Professional Documents
Culture Documents
Necrotizing Pneumonia and Lung Abscess
Uploaded by
Iman Khan0 ratings0% found this document useful (0 votes)
9 views11 pagesThis document provides information on various types of pneumonia and the microorganisms that commonly cause them. It discusses aspiration pneumonia caused by oral flora including anaerobic bacteria. Necrotizing pneumonia is associated with anaerobes like Bacteroides as well as Staphylococcus aureus. Pneumonia in immunocompromised patients can be caused by opportunistic pathogens like Pneumocystis jiroveci or Mycobacterium avium-intracellulare. Common bacterial causes of pneumonia include Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Klebsiella pneumoniae, and Legionella pneumophila. Viruses such as influenza
Original Description:
Original Title
Lung
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides information on various types of pneumonia and the microorganisms that commonly cause them. It discusses aspiration pneumonia caused by oral flora including anaerobic bacteria. Necrotizing pneumonia is associated with anaerobes like Bacteroides as well as Staphylococcus aureus. Pneumonia in immunocompromised patients can be caused by opportunistic pathogens like Pneumocystis jiroveci or Mycobacterium avium-intracellulare. Common bacterial causes of pneumonia include Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Klebsiella pneumoniae, and Legionella pneumophila. Viruses such as influenza
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views11 pagesNecrotizing Pneumonia and Lung Abscess
Uploaded by
Iman KhanThis document provides information on various types of pneumonia and the microorganisms that commonly cause them. It discusses aspiration pneumonia caused by oral flora including anaerobic bacteria. Necrotizing pneumonia is associated with anaerobes like Bacteroides as well as Staphylococcus aureus. Pneumonia in immunocompromised patients can be caused by opportunistic pathogens like Pneumocystis jiroveci or Mycobacterium avium-intracellulare. Common bacterial causes of pneumonia include Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Klebsiella pneumoniae, and Legionella pneumophila. Viruses such as influenza
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 11
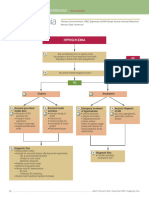
ASPIRATION PNEUMONIA NECROTIZING PNEUMONIA AND LUNG
Anaerobic oral flora (Bacteroides, Prevotella, ABSCESS
Fusobacterium,
Anaerobic bacteria (extremely common),
Peptostreptococcus), admixed with aerobic with or without mixed aerobic infection
bacteria
(Streptococcus pneumoniae, Staphylococcus Staphylococcus aureus, Klebsiella
aureus, pneumoniae, Streptococcus pyogenes
Haemophilus infl uenzae, and Pseudomonas PNEUMONIA IN THE
aeruginosa) IMMUNOCOMPROMISED HOST
CHRONIC PNEUMONIA Cytomegalovirus
Nocardia
Actinomyces
Pneumocystis jiroveci
Granulomatous: Mycobacterium tuberculosis Mycobacterium avium-intracellulare
and atypical Invasive aspergillosis
mycobacteria, Histoplasma capsulatum,
Coccidioides Invasive candidiasis
immitis, Blastomyces dermatitidis “Usual” bacterial, viral, and fungal organisms
(listed above)
Streptococcus pneumoniae
Most common cause of community-acquired acute pneumonia.
Examination of Gram-stained sputum; numerous
neutrophils containing the typical gram-positive, lancet shaped
diplococci S. pneumoniae is a part of the endogenous flora in 20% of
adults
In the early phase of illness, only 20% to 30% of patients have
positive blood cultures)
Pneumococcal vaccines containing capsular polysaccharides from the
common serotypes
Influenzavirus
• Type A viruses are most often involved.
• Hemagglutinins bind virus to cell receptors in the nasal passages
• Neuraminidase dissolves mucus and facilitates release of viral particles
• Influenza A produces worldwide epidemics. Pneumonia may be complicated by a superimposed bacterial pneumonia (usually Staphylococcus aureus).
• Influenza B causes major outbreaks.
• Antigen drift: minor mutation. Does not require new vaccine.
• Antigen shift: major mutation in hemagglutinin or neuraminidase. A new vaccine is required.
