applicable: when the surveyor determines that the standard’s requirements are out
of the hospital’s scope.
Dr. Ahmed Refat 60
Accreditation Process by GAHAR
Decisions:
• 3 years accreditation: overall compliance of 80% or more & each chapter scores not less than 70%
& no single whole standard scored not met & no single NSR standard scored not met.
• 2 years conditioned accreditation: overall compliance of 70% to less than 80% or each chapter
scores not less than 60% or one standard per chapter scored not met and no single NSR standard
scored not met.
• 1 year conditioned accreditation: overall compliance of 60% to less than 70% or each chapter
scores not less than 50% or two standards per chapter scored not met and no single NSR standard
scored not met.
• Rejection: overall compliance less than 60% or one chapter scored less than 50% or more than
two standards per chapter scored not met or one single NSR standard scored not met.
Dr. Ahmed Refat 61
National Safety Requirements
General patient safety
NSR. 01 Patient identification NSR. 02 Verbal & Telephone orders
NSR. 03 Hand hygiene NSR. 04 Catheter and tube misconnection
NSR. 05 Fall screening and prevention NSR. 06 Pressure ulcer prevention
NSR. 07 Handover communication NSR. 08 Critical alarms
NSR. 09 Recognition and response to clinical NSR. 10 Venous thromboembolism reduction
deterioration
NSR. 11 Critical results
Dr. Ahmed Refat 62
National Safety Requirements
Patient Identification NSR.01 ACT.03
Accurate patient identification through at least 2 identifiers to identify the patient and
other elements associated with his\her plan of care.
Hospital should have a policy to define:
• The 2 identifiers used for patient identification (name, date of birth, national ID,…)
• Situations requiring patient identification
• Tools and methods used to declare the identification
• Elements of care associated with patient identifier
• Special situations when this policy will not apply (newborn, accidents, disaster,…)
Dr. Ahmed Refat 63
National Safety Requirements
Patient Identification NSR.01 ACT.03
Hazards of incorrect patient Points of patient identification
identification
Dr. Ahmed Refat 64
National Safety Requirements
Verbal And Telephone Orders NSR.02 ICD.18
The hospital develops and implements a policy & procedures for receiving verbal and
telephone orders that addresses:
• Verbal orders
• Telephone orders
• Process of recording
• Read-back by the recipient
Dr. Ahmed Refat 65
National Safety Requirements
Verbal And Telephone Orders NSR.02 ICD.18
Dr. Ahmed Refat 66
National Safety Requirements
Hand hygiene NSR.03 ICD.18
Evidence-based hand hygiene guidelines are adopted & implemented throughout the
hospital to prevent healthcare acquired infections. The survey addresses:
• Healthcare professionals are trained for policies and procedures
• Hand hygiene posters and instructions, facilities and supplies are distributed at point of
relevance.
• Healthcare professionals comply with the policy and procedures.
Dr. Ahmed Refat 67
National Safety Requirements
Hand hygiene NSR.03 ICD.18
Dr. Ahmed Refat 68
National Safety Requirements
Catheter and tube misconnections NSR.04 ICD.35
Systems are implemented to prevent catheter and tube misconnections. The hospital
develops a policy and procedures for this cause, and it addresses:
• Responsibilty of connections and misconnection of tubes shouldn’t be left to non-
clinical staff.
• Labeling of high risk catheters.
• Avoidance of use of catheters with injection ports for these applications.
• Tracing all points from origins to attachment ports before making any connections,
reconnections or administering
Dr. Ahmed Refat 69
National Safety Requirements
Fall screening and prevention NSR.05 ICD.11
Patient’s risk of falling is screened, assessed, periodically reassessed and managed safely &
effectively. The hospital must develop and implement a policy that addresses fall screening
and prevention addressing:
• Patient risk screening at admission including medication and other factors with definite
timeframe for completion of assessment
• Frequency of reassessment with tailored care plans
• Methods of reducing fall risks (call system, corridor bars, bathroom bars, bedside rails,
wheelchairs and trolleys with locks).
Dr. Ahmed Refat 70
National Safety Requirements
Fall screening and prevention NSR.05 ICD.11
Dr. Ahmed Refat 71
National Safety Requirements
Pressure ulcer prevention NSR.06 ICD.12
Patient’s risk of developing pressure ulcers is screened, assessed, periodically reassessed
and managed safely & effectively. The hospital must develop and implement a policy that
addresses fall screening and prevention addressing:
• Patient risk screening at admission including skin assessment and other factors with
definite timeframe for completion of assessment
• Frequency of reassessment with tailored care plans
• Methods of reducing risk of pressure ulcers (pressure relieving devices & mattresses ).
Dr. Ahmed Refat 72
National Safety Requirements
Pressure ulcer prevention NSR.06 ICD.12
Dr. Ahmed Refat 73
National Safety Requirements
Handover communication NSR.07 ACT.09
A standardized approach to handover communication including an opportunity to ask &
respond to questions is implemented. The policy adopted by the hospital must address:
• A framework of communication and the occasions when it’s used.
