Professional Documents
Culture Documents
Bronchiectasis
Uploaded by
Muhammad Iyhan Nuriansyah0 ratings0% found this document useful (0 votes)
30 views21 pagesOriginal Title
Bronchiectasis.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
30 views21 pagesBronchiectasis
Uploaded by
Muhammad Iyhan NuriansyahCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 21
Bronchiectasis can arise from infectious or
noninfectious causes (Table 258-1).
Clues to the underlying etiology are often provided
by the pattern of lung involvement.
Focal bronchiectasis refers to bronchiectatic
changes in a localized area of the lung and can be
a consequence of obstruction of the airway—either
extrinsic (e.g., due to compression by adjacent
lymphadenopathy or parenchymal tumor mass) or
intrinsic (e.g., due to an airway tumor or aspirated
foreign body, a scarred/stenotic airway, or bronchial
atresia from congenital underdevelopment of the
airway).
Diffuse bronchiectasis is characterized by widespread
bronchiectatic changes throughout the lung and
often arises from an underlying systemic or infectious
disease process
More pronounced involvement of the upper lung fields is most common
in cystic fibrosis (CF) and is also observed in postradiation fibrosis,
corresponding to the lung region encompassed by the radiation port.
Bronchiectasis with predominant involvement of the lower lung fields
usually has its source in chronic recurrent aspiration (e.g., due to
esophageal motility disorders like those in scleroderma), end-stage
fibrotic lung disease (e.g., traction bronchiectasis from idiopathic
pulmonary fibrosis), or recurrent immunodeficiency-associated infections
(e.g., hypogammaglobulinemia).
Bronchiectasis resulting from infection by nontuberculous mycobacteria
[NTM; most commonly the Mycobacterium avium-intracellulare complex
(MAC)] often preferentially affects the midlung fields.
Congenital causes of bronchiectasis with predominant midlung field
involvement include the dyskinetic/immotile cilia syndrome.
Finally, predominant involvement of the central airways is reported in
association with allergic bronchopulmonary aspergillosis (ABPA), in which
an immune-mediated reaction to Aspergillus damages the bronchial
wall.
Congenital causes of central airway–predominant bronchiectasis
resulting from cartilage deficiency include tracheobronchomegaly
(Mounier-Kuhn syndrome) and Williams-Campbell syndrome.
In many cases, the etiology of bronchiectasis is not determined. In case
series, as many as 25–50% of patients referred for bronchiectasis have
idiopathic disease.
The epidemiology of bronchiectasis varies
greatly with the underlying etiology.
For example, patients born with CF often
develop significant clinical bronchiectasis in
late adolescence or early adulthood, although
atypical presentations of CF in adults in their
thirties and forties are also possible.
In contrast, bronchiectasis resulting from MAC
infection classically affects nonsmoking women
older than age 50 years.
In general, the incidence of bronchiectasis
increases with age.
Bronchiectasis is more common among
women than among men.
In areas where tuberculosis is prevalent, bronchiectasis
more frequently occurs as a sequela of granulomatous
infection.
Focal bronchiectasis can arise from extrinsic
compression of the airway by enlarged granulomatous
lymph nodes and/or from development of intrinsic
obstruction as a result of erosion of a calcified lymph
node through the airway wall (e.g., broncholithiasis).
Especially in reactivated tuberculosis, parenchymal
destruction from infection can result in areas of more
diffuse bronchiectasis.
Apart from cases associated with tuberculosis, an
increased incidence of non-CF bronchiectasis with an
unclear underlying mechanism has been reported as a
significant problem in developing nations.
It has been suggested that the high incidence of
malnutrition in certain areas may predispose to immune
dysfunction and development of bronchiectasis
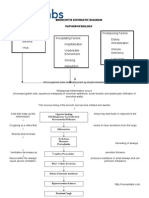
The most widely cited mechanism of infectious bronchiectasis
is the "vicious cycle hypothesis," in which susceptibility to
infection and poor mucociliary clearance result in microbial
colonization of the bronchial tree.
Some organisms, such as Pseudomonas aeruginosa, exhibit a
particular propensity for colonizing damaged airways and
evading host defense mechanisms.
Impaired mucociliary clearance can result from inherited
conditions such as CF or dyskinetic cilia syndrome, and it has
been proposed that a single severe infection (e.g.,
pneumonia caused by Bordetella pertussis or Mycoplasma
pneumoniae) can result in significant airway damage and
poor secretion clearance.
