Professional Documents
Culture Documents
Enthesopathy: Dr. Jufri Latief, SP.B., SP - OT
Uploaded by
rarasly0 ratings0% found this document useful (0 votes)
4 views43 pagesenthesiopathy
Original Title
Dr. Jufri Latief (Enthesiopathy) (Salinan Berkonflik Nisrina__Pc 2016-10-13)
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documententhesiopathy
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views43 pagesEnthesopathy: Dr. Jufri Latief, SP.B., SP - OT
Uploaded by
raraslyenthesiopathy
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 43
Enthesopathy
Dr. Jufri Latief, Sp.B., Sp.OT
BAGIAN ORTOPEDI DAN TRAUMATOLOGI
FAKULTAS KEDOKTERAN UMI
MAKASSAR
What is Enthesopathy?
Enthesopathy is a condition that
affects the entheses (e.g.
inflammation of the entheses).
The entheses are sites of
tendinous or ligamentous
attachment to the bone
Lateral Epicondylitis
(Tennis Elbow)
Tennis elbow is a painful inflammation of the tendon on
the lateral aspect of the elbow, caused by the pull of the
muscles which extend the wrist and fingers.
Signs and symptoms
Pain that radiates from the outside of your elbow into
your forearm and wrist
Pain when you touch or bump the outside of your
elbow
Pain when you extend your wrist
A weak grip
A painful grip during certain activities, such as shaking
hands or turning a doorknob
Risk factors
Repetitive stresses the wrists. Tennis
players, carpenters, gardeners, dentists
and musicians may be at particular risk.
Complications
Left untreated, can result in chronic pain
Treatment
Non operative
• (NSAIDs)
• Rest, ice, and physical therapy.
• Steroid injection
Operative
Medial Epicondylitis
(Golfer's Elbow)
is pain and inflammation on the inner side of the elbow,
where the tendons of the forearm muscles attach to the
bony bump on the inside of the elbow
Signs and symptoms
Pain and tenderness on the inner side of the
elbow. Sometimes the pain extends along the
inner side of the forearm. Your elbow may feel
stiff, and it may hurt to make a fist. You may
have weakness in your hands and wrists.
Risk factors
Repetitive stresses the wrists or fingers.
Complications
Left untreated, golfer's elbow can cause
persistent elbow pain.
Treatment
Non operative
• (NSAIDs)
• Rest, ice, and physical therapy.
• Steroid injection
Operative
STENOSING TENOSYNOVITIS
Inflammation of a synovial tendon
sheath which severely narrows the space
normally required for a tendon to pass
freely through its tunnel and beneath the
pulleys and ligaments
Risk Factors
More common in womenover age 30.
Diabetics.
Repetitive bending of the fingers, thumb
and wrist, gripping and grasping
STENOSING TENOSYNOVITIS
De Quervains Disease
Trigger Fingers
De Quervains Disease
Stenosing tenovaginitis of the first dorsal extensor
compartment
DIAGNOSIS
Local tenderness, pain and swelling
involve thumb
radiation of pain to the thumb and
forearm are frequent.
Positive Finklestein test
De Quervain’s
Treatment
Non operative
• Rest
• steroid injection
• anti-inflamatory
operative
Trigger Fingers
stenosing tenovaginitis of the flexor
tendon sheath(A1 pulley)
Aetiology
congenital (thumb)
• often not recognised until toddlers
• 30% resolve spontaneously
acquired (middle aged)
• idiopathic
• traumatic
• diabetes
• rheumatoid
Signs and symptoms
Affected finger may stiff and may click when move.
A bump (nodule) or tenderness at the base of the affected
finger
Eventually, the finger may not fully straighten.
Treatment
non operative
• Rest.
• Splinting.
• Finger exercises.
• Avoiding repetitive gripping.
• Nonsteroidal anti-inflammatory drugs
operative
Plantar Fasciitis
&
Heel Pain
What is plantar fasciitis?
Plantar fasciitis is an inflammation of the
plantar fascial tissue, often adjacent to its
insertion into the heel. This may be associated
one or more of the following:
• Pain
• Swelling
• Warmth of the affected area
• Redness of the adjacent skin
Anatomy of the Plantar Fascia
The plantar fascia is a
fibrous sheath which
extends from the base
of the toes to the heel.
It runs between the
skin/ subcutaneous
fat, and the deeper
muscles, tendons, and
bones.
