Professional Documents
Culture Documents
Fneur 14 1137453
Uploaded by
Eva ArdianahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fneur 14 1137453
Uploaded by
Eva ArdianahCopyright:
Available Formats
TYPE Original Research
PUBLISHED 17 February 2023
DOI 10.3389/fneur.2023.1137453
Subgrouping patients with
OPEN ACCESS zoster-associated pain according
to sensory symptom profiles: A
EDITED BY
Yan Lu,
Fourth Military Medical University, China
REVIEWED BY
Phillip R. Kramer,
cluster analysis
College of Dentistry, Texas A&M University,
United States
Ling Ye, Hee Jung Kim, Kyung Bong Yoon, Misun Kang, Yun Seok Yang
Sichuan University, China
Jian Cui, and Shin Hyung Kim*
Army Medical University, China
Yuto Uchida, Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei
Johns Hopkins Medicine, United States University College of Medicine, Seoul, Republic of Korea
*CORRESPONDENCE
Shin Hyung Kim
tessar@yuhs.ac Background and goal of study: Patients with zoster-associated pain exhibit a
SPECIALTY SECTION
variety of sensory symptoms and forms of pain and complain of different pain
This article was submitted to patterns. The purpose of this study is to subgroup patients with zoster-associated
Headache and Neurogenic Pain, pain who visited a hospital using painDETECT sensory symptom scores, analyze
a section of the journal
Frontiers in Neurology
their respective characteristics and pain-related data, and compare similarities and
differences among the groups.
RECEIVED 04 January 2023
ACCEPTED 06 February 2023 Materials and methods: The characteristics of 1,050 patients complaining of
PUBLISHED 17 February 2023 zoster-associated pain and pain-related data were reviewed retrospectively. To
CITATION identify subgroups of patients with zoster-associated pain according to sensory
Kim HJ, Yoon KB, Kang M, Yang YS and Kim SH
(2023) Subgrouping patients with
symptom profiles, a hierarchical cluster analysis was performed based on the
zoster-associated pain according to sensory responses to a painDETECT questionnaire. Demographics and pain-related data
symptom profiles: A cluster analysis. were compared among all subgroups.
Front. Neurol. 14:1137453.
doi: 10.3389/fneur.2023.1137453 Results and discussion: Patients with zoster-associated pain were classified into
COPYRIGHT
5 subgroups according to the distribution of sensory profiles, with each subgroup
© 2023 Kim, Yoon, Kang, Yang and Kim. This is exhibiting distinct differences in the expression of sensory symptoms. Patients
an open-access article distributed under the in cluster 1 complained of burning sensations, allodynia, and thermal sensitivity,
terms of the Creative Commons Attribution
License (CC BY). The use, distribution or but felt numbness less strongly. Cluster 2 and 3 patients complained of burning
reproduction in other forums is permitted, sensations and electric shock-like pain, respectively. Cluster 4 patients complained
provided the original author(s) and the of most sensory symptoms at similar intensities and reported relatively strong
copyright owner(s) are credited and that the
original publication in this journal is cited, in prickling pain. Cluster 5 patients suffered from both burning and shock-like pains.
accordance with accepted academic practice. Patient ages and the prevalence of cardiovascular disease were significantly lower
No use, distribution or reproduction is in cluster 1. Patients in clusters 1 and 4 reported longer pain duration compared
permitted which does not comply with these
terms. with those in clusters 2 and 3. However, no significant differences were found with
respect to sex, body mass index, diabetes mellitus, mental health problems, and
sleep disturbance. Pain scores, distribution of dermatomes and gabapentinoid use
were also similar among the groups.
Conclusions: Five different subgroups of patients with zoster-associated pain
were identified on the basis of sensory symptoms. A subgroup of younger patients
with longer pain duration showed specific and distinct symptoms, such as burning
sensations and allodynia. Unlike patients with acute or subacute pain, patients with
chronic pain were associated with diverse sensory symptom profiles.
KEYWORDS
zoster-associated pain, herpes zoster, cluster analysis, sensory symptoms, painDETECT
Frontiers in Neurology 01 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
Introduction
Cases of herpes zoster occur in at least 1 million people in
the United States every year, and the incidence rate has been
increasing worldwide over the past 20 years (1). Approximately
one-fifth of herpes zoster patients report some pain at 3
months after the onset of the disease, and the incidence rate of
postherpetic neuralgia (PHN) increases dramatically as patients age
(2, 3).
Patients with zoster-associated pain, including herpes zoster
infection and PHN, complain of diverse patterns of sensory
symptoms despite the common cause of the pain. Some patients
complain strongly of spontaneous pain, tingling sensations, and
electric-shock-like pain, while others suffer from hypersensitivity
to light touch or temperature. A simple and validated patient-
reported screening questionnaire, painDETECT, can detect these
characteristic sensory abnormalities (4, 5). Researchers have
attributed this difference in pain patterns to the relative
contributions of the peripheral and central mechanisms (6).
However, no specific biomarkers have been found with mechanisms
of zoster-associated pain. Therefore, subgrouping of patients
according to sensory phenotype can be clinically important in
patients with zoster-associated pain. Treatments that focus on
similar phenotypes would improve individualized pain therapy
and future clinical trial design (7, 8). Many investigators
have expressed similar thoughts on this subject, and multiple
studies have been conducted to identify the differences in the
dynamics of the somatosensory system for some peripheral
neuropathic pain conditions, including diabetic neuropathy
and PHN (9–13). However, few studies have focused on
zoster-associated pain from acute, subacute, and chronic pain
conditions. We assumed that patients with zoster-associated
pain who visit a hospital can be subgrouped into sensory
profiles according to the somatosensory mechanism like other
neuropathic pain.
The goal of this study is to classify patients with zoster-
associated pain into groups that clearly represent each
characteristic using a cluster analysis technique and to identify
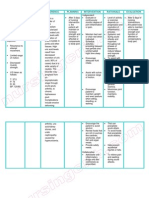
FIGURE 1
any similarities and differences in the characteristics of each
Flowchart for statistical methods.
cluster groups.