The presence of the microbes incites continued chronic
inflammation, with consequent damage to the airway wall,
continued impairment of secretion and microbial clearance,
and ongoing propagation of the infectious/inflammatory
cycle. Moreover, it has been proposed that mediators
released directly from bacteria can interfere with mucociliary
clearance.
Classic studies of the pathology of bronchiectasis from the
1950s demonstrated significant small-airway wall inflammation
and larger-airway wall destruction as well as dilation, with loss
of elastin, smooth muscle, and cartilage.
It has been proposed that inflammatory cells in the small
airways release proteases and other mediators, such as
reactive oxygen species and proinflammatory cytokines, that
damage the larger-airway walls. Furthermore, the ongoing
inflammatory process in the smaller airways results in airflow
obstruction.
It is believed that antiproteases, such as 1 antitrypsin, play an
important role in neutralizing the damaging effects of
neutrophil elastase and in enhancing bacterial killing. In
addition to emphysema, bronchiectasis has been observed in
patients with 1 antitrypsin deficiency.
Proposed mechanisms for noninfectious bronchiectasis include
immune-mediated reactions that damage the bronchial wall
(e.g., those associated with systemic autoimmune conditions
such as Sjögren's syndrome and rheumatoid arthritis). Traction
bronchiectasis refers to dilated airways arising from
parenchymal distortion as a result of lung fibrosis (e.g.,
postradiation fibrosis or idiopathic pulmonary fibrosis).
The most common clinical presentation is a persistent
productive cough with ongoing production of thick,
tenacious sputum. Physical findings often include
crackles and wheezing on lung auscultation, and
some patients with bronchiectasis exhibit clubbing of
the digits.
Mild to moderate airflow obstruction is often
detected on pulmonary function tests, overlapping
with that seen at presentation with other conditions,
such as chronic obstructive pulmonary disease
(COPD).
Acute exacerbations of bronchiectasis are usually
characterized by changes in the nature of sputum
production, with increased volume and purulence.
However, typical signs and symptoms of lung
infection, such as fever and new infiltrates, may not
be present.
The diagnosis is usually based on presentation with a
persistent chronic cough and sputum production
accompanied by consistent radiographic features.
While chest radiographs lack sensitivity, the presence of
"tram tracks" indicating dilated airways is consistent with
bronchiectasis.
Chest CT is more specific for bronchiectasis and is the
imaging modality of choice for confirming the diagnosis.
CT findings include airway dilation (detected as parallel
"tram tracks" or as the "signet-ring sign"—a cross-
sectional area of the airway with a diameter at least 1.5
times that of the adjacent vessel), lack of bronchial
tapering (including the presence of tubular structures
within 1 cm from the pleural surface), bronchial wall
thickening in dilated airways, inspissated secretions (e.g.,
the "tree-in-bud" pattern), or cysts emanating from the
bronchial wall (especially pronounced in cystic
bronchiectasis
The evaluation of a patient with bronchiectasis
entails elicitation of a clinical history, chest
imaging, and a workup to determine the
underlying etiology.
Evaluation of focal bronchiectasis almost always
requires bronchoscopy to exclude airway
obstruction by an underlying mass or foreign
body.
A workup for diffuse bronchiectasis includes
analysis for the major etiologies
Pulmonary function testing is an important
component of a functional assessment of the
patient.
Treatment of infectious bronchiectasis is
directed at the control of active
infection and improvements in secretion
clearance and bronchial hygiene so as
to decrease the microbial load within
the airways and minimize the risk of
repeated infections
Antibiotics targeting the causative or presumptive pathogen
(with Haemophilus influenzae and P. aeruginosa isolated
commonly) should be administered in acute exacerbations,
usually for a minimum of 7–10 days.
Decisions about treatment of NTM infection can be difficult, given
that these organisms can be colonizers as well as pathogens and
the prolonged treatment course often is not well tolerated.
Consensus guidelines have advised that diagnostic criteria for
true clinical infection with NTM should be considered in patients
with symptoms and radiographic findings of lung disease who
have at least two sputum samples positive on culture; at least
one bronchoalveolar lavage (BAL) fluid sample positive on
culture; a biopsy sample displaying histopathologic features of
NTM infection (e.g., granuloma or a positive stain for acid-fast
bacilli) along with one positive sputum culture; or a pleural fluid
sample (or a sample from another sterile extrapulmonary site)
positive on culture.
