Professional Documents
Culture Documents
Ketamine
Uploaded by
Malik Arif Ullah0 ratings0% found this document useful (0 votes)
6 views24 pagesKetamine is a dissociative anesthetic that produces anesthesia through antagonism of NMDA receptors in the brain and spinal cord. It is soluble in water and commonly administered intravenously or intramuscularly in doses of 2 mg/kg for induction of anesthesia. Ketamine increases heart rate and blood pressure while maintaining airway reflexes and ventilation. Emergence phenomena like delirium and hallucinations are common side effects. Ketamine is indicated for pediatric anesthesia, trauma/emergency settings, and high-risk patients due to its cardiovascular stability.
Original Description:
Original Title
4. Ketamine
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentKetamine is a dissociative anesthetic that produces anesthesia through antagonism of NMDA receptors in the brain and spinal cord. It is soluble in water and commonly administered intravenously or intramuscularly in doses of 2 mg/kg for induction of anesthesia. Ketamine increases heart rate and blood pressure while maintaining airway reflexes and ventilation. Emergence phenomena like delirium and hallucinations are common side effects. Ketamine is indicated for pediatric anesthesia, trauma/emergency settings, and high-risk patients due to its cardiovascular stability.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views24 pagesKetamine
Uploaded by
Malik Arif UllahKetamine is a dissociative anesthetic that produces anesthesia through antagonism of NMDA receptors in the brain and spinal cord. It is soluble in water and commonly administered intravenously or intramuscularly in doses of 2 mg/kg for induction of anesthesia. Ketamine increases heart rate and blood pressure while maintaining airway reflexes and ventilation. Emergence phenomena like delirium and hallucinations are common side effects. Ketamine is indicated for pediatric anesthesia, trauma/emergency settings, and high-risk patients due to its cardiovascular stability.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 24
KETAMINE
KETAMINE HYDROCHLORIDE
This is a phencyclidine derivative and was
introduced in 1965.
It differs from other i.v. anaesthetic agents
in many respects, and produces dissociative
anaesthesia rather than generalized
depression of the CNS.
PHYSICAL CHARACTERISTICS
AND PRESENTATION
Ketamine is soluble in water and is presented
as solutions of 10 mg/mL containing sodium
chloride to produce isotonicity
Ketamine is also avaliable in 50 or 100 mg/ml
in multidose vials which contain
benzethonium chloride 0.1 mg/mL as
preservative.
The pH of the solutions is 3.5–5.5.
MECHANISMS OF ACTION
Ketamine has multiple effects throughout the
central nervous system, inhibiting
polysynaptic reflexes in the spinal cord as
well as excitatory neurotransmitter effects in
selected areas of the brain.
Its effects are mediated primarily by
noncompetitive antagonism at the N-methyl-
D-aspartate (NMDA) receptor in the brain and
spinal cord.
MECHANISMS OF ACTION
Ketamine functionally “dissociates” the
thalamus (which relays sensory impulses
from the reticular activating system to the
cerebral cortex) from the limbic cortex
(which is involved with the awareness of
sensation).
Clinically, this state of dissociative
anesthesia may cause the patient to appear
conscious (eg, eye opening, swallowing,
muscle contracture) but unable to process or
respond to sensory input.
MECHANISMS OF ACTION
Other mechanisms of action of ketamine may
include an interaction with opioid receptors
Therefore it is consider a strong analgesic
and week anesthetic
DOSAGE AND ADMINISTRATION
Induction of anaesthesia is achieved with an
average dose of 2 mg/kg i.v;
larger doses may be required in some
patients, and smaller doses in the elderly or
shocked patient. In all cases, the drug should
be administered slowly. Additional doses of
1–1.5 mg/ kg are required every 5–10 min.
Between 8 and 10 mg/kg is used i.m.
A dose of 0.25–0.5 mg kg–1 or an infusion of
50 μg/kg/min may be used to produce
analgesia without loss of consciousness.
PHARMACOKINETICS
Absorption
Ketamine has been administered orally,
nasally, rectally, subcutaneously, and
epidurally, but in usual clinical practice it is
given intravenously or intramuscularly
Peak plasma levels are usually achieved
within 10–15 min after intramuscular
injection.
DISTRIBUTION
Ketamine is more lipid soluble and less
protein bound than thiopental.
These characteristics, along with ketamine-
induced increase in cerebral blood flow and
cardiac output, lead to rapid brain uptake
and subsequent redistribution (the
distribution half-life is 10–15 min).
