Urinary System and Body Fluids
Podocytes
�Functions of the Urinary System
The kidneys produce urine The ureters transport urine to the urinary bladder The urinary bladder stores urine The urethra transports urine to the outside of the body
�Functions of the Urinary System
The following functions are performed by the kidneys:
1. Excretion (eliminates waste) 2. Regulate blood volume and pressure 3. Regulation of the concentration of solutes in the blood (ion concentration) 4. Regulation of extracellular fluid pH 5. Regulation of red blood cell synthesis 6. Vitamin D production
�Kidney Anatomy and Histology
Location and External Anatomy of the Kidneys
Lie behind the peritoneum (retroperitoneal) on the posterior abdominal wall on each side of the vertebral column
�Kidney Anatomy and Histology
Surrounded by a renal capsule and fat and is held in place by the renal fascia The hilum, on the medial side of each kidney, is where blood vessels and nerves enter and exit the kidney
�Kidney Anatomy and Histology
The hilum, on the medial side of each kidney, is where blood vessels and nerves enter and exit the kidney
�Renal cortex
Renal medulla Renal column papilla of pyramid Renal sinus Major calyx Renal pelvis
Minor calyx Ureter Renal pyramid
�Internal Anatomy and Histology of the Kidneys
Two layers: cortex and medulla renal columns extend into the medulla between the renal pyramids tips of the renal pyramids project to the minor calyces Minor calyces open into the major calyces, which open into the renal pelvis Renal pelvis leads to the ureter
��Internal Anatomy and Histology of the Kidneys
Functional unit of the kidney - nephron Parts of a nephron: renal corpuscle proximal convoluted tubule loop of Henle distal convoluted tubule
�Internal Anatomy and Histology of the Kidneys
Renal corpuscle a. Bowmans capsule b. glomerulus.
�Internal Anatomy and Histology of the Kidneys
Proximal convoluted tubule - made up of simple cuboidal epithelial cells with brushing border of microvilli which increases the functional surface area for an optimum reabsorption and hormonal secretion.
�Internal Anatomy and Histology of the Kidneys
Loop of Henle:
a. descending and thin ascending limb - made up of simple squamous cells.
b. thick ascending limb - made up of simple cuboidal to low columnar cells
�Internal Anatomy and Histology of the Kidneys
Distal convoluted tubule (DCT) - made up of simple cuboidal cells. Last part of DCT and collecting duct - made up of simple cuboidal cells consisted of 2 types of cells: a. principal cell has receptor for antidiuretic hormone (ADH) and aldosteron. b. Intercalated cells function in regulating blood pH.
�Cortex
Medulla
Medulla
�Renal corpuscle (Bowmanns capsule and glomerulus) Bowmanns capsule is double layered cap on the glomerulus
a. Arteriole b. Parietal layer c. Proximal convoluted tubule d. Visceral layer
Renal tubules
P D
�Internal Anatomy and Histology of the Kidneys
. Fluid leaves the blood in the glomerulus and enters Bowmans capsule The nephron empties through the distal convoluted tubule into a collecting duct The collecting ducts empty into papillary ducts, which empty into minor calyces
�Internal Anatomy and Histology of the Kidneys
Cortical nephrons 85% of total nephrons Located in the cortex Juxtamedullary nephrons Are located at the cortexmedulla junction Have loops of Henle that deeply invade the medulla Have extensive thin segments Are involved in the production of concentrated urine
�Internal Anatomy and Histology of the Kidneys
Bowmans capsule a. outer parietal layer b. inner visceral layer consisting of podocytes Filtration membrane: a. Endothelium of glomerular capillaries (with fenestrae) b. Basement membrane c. Podocytes (with filtration slits)
�Capillary Beds of the Nephron
Every nephron has two capillary beds
Glomerulus Peritubular capillaries
Each glomerulus is:
Fed by an afferent arteriole Drained by an efferent arteriole
�Capillary Beds of the Nephron
Blood pressure in the glomerulus is high because: Arterioles are highresistance vessels Afferent arterioles have larger diameters than efferent arterioles Fluids and solutes are forced out of the blood throughout the entire length of the glomerulus
�Arteries and Veins of the Kidneys
Renal artery enters the kidney and branches many times, forming afferent arterioles
Efferent arterioles from the glomeruli supply the peritubular capillaries and vasa recta
�Arteries and Veins of the Kidneys
Peritubular capillaries and vasa recta join small veins that converge to form the renal vein, which exits the kidney
��Arteries and Veins of the Kidneys
Juxtaglomerular apparatus
