100% found this document useful (1 vote)
358 views32 pagesMenopause
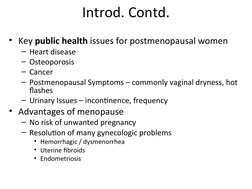
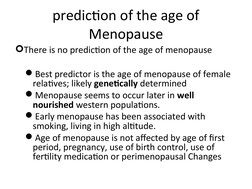
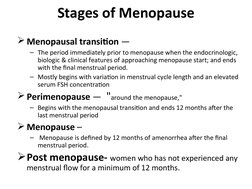
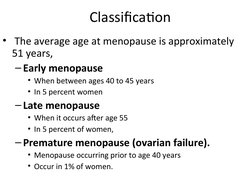
Menopause is defined as the permanent cessation of menstrual periods due to declining estrogen and progesterone levels from the ovaries. It typically occurs between ages 40-55. Key symptoms include hot flashes, vaginal dryness, urinary issues, and increased risk of osteoporosis and heart disease. Hormone therapy can effectively treat vasomotor symptoms and reduce risks of related diseases but should be used at the lowest dose for shortest time needed.
Uploaded by
Adefa ShiferawCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
358 views32 pagesMenopause
Menopause is defined as the permanent cessation of menstrual periods due to declining estrogen and progesterone levels from the ovaries. It typically occurs between ages 40-55. Key symptoms include hot flashes, vaginal dryness, urinary issues, and increased risk of osteoporosis and heart disease. Hormone therapy can effectively treat vasomotor symptoms and reduce risks of related diseases but should be used at the lowest dose for shortest time needed.
Uploaded by
Adefa ShiferawCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
- Introduction
- Prediction of the Age of Menopause
- Stages of Menopause
- Classification of Menopause
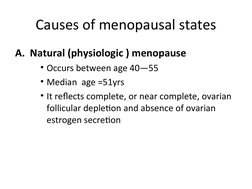
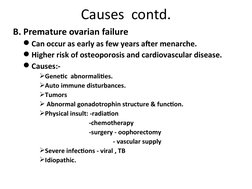
- Causes of Menopausal States
- Hormonal Changes of Menopause
- Menopause-related Symptoms
- Hot Flashes
- Pathophysiology
- Manifestations
- Treatment and Home Remedies
- Vaginal Dryness
- Bladder and Pelvic Changes
- Loss of Bone/Osteoporosis
- Impact on Cardiovascular and Mood
- Cognitive Function and Sexual Dysfunction
- Indications & Benefits of HRT
- Risks & Side Effects of HRT
- Contraindications for HRT
- Alternative Management
- Conclusion
- Assignments