Professional Documents
Culture Documents
Comprehensive Visual Inspection of The Cervix With Acetic Acid (VIA) and Lugol's Iodine (VILI)
Comprehensive Visual Inspection of The Cervix With Acetic Acid (VIA) and Lugol's Iodine (VILI)
Uploaded by
Mulugeta DagneOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comprehensive Visual Inspection of The Cervix With Acetic Acid (VIA) and Lugol's Iodine (VILI)
Comprehensive Visual Inspection of The Cervix With Acetic Acid (VIA) and Lugol's Iodine (VILI)
Uploaded by
Mulugeta DagneCopyright:
Available Formats
8/28/22, 7:26 PM Comprehensive Visual Inspection of the Cervix with Acetic Acid (VIA) and Lugol’s Iodine (VILI)
Cervical cancer in developing countries
Home About us Cervical cancer Education Countries Documents Links Files
Comprehensive Visual Inspection of the Cervix with Acetic Acid (VIA) and Lugol’s Iodine (VILI)
About the development of this course
This course has been developed in order to improve the screening skills of healthcare professionals working in the field of cervical cancer screening in low and medium resource incomes countries (LMIC).
What are the minimal requirements before doing this course?
The minimal requirements for reaching the objectives of this course are basic knowledge of the lower genital tract anatomy as well as of the benign cervical abnormalities (such as: polyps, hyperkeratosis, Na
cysts and cervicitis).
What are the visual inspections in the prevention of cervical cancer?
The visual inspection techniques include VIA (visual inspection with acetic acid) and VILI (visual inspection using Lugol’s iodine). These approaches are an attractive alternative to cytology-based screening i
What is VIA?
VIA is a visual examination of the uterine cervix after application of 3-5% acetic acid. If the cervical epithelium contains an abnormal load of cellular proteins, the acetic acid coagulates the proteins conferring
and white aspect of the concerned area. A precancerous lesion has higher protein content when compared to normal epithelium. As a consequence it becomes white (acetowhite) and is considered to be “VI
For practical consideration please note that the expected rate of cervical intraepithelial neoplasia grade 2 or worse (CIN2+) in an unscreened or poorly screened population is between 2-4%.
What is VILI?
VILI is a visual examination generally performed after the VIA test and requires the application of Lugol’s iodine, a compound that reacts with glycogen resulting in a brown or black coloration. Normal mature
epithelium contains glycogen. When in contact with Lugol’s iodine it becomes black, whereas precancerous lesions and cancer contain little or no glycogen thus turning yellow after Lugol application. Such a
considered to be “VILI positive”.
What is an HPV test?
HPV tests identify the presence of Human Papillomavirus (HPV) that is at the origin of cervical cancer. Women having an HPV-negative test are not at risk for developing cervical cancer in the next 5-10 year
20% and 30% of women (30-50 years old) in sub-Saharan Africa are HPV-positive but only a subgroup of them will have a CIN2+ lesion. The considerable advantage of HPV testing is that the women can pe
themselves (self-HPV).
What is the advantage of VIA/VILI testing in HPV-positive women?
Performing VIA/VILI in HPV-positive women is a screening option recommended by the World Health Organization (WHO). This allows selective VIA testing in high-risk populations. It is worth knowing that th
rate of CIN2+ in HPV-positive women (30-50 years old) is approximately 8-15%.
Who should be tested for HPV followed by a VIA/VILI test?
Women between the ages of 30 and 50 are eligible for cervical cancer screening using this method.
Who can perform VIA/VILI test?
Any healthcare providers can perform this examination. However, in order to perform VIA/VILI successfully and be efficient in reducing cervical cancer incidence, healthcare providers need to receive formal a
VIA/VILI training. Providing high-quality VIA/VILI screening is essential and requires continual training and close monitoring of such activity.
More information is available via the IARC website dedicated to cervical anatomy, VIA-based cervical cancer screening and management (http://www.iarc.fr) as well as in WHO | Guidelines for screening and
precancerous lesions for cervical cancer prevention and WHO | Use of cryotherapy for cervical intraepithelial neoplasia.
