Professional Documents
Culture Documents
Rheumatic Disorders Imaging and Diagnosis
Uploaded by
Yoga PribadiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rheumatic Disorders Imaging and Diagnosis
Uploaded by
Yoga PribadiCopyright:
Available Formats
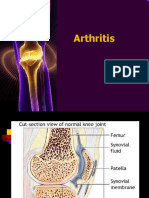
Inflammatory Rheumatic Disorders
Rheumatiod Arthritis
Important factors in the evolution of RA are:
1. genetic susceptibility an immunological reaction
2. possibly involving a foreign antigen, preferentially focused on synovial tissue
3. an inflammatory reaction in joints and tendon sheaths;
4. the appearance of rheumatoid factors (RF) and anti- citrullinated
5. antibodies (anti-CCP or ACPA) in the blood and synovium
6. perpetuation of the inflammatory process;
7. articular cartilage destruction
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Joint and Tendons Pathology
Extra–Articular Tissue:
• Rheumatoid Nodules,
• Lymphadenopathy
• Vasculitis
• Muscle weakness
• Visceral disease
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Clinical Features
In the early stage In the later stages
• Pain • Joint deformity becomes increasingly
• Constant pain and progressive joint
• Swelling destruction
• Loss of mobility in the proximal joint • “rheumatoid deformities : ulnar deviation of
of the fingers the finger, radial and volar displacement of
the wrists, valgus knees, valgus feet and
• Previous history of “muscle pain” clawed toe.
• Tiredness
• Loss of weight
The symptoms “spread” to others joint –
the wrists, feet, knee, shoulders.
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Imaging
X Rays
• Early stage, feature of synovitis: soft-
tissue swelling and periarticular
osteoporosis.
• Later stage, apperearance of marginal bony
erosions and narrowing of the articular
space, especially in the proximal joints of
the hand and feet.
• Advaced stage, articular destruction and
joint deformity are obvious. Flexion and
extention view of the cervical spine often
show subluxation at the atlantoaxial or
mid-cervical levels
Ultrasound scanning and MRI
• to look at soft tissue changes and early
erosion.
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Blood Investigations
Blood Investigations
• Normocytic, hypochromatic anemia is common and is a reflection of abnormal erythropoiesis due to diseasr activity.
• Rheuatoid factor are positive in about 80% of patients
• Antinuclear factor are present in 30 %.
Synovial biosy
• Synovial tissue may be obtained by needle biopsy, via the arthroscope, or by open operation. Unfortunately,
most of the histological features of rheumatoid arthritis are non-specific.
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Diagnosis
• Atypical forms of presentation are not uncommon.
• a bilateral, symmetrical polyarthritis involving the proximal joints of the hands or feet, and persisting for at
least 6 weeks.
• A positive test for RF in the absence of the above features is not sufficient evidence of rheumatoid arthritis,
nor does a negative test exclude the diagnosis if the other features are all present.
• The early stages may be punctuated by spells of quiescence, during which the diagnosis is doubted, but
sooner or later the more characteristic features appear.
• Older people, the onset is explosive, with the rapid appearance of severe joint pain and stiffness.
• Now and then (more so in young women) the disease starts with chronic pain and swelling of a single large
joint and it may take months or years before other joints are involved. The presence of tenderness on
squeezing across all metacarpophalangeal or metatarsophalangeal joints, early morning stiffness of at least 30
minutes and a raised ESR are highly suggestive of a diagnosis of rheumatoid arthritis.
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Differential Diagnostic
• Seronegative inflammatory polyarthritis
• Ankylosing spondylitis
• Reitee’s disease/reactive arthritis
• Polyarthicular gout
• Calcium pyrophosphate deposition disease
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Treatment
Medical management
Corticosteroid, metylprednisolon PO 30mg or i.m 120mg
Methotrexate 10-25 mg/week.
NSAIDs
Physiotherapy and occupational therapy
Surgical management
SEBELAS MARET UNIVERSITY
Inflammatory Rheumatic Disorders
Complications
Fixed deformities
Muscle weakness
Joint rupture
Infecion
Spinal cord vompression
Systemic vaculitis
Amyloidosis
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
There is considerable evidence for regarding ankylosing spondylitis (AS) as a genetically determined
immunopathological disorder.
