Professional Documents
Culture Documents
Drug Study 2
Uploaded by
Kristina Salariosa PachecoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Study 2
Uploaded by
Kristina Salariosa PachecoCopyright:
Available Formats
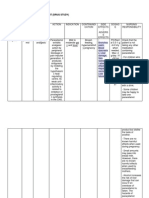
GENERIC NAME: Cefuroxime BRAND NAME: Ceftin, Zinacef Doctors Postoperative order: 750 mg/ IV ANST bid CLASSIFICATI
MECHANISM INDICATION DRUG ON OF ACTION INTERACTION >Antibiotic >Route: IV Parenteral: Drug-drug: >Cephalospor >Onset: >Lower >increased in (second Rapid respiratory nephrotoxicity generation) >Peak: infections with Immediate caused by aminoglycosides >Duration:18 Streptococcus >increased -24 hours pneumonia, S. bleeding effects >Metabolism: aureus, E. with oral Half-life: 1-2 coli, Klebsiella anticoagulants hours pnemoniae, >Distribution: H.influenzae, Drug-Lab test: Crosses the S. pyogenes >possibility of placenta, >Dermatologi false results of enters breast c infections tests urine milk caused by S. glucose using aureus, S. Benedicts pyogenes, E. solution, Fehlings coli, K. solution, Clinitest pneumonia, tablets, urinary Enterobacter 17-ketosteroids, >UTIs caused direct Coombs by E. coli, K. test pneumonia >Uncomplicat ed and disseminated gonorrhea caused by N. gonorrheae >Septicemia caused by S.
ADVERSE EFFECTS >CNS: headache, dizziness, lethargy, paresthesia >GI: nausea, vomiting, diarrhea, anorexia, abdominal pain, flatulence,pseudome mbranous colitis, hapatoxicity >GU: nephrotoxicity >Hematologic: Bone marrow depression >Hypersensitivity: ranging from rash to fever to anaphylaxis, serum sickness reaction >Local: pain, abscess at injection site, phlebitis, inflammation at I.V. site
NURSING RESPONSIBILITIES Assessment: >Hepatic and renal impairment, lactation, pregnancy >Physical: Skin status, liver function tests, renal function tests, culture of affected area, sensitivity tests Interventions: >Culture infection, and arrange for sensitivity tests before and during therapy if expected response is not seen >Give oral drug with food to decrease with G.I. upset and enhance absorption >Give oral drug to children who can swallow tablets, crushing the drug results in a bitter unpleasant taste >Have vitamin K available in ease hypothrombinemia >Discontinue if hypersensitivity reaction
pneumonia, S. aureus, E. coli, K. pneumonia, H. influenza >Meningitis caused by S. pneumonia, H influenza, S. aureus, N. meningitidis >Bone and joint infections due to S. aureus >Perioperativ e prophylaxis GENERIC NAME: Tramadol hydrochloride BRAND NAME: Ultram Doctors Postoperative order: 110 mg / IV/ q6hrs CLASSIFICATION MECHANISM OF INDICATION ACTION >Analgesic >Route: Oral >Relief to >Onset: 1 hour moderate to >Peak: 2 hour moderately > Metabolism: severe pain Hepatic, Half-life: 6-7 hours >Distribution: crosses placenta, enters breastmilk >Excretion: Urine
occurs
DRUG INTERACTION Drug-drug: >decreased effectiveness with carbamazepine >Increased risk of tramadol toxicity with monoamine oxidase inhibitor
ADVERSE EFFECTS >CNS: sedation, dizziness or vertigo, headache, confusion, dreaming, sweating anxiety, seizures >CV: hypotension, tachycardia, bradycardia
NURSING RESPONSIBILITIES Assessment: >History: Hypersensitivity to tramadol, pregnancy, acute intoxication with alcohol, opioids, psychotropic drugs or other centrally acting analgesics, lactation,
>Dermatologic: sweating, pruritus, rash, pallor, urticaria >GI: nausea, vomiting, dry mouth, constipation, flatulence
seizures, concomitant use of CNS depressant or monoamine oxidase inhibitor, renal or hepatic impairment >Physical: Skin colour, texture, lesions; orientation, reflexes , bilateral grip strength, affect; p, auscultation, BP; bowel sounds, normal output; LFTs, renal function test Interventions: >Control environment (temperature, lighting) if sweating or CNS effects occur. WARNING: limit use in patient with past present history of addiction to or dependence on opiods.