Special acknowledgements to:
Special acknowledgements to: Prof. Aldo Campana, Ulrike Meyer-Hamme MD, Manuela Undurraga Maliverno MD, Milena Alec MD, Nadia Berkane MD, and Isabelle Navarria-Forney MD, for invested time in
supervision and critical comments on this course.
Course contents
Module 1: Anatomy of the cervix, squamocolumnar junction, metaplastic change and transformation zone - Pierre Vassilakos, Raluca Negulescu, Rosa Pinto Catarino
Module 2: Basic knowledge for cervical cancer screening using VIA, VILI and HPV test - Patrick Petignat, Raluca Negulescu, Milena Alec
Module 3: Treatment of VIA/VILI positive cases - Ulrike Meyer-Hamme, Milena Alec, Patrick Petignat, Hugo De Vuyst, Manuela Undurraga Malinverno, Raluca Negulescu
Module 4: How to proceed - Patrick Petignat, Raluca Negulescu, Milena Alec
Module 5: Quality assurance of visual inspection of the cervix - Ulrike Meyer-Hamme, Milena Alec, Patrick Petignat
Edited by Aldo Campana, 07/17/2021 06:36:29
https://www.gfmer.ch/ccdc/victest.htm 1/1
You might also like
- 9 Chia Seeds Benefits and Side EffectsDocument6 pages9 Chia Seeds Benefits and Side EffectsAli HassanNo ratings yet
- Bates Chapter 1 Flashcards - QuizletDocument6 pagesBates Chapter 1 Flashcards - Quizletaznknight323No ratings yet
- Respiratory Acidosis: Prepared By: Riezel Umaming Kathleen Testado Hazel AlarillaDocument16 pagesRespiratory Acidosis: Prepared By: Riezel Umaming Kathleen Testado Hazel AlarillaDareRaymond100% (2)
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- Cervical Cancer & PreventionDocument56 pagesCervical Cancer & PreventionTanvir AhmedNo ratings yet
- Cervical Cancer in PregnancyDocument21 pagesCervical Cancer in Pregnancymineresearch100% (1)
- CPG - Management of Breast Cancer (2nd Edition)Document100 pagesCPG - Management of Breast Cancer (2nd Edition)umiraihana1No ratings yet
- PropofolDocument3 pagesPropofolamelwd100% (1)
- Classification of Vacutainer Tubes by Color and FunctionDocument5 pagesClassification of Vacutainer Tubes by Color and FunctionNandor SiliNo ratings yet
- Complete Dentures: The Role of Occlusion in Preservation and Prevention in Complete Denture ProsthodonticsDocument18 pagesComplete Dentures: The Role of Occlusion in Preservation and Prevention in Complete Denture ProsthodonticsSahana Rangarajan100% (1)
- Audiology Case Study Treatment Plan ProjectDocument16 pagesAudiology Case Study Treatment Plan Projectapi-313722056No ratings yet
- Visual ScreeningDocument35 pagesVisual ScreeningabhagaurNo ratings yet
- Visual Inspection With Lugol's Iodine (VILI) : Evidence To DateDocument19 pagesVisual Inspection With Lugol's Iodine (VILI) : Evidence To Datecry13No ratings yet
- Paper ConDocument10 pagesPaper ConmaryamparasNo ratings yet
- Methods of Detecting Cervical Cancer: January 2011Document8 pagesMethods of Detecting Cervical Cancer: January 2011anon_312640252No ratings yet
- Visual Inspection With Acetic Acid (VIA) : Evidence To DateDocument16 pagesVisual Inspection With Acetic Acid (VIA) : Evidence To DateruntunNo ratings yet
- Cervical Cancer Screening and Its ImportanceDocument3 pagesCervical Cancer Screening and Its ImportanceBest Nollywood TvNo ratings yet
- Ardahan 2011Document6 pagesArdahan 2011Andi WijayaNo ratings yet
