Professional Documents
Culture Documents
ALF and DILI
Uploaded by
Maryam OmarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ALF and DILI
Uploaded by
Maryam OmarCopyright:
Available Formats
Acute Liver Failure (ALF)
Faisal Abaalkhail, M.B.Ch.B, FACP, FRCPC
Consultant Gastroentrology and Transplant Hepatology
Adjunct Professor of Medicine, Al–Faisal University
Definition and clinical course of ALF
• ALF : acute deterioration of liver function without underlying chronic liver disease
SEVERE ACUTE LIVER INJURY (ALI)
• No underlying chronic liver disease*
• Liver damage
Up to 12 weeks post-jaundice,
(serum aminotransferases 23x ULN)
• Impaired liver function depending on sub-classification
(jaundice and coagulopathy)
HEPATIC ENCEPHALOPATHY (HE)
Crucial for the diagnosis of ALF
Mental alterations may be initially subtle
Intensive screening at the first sign of HE
is mandatory
ALF
*Patients with an acute presentation of chronic autoimmune hepatitis, Wilson disease and Budd–Chiari syndrome are considered as having ALF if they develop hepatic encephalopathy,
despite the presence of a pre-existing liver disease in the context of appropriate abnormalities in liver blood tests and coagulation profile;
EASL CPG ALF. J Hepatol 2017;66:1047–81
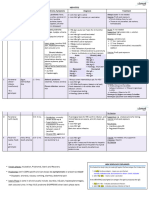
Sub-classifications of ALF
Weeks from development of jaundice to development of HE1
>28 weeks =
chronic liver
0 1 4 12 disease
Hyperacute1 Acute1 Subacute1
+++ ++ + Severity of coagulopathy2
+ ++ +++ Severity of jaundice2
Degree of intracranial
++ ++ +/- hypertension2
Chance of spontaneous
Good Moderate Poor
recovery2
Paracetamol
HBV Non-paracetamol drug-induced Typical cause2
HAV, HEV
+++ High severity; ++ Medium severity; + Low severity; +/- Present or absent
1. O'Grady JG, et al. Lancet 1993;342:2735; 2. Bernal W, et al. Lancet 2010;376:190201;
EASL CPG ALF. J Hepatol 2017;66:1047–81
Principal aetiologies of ALF
Viral
Hepatitis B, A, E
(less frequent CMV,
Drugs HSV, VZV, Dengue)
Paracetamol, anti-tuberculous, Toxins
chemotherapy, statins, NSAIDs, Amanita phalloides,
phenytoin, carbamazepine, ecstasy, phosphorus
flucloxacillin
ALF
Vascular Other
Budd–Chiari syndrome, Wilson disease, autoimmune,
hypoxic hepatitis lymphoma, malignancy, HLH
Pregnancy
Pre-eclamptic liver rupture,
HELLP, fatty liver of pregnancy
EASL CPG ALF. J Hepatol 2017;66:1047–81
Assessment and management at presentation
• Immediate measures
• Exclude cirrhosis, alcohol-induced liver injury or malignant infiltration
• Initiate early discussions with tertiary liver/transplant centre
• Even if not immediately relevant
• Screen intensively for hepatic encephalopathy
• Determine aetiology
• To guide treatment and determine prognosis
• Assess suitability for liver transplant
• Contraindications should not preclude transfer to tertiary liver/transplant centre
• Transfer to a specialized unit early
• If the patient has an INR >1.5 and onset of hepatic encephalopathy or other poor prognostic features
EASL CPG ALF. J Hepatol 2017;66:1047–81
Assessment and management at presentation
• Immediate measures
• Determine aetiology to guide treatment, especially LTx
Primary or secondary causes of ALF and need for transplantation
Disease group Hepatic/primary ALF Extrahepatic/secondary liver
failure and ACLF
Acute liver failure Drug related Hypoxic hepatitis (aka ischaemic)
Acute viral hepatitis Systemic diseases:
Toxin-induced ALF • Haemophagocytic syndromes
Budd–Chiari syndrome • Metabolic disease
Autoimmune • Infiltrative disease
Pregnancy related • Lymphoma
• Infections (e.g. malaria)
CLD presenting with a Fulminant presentation of Wilson disease Liver resection for either secondary deposits or
phenotype of ALF Autoimmune liver disease primary liver cancer
Budd–Chiari Alcoholic hepatitis
HBV reactivation
Possible indication for emergency LTx No indication for emergency LTx
EASL CPG ALF. J Hepatol 2017;66:1047–81
Differential diagnosis based on clinical features
Aetiology Clinical features
Paracetamol Very high levels of aminotransferases and low level of bilirubin. Rapidly progressive disease, acidosis and renal
impairment. Low phosphate may be seen as a good prognostic marker but replacement is required
Non-paracetamol Subacute clinical course can mimic cirrhosis, clinically and radiographically
Acute Budd–Chiari Abdominal pain, ascites and hepatomegaly; loss of hepatic venous signal and reverse flow in portal vein
syndrome on ultrasound
Wilson disease Young patient with Coombs (DAT)-negative haemolytic anaemia with a high bilirubin to ALP ratio;
Kayser–Fleischer ring; low serum uric acid level; markedly increased urinary copper
Mushroom poisoning Severe gastrointestinal symptoms after ingestion; development of early AKI
Autoimmune Usually subacute presentation – may have positive autoantibodies, elevated globulin and characteristic lymphocyte
pattern when compared to viral and seronegative aetiologies
Malignant infiltration History of cancer, massive hepatomegaly; elevated ALP or other tumour markers
Acute ischaemic injury Marked elevation of aminotransferases, increased lactic dehydrogenase and creatinine, which normalize soon after
stabilization of haemodynamic instability. Patients with severe congestive heart disease or
respiratory disease
Possible indication for emergency LTx No indication for emergency LTx
EASL CPG ALF. J Hepatol 2017;66:1047–81
Aetiologies with possible indication for LTx
• Drug-induced liver injury is the most frequent cause of severe ALI and ALF
• Especially paracetamol overdose
At admission, a toxicology screen and determination of paracetamol level are necessary in every patient, although
levels will frequently be negative. If the patient already has coagulopathy and increased serum aminotransferases, N-acetyl
cysteine therapy should be given
Prognosis is worse in patients with staggered ingestion of paracetamol. These cases are more likely to develop
multiple organ failure when compared to those with a single ingestion point
ALF caused by non-paracetamol drug-induced hepatotoxicity is a diagnosis of exclusion
EASL CPG ALF. J Hepatol 2017;66:1047–81
Aetiologies with possible indication for LTx
• Viral and autoimmune ALF
• HBV (most common), HAV, HEV, and VZV, HSV-1 and -2 (rare) can cause ALF
• Existence of other autoimmune conditions should raise suspicion of autoimmune hepatitis
Always screen for viral aetiologies
Suspect autoimmune aetiology in patients presenting other autoimmune disorders.
Liver biopsy may be needed if elevated globulin fraction and autoantibodies are absent.
Early treatment with steroids may be effective but list for emergency LTx if no improvement within 7 days
EASL CPG ALF. J Hepatol 2017;66:1047–81
Aetiologies with possible indication for LTx