• The requirements of staff presence, suitable environment and their responsibilities
• The recording of this handover and that the staff is well oriented to it
Dr. Ahmed Refat 74
National Safety Requirements
Handover communication NSR.07 ACT.09
Dr. Ahmed Refat 75
National Safety Requirements
Critical Alarms NSR.08 ICD.37
The hospital has an approved policy & procedures for managing critical alarms. The
hospital provides the staff members with enough training to understand and interpret the
different alarms for machines dealing with patients and how they should respond to each
of them. The policy adopted by the hospital must address:
• Inventory of critical alarms, their priorities and continuous testing
• Maintenance records with schedules, agreed settings, evidence of function and
malfunctions.
• Staff is aware with critical alarms, and they are trained for dealing with them.
Dr. Ahmed Refat 76
National Safety Requirements
Recognition of and response to clinical deterioration NSR.09 ICD.37
The hospital has an approved policy & procedures to ensure hospital-wide recognition of
and response to clinical deterioration. The hospital has a defined criteria for recognition of
clinical deterioration and the staff is educated about it. The policy adopted by the hospital
must address:
• Defining the criteria and educating the staff about it with defined responsibilities,
mechanism of response and time frame
• The response of teams is uniform and recorded together with the management of cases
• The assigned staff members are qualified and capable of handling these situations.
Dr. Ahmed Refat 77
National Safety Requirements
Venous thromboembolism reduction NSR.10 ICD.13
Patient’s risk of developing venous thromboembolism (deep venous thrombosis) is
screened, assessed, periodically reassessed and managed safely and effectively. The policy
adopted by the hospital must address:
• Defining the criteria and educating the staff about it with defined responsibilities,
mechanism of response and time frame
• The response of teams is uniform and recorded together with the management of cases
• The assigned staff members are qualified and capable of handling these situations.
Dr. Ahmed Refat 78
National Safety Requirements
Critical Results NSR.11 ICD. 30
Critical results are communicated timely, accurately and safely to secure the safety of
patients. The policy adopted by the hospital must include processes related to laboratory,
medical imaging devices, non-interventional cardiology laboratories and it must:
• Defining the list of critical results and values.
• The process of communicating the results and its timeframe including; mean of
communication, date and time, identification of reporting and receiving personnel, the
result of investigation and the measures taken in response.
• Records of this communication should be present at the areas of investigation and in
different sites of patient interaction with hospital staff.
Dr. Ahmed Refat 79
National Safety Requirements
Critical Results NSR.11 ICD. 30
Critical results are communicated timely, accurately and safely to secure the safety of
patients. The policy adopted by the hospital must include processes related to laboratory,
medical imaging devices, non-interventional cardiology laboratories and it must:
• Defining the list of critical results and values.
• The process of communicating the results and its timeframe including; mean of
communication, date and time, identification of reporting and receiving personnel, the
result of investigation and the measures taken in response.
• Records of this communication should be present at the areas of investigation and in
different sites of patient interaction with hospital staff.
Dr. Ahmed Refat 80
National Safety Requirements
Medication management and safety
NSR. 12 Abbreviations NSR. 13 Medication Reconciliation
NSR. 14 Medication storage and labelling NSR. 15 High alert medications and concentrated
electrolytes
NSR. 16 Look-alike and sound-alike medication
Dr. Ahmed Refat 81
National Safety Requirements
Abbreviations NSR.12 IMT. 04
The hospital defines standardized diagnosis codes, procedure codes, definitions, symbols
and abbreviations. The use of codes is done to squeeze writing into small spaces and save
time, but this may cause problems and harm if misinterpretation occurs. The hospital must:
• Define a list of approved symbols and abbreviations and another list of forbidden ones.
• Ensure the implementation of forbidden abbreviations list is delivered, understood and
applied by all healthcare professional.
• Situations when symbols and abbreviations are not allowed. (consents, discharge
summary)
Dr. Ahmed Refat 82
National Safety Requirements
Abbreviations NSR.12 IMT. 04
Dr. Ahmed Refat 83
National Safety Requirements
Medication Reconciliation NSR.13 MMS.10
Medications are reconciled across all interfaces of care in the hospital. This is a multi
disciplinary process requiring interaction between physicians, nurses, pharmacists and
other clinicians to avoid duplication of medication, omitting needed ones or incorrect
dosages. The hospital must
• Define situations where medication reconciliation is required (admission, during stay,
before discharge) and who is responsible for it and set a timeframe for its completion.
• Make sure that patients and their families are involved in this process
Dr. Ahmed Refat 84
National Safety Requirements
Medication Storage and labelling NSR.14 MMS.04
Medications are safely and securely stored in stores, pharmacies and patient-care areas
according to laws and regulation as this can reduce waste, incorrect dispensing, handling
and incidences of missed doses. Medications removed from their original containers into
unlabeled ones may result in tragic results. Also, appropriate storage conditions to protect
the stability of medications is a must. The policy must aim at:
• Maintaining safe & secured storage conditions and consistent with manufacturer’s
advice.
• Psychotropic, controlled and narcotic medications are stored are stored according to
laws and regulation
Dr. Ahmed Refat 85
National Safety Requirements
Medication Storage and labelling NSR.14 MMS.04
• An approved process of the use and storage of multi-dose medications.