MAC strains are the most common NTM pathogens, and the
recommended regimen for HIV-negative patients includes a
macrolide combined with rifampin and ethambutol. Consensus
guidelines also recommend macrolide susceptibility testing for
clinically significant MAC isolates
The numerous approaches employed to enhance
secretion clearance in bronchiectasis include
hydration and mucolytic administration,
aerosolization of bronchodilators and hyperosmolar
agents (e.g., hypertonic saline), and chest
physiotherapy (e.g., postural drainage, traditional
mechanical chest percussion via hand clapping to
the chest, or use of devices such as an oscillatory
positive expiratory pressure flutter valve or a high-
frequency chest wall oscillation vest).
The mucolytic dornase (DNase) is recommended
routinely in CF-related bronchiectasis but not in non-
CF bronchiectasis, given concerns about lack of
efficacy and potential harm in the non-CF
population
It has been proposed that control of the inflammatory response
may be of benefit in bronchiectasis, and relatively small-scale
trials have yielded evidence of alleviated dyspnea, decreased
need for inhaled -agonists, and reduced sputum production with
inhaled glucocorticoids.
However, no significant differences in lung function or
bronchiectasis exacerbation rates have been observed.
Risks of immunosuppression and adrenal suppression must be
carefully considered with use of anti-inflammatory therapy in
infectious bronchiectasis.
Nevertheless, administration of oral/systemic glucocorticoids may
be important in treating bronchiectasis due to certain etiologies,
such as ABPA, or noninfectious bronchiectasis due to underlying
conditions, especially that in which an autoimmune condition is
believed to be active (e.g., rheumatoid arthritis or Sjögren's
syndrome).
Patients with ABPA may also benefit from a prolonged course of
treatment with the oral antifungal agent itraconazole
In more severe cases of infectious bronchiectasis,
recurrent infections and repeated courses of
antibiotics can lead to microbial resistance to
antibiotics.
In certain cases, combinations of antibiotics that
have their own independent toxicity profiles may be
necessary to treat resistant organisms.
Recurrent infections can result in injury to superficial
mucosal vessels, with bleeding and, in severe cases,
life-threatening hemoptysis.
Management of massive hemoptysis usually requires
intubation to stabilize the patient, identifying the
source of bleeding, and protecting the nonbleeding
lung. Control of bleeding often necessitates bronchial
artery embolization and, in severe cases, surgery.
Outcomes of bronchiectasis vary widely
with the underlying etiology and may also
be influenced by the frequency of
exacerbations and (in infectious cases) the
specific pathogens involved.
In one study, the decline of lung function in
patients with non-CF bronchiectasis was
similar to that in patients with COPD, with
the forced expiratory volume in 1 s (FEV1)
declining by 50–55 mL per year as opposed
to 20–30 mL per year for healthy controls.
Reversal of an underlying
immunodeficient state (e.g., by
administration of gamma globulin for
immunoglobulin-deficient patients) and
vaccination of patients with chronic
respiratory conditions (e.g., influenza and
pneumococcal vaccines) can decrease
the risk of recurrent infections.
Patients who smoke should be
counseled about smoking cessation
After resolution of an acute infection in patients with recurrences
(e.g., 3 episodes per year), the use of suppressive antibiotics to
minimize the microbial load and reduce the frequency of
exacerbations has been proposed, although there is less
consensus with regard to this approach in non-CF-associated
bronchiectasis than there is in patients with CF-related
bronchiectasis.
Possible suppressive treatments include (1) administration of an
oral antibiotic (e.g., ciprofloxacin) daily for 1–2 weeks per month;
(2) use of a rotating schedule of oral antibiotics (to minimize the
risk of development of drug resistance); (3) administration of a
macrolide antibiotic daily or three times per week (with
mechanisms of possible benefit related to non-antimicrobial
properties, such as anti-inflammatory effects and reduction of
gram-negative bacillary biofilms); (4) inhalation of aerosolized
antibiotics [e.g., tobramycin inhalation solution (TOBI)] by select
patients on a rotating schedule (e.g., 30 days on, 30 days off)
with the goal of decreasing the microbial load without
encountering the side effects of systemic drug administration;
and (5) intermittent administration of IV antibiotics (e.g., "clean-
outs") for patients with more severe bronchiectasis and/or
resistant pathogens.
