Professional Documents
Culture Documents
Disposition of Nasal, Intravenous, and Oral Methadone in Healthy Volunteers
Uploaded by
Kristin BurghardtOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Disposition of Nasal, Intravenous, and Oral Methadone in Healthy Volunteers
Uploaded by
Kristin BurghardtCopyright:
Available Formats
Disposition of nasal, intravenous, and oral methadone in healthy volunteers
Objective: Nasal administration of many opioids demonstrates rapid uptake and fast onset of action. Nasal administration may be an alternative to intravenous and oral administration of methadone and was therefore studied in human volunteers. Methods: The study was approved by the Institutional Review Board of the University of Washington, Seattle. Eight healthy volunteers (6 men and 2 women) aged 19 to 33 years were enrolled after informed written consent was obtained. Subjects received 10 mg methadone hydrochloride nasally, orally, or intravenously on 3 separate occasions in a crossover design. Nasal methadone (50 mg/mL in aqueous solution) was given as a 100- L spray in each nostril (Pfeiffer BiDose sprayer). Blood samples for liquid chromatography-mass spectrometry analyses of methadone and the metabolite 2-ethyl-1,5-dimethyl-3,3-diphenylpyrrolinium were drawn for up to 96 hours. The methadone effect was measured by noninvasive infrared pupilometry coincident with blood sampling. Results: Nasal uptake of methadone was rapid, with maximum plasma concentrations occurring within 7 minutes. The maximum effects of intravenous, nasal, and oral methadone, on the basis of dark-adapted pupil diameter, were reached in about 15 minutes, 30 minutes, and 2 hours, respectively. The respective durations were 24, 10, and 8 hours. Both nasal and oral bioavailabilities were 0.85. Subjects reported that nasal methadone caused a burning sensation. Conclusions: Nasal administration of methadone results in rapid absorption and onset of effect and high bioavailability, which was greater than that reported for other nasal opioids, with a similar duration of effect. Nasal administration may be an alternative route of methadone administration; however, improved formulations are desirable to reduce nasal irritation. (Clin Pharmacol Ther 2002;72:536-45.)
Ola Dale, MD, PhD, Christine Hoffer, AS, Pamela Sheffels, BS, and Evan D. Kharasch, MD, PhD Seattle, Wash, and Trondheim, Norway
Oral opioids are the mainstay of long-term therapy for cancer pain in conjunction with radiotherapy and
From the Department of Anesthesiology, University of Washington, Seattle; and Department of Anesthesia and Medical Imaging, Norwegian University of Science and Technology, and Department of Anesthesia and Intensive Care, St Olavs University Hospital, Trondheim. Supported in part by Norwegian Research Council grant 136286/300 (O.D.), National Institutes of Health grants K24 DA00417 and R01DA 14211, a Merit Award from the Veterans Affairs Medical Research Bureau (E.D.K.), and National Institutes of Health grant M01-RR-00037 to the University of Washington General Clinical Research Center. Received for publication May 13, 2002; accepted July 2, 2002. Reprint requests: Ola Dale, MD, PhD, Department of Anesthesia and Medical Imaging, Norwegian University of Science and Technology, 7489 Trondheim, Norway. E-mail: ola.dale@medisin.ntnu.no Copyright 2002 by the American Society for Clinical Pharmacology & Therapeutics. 0009-9236/2002/$35.00 0 13/1/128386 doi:10.1067/mcp.2002.128386
chemotherapy.1,2 For the last decade, controlled-release oral morphine has been a principal therapy because it reasonably maintains analgesic concentrations within the desired therapeutic range. However, breakthrough pain with a rapid onset and brief duration is common,1,3 often occurring at the end of the regular opioid dosing interval.3 Thus current opioids for treatment of baseline pain frequently have an insufcient duration of action. Methadone has attracted renewed interest in palliative care.4-13 It differs from morphine pharmacologically by its antagonist action on the N-methyl-Daspartate receptor, its lack of active metabolites, its high oral bioavailability, its relative independence from renal excretion, and, nally, its long terminal halflife.11,14-23 The long terminal half-life may theoretically lead to accumulation and toxicity in patients4; however, a recent study demonstrated its safe use in outpatients.13 The usefulness of methadone for patients who are not properly treated with morphine, because of either adverse effects or inadequate pain relief, has
536
CLINICAL PHARMACOLOGY & THERAPEUTICS VOLUME 72, NUMBER 5
Dale et al
537
been documented in several reports, underlining the pharmacologic differences between the two opioids.24,25 Methadone is an inexpensive alternative to other opioids.8,26 Most patients with moderate to severe pain from cancer can be treated with oral opioids, but 50% to 70% will require alternative routes of administration.27 For methadone, only oral and intravenous commercial formulations are available, because subcutaneous infusion has been abandoned.28 Nasal administration is an alternative route that may achieve rapid opioid onset of effect. The nasal mucosa has characteristics that favor rapid drug uptake.29,30 Pharmacokinetic studies with various opioids have shown bioavailabilities of 50% to 70%, which are generally higher than for oral or rectal administration. Maximum serum concentrations have been reached 10 to 50 minutes after administration.30-35 Studies in postoperative patients with nasal opioids have demonstrated mean times of onset of pain relief from 12 to 16 minutes.30,36-38 The use of nasal fentanyl in patients with cancer pain has also been reported.39 The slow elimination and long duration of the methadone effect, allowing for relatively infrequent dosing, make it an attractive candidate for nasal administration in selected patients. The disposition of nasally administered methadone has not been previously studied. To use drugs by various routes safely, it is important to provide comparative pharmacokinetic data. Comparative time-course data on opioid effectsfor instance, noninvasive pupilometry40,41may show outcome differences after pharmacologic interventions.42-44 Thus the goal of this study was to compare the disposition and pharmacodynamics of orally, nasally, and intravenously administered methadone in young healthy volunteers. METHODS Ethics This study was conducted according to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board for Human Studies at the University of Washington Medical Center, Seattle, Wash. Informed written consent was obtained from subjects before inclusion. Inclusion and exclusion criteria Healthy male and female volunteers, aged 18 to 40 years, were eligible. Subjects with a history of liver disease, those who were taking any medications metabolized by or affecting cytochrome P450 (CYP) 3A, and those who had any local nasal disease, any history of drug allergies, or a history of drug abuse or professional
access to drugs of abuse were excluded from the study. Pregnant women were also excluded. Eight subjects (6 men and 2 women), aged 19 to 33 years, were studied. The weight and height (given as median with range in parentheses) of the men were 73.5 kg (59-99 kg) and 177 cm (167-182 cm), respectively, and those of the women were 59 kg (57-61 kg) and 151 cm (150-152 cm). Setting and design The setting for this study was the General Clinical Research Center facilities at the University of Washington Medical Center. Subjects received 10 mg methadone hydrochloride intravenously, orally, or nasally. Although the original design was a randomized 3-way crossover study, subjects were randomized to receive oral or intravenous methadone, followed by nasal methadone, because of a delay in obtaining the nasal formulation. Each study session consisted of a 13-hour stay in the clinical research center, followed by daily visits for 4 additional days. The sessions were separated by at least 1 week. Drug doses and administration Ten milligrams of methadone hydrochloride (corresponding to 8.94 mg free base) (Roxane Laboratories, Inc, Columbus, Ohio) was administered at each session. Commercial preparations were used for intravenous (10 mg/mL) and oral (2 mg/mL) administration. Nasal methadone was prepared by the hospital pharmacy by dissolving methadone (dry substance) in sterile water to a concentration of 50 mg/mL. The pH of the solution (5.4) was not adjusted. The nasal dose was given with a Pfeiffer BiDose sprayer (Ing. Erich Pfeiffer GmbH, Radolfzell, Germany); one actuation delivered 100 L in each nostril. Procedures Because certain foods may affect drug kinetics, volunteers were asked not to ingest alcohol, grapefruit, grapefruit juice, caffeine, or medications for 12 hours before and during each study period (6 days). Subjects were asked to abstain from food and liquids after midnight the day before methadone administration. For each methadone administration, one or two peripheral intravenous catheters were inserted in a hand or arm vein for drug administration and blood sampling. Subjects were monitored for 2 hours (blood pressure and oxygen saturation). Oxygen was administered if oxygen saturation decreased below 94%. Venous blood samples (5 mL) were drawn at 0, 2, 5, 10, 15, 30, 45, and 60 minutes and 1.5, 2, 3, 4, 5, 6, 7,
538
Dale et al
CLINICAL PHARMACOLOGY & THERAPEUTICS NOVEMBER 2002
Fig 1. The time course (0-96 hours) of plasma concentrations of methadone (mean and standard deviation [SD]) in 8 healthy volunteers after intravenous (IV), oral, and nasal administration of methadone hydrochloride (HCl) (10 mg). Pharmacokinetic calculations are shown in Table I.
Fig 2. The time course (0-2 hours) of plasma concentrations of methadone (mean and SD) in 8 healthy volunteers after IV, oral, and nasal administration of methadone HCl (10 mg). Note the linear scale on the ordinate. Pharmacokinetic calculations are shown in Table I. 8, 10, and 12 hours after drug administration on the rst day. Subjects were given a standard breakfast 2 hours after methadone administration and had free access to food thereafter. Subjects were admonished not to drive, operate machinery, or engage in any other dangerous activity for the remainder of the day. Subjects returned once daily for additional blood sampling at 24, 48, 72, and 96 hours after drug administration. Dark-adapted pupil diameter was assessed by noninvasive infrared pupilometry (Pupilscan, model 6; Fairville Medical Op-
CLINICAL PHARMACOLOGY & THERAPEUTICS VOLUME 72, NUMBER 5
Dale et al
539
tics, Inc, United Kingdom) at every methadone determination, except at 12 hours.40-42 In addition, pupilometry was performed at 3, 5, and 7 hours. Analysis Plasma concentrations of methadone and its metabolites 2-ethyl-1,5-dimethyl-3,3-diphenylpyrrolinium (EDDP) and 2-ethyl-5-methyl-3,3-diphenylpyrroline (EMDP) were determined by HPLC-positive electrospray mass spectrometry (Agilent 1100 MSD; Agilent Technologies, Palo Alto, Calif). The internal standard (7-dimethylamino-5,5-diphenyl-4-octanone, 2.5 ng) was added to plasma (0.5 mL), which was acidied, and then processed by solid phase extraction (Oasis MCX cartridges; Waters Corp, Milford, Mass) according to the manufacturers instructions. Eluents were evaporated to dryness under nitrogen and reconstituted in 50 L of 30% methanol, and 12 L was injected onto the HPLC. Compounds were eluted from a Zorbax Eclipse XDB-C18 column (2.1 50 mm, 5 m, with guard column) (Agilent Technologies) by an isocratic mobile phase of methanol, 55%, in 0.05% triuoroacetic acid (pH 3.6), at 0.25 mL/min and detected by single-ion monitoring (methadone mass to charge ratio [m/z], 310.1; EDDP m/z, 278.1; EMDP m/z, 264.1; and internal standard m/z, 324.1). Standard curves were prepared with the use of blank plasma and were linear over 0.5 to 200 ng/mL for methadone and 0.5 to 10 ng/mL for metabolites. The lower limit of quantication was dened by the lowest calibration sample. Interday coefcients of variation were 12%, 12%, and 9% for 1, 15, and 100 ng/mL methadone and 18% (1 and 5 ng/mL) for EDDP. Plasma concentration data were analyzed by noncompartmental techniques. Methadone clearance, volume of distribution, elimination rate, maximum concentration (Cmax), time to maximum methadone plasma concentration (tmax), and area under the curve (AUC) (linear trapezoidal rule) were calculated by computerized curve tting with WinNonlin Standard 3.0 (Pharsight Corporation, Mountain View, Calif). The following equations were used: Systemic clearance (CL) Dose/AUCiv. Observed oral clearance (CLoral) Dose/ AUCoral. Observed nasal clearance (CLn) Dose/ AUCn. Bioavailability (Fx) (AUCx/Dosey)/(AUCy/ Dosex). Primary and secondary outcome measures The primary outcome measure was bioavailability. The secondary outcome measures were as follows: methadone intravenous, oral, and nasal half-life, clearance, and volume of distribution; AUC of plasma meth-