Bony Origin of Plantar Fascia
The plantar fascia arises
from the bottom and inside
of the heel bone (medial
calcaneal tuberosity), along
with some of the small
intrinsic muscles of the foot.
Risk factors
Structural abnormality of the lower extremity
Abnormal amount of motion across joints
Abnormal position of bones & joints
Increased levels of activity
Increased body weight
Loss of elasticity in fibrous tissues
Systemic disease (eg. Rheumatic disease)
Plantar fasciitis can occur in
any foot type
It more commonly occurs in both
Flatfoot High Arch
(Pes Planus) (Pes Cavus)
and
What are the symptoms of
Plantar Fasciitis?
Some combination of these are usually present :
Pain on weight bearing Puffiness around the heel
May be sharp, dull or burning Pulling sensation when walking
Often worse on first arising Feels worse in low heeled shoes
Painful first few steps after rest Feels worse in unsupportive shoes
Walking may be painful Symptoms may be long standing
May throb in the evening May increase in severity over time
Tenderness to pressure is found at
one or more locations
Along the central portion of the
sole of the foot
Just in front of the heel and
toward the inside of the foot
Directly beneath the weight
bearing surface of the heel bone.
Most common with a “heel
spur”
Home Care of Plantar fasciitis
Ice the sore area after activit
Stretch the plantar fascia when its not painful
Wear supportive shoes, such as good runners
If tolerated, take over-the-counter anti-inflammatory medication
Treatment
Conservative treatment
• Heel stretching exercises
• Shoe inserts
• Night splints
• NSAIDs
• Steroid injections
Surgery
Rarely surgery is necessary…
There are various techniques to release the plantar fascia from its
attachment to the heel. This procedure is called a Plantar
Fasciotomy. It is reserved for those patients who fail to respond
to more conservative measures.
Achilles tendinitis
Achilles tendinitis is inflammation,
irritation, and swelling of the Achilles
tendon (the tendon that connects the
muscles of the calf to the heel).
Causes
overuse
arthritis
Symptoms
Pain in the heel
Swollen and warm.
Physical examination
Tenderness along the tendon
Pain in the area of the tendon when the
patient stands on their toes.
Treatment
Non operative
• (NSAIDs)
• Rest, ice, and physical therapy.
• Steroid injection
Operative
Dupuytren’s Contracture
nodular hypertrophy and contracture of the palmar fascia
Dupuytren’s Contracture
aetiology
genetic
geographical
smoking
alcohol
epilepsy
Dupuytren’s Contracture
clinical
middle aged
male 10 x female
nodular thickening in the palm
contracture of the ring and little finger
MCPJ and/or IPJ not DIPJ
Dupuytren’s Contracture
treatment
Surgery if :
rapidly progressive contracture
inconvenience
Thank You
You might also like
- Dr. Jenal (Enthesiopathy)Document37 pagesDr. Jenal (Enthesiopathy)Sadam_fasterNo ratings yet
- Plantar Fasciitis Exercises and Home TreatmentFrom EverandPlantar Fasciitis Exercises and Home TreatmentRating: 5 out of 5 stars5/5 (3)
- Plantas Fascitis FinalDocument23 pagesPlantas Fascitis Finalasraf amirullahNo ratings yet
- A Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Extensor Tendonitis, Diagnosis, Treatment and Related ConditionsNo ratings yet
- What Is Achilles Tendon Rupture?Document8 pagesWhat Is Achilles Tendon Rupture?Santok ChoirulNo ratings yet
- Soft Tissue Disorders and Fibromyalgia: Jaya Ravindran Consultant RheumatologistDocument54 pagesSoft Tissue Disorders and Fibromyalgia: Jaya Ravindran Consultant RheumatologistarunupadhayaNo ratings yet
- Massage PowerpoingDocument11 pagesMassage Powerpoingapi-550556129No ratings yet
