Professional Documents
Culture Documents
สำเนา pne
Uploaded by
Thanawat Sima0 ratings0% found this document useful (0 votes)
9 views32 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views32 pagesสำเนา pne
Uploaded by
Thanawat SimaCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 32
INTRODUCTION
• Pneumonia is an infection of the pulmonary
parenchyma.
• Pneumonia historically was typically classified as
- community-acquired (CAP),
- hospital-acquired (HAP),
- ventilator-associated (VAP)
- health care– associated
pneumonia (HCAP)
ETIOLOGY
• etiologic agents in CAP includes bacteria, fungi,
viruses, and protozoa.
ETIOLOGY
CLINICAL MANIFESTATION
• febrile with tachycardia and/or chills and/or sweats.
• Cough may be either nonproductive or productive
of mucoid, purulent, or blood-tinged sputum.
• Gross hemoptysis is suggestive of CA-MRSA
pneumonia.
• Dyspnea
• Pleuritic chest pain
• 20% : GI symptom
CLINICAL MANIFESTATION
PHYSICAL EXAM
• Finding vary on degree of consolidation W/WO pleural effusion
• increased respiratory rate and use of accessory muscles of respiration
• Palpation may reveal increased or decreased
tactile fremitus
• percussion note can vary from dull to flat
• Crackles, bronchial breath sounds, and possibly a pleural friction rub
may be heard on auscultation.
INVESTIGATION
IMAGING
• CXR : Etiology and severity
• CT
INVESTIGATION
CLINICAL DIAGNOSIS ETIOLOGIC DIAGNOSIS
• CXR : Etiology and • Sputum G/S, C/S
severity • Blood culture
• CT • Urinary antigen test
• PCR
• Serology
• Biomarker
GRAM’S STAIN AND CULTURE OF SPUTUM
• Gram’s staining may also identify certain pathogens
• Adequate for culture, a sputum sample must have
>25 neutrophils and <10 squamous epithelial cells
per low-power field.
• yield of positive cultures from sputum samples is
≤50%
Question 1: In Adults with CAP, Should Gram Stain
and Culture of Lower Respiratory Secretions Be
Obtained at the Time of Diagnosis?
RECOMMENDATION
1. are classified as severe CAP, Esp. Intubation (Septic shock
with need for vasopressors and Respiratory failure
requiring mechanical ventilation )
2. are being empirically treated for MRSA or P. aeruginosa
3. were previously infected with MRSA or P. aeruginosa,
especially those with prior respiratory tract infection
4. were hospitalized and received parenteral antibiotics,
whether during the hospitalization event or not, in the
last 90 days
BLOOD CULTURES
• The yield from blood cultures, even when samples
are collected before antibiotic therapy, is
disappointingly low.
• Only 5–14% of cultures of blood from patients
hospitalized with CAP are positive, and the most
frequently isolated pathogen is S. pneumoniae.
Question 2: In Adults with CAP, Should Blood Cultures
Be Obtained atthe Time of Diagnosis?
RECOMMENDATION
1. are classified as severe CAP, Esp. Intubation (Septic shock
with need for vasopressors and Respiratory failure
requiring mechanical ventilation )
2. are being empirically treated for MRSA or P. aeruginosa
3. were previously infected with MRSA or P. aeruginosa,
especially those with prior respiratory tract infection
4. were hospitalized and received parenteral antibiotics,
whether during the hospitalization event or not, in the
last 90 days
URINARY ANTIGEN TESTS
• The sensitivity and specificity of the
- Legionella urine antigen test are as high as 70%
and 99%, respectively.
- pneumococcal urine antigen test is also quite
sensitive and specific (70% and >90%,respectively).
• Both tests can detect antigen even after the
initiation of appropriate antibiotic therapy
Question 3: In Adults with CAP, Should Legionella and
Pneumococcal Urinary Antigen Testing Be Performed
at the Time of Diagnosis?
RECOMMENDATION
1. in cases where indicated by epidemiological
factors, such as association with a Legionella
outbreak or recent travel
2. in adults with severe CAP
Question 4: In Adults with CAP, Should a Respiratory Sample
Be Tested for Influenza Virus at the Time
of Diagnosis?