- Kyambogo University Faculty of EngineeringDocument17 pagesKyambogo University Faculty of EngineeringiangarvinsNo ratings yet
- Screening For Cancer Cervix by Visual Technique: University Sriwijaya Palembang Dept. Obstetrics and GynaecologyDocument35 pagesScreening For Cancer Cervix by Visual Technique: University Sriwijaya Palembang Dept. Obstetrics and GynaecologyMuthiah RamadhinaNo ratings yet
- Risk Factors of Cervical CanceDocument13 pagesRisk Factors of Cervical CanceAnis SolikahNo ratings yet
- Surabaya-Deteksi Dini Kanker Serviks UteriDocument32 pagesSurabaya-Deteksi Dini Kanker Serviks Uteripuskesmas manukan kulonNo ratings yet
- Effect of Cervicitis On Visual Inspection With Acetic AcidDocument5 pagesEffect of Cervicitis On Visual Inspection With Acetic AcidmonicamoniccNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyDr. Ivo Basílio Jr.No ratings yet
- WHO's Cervical Cancer Screening Programmes: Managerial GuidelinesDocument22 pagesWHO's Cervical Cancer Screening Programmes: Managerial GuidelinesMutiara JihadNo ratings yet
- Jgo 23 147Document6 pagesJgo 23 147Yosua_123No ratings yet
- Diagnosis and Treatment of Cervical Cancer in Pregnant WomenDocument6 pagesDiagnosis and Treatment of Cervical Cancer in Pregnant WomenSofi PiñaNo ratings yet
- Cervical CancerDocument22 pagesCervical CancerShandy Suwanto PutraNo ratings yet
- Epidemiology and Natural History Cervical CancerDocument30 pagesEpidemiology and Natural History Cervical Cancermuhammadnurul asmiNo ratings yet
- Can Visual Inspection With Acetic Acid Be Used As An Alternative To Pap Smear in Screening Cervical Cancer?Document5 pagesCan Visual Inspection With Acetic Acid Be Used As An Alternative To Pap Smear in Screening Cervical Cancer?Koda RiyahNo ratings yet
- Cc2013!66!72 Sankaranarayanan Incl T Page 2012Document5 pagesCc2013!66!72 Sankaranarayanan Incl T Page 2012ronie redsNo ratings yet
- Masas AnexialesDocument17 pagesMasas AnexialesEdwin CalleNo ratings yet
- Summary Recommendations of IFCPC 2021 Consensus Satellite Meeting On 25th JuneDocument7 pagesSummary Recommendations of IFCPC 2021 Consensus Satellite Meeting On 25th JuneVijay KumarNo ratings yet
- The Diagnostic Value of Ultrasound and Mammography in Detection of Breast Cancer in AlbaniaDocument10 pagesThe Diagnostic Value of Ultrasound and Mammography in Detection of Breast Cancer in AlbaniaIJPHSNo ratings yet
- Final Short PaperDocument4 pagesFinal Short PaperjeniferNo ratings yet
- Comparison and Correlation of VIA and Pap Smear in Detection of Precancerous Cervical LesionsDocument4 pagesComparison and Correlation of VIA and Pap Smear in Detection of Precancerous Cervical Lesionsbebek sakitNo ratings yet
- Breast Surgery Indications and TechniquesDocument302 pagesBreast Surgery Indications and TechniquesLasha OsepaishviliNo ratings yet
- Effective Screening10Document4 pagesEffective Screening10ponekNo ratings yet
- Guidelines For Cervical Cancer Screening in Malaysia 2023 Final (27.10.2023)Document66 pagesGuidelines For Cervical Cancer Screening in Malaysia 2023 Final (27.10.2023)p109403No ratings yet
- Successful Pregnancies in Female Cancer PatientsDocument16 pagesSuccessful Pregnancies in Female Cancer PatientsDolores GalloNo ratings yet
- gtg62 021211 OvarianmassesDocument14 pagesgtg62 021211 OvarianmassesMaryamNo ratings yet