- HeelDocument4 pagesHeelDoha EbedNo ratings yet
- Calcaneal SpurDocument19 pagesCalcaneal SpurucssNo ratings yet
- ACR Presentation-1Document37 pagesACR Presentation-1STARSHIPSNo ratings yet
- Created by Hanna H. Presented For Dr. Ryan Lambert Bellacov, Chiropractor in West Linn, ORDocument9 pagesCreated by Hanna H. Presented For Dr. Ryan Lambert Bellacov, Chiropractor in West Linn, ORIrene Sulinsia NapitupuluNo ratings yet
- Group 5Document70 pagesGroup 5Kathlene PamaNo ratings yet
- Dinah Hernandez MSN, PHN, RNDocument31 pagesDinah Hernandez MSN, PHN, RNMourian AmanNo ratings yet
- Precipitating FactorsDocument2 pagesPrecipitating FactorsCake ManNo ratings yet
- TendonitisDocument3 pagesTendonitisJingyi Xie0% (1)
- FeetDocument47 pagesFeetChandradatNo ratings yet
- Top of The Foot Pain and Swelling TreatmentDocument13 pagesTop of The Foot Pain and Swelling TreatmentNyanLinKyawNo ratings yet
- Prof. Dr. Widiastuti Samekto, Pak, Sps (K), MSCDocument34 pagesProf. Dr. Widiastuti Samekto, Pak, Sps (K), MSCLia AngelineNo ratings yet
- Posterior Tibial Tendon DysfunctionDocument2 pagesPosterior Tibial Tendon Dysfunctionvisa12345No ratings yet
- DG - Achilles TendinopathyDocument3 pagesDG - Achilles TendinopathyKoyasanNo ratings yet
- Tarsal Tunnel SyndromDocument12 pagesTarsal Tunnel SyndromV sNo ratings yet
- Exercise-Induced Leg Pain: Acsm Sports Medicine BasicsDocument2 pagesExercise-Induced Leg Pain: Acsm Sports Medicine BasicsNelson GarzonNo ratings yet
- Assignment of Biomechanics and ErgonomicsDocument13 pagesAssignment of Biomechanics and Ergonomicsmuhammadhamza muhammadiqbalNo ratings yet
- Carpal Tunnel Syndrome GuideDocument21 pagesCarpal Tunnel Syndrome Guiderudresh singhNo ratings yet
- CFTS-Common Foot PathologiesDocument18 pagesCFTS-Common Foot PathologiesCristi DanNo ratings yet
- Athritis, Kelainan Regional Jaringan Ikat Sendi, Infeksi Sendi Dan Kelainan Metabolik Tulang Dan SendiDocument85 pagesAthritis, Kelainan Regional Jaringan Ikat Sendi, Infeksi Sendi Dan Kelainan Metabolik Tulang Dan SendiamaliakhaNo ratings yet
- TenosynovitisDocument14 pagesTenosynovitisHimasree SagarikaNo ratings yet
- Dr. Abdul Rashad Senior Lecturer DPT, Mphill (Opt) Mppta United College of Physical TherapyDocument32 pagesDr. Abdul Rashad Senior Lecturer DPT, Mphill (Opt) Mppta United College of Physical Therapypasha100% (1)
- Bursitis/Tendinitis: DR M Arman Nasution SPPDDocument197 pagesBursitis/Tendinitis: DR M Arman Nasution SPPDdiah stanyaNo ratings yet
- Periarticular Disorders of ExtremitiesDocument59 pagesPeriarticular Disorders of Extremitiesskin_docNo ratings yet
- Planter Fasciitis: Biomechanical AetiologyDocument7 pagesPlanter Fasciitis: Biomechanical AetiologyMohan JoshiNo ratings yet
- Running Injuries: Prevention and RehabilitationDocument41 pagesRunning Injuries: Prevention and RehabilitationJose Redondo CamposNo ratings yet
- MOST COMMON MSD On The WorkplaceDocument38 pagesMOST COMMON MSD On The WorkplaceAbdulrahman Salim ZgamaNo ratings yet
- Neuromusculosklatal Disorders FK UnayaDocument62 pagesNeuromusculosklatal Disorders FK UnayaSuci MayveraNo ratings yet
- RHEUMATOLOGY PHYSICAL EXAM GUIDEDocument7 pagesRHEUMATOLOGY PHYSICAL EXAM GUIDERohit SharmaNo ratings yet
- Tendonitis Guide - Causes, Symptoms and Treatment OptionsDocument6 pagesTendonitis Guide - Causes, Symptoms and Treatment OptionsSylvia GraceNo ratings yet
- Chronical Injuries ofDocument45 pagesChronical Injuries ofapi-19916399No ratings yet
- Safety Measures and Management of Sports Injuries: Dr. Vida C. Suganob Medical Officer Iii 4/11/2019Document56 pagesSafety Measures and Management of Sports Injuries: Dr. Vida C. Suganob Medical Officer Iii 4/11/2019Darien Nova AcusarNo ratings yet
