Professional Documents
Culture Documents
Review of Respiratory Physiology
Uploaded by
lovelyc95Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Review of Respiratory Physiology
Uploaded by
lovelyc95Copyright:
Available Formats
Review of Respiratory
Physiology
Steady State
Lung O
2
Uptake rate
= Cell O
2
Utilization rate
Cell CO
2
Production rate
= Lung CO
2
Release rate
Gaseous Environment.
Atmosphere: Nitrogen and Oxygen,
negligible Carbon Dioxide.
Clinical Relevance of Environment
Altitude: PO
2
depends on P
B
Suffocation: PO
2
depends on fractional O
2
Oxygen therapy: PO
2
depends on fractional O
2
P F P
I I B
O O
2 2
47 = - ( )
Diffusion and Diffusion
Abnormality
Ficks Law for Diffusion for Gases
O
2
CO
2
T
P
1
P
2
A
( ) V
A D
T
P P
gas
=
1 2
Single Breath D
L
CO
Single inspiration of a dilute CO
mixture
10 second breath-hold
Measure CO uptake using infrared
detector to compare inspiratory and
expiratory concentrations
Normal Value: 25 ml/min/mmHg
Clinical Interpretation of D
L
CO.
Decreases with loss of surface area.
Decreases with increasing membrane
thickness
Decreases with ventilation/perfusion
mismatching
Summary: D
L
CO better index of overall
lung function than diffusion capabilities
per se.
Two Factors Affect Gas Transfer
Rate
Diffusion rate of a gas
Perfusion Rate (Pulmonary blood
flow)
Gases must be carried away to maintain
local diffusion gradients in the lung.
O
2
Diffusion during Normoxia
Lung Mechanics in Obstructive
and Restrictive Disease
Measuring vital capacity and its
subcomponents.
Use a spirometer.
TLC
RV
VC
TV
FRC
IC
IRV
ERV
RV
Can Use
Spiromenter
Cant Use a Spirometer
Measuring Residual Volume
Cant use a Spirometer
Use instead:
Nitrogen Washout
Helium Dilution Method
Plethysmograph
Obstructive Disease
Difficult to get air out of the lungs
Obstruct expiration
Examples:
emphysema
chronic bronchitis
asthma.
Restrictive Disease
Difficult to get air in to the lungs
Restrict inspiration
Examples:
intersitial fibrosis
sarcoidosis
muscular diseases
chestwall deformities.
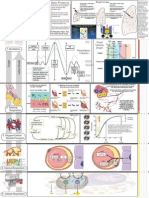
Lung Capacity and Disease
Summary
Obstructive Disease:
Decreased VC
Increased TLC, RV, FRC.
Restrictive Disease:
Decreased VC
Decreased TLC, RV, FRC.
Fig 5: Lung Capacity and
Disease
Normal
RV
ERV
TV
IRV
FRC
VC
Restrictive
RV
ERV
TV
IRV
FRC
VC
Obstructive
RV
ERV
TV
IRV
FRC
VC
125
100
75
50
25
0
%
N
o
r
m
a
l
T
L
C
Forced Vital Capacity
FEV
1.0
/ FVC Ratio
Small Airways Disease
FEF
25-75
Flow -Volume Curves
Peak Flow
Pulmonary Function Summary
Obstructive
Disease
Restrictive
Disease
FEV
1.0
Decreased Decreased
FVC Decreased Decreased
FEV
1.0
/FVC Decreased Unchanged or
Increased
Peak Flow Decreased Decreased or
Unchanged
RV/TLC Increased Unchanged
CLINICAL USE OF IDEAL
ALVEOLAR GAS VALUES
Ideal Alveolar Gas Equation.
P P
P
R
P F
R
R
A I
A
A I
O O
CO
CO O
2 2
2
2 2
1
= +
|
\
|
.
|
Clinically Useful Form:
Complete Form:
P P
P
R
A I
A
O O
CO
2 2
2
=
USE #1
Compare P
A
O
2
to P
a
O
2
Healthy people: P
A
O
2
= P
a
O
2
Two Approaches to Comparison
(P
A
O
2
- P
a
O
2
) difference
P
a
O
2
/ P
A
O
2
ratio
A-a Difference
P
A
O
2
- P
a
O
2
Normally 5-20 mmHg
Because of normal anatomical shunt
Ventilation/Perfusion mismatching.
A-a difference increases with
pulmonary disease.
Problem: Normal range changes on
100% O
2
.
a/A ratio
Normally averages just over 0.8 (Am.
Rev. Resp. Dis. 109: 142-145, 1974).
a/A ratio falls with pulmonary
disease.