granular cells of the afferent arteriole macula densa (part of the distal convoluted tubule) http://www.wisconline.com/objects/a p2204/ap2204.swf
�Urine Production
Kidneys filter the bodys entire plasma volume 60 times each day Glomerular filtrate: contains all plasma components except protein loses water, nutrients, and essential ions to become urine
�Urine Production
Urine contains metabolic wastes and unneeded substances Urine is produced by the processes of 1. Filtration 2. Tubular reabsorption 3. Tubular secretion
�Urine production
Glomerular filtration
Water and solutes smaller than proteins are forced through the capillary walls and pores of the glomerular capsule into the renal tubule
Tubular reabsorption
Water, glucose, amino acids and needed ions are transported out of the filtrate into the tubule cells and then enter the capillary blood
Tubular secretion - H+, K+, creatinine and drugs are removed from the peritubular
blood and secreted by the tubule cells into the filtrate
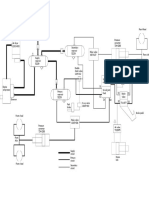
��Tab. 23.1
�Urine Formation
Fig. 23.7
�Abnormal urinary constituents
Substance Glucose Name of condition Possible causes Glycosuria Nonpathological: excessive intake of sugary foods Pathological: diabetes mellitus Nonpathological: physical excertion, pregnancy Pathological: glomerulonephritis, hypertension Urinary tract infection Bleeding in the urinary tract (due to trauma, kidney stones, infection) Various: transfusion reaction, hemolytic anemia Liver disease (hepatitis)
Proteins
Proteinuria Albuminuria
Pus (WBC Pyuria and bacteria) RBC Hemoglobin Bile pigment Hematuria Hemoglobinuria Bilirubinuria
�Urine Production
Filtration
The glomerular filtration rate is the amount of filtrate produce per minute The filtrate is plasma minus blood cells, platelets, and blood proteins Most (99%) of the filtrate is reabsorbed
�Urine Production
Filtration pressure is responsible for filtrate formation. Glomerular capillary pressure minus capsule pressure minus blood colloid osmotic pressure Changes are primarily caused by changes in glomerular capillary pressure
�Urine Production
Regulation of Glomerular Filtration Rate
Autoregulation dampens systemic blood pressure changes by altering afferent arteriole diameter
Under normal conditions, renal autoregulation maintains a nearly constant glomerular filtration rate Autoregulation entails two types of control Myogenic: responds to changes in pressure in the renal blood vessels Flow-dependent tubuloglomerular feedback: senses changes in the juxtaglomerular apparatus
Sympathetic stimulation decreases renal blood flow and afferent arteriole diameter
�Tubular Reabsorption
A transepithelial process whereby most tubule contents are returned to the blood
�Tubular Reabsorption
Transported substances move through three membranes Luminal and basolateral membranes of tubule cells Endothelium of peritubular capillaries Only Ca2+, Mg2+, K+, and some Na+ are reabsorbed via paracellular pathways
�Tubular Reabsorption
Filtrate is reabsorbed by: diffusion facilitated diffusion active transport symport antiport from the nephron and collecting ducts into the peritubular capillaries and vasa recta
�Tubular Reabsorption
Proximal convoluted tubule reabsorbs 65% of filtrate water and NaCl (solutes) Descending limb of the loop of Henle reabsorbs 15% of filtrate water Ascending limb of the loop of Henle reabsorbs 25% of filtrate NaCl Distal convoluted tubules and collecting ducts reabsorb up to 19% of filtrate water and 9%-10% of filtrate water respectively
�Tubular Reabsorption
Waste products and toxic substances are concentrated in the urine
�Reabsorption in the Proximal Convoluted Tubule
Fig. 23.9
�Reabsorption in the Thick Segment of the Ascending Limb of the Loop of Henle
Fig. 23.10
�Tubular Secretion
Substances are secreted in the proximal or distal convoluted tubules and the collecting ducts Hydrogen ions, K+, and some substances not produced in the body are secreted by antiport mechanisms
�Summary of Urine Concentrating Mechanism
Fig. 23.11
�Maintaining the Medullary Concentration Gradient
Necessary for the production of concentrated urine Addition of solutes increases the medullary interstitial fluid concentration. a. ascending limb of the loop of Henle adds NaCl, but not water b. Urea cycles between the collecting ducts and the thin segments of the loop of Henle
�Maintaining the Medullary Concentration Gradient
The vasa recta uses a countercurrent mechanism that removes reabsorbed water and solutes without disturbing the medullary concentration gradient http://www.cellphys.ubc. ca/undergrad_files/urine. swf
�Blood Flow Through the Vasa Recta