Pathology
1. an inflammatory reaction with cell
2. infiltration, granulation tissue formation and erosion of adjacent bone; (2) replacement of the granulation
tissue by fibrous tissue; and
3. ossification of the fibrous tissue, leading to ankylosis of the joint
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Clinical Features
Teenager or young adult
Backache
Stiffness
The symptoms are worse in the early morning and after inactivity
Swelling in peripheral joint such as ankle
Extraskeletal manifestation : general fatigue and loss of weight
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Imaging
X Rays, Cardinal sign is erosion and fuzziness of sacroiliac joint..
Later maybe periarticular sclerosis, especially on the iliac side of the joint and finally bony ankylosis.
• Earliest vertebra change is flattening of the normal anterior concavity of the vertebral body (‘squaring’)
• Later, ossification of the ligaments around the intervertebral discs produces delicate bridges (syndesmophytes)
• between adjacent vertebrae (Figure 3.8).
• Bridging at several levels gives the appearance of a ‘bamboo spine’
MRI, to allow detail investigation of sacroiliac joint and may showtypical erosion and features of inflammation
such as bone oedema.
Special investigation, The ESR and CRP are usually elevated suring active phases of the disease. HLA-B27 is
present in 95% of cases. Serological test for rheumatoid factor are usually negative.
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Diagnosis
Diagnosis is easy in pationts with rigidity and typical deformities.
• In over 10% of cases the disease starts with an asymmetrical inflammatory arthritis – usually of the hip, knee or ankle –
and it may be several years before back pain appears
• Atypical onset is more common in women
Mechanical disorders, low back pain in young adults the onset of pain usually is relatesd to specific physical
activities, stiffness is less pronouched and symptoms are eased rathe than agrgravated by inactivity.
• Diffuse idiopathic hyperostosis (Forestier’s disease), This is a fairly common disorder, predominantly of older
men, characterized by widespread ossification of ligaments and tendon insertions Other seronegative
spondyloarthropathies, A number of disorders are associated with vertebral and sacroiliac lesions indistinguishable from
those of ankylosing spondylitis. They are Reiter’s disease, psoriatic arthritis, ulcerative colitis, Crohn’s disease,
Whipple’s disease and Behçet’s syndrome. In each there are certain characteristic features: the rash or nail changes of
psoriasis, intestinal ulceration in inflammatory bowel disease, genitourinary and ocular inflammation in Reiter’s
disease, buccal and genital ulceration in Behçet’s syndrome
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Treatment
Treatment consists of:
(1) general measures to maintain satisfactory posture and preserve movement;
(2) anti-inflammatory drugs to counteract pain and stiffness;
(3) the use of TNF inhibitors for severe disease (with inhibitors of other cytokines such as IL-17 and IL-12/23
in development);
(4) operations to correct deformity or restore mobility.
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
• General measures, Swimming, dancing and gymnastics are ideal forms of recreation.
• Non-steroidal anti-inflammatory drugs
• Operation, significantly damaged hips can be treated by joint replacement, though this seldom provides more
than moderate mobility
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Reiter’s Syndrome and reactive Arthritis
• The syndrome described by Hans Reiter in 1916 is a clinical triad of urethritis, arthritis and conjungtivitis
occurring some weeks arter either dysentery or genitourinary infection
• Cause, familial aggregation, overlap with orther forms of seronegative spondyloarthropathy in first-degree
relatives and a close association with HLA-B27 point to a genetic predisposition, the bowel or genitourinary
infection acting as a trigger
• Gut pathogens include Shigella flexneri, Salmonella, Campylobacter species and Yersinia enterocolitica.
Lymphogranuloma venereum and Chlamydia trachomatis have been implicated as sexually transmitted
infections.