GENERIC NAME: Ketorolac tromethamine BRAND NAME: Acular, Acular LS, Acular PF (ophthalmic), Toradol Doctors Postoperative order: 30 mg / IV q8hrs CLASSIFICATION MECHANISM OF INDICATION DRUG ACTION INTERACTION >NSAID >Route: IV,IM >Short-term Drug-Drug: >Nonopioid >Onset: 30mins management of >increased risk analgesic >Peak: 1-2 hours pain (up to 5 of nephrotoxicity >Antipyretic >Duration 6 days) with other hours >Ophthalmic: nephrotoxins >Metabolism: Relief of ocular (aminiglycosides, Crosses placenta, itching due to cyclosporine) enters breast seasonal >increased risk milk conjunctivitis and of bleeding with Excretion: Urine relief of anticoagulants postoperative (warfarin), aspirin inflammation after cataract surgery
ADVERSE EFFECTS >CNS: headache, dizziness, somnolence, insomnia >Dermatologic: rash, pruritus, sweating, dry mucous membranes >GI: nausea, dyspepsia, GI pain, diarrhea, vomiting, constipation, flatulence, gastric or duodenal ulcer GU: dysuria, renal impairment Hematologic: bleeding, platelet inhibition with higher doses, neutropenia, eosinophilia, leucopenia, pancytopenia, thrombocytopeni a, argranulocytosis, granulocytopenia , aplastic anemia,
NURSING RESPONSIBILITIES Assessment: >History: Renal impairment, impaired hearing, allergies, hepatic, CV, and GI conditions, lactation, pregnancy >Physical: Skin color and lesions, orientation, reflexes, ophthalmologic and audiometric evaluation, peripheral sensation, peripheral edema, BP, respiratory adventitious sounds, CBC, clotting time, liver function tests, renal function test, serum electrolytes, stool guaiac Interventions: >Be aware that
decreased Hgb oc Hct, bone marrow depression, menorrhagia Respiratory: dyspnea, hemoptysis, bronchospasm, rhinitis Other: peripheral edema, anaphylactoid reactions to anaphylactic shock, local burning, stinging (ophthalmic)
the patient may be at risk for CV events, GI bleeding, renal toxicity, monitor accordingly >Do not use during labor, delivery or while nursing >keep emergency equipment readily available at time of initial dose in case of severe hypersensitivity reactions >Protect drug vials from light >Administer every 6 hours to maintain serum levels and control pain
GENERIC NAME: Ranitidine hydrochoride BRAND NAME: Apo-Ranitidine (CAN), CO Ranitidine (CAN), Gen- Ranitidine, Zantac Doctors Postoperative order: 50mg/ IV q8hrs while in NPO CLASSIFICATION MECHANISM OF INDICATION DRUG ADVERSE ACTION INTERACTION EFFECTS .>Histamine2 >Route: IV >Short-term Drug-Drug: >CNS: headache, antagonist >Onset: treatment of >increased malaise, Immediate duodenal ulcer effects of dizziness, >Peak: 5-10mins >Maintenance warfarin, tricyclic somnolence,
NURSING RESPONSIBILITIES Assessment: >History: Allergy to ranitidine, impaired renalor
>Duration: 8-12 hours >Metabolism: Hepatic, Half-life: 2-3 hours >Distribution: Cross placenta, enters breast milk >Excretion: Urine
therapy for duodenal ulcer at reduced dose >Short-term treatment of active, benign, gastric ulcer >Short-term treatment of GERD >Pathologic hypersecretory conditions >Treatment of erosive esophagitis >Treatment of heartburn, acid indigestion, sour stomach
antidepressants
insomnia, vertigo >CV: tachycardia, bradycardia, premature ventricular contractions >Dermatologic: Rash, alopecia >GI: constipation, diarrhea, vomiting, abdominal pain, hepatitis, increased alanine transaminase levels >GU: gynecomastia, impotence or decreased libido >Hematologic: leucopenia, granulocytopenia , thrombocytopeni a, pancytopenia >Local: pain at IM site, local burning or itching at IV site >Other: anthralgias
hepatic function, lactation, pregnancy >Physical: Skin lesions, orientation, affect pulse, baseline ECG, liver evaluation, abdominal examination, normal output, CBC, liver function test, renal function test Interventions: >Administer oral drug with meals and at bedtime >Decrease doses in renal and liver failure >Provide concurrent antacid therapy to relieve pain >Administer IM dose undiluted, deep into large muscle groups >Arrange for regular folow-up, including blood tests to evaluate effects
Feso4 GENERIC NAME: ferrous sulfate BRAND NAME: fer-iron, feosol, iberet Doctors Postoperative order: CLASSIFICATION MECHANISM OF ACTION Anti anemic > Elevates the serum iron concentration which then helps to form High or trapped in the reticuloendotheli al cells for storage and eventual conversion to a usable form of iron.