RECOMMENDATION
• When influenza viruses are circulating in the
community,
• we recommend testing for influenza with a rapid
influenza molecular assay (i.e., influenza nucleic
acid amplification test), which is preferred over a
rapid influenza diagnostic test (i.e., antigen test)
BIOMARKERS
The two most commonly substances can serve as markers
of severe inflammation
- C-reactive protein (CRP) : identification of
worsening disease or treatment failure
- procalcitonin (PCT) : distinguishing bacterial from viral
infection, determining the need for antibacterial
therapy, or deciding when to discontinue treatment.
Question 5: In Adults with CAP, Should Serum
Procalcitonin plus Clinical Judgment versus Clinical
Judgment Alone Be Used to Withhold Initiation of
Antibiotic Treatment?
RECOMMENDATION
• Empiric antibiotic therapy should be initiated in adults with
clinically suspected and radiographically confirmed CAP
regardless of initial serum procalcitonin level
• suggested that procalcitonin levels of <0.1 mg/L indicate a
high likelihood of viral infection, whereas levels >0.25 mg/L
indicate a high likelihood of bacterial pneumonia
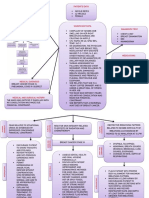
SITE OF CARE
• The two most frequently used are the Pneumonia Severity
Index (PSI), a prognostic model used to identify patients at
low risk of dying, and the CURB-65 criteria, a severity-of-
illness score.
PSI
CURB-65
Question 6: Should a Clinical Prediction Rule for
Prognosis plus Clinical Judgment versus Clinical
Judgment Alone Be Used to Determine Inpatient versus
Outpatient Treatment Location for Adults with CAP?
RECOMMENDATION
• recommend that clinicians use a validated clinical
prediction rule for prognosis, preferentially the
Pneumonia Severity Index (PSI) over the CURB-65.
• RCT demonstrated that use of the PSI safely
increases the proportion of patients who can
be treated in the outpatient setting.
Question 7: Should a Clinical Prediction Rule for
Prognosis plus Clinical Judgment versus Clinical
Judgment Alone Be Used to Determine Inpatient
General Medical versus Higher Levels of Inpatient
Treatment Intensity (ICU, StepDown, or Telemetry
Unit) for Adults with CAP?
RECOMMENDATION
ER , OPD IPD
- PSI (if > 90)
-CURB-65 (if ≥ 2)
Severity criteria
1. Septic shock with
ICU
need for
vasopressors
2.Respiratory failure
requiring
mechanical
ventilation
You might also like
- Nursing care process in patients with chronic obstructive pulmonary diseaseFrom EverandNursing care process in patients with chronic obstructive pulmonary diseaseNo ratings yet
- CAP BY DR ABBASDocument47 pagesCAP BY DR ABBASJohnson OlawaleNo ratings yet
- ADW Presentasi - Epidemiologi VAP Hippi 2023Document30 pagesADW Presentasi - Epidemiologi VAP Hippi 2023ERIE YUWITA SARINo ratings yet
- Pneumonia 2023 24Document26 pagesPneumonia 2023 24bazyan3aNo ratings yet
- Community-Acquired vs Hospital-Acquired PneumoniaDocument54 pagesCommunity-Acquired vs Hospital-Acquired PneumoniaPraise BechaydaNo ratings yet
- Cap CPGDocument40 pagesCap CPGMary Joy Oros-VallejeraNo ratings yet
- Pneumonia: Recent Evidence Based UpdatesDocument30 pagesPneumonia: Recent Evidence Based UpdatesAli AzamNo ratings yet
- Doc PneumoniaDocument73 pagesDoc PneumoniamarcelinecederNo ratings yet
- Cap Grand Rounds Presentation FinalDocument57 pagesCap Grand Rounds Presentation Finalapi-508924243No ratings yet