• Pathology, changes are essentially the same as those in ankylosing spondylitis
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Reiter’s Syndrome and reactive Arthritis
• Clinical feature, Acute Phase: marked by an asymmetrical inflammatory arthritis of the lower limb joints –
usually the knee and ankle but often the tarsal and toe joints as well. The joint may be acutely painful, hot and
swollen with a tense effusion, suggesting gout or infection, Tendo Achilles
• tenderness and plantar fasciitis, Conjunctivitis, urethritis and bowel
infections
• Less frequent, but equally characteristic, features are a vesicular or pustular dermatitis of the feet
(keratoderma blennorrhagica)
• Chronic Phase, characteristic of a spondyloarthropathy
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Reiter’s Syndrome and reactive Arthritis
• X Rays : Sacroiliaic and vertebral changes are similar to those of ankylosing spondylitis, Joints : erosive
arthritis
• Special investigation, Test for HLA-B27 are positive in 75% of patient with sacroiliitis
• Treatment, Reiter’s disease should be aimed at ensuring the infectious organism responsible has been cleared.
Symptomatic treatment could include the use of analgesia and non-steroidal anti-inflammatory drugs. If the
inflammatory response is aggressive, local injection of corticosteroids or even intramuscular
methylprednisolone may be useful.
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Psoriatic Arthritis
• Psoriatic arthritis is characterized by seronegative polysynovitis, erosive (sometimes very destructive)
arthritis, enthesitis and dactylitis and a significant incidence of sacroiliitis and spondylitis. The prevalence of
psoriasis is 1–2%, but only about 5% of those affected will develop psoriatic arthritis. The usual age at onset
is 30–50 years (often later than the skin lesions).
• Cause, strong genetic component, 60% of those with psoriatic spondylitis or sacroiliitis have HLA-B27
Psoriatic skin lesions may well be a reactive phenomenon, and the joint lesions a form of ‘reactive arthritis’
• Pathology, The joint changes are similar to those in rheumatoid arthritis – chronic synovitis with cell
infiltration and exudate, going on to fibrosis. Cartilage and bone destruction may be unusually severe
(‘arthritis mutilans’)
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Psoriatic Arthritis
• Clinical features:
• arthritis of distal interphalangeal joints, ‘arthritis mutilans’, asymmetrical large joint oligoarthritis and patterns mimicking rheumatoid
arthritis or ankylosing spondylitis.
• Psoriasis of the skin or nails usually precedes the arthritis, but hidden lesions (in the natal cleft or umbilicus) are easily overlooked
• the worst cases both the spine and the peripheral joints may be involved. Fingers and toes are severely deformed due to erosion and
instability of the interphalangeal joints (arthritis mutilans)
Imaging
X-Ray, Severe destruction of the inter phalangeal joint of the hand and feet
Ultrasound scanning and MRI May show grater definition of the extent and activity of synovitis
Special investigation, Rheumatoid factor almost always negative. HLA-B27 occours in 50-60%, especially in those with overt sacroiliitis.
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Psoriatic Arthritis
The important distinguishing features of psoriatic arthritis are:
1. asymmetrical joint distribution;
2. Involvement of distal finger joints
3. the presence of sacroiliitis or spondylitis;
4. the absence of rheumatoid nodules.
Treatment
• In mild disease no more than topical preparations to control the skin disease and NSAIDs
• Immunosuppressive agents (methotrexate) and TNF inhibitors
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Enteropathic Arthritis
Peripheral Arthritis,
• 15% of patients with inflammatory bowel disease.
• Pain and swelling may appear quite suddenly and last for 2–3 months before subsiding.
• Synovitis is usually the only feature but joint erosion can occur
Sacroiliitis and spondylitis
• 10% of patients with inflammatory bowel disease, and in half of these
• patients the clinical picture closely resembles that of
• ankylosing spondylitis
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Enteropathic Arthritis
Juvenile Idiopathic Arthritis,
• non-infective inflammatory joint disease of more than 3 months’ duration in children under 16 years of age
• Pain and swelling may appear quite suddenly and last for 2–3 months before subsiding.