Materials and methods Sensory symptom profiling using the
painDETECT questionnaire
Study population
Sensory symptom profiles due to herpes zoster were described
This study was approved by the Institutional Review Board of using the painDETECT questionnaire during the patient’s first visit
Yonsei University Health System, Seoul, Republic of Korea to our clinic. Patients complaining of neuropathic pain caused by
(No. 4-2022-0819). As it is a retrospective observational herpes zoster freely described their symptoms and filled out the
study, the requirement for obtaining informed consent validated Korean version of the painDETECT questionnaire under
from the patients was waived. This manuscript complies the supervision of a researcher (14). The questionnaire consisted
with the STROBE checklists applicable to observational of 9 questions asking for sensory symptoms, pain course patterns,
studies. Adult patients who complained of zoster-associated and radiating pain. Seven of the questions asked respondents
pain at their first visit from January 2016 to August 2021 to use a 0-to-5 Likert scale to describe pain quality associated
were enrolled. Patients with incomplete medical records or with various sensory symptoms: burning sensations, tingling or
those who did not complete the painDETECT questionnaire prickling sensations, pain by light touch, electric shock-like pain,
were excluded. pain on cold/heat sensation, numbness, and pain by slight pressure
Frontiers in Neurology 02 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
FIGURE 2
Study flowchart.
TABLE 1 Patient characteristics and pain-related data of 1,050 patients
(0 = never; 1 = hardly noticed; 2 = slightly; 3 = moderately;
with zoster-associated pain.
4 = strongly; 5 = very strongly). To eliminate differences in
individual pain-perception thresholds, an alternative value was Variables Total (n = 1,050)
obtained by subtracting the average value of all scores for each of
Patient characteristics
the 7 questions. In this alternative score, values above 0 represent
stronger sensations than individual average pain perception, and Age, years 63.86 ± 13.87
values below 0 represent less-intense sensations compared with Female sex 616 (58.7)
individual average pain perception (10). 2
Body mass index, kg/m 23.55 ± 3.13
Cardiovascular disease 362 (34.5)
Patient demographics and pain-related Diabetes mellitus 207 (19.7)
data measures Mental health problems 166 (15.8)
Sleep disturbance 563 (53.6)
Patient characteristics and pain-related data were gathered
Pain-related data
from electronic medical records. Patient characteristics included
age, sex, body mass index (BMI), presence of diagnosed Pain score, numeric rating scale 0–10
comorbidities, and sleep disturbances. Diagnosed comorbidities Average 5.57 ± 2.44
included cardiovascular disease, diabetes mellitus, and mental
Maximum 6.29 ± 2.41
health problems that required continuous medical intervention
with regular hospital visits. Mental health problems were defined Pain duration
as those requiring psychiatric treatment or medication due to < 1 month 302 (28.8)
depression, anxiety, and stress over the past year. Average and
1–3 months 315 (30.0)
maximum pain scores using a numeric rating scale (NRS), duration
≥ 3 months 433 (41.2)
of pain, dermatomes, and the use of a gabapentinoid at the time of
visit were identified as pain-related factors. The duration of pain Dermatomes
was classified into < 1 month (acute), 1–3 months (subacute), and Trigeminal, facial 201 (19.1)
≥ 3 months (chronic).
Cervical 167 (15.9)
Thoracic 546 (52.0)
Statistical analysis Lumbosacrum 136 (13.0)
Gabapentinoid use 846 (80.6)
Descriptive statistical analysis
Values are presented as mean ± standard deviation (SD) or number of patients (%).
Continuous variables were shown as mean ± standard
deviation (SD), and categorical variables was tabulated using
numbers (percentage). The normality of distribution was evaluated
using a Shapiro–Wilk test. Differences among the cluster groups used to determine the intergroup difference between the mean of
were analyzed using one-way analysis of variance and chi-squared the groups when significant differences existed. Statistical Package
tests. A Tukey’s post hoc test or a chi-squared post hoc difference was for the Social Sciences, version 26.0 (IBM Corp, Armonk, NY,
Frontiers in Neurology 03 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
FIGURE 3
Distribution of sensory symptom profiles of derived five cluster groups.
USA) was used to analyze the data. A P < 0.05 was considered 384 met the exclusion criteria, leaving 1,050 patients in the
statistically significant. analysis (Figure 2).
Demographic profiles and pain-related data for these patients
are shown in Table 1. Women accounted for more than 50% of the
Cluster analysis patient group, the mean age was 63.86 years, and the average BMI
A hierarchical cluster analysis was performed for subgrouping value was 23.55 kg/m2 . Cardiovascular disease, diabetes mellitus,
according to relevant sensory symptoms of zoster-associated and mental health problems were reported for 362, 207, and
pain (Figure 1). A hierarchical WARD approach with a squared 166 patients, respectively, and more than 50% of the patients
Euclidean distance measure described previously (9, 10) was complained of sleep disturbances. The mean average pain score was
applied. Cluster analysis was conducted using the Python program,
5.57 and the maximum pain score was 6.29 on the NRS. A total
version 3.8.15 with Scikit-learn version 1.0.2. The cut-off point for
of 302 patients were assessed at < 1 month after zoster infection,
the essential clusters was set at ∼ 10% of the total cases. We chose
315 patients had passed 1–3 months, and 433 patients complained
to refer to a cut-off point of 5 clusters because solutions with fewer
of pain for more than 3 months. There were 201 patients with
clusters could eliminate significant differences by the agglomerative
zoster in the trigeminal and facial nerve areas, 167 with zoster in
clustering. A solution with five essential clusters was obtained by
hierarchical WARD clustering as an optimal agreement on our the cervical dermatomes, 546 in the thoracic dermatomes, and 136
decision criteria. To demonstrate the evidence for the solution and in the lumbosacral dermatomes. Approximately 80.6% of patients
were taking a gabapentinoid to relieve pain.