- Community Acquired Pneumonia (Cap) : Yan FlorestaDocument74 pagesCommunity Acquired Pneumonia (Cap) : Yan FlorestaYan florestaNo ratings yet
- Hospital Acquired Pneumonia (HAP) : Professor Adel Khattab Prof. of Pulmonary Medicine Ain Shams UniversityDocument43 pagesHospital Acquired Pneumonia (HAP) : Professor Adel Khattab Prof. of Pulmonary Medicine Ain Shams UniversityHamsiah HalimNo ratings yet
- CAP by DR SarmaDocument76 pagesCAP by DR SarmaTina ReisaNo ratings yet
- Dr. R V S N Sarma., MD., MSC., (Canada) Consultant Physician & Chest Specialist Visit Us At: WWW - Drsarma.InDocument76 pagesDr. R V S N Sarma., MD., MSC., (Canada) Consultant Physician & Chest Specialist Visit Us At: WWW - Drsarma.InAndry Wahyudi AgusNo ratings yet
- PneumoniaDocument48 pagesPneumoniaDammaqsaa W BiyyanaaNo ratings yet
- Community Acquiredandhospital Acquiredpneumonia1Document29 pagesCommunity Acquiredandhospital Acquiredpneumonia1api-610938913No ratings yet
- Pneumonia 1Document31 pagesPneumonia 1Parushhni NandhagopalNo ratings yet
- Therapy 2 ch4Document74 pagesTherapy 2 ch4Emad MustafaNo ratings yet
- PneumoniasDocument58 pagesPneumoniasKai Edmond MarvellaNo ratings yet
- Healthcare-Associated Pneumonia (HCAP)Document20 pagesHealthcare-Associated Pneumonia (HCAP)mcvirgo014No ratings yet
- Pediatrics Community Acquired Pneumonia: Isimijola OpeyemiDocument30 pagesPediatrics Community Acquired Pneumonia: Isimijola OpeyemiFavourNo ratings yet
- Guidelines for HAP and VAP ManagementDocument43 pagesGuidelines for HAP and VAP ManagementSarah Ummah MNo ratings yet
- Hospital PneumoniaDocument12 pagesHospital PneumoniaKartika RezkyNo ratings yet
- Journal Reading ParuDocument53 pagesJournal Reading ParuDaniel IvanNo ratings yet
- New Guidelines for Selecting Appropriate Antibiotics in Community Acquired PneumoniaDocument169 pagesNew Guidelines for Selecting Appropriate Antibiotics in Community Acquired PneumoniaYuvarajan SivaNo ratings yet
- Risk Factors and Management of Community Acquired PneumoniaDocument53 pagesRisk Factors and Management of Community Acquired PneumoniaAtif100% (1)
- Pneumonia - Taking Your Breath Away: Symptoms, Causes and TreatmentDocument85 pagesPneumonia - Taking Your Breath Away: Symptoms, Causes and TreatmentBalamurugan SanthalingamNo ratings yet
- Philippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaDocument42 pagesPhilippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaMarion Andrea PoblacionNo ratings yet
- Cap Hap VapDocument2 pagesCap Hap Vapapi-535300613No ratings yet
- Lower Airway Dysfunctions: Margaret Xaira R. Mercado, RNDocument52 pagesLower Airway Dysfunctions: Margaret Xaira R. Mercado, RNMargaret Xaira Rubio MercadoNo ratings yet
- Power Point Pneumonia.3pptDocument43 pagesPower Point Pneumonia.3pptMelissa 'meli' LapianNo ratings yet
- Covid19 - Pathophysiology and ManagementDocument51 pagesCovid19 - Pathophysiology and ManagementMyraflor CaroNo ratings yet
- Community Acquired Pneumonia: - Hafsah GhazaliDocument19 pagesCommunity Acquired Pneumonia: - Hafsah GhazaliCIk ChaNo ratings yet
- Commmunity Acquired PneumoniaDocument20 pagesCommmunity Acquired PneumoniaAnggun Cahya MertyanaNo ratings yet
- Pulmonary Infection GuidelinesDocument16 pagesPulmonary Infection GuidelinesFawad AhmedNo ratings yet
- Diagnosis & Treatment of Healthcare-Associated Pneumonia: Beyond The GuidelineDocument57 pagesDiagnosis & Treatment of Healthcare-Associated Pneumonia: Beyond The GuidelineKei MiyazakiNo ratings yet