• Synovitis is usually the only feature but joint erosion can occur
Sacroiliitis and spondylitis
• 10% of patients with inflammatory bowel disease, and in half of these
• patients the clinical picture closely resembles that of
• ankylosing spondylitis
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Psoriatic Arthritis
• Clinical features:
• arthritis of distal interphalangeal joints, ‘arthritis mutilans’, asymmetrical large joint oligoarthritis and patterns mimicking rheumatoid
arthritis or ankylosing spondylitis.
• Psoriasis of the skin or nails usually precedes the arthritis, but hidden lesions (in the natal cleft or umbilicus) are easily overlooked
• the worst cases both the spine and the peripheral joints may be involved. Fingers and toes are severely deformed due to erosion and
instability of the interphalangeal joints (arthritis mutilans)
Imaging
X-Ray, Severe destruction of the inter phalangeal joint of the hand and feet
Ultrasound scanning and MRI May show grater definition of the extent and activity of synovitis
Special investigation, Rheumatoid factor almost always negative. HLA-B27 occours in 50-60%, especially in those with overt sacroiliitis.
SEBELAS MARET UNIVERSITY
Peripheral Spondyloarthopathies
Psoriatic Arthritis
• Clinical features:
• arthritis of distal interphalangeal joints, ‘arthritis mutilans’, asymmetrical large joint oligoarthritis and patterns mimicking rheumatoid
arthritis or ankylosing spondylitis.
• Psoriasis of the skin or nails usually precedes the arthritis, but hidden lesions (in the natal cleft or umbilicus) are easily overlooked
• the worst cases both the spine and the peripheral joints may be involved. Fingers and toes are severely deformed due to erosion and
instability of the interphalangeal joints (arthritis mutilans)
Imaging
X-Ray, Severe destruction of the inter phalangeal joint of the hand and feet
Ultrasound scanning and MRI May show grater definition of the extent and activity of synovitis
Special investigation, Rheumatoid factor almost always negative. HLA-B27 occours in 50-60%, especially in those with overt sacroiliitis.
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
Spinal fractures
Hyperkyphosis
Spinal cord compression
Lumbosacrol nerve root compression
SEBELAS MARET UNIVERSITY
Axial Sponduloarthropathies
Including Ankylosing Spondylitis
There is considerable evidence for regarding ankylosing spondylitis (AS) as a genetically determined
immunopathological disorder.
Pathology
1. an inflammatory reaction with cell
2. infiltration, granulation tissue formation and erosion of adjacent bone; (2) replacement of the granulation
tissue by fibrous tissue; and
3. ossification of the fibrous tissue, leading to ankylosis of the joint
SEBELAS MARET UNIVERSITY
You might also like
- Amputation - DR EKADocument41 pagesAmputation - DR EKADiah agungNo ratings yet
- Osteoarthritis & Rheumatoid ArthritisDocument60 pagesOsteoarthritis & Rheumatoid ArthritisSaya MenangNo ratings yet
- Review of Musculoskeletal TumorsDocument63 pagesReview of Musculoskeletal TumorsDanur AdiNo ratings yet
- Rheumatology: Osteoarthritis Rheumatoid Arthritis: Dr. Meg-Angela Christi AmoresDocument25 pagesRheumatology: Osteoarthritis Rheumatoid Arthritis: Dr. Meg-Angela Christi AmoresNinaNo ratings yet