• An approved process to deal with electric power outages
Dr. Ahmed Refat 86
National Safety Requirements
High alert medications and concentrated electrolytes NSR.15 MMS.06
High alert medications and concentrated electrolytes are identified, stored and dispensed
in a way that assures risk is minimized. High-alert medications are those with heightened
risk of harm to the patients if used in error. Concentrated electrolytes are like potassium ≥
2mEq/ml, potassium phosphate ≥ 3mmol/ml, sodium chloride ≥ 0.9% and magnesium
sulfate ≥ 50%. The policy must define:
• List all the high alert medications and all concentrated electrolytes used I the hospital.
• Strategies put into action to prevent inadvertent use & administration of these
medication.
Dr. Ahmed Refat 87
National Safety Requirements
Look-alike & sound-alike medication NSR.16 MMS.07
These are medications that are visually similar in similar appearance or packaging and
names of medications that have spelling similarities &/or phonetics. Confusion between
these medications may lead to harm, thus those medications must be high lightened and
physically separated. The hospital’s policy will:
• List all look-alike and sound-alike medications
• Define the storage and labelling requirements
• Define the dispensing requirements
Dr. Ahmed Refat 88
National Safety Requirements
Surgical, anesthesia and sedation
NSR. 17 Surgical site marking NSR. 18 Preoperative checklist
NSR. 19 Time-out NSR. 20 Instrument retention prevention
Dr. Ahmed Refat 89
National Safety Requirements
Surgical site marking NSR.17 SAS.05
Precise site where a surgery or invasive procedure shall be performed is clearly marked by
the physician with patient’s involvement by visible and clear right marking as an error
reduction strategy. (or a relative in case of children or teenagers or unconscious patients).
The hospital’s policy will:
• Ensure the staff is trained for the site marking and there is a unified mark across all
hospital sections.
• Define the timeframe for completing the site marking before the call for surgery.
Dr. Ahmed Refat 90
National Safety Requirements
Preoperative checklist NSR.18 SAS.06
Documents and equipment needed for procedure and anesthesia or sedation are verified
to be at hand, correct and properly functioning before calling the patient to prevent the
errors of using malfunctioning equipment or cancellation of surgery. Equipment sets can be
differed according to the type of surgery, invasive procedure, sedation or anesthesia. The
hospital’s policy assures:
• Preoperative verification is made before calling the patient
• Checklists are made, used and analyzed for improvement opportunities.
Dr. Ahmed Refat 91
National Safety Requirements
Time-Out NSR.19 SAS.07
Correct patient, procedure and body part is confirmed preoperatively and just before
starting a surgical or invasive procedure. The staff should also verify that the patient had
their prophylactic antibiotic or required medication before the operation. The hospital’s
policy assures:
• Preoperative timeout is made before the start of surgery involving the surgeon, nurse
and anesthesiologist.
• Checklists are made, used and analyzed for improvement opportunities.
Dr. Ahmed Refat 92
National Safety Requirements
Instrument retention prevention NSR.20 SAS.09
Accurate counting of sponges, needles and instruments pre and post procedure is verified
as missing any of these inside the patient’s body will cause serious morbidity in forms of
pain, sepsis or organ injury and will require reopening the patient’s body and may cause
morbidity. The hospital’s policy assures:
• Counting consumables is done pre, during and post surgery by two staff (the second is a
witness)
• Records are made with these instruments with the confirmation of the surgeon.
Dr. Ahmed Refat 93
National Safety Requirements
Environmental and facility safety
NSR. 21 Fire safety NSR. 22 Fire drill
NSR. 23 Hazardous material safety NSR. 24 Safety management plan
NSR. 25 Radiation safety program NSR. 26 Laboratory safety program
NSR. 27 Medical equipment safety NSR. 28 Utilities safety
Dr. Ahmed Refat 94
National Safety Requirements
Fire safety NSR.21 EFS.03
Fire and smoke safety plans address prevention, early detection, response and safe
evacuation in case of fire and/or other internal emergencies. In the event of fire,
suppression equipment need to be readily accessible to combat these fires with enough
and variable knowledge of staff of how to use these equipment, not cause panic and
evacuate safely if needed. The hospital’s policy assures:
• An ongoing risk assessment including:
– Compliance with civil defense regulations and with fire and building codes
– Fire and smoke separation for areas under construction and those with high risks
– Safety of all occupants including patients, families, staff, visitors and other personnel
Dr. Ahmed Refat 95
National Safety Requirements
Fire safety NSR.21 EFS.03
• An ongoing risk assessment including:
– Fire suppression systems are present in different areas of the hospital according to the content of each
department. Periodic inspection of these equipment is made.
• RACE and PASS drills are made
• Assigned responsibilities are oriented to all staff including high-risk patients evacuation
Dr. Ahmed Refat 96
National Safety Requirements
Dr. Ahmed Refat 97
National Safety Requirements
Fire drills NSR.22 EFS.05
Fire drills are performed in different clinical and non-clinical settings including at least one
unannounced drill annually. They are designed to the staff have the knowledge, experience
and self-confidence to operate successfully in the case of fire. A record is made that
includes; dates and timings, participating staff, involved areas, shift, evacuation and
corrective action plan. The hospital will:
• Hold a record will all fire drills and related data
• Train all staff on the RACE & PASS
Dr. Ahmed Refat 98
National Safety Requirements
Hazardous material safety NSR.23 EFS.06
The hospital plans safe handling, storage, usage and transportation of hazardous materials
(which are chemical materials that can pose a threat to the environment, life or health) and
waste disposal. These include; explosive, flammable, combustible and radioactive
materials. Hospital waste is all waste generated in any clinical setting while interacting with
a patient.