adone concentration versus time; AUC of plasma methadone metabolite concentrations (EDDP) versus time; pupil diameter; and AUC of pupil diameter versus time. Sample size determination Sample size was not calculated for this exploratory pilot study. Statistics Data are reported as mean and 95% condence interval (CI), mean and standard deviation (SD), or median and range when appropriate. ANOVA or t tests were used for group comparisons when appropriate. Kinetic and dynamic measures were compared by repeated-measures ANOVA. Post hoc testing was performed with the Student-Newman-Keuls method. RESULTS Pharmacokinetics The time course (mean and SD) for the plasma concentrations of methadone are displayed in Figs 1 and 2. The pharmacokinetic data (mean and 95% CI) are shown in Table I. Fig 1 shows the plasma concentration for the whole study period, whereas Fig 2 displays the rst 2 hours (in which it should be observed that the ordinate is linear). Interindividual variation in plasma concentrations after intravenous and nasal administration was considerable for the rst 15 minutes. The tmax values were 0.03 (rst sample), 0.12, and 2.1 hours for intravenous, oral, and nasal methadone, respectively (Table I). The corresponding Cmax values were 135, 43, and 114 ng/mL. Oral tmax and Cmax values were statistically different from the nasal and intravenous values. Mean terminal half-lives of 33 to 37 hours and clearances of 4300 to 6100 mL/h were observed for the 3 sessions (no statistically signicant difference). Oral and nasal absolute bioavailabilities were 0.85 (95% CI, 0.79-0.92) and 0.85 (95% CI, 0.7-1.10), respectively. Plasma concentrations of EDDP, the major metabolite of methadone, showed signicant interindividual variation and were much lower than those of methadone (Fig 3). The tmax value was statistically signicantly shorter after oral administration (2.1 hours) compared with intravenous administration (20.8 hours) (Table II). The mean apparent terminal half-lives observed for EDDP were 39 to 44 hours (no statistically signicant difference). EDDP AUCs and the AUC ratios (AUCEDDP/AUCmethadone) for the different administrations did not differ statistically. No EMDP was
540
Dale et al
CLINICAL PHARMACOLOGY & THERAPEUTICS NOVEMBER 2002
Table I. Pharmacokinetic variables after intravenous, oral, and nasal administration of methadone hydrochloride (10 mg) in 8 human volunteers studied in a crossover fashion
Route Intravenous Oral Nasal tmax (h) 0.03 2.1* (1.5-2.8) 0.12 (0.07-0.177) Cmax (ng/mL) 135 (90-179) 43* (32-54) 114 (76-153) t1/2 (h) 34.0 (26.7-41.3) 33.9 (27.2-40.4) 37.1 (29.1-45.2)
Data are presented as mean and 95% condence interval. tmax, Time to maximum methadone plasma concentration; Cmax, maximum concentration; t1/2, half-life; AUClast, area under the curve from time 0 to last sampling point; AUCinf, area under the curve from time 0 to innity; VZ (obs), observed volume of distribution in the terminal phase; CL (obs), observed clearance. *Statistically signicantly different (P .05) from intravenous and nasal administration.
Table II. Pharmacokinetic variables for 2-ethyl-1,5-dimethyl-3,3-diphenylpyrrolinium (EDDP) after intravenous, oral, and nasal administration of methadone hydrochloride (10 mg) in 8 human volunteers studied in a crossover fashion
Route Intravenous Oral Nasal tmax (h) 20.8 (12.4-28.4) 2.1* (1.3-2.8) 10.8 (3.1-18.4) Cmax (ng/mL) 3.5 (2.1-4.9) 4.5 (2.9-6.1) 3.0 (2.3-3.8) t1/2 (h) 45.3 (31.2-59.0) 39.8 (31.0-48.7) 48.0 (36.2-59.9) AUClast (h ng/mL) 195 (141-251) 198 (113-285) 171 (129-214) Ratio AUClast (EDDP/methadone) 0.13 (0.1-0.16) 0.15 (0.11-0.20) 0.14 (0.11-0.17)
Data are presented as mean and 95% condence interval. *Statistically signicantly different (P .05) from intravenous administration.
detected in any plasma sample above the lower limit of quantication. Pupilometry The time course (mean and SD) of dark-adapted pupil diameter after intravenous, oral, and nasal administration for the rst 24 hours is shown in Fig 4. No statistically signicant difference in the AUCs between the administrations was observed. After intravenous administration, dark-adapted pupil diameters were statistically signicantly different (2-way repeatedmeasures ANOVA, P .01) from the prestudy diameter from 0.033 to 24 hours. The same was true for oral and nasal administration from 2 to 10 hours and from 0.167 to 8 hours, respectively. Minimum pupil diameter occurred at 0.25 hour, 2 hours, and 0.5 hour after intravenous, oral, and nasal administration, respectively. Safety All subjects completed the 3 sessions. No severe adverse events occurred. No subject required supplemental oxygen. All subjects, however, reported stinging and burning in the nose after drug administration. All but one reported that symptoms dissipated within 3 to 5 minutes. One subject complained of pain persisting for almost 1 hour.
DISCUSSION This is the rst study of the pharmacokinetics and pharmacodynamics of nasal methadone. In addition, it is also the rst study reporting plasma concentrations of the methadone metabolites EDDP and EMDP in volunteers. The major ndings are that nasal methadone administration achieves rapid absorption, with a resulting rapid onset of action, closely resembling that of intravenous administration; that oral and nasal methadone bioavailabilities were equal and high; and that the duration of effect of a single 10-mg methadone dose (at least 8-24 hours, on the basis of pupil diameter) is similar to that reported for oral and intravenous methadone in chronic pain and postoperative clinical studies.6,45 However, an unmodied aqueous methadone formulation is associated with too much local irritation for clinical use. Local irritation has been reported with subcutaneously administered methadone and prohibited its use in patients with cancer pain, although this has recently been questioned.28,46 Nasal irritation or unpleasant taste has been reported for other nasal opioids,30 for instance, meperidine (INN, pethidine).37 However, such problems have not been seen with fentanyl.30 The nasal mucosa has features that may allow for very rapid uptake of xenobiotics.29,30 Previous pharmacokinetic studies on nasal administration of opioids
CLINICAL PHARMACOLOGY & THERAPEUTICS VOLUME 72, NUMBER 5
Dale et al
541
AUClast (h ng/mL) 1513 (1219-1807) 1258 (940-1546) 1258 (940-1576)
AUCinf (h ng/mL) 1774 (1340-2208) 1514 (1044-1986) 1499 (1070-1927)
VZ (obs) (mL) 253,406 (212,855-293,957) 304,290 (253,703-354,877) 343,789 (242,108-445,469)
CL (obs) (mL/h) 5400 (4197-6603) 6615 (4731-8500) 6614 (4730-8499)
such as alfentanil, fentanyl, sufentanil, oxycodone, buprenorphine, and butorphanol have shown that mean maximum serum concentrations were achieved between 5 and 49 minutes, although signicant interindividual variation was observed.30-35,47 It should be noted that in several of these studies the sampling was performed too infrequently to accurately determine tmax. Our data, with a mean tmax of 7 minutes, conrm that nasal absorption is ultrarapid for methadone, and as a consequence, rapid onset of effect may be expected. Methadone nasal bioavailability was 0.85, equivalent to oral bioavailability, although a larger interindividual variation was observed, as compared with oral bioavailability. Previous reported mean bioavailabilities for nasal opioids were 0.46 to 0.78. Several factors may reduce apparent nasal bioavailability. First, the nasal cavity generally cannot accommodate volumes greater than 150 to 200 L. Larger nasal volumes may pass directly into the oropharynx, may be swallowed, and therefore may be subject to gut