• Clinical: fever, headache, cough, myalgias, chest pain
• Vaccination: mandatory for people >65 yr old and people with chronic illnesses
• Associations: Reye syndrome with salicylate ingestion; Guillain-Barré syndrome
• Diagnosis: PCR
Rubeola
• Fever, cough, conjunctivitis, and excessive nasal mucus production
• Koplik spots in the mouth precede onset of the rash.
• Warthin-Finkeldey multinucleated giant cells are a characteristic finding
• Diagnosis: PCR
RSV • Most common cause of pneumonia and bronchiolitis (wheezing) in infants
• Infections primarily occur in winter.
• Causes otitis media in older children
• Hand washing and use of gloves prevents nosocomial outbreaks in nurseries
• Fusion protein causes cells to fuse, producing multinucleated giant cells.
• Rapid diagnosis by detection of antigen in nasopharyngeal wash. PCR is also useful for diagnosis.
SARS
• Develop severe respiratory infection
• Diagnose with viral detection by PCR assay or detection of antibodies
• Detection viral genome, PCR, ELISA
Chlamydia
Chlamydophila pneumoniae
• Second most common cause of atypical pneumonia
• Diagnosis: PCR
Chlamydia trachomatis
• Newborn pneumonia (passage through birth canal)
• Afebrile, staccato cough (choppy cough), conjunctivitis, and wheezing
• Diagnosis: PCR
Mycoplasma pneumoniae
• Most common cause of interstitial pneumonia
• Common in adolescents and military recruits (closed spaces)
• Risk factor for Guillain-Barré syndrome
• Insidious onset with low-grade fever
• Cold agglutinins in blood
• Complications: bullous myringitis, cold autoimmune hemolytic anemia caused by anti IgM antibodies
• Diagnosis: PCR
Coxiella burnetii • Usually transmitted without a vector
• Contracted by dairy farmers, veterinarians
• Associated with the birthing process of infected sheep, cattle, and goats and handling of milk or excrement
• Atypical pneumonia, myocarditis, granulomatous hepatitis
• Diagnosis: PCR
Streptococcus pneumoniae
• Gram-positive lancet-shaped diplococcus
• Most common cause of typical community-acquired pneumonia (50%–75%)
• Rapid onset, productive cough, signs of consolidation
• Urine antigen test is an excellent screen.
Staphylococcus aureus
• Gram-positive cocci in clumps
• Yellow sputum
• Commonly superimposed on influenza pneumonia and measles pneumonia
• Major lung pathogen in CF and IV drug abusers
• Accounts for 3%–5% of community-acquired pneumonias
• Hemorrhagic pulmonary edema, abscess formation, and pneumatoceles (thin-walled air-filled cysts that
develop in the lung parenchyma, usually after pneumonia;
• Diagnosis: culture, antigen detection, PCR
Corynebacterium diphtheriae
• Gram-positive rod
• Toxin inhibits protein synthesis by ADP ribosylation of elongation factor 2 involved in protein synthesis
• Toxin also impairs β-oxidation of fatty acids in the heart (myocarditis with fatty change).
• Toxin-induced pseudomembranous inflammation produces shaggy gray membranes in the oropharynx
and trachea; toxic myocarditis (death).
• Diagnosis: culture, PCR
Bacillus anthracis
• Gram-positive rod
• Habitat: soil
• Capsule inhibits phagocytosis
• Exotoxins: protective antigen (PA), edema factor (EF; activates adenylate cyclase), and lethal factor (LF; inhibits a signal transduction protein
involved in cell division).
• Transmission: direct contact with animal skins or products (most commonly sheep and cattle) and entry of the organisms
through abrasions or cuts; inhalation (use in germ warfare)
• Cutaneous anthrax (90%–95% of cases): occurs through direct contact with infected or contaminated animal products. Resembles insect bite but
eventually swells to form a black scab, or eschar, with a central area of necrosis (malignant pustule). If left untreated, death occurs in 20% of patients.
• Pulmonary anthrax: “first sign of the disease is death.” It is contracted by inhalation of spores that are present incontaminated hides or delivered by
biological weapons. Produces a necrotizing pneumonia, meningitis, and pronounced splenomegaly. It disseminates throughout the rest of the body,
leading to death.
• Prevention: A vaccine is available for high-risk patients (e.g., veterinarians, soldiers entering developing countries).