• An updated list of hazardous materials should be present with corresponding safety data
sheet
• Appropriate labelling, safe storage, handling and usage should be available.
• Required protective equipment and spill kits are available
Dr. Ahmed Refat 99
National Safety Requirements
Hazardous material safety NSR.23 EFS.06
• Documentation and investigation of different spill incidents and staff handling the spills
• Compliance of laws and regulation and availability of special licenses
• The evaluation includes
– Reviewing the program to ensure it’s covering all materials that are handled within the hospital
– Ensuring the safety of all staff dealing with hazardous materials and waste
– Safe storage, handling and usage of those materials
– Policies and procedures are clear for handling spill and exposure events
Dr. Ahmed Refat 100
National Safety Requirements
Hazardous material safety NSR.23 EFS.06
Dr. Ahmed Refat 101
National Safety Requirements
Safety management plan NSR.24 EFS.07
A safe work environment plan addresses high-risk areas, procedures, risk mitigation
requirements, tools and responsibilities. The hospital must have a safety plan that covers
building, property, medical equipment and systems to ensure safe physical environment
including periodic risk assessment, plans to prevent accidents, safety trainings depending
on job hazards, etc
• The evaluation includes
– Reviewing the safety plan
– Staff is aware of it and safety measures are implemented
– Instructions are posted in all risk areas
Dr. Ahmed Refat 102
National Safety Requirements
Safety management plan NSR.24 EFS.07
Safety plan includes:
• Proactive risk assessment
• Effective planning to prevent accidents and injuries
• Processes for pest and rodent control
• Identification of potential risks of system failure or staff behavior
• Regular inspection with documentation of results, corrective actions and follow up
• Safety training
Dr. Ahmed Refat 103
National Safety Requirements
Radiation safety program NSR.25 DAS.09
Radiation safety program is developed and implemented providing information and
training on the theory, hazards, biological effects, protective measures monitoring and
disposal of radioactive materials. The policy should aim at:
• Compliance with laws and regulations
• Ionizing and non-ionizing radiation equipment are maintained and calibrated
• Minimizing dosage exposure for patients and staff.
• Staff personal protective equipment are available
Dr. Ahmed Refat 104
National Safety Requirements
Laboratory safety program NSR.26 DAS.24
A comprehensive documented laboratory safety program is implemented including
chemical, biological, physical and radioactive hazards. A safety programs should be desined
to maintain a safe environment for staff, patients and families including at least:
• Safety measures for healthcare professional, specimen, environment and equipment
• Incidents handling and corrective action plans
• Proper disposal of laboratory waste
• Material safety data sheets (MSDS)
• Handling chemical spills
• Instruction for the use PPEs
Dr. Ahmed Refat 105
National Safety Requirements
Medical equipment safety NSR.27 EFS.10
Medical equipment plan ensures safe selection, inspection testing, maintenance, and use
of medical equipment. Lazy and incompetent monitoring and management of medical
equipment lead to inefficiency and harms to patients. A plan is required to
• Developing criteria for selection of medical equipment, its inspection and testing
• Training staff on its safe usage
• Periodic preventive maintenance and calibration and malfunction management
• Dealing with equipment hazards and adverse events
• Updating, retiring and replacing
Dr. Ahmed Refat 106
National Safety Requirements
Utilities safety NSR.28 EFS.11
Essential utilities plan addresses regular inspection, maintenance, testing and repair
including mechanical, electrical, waste, technology and information management. A plan is
required to
• List all utility key systems, with its layout and staff training
• Regular inspection and testing schedules
• Fuel powered generator management
• Water tanks cleaning, disinfection and testing
Dr. Ahmed Refat 107
IPSGs
International patient safety goals
The World Health Organisation (WHO) define patient safety as “the absence of preventable
harm to a patient during the process of health care and reduction of risk of unnecessary
harm associated with health care to an acceptable minimum”.
134 million adverse events occur in hospitals in low and middle income countries
Dr. Ahmed Refat 108
IPSGs
Dr. Ahmed Refat 109
IPSGs
Dr. Ahmed Refat 110
IPSGs
IPSG NSR
IPSG1 Identify patient correctly NSR 1 Patient Identification
IPSG 2 Improve effective communication NSR 2 Verbal & Telephone Order
NSR 7 Handover communications
NSR 11 Critical Results
IPSG 3 Improve the safety of high-alert NSR 15 High alert medications and
medications concentrated electrolytes
NSR 16 Look-alike and Sound-alike
medications
Dr. Ahmed Refat 111
IPSGs
IPSG NSR
IPSG 4 Ensure safe surgery NSR 17 Surgical site marking
NSR 18 Preoperative checklist
NSR 19 Time-out
NSR 20 Instrument Retention Prevention
IPSG 5 Reduce the risk of health care- NSR 3 Hand hygiene
associated infections NSR 4 Catheter & tube misconnections
IPSG 6 Reduce the risk of patient harm NSR 5 Fall screening and prevention
resulting from falls NSR 24 Safety Management plan
NSR 28 Utilities safety
Dr. Ahmed Refat 112
Tracer methodology
The tracer methodology uses information from an organization to follow the experience of
care, treatment, or services for a number of patients through the organization’s entire
health care delivery process to identify performance issues in one or more step or in the
transition of care between interfaces and settings.