• Uncommon aetiologies
Assessment of the clinical context is crucial to identify less common causes of ALF
Acute Budd–Chiari syndrome should be suspected in ALF presenting with gross ascites. Diagnosis is based on imaging
techniques
Wilson disease should be suspected with Coombs-negative haemolytic anaemia and high bilirubin to ALP ratio
In cases of HELLP and AFLP in pregnancy, the treatment of choice is prompt delivery of the baby, especially in case of
elevated lactate levels and hepatic encephalopathy. Screening for putative fatty acid defects should be offered
Screen for systemic diseases presenting as ALF
EASL CPG ALF. J Hepatol 2017;66:1047–81
General support outside ICU
Laboratory analyses at admission
Assess disease severity Check aetiology Test for complications
• PT, INR or factor V and full coagulation • Toxicology screen in urine and • Lipase or amylase
screen paracetamol serum level
• Liver blood tests* • Viral serological screen
• Renal function – HBsAg, anti-HBc IgM (HBV DNA),
– Urine output: hourly HDV if positive for HBV
– Urea† – anti HAV IgM
– Creatinine may be difficult to assay – anti-HEV IgM
in the context of elevated bilirubin – anti-HSV IgM, anti-VZV IgM,
• Arterial blood gas and lactate CMV, HSV, EBV, parvovirus and
VZV PCR
• Arterial ammonia
• Autoimmune markers‡
*Including LDH, conjugated and unconjugated bilirubin and creatinine kinase;
†
Low urea is a marker of severe liver dysfunction;
‡
ANAs, ASMA, anti-soluble liver antigen, globulin profile, ANCAs, HLA typing
EASL CPG ALF. J Hepatol 2017;66:1047–81
General support outside ICU
Diagnosis, monitoring and care at admission
Diagnostic tests Routine monitoring Standard care Preventative measures
• Cultures (respiratory, blood, • Oxygen saturation, blood • Glucose infusions • Avoid sedatives
urine) pressure, heart rate, (10–20%)* • Avoid hepatotoxic and
• Chest X-ray/ECG/liver respiratory rate, hourly urine • Stress ulcer prophylaxis nephrotoxic drugs
echography: axial imaging of output
• Restrict clotting factors unless
the abdomen and chest may • Clinical neurological status
active bleeding
also be required
• NAC in early stage, even in
• ECG
non-paracetamol cases
In case of HE
• Transfer to an appropriate level of care (ideally critical care) at the first symptoms of mental alterations
• Quiet surrounding, head of bed >30°C, head in neutral position and intubate, ventilate, and sedate if progression to >3 coma
• Low threshold for empirical start of antibiotics if haemodynamic deterioration and/or increasing encephalopathy with inflammatory
phenotype
• In case of evolving HE, intubation and sedation prior to the transfer
• Ensure volume replete and normalize biochemical variables (Na, Mg, PO4, K)
*Glycaemic target ± 140 mg/dl, Na 135–145 mmol/l;
EASL CPG ALF. J Hepatol 2017;66:1047–81
Organ-specific management
Main organ-specific complications in ALF
Coagulation/haemostasis Neurological = cerebral oedema Cranial hypertension
Unbalanced haemostasis Brain death
Thrombocytopenia
Infection Acute liver failure Metabolic
Bacterial, fungal Hypoglycaemia
Pneumopathy Hyponatraemia
Septicaemia Hypophosphataemia
Urinary infection Hypokalaemia
Haemodynamic Pulmonary Renal
Hyperkinetic syndrome Pneumopathy Toxic
Arrhythmia Acute respiratory distress syndrome Functional
Pulmonary overload
EASL CPG ALF. J Hepatol 2017;66:1047–81
Drug Induced Liver Injury
(DILI)