Lower limit normal:
young (room air) : 0.74
older (room air) : 0.78
Both groups (100% O
2
): 0.82
(A-a) Difference vs. a/A Ratio
Normal
Normal
(
A
-
a
)
P
O
2
D
i
f
f
e
r
e
n
c
e
(
m
m
H
g
)
a
/
A
P
O
2
r
a
t
i
o
Sick
Sick
Use #2
P
A
O
2
Estimates P
c
O
2
Useful for calculation of Venous
Admixture or Shunt
Venous Admixture
'
'
Q
Q
C C
C C
S
T
c a
c v
O O
O O
=
2 2
2 2
Q
T
C
a
O
2
(Q
T
- Q
s
) C
c
O
2
Q
s
C
v
O
2
P
A
O
2
Diagnosis of True Shunt
Breathing 100% oxygen -
will not abolish hypoxemia due to
shunt
REASON: shunted blood never
exposed to the high alveolar PO
2
.
Blood Gases
Oxygen Blood Gas Quantities
Partial Pressure
Saturation
Content
Carrying Capacity: O
2
content at
100% saturation.
Significance of Sigmoid Curve
4 Point Curve
Critical PO
2
V
Defining Content and Capacity
C Hb
S
O
O
2
2
136
100%
= - - . [ ]
%
Blood
Hemoglobin --> Allows Blood to hold
more oxygen.
P
50
: Reciprical to Hb-O
2
Affinity
(H
+
, CO
2
, Temp, & 2,3-DPG)
Capacity: Anemia, Polycythemia
Hematocrit
Hemoglobin
Hemoglobin variants exist (e.g. Hb
f
)
Four (+one) Things Change
Oxyhemoglobin Affinity
Hydrogen Ion Concentration, [H
+
]
Carbon Dioxide Partial Pressure, PCO
2
Temperature
[2,3-DPG]
Special Case: Carbon Monoxide
Three Things That Change O
2
Carrying Capacity
Changes in Hb Concentration
Presence of Carbon Monoxide
Formation of Methemoglobin
Minute Ventilation
Flow (vol/time) moved into or out of
the lungs.
Measured by collecting expired
volume for a fixed time.
Normal value is 7.5 L/min (BTPS).
V V f
E T
=
Partitioning Minute Ventilation.
Alveolar Ventilation: the volume per
min entering gas exchange surfaces.
Dead space Ventilation: the volume
per min that is wasted
( ) V V V V V f V f V f
A E d T d T d
= = =
Alveolar Ventilation Equation.
(Rearranged)
P
V (STPD)
863 mmHg
A
CO
CO
2
2
=
( ) V BTPS
A
Defining Adequate Ventilation
Normal--> P
a
CO
2
= 40 mmHg
Hypoventilation --> High P
a
CO
2
Hyperventilation --> Low P
a
CO
2
Respiratory Acid-Base
Henderson-Hasselbach Equation:
Changes in PCO
2
cause changes in [H
+
] by
mass action.
Increased PCO
2
resp. acidosis
Decreased PCO
2
resp. alkalosis.
CO H O H CO H HCO
2 2 2 3 3
+ +
+ Carbonic Anhydrase
pH
HCO
P
CO
= +
6 1
0 03
3
2
. log
[ ]
( . )
CAUSES OF HYPOXEMIA
Low F
I
O
2
Hypoventilation
True shunt
Diffusion Abnormality
Ventilation / Perfusion Mismatching
Hypoxemia Analysis
Step 1
Is P
A
CO
2
> 40 mmHg
AND
a/A > 0.74 or (A-a) < 20 mmHg
Pure
Hypoventilation
yes
Choose between:
Shunt
Diffusion Abnormality
V/Q Mismatching
No
Continue
Hypoxemia Analysis
Step 2
Can
Hypoxemia be eliminated
by 100% O
2
True
Shunt
No
Choose between:
Diffusion Abnormality
V/Q Mismatching
Yes
Continue
Hypoxemia Analysis
Step 3
Is the D
L
CO
Normal
?
Diffusion Normal
must be
V/Q Mismatching
yes
No
Cant choose between:
Diffusion Abnormality
V/Q Mismatching
or Combination
Questions?