Dr. Ahmed Refat 113
Tracer methodology
Individual tracer methodology:
Designed to “trace” the care experiences that a patient had while receiving services from
the organization. It is a way to analyze the organization’s system of providing care,
treatment or services using actual patients as the framework for assessing standards
compliance. Patients selected for these tracers will likely be those in high-risk areas or
whose diagnosis, age or type of services received may enable the best in-depth evaluation
of the organization’s processes and practices.
Dr. Ahmed Refat 114
Tracer methodology
Individual tracer methodology:
During an individual tracer, the focus is on an individual patient’s experience in the health
care organization. The patient’s record serves as a guide along the path of care. The
surveyor assesses compliance with standards as they relate to the care, treatment, and
services the organization provides to the patient. The surveyor chooses the patient based
on the organization’s care, treatment, and services as well as its top risk areas and the
complexity of the patient’s care.
Dr. Ahmed Refat 115
Tracer methodology
Individual tracer methodology:
Starting where the patient is located, the surveyor first reviews the medical record with the
staff person responsible for the patient’s care. The surveyor then follows the path of
patient care from admission through and possibly beyond discharge (or the end of an
episode of care).
Dr. Ahmed Refat 116
Tracer methodology
Tracers rarely take a straight route. The surveyor diverges onto new paths while following
opportunities for investigation. It may require several tracers to cover everything. Surveyors
can visit—and revisit—any area of the organization related to the care of the patient or the
functioning of a system.
Dr. Ahmed Refat 117
Tracer methodology
Target:
Surveyor targets an individual patient that can give an accurate representation of hospital’s
functions. Tracer patient may change during the course of tracing and new tracer subjects
may also arise.
Dr. Ahmed Refat 118
Tracer methodology
Review:
Surveyor reviews documents as medical records, policies, procedures management plans
and data reports to verify compliance with documentation standards and to clarify issue.
Again, document review may reveal new tracer targets
Dr. Ahmed Refat 119
Tracer methodology
Assess:
Assessment of compliance with standards is done through observations and asking
questions. Some predefined lists of tracer questions are planned at start and others come
by through the course of tracing.
Dr. Ahmed Refat 120
Tracer methodology
Communicate
Surveyor communicates with tracer participants, asking questions and sharing concerns
with various communication skills to create supportive and interactive exchange of
information.
Dr. Ahmed Refat 121
Tracer methodology
Educate :
The surveyor educates tracer participants whenever possible to help organizations solve
compliance problems offering suggestions in an objective, blame-free manner to help
foster cooperation and demonstrate commitment.
Dr. Ahmed Refat 122
Tracer methodology
Report
The surveyor reports the results of the tracer, which are shared in a clear and timely way so
the organization can make any required improvements.
Dr. Ahmed Refat 123
Tracer methodology
Report
The surveyor reports the results of the tracer, which are shared in a clear and timely way so
the organization can make any required improvements.
Dr. Ahmed Refat 124
Tracer methodology
• Medical record department
• What is your process to admit new patients?
• When a patient is admitted, what members of the staff are involved? How are patients and
families involved in the process?
• What methods are used to identify the patient during the registration process?
• If the patient presents at admission with any high-risk factors, such as diabetes or self-harm, what
additional assessments are performed or ordered for referral, if any?
Dr. Ahmed Refat 125
Tracer methodology
Emergency department (Doctor)
• What are your time frames for completion of initial screenings/assessments and how do you
communicate results with staff?
• What kinds of screenings/assessments do you perform? Who conducts them?
• If the patient presents at admission with any high-risk factors, such as diabetes or self-harm, what
additional assessments are performed or ordered for referral, if any?
• Please describe your interdisciplinary care team planning process.
• How is the triage process done in the emergency department?
• How is your pain assessment process done?
• How is the patient’s privacy maintained during patient assessment?
Dr. Ahmed Refat 126
Tracer methodology
Emergency department (Nurse)
• What happens when a patient arrives in the emergency department?
• What is your triage process in the emergency department?
• Please describe your interdisciplinary care team planning process.
• How does the emergency department interface with the radiology department when an x-ray is
needed?
• What is the process to deliver a sample to the laboratory from the emergency department?
Dr. Ahmed Refat 127
Tracer methodology
Emergency department (Patient)
• Did you sign a consent form
• Have you been informed of your financial expectation for your care ,treatment, services?
Dr. Ahmed Refat 128
Tracer methodology
Radiology unit
• Where are the radiation safety equipment used to protect patient and minimize over exposure?
• What are the PPEs used during test performing?
• How does the emergency department interface with the radiology department when an x-ray is
needed?
• How do you identify the patient to ensure that you are performing the ordered radiology test on
the correct patient?
• How are radiology test results communicated back to the ordering provider?
• What are the quality control activity performed on radiology equipment to ensure it is functioning
properly?
Dr. Ahmed Refat 129
Tracer methodology
• Laboratory dept. (Lab doctor)
• How do you document when a test order is made?
• What is your critical values identification policy?
• What is the required timeline for reporting critical result?
• How do you ensure the privacy of test results? What process is in place to secure your electronic
records?
• How do you ensure that the critical values you report are accurate? Where are the reference
ranges for your test results?