- Osteoarthritis & Gouty ArthritisDocument94 pagesOsteoarthritis & Gouty ArthritisStar CruiseNo ratings yet
- Ra and Osteoarthritis R IfDocument43 pagesRa and Osteoarthritis R IfsnfhanNo ratings yet
- DR Sutap Yadav: Seronegative SpondyloarthropathiesDocument45 pagesDR Sutap Yadav: Seronegative SpondyloarthropathiesAyush PaudelNo ratings yet
- Musculoskeletal Disorders GuideDocument36 pagesMusculoskeletal Disorders GuideFitria UlfahNo ratings yet
- Rheumatoid Arthritis Module IDocument14 pagesRheumatoid Arthritis Module ISamhitha Ayurvedic ChennaiNo ratings yet
- OSTEOARTHRITISDocument36 pagesOSTEOARTHRITISHzm Mus83% (12)
- Osteoarthritis 191016103144Document49 pagesOsteoarthritis 191016103144dr.abouzaid098No ratings yet
- Presentasi Radiologi: Dita Ayu Pertiwi FAA 114 016Document88 pagesPresentasi Radiologi: Dita Ayu Pertiwi FAA 114 016dita ayuNo ratings yet
- Pathology: Osteoarthritis Pathology: OsteoarthritisDocument4 pagesPathology: Osteoarthritis Pathology: OsteoarthritisWaseem Khan AfridiNo ratings yet
- Arthritis: Prepared By: Salini D/O Vasudevan Supervisor: DR JaneDocument73 pagesArthritis: Prepared By: Salini D/O Vasudevan Supervisor: DR Janeumanantini06No ratings yet
- Lecture 3:osteoarthritis (2007 Powerpoint)Document54 pagesLecture 3:osteoarthritis (2007 Powerpoint)j.doe.hex_87100% (1)
- L25 Inflammatory Joint DiseasesDocument27 pagesL25 Inflammatory Joint Diseases8ht2twrg5fNo ratings yet
- Arthritis Types: Osteoarthritis, Gout, RheumatoidDocument22 pagesArthritis Types: Osteoarthritis, Gout, RheumatoidbellayuandaNo ratings yet
- Inflammatory Joint Diseases Handout-Admission ExamDocument11 pagesInflammatory Joint Diseases Handout-Admission ExamNona NadimNo ratings yet
- Osteoarthritis (Oa) : Prakash Thakulla InternDocument48 pagesOsteoarthritis (Oa) : Prakash Thakulla InternPrakash ThakullaNo ratings yet
- Osteo Arthit IsDocument19 pagesOsteo Arthit IsShaa ShawalishaNo ratings yet
- Joint Syndrome. Osteoarthritis. Solodenkova K.S.Document40 pagesJoint Syndrome. Osteoarthritis. Solodenkova K.S.Abdullah KhanNo ratings yet
- Osteoarthritis and HomoeopathyDocument6 pagesOsteoarthritis and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- Curs 9 Imagistica MSKDocument62 pagesCurs 9 Imagistica MSKn bNo ratings yet
- Faculty of MedicineDocument28 pagesFaculty of MedicineRana AtefNo ratings yet
- Rheum RCC ReviewDocument139 pagesRheum RCC Reviewahmed mahamedNo ratings yet
- Oa Ar GoutDocument18 pagesOa Ar GoutnerdwaldoNo ratings yet
- Osteoarthiti1 in EngDocument3 pagesOsteoarthiti1 in EngVhyanVhyanNo ratings yet
- S8 - Musculoskeletal SystemDocument23 pagesS8 - Musculoskeletal Systemyouservezeropurpose113No ratings yet
- Orthopedicdisorders 121221093512 Phpapp01Document93 pagesOrthopedicdisorders 121221093512 Phpapp01sarikaNo ratings yet
- Arthritis 180325095830 PDFDocument77 pagesArthritis 180325095830 PDFHesoca HuxNo ratings yet
- Osteoarthritis: (Degenerative Arthritis/osteoarthrosis/hypertrophic Arthritis)Document64 pagesOsteoarthritis: (Degenerative Arthritis/osteoarthrosis/hypertrophic Arthritis)Linda SugiartoNo ratings yet
- ARTHRITIS LectureDocument5 pagesARTHRITIS LectureMacDonald KarikariNo ratings yet
- Bone andDocument33 pagesBone andSuci MayveraNo ratings yet
- Osteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRDocument28 pagesOsteoartritis: Dr. Dewi Nur Fiana.,Sp - KFRgita cahayaNo ratings yet
- Osteoarthritis AapmrDocument5 pagesOsteoarthritis AapmrBiandaNo ratings yet
- ArthritisDocument13 pagesArthritisAishath Samha HussainNo ratings yet
- Osteonecrosis: Avascular NecrosisDocument8 pagesOsteonecrosis: Avascular NecrosisJezreel BonaNo ratings yet
- Medial End of ClavicleDocument49 pagesMedial End of ClavicleTefera LeteboNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument29 pagesDr. Ali's Uworld Notes For Step 2 CKuyes100% (1)
- Seronegatice ArthritisDocument23 pagesSeronegatice ArthritissamreignsNo ratings yet
- CBT Ortho 1Document45 pagesCBT Ortho 1putri umepalNo ratings yet
- Classification of Disorders of Musculoskeletal System (MSK) : Presented By: Siti Sarah Maha Dewi Bong Jen NeeDocument69 pagesClassification of Disorders of Musculoskeletal System (MSK) : Presented By: Siti Sarah Maha Dewi Bong Jen NeeBONG AIKCHINGNo ratings yet
- Joint Pain Guide: Causes, Symptoms and Treatment EvaluationDocument37 pagesJoint Pain Guide: Causes, Symptoms and Treatment EvaluationMuhammad MakkiNo ratings yet
- OsteoarthritisDocument61 pagesOsteoarthritisTony HermawanNo ratings yet
- Rheumatoid ArthritisDocument52 pagesRheumatoid ArthritisArun NingarajappaNo ratings yet
- X FactorDocument6 pagesX Factorlestari bmNo ratings yet
- Group 10 NCM 112 - (Osteonecrosis)Document8 pagesGroup 10 NCM 112 - (Osteonecrosis)Jezreel BonaNo ratings yet
- Osteo Arthritis and Inflammatory Arthritis: DR - Yanto Budiman. SP - Rad, M.Kes Bagian Radiologi FK/RS. Atma JayaDocument45 pagesOsteo Arthritis and Inflammatory Arthritis: DR - Yanto Budiman. SP - Rad, M.Kes Bagian Radiologi FK/RS. Atma JayaMira FindoroNo ratings yet
- JurnalDocument5 pagesJurnalQorin Diin ArifniNo ratings yet
- Knee Osteoarthritis: DefinitionDocument19 pagesKnee Osteoarthritis: DefinitionShrouq BadrNo ratings yet
- Rheumatoid Arthritis PTDocument25 pagesRheumatoid Arthritis PTyosra adamNo ratings yet
- Pathology of Musculoskeletal System: Bone Tumors and DiseasesDocument68 pagesPathology of Musculoskeletal System: Bone Tumors and DiseaseswilliamNo ratings yet
- Orthopaedic and Traumatology: Dr. Sukry Asdar Putra Hasibuan, SP - OTDocument37 pagesOrthopaedic and Traumatology: Dr. Sukry Asdar Putra Hasibuan, SP - OTNiaUlfaAngreiniTambunanNo ratings yet
- Degenerative Disorders of JointsDocument25 pagesDegenerative Disorders of JointsayuNo ratings yet
- ARTHRITIS TB KNEE HIP BPTDocument84 pagesARTHRITIS TB KNEE HIP BPTMiso100% (1)
- RheumatoidDocument35 pagesRheumatoidDeva LekshmiNo ratings yet
- Ankylosing SpondylitisDocument17 pagesAnkylosing Spondylitislesliejose1995No ratings yet
- JointsDocument68 pagesJointsLaine ZeeNo ratings yet
- Legg Calve PerthesDocument7 pagesLegg Calve PerthesNelhbenson LaurenteNo ratings yet
- 8 - Genetic Disorders, Skeletal Dysplasias and MalformationsDocument23 pages8 - Genetic Disorders, Skeletal Dysplasias and MalformationsYoga PribadiNo ratings yet
- Gout and crystal deposition diseasesDocument5 pagesGout and crystal deposition diseasesYoga PribadiNo ratings yet
- Compartment Syndrome PDFDocument187 pagesCompartment Syndrome PDFAmayaNo ratings yet