and liver presystemic metabolism. For the majority of the above-mentioned studies, this may explain the rather low bioavailabilities reported. Conversely, in our study, adequate (ie, smaller) volumes were used. Second, the nasal mucosa contains drug-metabolizing enzymes, including CYP3A, which is responsible for methadone metabolism.30,48-50 Thus there is a potential for presystemic methadone metabolism in the nasal mucosa. However, EDDP formation did not differ between the routes of administration; thus we found no evidence for presystemic metabolism of methadone. The validity of this conclusion is limited by a large interindividual variation in a small number of subjects. Although the major focus of this study was nasal administration, we conrm the previously reported methadone oral bioavailability of 0.79 in 5 healthy volunteers.19 In that study individual bioavailability ranged from 0.41 to 0.99, whereas our subjects apparently had less variation (0.74 to 0.95). However, data from 9 cancer patients demonstrated a mean oral bioavailability of 0.79 (range, 0.60-0.95).20 Methadone
clearance, volume of distribution, and terminal half-life did not differ between groups and were similar to previously published data on methadone kinetics.19,20,45,51,52 The methadone dose used in our volunteers is less than what might be used clinically in opioid-tolerant patients with chronic pain; care should be taken if extrapolations are made. Additional studies are required to determine the disposition of larger nasal methadone doses, preferably with a nasal methadone formulation that is less locally irritating. To the best of our knowledge, the time course of methadone metabolite plasma concentrations after single-dose administration has not been previously published. Because we used a sensitive and specic liquid chromatography-mass spectrometry method, we have been able to provide these data. EDDP is not pharmacologically active, and concentration measurements permit determination of presystemic elimination. Presystemic elimination was not a prominent feature in nasal methadone pharmacokinetics in healthy volunteers, consistent with the bioavailability observed. In addition, the observation in patients with cancer that methadone is a low-extraction drug ts our observations.52 Methadone is usually given as a racemic mixture. Studies in patients with chronic pain have demonstrated that the analgesically active R-enantiomer has a significantly longer elimination half-life, a more rapid clearance, and a larger volume of distribution. However, oral lag times and bioavailabilities did not differ.53 In contrast, total clearance and AUC did not differ between the stereoisomers, whereas oral tmax was slower for R-methadone compared with S-methadone in opioid replacement patients receiving methadone.54 This means that our data on racemic bioavailability, our primary outcome measure, probably reect those of the respective enantiomers. However, any pharmacokinetic-pharmacodynamic modeling would require knowledge of active R-enantiomer concentrations rather than racemic concentration and is beyond the scope of this investigation. Thus future studies on
542
Dale et al
CLINICAL PHARMACOLOGY & THERAPEUTICS NOVEMBER 2002
Fig 3. The time course (0-8 hours) of plasma concentrations of the methadone metabolite 2-ethyl-1,5-dimethyl-3,3-diphenylpyrrolinium (EDDP) (mean and SD) in 8 healthy volunteers after IV, oral, and nasal administration of methadone HCl (10 mg). Note the linear scale on the ordinate. Pharmacokinetic calculations are shown in Table II.
Fig 4. The time course (0-24 hours) of resting pupil diameter (mean and SD) in 8 healthy volunteers after intravenous (iv), oral, and nasal administration of methadone HCl (10 mg). For the intravenous administration, resting pupil diameters were statistically signicantly different (2-way repeatedmeasures ANOVA, P .01) from prestudy diameter in the period 0.033 to 24 hours. The same was true for oral administration between 2 and 10 hours and between 0.167 and 8 hours for the nasal study. The time points for the smallest mean pupil diameter rst observed were 0.25 hour, 2 hours, and 0.5 hour for intravenous, oral, and nasal administration, respectively.
CLINICAL PHARMACOLOGY & THERAPEUTICS VOLUME 72, NUMBER 5
Dale et al
543
nasal methadone aiming at establishing a relationship between serum concentrations and clinical effect should include stereoselective analysis. Pupil size was used to assess the effects of methadone. Pupil size is a highly signicant indicator of experimental pain intensity,55 as well the central effects of opioids.42-44 Pupilometry has been extensively validated.40,41,56,57 In this study we utilized dark-adapted resting pupil diameter, rather than dynamic pupil measurements, as used previously.42 Our pupilometry data thus demonstrate that rapid absorption of nasal methadone results in a rapid onset of action (10 minutes, with a maximum effect at about 30 minutes), only slightly slower than for intravenous administration but much faster than for oral administration (2 hours). The intravenous and nasal pupilometry data compare well with clinical data on pain management demonstrating median onset times of 12 to 21 minutes and median times to maximum effect from 26 to 106 minutes.30,36-38,58 In conclusion, we have shown that nasal methadone displays rapid uptake and onset of effect, a long duration of effect, and a high bioavailability similar to that of the oral formulation. No signicant presystemic metabolism was seen. Nasal administration may be an advantageous route of methadone dosing. However, the unmodied aqueous formulation of methadone is not optimal for clinical use because of local irritation.
We thank Mikkel Juul, Dansk Glaskontor, Denmark, for supplying the Pfeiffer BiDose nasal sprayers. We also appreciate the contribution of the staff of the General Clinical Research Center, as well as Sheree Miller and her colleagues at the Hospital Pharmacy.
8.
9.
10.
11.
12.
13.
14.
15.
16.
References
1. Zech DF, Grond S, Lynch J, Hertel D, Lehmann KA. Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study. Pain 1995;63:65-76. 2. Levy MH. Pharmacologic treatment of cancer pain. N Engl J Med 1996;335:1124-32. 3. Portenoy RK, Hagen NA. Breakthrough pain: denition, prevalence and characteristics. Pain 1990;41:273-81. 4. Ripamonti C, Zecca E, Bruera E. An update on the clinical use of methadone for cancer pain. Pain 1997;70: 109-15. 5. Fainsinger R, Schoeller T, Bruera E. Methadone in the management of cancer pain: a review. Pain 1993;52:13747. 6. Ripamonti C, Zecca E, Brunelli C, Rizzio E, Saita L, Lodi F, et al. Rectal methadone in cancer patients with pain. A preliminary clinical and pharmacokinetic study. Ann Oncol 1995;6:841-3. 7. Bruera E, Watanabe S, Fainsinger RL, Spachynski K, Suarez-Almazor M, Inturrisi C. Custom-made capsules 17.