You might also like
- How It Works - Human BodyDocument180 pagesHow It Works - Human BodyMargo Sun94% (36)
- 8.aviation, Space and Deep Sea Diving PhysiologyDocument5 pages8.aviation, Space and Deep Sea Diving PhysiologyCLEMENTNo ratings yet
- Mechanical VentilationDocument16 pagesMechanical VentilationArt Christian Ramos88% (8)
- Arterial Blood GasDocument255 pagesArterial Blood GasMark Joshua S CruzNo ratings yet
- Ruppels Manual of Pulmonary Function Testing 10th Edition Mottram Test BankDocument13 pagesRuppels Manual of Pulmonary Function Testing 10th Edition Mottram Test Bankkhuyentryphenakj1100% (30)
- Anatomy Midterm Study GuideDocument53 pagesAnatomy Midterm Study Guidelovelyc95No ratings yet
- Lung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyFrom EverandLung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyNo ratings yet
- Anatomy of The Intercostal SpaceDocument17 pagesAnatomy of The Intercostal Spacelovelyc95No ratings yet
- Anatomy of The Intercostal SpaceDocument17 pagesAnatomy of The Intercostal Spacelovelyc95No ratings yet
- Occupational Therapy - Play, SIs and BMTsDocument3 pagesOccupational Therapy - Play, SIs and BMTsAnnbe Barte100% (1)
- Arterial Blood Gas InterpretationDocument65 pagesArterial Blood Gas InterpretationDaniel AryanNo ratings yet
- Time The Secret KillerDocument7 pagesTime The Secret KillerFarhan Rehman100% (1)
- Chapter 1 NS Objective QuestionsDocument8 pagesChapter 1 NS Objective QuestionsSadasivarao GaddeNo ratings yet
- Msds Buffer AsetatDocument6 pagesMsds Buffer AsetatAnnisa SeptianiNo ratings yet
- Antigen & AntibodiesDocument16 pagesAntigen & AntibodiesYing Ming TangNo ratings yet
- Arterial Blood Gas - ppt1Document53 pagesArterial Blood Gas - ppt1Madhuri100% (1)
- Syllabus NCM 103Document11 pagesSyllabus NCM 103ivanguzman86No ratings yet
- Abg 3Document43 pagesAbg 3Montasir AhmedNo ratings yet
- Metabolic Rate and Alveolar VentilationDocument9 pagesMetabolic Rate and Alveolar VentilationSimran SukhijaNo ratings yet
- Biomechanical Comparison of Axial and Tilted Implants For Mandibular Full-Arch Fixed ProsthesesDocument9 pagesBiomechanical Comparison of Axial and Tilted Implants For Mandibular Full-Arch Fixed ProsthesesTeresa BeltranNo ratings yet
- Blood Gas AnalysisDocument52 pagesBlood Gas AnalysisKresna Dharma SuryanaNo ratings yet
- Disorders of Gas Exchange: Hypercapnia and HypoxiaDocument26 pagesDisorders of Gas Exchange: Hypercapnia and HypoxiaBelehuz Cristina OanaNo ratings yet
- Acidosis Alkalosis BiochemistryDocument31 pagesAcidosis Alkalosis BiochemistryliyaNo ratings yet
- Abnormal Ventilation, Abnormal Gas ExchangeDocument52 pagesAbnormal Ventilation, Abnormal Gas ExchangekateNo ratings yet
- ABGDocument16 pagesABGKesavanVeeraNo ratings yet
- ABG InterpretationDocument38 pagesABG Interpretationmahmod omerNo ratings yet
- Rs4-Gas Exchange and TransportDocument5 pagesRs4-Gas Exchange and TransportGabriella ChafrinaNo ratings yet
- V/Q and Oxygen: Anuja Abayadeera Part 1B AnaesthsiologyDocument42 pagesV/Q and Oxygen: Anuja Abayadeera Part 1B Anaesthsiologyv_vijayakanth7656No ratings yet
- Arterial Blood Gas: Interpretation and Clinical ImplicationsDocument112 pagesArterial Blood Gas: Interpretation and Clinical ImplicationsmatrixtrinityNo ratings yet
- Interpretation of Arterial Blood Gases and Acid-Base DisordersDocument44 pagesInterpretation of Arterial Blood Gases and Acid-Base DisordersSuren VishvanathNo ratings yet
- Acute Respiratory Failure Learning Guide: Phone: Email: Campus AddressDocument8 pagesAcute Respiratory Failure Learning Guide: Phone: Email: Campus Addressiancooke09No ratings yet