- Thesis Statement On Cervical CancerDocument6 pagesThesis Statement On Cervical Cancerbkx3abyc100% (2)
- Cervical Cancer Main WorkDocument41 pagesCervical Cancer Main WorkocmainNo ratings yet
- Ca CervixDocument8 pagesCa CervixJanneth CardenasNo ratings yet
- JR 1 ToraDocument9 pagesJR 1 ToraCitra DewiNo ratings yet
- Management of Cervical CancerDocument29 pagesManagement of Cervical CancersangheetaNo ratings yet
- Pemeriksaan IVA Endy BandungDocument38 pagesPemeriksaan IVA Endy BandungpasebatNo ratings yet
- Palpable Nodules After Autologous Fat Grafting in Breast Cancer Patients: Incidence and Impact On Follow-UpDocument9 pagesPalpable Nodules After Autologous Fat Grafting in Breast Cancer Patients: Incidence and Impact On Follow-UpMarcos LouroNo ratings yet
- Cervical Cancer ManagementDocument20 pagesCervical Cancer ManagementinayahsyNo ratings yet
- Cervical Cytology in Women With Abnormal Cervix.: Dr. Veena Rahatgaonkar, Dr. Savita MehendaleDocument4 pagesCervical Cytology in Women With Abnormal Cervix.: Dr. Veena Rahatgaonkar, Dr. Savita MehendaleIOSR Journal of PharmacyNo ratings yet
- ASCCP Management Guidelines August 2014Document24 pagesASCCP Management Guidelines August 2014L I100% (1)
- Zhang 2013Document10 pagesZhang 2013ayuNo ratings yet
- Did El Phys Uterus 865821Document6 pagesDid El Phys Uterus 865821Agus TriwiNo ratings yet
- Ijgc 2020 001996Document8 pagesIjgc 2020 001996Sulaeman Andrianto SusiloNo ratings yet
- Ijcm 40 203Document5 pagesIjcm 40 203Aulia Putri ANo ratings yet
- ASCCP Management Guidelines - August 2014 PDFDocument24 pagesASCCP Management Guidelines - August 2014 PDFAnita BlazevskaNo ratings yet
- Evidence-Based, Alternative Cervical Cancer Screening Approaches in Low-Resource SettingsDocument6 pagesEvidence-Based, Alternative Cervical Cancer Screening Approaches in Low-Resource Settingschica_asNo ratings yet
- Ibreast Exam Overview 2Document16 pagesIbreast Exam Overview 2ikhan1234No ratings yet
- Nims MedsDocument13 pagesNims MedsWeng Villaverde PampoNo ratings yet
- Antenatal Fetal AssessmentDocument7 pagesAntenatal Fetal AssessmentFitriana Nur RahmawatiNo ratings yet
- A Case Presentation On AgiosarcomaDocument48 pagesA Case Presentation On AgiosarcomaAsniah Hadjiadatu AbdullahNo ratings yet
- Artigo Sobre CancerDocument10 pagesArtigo Sobre CancerSérgio Anick da Silva Brito SegundoNo ratings yet
- Intl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDocument17 pagesIntl J Gynecology Obste - 2021 - Bhatla - Cancer of The Cervix Uteri 2021 UpdateDamian BarrancoNo ratings yet
- Maternal and Fetal Outcomes in Patients With Systemic Lupus ErythematosusDocument6 pagesMaternal and Fetal Outcomes in Patients With Systemic Lupus ErythematosusWaris ZegaNo ratings yet
- Endoscopy in Pediatric Inflammatory Bowel DiseaseFrom EverandEndoscopy in Pediatric Inflammatory Bowel DiseaseLuigi Dall'OglioNo ratings yet
- Breast Cancer in Young WomenFrom EverandBreast Cancer in Young WomenOreste GentiliniNo ratings yet
- How to Perform Ultrasonography in EndometriosisFrom EverandHow to Perform Ultrasonography in EndometriosisStefano GuerrieroNo ratings yet
- Hambiso PHCU SBC PlanDocument15 pagesHambiso PHCU SBC PlanMulugeta DagneNo ratings yet