Awakening is due to redistribution from brain
to peripheral compartments.
BIOTRANSFORMATION
Metabolism occurs predominantly in the liver
by demethylation and hydroxylation of the
cyclohexanone ring; among the metabolites
is norketamine, which is pharmacologically
active.
Approximately 80% of the injected dose is
excreted renally as glucuronides; only 2.5% is
excreted unchanged.
The elimination half-life is approximately 2.5
h. Distribution and elimination are slower if
halothane, benzodiazepines or barbiturates
are administered concurrently.
CENTRAL NERVOUS SYSTEM
Ketamine is extremely lipidsoluble.
After i.v injection, it induces anaesthesia in
30–60 s. A single i.v. dose produces
unconsciousness for 10–15 min.
Ketamine is also effective within 3–4 min
after i.m. injection and has a duration of
action of 15–25 min. It is a potent somatic
analgesic at subanaesthetic blood
concentrations
CENTRAL NERVOUS SYSTEM
Induction of anaesthesia is smooth, but
emergence delirium may occur, with
restlessness, disorientation and agitation. Vivid
and often unpleasant nightmares or
hallucinations may occur during recovery and for
up to 24 h.
The incidences of emergence delirium and
hallucinations are reduced by avoidance of
verbal and tactile stimulation during the
recovery period, or by concomitant
administration of opioids, butyrophenones,
benzodiazepines or physostigmine however,
unpleasant dreams may persist.
CENTRAL NERVOUS SYSTEM
Nightmares are reported less commonly by
children and elderly patients
Cerebral metabolic rate is increased in
several regions of the brain, and CBF,
cerebral blood volume and intracranial
pressure (ICP) increase
This unique clinical state is typified by
catalepsy in which the eyes may remain open
with a slow nystagmic gaze & the corneal
and light reflexes remain intact.
CARDIOVASCULAR SYSTEM
Arterial pressure increases by up to 25% and
heart rate by approximately 20%.
Cardiac output may increase, and myocardial
oxygen consumption increases;
There is increased myocardial sensitivity to
adrenaline.
Sympathetic stimulation of the peripheral
circulation is decreased, resulting in
vasodilatation in tissues innervated
predominantly by α-adrenergic receptors, and
vasoconstriction in those with β-receptors.
RESPIRATORY SYSTEM
Transient apnoea may occur after i.v.
injection, but ventilation is well maintained
thereafter and may increase slightly unless
high doses are given.
Pharyngeal and laryngeal reflexes and a
patent airway are maintained well in
comparison with other i.v. agents; however,
their presence cannot be guaranteed, and
normal precautions must be taken to protect
the airway and prevent aspiration. Bronchial
muscle is dilated.
RESPIRATORY SYSTEM
The increased salivation associated with
ketamine can be attenuated by
premedication with an anticholinergic agent
such as glycopyrrolate
Skeletal Muscle. Muscle tone is usually
increased. Spontaneous movements may occur,
but reflex movement in response to surgery is
uncommon.
Gastrointestinal System. Salivation is
increased.
Uterus and Placenta. Ketamine crosses the
placenta readily. Fetal concentrations are
approximately equal to those in the mother.
The Eye. Intraocular pressure increases,
although this effect is often transient. Eye
movements often persist during surgical
anaesthesia.
ADVERSE EFFECTS
Emergence delirium, nightmares and
hallucinations
Hypertension and tachycardia – this may be
harmful in previously hypertensive patients
and in those with ischaemic heart disease
Prolonged recovery
Salivation – anticholinergic premedication is
essential
Increased intracranial pressure
Allergic reactions – skin rashes have been
reported
INDICATIONS
The high-risk patient. Ketamine is useful in the
shocked patient. Arterial pressure may decrease if
hypovolaemia is present, and the drug must be given
cautiously. These patients are usually heavily sedated
in the postoperative period, and the risk of nightmares
is therefore minimized.
Paediatric anaesthesia. Children undergoing minor
surgery, investigations (e.g. cardiac catheterization),
ophthalmic examinations or radiotherapy may be
managed successfully with ketamine administered
either i.m. or i.v.
Difficult locations. Ketamine has been used
successfully at the site of accidents, and for analgesia
and anaesthesia in casualties of war
INDICATION
Analgesia and sedation. The analgesic
action of ketamine may be used when
wound dressings are changed, or while
positioning patients with pain before
performing regional anaesthesia (e.g.
fractured neck of femur). Ketamine has been
used to sedate asthmatic patients in the ICU.