INDICATION >Prevention and treatment of iron deficiency anemias. > Dietary supplement for iron.
DRUG INTERACTION >The following medications may reduce the absorption of ferrous sulfate: ACE Inhibitors Bile Acid Sequestrants Birth Control Medications Carbidopa, levadopa Cimetidine Famotidine Levothyroxine Nizatidine Proton-pump Inhibitors Quinolones Tetracycline
ADVERSE EFFECTS >Dizziness N&V Nasal Congestion Dyspnea Hypotension CHF MI Muscle cramps Flushing
NURSING RESPONSIBILITIES Assessment: >Advise patient to take medicine as prescribed. Caution patient to make position changes slowly to minimize orhtostatic hypotension. Instruct patient to avoid concurrent use of alcohol or OTC medicine without consulting the physician. Advise patient to consult physician if irregular heartbeat, dyspnea, swelling of hands and feet and hypotension occurs. Inform patient that angina
attacks may occur 30 min. after administration due reflex tachycardia. Encourage patient to comply with additional intervention for hypertension like proper diet, regular exercise, lifestyle changes and stress management.
ascorbic ACID GENERIC NAME: BRAND NAME: Doctors Postoperative order: CLASSIFICATION MECHANISM OF ACTION >vitamins > Ascorbic acid is a functional and principal in vivo form of vitamin C, an essential water-soluble vitamin which is fundamental in the synthesis of collagen and intercellular
INDICATION > Prophylaxis and treatment of scurvy and as a dietary supplement. >Increases protection mechanism of the immune system, thus supporting
DRUG INTERACTION Deferroxamine, hormonal contraceptives, flufenazine,eleme ntal iron, salicylates, warfarin, fluphenazine, disulfiram, mexiletine,
ADVERSE EFFECTS >GI: Nausea, vomiting, heartburn, diarrhea. >Hematologic: Acute hemolytic anemia (patients with deficiency of G6PD); sickle cell crisis. >CNS: Headache
NURSING RESPONSIBILITIES Assessment: >
materials.
wound healing. Necessary for wound healing and resistance to infection.
vitamin B12.
(high doses). Urogenital: Urethritis, dysuria, crystalluria (high doses) > Other: Mild soreness at injection site; dizziness and temporary faintness with rapid IV administration.
mefenamic acid GENERIC NAME: BRAND NAME: ponstel Doctors Postoperative order: CLASSIFICATION MECHANISM OF ACTION Non steroidal anti >aspirin like drug inflammatory that has analgesic, anti pyretic and anti inflammatory activities.