- Common Foot ProblemsDocument3 pagesCommon Foot ProblemsBryan QuebralNo ratings yet
- Musculoskeletal DisordersDocument40 pagesMusculoskeletal DisordersRajalakshmi ShenoyNo ratings yet
- Best Homeopathic Remedies for Knee PainDocument29 pagesBest Homeopathic Remedies for Knee PainKrish MotupalliNo ratings yet
- Tarsal Tunnel SyndromeDocument2 pagesTarsal Tunnel Syndromeannisa shezanNo ratings yet
- Achilles TendinitisDocument10 pagesAchilles TendinitisS MediaNo ratings yet
- PLANTAR FASCIITIS AND HEEL PAIN GUIDEDocument6 pagesPLANTAR FASCIITIS AND HEEL PAIN GUIDECinthia Christina DewiNo ratings yet
- Knee OA & TFDocument17 pagesKnee OA & TFShabana AfzalNo ratings yet
- Symptoms and Signs of Musculoskeletal DisordersDocument70 pagesSymptoms and Signs of Musculoskeletal DisordersErde NmuNo ratings yet
- Peripheral Nerve Disorders ReviewDocument66 pagesPeripheral Nerve Disorders ReviewReno Andri0% (1)
- Physiotherapy in Portage La Prairie and Emerald Park For FootDocument11 pagesPhysiotherapy in Portage La Prairie and Emerald Park For Footdrrabe3No ratings yet
- Pe of The Joint - GoutDocument50 pagesPe of The Joint - GoutCharisse Ann GasatayaNo ratings yet
- Relieve Ball of Foot Pain with Metatarsalgia TreatmentDocument18 pagesRelieve Ball of Foot Pain with Metatarsalgia TreatmentKapil LakhwaraNo ratings yet
- Heel Pain Caused by Plantar FasciitisDocument2 pagesHeel Pain Caused by Plantar FasciitisConstantin BorsNo ratings yet
- Common Foot and Ankle ProblemsDocument62 pagesCommon Foot and Ankle ProblemsYasmeen Bibi100% (1)
- Calcaneal SpursDocument10 pagesCalcaneal Spurskrishnamoorthy abiramanNo ratings yet
- De Quervain's TendinosisDocument19 pagesDe Quervain's TendinosisSze Wing LeeNo ratings yet
- Accessory Navicular SyndromeDocument3 pagesAccessory Navicular SyndromeTojiNo ratings yet
- Tarsal Tunnel SyndromeDocument2 pagesTarsal Tunnel SyndromeAtang KusmanNo ratings yet
- Bursitis-Tendonitis-Dr - Amit PatelDocument52 pagesBursitis-Tendonitis-Dr - Amit PatelAmitNo ratings yet
- De Quervain's TendinosisDocument19 pagesDe Quervain's TendinosisSze Wing LeeNo ratings yet
- Tarsal Tunnel SyndromeDocument18 pagesTarsal Tunnel Syndromeramadhanadlansyah7No ratings yet
- Neuroleptic Malignant SyndromeDocument7 pagesNeuroleptic Malignant SyndromeraraslyNo ratings yet
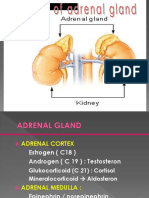
- CushingDocument67 pagesCushingraraslyNo ratings yet
- Bone Marrow Hematopoiesis: Formation of Blood CellsDocument44 pagesBone Marrow Hematopoiesis: Formation of Blood Cellsviviyanti znNo ratings yet
- Pedoman Penulisan KTI PDFDocument60 pagesPedoman Penulisan KTI PDFraraslyNo ratings yet
- Eye TreatmentDocument14 pagesEye Treatmentsk sharmaNo ratings yet
- Etiology, Prevalence, and Treatment of Dry Eye Disease: Clinical Ophthalmology DoveDocument8 pagesEtiology, Prevalence, and Treatment of Dry Eye Disease: Clinical Ophthalmology DoveraraslyNo ratings yet
- Oksitoksin Dan EndotoksinDocument1 pageOksitoksin Dan EndotoksinraraslyNo ratings yet
- Review ArticleDocument13 pagesReview ArticleJessica Alexandria WuNo ratings yet
- Pasan Ko Ang DaigdigDocument1 pagePasan Ko Ang DaigdigJermaine Rae Arpia Dimayacyac0% (1)
- Afsm 2011Document4 pagesAfsm 2011Rakshit SehgalNo ratings yet
- The Financial ExpertDocument16 pagesThe Financial ExpertVinay Vishwakarma0% (1)
- Recommended Curriculum: Seven (7) Types of CurriculumDocument1 pageRecommended Curriculum: Seven (7) Types of CurriculummoyesaNo ratings yet
- Friedan Explores "Problem With No NameDocument13 pagesFriedan Explores "Problem With No NameRoxana Daniela AjderNo ratings yet