You might also like
- Bronchiectasis: DR Budi Enoch SPPDDocument21 pagesBronchiectasis: DR Budi Enoch SPPDVito CuyNo ratings yet
- Etiology: An Irreversible Airway Dilation That Involves The Lung inDocument3 pagesEtiology: An Irreversible Airway Dilation That Involves The Lung inOlli TherineNo ratings yet
- B&lung AbscessDocument21 pagesB&lung Abscessnathan asfahaNo ratings yet
- DifferentialsDocument7 pagesDifferentialsStewart Garneth Reston RancesNo ratings yet
- Hypothesis", in Which Susceptibility To Infection and Poor Mucociliary Clearance ResultDocument2 pagesHypothesis", in Which Susceptibility To Infection and Poor Mucociliary Clearance ResultAngelique Mae Mortejo SalarzaNo ratings yet
- I Lower Respiratory System PathologyDocument12 pagesI Lower Respiratory System PathologyBaha Al AdaylehNo ratings yet
- 3 BronchiectasisDocument29 pages3 BronchiectasisЕвгений ХанькоNo ratings yet
- The Kursk State Medical University: Lecture For Self-Training of 6-th Medical Course English-Speaking StudentsDocument15 pagesThe Kursk State Medical University: Lecture For Self-Training of 6-th Medical Course English-Speaking StudentsDaniel FunkNo ratings yet
- Bronchiectasis: Getnet Alemu, MD Huchs Feb 3, 2012Document38 pagesBronchiectasis: Getnet Alemu, MD Huchs Feb 3, 2012yosefNo ratings yet
- Bronchiectasis OkDocument60 pagesBronchiectasis OkImmanuelNo ratings yet
- Lung Abscess: Presented byDocument36 pagesLung Abscess: Presented byPalanki Gopal100% (1)
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Broncho PneumoniaDocument21 pagesBroncho PneumoniaRiad GagahNo ratings yet
- Lung Abscess Bronchoectasis PleurisynDocument19 pagesLung Abscess Bronchoectasis Pleurisynmarco luenaNo ratings yet
- BronchiectasisDocument9 pagesBronchiectasisIS99057No ratings yet
- Pulmonary PathologyDocument46 pagesPulmonary PathologyMuostafa KamelNo ratings yet
- Laporan Pendahuluan Asuhan Keperawatan Anak Pada Klien Dengan BronkhitisDocument14 pagesLaporan Pendahuluan Asuhan Keperawatan Anak Pada Klien Dengan BronkhitisDicky Aris SetiawanNo ratings yet
- 2.BE PathogenesisDocument7 pages2.BE PathogenesisJaya Semara PutraNo ratings yet
- Lung AbcessDocument11 pagesLung AbcessGul SapiNo ratings yet
- Bronchiectasis: Dr. Kapil Rastogi MPT (Cardiopulmonary) Assistant ProfessorDocument18 pagesBronchiectasis: Dr. Kapil Rastogi MPT (Cardiopulmonary) Assistant ProfessorKavya MittalNo ratings yet
- Lec.2 Respirotary System SaifDocument19 pagesLec.2 Respirotary System Saifs2111110520No ratings yet
- Bronchial ObstructionDocument137 pagesBronchial ObstructionGrajdianu Natalia100% (1)
- Default PDFDocument29 pagesDefault PDFNilson Morales CordobaNo ratings yet
- Bronchiectasis SymptomsDocument10 pagesBronchiectasis SymptomsGolam MasudNo ratings yet
- Lung Abscess: DR Budi Enoch SPPDDocument14 pagesLung Abscess: DR Budi Enoch SPPDLia pramitaNo ratings yet
- Bronchitis PathophysiologyDocument23 pagesBronchitis PathophysiologyRama Setya Bagaskara100% (2)
- Mr. Maheboob 1 Year M.SC Nursing Govt College of Nursing HolenarsipurDocument44 pagesMr. Maheboob 1 Year M.SC Nursing Govt College of Nursing HolenarsipurDr Tahira NihalNo ratings yet
- Professor Youry Vladimirovitch PlotnicovDocument109 pagesProfessor Youry Vladimirovitch PlotnicovOxana TulbeaNo ratings yet
- BrochiectasisDocument34 pagesBrochiectasisAndi Wija Indrawan PangerangNo ratings yet
- Bronchiectasis: Yuping GuoDocument75 pagesBronchiectasis: Yuping GuoAmeliaNo ratings yet
- Main Image ©muratseyit/istockphotoDocument10 pagesMain Image ©muratseyit/istockphotoade_liaNo ratings yet
- Study Guide 2Document16 pagesStudy Guide 2cNo ratings yet