INDICATION > relief of pain including muscular, rheumatic, traumatic, dental, post op and post partum pain, headache, migraine, fever
DRUG INTERACTION Anticoagulants Increased risk of gastric erosion and bleeding. Cyclosporine Nephrotoxicity of both agents may
ADVERSE EFFECTS >Cardiovascular Edema; weight gain; CHF; altered BP; palpitations; chest pain; bradycardia;
NURSING RESPONSIBILITIES Assessment: >
and dysmenorrhea
be increased. CYP-450 Exercise caution when coadministering mefenamic acid with drugs known to inhibit the isoenzyme 2C9. Lithium Serum lithium levels may be increased. Methotrexate Increased methotrexate levels. Salicylates Additive GI toxicity.
tachycardia.
>CNS Headache; vertigo; drowsiness; dizziness; insomnia. >Dermatologic Rash; urticaria; purpura. >EENT Blurred vision; tinnitus; salivation; glossitis. >GI Diarrhea; dry mouth; vomiting; abdominal pain; dyspepsia; GI bleeding; nausea; constipation; flatulence.
>Genitourinary Hematuria; proteinuria; dysuria; renal failure. >Hematologic Decreased hematocrit; bleeding; neutropenia; leukopenia; pancytopenia; eosinophilia; thrombocytopeni a. >Hepatic Mild elevations in LFT results. >Respiratory Bronchospasm; laryngeal edema; rhinitis; dyspnea; pharyngitis; hemoptysis; shortness of
breath. >Miscellaneous Autoimmune hemolytic anemia may occur if used long term.
Diphenhydramine GENERIC NAME: BRAND NAME: benadryl Doctors Postoperative order: CLASSIFICATION MECHANISM OF ACTION Anti histamine >Antagonizes the effect of histamine at H1 receptor sites; does not bind or inactivate histamine
INDICATION > Allergic diseases such as hay fever, allergic rhinitis, urticaria, angioedema, atopic dermatitis, contact dermatitis, gastrointestinal allergy, pruritus, physical allergies, reactions to injection of contrast media,
DRUG INTERACTION Masks ototoxicity produced by aminoglycosides. Increases gastric degradation of levodopa and decreases its absorption by reduction of gastric emptying. Antagonises
ADVERSE EFFECTS >CNS: headache, fatigue, anxiety, tremors, vertigo, confusion, depression, seizures, hallucinations CV: tachycardia, palpitations, orthostaic hypotension,
NURSING RESPONSIBILITIES Assessment: >
reactions to therapeutic preparations and allergic transfusion reactions; also postoperative nausea and vomiting, motion sickness, and quieting emotionally disturbed children.
therapeutic effects of cholinergic agents e.g. tacrine, donezepil and neuroleptics. Valerian, St. John's wort, Kava Kava and gotu kola may increase CNS depression. Potentially Fatal: Potentiates CNS depression with alcohol, barbiturates, analgesics, sedatives and neuroleptics. Additive antimuscarinic action with MAOIs, atropine and TCAs.
heart failure EENT: blurred vision GI: dry mouth, nausea, vomiting, constipation, flatulence GU: urinary hesitancy or frequency, urine retention Hematologic: leukopenia Skin: photosensitivity, dermatitis
calcium gluconate GENERIC NAME: BRAND NAME: Doctors Postoperative order: CLASSIFICATION MECHANISM OF ACTION >Calcium gluconate is
used to prevent or treat negative calcium balance. It also helps
INDICATION >
DRUG INTERACTION
Co-admin of high calcium doses with thiazide diuretics may result in milk-alkali
ADVERSE EFFECTS >GI irritation; softtissue calcification, skin sloughing or necrosis after IM/SC inj.
NURSING RESPONSIBILITIES Assessment: >
facilitate nerve and muscle performance as well as normal cardiac function. Absorption: Soluble calcium is predominantly absorbed from the small intestine by active transport and passive diffusion. Small intestines by active transport and passive diffusion. There is increased absorption in calcium deficiency and during childhood, pregnancy and lactation. Distribution: Crosses the placenta and enters breast milk. Excretion: Excreted mainly in the kidneys (as excess calcium), faeces (as unabsorbed calcium) with traces found in sweat, skin, hair and nails.
syndrome and hypercalcaemia. May potentiate digoxin toxicit y. Decreases effects of calcium-channel blockers. Enhanced absorption with calcitriol (a vitamin D metabolite).