- 7 - Metabolic and Endocrine Bone DisordersDocument16 pages7 - Metabolic and Endocrine Bone DisordersYoga PribadiNo ratings yet
- Infection: Sebelas Maret UniversityDocument19 pagesInfection: Sebelas Maret UniversityYoga PribadiNo ratings yet
- Revascularization of A Crushed Foot and Ankle MortisDocument7 pagesRevascularization of A Crushed Foot and Ankle MortisYoga PribadiNo ratings yet
- Utility of Near-Infrared Spectroscopy in The Diagnosis of Lower Extremuty Compartment SyndromeDocument6 pagesUtility of Near-Infrared Spectroscopy in The Diagnosis of Lower Extremuty Compartment SyndromeYoga PribadiNo ratings yet
- Acute Femoral Shortening For Reconstruction of A Complex Lower Extremity Crush InjuryDocument5 pagesAcute Femoral Shortening For Reconstruction of A Complex Lower Extremity Crush InjuryYoga PribadiNo ratings yet
- "Ample": Advance Trauma and Live Support 9 EditionDocument3 pages"Ample": Advance Trauma and Live Support 9 EditionYoga PribadiNo ratings yet
- Lower Extremity Compartment SyndromeDocument6 pagesLower Extremity Compartment SyndromeYoga PribadiNo ratings yet
- "Ample": Advance Trauma and Live Support 9 EditionDocument3 pages"Ample": Advance Trauma and Live Support 9 EditionYoga PribadiNo ratings yet
- Limb Salvage SurgeryDocument11 pagesLimb Salvage SurgeryYoga PribadiNo ratings yet
- Acute Femoral Shortening For Reconstruction of A Complex Lower Extremity Crush InjuryDocument5 pagesAcute Femoral Shortening For Reconstruction of A Complex Lower Extremity Crush InjuryYoga PribadiNo ratings yet
- Amputation in Crush Syndrome A Case ReportDocument5 pagesAmputation in Crush Syndrome A Case ReportYoga PribadiNo ratings yet
- Open Fracture: Sebelas Maret UniversityDocument15 pagesOpen Fracture: Sebelas Maret UniversityYoga PribadiNo ratings yet
- Basic Surgical InstrumenDocument36 pagesBasic Surgical InstrumenYoga PribadiNo ratings yet
- Soal TraumaDocument10 pagesSoal TraumaYoga PribadiNo ratings yet
- 18 - The BackDocument48 pages18 - The BackYoga PribadiNo ratings yet
- Open Fracture: Sebelas Maret UniversityDocument15 pagesOpen Fracture: Sebelas Maret UniversityYoga PribadiNo ratings yet
- Trauma 2Document3 pagesTrauma 2Yoga PribadiNo ratings yet
- Q 3 DewqcacsDocument1 pageQ 3 DewqcacsYoga PribadiNo ratings yet
- DQWD 21 D 2Document1 pageDQWD 21 D 2Yoga PribadiNo ratings yet
- Top 10 Ortho Urgent Care Injuries Clark WEBDocument57 pagesTop 10 Ortho Urgent Care Injuries Clark WEBYoga PribadiNo ratings yet
- Cauda Equina Syndrome: Signs, Symptoms, and Surgical TimingDocument35 pagesCauda Equina Syndrome: Signs, Symptoms, and Surgical TimingVamsi MohanNo ratings yet
- Orthopedic Emergencies Booklet and Post Test WatermarkedDocument34 pagesOrthopedic Emergencies Booklet and Post Test Watermarkedbudi tambunanNo ratings yet
- EEG Waveform Guide: Alpha, Beta, Theta & Delta Frequencies ExplainedDocument9 pagesEEG Waveform Guide: Alpha, Beta, Theta & Delta Frequencies ExplainedsvchaudhariNo ratings yet
- Jurnal Polip ServiksDocument5 pagesJurnal Polip ServiksSilvi IndahrhaNo ratings yet
- Semiology 998Document121 pagesSemiology 998Popescu Nicusor100% (1)
- 6-Month Usmle Step 1 Sample Schedule Day Event Subjects Pathoma TasksDocument15 pages6-Month Usmle Step 1 Sample Schedule Day Event Subjects Pathoma Tasksone twoNo ratings yet