18.
19.
20.
21.
22.
and suppositories of methadone for patients on high-dose opioids for cancer pain. Pain 1995;62:141-6. Thomas Z, Bruera E. Use of methadone in a highly tolerant patient receiving parenteral hydromorphone. J Pain Symptom Manage 1995;10:315-7. Gagnon B, Bruera E. Differences in the ratios of morphine to methadone in patients with neuropathic pain versus non-neuropathic pain. J Pain Symptom Manage 1999;18:120-5. Mercadante S, Casuccio A, Agnello A, Serretta R, Calderone L, Barresi L. Morphine versus methadone in the pain treatment of advanced-cancer patients followed up at home. J Clin Oncol 1998;16:3656-61. Ripamonti C, Groff L, Brunelli C, Polastri D, Stavrakis A, De Conno F. Switching from morphine to oral methadone in treating cancer pain: what is the equianalgesic dose ratio? J Clin Oncol 1998;16:3216-21. Ripamonti C, De Conno F, Groff L, Belzile M, Pereira J, Hanson J, et al. Equianalgesic dose/ratio between methadone and other opioid agonists in cancer pain: comparison of two clinical experiences. Ann Oncol 1998;9:7983. Mercadante S, Casuccio A, Agnello A, Barresi L. Methadone response in advanced cancer patients with pain followed at home. J Pain Symptom Manage 1999;18: 188-92. Gorman AL, Elliott KJ, Inturrisi CE. The d- and l-isomers of methadone bind to the non-competitive site on the N-methyl-D-aspartate (NMDA) receptor in rat forebrain and spinal cord. Neurosci Lett 1997;223:5-8. Davis AM, Inturrisi CE. d-Methadone blocks morphine tolerance and N-methyl-D-aspartate-induced hyperalgesia. J Pharmacol Exp Ther 1999;289:1048-53. Ebert B, Andersen S, Krogsgaard-Larsen P. Ketobemidone, methadone and pethidine are non-competitive N-methyl-D-aspartate (NMDA) antagonists in the rat cortex and spinal cord. Neurosci Lett 1995;187:165-8. Manfredi PL, Borsook D, Chandler SW, Payne R. Intravenous methadone for cancer pain unrelieved by morphine and hydromorphone: clinical observations. Pain 1997;70:99-101. Sawe J. High-dose morphine and methadone in cancer patients. Clinical pharmacokinetic considerations of oral treatment. Clin Pharmacokinet 1986;11:87-106. Meresaar U, Nilsson MI, Holmstrand J, Anggard E. Single dose pharmacokinetics and bioavailability of methadone in man studied with a stable isotope method. Eur J Clin Pharmacol 1981;20:473-8. Gourlay GK, Cherry DA, Cousins MJ. A comparative study of the efcacy and pharmacokinetics of oral methadone and morphine in the treatment of severe pain in patients with cancer. Pain 1986;25:297-312. Leng G, Finnegan MJ. Successful use of methadone in nociceptive cancer pain unresponsive to morphine. Palliat Med 1994;8:153-5. Hunt G, Bruera E. Respiratory depression in a patient
544
Dale et al
CLINICAL PHARMACOLOGY & THERAPEUTICS NOVEMBER 2002
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
receiving oral methadone for cancer pain. J Pain Symptom Manage 1995;10:401-4. Lawlor PG, Turner KS, Hanson J, Bruera ED. Dose ratio between morphine and methadone in patients with cancer pain: a retrospective study. Cancer 1998;82:1167-73. Morley JS, Watt JW, Wells JC, Miles JB, Finnegan MJ, Leng G. Methadone in pain uncontrolled by morphine. Lancet 1993;342:1243. Crews JC, Sweeney NJ, Denson DD. Clinical efcacy of methadone in patients refractory to other mu-opioid receptor agonist analgesics for management of terminal cancer pain. Case presentations and discussion of incomplete cross-tolerance among opioid agonist analgesics. Cancer 1993;72:2266-72. Watanabe S, Belzile M, Kuehn N, Hanson J, Bruera E. Capsules and suppositories of methadone for patients on high-dose opioids for cancer pain: clinical and economic considerations. Cancer Treat Rev 1996;22(Suppl A): 131-6. Coyle N, Adelhardt J, Foley KM, Portenoy RK. Character of terminal illness in the advanced cancer patient: pain and other symptoms during the last four weeks of life. J Pain Symptom Manage 1990;5:83-93. Bruera E, Fainsinger R, Moore M, Thibault R, Spoldi E, Ventafridda V. Local toxicity with subcutaneous methadone. Experience of two centers. Pain 1991;45:141-3. Mygind N. Nasal allergy. In: Structure and ultrastructure of the nose. Oxford (UK): Blackwell Scientic Publications; 1978. p. 3-38. Dale O, Hjortkjr R, Kharasch ED. Nasal administration of opioids for pain management in adults. Acta Anaesthesiol Scand 2002;46:759-70. Schwagmeier R, Boerger N, Meissner W, Striebel HW. Pharmacokinetics of intranasal alfentanil. J Clin Anesth 1995;7:109-13. Striebel HW, Kramer J, Luhmann I, Rohierse-Hohler I, Rieger A. Pharmakokinetische Studie zur intranasalen Gabe von Fentanyl. Der Schmerz 1993;7:122-5. Takala A, Kaasalainen V, Seppala T, Kalso E, Olkkola KT. Pharmacokinetic comparison of intravenous and intranasal administration of oxycodone. Acta Anaesthesiol Scand 1997;41:309-12. Eriksen J, Jensen NH, Kamp-Jensen M, Bjarno H, Friis P, Brewster D. The systemic availability of buprenorphine administered by nasal spray. J Pharm Pharmacol 1989;41:803-5. Shyu WC, Mayol RF, Pfeffer M, Pittman KA, Gammans RE, Barbhaiya RH. Biopharmaceutical evaluation of transnasal, sublingual, and buccal disk dosage forms of butorphanol. Biopharm Drug Dispos 1993;14:371-9. Striebel HW, Pommerening J, Rieger A. Intranasal fentanyl titration for postoperative pain management in an unselected population. Anaesthesia 1993;48:753-7. Striebel WH, Malewicz J, Hermanns K, Castello R. Intranasal meperidine titration for postoperative pain relief. Anesth Analg 1993;76:1047-51.