Hypercalcaemia characterised by anorexia, nausea, vomiting, constipation, abdominal pain, muscle weakness, mental disturbances, polydipsia, polyuria, nephrocalcinosis, renal calculi; chalky taste, hot flushes and peripheral vasodilation. Potentially Fatal: Cardiac arrhythmias and coma.
You might also like
- Generic NameDocument8 pagesGeneric Namemel aquinoNo ratings yet
- Cva Smh301 (Next)Document14 pagesCva Smh301 (Next)Christine OjedaNo ratings yet
- Drug StudyDocument9 pagesDrug StudyShiara Ruth EdrosoloNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Diagnosis Planning Implementation Rationale Evaluationthomasfinley44No ratings yet
- Dugs CVADocument10 pagesDugs CVAMarie AntoinetteNo ratings yet
- Ranitidine Hydrochloride: Generic Name Therapeutic Actions Indications Side Effects Nursing ActionsDocument5 pagesRanitidine Hydrochloride: Generic Name Therapeutic Actions Indications Side Effects Nursing ActionsAyanne ArcenaNo ratings yet
- Drug StudyDocument6 pagesDrug StudyChickz HunterNo ratings yet
- Medication Work Sheet For MedSurgDocument5 pagesMedication Work Sheet For MedSurgRyanMitchell100% (2)
- Stan Drug StudyDocument10 pagesStan Drug StudyIvan Louise Fajardo ManiquizNo ratings yet
- Drug StudiesDocument16 pagesDrug Studiesvitcloud23100% (2)
- Drug Study ProjectDocument7 pagesDrug Study ProjectMaRic Gabutin Guerra100% (1)
- TB Drug StudyDocument15 pagesTB Drug StudyKaloy KamaoNo ratings yet
- Drugs Study, Nursing, PreoperativeDocument9 pagesDrugs Study, Nursing, PreoperativeKevin Sam AguirreNo ratings yet
- Complete Drug StudyDocument239 pagesComplete Drug StudyRPh Krishna Chandra Jagrit0% (1)
- Ciprofloxacin CiproDocument1 pageCiprofloxacin CiproKristi WrayNo ratings yet
- NCP DrugDocument13 pagesNCP DrugMhar CamposanoNo ratings yet
- Drug StudyDocument8 pagesDrug StudySarie LevitaNo ratings yet
- Drug StudyDocument6 pagesDrug StudyNajmah Saaban100% (1)
- Mefenamic Acid Drug ProfileDocument3 pagesMefenamic Acid Drug ProfileAhmad WaliNo ratings yet
- Name of Drug Mechanism of Action Indications Contra-Indications Side Effects Nursing ConsiderationsDocument10 pagesName of Drug Mechanism of Action Indications Contra-Indications Side Effects Nursing ConsiderationsmidskiescreamzNo ratings yet
- Drug StudyDocument7 pagesDrug StudyCee SanchezNo ratings yet
- Drug StudyDocument4 pagesDrug StudyCharlayne AnneNo ratings yet
- Drug StudyDocument7 pagesDrug StudyJoy Jarin100% (1)
- Hesi Maternity Ob PDFDocument32 pagesHesi Maternity Ob PDFcclaire197% (37)
- Ward6 Drug StudyDocument6 pagesWard6 Drug StudyMichael Lloyd T. SabijonNo ratings yet
- Drug StudyDocument13 pagesDrug StudyAldrin Ian Oraza AlpeNo ratings yet
- Drug StudyDocument5 pagesDrug StudyJanine Erika Julom BrillantesNo ratings yet
- Drug StudyDocument10 pagesDrug StudyDeca TanNo ratings yet
- Drug Study 2Document9 pagesDrug Study 2Justin PasaronNo ratings yet
- Drug and ClassificationDocument4 pagesDrug and ClassificationdavidcalaloNo ratings yet
- Drug StudyDocument8 pagesDrug StudyRizzi DeveraNo ratings yet
- Drugs StudyDocument7 pagesDrugs Studymcmac24No ratings yet
- CHH Drug Study Week 2Document25 pagesCHH Drug Study Week 2maryxtine24No ratings yet