Faisal Abaalkhail, M.B.Ch.B, FACP, FRCPC
Consultant Gastroentrology and Transplant Hepatology
Adjunct Professor of Medicine, Al–Faisal University
Idiosyncratic DILI: a complex drug–host interaction 1
Drug Drug
Drug
Cellular injuryCellular injury initiation
Cellular
initiation injury initiation
Pharmacological responses
Pharmacological Pharmacological
responses
Reactive responses
metabolites, drug elimination
Reactive metabolites, drug elimination
Reactive metabolites, drugToxicological
eliminationresponses
Toxicological Toxicological responses
responses
Covalent binding, haptenization,
oxidative stress,Covalent
mitochondrial injury, ER stress
Drug properties binding, haptenization, Host factors
properties Covalent binding, haptenization,
Drug properties oxidative Cell
stress, Hosthost
mitochondrial injury, ER stress Possible
death factors
factors
oxidative stress, mitochondrial
Physicochemical injury,
Apoptosis, ER stress
necrosis, DAMP release Genetic variants
Pharmacological
Physiochemical Cell death Race/ethnicity Genetic variants
iochemical Toxicological
Pharmacological Cell death Apoptosis, necrosis, DAMP release Genetic
Age variants Race/ethnicity
macological ToxicologicalApoptosis, necrosis, DAMP release Race/ethnicity
Gender Age
xicological Biophysical effects
Bio-physiological effects Host response to injury insult Age state
Reproductive Gender
iological effects Gender
Nutrition/alcohol/smoking Reproductive state
Immune/inflammation Lifestyles statenutrition, alcohol, smoking
Reproductive
Host response to injury insult Disease conditions Lifestyles
Host response to injury insult nutrition, alcohol, smoking
Medications Disease conditions
Immune/ Lifestyles
Repair Tissue injury Gut flora Medications
Disease conditions
Immune/ inflammation Medications Gut flora
inflammation
Clinical manifestation and outcome Gut flora
1. Chen, et al. J Hepatol 2015;63:503–14. EASL CPG DILI. J Hepatol 2019;70:122261.
Definition and classification of liver injury
• Serum aminotransferases (ALT/AST), ALP, and TBL levels remain the mainstay for detecting and classifying
liver damage in suspected DILI
General
• DILI should be classified as hepatocellular, cholestatic or mixed according to the pattern of elevation of liver
enzymes based on the first set of laboratory tests available in relation to the clinical event
Aminotransferases
• ALT, ALP and TBL : define liver damage and liver dysfunction in DILI. AST values can reliably substitute ALT in calculating the
pattern of injury when the latter is unavailable at DILI recognition, whereas GGT is less reliable as an ALP substitute
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis of DILI relies largely on exclusion of alternative causes of
liver damage
Laboratory work-up
• Tests for HCV-RNA and ant-HEV IgM (or HEV-RNA) are suggested in patients with suspected DILI to
exclude acute hepatitis C and/or E, particularly in those cases not compatible with the drug signature of
the suspected causative agent and/or with high transaminase levels
Imaging
• An abdominal ultrasound should be undertaken in all patients suspected of DILI. The use of additional
imaging studies relies on the clinical context
Liver biopsy
• Liver biopsy may be considered during the investigation of selected patients suspected to suffer DILI, as liver
histology can provide information that can support the diagnosis of DILI or an alternative diagnosis
• Liver biopsy may be performed in patients suspected to have DILI when serology raises the possibility
of AIH
• Liver biopsy may be considered in patients when suspected DILI progresses or fails to resolve on withdrawal of the
causal agent as the liver histology may provide prognostic information assisting clinical management
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis: a stepwise approach
Abnormal biochemistry/acute hepatitis
DILI suspicion
Features supporting toxic aetiology
Skin involvement, kidney injury, previous DILI episodes
Careful enquiry of exposure to HDS, drugs, OTC drugs*
Potential pitfalls Discontinue non-essential drugs/HDS treatment
Lack of information (eg. dose, duration), several medications,
hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox)
Calculate biochemical pattern of liver injury
𝐀𝐋𝐓 / 𝐔𝐋𝐍 Hepatocellular Mixed Cholestatic
(𝐑 )
𝐀𝐋𝐏 / 𝐔𝐋𝐍 R≥5 2>R<5 ≤2