• Diagnosis: culture, PCR
Actinomyces israelii
• Gram-positive filamentous bacteria. Strict anaerobe. Present in normal flora in the tonsils and adenoids.
• Produces draining sinuses in the jaw, abscesses in chest cavity, and abdomen. Pus contains sulfur granules (yellow specks) that contain the bacteria.
• Diagnosis: gram stain, culture
Nocardia asteroides
• Gram-positive filamentous bacteria. Strict aerobe. Partially acid fast.
• Produces granulomatous microabscesses in the lungs
• Frequently disseminates to the CNS and kidneys
• Diagnosis: culture, antibody detection
Bacteria gram-negative
Bordetella pertussis
• Gram-negative rod
• Pili attach to cilia in the upper respiratory tract. Toxin stimulates adenylate cyclase, which catalyzes the addition of ADP
ribose to the inhibitory subunit of the G protein complex. Toxin also produces absolute lymphocytosis (normal-appearing
lymphocytes) often in leukemoid reaction range.
• Produces whooping cough. Transmitted by droplet infection.
• Catarrhal phase: lasts 1–2 weeks. Mild coughing, rhinorrhea, and conjunctivitis.
• Paroxysmal coughing phase: lasts 2–5 weeks. Characteristic 4–5 coughs in succession on expiration, followed by an
inspiratory whoop. Absolute lymphocytosis may produce a leukemoid reaction (20,000–50,000 cells/mm3). Lymphocytes
are normal in appearance.
• Convalescence phase: lasts 1–2 weeks. Slow decline in coughing and lymphocytosis.
• Complications: hemorrhage into skin, conjunctiva, bronchus, brain from coughing. Otitis media, meningoencephalitis
(10%), rectal prolapse from coughing, and pneumonia. Pneumonia is the most common cause of death in children
<3 yr old. Children <1 yr old have no protection from the mother’s immunoglobulins.
• Diagnosis: nasopharyngeal swabs using special cough plate; direct immunofluorescence of swab material
Haemophilus influenza
• Gram-negative rod
• Common cause of sinusitis, otitis media, and conjunctivitis (pink eye)
• Accounts for 3%–10% of community-acquired pneumonias
• Inspiratory stridor may be caused by acute epiglottitis.
• Swelling of the epiglottis produces a “thumbprint sign” on a lateral radiograph of the neck
• Most common bacterial cause of acute exacerbation of preexisting COPD
• Diagnosis: culture, antigen detection
Moraxella catarrhalis
• Gram-negative diplococcus
• Common cause of typical pneumonia, especially in older adults
• Second most common pathogen causing acute exacerbation of COPD
• Common cause of chronic bronchitis, sinusitis, and otitis media
Pseudomonas aeruginosa
• Green sputum (pyocyanin pigment)
• Water-loving bacteria most often transmitted by respirators
• Most common cause of nosocomial pneumonia and death caused by pneumonia in CF
• Pneumonia is often associated with infarction caused by vessel invasion by the bacteria
Klebsiella pneumoniae
• Gram-negative fat rod surrounded by a mucoid capsule
• Common gram-negative organism causing lobar pneumonia and typical pneumonia in elderly patients in nursing homes
• Common cause of pneumonia in alcoholics; however, S. pneumoniae is still the most common pneumonia in alcoholics
• Typical pneumonia associated with blood-tinged, thick, mucoid currant jelly sputum
• Lobar consolidation and abscess formation are common.
Legionella pneumophila
• Gram-negative rod (requires IF stain or Dieterle silver stain to identify in tissue
• Water-loving bacterium (water coolers; mists in produce section of grocery stores; outdoor restaurants in summer; rain forests in zoos)
• Risk factors: alcoholic, smoker, immunosuppression
• Interstitial pneumonia associated with high fever, dry cough, flulike symptoms. Accounts for 2%–8% of adult community-acquired
pneumonias.
• May produce tubulointerstitial disease with destruction of the JG apparatus leading to hyporeninemic hypoaldosteronism
(type IV renal tubular acidosis [hyponatremia, hyperkalemia, metabolic acidosis]).
• Urine antigen test is an excellent screen.
Yersinia pestis • Gram-negative rod
• Cause of plague
• Transmitted by bite of rat flea. person to person by droplet infection.