- KetorolacDocument5 pagesKetorolacMichelle Ann P. NacuaNo ratings yet
- Common Bile DuctDocument28 pagesCommon Bile DuctAmanda ScarletNo ratings yet
- Gastrointestinal System: Antihistamine Half-Life: Onset: Peaks: DurationDocument3 pagesGastrointestinal System: Antihistamine Half-Life: Onset: Peaks: DurationsyerlyNo ratings yet
- Nifedipine and Prednisone Drug StudyDocument5 pagesNifedipine and Prednisone Drug StudyAllyne GavinoNo ratings yet
- Jam (Drug Study)Document11 pagesJam (Drug Study)Vincent QuitorianoNo ratings yet
- Grp25 Rivera, Mikhail Bien.. MICU Drug StudyDocument11 pagesGrp25 Rivera, Mikhail Bien.. MICU Drug Studysinister17No ratings yet
- Medication Classificatio N Action Indication Contraindication Adverse Effect Nursing Intervention Generic Name: CNS: GIDocument4 pagesMedication Classificatio N Action Indication Contraindication Adverse Effect Nursing Intervention Generic Name: CNS: GIKathleenDawalNo ratings yet
- NLM MedicatingDocument11 pagesNLM MedicatingQuimberly ModequilloNo ratings yet
- CelecoxibDocument2 pagesCelecoxibXtinegoNo ratings yet
- Drug StudyDocument8 pagesDrug Studykarenkaren09No ratings yet
- Drug Name General Action Specific Action Indication Contraindication Adverse Effect Nursing ResDocument9 pagesDrug Name General Action Specific Action Indication Contraindication Adverse Effect Nursing ResDustin JohnNo ratings yet
- Drug StudyDocument5 pagesDrug StudyJann Zaniel Allayne RiNo ratings yet
- Drug StudyDocument4 pagesDrug StudyAbigail LonoganNo ratings yet
- DrugsDocument11 pagesDrugsClarence Lyndyll ToldingNo ratings yet
- Case Presentation - Hypovolemic ShockDocument19 pagesCase Presentation - Hypovolemic ShockIvy Jenica Mamuad50% (2)
- Doms DrugsDocument5 pagesDoms DrugsMikz JocomNo ratings yet
- Drug Study GentamicinDocument3 pagesDrug Study GentamicinEARL GERALD RICAFRANCANo ratings yet
- Final Drug StudyDocument22 pagesFinal Drug StudyPaula Xavier AlfalahiNo ratings yet
- Hemostan, Methergine CA Gluconate2Document4 pagesHemostan, Methergine CA Gluconate2Stacy MC PelitoNo ratings yet
- Drug Analysis: Submitted By: GALICINAO, Gretta Shalou GDocument9 pagesDrug Analysis: Submitted By: GALICINAO, Gretta Shalou GggalicinaoNo ratings yet
- Drug Study 1Document4 pagesDrug Study 1bibet_martijaNo ratings yet
- Management of HyperuricemiaDocument23 pagesManagement of HyperuricemiaSoad ShedeedNo ratings yet
- Drug Study For FractureDocument4 pagesDrug Study For FractureitsmeayaNo ratings yet
- Drug StudyDocument70 pagesDrug Studyjahmaicao50% (2)
- Mefenamic Acid Indication, Dosage, Side Effect, Precaution MIMS MalaysiaDocument1 pageMefenamic Acid Indication, Dosage, Side Effect, Precaution MIMS MalaysianuruladyanisaifuzzamanNo ratings yet
- IJSCR 109192 Session ReportDocument11 pagesIJSCR 109192 Session ReportFarhan ShahzadNo ratings yet
- On January 1 2017 Plutonium Corporation Acquired 80 of TheDocument1 pageOn January 1 2017 Plutonium Corporation Acquired 80 of TheMuhammad ShahidNo ratings yet
- An Investigation Into The Use of GAMA Water Tunnel For Visualization of Vortex Breakdown On The Delta WingDocument7 pagesAn Investigation Into The Use of GAMA Water Tunnel For Visualization of Vortex Breakdown On The Delta WingEdy BudimanNo ratings yet