*record start and stop dates;
†
hepatic vascular disease, chronic hepatitis,
fibrosis, microvesicular steatosis
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis
DILI suspicion
Features supporting toxic aetiology
Skin involvement, kidney injury, previous DILI episodes
Careful enquiry of exposure to HDS, drugs, OTC drugs*
Potential pitfalls Discontinue non-essential drugs/HDS treatment
Lack of information (eg. dose, duration), several medications,
hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox)
Calculate biochemical pattern of liver injury
𝐀𝐋𝐓 / 𝐔𝐋𝐍 Hepatocellular Mixed Cholestatic
(𝐑 )
𝐀𝐋𝐏 / 𝐔𝐋𝐍 R≥5 2>R<5 ≤2
Search for alternative causes
*record start and stop dates;
†
hepatic vascular disease, chronic hepatitis,
fibrosis, microvesicular steatosis
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis
DILI suspicion
Features supporting toxic aetiology
Skin involvement, kidney injury, previous DILI episodes
Careful enquiry of exposure to HDS, drugs, OTC drugs*
Potential pitfalls Discontinue non-essential drugs/HDS treatment
Lack of information (eg. dose, duration), several medications,
hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox)
Calculate biochemical pattern of liver injury
𝐀𝐋𝐓 / 𝐔𝐋𝐍 Hepatocellular Mixed Cholestatic
(𝐑 )
𝐀𝐋𝐏 / 𝐔𝐋𝐍 R≥5 2>R<5 ≤2
Search for alternative causes
• Viral infections (HAV, HBV, HCV, HEV, EBV, CMV)
• Alcohol-related liver disease, hepatic ischaemia
• Autoantibody titres, ↑ IgG
*record start and stop dates;
†
hepatic vascular disease, chronic hepatitis,
fibrosis, microvesicular steatosis
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis: a stepwise approach Abnormal biochemistry/acute hepatitis
DILI suspicion
Features supporting toxic aetiology
Skin involvement, kidney injury, previous DILI episodes
Careful enquiry of exposure to HDS, drugs, OTC drugs*
Potential pitfalls Discontinue non-essential drugs/HDS treatment
Lack of information (eg. dose, duration), several medications,
hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox)
Calculate biochemical pattern of liver injury
𝐀𝐋𝐓 / 𝐔𝐋𝐍 Hepatocellular Mixed Cholestatic
(𝐑 )
𝐀𝐋𝐏 / 𝐔𝐋𝐍 R≥5 2>R<5 ≤2
Search for alternative causes
• Viral infections (HAV, HBV, HCV, HEV, EBV, CMV) • Benign/malignant biliary obstruction
• Alcohol-related liver disease, hepatic ischaemia • Primary biliary cholangitis
• Autoantibody titres, ↑ IgG • Primary sclerosing cholangitis
*record start and stop dates;
†
hepatic vascular disease, chronic hepatitis,
fibrosis, microvesicular steatosis
EASL CPG DILI. J Hepatol 2019;70:122261.
Diagnosis: a stepwise approach
Abnormal biochemistry/acute hepatitis
DILI suspicion
Features supporting toxic aetiology
Skin involvement, kidney injury, previous DILI episodes
Careful enquiry of exposure to HDS, drugs, OTC drugs*
Potential pitfalls Discontinue non-essential drugs/HDS treatment
Lack of information (eg. dose, duration), several medications,
hidden HDS and OTC drug intake Search in hepatotoxicity resources (Liver tox)
Calculate biochemical pattern of liver injury
𝐀𝐋𝐓 / 𝐔𝐋𝐍 Hepatocellular Mixed Cholestatic
(𝐑 )
𝐀𝐋𝐏 / 𝐔𝐋𝐍 R≥5 2>R<5 ≤2
Search for alternative causes
• Viral infections (HAV, HBV, HCV, HEV, EBV, CMV) • Benign/malignant biliary obstruction
• Alcohol-related liver disease, hepatic ischaemia • Primary biliary cholangitis
• Autoantibody titres, ↑ IgG • Primary sclerosing cholangitis
Consider liver biopsy if
• Negative or incomplete rechallenge
*record start and stop dates; • Acute or chronic atypical presentation †
†
hepatic vascular disease, chronic hepatitis,
fibrosis, microvesicular steatosis • Autoimmune hepatitis
EASL CPG DILI. J Hepatol 2019;70:122261.
Therapy
• Most important initial step in terms of management of suspected DILI is to discontinue the implicated
agent
Specific therapies
• Cholestyramine: a short administration may be used to decrease the course of
hepatotoxicity induced by very selected drugs, such as leflunomide and terbinafine
• Carnitine may be used to decrease the course of valproate hepatotoxicity
• The efficacy of NAC to improve the severity of liver injury from drugs other than paracetamol
may not be significantly substantiated
• The efficacy of UDCA to reduce the severity of liver injury may not be significantly
substantiated
EASL CPG DILI. J Hepatol 2019;70:122261.