Fig. 23.13
�Hormonal Regulation of Urine Concentration and Volume
Antidiuretic Hormone (ADH)
Secreted by the posterior pituitary Inhibits diuresis This equalizes the osmolality of the filtrate and the interstitial fluid Increases water permeability in the distal convoluted tubules and collecting ducts by stimulating the insertion of aquaporin-2 molecules into apical membranes In the presence of ADH, 99% of the water in filtrate is reabsorbed
�Hormonal Regulation of Urine Concentration and Volume
ADH regulates blood osmolality by altering water reabsorption
An increase in blood osmolality or a significant decrease in blood pressure stimulates increased ADH secretion Increases water reabsorption and as a result Blood osmolality decreases Blood volume and blood pressure increase Urine concentration increases Urine volume decreases
�Hormonal Regulation of Urine Concentration and Volume
A decrease in blood osmolality or a significant increase in blood pressure stimulates decreased ADH secretion
Decreases water reabsorption and as a result Blood osmolality increases Blood volume and blood pressure decrease Urine concentration decreases Urine volume increases
�Effect of ADH on Water Movement
Fig. 23.14
��Hormonal Regulation of Urine Concentration and Volume
ReninAngiotensinAldosterone
Renin, produced by the kidneys, causes the conversion of angiotensinogen to angiotensin I Angiotensin-converting enzyme converts angiotensin I into angiotensin II, which stimulates aldosterone secretion from the adrenal cortex Aldosterone affects Na+ and Cl - transport in the nephron and collecting ducts by stimulating an increase in transport proteins
�Effect of Aldosterone on Ion Movement
Fig. 23.15
�Hormonal Regulation of Urine Concentration and Volume
Atrial Natriuretic Hormone Produced by the heart when blood pressure increases Inhibits Na+ reabsorption in the kidneys, resulting in increased urine volume and decreased blood volume and blood pressure Inhibits ADH secretion and dilates arteries and veins
�ANH and the Regulation of Na+ and Water
Fig. 23.16
�Anatomy and Histology of the Ureters and Urinary Bladder
The walls of the ureter and urinary bladder consist of 1. Mucosa Epithelium
Transitional epithelium permits changes in size
Lamina propria loose connective tissue 2. Muscular coat
Contraction of the smooth muscle moves urine Inner longitudinally and outer circular The muscle of bladder is called detrusor muscle
3. Fibrous adventitia
�Ureter
Urinary bladder
�Anatomy and Histology of the Urethra
The urethra is lined with transitional and stratified squamous epithelium
Males have an internal urethral sphincter of smooth muscle that prevents retrograde ejaculation of semen An external urethral sphincter of skeletal muscle allows voluntary control of urination
�Fig. 23.17
�Urine Movement
Urine Flow Through the Nephron and Ureters
A pressure gradient causes urine to flow from Bowmans capsule to the ureters Peristalsis moves urine through the ureters
�Urine Movement
Micturition Reflex
Stretch of the urinary bladder stimulates a reflex that causes the urinary bladder to contract and inhibits the external urethral sphincter Higher brain centers can stimulate or inhibit the micturition reflex Voluntary relaxation of the external urethral sphincter permits urination and contraction prevents it
�Micturition Reflex
Fig. 23.18
��Effects of Aging on the Kidneys
There is a gradual decrease in the size of the kidney
Associated with a decrease in renal blood flow The number of functional nephrons decreases
Renin secretion and vitamin D synthesis decreases Nephron secretion and absorbtion declines
�Body Fluids
Today body water volume (60%) body weight Intracellular fluid is inside cells (40%) Extracellular fluid is outside cells (20%)and includes interstitial fluid (80%) and plasma (20%)
�Intracellular Fluid
Substances used or produced inside the cell Substances exchanged with the extracellular fluid Plasma membrane regulates the movement of materials The difference between intracellular and extracellular fluid concentrations determines water movement
�Regulation of Intracellular Fluid
Fig. 23.19
�Regulation of Body Fluid Concentration and Volume Water Input
Ingested (90%) or produced in metabolism (10%) Habit and social setting influence thirst
Increase in extracellular osmolality Decrease in blood pressure stimulates the sense of thirst
Wetting of the oral mucosa or stretch of the gastrointestinal tract inhibits thirst
�Regulation of Body Fluid Concentration and Volume Water Output