Developing countries. Ketamine is used
extensively in countries where anaesthetic
equipment and trained staff are in short
supply.
ABSOLUTE
CONTRAINDICATIONS
Airway obstruction – although the airway is
maintained better with ketamine than with
other agents, its patency cannot be
guaranteed.
Inhalational agents should be used for
induction of anaesthesia if airway
obstruction is anticipated.
Raised intracranial pressure.
PRECAUTIONS
Cardiovascular disease. Ketamine is
unsuitable for patients with pre-existing
hypertension, ischaemic heart disease or
severe cardiac decompensation.
Repeated administration. Because of the
prolonged recovery period, ketamine is not
the most suitable drug for frequent
procedures, e.g. prolonged courses of
radiotherapy, as it disrupts sleep and eating
patterns.
Outpatient anaesthesia. The prolonged
recovery period and emergence phenomena
make ketamine unsuitable for adult
outpatients.
THANK YOU
You might also like
- Ketamine ?Document42 pagesKetamine ?Shaik NisaNo ratings yet
- Uia 13 DELAYED AWAKENING OR EMERGENCE FROM ANAESTHESIADocument3 pagesUia 13 DELAYED AWAKENING OR EMERGENCE FROM ANAESTHESIAsunny kumarNo ratings yet
- Delayed Awakening From AnaesthesiaDocument3 pagesDelayed Awakening From AnaesthesiaSenthooran ArudshivsmNo ratings yet
- Presentation 2Document20 pagesPresentation 2Muhammad UmairNo ratings yet
- KetamineDocument37 pagesKetamineRajesh Reddy Chintakunta100% (1)
- Evaluation and Management of Delayed Awakening or Emergence From AnaesthesiaDocument19 pagesEvaluation and Management of Delayed Awakening or Emergence From AnaesthesiaMuhammad UmairNo ratings yet
- Skeletal Muscle RelaxantsDocument34 pagesSkeletal Muscle RelaxantsLohithNo ratings yet
- Neuropharma AntidementiaDocument29 pagesNeuropharma AntidementiaKeanne Paula AmamanglonNo ratings yet
- Anaesthesia Drugs Used CommonlyDocument6 pagesAnaesthesia Drugs Used CommonlyAmar Mahesh KalluNo ratings yet
- Ketalar (Ketamine Hydrochloride Injection, USP) : Special NoteDocument9 pagesKetalar (Ketamine Hydrochloride Injection, USP) : Special NoteLou Gazo ChoNo ratings yet
- Local Anesthetics (Slide Show)Document24 pagesLocal Anesthetics (Slide Show)Sheena Lou Regencia SalomonNo ratings yet
- Ketamine A Review Update 2005Document5 pagesKetamine A Review Update 2005HAPPINESS J. BASUTUNo ratings yet
- Intravenous AnestheticsDocument5 pagesIntravenous AnestheticsPM Basiloy - AloNo ratings yet
- Ketalar KetaminDocument10 pagesKetalar KetaminLeonardo JeversonNo ratings yet
- Obat Ayu (Anestesi)Document11 pagesObat Ayu (Anestesi)Ayu PratiwiNo ratings yet
- Drug Study..DokcyDocument7 pagesDrug Study..DokcyPeArl Peralta0% (1)
- Induction AgentsDocument100 pagesInduction AgentsSulfikar TknNo ratings yet
- Sedation of Patients in ICUDocument9 pagesSedation of Patients in ICUAlfrin AntonyNo ratings yet
- DISSociative AnaesthesiaDocument3 pagesDISSociative Anaesthesiamohit jainNo ratings yet
- CardiotropicsDocument4 pagesCardiotropicsbeans taralaNo ratings yet
- Local Anesthesia and Concious SedationDocument43 pagesLocal Anesthesia and Concious Sedationpawi18No ratings yet
- Drug StudyDocument8 pagesDrug Studykarenkaren09No ratings yet
- UNIT: Internal Medicine REG NO.: BMS/2014/72732 DATE: 30/7/2021 ASSIGNMENT: Status EpilepticusDocument10 pagesUNIT: Internal Medicine REG NO.: BMS/2014/72732 DATE: 30/7/2021 ASSIGNMENT: Status EpilepticusGladys MainaNo ratings yet
- In Tub at IonDocument6 pagesIn Tub at IonWinnieChin LeeNo ratings yet