- Blood Gas Analysis: Respiratory DisordersDocument15 pagesBlood Gas Analysis: Respiratory DisordersYogeshRavalNo ratings yet
- Arterial Blood Gas InterpretationDocument66 pagesArterial Blood Gas InterpretationlenafitriyaniNo ratings yet
- AbgDocument66 pagesAbgIan OrwaNo ratings yet
- FormulasDocument2 pagesFormulasJen NeeNo ratings yet
- Acid-Base Balance & Blood GasesDocument39 pagesAcid-Base Balance & Blood GasesSulaiman TahsinNo ratings yet
- Common Causes of HypoxemiaDocument6 pagesCommon Causes of HypoxemiaSamantha LuiNo ratings yet
- Ventilation and PerfusionDocument2 pagesVentilation and PerfusionJayricDepalobosNo ratings yet
- Abg AnalysisDocument65 pagesAbg AnalysisSyed Farooque AliNo ratings yet
- Acidosis Alkalosis BiochemistryDocument28 pagesAcidosis Alkalosis BiochemistryDocSam048No ratings yet
- Respiratory Physiology: Dr. Okon MRCSDocument41 pagesRespiratory Physiology: Dr. Okon MRCSEdwin OkonNo ratings yet
- Arterial Blood Gas InterpretationDocument66 pagesArterial Blood Gas InterpretationkabatchinoooNo ratings yet
- Respiratory Acid-Base DisordersDocument13 pagesRespiratory Acid-Base DisordersAlfredo PreciadoNo ratings yet
- Interpret The Abgs in A Stepwise Manner:: Reference ReferenceDocument6 pagesInterpret The Abgs in A Stepwise Manner:: Reference ReferenceYogeshRavalNo ratings yet
- ABGDocument45 pagesABGHasan SudirgoNo ratings yet
- Basics in Arterial Blood Gas InterpretationDocument41 pagesBasics in Arterial Blood Gas InterpretationyasinNo ratings yet
- EOVSABDocument28 pagesEOVSABRobert KerwickNo ratings yet
- Respiratory ICU PDFDocument130 pagesRespiratory ICU PDFAhmed Shihab AhmedNo ratings yet
- Acid-Base - FDocument14 pagesAcid-Base - Fotiang deniceNo ratings yet
- Transpulmonary Pressure Ppul - Pip: Decreased Volume Increased Pressure Increased Volume Decreased PressureDocument1 pageTranspulmonary Pressure Ppul - Pip: Decreased Volume Increased Pressure Increased Volume Decreased Pressurelovelyc95No ratings yet
- Translateturn Off Instant TranslationDocument38 pagesTranslateturn Off Instant TranslationListaNo ratings yet
- Anesthesia PointsDocument5 pagesAnesthesia PointsRedNo ratings yet
- AbgDocument30 pagesAbgSyan HamzahNo ratings yet
- Blood Gas & Electrolyte Analysis: Dr.D.Chandrasekaran, PH.D, Assistant Professor, Dept. of ClinicsDocument23 pagesBlood Gas & Electrolyte Analysis: Dr.D.Chandrasekaran, PH.D, Assistant Professor, Dept. of ClinicsMalatesh d sNo ratings yet
- Arterial Blood Gas InterpretationDocument69 pagesArterial Blood Gas InterpretationostuffeNo ratings yet
- Blood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical CareDocument48 pagesBlood Gases (Abgs) Interpretation Dr/Baha Eldin Hassan Ahmed Fellow Paediatric Critical Carehagir alhajNo ratings yet
- LRP CriticalCare Sample2Document46 pagesLRP CriticalCare Sample2Aniket ChoudharyNo ratings yet
- AbgDocument38 pagesAbgroopaNo ratings yet
- IT 17 - ZUL HypoxiaDocument22 pagesIT 17 - ZUL HypoxiaImanda Husna SilalahiNo ratings yet
- Oxygen Cascade - SHANTHINIDocument57 pagesOxygen Cascade - SHANTHINIMani BharathiNo ratings yet
- Respiratory Failure (ACUTE) : Dora M Alvarez MD LH 2004Document72 pagesRespiratory Failure (ACUTE) : Dora M Alvarez MD LH 2004Lovely San SebastianNo ratings yet
- AbgDocument66 pagesAbgindyaphdNo ratings yet
- Oxygen Therapy: Dr. Subhankar ChatterjeeDocument49 pagesOxygen Therapy: Dr. Subhankar ChatterjeesubhankarNo ratings yet
- Arterial Blood Gas AnalysisDocument23 pagesArterial Blood Gas AnalysisVartika SainiNo ratings yet
- Abg InterpretationDocument52 pagesAbg InterpretationCirugia Cardiovascular NeivaNo ratings yet
- Interpretasi Agd Juni 2020Document34 pagesInterpretasi Agd Juni 2020Christiana TrijayantiNo ratings yet