- Penatalaksanaan CAPDocument31 pagesPenatalaksanaan CAPridhoNo ratings yet
- Community Acquired Pneumonia: - Hafsah GhazaliDocument19 pagesCommunity Acquired Pneumonia: - Hafsah GhazaliloribyseaNo ratings yet
- Dr. Reviono, DR., SP.P (K) - Update Diagnosis and Management JeroveciDocument20 pagesDr. Reviono, DR., SP.P (K) - Update Diagnosis and Management JeroveciOlivia DwimaswastiNo ratings yet
- Anesthaesia and Intensive CareDocument139 pagesAnesthaesia and Intensive CareIvan Kurniadi100% (2)
- Aspiration PneumoniaDocument34 pagesAspiration PneumoniaSelva VsNo ratings yet
- COVID - 19 Diagnosis - Current Updates FinalDocument63 pagesCOVID - 19 Diagnosis - Current Updates FinalDr. Gurbilas P. SinghNo ratings yet
- ICU Sepsis Management GuideDocument139 pagesICU Sepsis Management GuideMuhammad Farid100% (1)
- Pneumonia GuideDocument68 pagesPneumonia GuidefatiniNo ratings yet
- 2 Testing April 2021Document8 pages2 Testing April 2021Malcolm M YaduraNo ratings yet
- Tuesday Conference Approach To Community Acquired Pneumonia: Selim Krim, MD Assistant Professor TtuhscDocument37 pagesTuesday Conference Approach To Community Acquired Pneumonia: Selim Krim, MD Assistant Professor TtuhscKartika RezkyNo ratings yet
- Nosocomial PneumoniasDocument103 pagesNosocomial PneumoniasMuhammad Jahari SupiantoNo ratings yet
- Hospital Acquired Pneumonia GuideDocument29 pagesHospital Acquired Pneumonia GuideReman HakroushNo ratings yet
- HCAI Part 1: Ventilated Associated Pneumonia and Device Associated InfectionsDocument35 pagesHCAI Part 1: Ventilated Associated Pneumonia and Device Associated Infectionsjoee ahmedNo ratings yet
- Pneumonia Disease of LungDocument42 pagesPneumonia Disease of LungArmoured SpartanNo ratings yet
- PCAP Report ClerkshipDocument54 pagesPCAP Report ClerkshipMichelleAquinoSuzukiNo ratings yet
- New antibiotics for sepsis managementDocument27 pagesNew antibiotics for sepsis managementOlivia DwimaswastiNo ratings yet
- COVID-19 Management ProtocolDocument13 pagesCOVID-19 Management ProtocolajiNo ratings yet
- 3 Pulmonary Fungal and Viral Infections Part 3 Viruses and UnusualDocument28 pages3 Pulmonary Fungal and Viral Infections Part 3 Viruses and UnusualjimmyneumologiaNo ratings yet
- HAP Guideline Summary in 38 CharactersDocument20 pagesHAP Guideline Summary in 38 CharactersMradipta Arrya MNo ratings yet
- Procalcitonin2Document6 pagesProcalcitonin2zivl1984No ratings yet
- Management of Community Acquired PneumoniaDocument2 pagesManagement of Community Acquired Pneumoniaab_ghaffar_latiffi9337No ratings yet
- Clinical Pulmonary Infection Score: Preceptor: Dr. Hj. Liliriawati Ananta Kahar Sp. An, KICDocument20 pagesClinical Pulmonary Infection Score: Preceptor: Dr. Hj. Liliriawati Ananta Kahar Sp. An, KIChilda kimNo ratings yet
- Case Studies of Lower Respiratory Tract InfectionsDocument25 pagesCase Studies of Lower Respiratory Tract InfectionsMarianNo ratings yet
- Respiratory Tract InfectionsDocument26 pagesRespiratory Tract InfectionsyousefismailrootNo ratings yet
- Investigate CAP Severity & CausesDocument27 pagesInvestigate CAP Severity & CausesRoshana Mallawaarachchi0% (1)
- HCUP Methods SeriesDocument30 pagesHCUP Methods SeriesThanawat SimaNo ratings yet
- Dhanwal DK2011Document9 pagesDhanwal DK2011M MNo ratings yet
- สำเนา Journal uro newDocument23 pagesสำเนา Journal uro newThanawat SimaNo ratings yet