- Muscle RelaxantDocument42 pagesMuscle RelaxantMirza Shaharyar BaigNo ratings yet
- Facilitate Mechanical Ventilation in Intensive Care: AdultDocument2 pagesFacilitate Mechanical Ventilation in Intensive Care: AdultVaniNo ratings yet
- RX - Citicoline, Kalium, Ketosteril, Methycobal, Myonal, Lipolin GelDocument6 pagesRX - Citicoline, Kalium, Ketosteril, Methycobal, Myonal, Lipolin GelntootNo ratings yet
- Anasthetic DrugsDocument62 pagesAnasthetic DrugsMilda InayahNo ratings yet
- Hesi Maternity Ob PDFDocument32 pagesHesi Maternity Ob PDFcclaire197% (37)
- Suxamethonium Dosage, Side Effect MIMS - Com PhilippinesDocument2 pagesSuxamethonium Dosage, Side Effect MIMS - Com PhilippinesWay LyanNo ratings yet
- IV Anesthetic AgentsDocument72 pagesIV Anesthetic AgentsRaghavendra PrasadNo ratings yet
- Drug StudyDocument4 pagesDrug StudyTeanu Jose Gabrillo TamayoNo ratings yet
- Anesthesia Review: Vic V. Vernenkar, D.O. St. Barnabas Hospital Dept. of SurgeryDocument42 pagesAnesthesia Review: Vic V. Vernenkar, D.O. St. Barnabas Hospital Dept. of SurgeryAnil vaddiNo ratings yet
- Anesthesia ReviewDocument42 pagesAnesthesia ReviewMukhtar Khan0% (1)
- Nursing Diagnosis: Aurelio, Lyca Mae M. BSN II-DDocument2 pagesNursing Diagnosis: Aurelio, Lyca Mae M. BSN II-DLyca Mae AurelioNo ratings yet
- Atracurium BesylateDocument3 pagesAtracurium BesylateWidya WidyariniNo ratings yet
- Anti-Convulsants/Antiepileptic Drugs: Prepared By: DR Sana FaheemDocument23 pagesAnti-Convulsants/Antiepileptic Drugs: Prepared By: DR Sana Faheemaziz aliNo ratings yet
- RSI Pharmacology For The Emergency Medicine PhysicianDocument2 pagesRSI Pharmacology For The Emergency Medicine PhysicianGuide LPNo ratings yet
- Pharmacology of AnaestheticDocument72 pagesPharmacology of AnaestheticOmar HamwiNo ratings yet
- Dekinet Tablets: Use in PregnancyDocument3 pagesDekinet Tablets: Use in Pregnancyddandan_2No ratings yet
- Drug StudyDocument9 pagesDrug StudyKate Chavez100% (3)
- Drug Study 2Document8 pagesDrug Study 2rey_tengNo ratings yet
- Status EpilepticusDocument42 pagesStatus EpilepticusJesse EstradaNo ratings yet
- Post Operative CareDocument67 pagesPost Operative Care5alifa55No ratings yet
- General Anesthetic Generic Name Brand NameDocument141 pagesGeneral Anesthetic Generic Name Brand NameLouise OpinaNo ratings yet
- Antiepileptic DrugsDocument65 pagesAntiepileptic DrugsZarish IftikharNo ratings yet
- Uia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREDocument4 pagesUia 11 ANAESTHESIA AND CHRONIC RENAL FAILUREfadhiliNo ratings yet
- ORDocument7 pagesORMay EvelynNo ratings yet
- Drug File SupriyaDocument36 pagesDrug File SupriyaSalim MinjNo ratings yet
- Neuromuscular Blocking AgentsnewDocument22 pagesNeuromuscular Blocking Agentsnewvinay0717100% (1)
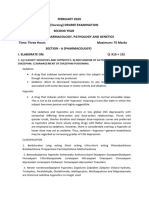
- 2020 Feb Answer KeyDocument27 pages2020 Feb Answer KeyAjitha boopathiNo ratings yet
- Drug StudyDocument7 pagesDrug StudydivineNo ratings yet
- Status Epilepticus and Its Management AssignmentDocument11 pagesStatus Epilepticus and Its Management AssignmentStanley KarugaNo ratings yet
- AnestesiDocument59 pagesAnestesiJeffrey EkaNo ratings yet
- Lecture On Pharmacology of Anesthetic Drugs: Yizez Mebratu 23APR11Document90 pagesLecture On Pharmacology of Anesthetic Drugs: Yizez Mebratu 23APR11Tefera LeteboNo ratings yet
- Cloxacillin, Sodium: How Should I Take Cloxacillin?Document7 pagesCloxacillin, Sodium: How Should I Take Cloxacillin?Stacy MC PelitoNo ratings yet