- Abses Paru JurnalDocument7 pagesAbses Paru JurnalLestariNo ratings yet
- Abscess of The Lung Current Therapeutic OptionsDocument9 pagesAbscess of The Lung Current Therapeutic OptionsTalat AksuNo ratings yet
- Azhaar TopicDocument4 pagesAzhaar Topicbalab2311No ratings yet
- A. Synthesis of The Disease 1) Definition of The Disease (Book-Based)Document11 pagesA. Synthesis of The Disease 1) Definition of The Disease (Book-Based)glmachic021No ratings yet
- Syndrom of Consolidated Pulmonary Tissue. Pneumonia. Athelectasis. Andrei IchimDocument114 pagesSyndrom of Consolidated Pulmonary Tissue. Pneumonia. Athelectasis. Andrei IchimYan Sheng Ho100% (1)
- Dapus 3Document10 pagesDapus 3Yan Agus AchtiarNo ratings yet
- Article About CaughDocument8 pagesArticle About CaughNour AlhazzaaNo ratings yet
- IDSA Aspergillosis 2016-31-60 (1) - 1-25-1-15Document15 pagesIDSA Aspergillosis 2016-31-60 (1) - 1-25-1-15faradibaNo ratings yet
- IDSA Aspergillosis 2016-31-60 (1) - 1-25Document25 pagesIDSA Aspergillosis 2016-31-60 (1) - 1-25faradibaNo ratings yet
- Lung AbscessDocument7 pagesLung AbscessItha Maghfirah100% (1)
- Diseases of The Respiratory System and Circulatory SystemDocument7 pagesDiseases of The Respiratory System and Circulatory SystemMaria Teresa GimenoNo ratings yet
- Respiratory System DisordersDocument9 pagesRespiratory System Disordersasop06No ratings yet
- Bacterial Destruction of The LungsDocument46 pagesBacterial Destruction of The LungsAhmad Abu KushNo ratings yet
- Endobronchial Tuberculosis An OverviewDocument5 pagesEndobronchial Tuberculosis An OverviewPramesti Fitria KNo ratings yet
- Bronchiectasis DesieDocument77 pagesBronchiectasis DesieAbebe GelawNo ratings yet
- Pneumonia, BronchiolitisDocument65 pagesPneumonia, BronchiolitisYemata HailuNo ratings yet
- Childhood Adult: Bronchiectasis in PulmonaryDocument9 pagesChildhood Adult: Bronchiectasis in PulmonaryphobicmdNo ratings yet
- COPD Pathophisiology NarrativeDocument3 pagesCOPD Pathophisiology NarrativejojrNo ratings yet
- Pneumatocele: BackgroundDocument8 pagesPneumatocele: BackgroundSilmi Noor RachniNo ratings yet
- Lung Abscess in Adults - UpToDateDocument32 pagesLung Abscess in Adults - UpToDateAntonela Esther Quijada BenitoNo ratings yet
- Makalah Radiologi TB BE v0.1Document15 pagesMakalah Radiologi TB BE v0.1giovannigyoNo ratings yet
- BronchiectasisDocument64 pagesBronchiectasisbrijeshNo ratings yet
- Establish An AirwayDocument7 pagesEstablish An AirwayMarionne James Jaranilla DinongNo ratings yet
- X Ray InterprationDocument6 pagesX Ray InterprationMelvita KurniawanNo ratings yet
- Chapter 4 BronchiectasisDocument10 pagesChapter 4 BronchiectasisAlmira SiamNo ratings yet
- Lung Abscess Bronchiectasis TuberculosisDocument19 pagesLung Abscess Bronchiectasis Tuberculosisajjju02No ratings yet
- Study Notes Respiratory SystemDocument19 pagesStudy Notes Respiratory SystemAnde Mangkuluhur Azhari ThalibbanNo ratings yet
- Bronchiectasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandBronchiectasis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Esh Guidelines DefDocument99 pagesEsh Guidelines DefMuhammad Iyhan NuriansyahNo ratings yet
- BronchiectasisDocument21 pagesBronchiectasisMuhammad Iyhan NuriansyahNo ratings yet
- DR Budi Enoch SPPDDocument29 pagesDR Budi Enoch SPPDMuhammad Iyhan NuriansyahNo ratings yet
- Anchalee Pulmonary Manifestation in AIDSDocument105 pagesAnchalee Pulmonary Manifestation in AIDSsuho exoNo ratings yet