to rearrange the cases based on these results, a k-means cluster
analysis was performed. This analysis led to equal results, which A cluster analysis was performed using the Korean version
provides support for our chosen solution. of painDETECT to identify the subgroups of patients showing
typical sensory neuropathic symptoms as 5 distinct clusters
The cluster is represented by a pattern of questionnaire
scores, indicating the typical pathological structure of each (Figure 3). Patients in cluster 1 complained of all three symptoms:
group. All profiles were given individually adjusted scores (see burning sensations, allodynia, and thermal sensitivity, although
a lack of numbness was also reported. Patients in clusters 2
above). Heuristic interpretations of clusters were provided by
experts. Statistical analysis was not performed because this was a and 3 complained of severe burning sensation and electric-
heuristic approach. shock-like pain, respectively. Cluster 4 patients reported relatively
strong tingling pain with an intensity similar to that of most
sensory symptoms. Cluster 5 patients reported both burning and
Results shock-like pains.
A comparison was conducted to determine whether there was a
During the study period, 1,434 patients visited our difference in the characteristics and pain-related data of the patient
clinic for zoster-associated pain. Among these patients, groups between the 5 clusters (Table 2). Patient age (cluster 1 vs. 2,
Frontiers in Neurology 04 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
TABLE 2 Comparison of demographics, pain-related data, and affected dermatomes among the five cluster group.
Cluster label Cluster 1 Cluster 2 Cluster 3 Cluster 4 Cluster 5
(n = 171) (n = 228) (n = 296) (n = 203) (n = 152)
Patient characteristics
Age, years∗ 60.25 ± 14.222,3,4,5 65.37 ± 14.611 64.26 ± 13.12 1 64.25 ± 13.571 64.32 ± 13.661
Female sex 88 (51.5) 132 (57.9) 184 (62.2) 114 (56.2) 98 (64.5)
2
Body mass index, kg/m 23.81 ± 2.86 23.52 ± 3.07 23.68 ± 3.37 23.69 ± 3.02 23.03 ± 3.01
2,3,4,5 1 1 1
Cardiovascular disease∗∗ 35 (20.5) 89 (39.0) 110 (37.2) 68 (33.5) 60 (39.5)1
Diabetes mellitus 29 (17.0) 53 (23.2) 56 (18.9) 38 (18.7) 31 (20.4)
Mental health problems 20 (11.7) 40 (17.5) 56 (18.9) 22 (10.8) 28 (18.4)
Sleep disturbance 95 (55.6) 116 (50.9) 157 (53.0) 107 (52.7) 88 (57.9)
Pain-related data
Pain score, numeric rating scale, 0–10
Average 5.23 ± 2.54 5.46 ± 2.43 5.82 ± 2.39 5.51 ± 2.40 5.73 ± 2.42
Maximum 6.05 ± 2.55 6.35 ± 2.45 6.41 ± 2.32 6.06 ± 2.41 6.57 ± 2.35
Pain durations
< 1 month 49 (28.7) 70 (30.7) 99 (33.4) 45 (22.2) 39 (25.7)
1-3 months 41 (24.0) 78 (34.2) 85 (28.7) 61 (30.0) 50 (32.9)
2,3 1,4 1,4 2,3
≥ 3 months∗∗ 81 (47.4) 80 (35.1) 112 (37.8) 97 (47.8) 63 (41.4)
Dermatomes
Trigeminal, facial 39 (22.8) 47 (20.6) 55 (18.6) 33 (16.3) 27 (17.8)
Cervical 29 (17.0) 40 (17.5) 35 (11.8) 38 (18.7) 25 (16.4)
Thoracic 83 (48.5) 115 (50.4) 162 (54.7) 108 (53.2) 78 (51.3)
Lumbosacrum 20 (11.7) 26 (11.4) 44 (14.9) 24 (11.8) 22 (14.5)
Gabapentinoid use 141 (82.5) 183 (80.3) 227 (76.7) 164 (80.8) 131 (86.2)
Values are presented as mean ± standard deviation (SD) or number of patients (%). ∗ Tukey’s multiple comparison test (p < 0.05); ∗∗ Chi-square post hoc difference (p < 0.05). 1, vs. cluster 1; 2,
vs. cluster 2; 3, vs. cluster 3; 4, vs. cluster 4; 5, vs. cluster 5.
p = 0.001; cluster 1 vs. 3, p = 0.002; cluster 1 vs. 4, p = 0.006; cluster challenging and insufficiently effective. This study was designed to
1 vs. 5, p = 0.009) and the prevalence of cardiovascular disease classify patients with zoster-associated pain based on abnormalities
(cluster 1 vs. 2, p < 0.001; cluster 1 vs. 3, p < 0.001; cluster 1 vs. in sensory symptoms because it would be ideal and effective to
4, p = 0.005; cluster 1 vs. 5, p < 0.001) were significantly lower stratify patients according to the pain mechanism (15).
in cluster 1 than those in the other clusters. In addition, clusters Distinct sensory abnormalities associated with pain perceived
1 and 4 had a relatively high proportion of patients complaining by patients can be self-assessed, and they are largely divided into
of pain for more than 3 months (chronic) compared to clusters spontaneous sensory sensation (burning, tingling, and electric-
2 and 3 (cluster 1 vs. 2, p = 0.013; cluster 1 vs. 3, p = 0.044; shock-like pain), stimulus-evoked positive sensory symptoms (pain
cluster 4 vs. 2, p = 0.007; cluster 4 vs. 3, p = 0.027). However, there evoked by light touch, thermally evoked pain, and pressure-evoked
were no significant differences in sex, BMI, medical comorbidities pain), and stimulus-evoked negative sensory symptom (numbness)
including diabetes mellitus and mental health problems, and sleep (7, 16). The variations in the mechanisms of symptom generation
disturbance between clusters. Also, the average and maximum pain are explained by plastic changes in the central nervous system and
scores on the NRS, the dermatomes to which the lesion belongs, remaining peripheral nociceptors (6, 17).