• Macrophages cannot kill bacteria because V and W antigens provide protection.
• Three types of disease: bubonic (most common), pneumonic (transmitted by aerosol), and septicemic
• Bubonic type: bite by rat flea that has recently bitten an infected ground squirrel. Infected lymph nodes enlarge (usually
in the groin), mat together, and drain to the surface (buboes).
Cryptococcus neoformans
• Budding yeast with narrow-based buds. Surrounded by a thick capsule Forms pseudohyphae Found
in pigeon excreta (around buildings, outside office windows, under bridges;
• Primary lung disease (40%): granulomatous inflammation with caseation. Do not have to be
immunocompromised to acquire the disease.
Aspergillus fumigatus • branching septate hyphae
• Aspergilloma: fungus ball (visible on radiography) may develop in a preexisting cavity in the lung
(e.g., old TB site).
Cause of massive hemoptysis (invades blood vessels).
• Allergic bronchopulmonary aspergillosis: type I and type III HSRs. IgE levels increased and
eosinophilia is present. There is intense inflammation of airways and mucus plugs in the terminal
bronchioles. Repeated attacks may lead to bronchiectasis and interstitial lung disease.
• Vessel invader: causes hemorrhagic infarctions and a necrotizing bronchopneumonia
Mucor spp.
• Wide-angled hyphae without septa • Clinical settings: diabetes mellitus, immunosuppressed patients
• Vessel invader and produces hemorrhagic infarctions in the lung.
• Invades the frontal lobes in patients with diabetic ketoacidosis (rhinocerebral mucormycosis)
Coccidioides immitis
• Contracted by inhaling arthrospores in dust
• Spherules with endospores in tissues
• Flulike symptoms and erythema nodosum
• Granulomatous inflammation with caseous necrosis
Histoplasma capsulatum
• Most common systemic fungal infection
• Contracted by inhalation of microconidia in dust contaminated with excreta from bats
• Yeast forms are present in macrophages
• Granulomatous inflammation with caseous necrosis
• Simulates TB lung disease: produces coin lesions, consolidations, miliary spread, and cavitation
• Marked dystrophic calcification of granulomas.
Blastomyces dermatitidis
Most often associated with fishing (most common), hunting, gardening, exposure to beaver dams (beavers are reservoirs for the fungus)
• Yeasts have broad-based buds and nuclei
• Male-dominant disease
• Produces skin and lung disease. Skin lesions simulate squamous cell carcinoma.
• Granulomatous inflammation with caseous necrosis
Pneumocystis jiroveci • Cysts and trophozoites are present in tissue. Cysts attach to type I pneumocytes in the lungs.
• Similar to fungi but have no ergosterol in the plasma membrane
• Primarily an opportunistic infection. Occurs when the CD4 count is <200 cells/mm3.
• Common initial AIDS-defining infection
• Predominantly produces pulmonary disease with dense consolidation and patchy areas of induration in the lungs Patients develop fever, dyspnea, and severe hypoxemia. Diffuse
intraalveolar foamy exudates with cup-shaped
cysts are best visualized with silver or Giemsa stains.