You might also like
- Liver - Dr. Allam 2021 PDFDocument70 pagesLiver - Dr. Allam 2021 PDFMohammedNo ratings yet
- Acute Liver Failure - EASL 2017Document44 pagesAcute Liver Failure - EASL 2017Eugenia DoagaNo ratings yet
- Acute Liver Failure EASL 2017Document44 pagesAcute Liver Failure EASL 2017AlionuskaDraganNo ratings yet
- Acute Liver Failure - EASL CPG Slide DeckDocument31 pagesAcute Liver Failure - EASL CPG Slide Deckdoctorali1995No ratings yet
- Acut Hepatitis-1Document46 pagesAcut Hepatitis-1Ajeet LohanaNo ratings yet
- Acute Liver Failure EASL CPGDocument57 pagesAcute Liver Failure EASL CPGRicky Cornelius Tarigan0% (1)
- Acute Liver Failure EASL CPGDocument57 pagesAcute Liver Failure EASL CPGFatima Medriza DuranNo ratings yet
- MedsDocument6 pagesMedsJim RashidNo ratings yet
- ACLF AbhishekDocument56 pagesACLF AbhishekGavi Siddanagowda PatilNo ratings yet
- Revision Notes Dr. A. MowafyDocument222 pagesRevision Notes Dr. A. MowafyMohammed RisqNo ratings yet
- Falla HepaticaDocument24 pagesFalla HepaticaCbrera ValentinaNo ratings yet
- Cyanosis in Congenital Heart Disease:: Eisenmenger's Syndrome or Not ?Document37 pagesCyanosis in Congenital Heart Disease:: Eisenmenger's Syndrome or Not ?Eva FaridahNo ratings yet
- Acute Liver FailureDocument20 pagesAcute Liver FailureMarian AndrianaNo ratings yet
- Fígado Acute Liver FailureDocument6 pagesFígado Acute Liver FailureEdson MarquesNo ratings yet
- HepatitisDocument3 pagesHepatitisapi-648401824No ratings yet
- TBL 5 (Surgical Jaundice)Document33 pagesTBL 5 (Surgical Jaundice)Irsyad SiddeeqNo ratings yet
- ASACLASS Renew3Document3 pagesASACLASS Renew3docwepNo ratings yet
- He HepatitisDocument4 pagesHe HepatitisMayar JaradNo ratings yet
- Gastroenterology Handouts Spring 2019Document27 pagesGastroenterology Handouts Spring 2019Sasoo EmadNo ratings yet
- Clinical Assessment in Acute Heart Failure: Review ArticleDocument17 pagesClinical Assessment in Acute Heart Failure: Review ArticleAnonymous NeRC5JYiSNo ratings yet
- Acute Fulminant Hepatic Failure Due To Hepatitis A Virus: A Case ReportDocument3 pagesAcute Fulminant Hepatic Failure Due To Hepatitis A Virus: A Case ReportTor JaNo ratings yet
- Slides DR Ashgar Approach To LFTs 12.12.2021Document47 pagesSlides DR Ashgar Approach To LFTs 12.12.2021Maryam OmarNo ratings yet
- Khanna 2018Document20 pagesKhanna 2018wahid akbarNo ratings yet
- CD Hepatitis - Dr. Yapendon 2014Document13 pagesCD Hepatitis - Dr. Yapendon 2014jeccomNo ratings yet
- Chronic Liver DiseaseDocument3 pagesChronic Liver DiseaseNikey LimNo ratings yet
- Canine Chronic Hepatitis: Diagnosis & TreatmentDocument8 pagesCanine Chronic Hepatitis: Diagnosis & TreatmentThamil ArasanNo ratings yet
- Acute Liver FailureDocument43 pagesAcute Liver FailureÁýáFáŕőúgNo ratings yet
- 2-LFT Case Report Key AnswerDocument5 pages2-LFT Case Report Key AnswerAbdullah AlthobaitiNo ratings yet
- Module 7Document8 pagesModule 7soriano2214989No ratings yet
- Autoimmune Liver DeseaseDocument4 pagesAutoimmune Liver DeseaseJankirk BacierraNo ratings yet
- Hepatology MRCP1Document87 pagesHepatology MRCP1Raouf Ra'fat SolimanNo ratings yet
- R Falla Hepatica 16 GuiasDocument35 pagesR Falla Hepatica 16 GuiasRICARDO BOSSANo ratings yet
- Acute Liver FailureDocument46 pagesAcute Liver FailureDoc On CallNo ratings yet