and the use of gabapentinoids were similar between cluster groups. An analysis of patients with zoster-associated pain on the
basis of sensory phenotype found that patients in cluster 1
suffered primarily from thermally evoked pain and mechanical
Discussion allodynia, but not numbness. Allodynia is due to central spinal
cord sensitization and is induced by activation of touch-
Patients with zoster-associated pain account for a large sensitive cutaneous Aβ-fibers that terminate in synapses of
proportion of those with neuropathic-like pain symptoms. Despite nociceptive second-order neurons in the central nervous system
an increased understanding of the pathophysiological mechanism (18). Thermally evoked pain is due to peripheral sensitization
of neuropathic pain, treatment of zoster-associated pain remains of nociceptive afferents; it is characteristic of hyperactive and
Frontiers in Neurology 05 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
sensitized cutaneous nociceptors (19). However, numbness is a interpretation of evoked pain and negative symptoms. Also, pain
sensory symptom that involves a loss of afferent function (11). perceptions are subjective and could be confounded by personal
Cluster 1 patients therefore have irritable nociceptors and their skin factors (7). To minimize these shortcomings, the scores of the
innervation is intact (20). In studies of patients with peripheral questionnaire were adjusted by individual means. A longitudinal
neuropathic pain, it was possible to predict that thermally study would be necessary to proceed with clustering in an objective
evoked pain and allodynia would have an analgesic effect by psychophysical approach (e.g., Quantitative sensory testing (QST)
applying 8% topical capsaicin patches (21) and intracutaneous or morphological data from skin biopsies). In addition, we
botulinum toxin (22). Patients in cluster 2, 3, and 5 suffered used an actual clinical practice model in which the majority of
spontaneous pain without cutaneous hypersensitivity and marked attending patients had undergone some interventional treatments
sensory deafferentation, caused by ectopic neuronal firing within or had been prescribed medications, including gabapentinoids.
the nociceptive pathways and secondary sensitization of central This class of medications modulates pain processing and central
nociceptive neurons (11). Abnormal expression of voltage-gated sensitization. However, because there was no difference in the ratio
sodium channels is associated with ectopic nerve activity (23). An of gabapentinoid use for each subgroup, this factor would not have
animal study has shown increases and changes in voltage-gated ion had a significant impact on the interpretation of the results.
channels at impaired peripheral nerves in rats with varicellar zoster
virus. These sensitized pain behaviors were reversed by sodium
channel blockers (24). Peripheral analgesic lidocaine patches
selectively block sodium channels of small damaged peripheral Conclusion
nerve fibers without severe systemic adverse effects. Therefore, in
this case, applying topical lidocaine is appropriate for the control In conclusion, despite the common cause of the pain, some
of localized peripheral neuropathic pain (25). Patients in cluster differences in the distribution of sensory profiles were evident
4 tended to experience relatively strong tingling sensations, but among patients with zoster-associated pain. In particular, a
were also characterized by relatively mild abnormalities due to subgroup with younger patients who experienced longer durations
the overlap of pathophysiological mechanisms. There are two of pain reported specific and distinct positive symptoms, such
possible causes of these symptom constellations. First, these as burning sensations and allodynia. Unlike patients with acute
patients perceived all neuropathic pain at similar frequencies and or subacute pain, patients with chronic pain were associated
intensities. The second possibility is that these patients are people with diverse sensory symptom profiles. These results indicate that
who tend to answer in a similar manner. These patients responded patients can be subgrouped according to patient-reported sensory
similarly to all questions because they could not discriminate symptoms of zoster-associated pain, although the central and
between the abnormalities in sensory symptoms. Such patients peripheral mechanisms of pain vary among subjects. This approach
should be excluded from the clinical trial of a medication that may help determine the most appropriate pain treatment for each
targets specific pathophysiologies. individual of this population.
In the present study, the patients belonging to cluster 1
were younger than those of the other clusters. Although results
conflicted depending on the animal model and experimental Data availability statement
stimuli, preclinical data suggest that advanced age may be related to
increased pain sensitivity (26). However, the relationship between The raw data supporting the conclusions of this article will be
age and pain sensitivity is unclear in zoster-related pain. Moreover, made available by the authors, without undue reservation.
patients in cluster 1 reported experiencing pain for a longer
time, although they were younger. Age may therefore not be an
independent factor associated with specific sensory symptoms. In
the current study, some differences in sensory symptoms according Ethics statement
to duration of zoster-associated pain were also observed. In chronic
pain conditions, the alteration of central processing of pain is a The studies involving human participants were reviewed and
major contributing factor in pain symptoms (6). While previous approved by the Institutional Review Board of Yonsei University
studies (11, 12) were conducted primarily on PHN patients, our Health System, Seoul, Republic of Korea. Written informed consent
study included all periods of pain, with more than half of patients for participation was not required for this study in accordance with
reporting acute and subacute periods. Tissue inflammation and the national legislation and the institutional requirements.
destruction, activation of nociceptive neurons, abnormal impulses,
and neural injury during the early infection period cause a
strong nociceptive barrage, creating acute pain and allodynia (27).
Considering the complexity of zoster-associated pain, this study Author contributions
confirms different therapeutic approaches are needed to manage
pain according to their pain duration in this population. Conceptualization, writing—review and editing, and
This study has several limitations. As a retrospective study supervision: SHK and KBY. Software and validation: HJK
conducted in a single center, selective bias or information bias and MK. Formal analysis and data curation: HJK and YSY.
is possible. PainDETECT is a reliable questionnaire to assess Writing—original draft preparation: HJK and SHK. Project
differences in sensory perception intensity, but there is a paucity of administration and methodology: HJK. Funding acquisition:
Frontiers in Neurology 06 frontiersin.org
Kim et al. 10.3389/fneur.2023.1137453
SHK. All authors contributed to the article and approved the Conflict of interest
submitted version.