38. Schwesinger WH, Reynolds JC, Harshaw DH, Frakes LA. Transnasal butorphanol and intramuscular meperidine in the treatment of postoperative pain. Adv Ther 1992;9:123-9. 39. Zeppetella G. An assessment of the safety, efcacy, and acceptability of intranasal fentanyl citrate in the management of cancer-related breakthrough pain: a pilot study. J Pain Symptom Manage 2000;20:253-8. 40. Weinhold LL, Bigelow GE. Opioid miosis: effects of lighting intensity and monocular and binocular exposure. Drug Alcohol Depend 1993;31:177-81. 41. Radzius A, Welch P, Cone EJ, Henningfeld JE. A portable pupilometer system for measuring pupillary size and light reex. Behav Res Methods Instrum Comput 1989;21:611-8. 42. Phimmasone S, Kharasch ED. A pilot evaluation of alfentanil-induced miosis as a noninvasive probe for hepatic cytochrome P450 3A4 (CYP3A4) activity in humans. Clin Pharmacol Ther 2001;70:505-17. 43. Lotsch J, Skarke C, Schmidt H, Grosch S, Geisslinger G. The transfer half-life of morphine-6-glucuronide from plasma to effect site assessed by pupil size measurement in healthy volunteers. Anesthesiology 2001; 95:1329-38. 44. Dershwitz M, Walsh JL, Morishige RJ, Connors PM, Rubsamen RM, Shafer SL, et al. Pharmacokinetics and pharmacodynamics of inhaled versus intravenous morphine in healthy volunteers. Anesthesiology 2000;93: 619-28. 45. Gourlay GK, Wilson PR, Glynn CJ. Pharmacodynamics and pharmacokinetics of methadone during the perioperative period. Anesthesiology 1982;57:458-67. 46. Mathew P, Storey P. Subcutaneous methadone in terminally ill patients: manageable local toxicity. J Pain Symptom Manage 1999;18:49-52. 47. Helmers JH, Noorduin H, Van Peer A, Van Leeuwen L, Zuurmond WW. Comparison of intravenous and intranasal sufentanil absorption and sedation. Can J Anaesth 1989;36:494-7. 48. Gervasi PG, Longo V, Naldi F, Panattoni G, Ursino F. Xenobiotic-metabolizing enzymes in human respiratory nasal mucosa. Biochem Pharmacol 1991;41:177-84. 49. Longo V, Pacici GM, Panattoni G, Ursino F, Gervasi PG. Metabolism of diethylnitrosamine by microsomes of human respiratory nasal mucosa and liver. Biochem Pharmacol 1989;38:1867-9. 50. Yokose T, Doy M, Taniguchi T, Shimada T, Kakiki M, Horie T, et al. Immunohistochemical study of cytochrome P450 2C and 3A in human non-neoplastic and neoplastic tissues. Virchows Arch 1999;434:401-11. 51. Nilsson MI, Meresaar U, Anggard E. Clinical pharmacokinetics of methadone. Acta Anaesthesiol Scand Suppl 1982;74:66-9. 52. Inturrisi CE, Colburn WA, Kaiko RF, Houde RW, Foley KM. Pharmacokinetics and pharmacodynamics of meth-
CLINICAL PHARMACOLOGY & THERAPEUTICS VOLUME 72, NUMBER 5
Dale et al
545
adone in patients with chronic pain. Clin Pharmacol Ther 1987;41:392-401. 53. Kristensen K, Blemmer T, Angelo HR, Christrup LL, Drenck NE, Rasmussen SN, et al. Stereoselective pharmacokinetics of methadone in chronic pain patients. Ther Drug Monit 1996;18:221-7. 54. Foster DJ, Somogyi AA, Dyer KR, White JM, Bochner F. Steady-state pharmacokinetics of (R)- and (S)methadone in methadone maintenance patients. Br J Clin Pharmacol 2000;50:427-40. 55. Ellermeier W, Westphal W. Gender differences in pain ratings and pupil reactions to painful pressure stimuli. Pain 1995;61:435-9.
56. Belani KG, Sessler DI, Larson MD, Lopez MA, Washington DE, Ozaki M, et al. The pupillary light reex. Effects of anesthetics and hyperthermia. Anesthesiology 1993;79:23-7. 57. Fosnaugh JS, Bunker EB, Pickworth WB. Daily variation and effects of ambient light and circadian factors on the human light reex. Methods Find Exp Clin Pharmacol 1992;14:545-53. 58. Toussaint S, Maidl J, Schwagmeier R, Striebel HW. Patient-controlled intranasal analgesia: effective alternative to intravenous PCA for postoperative pain relief. Can J Anaesth 2000;47:299-302.
You might also like
- Statistical Analysis PlanDocument92 pagesStatistical Analysis PlanhimeshagrawalNo ratings yet
- London Medicines Evaluation Network Reviews Pharmacokinetic Profiles of Extended-Release MethylphenidateDocument9 pagesLondon Medicines Evaluation Network Reviews Pharmacokinetic Profiles of Extended-Release Methylphenidateassajadda lizikriNo ratings yet
- Catalyst RX Formulary IntroductionDocument4 pagesCatalyst RX Formulary IntroductionRahul MishraNo ratings yet
- AL y Signos VitalesDocument7 pagesAL y Signos VitalesPedro Jose Rios GNo ratings yet
- Guía de Dosis de AntipsicóticosDocument8 pagesGuía de Dosis de AntipsicóticoskarlunchoNo ratings yet
- Medoral 21 E579Document8 pagesMedoral 21 E579AngiPaolaPuiconRuizNo ratings yet
- Anesth Analg-2012-Corcoran-640-51 PDFDocument12 pagesAnesth Analg-2012-Corcoran-640-51 PDFBijay KCNo ratings yet
- Open Label Clinical Study To Evaluate The Safety and Tolerability of TreprostinilDocument14 pagesOpen Label Clinical Study To Evaluate The Safety and Tolerability of TreprostinilMaria Jose Contreras SilvaNo ratings yet
- DTH 14650Document19 pagesDTH 14650Evelyn LimNo ratings yet
- Premedication With Oral Tramadol Reduces Severity of Postoperative Shivering After General AnesthesiaDocument6 pagesPremedication With Oral Tramadol Reduces Severity of Postoperative Shivering After General AnesthesiaFajar NarakusumaNo ratings yet
- JeradDocument10 pagesJeradzaimmuhtarNo ratings yet
- FentanylDocument12 pagesFentanylUtomo FemtomNo ratings yet
- 0300060513485864Document11 pages0300060513485864Aashish KalikaNo ratings yet
- Medication Use During End-Of-Life Care in A Palliative Care CentreDocument9 pagesMedication Use During End-Of-Life Care in A Palliative Care CentreCaio CandidoNo ratings yet