- Public Relations VECODDocument30 pagesPublic Relations VECODMulugeta DagneNo ratings yet
- Emotional IntelligenceDocument45 pagesEmotional IntelligenceMulugeta DagneNo ratings yet
- Delegation of AuthorityDocument16 pagesDelegation of AuthorityMulugeta DagneNo ratings yet
- ARVNurse Training WorkbookDocument57 pagesARVNurse Training WorkbookMulugeta DagneNo ratings yet
- ARVNurse Training ManualDocument71 pagesARVNurse Training ManualMulugeta DagneNo ratings yet
- Colposcopy and Treatment of Cervical Intraepithelial Neoplasia - A Beginners' ManualDocument10 pagesColposcopy and Treatment of Cervical Intraepithelial Neoplasia - A Beginners' ManualMulugeta DagneNo ratings yet
- Early Detection, Prevention, and Infections Branch (EPR) - IARCDocument5 pagesEarly Detection, Prevention, and Infections Branch (EPR) - IARCMulugeta DagneNo ratings yet
- Record Management AdjestedDocument25 pagesRecord Management AdjestedMulugeta DagneNo ratings yet
- All Communication IPV2 Rota HPVDocument24 pagesAll Communication IPV2 Rota HPVMulugeta DagneNo ratings yet
- Decision Making 11Document9 pagesDecision Making 11Mulugeta DagneNo ratings yet
- SOAEMgt Urti PRNTDocument2 pagesSOAEMgt Urti PRNTMulugeta DagneNo ratings yet
- General Frame WorkDocument85 pagesGeneral Frame WorkMulugeta DagneNo ratings yet
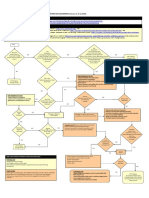
- VHF Algo PDFDocument1 pageVHF Algo PDFMulugeta DagneNo ratings yet
- 4.raggasaa Kabbadaa: Kan Ji'a Hagaya Bara 2012Document5 pages4.raggasaa Kabbadaa: Kan Ji'a Hagaya Bara 2012Mulugeta DagneNo ratings yet
- Assessment - Attempt ReviewDocument10 pagesAssessment - Attempt ReviewMulugeta DagneNo ratings yet
- Public Administration and BureaucracyDocument12 pagesPublic Administration and BureaucracyMulugeta DagneNo ratings yet
- Challenge Rules and Eligibility - Million Hearts®Document6 pagesChallenge Rules and Eligibility - Million Hearts®Mulugeta DagneNo ratings yet
- Oscar Sanchez: After Hospital Care Plan ForDocument12 pagesOscar Sanchez: After Hospital Care Plan ForMulugeta DagneNo ratings yet
- Indicative Target TemplateDocument11 pagesIndicative Target TemplateMulugeta DagneNo ratings yet
- FPCurriculum OnlineDocument166 pagesFPCurriculum OnlineMulugeta DagneNo ratings yet
- End of Life Care - Elearning For HealthcareDocument9 pagesEnd of Life Care - Elearning For HealthcareMulugeta DagneNo ratings yet
- Antibiotic Time Out Tool: AHRQ Safety Program For Improving Antibiotic UseDocument4 pagesAntibiotic Time Out Tool: AHRQ Safety Program For Improving Antibiotic UseMulugeta DagneNo ratings yet
- Clinical Audit Where ToDocument13 pagesClinical Audit Where ToMulugeta DagneNo ratings yet
- Working With Patient and Family Advisors:: AHRQ Safety Program For Perinatal CareDocument42 pagesWorking With Patient and Family Advisors:: AHRQ Safety Program For Perinatal CareMulugeta DagneNo ratings yet
- After Hospital Care Plan For: (Patient Name) Discharge Date: (Discharge Date)Document7 pagesAfter Hospital Care Plan For: (Patient Name) Discharge Date: (Discharge Date)Mulugeta DagneNo ratings yet
- H HC CG & Qic A P W: Ambiso Ction LAN OrksheetDocument2 pagesH HC CG & Qic A P W: Ambiso Ction LAN OrksheetMulugeta DagneNo ratings yet
- Social and Behavioral Change Communication: Key FactsDocument2 pagesSocial and Behavioral Change Communication: Key FactsMulugeta DagneNo ratings yet