The authors declare that the research was conducted in the
absence of any commercial or financial relationships that could be
Funding construed as a potential conflict of interest.
This study was supported by the Faculty
Research grant of Yonsei University College of Publisher’s note
Medicine (No. 6-2022-0048).
All claims expressed in this article are solely those of the
authors and do not necessarily represent those of their affiliated
Acknowledgments organizations, or those of the publisher, the editors and the
reviewers. Any product that may be evaluated in this article, or
The authors thank C. H. Hwang for helping analyze the data in claim that may be made by its manufacturer, is not guaranteed or
this study. endorsed by the publisher.
References
1. Rosamilia LL. Herpes zoster presentation, management, and 14. Sung JK, Choi JH, Jeong J, Kim WJ, Lee DJ, Lee SC, et al. Korean version of the
prevention: a modern case-based review. Am J Clin Dermatol. (2020) pain detect questionnaire: a study for cultural adaptation and validation. Pain Pract.
21:97–107. doi: 10.1007/s40257-019-00483-1 (2017) 17:494–504. doi: 10.1111/papr.12472
2. Johnson RW, Rice AS. Clinical practice. Postherpetic neuralgia N Engl J Med. 15. Forstenpointner J, Otto J, Baron R. Individualized neuropathic
(2014) 371:1526–33. doi: 10.1056/NEJMcp1403062 pain therapy based on phenotyping: are we there yet? Pain. (2018)
159:569–75. doi: 10.1097/j.pain.0000000000001088
3. Meera S, Aijun C. Modalities in managing postherpetic neuralgia. Korean J Pain.
(2018) 31:235–43. doi: 10.3344/kjp.2018.31.4.235 16. Cappelleri JC, Koduru V, Bienen EJ, Sadosky A. Characterizing neuropathic pain
profiles: enriching interpretation of pain detect. Patient Relat Outcome Meas. (2016)
4. Freynhagen R, Baron R, Gockel U, Tölle TR. Pain detect: a new screening
7:93–9. doi: 10.2147/PROM.S101892
questionnaire to identify neuropathic components in patients with back pain. Curr Med
Res Opin. (2006) 22:1911–20. doi: 10.1185/030079906X132488 17. Bannister K, Sachau J, Baron R, Dickenson AH. Neuropathic pain:
mechanism-based therapeutics. Annu Rev Pharmacol Toxicol. (2020)
5. Vollert J, Kramer M, Barroso A, Freynhagen R, Haanpää M, Hansson P,
60:257–74. doi: 10.1146/annurev-pharmtox-010818-021524
et al. Symptom profiles in the pain detect questionnaire in patients with peripheral
neuropathic pain stratified according to sensory loss in quantitative sensory testing. 18. Jensen TS, Finnerup NB. Allodynia and hyperalgesia in neuropathic
Pain. (2016) 157:1810–8. doi: 10.1097/j.pain.0000000000000588 pain: clinical manifestations and mechanisms. Lancet Neurol. (2014)
13:924–35. doi: 10.1016/S1474-4422(14)70102-4
6. Pappagallo M, Oaklander AL, Quatrano-Piacentini AL, Clark MR, Raja
SN. Heterogenous patterns of sensory dysfunction in postherpetic neuralgia 19. McKemy DD, Neuhausser WM, Julius D. Identification of a cold receptor
suggest multiple pathophysiologic mechanisms. Anesthesiology. (2000) 92:691– reveals a general role for TRP channels in thermosensation. Nature. (2002) 416:52–
8. doi: 10.1097/00000542-200003000-00013 8. doi: 10.1038/nature719
7. Baron R, Förster M, Binder A. Subgrouping of patients with neuropathic pain 20. Mahn F, Hüllemann P, Gockel U, Brosz M, Freynhagen R, Tölle TR, et al. Sensory
according to pain-related sensory abnormalities: a first step to a stratified treatment symptom profiles and co-morbidities in painful radiculopathy. PLoS ONE. (2011)
approach. Lancet Neurol. (2012) 11:999–1005. doi: 10.1016/S1474-4422(12)70189-8 6:e18018. doi: 10.1371/journal.pone.0018018
8. Reimer M, Helfert SM, Baron R. Phenotyping neuropathic pain patients: 21. Mainka T, Malewicz NM, Baron R, Enax-Krumova EK, Treede RD, Maier
implications for individual therapy and clinical trials. Curr Opin Support Palliat Care. C. Presence of hyperalgesia predicts analgesic efficacy of topically applied capsaicin
(2014) 8:124–9. doi: 10.1097/SPC.0000000000000045 8% in patients with peripheral neuropathic pain. Eur J Pain. (2016) 20:116–
29. doi: 10.1002/ejp.703
9. Koroschetz J, Rehm SE, Gockel U, Brosz M, Freynhagen R, Tölle TR, et al.
Fibromyalgia and neuropathic pain–differences and similarities. A comparison of 22. Attal N, de Andrade DC, Adam F, Ranoux D, Teixeira MJ, Galhardoni R,
3057 patients with diabetic painful neuropathy and fibromyalgia. BMC Neurol. (2011) et al. Safety and efficacy of repeated injections of botulinum toxin A in peripheral
11:55. doi: 10.1186/1471-2377-11-55 neuropathic pain (BOTNEP): a randomised, double-blind, placebo-controlled trial.