Lost through evaporation from the respiratory system and the skin (insensible perspiration and sweat) (35%) Loss into the gastrointestinal tract normally is small (4%) The kidneys are the primary regulator of water excretion (61%)
�Tab. 23.3
�Effect of Blood Osmolality and Pressure on Water Intake
Fig. 23.20
�Regulation of Body Fluid Concentration and Volume Regulation of Extracellular Fluid Osmolality
An increase in extracellular fluid osmolality stimulates thirst and ADH secretion
Increased fluid intake Increased water reabsorption in the kidneys
A decrease in extracellular osmolality inhibits thirst and decreases ADH secretion
Decreased fluid intake Decreased water reabsorption in the kidneys
�Summary of Blood Osmolality Regulation
Fig. 23.21
�Regulation of Body Fluid Concentration and Volume
Regulation of Extracellular Fluid Volume
Decreased extracellular fluid volume results in
Increased aldosterone secretion Decreased ANH secretion Increased ADH secretion Increased sympathetic stimulation of the afferent arterioles Increased thirst Decreased glomerular filtration rate Increased reabsorption of Na+ and water
�Regulation of Body Fluid Concentration and Volume
Regulation of Extracellular Fluid Volume
Increased extracellular fluid volume results in
Decreased aldosterone secretion Increased ANH secretion Decreased ADH secretion Decreased sympathetic stimulation of the afferent arterioles Decreased thirst Increased glomerular filtration rate Decreased reabsorption of Na+ and water
�Summary of Blood Volume Regulation
Fig. 23.22
�Regulation of Specific Electrolytes in the Extracellular Fluid Regulation of Sodium Ions
The kidneys are the major route by which Na+ is excreted Excretion is regulated by aldosterone and ANH Lost in sweat With association anions are responsible for 90%-95% of extracellular osmotic pressure
�Tab. 23.4
�Regulation of Specific Electrolytes in the Extracellular Fluid
Regulation of Chloride Ions
Dominant negatively charged ions in extracellular fluid Regulated by the mechanisms regulating cations
Regulation of Potassium Ions
Reabsorbed from the proximal convoluted tubule Secreted into the distal convoluted tubule Aldosterone increases the amount of K+ secreted
�Summary of Blood K+ Regulation
Fig. 23.23
�Tab. 23.5
�Regulation of Specific Electrolytes in the Extracellular Fluid
Regulation of Calcium Ions
Parathyroid hormone increases extracellular Ca2+ levels
Increases osteoclast activity Increases reabsorption from the kidneys Stimulates active vitamin D production
Vitamin D stimulates Ca2+ uptake in the intestines Calcitonin decreases extracellular Ca2+ levels by inhibiting osteoclasts
�Summary of Blood Ca2+ Regulation
Fig. 23.24
�Tab. 23.6
�Regulation of Acid-Base Balance
Acids release H+ into solution, and bases remove them Buffers respond almost instantaneously to changes in pH, whereas the respiratory system takes minutes and the kidneys may take hour to days The kidneys have the greatest ability to regulate pH precisely
�Summary of Acid-Base Balance Regulation
Fig. 23.25
�Regulation of Acid-Base Balance
Buffer Systems
A buffer resists changes in pH
When H+ are added to a solution, the buffer removes them When H+ are removed from a solution, the buffer replaces them
Carbonic acid/bicarbonate, proteins, phosphate compounds, and ammonia are important buffers
�Respiratory Regulation of Acid-Base Balance
Achieved through the carbonic acid/bicarbonate buffer system
As carbon dioxide levels increase, pH decreases As carbon dioxide levels decrease, pH increases Carbon dioxide levels and pH affect the respiratory centers
�Respiratory Regulation of Acid-Base Balance
The pH affects the respiratory centers Hypoventilation increases blood carbon dioxide levels, and hyperventilation decreases blood carbon dioxide levels
Decreased pH increases the rate and depth of respiration, which lowers carbon dioxide levels and increases blood pH Increased pH decreases the rate and depth of respiration, which increases carbon dioxide levels and decreases blood pH
�Respiratory Regulation of Body Acid-Base Balance
Fig. 23.26
�Renal Regulation of Acid-Base Balance
For each H+ added to the blood, a HCO3- is removed; for each H+ removed from the blood, a HCO3- is added For each H+ secreted into the filtrate, a HCO3- is removed from the filtrate and a HCO3- is added to the blood Hydrogen phosphate (HPO42-) and ammonia (NH3) are the major non-bicarbonate bases in the filtrate
When H+ combines with HPO42- and NH3, the filtrate is buffered, allowing additional H+ to be secreted For each H+ that combines with HPO42- and NH3, a new HCO3- is added to the blood
The metabolism of glutamine produces new HCO3-
�Reabsorption of HCO3-
Fig. 23.27
�Hydrogen Ion Secretion
Fig. 23.28
�Page 759