• Chest radiography shows diffuse alveolar and interstitial infiltrates
You might also like
- Infectious Diseases USMLE NotesDocument32 pagesInfectious Diseases USMLE NotesAndrew SagalovNo ratings yet
- ATC Study GuideDocument23 pagesATC Study Guideshanaz_mayerNo ratings yet
- Ils MSL Dme SystemDocument91 pagesIls MSL Dme SystemH R VALANo ratings yet
- Respiratory Viruses: Organisms Causing PneumoniaDocument17 pagesRespiratory Viruses: Organisms Causing PneumoniaSherree HayesNo ratings yet
- Zang-Fu Syndrome Differentiation - UERMDocument113 pagesZang-Fu Syndrome Differentiation - UERMNathaniel P. Peralta0% (1)
- Word List UrinalysisDocument2 pagesWord List Urinalysischerry100% (1)
- Vor Dme and NDB DraftDocument5 pagesVor Dme and NDB DraftJohn Kevin DiciembreNo ratings yet
- Reaching The Age of Adolescence - Class Notes - Pariksha AbhyasDocument58 pagesReaching The Age of Adolescence - Class Notes - Pariksha Abhyastechnoharshil201100% (1)
- Fungal Infections of The BrainDocument50 pagesFungal Infections of The Braingetnus100% (1)
- 00 Introduction To Aviation TranscriptDocument9 pages00 Introduction To Aviation TranscriptAvtechNo ratings yet
- The Frequencies of Rifing From The First Frequencies DiscoveredDocument2,340 pagesThe Frequencies of Rifing From The First Frequencies Discovereddragana8moracaNo ratings yet
- Candidosis A New ChallengeDocument7 pagesCandidosis A New ChallengeSalvador contreras huertaNo ratings yet
- Atypical PneumoniaDocument30 pagesAtypical PneumoniachandanNo ratings yet
- Infectious Diseases of The Respiratory SystemDocument51 pagesInfectious Diseases of The Respiratory SystemFachriza EffendiNo ratings yet
- Candidiasis Medical MycologyDocument58 pagesCandidiasis Medical MycologyNoor MemonNo ratings yet
- Psychiatric Emmergency MGT 2 PDFDocument51 pagesPsychiatric Emmergency MGT 2 PDFFan Eli100% (4)
- Ils, MLS, TLSDocument9 pagesIls, MLS, TLSMaria CamiLa Roxanne Viernes100% (1)
- ADFDocument11 pagesADFManish MishraNo ratings yet
- Vulvovaginitis: by James Holencik, DODocument70 pagesVulvovaginitis: by James Holencik, DOSyarifa YuliaNo ratings yet
- A Report OnDocument56 pagesA Report OnweepauNo ratings yet
- ActinomycosisDocument26 pagesActinomycosistummalapalli venkateswara rao100% (1)
- Market Survey On Candida Drugs and ProbioticsDocument27 pagesMarket Survey On Candida Drugs and ProbioticsStephen MooreNo ratings yet
- Approaches: U.S. Terminal Procedures ChartDocument21 pagesApproaches: U.S. Terminal Procedures ChartNick TsangNo ratings yet
- Opportunistic MycosesDocument7 pagesOpportunistic MycosesDee GeeNo ratings yet
- Oral CandidiasisDocument5 pagesOral CandidiasisJNo ratings yet
- Candidiasis - Causes, Symptoms, Treatment, DiagnosisDocument5 pagesCandidiasis - Causes, Symptoms, Treatment, DiagnosisChaiwa JustineNo ratings yet
- Aircraft Electrical & Electronic Systems What Is Avionics?: ADF DME EAT EfisDocument8 pagesAircraft Electrical & Electronic Systems What Is Avionics?: ADF DME EAT EfisArslanKhanNo ratings yet
- Candidiasis (Hasznalt)Document4 pagesCandidiasis (Hasznalt)Ilyes FerenczNo ratings yet
- Mucocutaneus Candidiasis: Dosen Pembimbing: DR - Dr.anni Andriani, SP - KK Pembimbing Residen: Dr. EvelynDocument37 pagesMucocutaneus Candidiasis: Dosen Pembimbing: DR - Dr.anni Andriani, SP - KK Pembimbing Residen: Dr. EvelynHamizah Hasbullah100% (1)
- PneumoniaDocument120 pagesPneumoniaSaklenali LoniNo ratings yet
- Lecture 1-Introduction To RANDocument20 pagesLecture 1-Introduction To RANzuliana100% (1)
- Candidiasis 1Document5 pagesCandidiasis 1jodericoNo ratings yet