Dr. Ahmed Refat 130
Tracer methodology
Laboratory dept. (Lab technician)
• How are the orders communicated to lab and how are the test results communicated back to the
ordering provider?
• Do you keep a logbook for lab equipment calibration & maintenance?
• Who interprets the test results, and how are they sent to the ordering practitioner or provider?
• What are the PPEs used during test performing?
Dr. Ahmed Refat 131
Tracer methodology
ICU& Inpatient (Doctor)
• Where is the referral form for this patient?, What information did you receive from emergency
department?
• How are medications prescribed for your current patients?
• What is your discharge planning process? When does discharge planning begin? Who is involved?
• How do you document the care, treatment, and services you are providing to the patient?
• How is information in the medical record communicated to relevant staff for care planning
purposes
• Please describe your interdisciplinary care team planning process.
Dr. Ahmed Refat 132
Tracer methodology
ICU& Inpatient (Nurse)
• How do you ensure that cleaning and disinfection are performed in a consistent and effective
manner?
• How do you communicate any concerns about skin & pressure ulcers issues during assessment?
• What is the process for assessing a patient for falls risk? What ongoing fall assessments and
reassessments do you conduct?
• What criteria are used for a falls risk designation? What else can trigger a falls risk designation?
• What do you do when you see an environmental risk for falls, such as a spill?
Dr. Ahmed Refat 133
Tracer methodology
ICU& Inpatient (Nurse)
• What kind of family education do you provide? Can I see what information you provide them?
• What are your protocols for preventing CLABSIs – CAUTIs -VAP?
• How do you confirm the patient’s identity for medication administration?
• What are the high-alert and hazardous medications you keep in the facility?
• How do you maintain patient confidentiality?
• How do you attend to hand hygiene policies and procedures?
• What measures are active to handle hazardous waste segregation policies and procedures?
Dr. Ahmed Refat 134
Tracer methodology
ICU& Inpatient (Patient)
• What tests did you undergo? Were you informed of the reasons and the results of each test?
• What were you told about the forms that you signed?
Dr. Ahmed Refat 135
Tracer methodology
Hemodialysis (Doctor)
• How do you monitor the patients on anti-coagulant therapies?
• Where do you record the and follow up with the dialysis regimen for this patient?
• Were you vaccinated and periodically tested for viral infections?
Dr. Ahmed Refat 136
Tracer methodology
Hemodialysis (Nurse)
• How do you ensure that cleaning and disinfection are performed in a consistent and effective
manner?
• How do you ensure that manufacturer’s guidelines for the type of high-level disinfectant solutions
used are available to staff?
• Describe your vaccination program. Who is in charge of managing the program?
• How do you handle blood transfusion orders and consents?
Dr. Ahmed Refat 137
Tracer methodology
Hemodialysis (Patient)
• Instruction given to patient regarding hemodialysis procedure ,anti-coagulant therapy drug
interaction
• Discharge summary for patient, prescribed medication, activity ,follow up
Dr. Ahmed Refat 138
You might also like
- CBMEC - Skilled Care PharmacyDocument3 pagesCBMEC - Skilled Care PharmacyNors Pataytay67% (3)
- Quality and Performance Excellence 8E Chapter 1Document44 pagesQuality and Performance Excellence 8E Chapter 1Aisah Reem100% (1)
- Business Ethics & Customer SatisfactionDocument12 pagesBusiness Ethics & Customer SatisfactionNeha Jain0% (1)
- Shortcuts in Esthetic DentistryDocument1 pageShortcuts in Esthetic DentistryGabriel Lazar100% (1)
- Polyhedron #140 - Llurth DreierDocument8 pagesPolyhedron #140 - Llurth DreierGeorge Krashos100% (1)
- Armitage's Garden Annuals A Color Encyclopedia, 2004Document368 pagesArmitage's Garden Annuals A Color Encyclopedia, 2004iuliabogdan22100% (8)
- 10 1 1 695 3351Document3 pages10 1 1 695 3351mahadabrata21No ratings yet
- HIM403 2 Material Unit 1Document46 pagesHIM403 2 Material Unit 1Diana GraceNo ratings yet
- Healthcare Quality ConceptsDocument28 pagesHealthcare Quality Conceptsmatrixkhalifa9955No ratings yet
- Quality Assurance (Autosaved)Document75 pagesQuality Assurance (Autosaved)OGU CourageNo ratings yet
- Quality AssuranceDocument57 pagesQuality AssuranceAmy Lalringhluani67% (3)
- T Q M C: Otal Uality Anagement OnceptsDocument6 pagesT Q M C: Otal Uality Anagement OnceptsSaif Ur RahmanNo ratings yet