Lancet Neurol. (2016) 15:555–65. doi: 10.1016/S1474-4422(16)00017-X
10. Baron R, Tölle TR, Gockel U, Brosz M, Freynhagen R, A. cross-sectional
cohort survey in 2100 patients with painful diabetic neuropathy and postherpetic 23. Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis,
neuralgia: differences in demographic data and sensory symptoms. Pain. (2009) pathophysiological mechanisms, and treatment. Lancet Neurol. (2010)
146:34–40. doi: 10.1016/j.pain.2009.06.001 9:807–19. doi: 10.1016/S1474-4422(10)70143-5
11. Rehm S, Grobkopf M, Kabelitz M, Keller T, Freynhagen R, Tölle TR, 24. Garry EM, Delaney A, Anderson HA, Sirinathsinghji EC, Clapp RH, Martin
et al. Sensory symptom profiles differ between trigeminal and thoracolumbar WJ, et al. Varicella zoster virus induces neuropathic changes in rat dorsal root ganglia
postherpetic neuralgia. Pain Rep. (2018) 3:e636. doi: 10.1097/PR9.00000000000 and behavioral reflex sensitisation that is attenuated by gabapentin or sodium channel
00636 blocking drugs. Pain. (2005) 118:97–111. doi: 10.1016/j.pain.2005.08.003
12. Gierthmühlen J, Braig O, Rehm S, Hellriegel J, Binder A, 25. Wolff RF, Bala MM, Westwood M, Kessels AG, Kleijnen J. 5% lidocaine-
Baron R. Dynamic of the somatosensory system in postherpetic medicated plaster vs. other relevant interventions and placebo for post-herpetic
neuralgia. Pain Rep. (2018) 3:e668. doi: 10.1097/PR9.00000000000 neuralgia (PHN): a systematic review. Acta Neurol Scand. (2011) 123:295–
00668 309. doi: 10.1111/j.1600-0404.2010.01433.x
13. Choi K, Kwon O, Suh BC, Sohn E, Joo IS, Oh J. Subgrouping 26. Yezierski RP. The effects of age on pain sensitivity: preclinical studies. Pain Med.
of peripheral neuropathic pain patients according to sensory (2012) 13:S27–36. doi: 10.1111/j.1526-4637.2011.01311.x
symptom profile using the Korean version of the pain detect
questionnaire. J Korean Med Sci. (2022) 37:e8. doi: 10.3346/jkms.202 27. Rowbotham MC, Petersen KL. Zoster-associated pain and neural dysfunction.
2.37.e8 Pain. (2001) 93:1–5. doi: 10.1016/S0304-3959(01)00328-1
Frontiers in Neurology 07 frontiersin.org
You might also like
- Sleep OpiodsDocument8 pagesSleep OpiodsboboNo ratings yet
- Pediatrics - Neonatal ICUDocument2 pagesPediatrics - Neonatal ICUJasmine KangNo ratings yet
- Nursing Care Plan Gouty ArthritisDocument2 pagesNursing Care Plan Gouty Arthritisderic94% (17)
- Effect of Hypnotic Suggestion On Fibromy PDFDocument6 pagesEffect of Hypnotic Suggestion On Fibromy PDFCarlos CondeNo ratings yet
- FNCPDocument4 pagesFNCPJonalyn Tumanguil100% (2)
- HCC Coding Feb 2022 ICD-10 InformantDocument2 pagesHCC Coding Feb 2022 ICD-10 InformantSonali PawarNo ratings yet
- HSU Pre-Enrollment Medical Record Form (FRESHMAN)Document4 pagesHSU Pre-Enrollment Medical Record Form (FRESHMAN)ChristnerNo ratings yet
- Source of Infections 1. Endogenous SourceDocument6 pagesSource of Infections 1. Endogenous SourceDeepu VijayaBhanuNo ratings yet
- Hiv Case StudyDocument2 pagesHiv Case Studyapi-485814878No ratings yet
- Referred Muscle Pain Basic and Clinical FindingsDocument9 pagesReferred Muscle Pain Basic and Clinical FindingsaavalverdeNo ratings yet
- Fibromyalgia and Neuropathic Pain - Differences and Similarities. A Comparison of 3057 Patients With Diabetic Painful Neuropathy and FibromyalgiaDocument9 pagesFibromyalgia and Neuropathic Pain - Differences and Similarities. A Comparison of 3057 Patients With Diabetic Painful Neuropathy and FibromyalgiaErica Jade WilmesNo ratings yet
- NIH Public Access: Author ManuscriptDocument25 pagesNIH Public Access: Author ManuscriptsoylahijadeunvampiroNo ratings yet
- Dolor Radicular y Pseudo Dolor Radicular Freynhagen 2008Document10 pagesDolor Radicular y Pseudo Dolor Radicular Freynhagen 2008Victor Andrés Olivares IbarraNo ratings yet
- Asesemen PsikoDocument5 pagesAsesemen PsikofajarNo ratings yet
- Articulo Ingles QuemadurasDocument17 pagesArticulo Ingles QuemadurasAndrea RiveraNo ratings yet
- Barriers To Reconceptulization of Chronic Pain Moseley PDFDocument6 pagesBarriers To Reconceptulization of Chronic Pain Moseley PDFpfi_jenNo ratings yet
- Episodic (Breakthrough) PainDocument8 pagesEpisodic (Breakthrough) PainDiklat Medis Eka HospitalNo ratings yet
- European Journal of Pain - 2017 - Arendt Nielsen - Assessment and Manifestation of Central Sensitisation Across DifferentDocument26 pagesEuropean Journal of Pain - 2017 - Arendt Nielsen - Assessment and Manifestation of Central Sensitisation Across DifferentLucas Mamud MeroniNo ratings yet
- Distrofia SimpaticaDocument11 pagesDistrofia SimpaticaDiego Agustin ZarzaNo ratings yet
- Introduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainDocument2 pagesIntroduction: Recommendations For The Diagnosis, Assessment, and Treatment of Neuropathic PainFran WermannNo ratings yet
- Occurrence and Clinical Evolution of Neuropathic Dysesthetic Pain in Multiple Sclerosis (2-Year Prospective Study)Document5 pagesOccurrence and Clinical Evolution of Neuropathic Dysesthetic Pain in Multiple Sclerosis (2-Year Prospective Study)Nana ShkodinaNo ratings yet