- Candidiasis A Fungal Infection Current Challenges and ProgressDocument11 pagesCandidiasis A Fungal Infection Current Challenges and ProgressLau's WorldNo ratings yet
- Candidiasis: International Class MakalahDocument16 pagesCandidiasis: International Class MakalahIrwan AzizNo ratings yet
- Free RadicalsDocument31 pagesFree RadicalsAlishba FaixanNo ratings yet
- Agents of Respiratory DiseaseDocument25 pagesAgents of Respiratory DiseaseAbid AliNo ratings yet
- Health9 - q1 - Mod4 - Effects of Environmental Issues - v3Document22 pagesHealth9 - q1 - Mod4 - Effects of Environmental Issues - v3HARLEY L. TAN89% (9)
- Candida Krusei TreatmentDocument2 pagesCandida Krusei TreatmentMohannad AhmedNo ratings yet
- Faa-Ct-8080-3 IfrDocument209 pagesFaa-Ct-8080-3 Ifrpapa_danny100% (2)
- Pneumonia: Martianus P, S.Farm.,M.Farm - Klin.,AptDocument30 pagesPneumonia: Martianus P, S.Farm.,M.Farm - Klin.,AptmadewikewirantiNo ratings yet
- Cell Structure of Cryptococcus FungiDocument19 pagesCell Structure of Cryptococcus FungiArshjyoti SinghNo ratings yet
- FlaraxinDocument53 pagesFlaraxinwereld2all100% (2)
- Respiratory and Nosocomial InfectionsDocument70 pagesRespiratory and Nosocomial InfectionsCezar Alexander GuevaraNo ratings yet
- Microbial Diseases of Respiratory System AO Rev3Document40 pagesMicrobial Diseases of Respiratory System AO Rev3rahafahmed20043No ratings yet
- Pneumonia 2Document43 pagesPneumonia 2Chol ArouNo ratings yet
- Pneumonia II MicrobesDocument15 pagesPneumonia II MicrobespuniariNo ratings yet
- The Lower Respiratory Tract InfectionsDocument19 pagesThe Lower Respiratory Tract Infectionshibasirag22No ratings yet
- Lung AbscessDocument30 pagesLung AbscessArmoured SpartanNo ratings yet
- Kuliah Respi Bakteri TDK Lazim Revisi TambahanDocument23 pagesKuliah Respi Bakteri TDK Lazim Revisi TambahanIzza Ayudia HakimNo ratings yet
- MicroPara BSN1A Neuro Gastro Genito Urinary InfectionDocument56 pagesMicroPara BSN1A Neuro Gastro Genito Urinary InfectionRoshwell RegalaNo ratings yet
- Basic 2021 TanvirDocument11 pagesBasic 2021 TanvirRA TanvirNo ratings yet
- Microbial Diseases of The Nervous System: DR Sonnie P. Talavera 08162009 OlfuDocument162 pagesMicrobial Diseases of The Nervous System: DR Sonnie P. Talavera 08162009 Olfuone_nd_onlyu0% (1)
- Bacterial Infection On Respiration Tract: Ike Irmawati P.A, Msi Med Mikrobiologi FK YarsiDocument39 pagesBacterial Infection On Respiration Tract: Ike Irmawati P.A, Msi Med Mikrobiologi FK YarsiCamila SuhendarNo ratings yet
- Lower Airway DiseasesDocument70 pagesLower Airway DiseasesAavash PradhanNo ratings yet
- ASOMDocument41 pagesASOMArunkumar S KumarNo ratings yet
- Communicable Disease: Person To Person Microbial DiseasesDocument19 pagesCommunicable Disease: Person To Person Microbial Diseasesnormina_balabagan9655No ratings yet
- Notes MICROBIAL DISEASES and EPIDEMIOLOGYDocument12 pagesNotes MICROBIAL DISEASES and EPIDEMIOLOGYDaniella TupasNo ratings yet
- L - 2 - GR (-) CocciDocument82 pagesL - 2 - GR (-) CocciFahim NadvyNo ratings yet
- Open Infections 2Document76 pagesOpen Infections 2Jehad AlzubairNo ratings yet
- Pneumonia in Plab PDFDocument6 pagesPneumonia in Plab PDFBeaulahNo ratings yet
- PNEUMONIADocument44 pagesPNEUMONIAReshama JamankarNo ratings yet
- Pericardial DX Endocarditis MyocarditisDocument14 pagesPericardial DX Endocarditis MyocarditisJefry SNo ratings yet
- Pediatric NotesDocument61 pagesPediatric NotesMatusala BafaNo ratings yet
- Week 1 TropMedDocument96 pagesWeek 1 TropMedmyqurandiaryNo ratings yet