- Workforce Plan 20xx-20xxDocument22 pagesWorkforce Plan 20xx-20xxRani EndarweniNo ratings yet
- Herbal Cosmetics: Used For Skin and Hair: December 2012Document8 pagesHerbal Cosmetics: Used For Skin and Hair: December 2012Mas NuriNo ratings yet
- Cs504-Midterm Solved Subjective With Refrences by Moaaz PDFDocument14 pagesCs504-Midterm Solved Subjective With Refrences by Moaaz PDFSijjusha100% (1)
- Review Center Association of The Philippines vs. Ermita 583 SCRA 428, April 02, 2009, G.R. No. 180046Document2 pagesReview Center Association of The Philippines vs. Ermita 583 SCRA 428, April 02, 2009, G.R. No. 180046Almer Tinapay100% (1)
- 2nd EditionDocument93 pages2nd EditionDhandapani NagarajanNo ratings yet
- Cold War Irma MartinezDocument11 pagesCold War Irma Martinezapi-244604538No ratings yet
- Education and Social ChangeDocument13 pagesEducation and Social ChangeBert M DronaNo ratings yet
- Echocardiography in Congenital Heart Disease - Expert Consult - Online and Print, 1e (Practical Echocardiography)Document239 pagesEchocardiography in Congenital Heart Disease - Expert Consult - Online and Print, 1e (Practical Echocardiography)Sofia OliveiraNo ratings yet
- Engineering Prob & Stat Lecture Notes 6Document12 pagesEngineering Prob & Stat Lecture Notes 6EICQ/00154/2020 SAMUEL MWANGI RUKWARONo ratings yet
- 0607 s14 Ms 43Document6 pages0607 s14 Ms 43wizard guyNo ratings yet
- 1 Thomas Hardy - Hap PDFDocument1 page1 Thomas Hardy - Hap PDFVirág KovácsNo ratings yet
- Chapter9E2010 PDFDocument29 pagesChapter9E2010 PDFmariahx91No ratings yet
- Cir vs. GJM 202695Document1 pageCir vs. GJM 202695magenNo ratings yet
- Perceived Benefits and Costs of Romantic Relationships For Young People Differences by Adult Attachment Style PDFDocument19 pagesPerceived Benefits and Costs of Romantic Relationships For Young People Differences by Adult Attachment Style PDFValejahNo ratings yet
- Feminine Beauty, National Identity and Political Conflict in Postwar ItalyDocument21 pagesFeminine Beauty, National Identity and Political Conflict in Postwar ItalyHugyecz DorinaNo ratings yet
- Employees' Adaptability and Perceptions of Change-Related Uncertainty: Implications For Perceived Organizational Support, Job Satisfaction, and PerformanceDocument12 pagesEmployees' Adaptability and Perceptions of Change-Related Uncertainty: Implications For Perceived Organizational Support, Job Satisfaction, and PerformancesatirgNo ratings yet
- Remedial Law 2020 Atty. EsguerraDocument420 pagesRemedial Law 2020 Atty. Esguerrarokszie80% (10)
- James Et Al-2017-Earth Surface Processes and LandformsDocument20 pagesJames Et Al-2017-Earth Surface Processes and Landformsqwerrty1029384756No ratings yet
- Andrew Balkin - CapstoneDocument147 pagesAndrew Balkin - CapstoneTrần Tâm PhươngNo ratings yet
- Thiruppugal Pathigam - Song 923 ("Madhi-Yālvi - Thagan-Āgi")Document7 pagesThiruppugal Pathigam - Song 923 ("Madhi-Yālvi - Thagan-Āgi")apjbalamuruganNo ratings yet
- NP Performance Appraisal Sample PDFDocument2 pagesNP Performance Appraisal Sample PDFHamss Ahmed80% (5)
- Lesson PlanDocument3 pagesLesson Planapi-479604636No ratings yet
- A Literature Survey On The Accuracy of Software Effort Estimation ModelsDocument6 pagesA Literature Survey On The Accuracy of Software Effort Estimation Modelsutkarsh sharmaNo ratings yet
- CLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 pagesCLASIFICACION RESUMEN Caton - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasNo ratings yet
- Change Management PresentationDocument15 pagesChange Management PresentationAshu AyshaNo ratings yet