- Medication Assisted Treatment of Opioid Use.2Document13 pagesMedication Assisted Treatment of Opioid Use.2tatanmenaNo ratings yet
- The Effectsof Diaphragmatic Breathingand Omeprazoleon Respiratory Indicesand Diaphragmatic Excursionin Patientswith Gastroesophageal Reflux DiseaseDocument6 pagesThe Effectsof Diaphragmatic Breathingand Omeprazoleon Respiratory Indicesand Diaphragmatic Excursionin Patientswith Gastroesophageal Reflux DiseaseSHAFANA PUTRI -No ratings yet
- Dexketoprofen/tramadol: Randomised Double-Blind Trial and Confirmation of Empirical Theory of Combination Analgesics in Acute PainDocument13 pagesDexketoprofen/tramadol: Randomised Double-Blind Trial and Confirmation of Empirical Theory of Combination Analgesics in Acute PainskripsianiNo ratings yet
- Research: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysisDocument7 pagesResearch: Corticosteroids For Pain Relief in Sore Throat: Systematic Review and Meta-AnalysiswindaintanpNo ratings yet
- Respiratory ResearchDocument32 pagesRespiratory ResearchNuno DuarteNo ratings yet
- Lack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled TrialDocument12 pagesLack of Efficacy of Long-Term, Low-Dose Azithromycin in Chronic Rhinosinusitis: A Randomized Controlled Trialpaijo09No ratings yet
- Disertasi BiofarmasiDocument167 pagesDisertasi BiofarmasiJerry Skate RasBebasNo ratings yet
- Theobromine Inhibits CoughDocument16 pagesTheobromine Inhibits CoughRaffaello MobiliaNo ratings yet
- Adalimumab added to methotrexate increases remission in early rheumatoid arthritisDocument10 pagesAdalimumab added to methotrexate increases remission in early rheumatoid arthritisElenaChiriacovaNo ratings yet
- 2019 A&a Dez MetadonaDocument3 pages2019 A&a Dez MetadonajaquelinemiyakeNo ratings yet
- A comparison of midazolam and diazepam for dental sedationDocument5 pagesA comparison of midazolam and diazepam for dental sedationGu GuuNo ratings yet
- Ncologist: R I FDADocument7 pagesNcologist: R I FDAapi-26302710No ratings yet
- Ijohns 2015031219070250Document9 pagesIjohns 2015031219070250listyaNo ratings yet
- AminoglicozideDocument7 pagesAminoglicozideDiana Mihaela BadescuNo ratings yet
- Cerminara Et Al 2017 A Single Center Retrospective Analysis of A Protocol For High Dose Methotrexate and LeucovorinDocument9 pagesCerminara Et Al 2017 A Single Center Retrospective Analysis of A Protocol For High Dose Methotrexate and Leucovorinanton.neonatusNo ratings yet
- PIIS2213260017304745Document10 pagesPIIS2213260017304745Juan Pablo CasanovaNo ratings yet
- Journal - Medication Dry Mounth 2018 - Tan EdwinDocument9 pagesJournal - Medication Dry Mounth 2018 - Tan EdwinranisaNo ratings yet
- Drug Delivery Systems - An Update ReviewDocument10 pagesDrug Delivery Systems - An Update ReviewenzomontresolNo ratings yet
- Comparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsDocument5 pagesComparative in Vitro Dissolution and in Vivo Bioequivalence of Two Diclofenac Enteric Coated FormulationsgeoaislaNo ratings yet
- Ropvacaina VS Lidocaina Premdicacion IotDocument6 pagesRopvacaina VS Lidocaina Premdicacion IotFaith Lu PenalozaNo ratings yet
- Background: Pharmacotherapy For Hypertension in Women of Different RacesDocument6 pagesBackground: Pharmacotherapy For Hypertension in Women of Different RacesRisma S PNo ratings yet
- Menyhei 1994Document4 pagesMenyhei 1994Anett Pappné LeppNo ratings yet
- Hope 4 Lancet 2019Document12 pagesHope 4 Lancet 2019Marco Cordova RosellNo ratings yet
- Timing is important in medication administration; a timely review of chronotherapy researchDocument15 pagesTiming is important in medication administration; a timely review of chronotherapy researchCarlos RomeroNo ratings yet
- The Role of Dexmedetomidine (Precedex) in The Sedation of Critically Ill PatientsDocument4 pagesThe Role of Dexmedetomidine (Precedex) in The Sedation of Critically Ill Patientspshz05No ratings yet
- 223 2012 Article 9639Document10 pages223 2012 Article 9639Daniela CerianiNo ratings yet
- Introduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlDocument6 pagesIntroduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlnadaNo ratings yet
- Methamphetamine and Amphetamine Pharmacokinetics in Oral Fluid and Plasma After Controlled Oral Methamphetamine Administration To Human VolunteersDocument12 pagesMethamphetamine and Amphetamine Pharmacokinetics in Oral Fluid and Plasma After Controlled Oral Methamphetamine Administration To Human VolunteersemmypuspitasariNo ratings yet
- Medoral 20 E459Document5 pagesMedoral 20 E459Tania RodriguezNo ratings yet
- Receptor Antagonist, Asthma, Seratrodast, Montelukast, Peak Expiratory Flow (PEF), Eosinophil Cationic Protein (ECP), AlbuminDocument10 pagesReceptor Antagonist, Asthma, Seratrodast, Montelukast, Peak Expiratory Flow (PEF), Eosinophil Cationic Protein (ECP), AlbuminZuventusHealthcareNo ratings yet
- MeduriDocument4 pagesMeduriSilvia Leticia BrunoNo ratings yet
- AnestesiDocument17 pagesAnestesibodroNo ratings yet
- Systematic Review and Network Meta-Analysis of Stroke Prevention Treatments in Patients With Atrial FibrillationDocument15 pagesSystematic Review and Network Meta-Analysis of Stroke Prevention Treatments in Patients With Atrial FibrillationAlicePastranaNo ratings yet
- A Double-Blind Randomized Controlled Trial of Normal Saline, Lactated Ringer's, and Hypertonic Saline Nasal Irrigation Solution After Endoscopic Sinus SurgeryDocument7 pagesA Double-Blind Randomized Controlled Trial of Normal Saline, Lactated Ringer's, and Hypertonic Saline Nasal Irrigation Solution After Endoscopic Sinus SurgeryYasdika ImamNo ratings yet