- Unit 1 Introduction To Adolescence: 1.0 ObjectivesDocument33 pagesUnit 1 Introduction To Adolescence: 1.0 ObjectivesMulugeta DagneNo ratings yet
- Beliefs-Values-Attitudes and Their Impact On Our Performance As FacilitatorsDocument23 pagesBeliefs-Values-Attitudes and Their Impact On Our Performance As FacilitatorsMulugeta DagneNo ratings yet
- Borderline Personality Disorder Write Up 2Document8 pagesBorderline Personality Disorder Write Up 2Sreejita GhoshNo ratings yet
- Post Covid Effects On Annavaha Srotas W.S.R To Manasika BhavaDocument5 pagesPost Covid Effects On Annavaha Srotas W.S.R To Manasika BhavaEditor IJTSRDNo ratings yet
- SPECIMEN HANDLING GUIDELINE CorrectedDocument90 pagesSPECIMEN HANDLING GUIDELINE CorrectedDavindu AnushkaNo ratings yet
- Autism: DefinitionDocument6 pagesAutism: DefinitionBallave SudiptaNo ratings yet
- JC Effect of Gastric Lavage On Meconium Aspiration Syndrome and Feed Intolerance in Vigorous Infants Born With Meconium Stained Amniotic Fluid - A Randomized Control TrialDocument22 pagesJC Effect of Gastric Lavage On Meconium Aspiration Syndrome and Feed Intolerance in Vigorous Infants Born With Meconium Stained Amniotic Fluid - A Randomized Control TrialAbhinav AggarwalNo ratings yet
- Obat Pagi: No Generik Paten Sediaan Harga/tab Antibiotik, Antivirus, AntijamurDocument2 pagesObat Pagi: No Generik Paten Sediaan Harga/tab Antibiotik, Antivirus, Antijamursatria12No ratings yet
- Rahul BiologyDocument17 pagesRahul BiologykeerthiNo ratings yet
- Daily Medical Report Laporan Harian MedikDocument18 pagesDaily Medical Report Laporan Harian MedikLehman ManNo ratings yet
- A General Overview of Post Extraction Complicationsprevention Management and Importance of Post Extraction AdvicesDocument13 pagesA General Overview of Post Extraction Complicationsprevention Management and Importance of Post Extraction AdvicesBilqist Savannah PutriNo ratings yet
- Fimmu 10 00594Document13 pagesFimmu 10 00594Aleksandar DimkovskiNo ratings yet
- COVID - National Resources - UPDocument5 pagesCOVID - National Resources - UPVidit DixitNo ratings yet
- Detailed Lesson Plan in Mapeh 8Document13 pagesDetailed Lesson Plan in Mapeh 8Jeoffrey ArceNo ratings yet
- TRIUMPHANT COLLEGE COVID-19 TRAINING NewDocument26 pagesTRIUMPHANT COLLEGE COVID-19 TRAINING NewDaniellaNo ratings yet
- Doctors CV TemplateDocument3 pagesDoctors CV TemplateBoopathi KalaiNo ratings yet
- K5 - Family AssessmentDocument30 pagesK5 - Family AssessmentedelinNo ratings yet
- Work Conference Xvi: Final AnnouncementDocument23 pagesWork Conference Xvi: Final AnnouncementDyan TonyNo ratings yet
- 2019 Guide For ImmunizationDocument195 pages2019 Guide For ImmunizationReigner paul DavidNo ratings yet
- Standard 8Document8 pagesStandard 8Bridget GumboNo ratings yet
- B-Cell LymphomaDocument77 pagesB-Cell LymphomaH.B.ANo ratings yet
- Normal Value For Urine TestDocument2 pagesNormal Value For Urine TestMarcellino NernereNo ratings yet
- Endocrinologcazuri LP Limba EnglezăDocument17 pagesEndocrinologcazuri LP Limba EnglezăAna AlexandraNo ratings yet
- Ginjal PolikistikDocument6 pagesGinjal PolikistikNovi YudiaNo ratings yet
- Answers To PolioDocument3 pagesAnswers To PolioYoyoyo 123123No ratings yet