- Silicon NPN Power Transistors: Inchange Semiconductor Product SpecificationDocument3 pagesSilicon NPN Power Transistors: Inchange Semiconductor Product SpecificationdenitoNo ratings yet
- Ebook PDF Campbell Essential Biology 6th Edition by Eric J Simon PDFDocument41 pagesEbook PDF Campbell Essential Biology 6th Edition by Eric J Simon PDFmary.martin56997% (35)
- MsdsDocument10 pagesMsdsmcgteccadNo ratings yet
- Departmental Acc.Document22 pagesDepartmental Acc.Somsindhu Nag100% (2)
- Di450 Di550 GeneralDocument115 pagesDi450 Di550 GeneralSMART REFILLNo ratings yet
- Rereading Rudyard Kipling's Kim in The Light of The Notion 'Dialogue of Civilizations': A Multicultural PerspectiveDocument14 pagesRereading Rudyard Kipling's Kim in The Light of The Notion 'Dialogue of Civilizations': A Multicultural Perspectivesakura yuimikoNo ratings yet
- Pentel Ink Pen - Google SearchDocument1 pagePentel Ink Pen - Google SearchDhruv WNo ratings yet
- LG DVD LH-D6430Document54 pagesLG DVD LH-D6430videosonNo ratings yet
- Level Five Chapter (Azad)Document17 pagesLevel Five Chapter (Azad)Tajmohammad ZarifNo ratings yet
- E2 PTAct 2 9 1 DirectionsDocument2 pagesE2 PTAct 2 9 1 DirectionsAsad RiazNo ratings yet
- Methods of Rainwater HarvestingDocument11 pagesMethods of Rainwater HarvestingAnantHimanshuEkkaNo ratings yet
- (WHO) Intensive Care Unit (ICU)Document4 pages(WHO) Intensive Care Unit (ICU)desiveronikaNo ratings yet
- Daleys Notebook The Magic Memories 105Document8 pagesDaleys Notebook The Magic Memories 105AndreaClementePancotti100% (1)
- Online Learning Amid The COVID-19 Pandemic: Students PerspectivesDocument8 pagesOnline Learning Amid The COVID-19 Pandemic: Students PerspectivesMichelle Gliselle Guinto MallareNo ratings yet
- (COOPER-LIGHTING) Lighting Design GuideDocument2 pages(COOPER-LIGHTING) Lighting Design Guidejay.divsNo ratings yet
- Chapter 050Document23 pagesChapter 050dtheart2821100% (5)
- Syllabus 4th SemDocument3 pagesSyllabus 4th SemPrianca PrathapNo ratings yet
- Role Play The Evolution of NursingDocument6 pagesRole Play The Evolution of NursingEvien FrancheskaNo ratings yet
- Use in North America vs. Europe: Outdoor SpaceDocument27 pagesUse in North America vs. Europe: Outdoor SpaceDB FasikaNo ratings yet
- Enjoy Your T PDF Package!: RainsDocument85 pagesEnjoy Your T PDF Package!: RainsslixsterNo ratings yet
- The Revised MSX Red BookDocument302 pagesThe Revised MSX Red BookfreeTerp100% (1)
- Cooling Load Calculation ProcedureDocument2 pagesCooling Load Calculation ProcedurezampacaanasNo ratings yet
- Sandwich PDFDocument26 pagesSandwich PDFIvan BorodavkaNo ratings yet
- Dezinfectia AmprentelorDocument6 pagesDezinfectia Amprentelorbarby17_2005No ratings yet
- My Dreaming PreschoolDocument36 pagesMy Dreaming PreschoolrosalindaNo ratings yet
- The - Irish - Times Top 1000 Page 5,6Document2 pagesThe - Irish - Times Top 1000 Page 5,6glad.deeringNo ratings yet
- Sunjoy A102008100 Assembly Instruction enDocument35 pagesSunjoy A102008100 Assembly Instruction enTerrence JonesNo ratings yet
- Speaking Scripts PDFDocument36 pagesSpeaking Scripts PDFGurjinder Singh100% (2)
- Pengumuman Kelulusan PMB PKN STAN Prodi Diploma I, III, IV PKN STAN 2017Document2 pagesPengumuman Kelulusan PMB PKN STAN Prodi Diploma I, III, IV PKN STAN 2017Shely NoviaNo ratings yet
- BS en 00931-1998Document20 pagesBS en 00931-1998Amer AmeryNo ratings yet