- Fneur 14 1104817Document6 pagesFneur 14 1104817geowalker7092No ratings yet
- Chronic Pain 1: SeriesDocument16 pagesChronic Pain 1: Seriesginamilena90No ratings yet
- Behrman 2007Document7 pagesBehrman 2007neurologi standart4No ratings yet
- Oup Accepted Manuscript 2017Document27 pagesOup Accepted Manuscript 2017Zilga ReginaNo ratings yet
- Pain and Gender Differences A Clinical ApproachDocument6 pagesPain and Gender Differences A Clinical ApproachMarianaNo ratings yet
- Kinesiophobia and Maladaptive Coping Strategies Prevent Improvements in Pain Catastrophizing Following Pain Neuroscience Education in FibromyalgiaDocument9 pagesKinesiophobia and Maladaptive Coping Strategies Prevent Improvements in Pain Catastrophizing Following Pain Neuroscience Education in FibromyalgiaCelia CaballeroNo ratings yet
- Axial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Document8 pagesAxial Low Back Pain One Painful Area - Many Perceptions and Mechanisms - Förster Et Al '13Craig ChambersNo ratings yet
- International Spinal Cord Injury Pain Classification: Part I. Background and DescriptionDocument5 pagesInternational Spinal Cord Injury Pain Classification: Part I. Background and DescriptionAyat BissNo ratings yet
- Wilson DJ Williams M Butler D 2009Document11 pagesWilson DJ Williams M Butler D 2009vicente gaticaNo ratings yet
- Neuropathic Pain: Definition, Assessment and Epidemiology: SciencedirectDocument10 pagesNeuropathic Pain: Definition, Assessment and Epidemiology: SciencedirectLidwina ApyakaNo ratings yet
- Bmjsem 2022 001387Document4 pagesBmjsem 2022 001387PsychoPompNo ratings yet
- Neuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeDocument8 pagesNeuropathic Pain: Redefinition and A Grading System For Clinical and Research Purposes - TreedeNahu SteinmannNo ratings yet
- Orofacial PainDocument7 pagesOrofacial PainAkram AlsharaeeNo ratings yet
- Wound ExudateDocument15 pagesWound ExudateShannastaniar AisyaNo ratings yet
- Sal Affi 2004Document9 pagesSal Affi 2004EriC. ChaN.No ratings yet
- 2013 Jankowski PainDocument6 pages2013 Jankowski PainOlga VolyanskaNo ratings yet
- Pain Practice - 2023 - YoonDocument14 pagesPain Practice - 2023 - YoonAbbey WaltzNo ratings yet
- Actcr 1 (3) 14Document8 pagesActcr 1 (3) 14Robinson Trujillo CabanillaNo ratings yet
- Jurnal Neuropaty DM 1Document14 pagesJurnal Neuropaty DM 1peniNo ratings yet
- Research in Nursing Health - 2014 - Henoch - Symptom Distress Profiles in Hospitalized Patients in Sweden ADocument12 pagesResearch in Nursing Health - 2014 - Henoch - Symptom Distress Profiles in Hospitalized Patients in Sweden AflorenceNo ratings yet
- The Pain Anxiety Symptoms Scale - Development and Validation of A Scale To Measure Fear of PainDocument7 pagesThe Pain Anxiety Symptoms Scale - Development and Validation of A Scale To Measure Fear of Painapi-291366747No ratings yet
- J Pain 2003 12 024Document10 pagesJ Pain 2003 12 024fmvxlxdziltmjfurtuNo ratings yet
- Pseudoradicular and Radicular Low-Back Pain: How To Diagnose Clinically?Document3 pagesPseudoradicular and Radicular Low-Back Pain: How To Diagnose Clinically?adeNo ratings yet
- Human Brain Mechanisms of Pain PerceptionDocument22 pagesHuman Brain Mechanisms of Pain Perceptionnynaeve_almeeraNo ratings yet
- Original Reports: Characterization of Hyperacute Neuropathic Pain After Spinal Cord Injury: A Prospective StudyDocument9 pagesOriginal Reports: Characterization of Hyperacute Neuropathic Pain After Spinal Cord Injury: A Prospective Studyezequiel zaragoza juarezNo ratings yet
- ArchRheumatol 33 418Document6 pagesArchRheumatol 33 418qwerty hrNo ratings yet
- Relationship Between Sleep, Pain and Inflammatory Markers in Patients With Rheumatoid ArthritisDocument7 pagesRelationship Between Sleep, Pain and Inflammatory Markers in Patients With Rheumatoid Arthritisaria tristayanthiNo ratings yet
- Mahnig 2016Document7 pagesMahnig 2016Ayat BissNo ratings yet
- Vital Signs: Valid Indicators To Assess Pain in Intensive Care Unit Patients? An Observational, Descriptive StudyDocument7 pagesVital Signs: Valid Indicators To Assess Pain in Intensive Care Unit Patients? An Observational, Descriptive Studybardah wasalamahNo ratings yet
- Central Sensitization in Opioid Use Disorder A.5Document10 pagesCentral Sensitization in Opioid Use Disorder A.5Gretchen Cuda KroenNo ratings yet
- Use of S-LANSS, A Tool For Screening Neuropathic Pain, ForDocument8 pagesUse of S-LANSS, A Tool For Screening Neuropathic Pain, ForTri UtomoNo ratings yet
- Assessment and Manifestation of Central Sensitisation Across Different Chronic Pain ConditionsDocument26 pagesAssessment and Manifestation of Central Sensitisation Across Different Chronic Pain Conditions杨钦杰No ratings yet
- Chapman 1999Document32 pagesChapman 1999Rully KasimNo ratings yet