- Prolonged Cholestasis Due To Hepatitis A Virus Infection in A Young Adolescent Male With A Known Case of Hemoglobin E Disease: Early Response To Steroid TherapyDocument4 pagesProlonged Cholestasis Due To Hepatitis A Virus Infection in A Young Adolescent Male With A Known Case of Hemoglobin E Disease: Early Response To Steroid TherapyBOHR International Journal on GastroenterologyNo ratings yet
- LIVERDISEASEDocument82 pagesLIVERDISEASEHervis FantiniNo ratings yet
- Hepatic EncephalopathyDocument1 pageHepatic Encephalopathykarla.isehemm.idrogo.quirozNo ratings yet
- Farmakoterapi SirosisDocument27 pagesFarmakoterapi SirosisfizaNo ratings yet
- JaundiceDocument17 pagesJaundiceDarwithaNo ratings yet
- Ref 4Document13 pagesRef 4indah setiyaniNo ratings yet
- Acute Hepatitis+alf 678Document37 pagesAcute Hepatitis+alf 678Sheren GamaleldenNo ratings yet
- Hepatic EmergenciesDocument76 pagesHepatic EmergenciesAbdelrahman MokhtarNo ratings yet
- 2018 Hepatitis Viral InfectionDocument51 pages2018 Hepatitis Viral Infectionkomang nickoNo ratings yet
- English ReportDocument35 pagesEnglish ReportOana KoppandiNo ratings yet
- GUIA de Insuficiencia Hepatica AgudaDocument35 pagesGUIA de Insuficiencia Hepatica AgudaHernan GonzalezNo ratings yet
- Fulminant Hepatic FailureDocument53 pagesFulminant Hepatic FailureAR KarthickNo ratings yet
- Approach To Elevated LFTDocument42 pagesApproach To Elevated LFTAnant PachisiaNo ratings yet
- HEPATITISDocument4 pagesHEPATITISYalin AbouhassiraNo ratings yet
- Review: Liver Dysfunction in Critical IllnessDocument17 pagesReview: Liver Dysfunction in Critical IllnessRoger Ludeña SalazarNo ratings yet
- Liver BPDocument23 pagesLiver BPiuyjgtrfNo ratings yet
- NURS 1301 Editing CVA CASE Study Need To FinishDocument13 pagesNURS 1301 Editing CVA CASE Study Need To FinishabbieNo ratings yet
- Varices Esophagus PDFDocument7 pagesVarices Esophagus PDFDimas ErlanggaNo ratings yet
- Global Prevalence of Hepatitis CDocument28 pagesGlobal Prevalence of Hepatitis CDr-dina MohammedNo ratings yet
- Alf Ajay AgadeDocument84 pagesAlf Ajay AgadeVinay PatilNo ratings yet
- L8 - Hepatic EnzymesDocument30 pagesL8 - Hepatic Enzymesyouservezeropurpose113No ratings yet
- Hepatitis PDFDocument61 pagesHepatitis PDFYahya Taqiuddin RobbaniNo ratings yet
- Journal Reading: "Acute Decompensation and Acute-on-Chronic Liver Failure"Document27 pagesJournal Reading: "Acute Decompensation and Acute-on-Chronic Liver Failure"Tanani FebriantyNo ratings yet
- Case Report TIADocument6 pagesCase Report TIAjuntumagantangNo ratings yet
- Fulminant Hepatic Failure (FHF) (Acute Liver Failure (ALF) ) : DR / Reyad AlfakyDocument108 pagesFulminant Hepatic Failure (FHF) (Acute Liver Failure (ALF) ) : DR / Reyad AlfakypadmaNo ratings yet
- Cirrhosis V2-1Document1 pageCirrhosis V2-1El MaheritoNo ratings yet
- CK-MB Isoenzyme: Immunoinhibition MethodDocument2 pagesCK-MB Isoenzyme: Immunoinhibition MethodFariz KasyidiNo ratings yet
- IMMUNITYDocument5 pagesIMMUNITYKebbewar KhaledNo ratings yet
- Lesson Plan in Arteries and VeinsDocument3 pagesLesson Plan in Arteries and VeinsHarold BadillaNo ratings yet
- Module 4 Digestive SystemDocument9 pagesModule 4 Digestive SystemupadhiNo ratings yet
- Lesson #7 - Transporting Materials Across CellsDocument37 pagesLesson #7 - Transporting Materials Across CellsMaya AwadNo ratings yet
- CASE STUDY ABRUPTIO PLACENTA BSN 2 H For Printing NA FINAL NAaaaaaaDocument36 pagesCASE STUDY ABRUPTIO PLACENTA BSN 2 H For Printing NA FINAL NAaaaaaaisaacdarylNo ratings yet