- Lactulose: (Enuluse, Kristalose, Duphalac, Chronulac Syrup)Document30 pagesLactulose: (Enuluse, Kristalose, Duphalac, Chronulac Syrup)Joanna Dela Torre100% (2)
- 91 Diabetic Striatopathy EndotextDocument10 pages91 Diabetic Striatopathy EndotextReena SinghNo ratings yet
- Tugas Materi Semester 2 (Endokrin, Disgestif, Urinaria)Document11 pagesTugas Materi Semester 2 (Endokrin, Disgestif, Urinaria)18111063 adelya larasatiNo ratings yet
- Huntington's Disease Information SheetDocument2 pagesHuntington's Disease Information SheetJerby Anne BasilioNo ratings yet
- Physical Examination of The NewbornDocument70 pagesPhysical Examination of The NewbornBeaflor Javier CaldozoNo ratings yet
- Abdominal Examination: OSCE ChecklistDocument2 pagesAbdominal Examination: OSCE ChecklistWafa Abdalla100% (2)
- Understanding Leukemia From A Lab PerspectiveDocument48 pagesUnderstanding Leukemia From A Lab PerspectiveGlorya NathasiaNo ratings yet
- Gingival Enlargement - DelDocument64 pagesGingival Enlargement - DeldelsaNo ratings yet
- LE 3 PTH Theoretical (2020A)Document13 pagesLE 3 PTH Theoretical (2020A)Monique BorresNo ratings yet
- Consensus criteria for diagnosing GDM following landmark HAPO studyDocument6 pagesConsensus criteria for diagnosing GDM following landmark HAPO studyRaul Garcia Salas CastilloNo ratings yet
- Thesis Rodulfo Eye Re (Formation) Integration of Architecture and Vision Therapy For The VisualimpairedDocument69 pagesThesis Rodulfo Eye Re (Formation) Integration of Architecture and Vision Therapy For The VisualimpairedPierre RodulfoNo ratings yet
- Pocket Book of Hospital Care For Children - Guidleines For The Management of Common Illnesses With Limited Resources. (2012, World Health Organization)Document442 pagesPocket Book of Hospital Care For Children - Guidleines For The Management of Common Illnesses With Limited Resources. (2012, World Health Organization)Sadia YousafNo ratings yet
- Phocomelia: A Case Study: March 2014Document3 pagesPhocomelia: A Case Study: March 2014Nexi anessaNo ratings yet
- Appendix ADocument62 pagesAppendix AViresh BatraNo ratings yet
- Communicable DiseasesDocument164 pagesCommunicable DiseasesJasmin Jacob33% (3)
- Blue Red LesionDocument14 pagesBlue Red LesionXara Barretto MagadiaNo ratings yet
- Gestational Hypertension - UTD PDFDocument21 pagesGestational Hypertension - UTD PDFShahar Perea ArizaNo ratings yet
- Adi Bestara EKG at A Glance NewestDocument113 pagesAdi Bestara EKG at A Glance Newestkarpax21100% (1)
- Rishabh Letter Draft-1Document2 pagesRishabh Letter Draft-1Rishabh AgarwalNo ratings yet
- Biomo306 Quiz One QuestionsDocument5 pagesBiomo306 Quiz One QuestionsAdrianNo ratings yet
- Megaloblastic AnemiaDocument26 pagesMegaloblastic AnemiaAbdifatah Abdiwali mohamedNo ratings yet
- Cardiology - Dr. Allam 2021Document141 pagesCardiology - Dr. Allam 2021MohammedNo ratings yet
- RTC ShockDocument16 pagesRTC ShockMarcelNo ratings yet
- Koding Icd 10 & Icd 9 NewwDocument30 pagesKoding Icd 10 & Icd 9 NewwJar Jar79% (14)
- Internal Medicine (I) Log Book Black Color TypingDocument48 pagesInternal Medicine (I) Log Book Black Color TypingQasim HaleimiNo ratings yet
- AML Case Study AnalysisDocument14 pagesAML Case Study AnalysisIssaiah Nicolle CeciliaNo ratings yet