- 8 Quality Management PrinciplesDocument3 pages8 Quality Management PrinciplesNik NurfarahiyahNo ratings yet
- QMS-Concept Note (MERF)Document4 pagesQMS-Concept Note (MERF)mba07-807No ratings yet
- Inspection: Introduction To QualityDocument10 pagesInspection: Introduction To QualityTseniNo ratings yet
- Quality AssuranceDocument31 pagesQuality Assurancebemina ja100% (1)
- Applications of Quality ControlDocument8 pagesApplications of Quality Controlritesh MishraNo ratings yet
- Quality Assurance: An Introduction For Healthcare ProfessionalsDocument38 pagesQuality Assurance: An Introduction For Healthcare ProfessionalsZuraidah WahabNo ratings yet
- QualityDocument5 pagesQualityKairuz Demson AquilamNo ratings yet
- QMSDocument124 pagesQMSPatrick OmpadNo ratings yet
- IILM Institute For Higher Education: Quality Management ProjectDocument10 pagesIILM Institute For Higher Education: Quality Management ProjectPratibha JainNo ratings yet
- Quality Management System ModuleDocument181 pagesQuality Management System ModuleJhonrick MagtibayNo ratings yet
- TQM in HealthcareDocument4 pagesTQM in HealthcareALtit66No ratings yet
- Quality Control & Quality Improvement: Under SupervisionDocument20 pagesQuality Control & Quality Improvement: Under Supervisionheba abd elazizNo ratings yet
- Quality and Internal Audit: Chartered Institute of Internal AuditorsDocument4 pagesQuality and Internal Audit: Chartered Institute of Internal AuditorsAryNo ratings yet
- Ads411 (Tutorial)Document2 pagesAds411 (Tutorial)Nur Diana NorlanNo ratings yet
- Cebu Normal University Graduate StudiesDocument21 pagesCebu Normal University Graduate StudiesDoroy ManlosaNo ratings yet
- Quality Management Q&ADocument11 pagesQuality Management Q&AMuhaimin ShahNo ratings yet
- Chapter 11 Total Quality ManagementDocument17 pagesChapter 11 Total Quality Managementdubeyvimal389No ratings yet
- Total Quality Management in HealthcareDocument4 pagesTotal Quality Management in HealthcarePulkit JainNo ratings yet
- Introduction To Quality and Performance ExcellenceDocument44 pagesIntroduction To Quality and Performance ExcellenceenockNo ratings yet
- All LOs Establish Quality Standard PDFDocument20 pagesAll LOs Establish Quality Standard PDFHabteNo ratings yet
- Concept of Total Quality ManagementDocument13 pagesConcept of Total Quality ManagementXavel ZangNo ratings yet
- Developing Standars QSM LXZHYN TALARO GROUP 3Document15 pagesDeveloping Standars QSM LXZHYN TALARO GROUP 3jeri miahNo ratings yet
- Establish Quality StandardDocument75 pagesEstablish Quality StandardJaleto sunkemo100% (1)
- Final CPHQ April 18 HandoutsDocument404 pagesFinal CPHQ April 18 HandoutsNisreen Mahaya100% (4)
- Quality in Healthcare and AccreditationDocument27 pagesQuality in Healthcare and AccreditationManigandanNo ratings yet
- Quality Management in HospitalDocument18 pagesQuality Management in HospitalDr. Asma Qureshi100% (1)
- ERP - Part A (B. Ingris) Mohamad AlfiantoDocument2 pagesERP - Part A (B. Ingris) Mohamad Alfiantomohamad alfiantoNo ratings yet
- Apply Quality ControlDocument42 pagesApply Quality Controlteka atsbha100% (1)
- 1 Chapter 1 IntroductionDocument61 pages1 Chapter 1 IntroductionInquisitor SultanNo ratings yet
- Final Year ProjectDocument94 pagesFinal Year Projectgaurav75% (4)
- Total Quality ManagementDocument18 pagesTotal Quality ManagementOlusegun OlugbadeNo ratings yet
- Quality ManagementDocument13 pagesQuality ManagementDivya ToppoNo ratings yet
- Quality Management & AuditingDocument14 pagesQuality Management & AuditingengramdadcmoshNo ratings yet
- TQM To Print in LongDocument50 pagesTQM To Print in LongMedwin Adam VillapandoNo ratings yet
- Quality Assurance in NursingDocument4 pagesQuality Assurance in NursingWaaberrin100% (2)
- ReviewerDocument6 pagesReviewerJulaiza Mae SartoriusNo ratings yet
- Quality Assurance SeminarDocument26 pagesQuality Assurance Seminarselja100% (6)
- Implementing The New Quality Assurance Framework: By: Christine Joy Alonday Bsn4Document8 pagesImplementing The New Quality Assurance Framework: By: Christine Joy Alonday Bsn4yasiraNo ratings yet
- Total Quality Management in Healthcare TDocument5 pagesTotal Quality Management in Healthcare TLukasNo ratings yet
- Quality Assurance in Perioperative NursingDocument39 pagesQuality Assurance in Perioperative NursingbummyNo ratings yet
- Quality Assurance in NursingDocument12 pagesQuality Assurance in NursingPhebeDimple100% (3)
- Unit 9 - Customer SatisfactionDocument7 pagesUnit 9 - Customer SatisfactionMark Bacuel100% (1)
- Total Quality Management ReportDocument37 pagesTotal Quality Management Reportmonir61No ratings yet