- Solution Manual For Laboratory Manual For Anatomy Physiology Featuring Martini Art Main Version Plus Masteringap With Etext Package 5 e Michael G WoodDocument4 pagesSolution Manual For Laboratory Manual For Anatomy Physiology Featuring Martini Art Main Version Plus Masteringap With Etext Package 5 e Michael G WoodKarenAcevedotkoi100% (40)
- AP13 EndocrineDocument12 pagesAP13 EndocrinePay per PrintNo ratings yet
- RLE Checklist Administering Oxygen by Cannula or FacemaskDocument2 pagesRLE Checklist Administering Oxygen by Cannula or FacemaskQuantum XavierNo ratings yet
- Q2 Long Test 2 Levels of Biological OrganizationDocument4 pagesQ2 Long Test 2 Levels of Biological OrganizationCastolo Bayucot JvjcNo ratings yet
- FST (Boys) 2023Document3 pagesFST (Boys) 2023Abdul qadoosNo ratings yet
- Ocular Drug Delivery and PermeablityDocument63 pagesOcular Drug Delivery and PermeablityDr AYAL TILAHUN MIHIRETIENo ratings yet
- AquactivLS BrochureDocument2 pagesAquactivLS Brochurepjanovic.rajkaNo ratings yet
- Development of Some Abdominal VisceraDocument5 pagesDevelopment of Some Abdominal VisceraAbdullah Al-MuhaiminNo ratings yet
- Sexuality and Its Disorders Development Cases and Treatment 1St Edition Abrams Test Bank Full Chapter PDFDocument27 pagesSexuality and Its Disorders Development Cases and Treatment 1St Edition Abrams Test Bank Full Chapter PDFkhaidu00drxn100% (9)
- Hematopoiesis: Pluri - Several) or Hemocytoblasts. These Cells Have The Capacity To Develop Into Many Different Types ofDocument12 pagesHematopoiesis: Pluri - Several) or Hemocytoblasts. These Cells Have The Capacity To Develop Into Many Different Types ofRajender ArutlaNo ratings yet
- MCQs InvertebratesDocument6 pagesMCQs InvertebratesHumaira Shah100% (1)
- KN 4@enzl 8 Ha 4 B 6 CC 9 eDocument26 pagesKN 4@enzl 8 Ha 4 B 6 CC 9 eRamzen Raphael DomingoNo ratings yet
- Acute Toxicity and Cytotoxicity of Pereskia Aculeata, A Highly Nutritious Cactaceae PlantDocument7 pagesAcute Toxicity and Cytotoxicity of Pereskia Aculeata, A Highly Nutritious Cactaceae PlantGleice ReinertNo ratings yet
- A Study On Two-Layered Model (Casson-Newtonian) For Blood Ow Through An Arterial Stenosis: Axially Variable Slip Velocity at The WallDocument14 pagesA Study On Two-Layered Model (Casson-Newtonian) For Blood Ow Through An Arterial Stenosis: Axially Variable Slip Velocity at The WallRicardoNo ratings yet
- 13 Abdomen Part IDocument12 pages13 Abdomen Part IMonique BorresNo ratings yet
- EDTA FinalDocument4 pagesEDTA FinalRaffaharianggaraNo ratings yet
- ТФ тест2021Document20 pagesТФ тест2021Balzhan SabyrNo ratings yet
- The Oral CavityDocument23 pagesThe Oral CavityHamzaNo ratings yet
- Cambridge International AS & A Level: Biology 9700/22 March 2021Document15 pagesCambridge International AS & A Level: Biology 9700/22 March 2021Pom GNo ratings yet
- M.Pharm PharmaceuticsDocument13 pagesM.Pharm PharmaceuticsBilla NNo ratings yet
- Regulation of Body Fluids: Compare and Contrast Process in Plants and AnimalsDocument16 pagesRegulation of Body Fluids: Compare and Contrast Process in Plants and AnimalsPaopao Macalalad100% (4)
- To Study The Effect of PH On Seed GerminationDocument20 pagesTo Study The Effect of PH On Seed Germinationrautshreyash220% (1)
- Blood Module Questions 2018 (D'23)Document22 pagesBlood Module Questions 2018 (D'23)bilqeesNo ratings yet
- List Harga E-Katalog PT SAM Tahun 2021Document7 pagesList Harga E-Katalog PT SAM Tahun 2021Sony ArianaNo ratings yet