- Classification of PneumoniaDocument13 pagesClassification of PneumoniaRaisa DilaNo ratings yet
- Subarachnoid Hemorrhage: Continuumaudio Interview Available OnlineDocument35 pagesSubarachnoid Hemorrhage: Continuumaudio Interview Available OnlineJose DavidNo ratings yet
- Hubungan Hipertensi Dengan Stroke Pada Pasien Poliklinik Neurologi RSUP Sanglah DenpasarDocument4 pagesHubungan Hipertensi Dengan Stroke Pada Pasien Poliklinik Neurologi RSUP Sanglah DenpasarlidawatiNo ratings yet
- Ebook Kanskis Clinical Ophthalmology A Systematic Approach PDF Full Chapter PDFDocument67 pagesEbook Kanskis Clinical Ophthalmology A Systematic Approach PDF Full Chapter PDFarchie.abney272100% (26)
- Charef 8 Week 10Document7 pagesCharef 8 Week 10Rechiel BagoodNo ratings yet
- Dzexams 2am Anglais 833192Document3 pagesDzexams 2am Anglais 833192sarasara199630No ratings yet
- Anaesthesia For Tonsillectomy TOTW 051 2007 230316 022350Document10 pagesAnaesthesia For Tonsillectomy TOTW 051 2007 230316 022350Srihari JanakiNo ratings yet
- IELTS Health Vocabulary: Part 1-Style QuestionsDocument3 pagesIELTS Health Vocabulary: Part 1-Style QuestionsYasemen KaramanNo ratings yet
- Individual Assignment: Name: Md. Rakib Mallick ID: 1921448 Course ID: MGT380Document12 pagesIndividual Assignment: Name: Md. Rakib Mallick ID: 1921448 Course ID: MGT380Onin HasanNo ratings yet
- Hypoglycemia - Schermerhorn, ThomasDocument2 pagesHypoglycemia - Schermerhorn, ThomasJuanMartínezNo ratings yet
- Surgery Short Case - HydroceleDocument1 pageSurgery Short Case - HydroceleHeroNo ratings yet
- Test Bank For Community Oral Health Practice For The Dental Hygienist 3rd Edition GeurinkDocument36 pagesTest Bank For Community Oral Health Practice For The Dental Hygienist 3rd Edition Geurinkchiragramallfsk7100% (43)
- Ca1 Pharmacology HandoutDocument19 pagesCa1 Pharmacology HandoutGabriel VillegasNo ratings yet
- Petunjuk Praktikum Lung Function Test B.1Document13 pagesPetunjuk Praktikum Lung Function Test B.1Inas Nabila AlhariNo ratings yet
- Thyroid Gland ExaminationDocument4 pagesThyroid Gland ExaminationMariana Ungur100% (1)
- Presentation On Anger Management: Submitted To - Dr. (MRS.) Anu SharmaDocument27 pagesPresentation On Anger Management: Submitted To - Dr. (MRS.) Anu SharmaHardeep KaurNo ratings yet
- Medical Terminology Chapter 3 With Complete Solutions 100 23 2024Document17 pagesMedical Terminology Chapter 3 With Complete Solutions 100 23 2024Gregg ProducerNo ratings yet
- Patho mcq16Document9 pagesPatho mcq16محمد العراقيNo ratings yet
- Managing Heart Failure in Primary Care: A Case Study ApproachDocument331 pagesManaging Heart Failure in Primary Care: A Case Study ApproachRaul FernandoNo ratings yet
- Pressure Ulcers - Back To The BasicsDocument11 pagesPressure Ulcers - Back To The BasicsHari Prasath T RNo ratings yet
- Single Leg Stance Test - PhysiopediaDocument4 pagesSingle Leg Stance Test - PhysiopediaVishaw Dev JoshiNo ratings yet
- Canine ParvovirusDocument13 pagesCanine ParvovirusSandrine WoolcockNo ratings yet
- Bacan Stone Is A Kind of Precious StonesDocument3 pagesBacan Stone Is A Kind of Precious StonesRikson TandelilinNo ratings yet
- Goodpasture Syndrome - LecturetteDocument4 pagesGoodpasture Syndrome - LecturetteAngela QuiñonesNo ratings yet
- Dermatofibroma Updated January 2020 - Lay Reviewed January 2020Document3 pagesDermatofibroma Updated January 2020 - Lay Reviewed January 2020Gandhi BossNo ratings yet
- Algorithm-ACLS CA 200731Document1 pageAlgorithm-ACLS CA 200731Hyunsoo EllisNo ratings yet