- Analytical Study To Understand The Role of Homoeopathic Medicines in Patients Suffering From The Complaint of Back PainDocument3 pagesAnalytical Study To Understand The Role of Homoeopathic Medicines in Patients Suffering From The Complaint of Back PainEditor IJTSRDNo ratings yet
- J Pain 2004 12 010Document8 pagesJ Pain 2004 12 010Ines Ruiz MaquedaNo ratings yet
- Applying Modern Pain Neuroscience in Clinical - 2014Document12 pagesApplying Modern Pain Neuroscience in Clinical - 2014Juci FreitasNo ratings yet
- Overactivity in Chronic Pain, The Role of Pain-Related Endurance and Neuromuscular ActivityDocument10 pagesOveractivity in Chronic Pain, The Role of Pain-Related Endurance and Neuromuscular ActivityVizaNo ratings yet
- Castel ADocument12 pagesCastel Ahelenlamlam200011No ratings yet
- EFNS Guideline 2004 Neuropathic Pain AssessmentDocument10 pagesEFNS Guideline 2004 Neuropathic Pain AssessmentDeni Andre AtmadinataNo ratings yet
- Dok Baru 2019-03-19 20.02.14Document9 pagesDok Baru 2019-03-19 20.02.14noflin oxyaniNo ratings yet
- Central Sensitization in Patients With Rheumatoid Arthritis: A Systematic Literature ReviewDocument12 pagesCentral Sensitization in Patients With Rheumatoid Arthritis: A Systematic Literature ReviewJuliana FeronNo ratings yet
- Novel Approach Towards Musculoskeletal PhenotypesDocument12 pagesNovel Approach Towards Musculoskeletal Phenotypescelia Diz CastilloNo ratings yet
- 201705gillespie 1Document9 pages201705gillespie 1Jose PerezNo ratings yet
- Threat of Pain Influences Social Context Effects On Verbal Pain ReportDocument9 pagesThreat of Pain Influences Social Context Effects On Verbal Pain ReportEmilie BergeronNo ratings yet
- Artigos Coderre1997Document65 pagesArtigos Coderre1997JonasMarçaloNo ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- Abm 14142Document8 pagesAbm 14142Eva ArdianahNo ratings yet
- 464 2020 Article 7766Document7 pages464 2020 Article 7766Eva ArdianahNo ratings yet
- Pui 2006Document13 pagesPui 2006Eva ArdianahNo ratings yet
- Sardjono 2021 IOP Conf. Ser. Earth Environ. Sci. 794 012046Document12 pagesSardjono 2021 IOP Conf. Ser. Earth Environ. Sci. 794 012046Eva ArdianahNo ratings yet
- Childhood AsthmaDocument9 pagesChildhood AsthmaJaved IqbalNo ratings yet
- Interstitial Pulmonary PatternsDocument12 pagesInterstitial Pulmonary PatternsjohnNo ratings yet
- Kode Icd X Permenkes No 5 Tahun 2014Document6 pagesKode Icd X Permenkes No 5 Tahun 2014may rosa bintangNo ratings yet
- Vidas Sars-Cov-2: Two Immunoassay Tests To Detect Igm & Igg AntibodiesDocument2 pagesVidas Sars-Cov-2: Two Immunoassay Tests To Detect Igm & Igg AntibodiesRed OneNo ratings yet
- Secondary Prevention Stroke AHA ChecklistDocument1 pageSecondary Prevention Stroke AHA ChecklistGyörgy HalászNo ratings yet
- Asthma: Differential Diagnosis and ComorbiditiesDocument9 pagesAsthma: Differential Diagnosis and ComorbiditiesQuel PaivaNo ratings yet
- Original Research Article: Vitan Patel, Minal Shastri, Nisha Gaur, Prutha Jinwala, Abhishek Y. KadamDocument5 pagesOriginal Research Article: Vitan Patel, Minal Shastri, Nisha Gaur, Prutha Jinwala, Abhishek Y. KadamTam LyNo ratings yet
- More Information: Help Stop The Spread of Covid-19Document2 pagesMore Information: Help Stop The Spread of Covid-19timgourNo ratings yet
- Valerie Curtis, Why Disgust MattersDocument13 pagesValerie Curtis, Why Disgust Mattersmaria berbaraNo ratings yet
- COPD NEW GuidelinesDocument45 pagesCOPD NEW GuidelinesMuhammad HaneefNo ratings yet
- MumpsDocument1 pageMumpsFikri PutroNo ratings yet
- Hair NailsDocument4 pagesHair Nailsapi-26570979No ratings yet
- Lung Dictionary Nov18 d070819Document60 pagesLung Dictionary Nov18 d070819KEZZIA MAE ABELLANo ratings yet
- 4.daftar Pustaka Artikel BagusDocument5 pages4.daftar Pustaka Artikel BagusJono ParmiNo ratings yet
- Elements of Informed Consent For Blood and Blood ProductsDocument2 pagesElements of Informed Consent For Blood and Blood ProductsKarl RobleNo ratings yet
- Nursing Care Plan Hypertension - Hypertension - Blood PressureDocument1 pageNursing Care Plan Hypertension - Hypertension - Blood PressureElay PedrosoNo ratings yet
- Teste de Rastreamento de Alterações de Fala para CriançasDocument6 pagesTeste de Rastreamento de Alterações de Fala para CriançassandrmrNo ratings yet
- Lec 5 New Castle DiseaseDocument38 pagesLec 5 New Castle Diseasebasit abdulNo ratings yet
- Jurnal Hubungan-Perawatan-Tali-Pusat-Dengan-Kej-3e562ac0Document10 pagesJurnal Hubungan-Perawatan-Tali-Pusat-Dengan-Kej-3e562ac0Edwar RusdiantoNo ratings yet
- Microbiology Syllabus For 3 Year: General BacteriologyDocument3 pagesMicrobiology Syllabus For 3 Year: General Bacteriologyسارة عبد الكاظم مكطوفNo ratings yet
- Fortum Injection: Consumer Medicine InformationDocument4 pagesFortum Injection: Consumer Medicine Informationthariq mubarakNo ratings yet
- Overview of New Death Certificate PDFDocument59 pagesOverview of New Death Certificate PDFFaisol KabirNo ratings yet
- ICD-10 Codes - 2-20-2021Document4 pagesICD-10 Codes - 2-20-2021Viva medical centerNo ratings yet