0% found this document useful (0 votes)
75 views24 pagesAcid-Base Homeostasis Overview
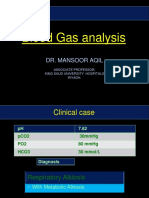
This document discusses acid-base homeostasis. It notes that fluid, electrolyte and acid-base balance are critical to health and maintained by intake/output and renal/pulmonary systems. The major buffer system is carbonic acid-bicarbonate, which regulates pH levels and is controlled by kidneys. Disturbances can cause acidosis or alkalosis. Diagnosis involves analyzing blood gases including pH, pCO2, HCO3 levels. A case example describes diabetic ketoacidosis in a patient presenting with high blood glucose, ketones, and low pH. Treatment involved insulin, IV fluids and bicarbonate to correct electrolyte and acid-base imbalances.
Uploaded by
Red DemonCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
75 views24 pagesAcid-Base Homeostasis Overview
This document discusses acid-base homeostasis. It notes that fluid, electrolyte and acid-base balance are critical to health and maintained by intake/output and renal/pulmonary systems. The major buffer system is carbonic acid-bicarbonate, which regulates pH levels and is controlled by kidneys. Disturbances can cause acidosis or alkalosis. Diagnosis involves analyzing blood gases including pH, pCO2, HCO3 levels. A case example describes diabetic ketoacidosis in a patient presenting with high blood glucose, ketones, and low pH. Treatment involved insulin, IV fluids and bicarbonate to correct electrolyte and acid-base imbalances.
Uploaded by
Red DemonCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd