Professional Documents
Culture Documents
Resuscitation Newborn
Uploaded by
Poonam Rana0 ratings0% found this document useful (0 votes)
9 views23 pagesOriginal Title
resuscitation newborn
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views23 pagesResuscitation Newborn
Uploaded by
Poonam RanaCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 23
IMMEDIATE MANAGEMENT
Three situations require immediate management:
gasping or not breathing (below), cyanosis (blueness)
or breathing with difficulty .
GASPING OR NOT BREATHING
GENERAL MANAGEMENT
• Dry the baby, remove the wet cloth and wrap the baby
in a dry, warm cloth.
• Clamp and cut the cord immediately if not already
done.
• Move the baby to a firm, warm surface under a radiant
heater for resuscitation.
• Observe standard infection prevention practices when
caring for and resuscitating a newborn .
RESUSCITATION
1. Resuscitation equipment
To avoid delays during an emergency situation, it is vital
to ensure that equipment is in good condition before
resuscitation is needed:
• Have the appropriate size masks available according to
the expected size of the baby (size 1 for a normal weight
newborn and size 0 for a small newborn).
• Block the mask by making a tight seal with the palm of
your hand and squeeze the bag:
-If you feel pressure against your hand, the bag is
generating adequate pressure.
- If the bag reinflates when you release the grip, the bag
is functioning properly.
2. OPENING THE AIRWAY
Position the newborn
• Place the baby on its back.
• Position the head in a slightly extended position
to open the airway.
• Keep the baby wrapped or covered, except for
the face and upper chest.
• Clear the airway by suctioning first the mouth
and then the nostrils. If blood or meconium is in
the baby's mouth or nose, suction immediately to
prevent aspiration.
Note: Do not suction deep in the throat as this may
cause the baby's heart to slow or the baby may stop
breathing.
• Reassess the baby:
- If the newborn starts crying or breathing, no
further immediate action is needed. Proceed with
initial care of the newborn
• If the baby is still not breathing, start
ventilating .
FIGURE: Correct position of the head for
ventilation; note that the neck is less extended than
in adults
3. VENTILATING THE NEWBORN
Recheck the newborn's position. The neck should
be slightly extended .
Position the mask and check the seal.
Place the mask on the newborn's face. It should
cover the chin, mouth and nose;
Form a seal between the mask and the face;
Squeeze the bag with two fingers only or with
the whole hand, depending on the size of the
bag;
Check the seal by ventilating twice and
observing the rise of the chest.
Once a seal is ensured and chest movement is
present, ventilate the newborn. Maintain the
correct rate (approximately 40 breaths per minute)
and pressure (observe the chest for an easy rise and
fall):
• If the baby's chest is rising, ventilation pressure is
probably adequate;
• If the baby's chest is not rising:
-Repeat suction of mouth and nose to remove mucus,
blood or meconium from the airway.
-Recheck and correct, if necessary, the position of
the newborn .
-Reposition the mask on the baby's face to improve
the seal between mask and face;
-Squeeze the bag harder to increase ventilation
pressure.
• Ventilate for 1 minute and then stop and quickly
assess if the newborn is breathing spontaneously:
• If breathing is normal (30-60 breaths per minute)
and there is no indrawing of the chest and no
grunting for 1 minute, no further resuscitation is
needed. Proceed with initial care of the newborn.
• If the newborn is not breathing, or the breathing
is weak, continue ventilating until spontaneous
breathing begins.
• Ventilation with bag and mask
• If the newborn starts crying, stop ventilating and
continue observing breathing for 5 minutes after
crying stops:
• If breathing is normal (30-60 breaths per minute)
and there is no indrawing of the chest and no
grunting for 1 minute, no further resuscitation is
needed. Proceed with initial care of the newborn.
• If the respiratory rate is less than 30 breaths per
minute, continue ventilating;
• If there is severe indrawing of the chest, ventilate
with oxygen, if available. Arrange to transfer the
baby to the most appropriate service for the care of
sick newborns.
• If the newborn is not breathing regularly after
20 minutes of ventilation:
-Transfer the baby to the most appropriate service
for the care of sick newborns;
-During the transfer, keep the newborn warm and
ventilated, if necessary.
-If there is no gasping or breathing at all after 20
minutes of ventilation, stop ventilating; the baby is
stillborn.
- Provide emotional support to the family
CARE AFTER SUCCESSFUL RESUSCITATION
Prevent heat loss:
• Place the baby skin-to-skin on the mother's chest
and cover the baby's body and head;
• Alternatively, place the baby under a radiant heater.
• Examine the newborn and count the number of
breaths per minute:
• If the baby is cyanotic (bluish) or is having
difficulty breathing (less than 30 or more than 60
breaths per minute, indrawing of the chest or
grunting), give oxygen by nasal catheter.
Measure the baby's axillary temperature:
• If the temperature is 36.5°C or more, keep the
baby skin-to- skin on the mother's chest and
encourage breastfeeding;
• If the temperature is less than 36.5°C, rewarm
the baby.
• Encourage the mother to begin breastfeeding. A
newborn that required resuscitation is at higher
risk of developing hypoglycaemia:
• If suckling is good, the newborn is recovering
well;
• If suckling is not good, transfer the baby to the
appropriate service for the care of sick newborns.
• Ensure frequent monitoring of the newborn
during the next 24 hours. If signs of breathing
difficulties recur, arrange to transfer the baby to
the most appropriate service for the care of sick
newborns.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Types of Volcanoes - ShapeDocument2 pagesTypes of Volcanoes - ShapejeffersonNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Psycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsDocument29 pagesPsycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsPoonam RanaNo ratings yet
- Somatoform Disorders 2019Document91 pagesSomatoform Disorders 2019Poonam RanaNo ratings yet
- Additional Character OptionsDocument30 pagesAdditional Character Optionsdreaming geckoNo ratings yet
- Cae Grammar TensesDocument4 pagesCae Grammar TensesYana MarinkovaNo ratings yet
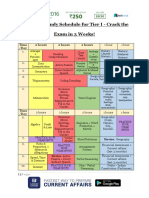
- SSC CHSL Study Schedule For Tier I - Crack The Exam in 3 Weeks!Document3 pagesSSC CHSL Study Schedule For Tier I - Crack The Exam in 3 Weeks!Tushita80% (15)
- Premature Rupture of MembraneDocument15 pagesPremature Rupture of MembranePoonam RanaNo ratings yet
- Pierre Jeanneret Private ResidencesDocument21 pagesPierre Jeanneret Private ResidencesKritika DhuparNo ratings yet
- Obstetric Haemorrhage: EsmoeDocument40 pagesObstetric Haemorrhage: EsmoePoonam RanaNo ratings yet
- Cisco Start CatalogDocument4 pagesCisco Start CatalogqntttNo ratings yet
- History Taking & MSE PsychiatricDocument10 pagesHistory Taking & MSE PsychiatricPoonam RanaNo ratings yet
- Anorexia NervosaDocument5 pagesAnorexia NervosaPoonam RanaNo ratings yet
- StressDocument23 pagesStressPoonam RanaNo ratings yet
- Psychosomatic DisordersDocument11 pagesPsychosomatic DisordersPoonam RanaNo ratings yet
- RehabDocument105 pagesRehabPoonam RanaNo ratings yet
- National Medical College Nursing Campus: (Affiliated To Tribhuwan University) Birgunj, ParsaDocument3 pagesNational Medical College Nursing Campus: (Affiliated To Tribhuwan University) Birgunj, ParsaPoonam RanaNo ratings yet
- Counseling VsDocument4 pagesCounseling VsPoonam RanaNo ratings yet
- 1 Frederick WDocument6 pages1 Frederick WPoonam RanaNo ratings yet
- Stress, Anxiety and Depression Among Adolescents in Secondary School of ButwalDocument6 pagesStress, Anxiety and Depression Among Adolescents in Secondary School of ButwalPoonam RanaNo ratings yet
- BioethicsDocument22 pagesBioethicsPoonam RanaNo ratings yet
- Functional Psychosis: Characterized by Disturbances in Thinking, EmotionDocument33 pagesFunctional Psychosis: Characterized by Disturbances in Thinking, EmotionPoonam RanaNo ratings yet
- Ebola Virus DiseaseDocument3 pagesEbola Virus DiseasePoonam RanaNo ratings yet
- Post-Term PregnancyDocument21 pagesPost-Term PregnancyPoonam RanaNo ratings yet
- Epidemiology-I 2021 (STD Copy)Document42 pagesEpidemiology-I 2021 (STD Copy)Poonam RanaNo ratings yet
- Dr. S.K.SDocument29 pagesDr. S.K.SPoonam RanaNo ratings yet
- Amniotic Fluid Embolism: Women's Hospital School of Medicine Zhejiang Un Iversity Wang ZhengpingDocument19 pagesAmniotic Fluid Embolism: Women's Hospital School of Medicine Zhejiang Un Iversity Wang ZhengpingPoonam RanaNo ratings yet
- Pediatric Nursing 6th Class 2078Document67 pagesPediatric Nursing 6th Class 2078Poonam RanaNo ratings yet
- Meconium Stained Amniotic FluidDocument21 pagesMeconium Stained Amniotic FluidPoonam RanaNo ratings yet
- Shock in The Obstetric Patient: William Schnettler, MD FacogDocument42 pagesShock in The Obstetric Patient: William Schnettler, MD FacogPoonam RanaNo ratings yet
- Mechanism of Labour in Breech: Amarendra B. Singh 090201263Document15 pagesMechanism of Labour in Breech: Amarendra B. Singh 090201263Poonam RanaNo ratings yet
- 1st Internal Assessment: Marks Marks RN Students Name Midwifery III Child Health NursingDocument4 pages1st Internal Assessment: Marks Marks RN Students Name Midwifery III Child Health NursingPoonam RanaNo ratings yet
- Joshi Abhishek F.Y.P.B.B.SC - Nursing Govt College of Nursing JamnagarDocument49 pagesJoshi Abhishek F.Y.P.B.B.SC - Nursing Govt College of Nursing JamnagarPoonam RanaNo ratings yet
- Pass Out CertificateDocument1 pagePass Out CertificatePoonam RanaNo ratings yet
- Bio-Stat Class 2 and 3Document58 pagesBio-Stat Class 2 and 3Poonam RanaNo ratings yet
- Geriatric Nursing First ClassDocument45 pagesGeriatric Nursing First ClassPoonam RanaNo ratings yet
- Gastrointestinal Disorder (3 Class) : 07/13/2021 Ms. Abja Sapkota 1Document40 pagesGastrointestinal Disorder (3 Class) : 07/13/2021 Ms. Abja Sapkota 1Poonam RanaNo ratings yet
- Japanese ScriptDocument67 pagesJapanese ScriptBrat_princeNo ratings yet
- Vienza: Lighting and SecurityDocument4 pagesVienza: Lighting and SecurityShadi AbdelsalamNo ratings yet
- Week 1Document15 pagesWeek 1Jamaica AlejoNo ratings yet
- Refrigeration Technology: SymbolsDocument44 pagesRefrigeration Technology: SymbolsGaluh AjengNo ratings yet
- 2006 Amc8Document12 pages2006 Amc8Yuhang HeNo ratings yet
- Normalization ExercisesDocument2 pagesNormalization ExercisesAnh DiệuNo ratings yet
- 2023 - Ver4.3 - Landslide Assessments in British Columbia Version 4.1Document184 pages2023 - Ver4.3 - Landslide Assessments in British Columbia Version 4.1yehnafarNo ratings yet
- Tugas BingDocument10 pagesTugas BingAmelasNo ratings yet
- Pointy Hat - The Cowboy - Ranger ConclaveDocument5 pagesPointy Hat - The Cowboy - Ranger Conclave678ojyhiopNo ratings yet
- Background: The Islamic World of Academy of ScienceDocument5 pagesBackground: The Islamic World of Academy of ScienceNusrat MaqboolNo ratings yet
- Deutscher National-KatechismusDocument3 pagesDeutscher National-KatechismusitsgabbywanNo ratings yet
- An Introduction To Uhde Oil & Gas: Thyssenkrupp Uhde - Engineering With IdeasDocument40 pagesAn Introduction To Uhde Oil & Gas: Thyssenkrupp Uhde - Engineering With IdeasHany FathyNo ratings yet
- Providing Technical Support and Essential Supplies: Asia Pacific Strategy For Emerging Diseases (APSED)Document2 pagesProviding Technical Support and Essential Supplies: Asia Pacific Strategy For Emerging Diseases (APSED)Legal Affairs OfficeNo ratings yet
- Communityhealth 141122094330 Conversion Gate02Document22 pagesCommunityhealth 141122094330 Conversion Gate02Titser JoNo ratings yet
- Present Perfect TestDocument6 pagesPresent Perfect TestMárta FábiánNo ratings yet
- General Rules ICT Lab Rules PE & Gym RulesDocument1 pageGeneral Rules ICT Lab Rules PE & Gym Rulestyler_froome554No ratings yet
- Global Forecasts DiscussionDocument10 pagesGlobal Forecasts DiscussionkareemarfaNo ratings yet
- Presentation On Modal Auxiliary VerbsDocument18 pagesPresentation On Modal Auxiliary VerbsAbdelhafid ZaimNo ratings yet
- CW-80 ManualDocument12 pagesCW-80 ManualBrian YostNo ratings yet
- Practice Paper 1 Class X Social Science Time 3 Hrs. M.M 80 General InstructionsDocument6 pagesPractice Paper 1 Class X Social Science Time 3 Hrs. M.M 80 General Instructionsvvs .b.s1453No ratings yet
- Business Income Calculation UdomDocument23 pagesBusiness Income Calculation UdomMaster Kihimbwa100% (1)
- The Wise Old WomenDocument2 pagesThe Wise Old WomenLycoris FernandoNo ratings yet
- Culture and CraftDocument27 pagesCulture and CraftFreya UmelNo ratings yet
- Charmed - 3x13 - Bride and Gloom - enDocument50 pagesCharmed - 3x13 - Bride and Gloom - enGa ConNo ratings yet