- Diagnostic Care Management PaperDocument40 pagesDiagnostic Care Management PaperPatrick Louie MaglayaNo ratings yet
- Quality Management Essay 2.editedDocument18 pagesQuality Management Essay 2.editedJohn Mureithi NjugunaNo ratings yet
- ISO Quality Management PrinciplesDocument2 pagesISO Quality Management PrincipleszohaibimranNo ratings yet
- The Total Quality Management: Prof: Mohammad Al NuaimiDocument53 pagesThe Total Quality Management: Prof: Mohammad Al NuaimiRaghad MasarwehNo ratings yet
- TQM Lec 1Document15 pagesTQM Lec 1Dina Lutfy SharafNo ratings yet
- Quality ControlDocument7 pagesQuality Controlritesh MishraNo ratings yet
- Establishqualitystandard 210614091508Document75 pagesEstablishqualitystandard 210614091508Asegid AyeleNo ratings yet
- DLL - Tle 6 - Q4 - W8Document4 pagesDLL - Tle 6 - Q4 - W8RafaelNo ratings yet
- Peony Patterns Myrtle Printable Skirt PiecesDocument30 pagesPeony Patterns Myrtle Printable Skirt PiecesVanessa PinedaNo ratings yet
- Database Concepts Class 12 Computer ScienceDocument13 pagesDatabase Concepts Class 12 Computer ScienceShaku Joshi100% (1)
- 5 CFLM 1 Related Philippine LawsDocument37 pages5 CFLM 1 Related Philippine LawsAlex LagardeNo ratings yet
- AMC Process in Plant Maintenance: Kalyan ChakravarthiDocument9 pagesAMC Process in Plant Maintenance: Kalyan Chakravarthivadiraj tanjoreNo ratings yet
- Pipe NotesDocument3 pagesPipe NotesAndiappan PillaiNo ratings yet
- Colorful Brush Strokes Presentation TemplateDocument12 pagesColorful Brush Strokes Presentation TemplateEllen Mae M. CabadingNo ratings yet
- Maven & Junit IntroductionDocument25 pagesMaven & Junit IntroductionAmine BesrourNo ratings yet
- Dynamics of Rigid Bodies: Work and EnergyDocument11 pagesDynamics of Rigid Bodies: Work and EnergyJancis TugadeNo ratings yet
- Employee Separation and Retention: Source: Mcgraw Hill, Human Resource Management, Noe Et El 2016Document29 pagesEmployee Separation and Retention: Source: Mcgraw Hill, Human Resource Management, Noe Et El 2016Dennis Alea100% (1)
- The Depression Anxiety Stress Scales: Skala Tekanan, Kebimbangan, Dan Kemurungan (Dass-21)Document2 pagesThe Depression Anxiety Stress Scales: Skala Tekanan, Kebimbangan, Dan Kemurungan (Dass-21)Calla Yee100% (3)
- Residual DepositsDocument3 pagesResidual Depositsyosia luther100% (1)
- Plastic Materials - AcronymsDocument4 pagesPlastic Materials - Acronymsabhi030689No ratings yet
- Types of MarriagesDocument4 pagesTypes of MarriagesManushi YadavNo ratings yet
- My Courses: Home UGRD-GE6114-2113T Week 10: Midterm Examination Midterm ExamDocument11 pagesMy Courses: Home UGRD-GE6114-2113T Week 10: Midterm Examination Midterm ExamMiguel Angelo GarciaNo ratings yet
- AN/PRC-150 (C) : Applications HandbookDocument36 pagesAN/PRC-150 (C) : Applications HandbookMag Fhearadhaigh100% (2)
- Facts About Ecological ImbalanceDocument4 pagesFacts About Ecological ImbalanceSIKHA A SNo ratings yet
- Support Adform Com Documentation Build Html5 Banners Other Building Tools Google Web DesignerDocument5 pagesSupport Adform Com Documentation Build Html5 Banners Other Building Tools Google Web DesignerMartin_Arrieta_GNo ratings yet
- Secured Data Sharing and Access Control For Cloud Based Data Storage UpdatedDocument5 pagesSecured Data Sharing and Access Control For Cloud Based Data Storage UpdatedBalu NayuduNo ratings yet
- Labor Code Art 156-167Document29 pagesLabor Code Art 156-167Charlotte GallegoNo ratings yet
- Abb AmvacDocument50 pagesAbb AmvacvjrNo ratings yet
- Sporothrix Brasiliensis and Feline Sporotrichosis in The Metropolitan Region of Rio de Janeiro, Brazil (1998-2018)Document14 pagesSporothrix Brasiliensis and Feline Sporotrichosis in The Metropolitan Region of Rio de Janeiro, Brazil (1998-2018)NealNo ratings yet
- Rudolf Dinu - Romanian Foreign Policy 1878-1914 DRAFTDocument30 pagesRudolf Dinu - Romanian Foreign Policy 1878-1914 DRAFTRaulIancuNo ratings yet
- Profibus-According To Iec 61158en 50170Document58 pagesProfibus-According To Iec 61158en 50170mohammedrezaeeNo ratings yet
- Reality Construction of Disaster Discourses On Twitter: Analysis of Corpus-Assisted Discourse Study On Forest Fires in Indonesia From 2014-2019Document12 pagesReality Construction of Disaster Discourses On Twitter: Analysis of Corpus-Assisted Discourse Study On Forest Fires in Indonesia From 2014-2019Muhammad Rifqi Ma'arifNo ratings yet
- Environment Clearance Status Query Form: SearchDocument6 pagesEnvironment Clearance Status Query Form: SearchPankaj RajbharNo ratings yet
- Ulo BDocument2 pagesUlo BMarjorie Joy MartirNalupa AninoNo ratings yet