- Finned Surfaces: Name:Mohamed Hassan Soliman ID:190513 DR - Mohamed HassanDocument7 pagesFinned Surfaces: Name:Mohamed Hassan Soliman ID:190513 DR - Mohamed HassanMohamed HassanNo ratings yet
- Larranaga V CADocument15 pagesLarranaga V CAKhay AnnNo ratings yet
- Amigurumi Angel FishDocument3 pagesAmigurumi Angel FishcapricorntranNo ratings yet
- Sadza: ChickenDocument13 pagesSadza: ChickenTsitsi Ngara SibandaNo ratings yet
- Hm1317cb PBDocument4 pagesHm1317cb PBJose SanchezNo ratings yet
- Contrasting MO and VB TheoryDocument4 pagesContrasting MO and VB TheoryPhillimonNo ratings yet
- Cultural Identity - EditedDocument6 pagesCultural Identity - EditedBrian KipkoechNo ratings yet
- Loading Ericsson GPEH Files - Into ANALYZER - Tech NotesDocument9 pagesLoading Ericsson GPEH Files - Into ANALYZER - Tech Notesbmaia18No ratings yet
- Thesis Ankit Yadav (12BBT0021)Document72 pagesThesis Ankit Yadav (12BBT0021)AnkitMohilNo ratings yet
- Budget Preparation: Lesson 3.2Document24 pagesBudget Preparation: Lesson 3.2JOSHUA GABATERONo ratings yet
- Hci - Web Interface DesignDocument54 pagesHci - Web Interface DesigngopivrajanNo ratings yet
- Vice President Procurement Supply Chain in Dallas TX Resume Gary McKownDocument3 pagesVice President Procurement Supply Chain in Dallas TX Resume Gary McKownGarymckownNo ratings yet
- L3 - Lesson PlanDocument6 pagesL3 - Lesson PlanPaola PinedaNo ratings yet
- 123 AP / 0123 TS: Intermediate Public Examinations - 2024Document3 pages123 AP / 0123 TS: Intermediate Public Examinations - 2024srinivasveeravalli123aNo ratings yet
- Sentence Transformation - Perfect TensesDocument3 pagesSentence Transformation - Perfect TensesMaría Esperanza Velázquez Castillo100% (2)
- Pleural Fluid AspirationDocument2 pagesPleural Fluid AspirationThe Multilingual MedicNo ratings yet
- Dependent PrepositionDocument4 pagesDependent PrepositionSolange RiveraNo ratings yet
- Divorce LegislationDocument9 pagesDivorce LegislationJedi Argyll BalisongNo ratings yet
- Maximus Price ResumeDocument2 pagesMaximus Price Resumeapi-491233681No ratings yet
- 440465-Aanchal ResumeDocument5 pages440465-Aanchal ResumevinodbhosaleNo ratings yet
- Piano 2023 2024 Grade 6Document13 pagesPiano 2023 2024 Grade 6Lucas Moreira0% (1)
- Experimentation, Orgasms, and The Rise of Anal Sex. - by William Saletan - SDocument13 pagesExperimentation, Orgasms, and The Rise of Anal Sex. - by William Saletan - Saweawerwerwe100% (1)
- First Degree Price DiscriminationDocument19 pagesFirst Degree Price DiscriminationRavi KiranNo ratings yet
- That Thing Called Tadhana ReviewDocument5 pagesThat Thing Called Tadhana ReviewLian BastidaNo ratings yet
- Senate - Community Projects 2009-10Document98 pagesSenate - Community Projects 2009-10Elizabeth Benjamin100% (3)
- Turla v. CaringalDocument2 pagesTurla v. CaringalTrina RiveraNo ratings yet
- One Pager by Capgemini Mechanical Design and Simulation ServicesDocument4 pagesOne Pager by Capgemini Mechanical Design and Simulation ServicesSmita GadreNo ratings yet