- Oxygen Therapy: Dr. Rajesh AroraDocument59 pagesOxygen Therapy: Dr. Rajesh ArorarkdivyaNo ratings yet
- ABG InterpretationDocument49 pagesABG InterpretationMuhammad Fathullah MazparNo ratings yet
- Respiratory Failure: Lack of Respiratory SuccessDocument41 pagesRespiratory Failure: Lack of Respiratory SuccessYS NateNo ratings yet
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- Menstrual Cycle and Fertility by Neville Mvo NgumDocument7 pagesMenstrual Cycle and Fertility by Neville Mvo Ngumlovelyc95No ratings yet
- Hobden Antibiotics II 09Document12 pagesHobden Antibiotics II 09lovelyc95No ratings yet
- Embryo For Real CycleDocument31 pagesEmbryo For Real Cyclelovelyc95No ratings yet
- CHAPT 05 Intestinal AbsorptionDocument14 pagesCHAPT 05 Intestinal Absorptionlovelyc95No ratings yet
- Make Your Self ClearDocument5 pagesMake Your Self Clearlovelyc95No ratings yet
- Anatomy: Important Vessels and Source of BleedingDocument87 pagesAnatomy: Important Vessels and Source of Bleedinglovelyc95No ratings yet
- Your Fearless Leaders:: SSN Anatomy #2Document10 pagesYour Fearless Leaders:: SSN Anatomy #2lovelyc95No ratings yet
- Anatomy of The Intercostal SpaceDocument17 pagesAnatomy of The Intercostal Spacelovelyc95No ratings yet
- Review Quiz - Chapter 16: Head & Neck: C. Laryngeal CarcinomaDocument4 pagesReview Quiz - Chapter 16: Head & Neck: C. Laryngeal Carcinomalovelyc95No ratings yet
- Cell Signaling Objectives - SanchezDocument14 pagesCell Signaling Objectives - Sanchezlovelyc95No ratings yet
- ObgynDocument1 pageObgynlovelyc95No ratings yet
- Amino AcidDocument33 pagesAmino Acidlovelyc95100% (1)
- B9780702031458000636 WebDocument13 pagesB9780702031458000636 WebChristopher BermeoNo ratings yet
- The MoneraDocument19 pagesThe MoneraNaufal Taufiq AmmarNo ratings yet
- Materi Kep. Kritis Acute GI BleedingDocument35 pagesMateri Kep. Kritis Acute GI Bleedingharsani auroraNo ratings yet
- April PhysiologyDocument2 pagesApril Physiologyapi-284800663No ratings yet
- Histology - Respiratory SystemDocument14 pagesHistology - Respiratory SystemAbiola NerdNo ratings yet
- Detection of Leukemia in Human Blood Sample Based On Microscopic Images: A StudyDocument8 pagesDetection of Leukemia in Human Blood Sample Based On Microscopic Images: A StudySaku RaNo ratings yet
- Unit 5.2 RespirationsDocument5 pagesUnit 5.2 RespirationsAssasination ClassroomNo ratings yet
- Materi HE GinjalDocument61 pagesMateri HE GinjalYafi Dyah C.INo ratings yet
- Basic of Cardiovascular and Respiratory SystemDocument59 pagesBasic of Cardiovascular and Respiratory SystemMonika ChaikumarnNo ratings yet
- CPR Review Worksheet Ans KeyDocument9 pagesCPR Review Worksheet Ans Keyapi-234803876No ratings yet
- Essencial Phrasal VerbsDocument4 pagesEssencial Phrasal VerbsalvereNo ratings yet
- B.SC Botany Sem 1 To 6 2017Document72 pagesB.SC Botany Sem 1 To 6 2017Jay ShethNo ratings yet
- List of ContributorsDocument485 pagesList of ContributorsRock BandNo ratings yet
- Journal of EthnopharmacologyDocument9 pagesJournal of EthnopharmacologyKaryn Olascuaga-CastilloNo ratings yet
- Scientific Posts: Csir-National Botanical Research InstituteDocument10 pagesScientific Posts: Csir-National Botanical Research InstituteYogesh KapilNo ratings yet
- Medical Complications of Type 2 DiabetesDocument422 pagesMedical Complications of Type 2 DiabetesMayracpp.16No ratings yet
- Omm Exam 3 LGTDocument59 pagesOmm Exam 3 LGTSolomon Seth SallforsNo ratings yet
- Pemicu 2Document109 pagesPemicu 2claudiasNo ratings yet
- 0046 8177 (93) 90013 7Document12 pages0046 8177 (93) 90013 7Carmen Gomez MuñozNo ratings yet
- EOT2 BiologyDocument21 pagesEOT2 BiologyKasumi SatoNo ratings yet