- High Salivary Soluble L-Selectin and Interleukin-7 Levels in Asian Indian Patients With Primary Sjögren's SyndromeDocument5 pagesHigh Salivary Soluble L-Selectin and Interleukin-7 Levels in Asian Indian Patients With Primary Sjögren's SyndromeMaite Fernanda CuturrufoNo ratings yet
- Chromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Document5 pagesChromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Jun JoniNo ratings yet
- Theories of NeurosisDocument170 pagesTheories of NeurosisemilvulcuNo ratings yet
- Wound Debridement-FinalDocument3 pagesWound Debridement-FinaljessicagrepoNo ratings yet
- Meniscus Injuries: Uhuebor David Mbbs (Lagos)Document23 pagesMeniscus Injuries: Uhuebor David Mbbs (Lagos)Uhuebor DavidNo ratings yet
- Joslin Diabetes Center Clinical GuideDocument16 pagesJoslin Diabetes Center Clinical GuideNikolaus TalloNo ratings yet
- BPHDocument20 pagesBPHHerly KakaNo ratings yet
- Vibrio CholeraeDocument20 pagesVibrio CholeraeChockalingam MeenakshisundaramNo ratings yet
- My 5senserelativ (App) : Pedro Pérez Juan Gómez Luis Mejía Group 0 English IIIDocument4 pagesMy 5senserelativ (App) : Pedro Pérez Juan Gómez Luis Mejía Group 0 English IIIjarles mauricio hernandez parraNo ratings yet
- Management of Tinea Corporis, Tinea CrurisDocument10 pagesManagement of Tinea Corporis, Tinea CrurisRansidelenta Vistaprila ElmardaNo ratings yet
- RL2 CCR Book March-2021-P117-118Document2 pagesRL2 CCR Book March-2021-P117-118Judah ObengNo ratings yet
- McqepilipsyDocument3 pagesMcqepilipsyNguyen Anh TuanNo ratings yet
- ThesisDocument30 pagesThesisSimran JosanNo ratings yet
- Akshata Sawant Final Article 1Document16 pagesAkshata Sawant Final Article 1SonuNo ratings yet
- Antimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaDocument9 pagesAntimicrobial Resistance Trends in Bacterial Keratitis Over 5 Years in Sydney, AustraliaBima RizkiNo ratings yet
- Overview of Nephrotic SyndromeDocument19 pagesOverview of Nephrotic Syndromefarmasi_hm100% (1)
- Orthodontic Treatment in Systemic DisordersDocument9 pagesOrthodontic Treatment in Systemic DisordersElizabeth Diaz BuenoNo ratings yet
- OttoDocument13 pagesOttoyoshikaNo ratings yet
- Prosta LacDocument16 pagesProsta LacantoniofacmedNo ratings yet
- Journal of Health Education: Medication Adherence of Tuberculosis Patients in Yogyakarta: A Cross Sectional StudyDocument12 pagesJournal of Health Education: Medication Adherence of Tuberculosis Patients in Yogyakarta: A Cross Sectional StudyDesy AmaliaNo ratings yet
- Pregnancy TestDocument13 pagesPregnancy TestAbdirahman YznNo ratings yet
- Approach To SplenomegalyDocument37 pagesApproach To SplenomegalySarath Menon R100% (1)
- Critical Care Unit / Intensive Care UnitDocument83 pagesCritical Care Unit / Intensive Care Unitpreet kaurNo ratings yet
- Lipid Profile: HDL & LDL CholesterolDocument6 pagesLipid Profile: HDL & LDL CholesterolQasmNo ratings yet
- Acute Limb Ischemia SiteDocument23 pagesAcute Limb Ischemia Sitedokteraan100% (2)
- Efficacy and Safety of Twice Vs Once Daily ALAADocument11 pagesEfficacy and Safety of Twice Vs Once Daily ALAAOmar AyashNo ratings yet
- First Aid For BurnsDocument21 pagesFirst Aid For Burnsgashbin MahdyNo ratings yet
- The Gut Microbiota in Anxiety and Depression - A Systematic Review (Simpson Et Al, 2020)Document18 pagesThe Gut Microbiota in Anxiety and Depression - A Systematic Review (Simpson Et Al, 2020)GokushimakNo ratings yet
- Test Bank For Nursing Assistant A Nursing Process Approach 11th EditionDocument7 pagesTest Bank For Nursing Assistant A Nursing Process Approach 11th EditionLarry Cessor100% (26)
- Adorio Partograph ScenarioDocument2 pagesAdorio Partograph Scenariojonathan liboonNo ratings yet