- สำเนา pharyngitisDocument47 pagesสำเนา pharyngitisThanawat SimaNo ratings yet
- สำเนา plant foodDocument53 pagesสำเนา plant foodThanawat SimaNo ratings yet
- A Cost-Utility Analysis of Cervical Cancer Screening and Human Papillomavirus Vaccination in The PhilippinesDocument17 pagesA Cost-Utility Analysis of Cervical Cancer Screening and Human Papillomavirus Vaccination in The PhilippinesYukiko CalimutanNo ratings yet
- HazMat IAP PlanDocument12 pagesHazMat IAP PlanVanitta RangsitananNo ratings yet
- Medicalization of BeautyDocument10 pagesMedicalization of BeautyhalohaiNo ratings yet
- For Your Youngest PatientsDocument2 pagesFor Your Youngest PatientsMarjorie BobadillaNo ratings yet
- Wa0007.Document47 pagesWa0007.KARLA JOHANNA TARIRA BARROSONo ratings yet
- Patient Engagement and Safety - PSNetDocument5 pagesPatient Engagement and Safety - PSNetanithaNo ratings yet
- Hemorrhagic ShockDocument2 pagesHemorrhagic ShockPharhana PuterieNo ratings yet
- Confidentiality and JusticeDocument3 pagesConfidentiality and JusticeRaseff Tesorero50% (2)
- Ayushman Bharat YojanaDocument28 pagesAyushman Bharat YojanaParth VasaveNo ratings yet
- Or Drug StudyDocument7 pagesOr Drug StudyNikki M. ArapolNo ratings yet
- Nejmoa 1805374Document10 pagesNejmoa 1805374Lia Diana RaileanuNo ratings yet
- Orthotics For Beginners'!: or How Not To Fail Your FRCS Questions in OrthoticsDocument26 pagesOrthotics For Beginners'!: or How Not To Fail Your FRCS Questions in OrthoticsRudiyantoNo ratings yet
- Refsum DiseaseDocument11 pagesRefsum DiseasechindyismailNo ratings yet
- BM Project On SpirometerDocument11 pagesBM Project On SpirometerAnushka NardeNo ratings yet
- Swami SIVANANDA - Practice of Ayurveda DDocument170 pagesSwami SIVANANDA - Practice of Ayurveda Dthomas100% (1)
- Somatom Emotion 6 SpecialDocument98 pagesSomatom Emotion 6 SpecialGabriel PaucarNo ratings yet
- 17th Asian Games Incheon 2014Document44 pages17th Asian Games Incheon 2014dantevermillionNo ratings yet
- InjectableDocument26 pagesInjectableAan KurniawanNo ratings yet
- Knowing What Works in Health Care A Roadmap For The Nation 2008 IOM PDFDocument279 pagesKnowing What Works in Health Care A Roadmap For The Nation 2008 IOM PDFcraigtanioNo ratings yet
- Pediatricians' Letter To LCS Superintendent Rocky HannaDocument2 pagesPediatricians' Letter To LCS Superintendent Rocky HannaWCTV Digital TeamNo ratings yet
- Breast Cancer Concept MapDocument2 pagesBreast Cancer Concept MapMaria Cristina100% (1)
- Blood Culture Collection ProcedureDocument2 pagesBlood Culture Collection ProcedureNestor PlasabasNo ratings yet
- Research Paper Polio EssayDocument9 pagesResearch Paper Polio Essayapi-254516775No ratings yet
- GE Healthcare AnestesiaDocument128 pagesGE Healthcare AnestesiaLuis Alberto Jiménez AcataNo ratings yet
- THE STATE v. KWAKU NKYIDocument4 pagesTHE STATE v. KWAKU NKYISolomon BoatengNo ratings yet
- Principles of Spine Trauma and Spinal Deformities PDFDocument34 pagesPrinciples of Spine Trauma and Spinal Deformities PDFVirlan Vasile CatalinNo ratings yet
- Mbbs Freshers ResumeDocument9 pagesMbbs Freshers ResumeTalha Noorani50% (2)
- Drugs AufDocument6 pagesDrugs AufBrian OballoNo ratings yet
- Abrasion and Laceration Wound CareDocument5 pagesAbrasion and Laceration Wound CareEtriNo ratings yet
- Tanzania Health System Assessment 2010Document135 pagesTanzania Health System Assessment 2010Anney Mwakabonga100% (1)