- Evaluation of The Buccal Vestibule-Palatal Diffusion of 4% Articaine Hydrochloride in Impacted Maxillary Third Molar ExtractionsDocument4 pagesEvaluation of The Buccal Vestibule-Palatal Diffusion of 4% Articaine Hydrochloride in Impacted Maxillary Third Molar ExtractionsDRPRIYA007No ratings yet
- Three Anxiety Protocols Compared for Tooth ExtractionDocument8 pagesThree Anxiety Protocols Compared for Tooth ExtractionDiego LemurNo ratings yet
- Pharmacokinetics of Oral and Intravenous Paracetamol (Acetaminophen) When Co-Administered With Intravenous Morphine in Healthy Adult SubjectsDocument10 pagesPharmacokinetics of Oral and Intravenous Paracetamol (Acetaminophen) When Co-Administered With Intravenous Morphine in Healthy Adult SubjectsRara MaharrumNo ratings yet
- The Effect of Delmopinol Mouthwash On Aphthous StomatitisDocument19 pagesThe Effect of Delmopinol Mouthwash On Aphthous StomatitisAthenaeum Scientific PublishersNo ratings yet
- A Career in The Pharmaceutical SciencesDocument19 pagesA Career in The Pharmaceutical SciencesDrSandeep NarulaNo ratings yet
- Mephedrone Pharmacokinetics After Intravenous and Oral Administration in Rats: Relation To PharmacodynamicsDocument23 pagesMephedrone Pharmacokinetics After Intravenous and Oral Administration in Rats: Relation To PharmacodynamicsReal GuruNo ratings yet
- Remifentanil Compared With Midazolam and Pethidine Sedation During Colonoscopy: A Prospective, Randomized StudyDocument7 pagesRemifentanil Compared With Midazolam and Pethidine Sedation During Colonoscopy: A Prospective, Randomized Studyade_liaNo ratings yet
- Jced 7 E84Document5 pagesJced 7 E84Karina HernandezNo ratings yet
- M34 16Document2 pagesM34 16Ana Tomas PetrovicNo ratings yet
- Ismail 2013Document6 pagesIsmail 2013Nawang WulanNo ratings yet
- Antiepileptic Drugs-Best Practice Guidelines ForDocument38 pagesAntiepileptic Drugs-Best Practice Guidelines ForAbraham Escobedo MoratillaNo ratings yet
- A Model Informed Method For The Purpose of Precision Dosing of Isoniazid in Pulmonary TuberculosisDocument11 pagesA Model Informed Method For The Purpose of Precision Dosing of Isoniazid in Pulmonary TuberculosisNitish TankNo ratings yet
- Parakh 2017Document5 pagesParakh 2017Muhammad Ali Syahrun MubarokNo ratings yet
- Trenaxamic AcidDocument9 pagesTrenaxamic AciddesyhavizhahNo ratings yet
- Pro DrugsDocument46 pagesPro DrugsAditya KotamrajuNo ratings yet
- Research Triangle Regions Life Sciences Directory 2012Document50 pagesResearch Triangle Regions Life Sciences Directory 2012hitexNo ratings yet
- Indian Pharmacopoeia Download PDFDocument3 pagesIndian Pharmacopoeia Download PDFManuel Alberto Castillo Aguirre25% (4)
- Drug effects and clinical trials overviewDocument1 pageDrug effects and clinical trials overviewKlare TyNo ratings yet
- Farmakokinetika 1Document19 pagesFarmakokinetika 1Sari Ranial ZhaptaNo ratings yet
- Pyy 071Document16 pagesPyy 071Stella SulartoNo ratings yet
- of M.pharmDocument13 pagesof M.pharmVivek Patel ViksNo ratings yet
- The Production of MedicinesDocument9 pagesThe Production of MedicinesAngelNo ratings yet
- Course Curriculum EwuDocument4 pagesCourse Curriculum EwudearshuvroNo ratings yet
- Butilbromuro de Hioscina Una Revisión de Su Uso en El Tratamiento de Cólicos y Dolor AbdominalDocument6 pagesButilbromuro de Hioscina Una Revisión de Su Uso en El Tratamiento de Cólicos y Dolor AbdominalalexqaNo ratings yet
- Storage and Transportation of Investigational Drug ProductsDocument4 pagesStorage and Transportation of Investigational Drug ProductsDilawar BakhtNo ratings yet
- Drugs and The BodyDocument5 pagesDrugs and The BodyValones BeaNo ratings yet
- FDA Draft Guidance on Bioequivalence Studies for Dienogest; Estradiol ValerateDocument2 pagesFDA Draft Guidance on Bioequivalence Studies for Dienogest; Estradiol ValerateAna BelgaNo ratings yet
- Pharmacokinetic ParametersDocument29 pagesPharmacokinetic Parametersfaisalnadeem100% (1)
- Week4 PTC Formulary DispensingDocument7 pagesWeek4 PTC Formulary DispensingChunnie JakosalemNo ratings yet
- Rebamipide, A Gastro-Protective and Anti-Inflammatory Drug, Promotes Gastric Ulcer Healing Following Eradication TherapyDocument4 pagesRebamipide, A Gastro-Protective and Anti-Inflammatory Drug, Promotes Gastric Ulcer Healing Following Eradication TherapySilvester HenryNo ratings yet
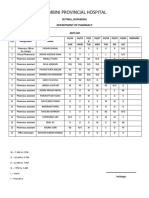
- Lumbini Provincial Hospital: Department of PharmacyDocument2 pagesLumbini Provincial Hospital: Department of PharmacyImdadHussainOPositiveNo ratings yet
- p1 PDFDocument79 pagesp1 PDFJames PerianayagamNo ratings yet
- Nearest Pharmacy Delivery ServiceDocument5 pagesNearest Pharmacy Delivery ServiceJayanath SamarasingheNo ratings yet
- UntitledDocument12 pagesUntitledjhony192No ratings yet
- Cpdprogram Pharmacy 82318Document81 pagesCpdprogram Pharmacy 82318PRC BoardNo ratings yet
- TDM UtsDocument285 pagesTDM Utsnabila auliaNo ratings yet
- PRELIMSDocument21 pagesPRELIMSPrincess NicoleNo ratings yet
- Rancangan Dan Pengembangan FormulaDocument60 pagesRancangan Dan Pengembangan FormulaI M BrotoNo ratings yet
- Pharmaceutical absorption and bioavailabilityDocument18 pagesPharmaceutical absorption and bioavailabilityFredNo ratings yet
- PHARMECUETICALDocument3 pagesPHARMECUETICALgaming loverNo ratings yet
- ADMINISTRATIVE ORDER No. 144 S. 2004Document2 pagesADMINISTRATIVE ORDER No. 144 S. 2004Mae GandaNo ratings yet