Professional Documents
Culture Documents
Audit Poster 5
Uploaded by
api-286232866Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Audit Poster 5
Uploaded by
api-286232866Copyright:
Available Formats
Service evaluation: Identifying the reasons for decreased patient interaction with East Coast Community Healthcare (ECCH)
using Self-Referral cards
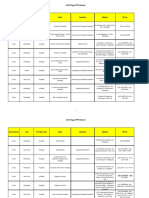
Introduction: Demographic Value
Articles and papers on self-referral (SR) systems in general state:
• Number of participants 36
Direct access to healthcare encourages
autonomy from patients, allowing for AHP's to use Gender (Percentage of Male participants) 42%
their time more effectively to treat people who are in
need (Riggare, 2016).
• When direct access is used, it is Age (mean age and sd) 71 sd=10.7
not for inappropriate reasons (Ferguson, Griffin and
Mulcahy, 1999), so the service is not being misused. Percentage of TKR patients contacted 56%
• One drawback is that some patients,
especially elderly, struggle to navigate these systems. With the Average interval between discharge and 17 days
lack of knowledge of the job role and promotion of patient- final attempted phone call
directed systems, underuse of the service is seen (Igwesi-
Chidobe et al., 2020). Percentage of phone calls answered 92% (33/36)
• NICE Guidelines state that patients should be able to actively
participate in their care NICE (2021).
Implications:
Following discharge from orthopedic knee/hip surgery, patients who are • Drawing a conclusion from this data, the procedure used to give the SR
not referred by the hospital are given a SR card to contact ECCH for PT need information is mostly effective, and the reason for decreased contact with
be. Since the introduction of the self-referral system, ECCH is that patients feel they don't need it.
The East Coast Community Healthcare (ECCH) team have highlighted the fact • As 10 participants do not recall being given the card, the inpatient services
that the uptake of SR is lower than expected. may need to be improved to ensure that patients are able to remember
what the card is and its purpose. While also possibly changing the format
This audit plans to identify the true percentage of patients failing to self- of the card to make it easier to remember, record keeping can also be
refer to ECCH after elective joint replacement surgery and find out the altered to ensure that all eligible patients are given a card.
reasons why. • Further research can be done with a larger sample size to see if these
findings are true. While additional research can explore why patients did
not feel they need physiotherapy.
Methods:
A Data Protection Impact Assessment form and Good Clinical Practice/ Reference list
Ferguson, A., Griffin, E. and Mulcahy, C. (1999). Patient Self-referral to Physiotherapy in
Information Governance training was completed prior to any patient contact. General Practice - A Model for the New NHS? Physiotherapy, 85(1),
Telephone calls were made to patients between 1-4 weeks post discharge pp.13–20. doi:https://doi.org/10.1016/s0031-9406(05)66059-2.
from JPUH. Closed and open-ended questions were used allow for qualitative Igwesi-Chidobe, C.N., Bishop, A., Humphreys, K., Hughes, E., Protheroe, J., Maddison, J. and
and quantitative data. Bartlam, B. (2020). Implementing patient direct access to musculoskeletal physiotherapy in
A flow map and script was used during phone calls, for consistency and to By Lucas Van-Eda & Ollie Sutton (Student Physiotherapists) primary care: views of patients, general practitioners, physiotherapists and clinical
commissioners in England. Physiotherapy. doi:https://doi.org/10.1016/j.physio.2020.07.002.
reduce researcher bias.
NICE (2021). 1 Guidance | Patient experience in adult NHS services: improving the experience
The results of these phone calls were collected in an excel spreadsheet along of care for people using adult NHS services | Guidance | NICE. [online] Nice.org.uk. Available
Acknowledgements:
with demographic information and analysed to find common themes. The at:
Orthopedic team
data was stored securely on an Excel spreadsheet. https://www.nice.org.uk/guidance/cg138/chapter/1-Guidance#enabling-patients-to-actively-
Research team participate-in-their-care
Information governance team .
Riggare, S. (2016). Self referral to physiotherapy and other services would empower patients
Reference list
Ferguson, A., Griffin, E. and Mulcahy, C. (1999). Patient Self-referral to Physiotherapy in
General Practice - A Model for the New NHS? Physiotherapy, 85(1), pp.13–20.
doi:https://doi.org/10.1016/s0031-9406(05)66059-2.
Igwesi-Chidobe, C.N., Bishop, A., Humphreys, K., Hughes, E., Protheroe, J., Maddison,
J. and Bartlam, B. (2020). Implementing patient direct access to musculoskeletal
physiotherapy in primary care: views of patients, general practitioners, physiotherapists
and clinical commissioners in England. Physiotherapy.
doi:https://doi.org/10.1016/j.physio.2020.07.002.
NICE (2021). 1 Guidance | Patient experience in adult NHS services: improving the
experience of care for people using adult NHS services | Guidance | NICE. [online]
Nice.org.uk. Available at:
https://www.nice.org.uk/guidance/cg138/chapter/1-Guidance#enabling-patients-to-activel
y-participate-in-their-care
.
Riggare, S. (2016). Self referral to physiotherapy and other services would empower
patients and doctors. BMJ, p.h6977. doi:https://doi.org/10.1136/bmj.h6977.
•Methods:
A DPIA (GIVE FULL WORDS BEFORE USING ACRONYM) form and GCP (LIST FULL
WORDS) / information governance (IG) training was completed prior to any patient
contact.
Telephone calls were made to patients between 1-4 weeks post discharge from JPUH.
Closed and open-ended questions were used allow for qualitative and quantitative
data.
A flow map and script was used during phone calls, for consistency and to reduce
Methods: researcher bias.
Demographic data of 36 patients collected into a spreadsheet; this is stored The results of these phone calls were collected in an excel spreadsheet along with
securely to avoid risks to confidentiality. demographic information and analysed to find common themes. The data was stored
securely on an Excel spreadsheet.
A DPIA form and GCP/ information governance training was completed prior
to any patient contact.
Phone calls were provided to patients 1-4 weeks post discharge from JPUH.
Closed and open-ended questions are used allow for qualitative and
quantitative data.
A flow map and script was used during phone calls, this is used to help keep
consistency across all patients and avoid researcher bias.
The results of these phone calls was collected in an excel spreadsheet and is
analysed to find common themes.
You might also like
- DHS v. New York Motion To Lift or Modify StayDocument261 pagesDHS v. New York Motion To Lift or Modify StayWashington Free BeaconNo ratings yet
- Nursing Responsibilities For The Patient Will Undergo Cardiac CatheterizationDocument4 pagesNursing Responsibilities For The Patient Will Undergo Cardiac CatheterizationCharlene Jacobe Cornista100% (1)
- Previous Board Exam Questions No RatioDocument56 pagesPrevious Board Exam Questions No RatioNovemia Rose TisonNo ratings yet
- Kuwait Hospital Annual ReportDocument84 pagesKuwait Hospital Annual ReportHosam GomaaNo ratings yet
- Case Quality Management - Mayra SalirrosasDocument2 pagesCase Quality Management - Mayra Salirrosasmayra salirrosas100% (1)
- Gregory, S., Bolling, D. R., & Langston, N. F. (2014) - Partnerships and New Learning Models To Create The Future Perioperative Nursing WorkforceDocument11 pagesGregory, S., Bolling, D. R., & Langston, N. F. (2014) - Partnerships and New Learning Models To Create The Future Perioperative Nursing WorkforceJohnson100% (1)
- p5 - Remote Monitoring Systems For Chronic PatientsDocument12 pagesp5 - Remote Monitoring Systems For Chronic PatientsShruthi KrishnamoorthyNo ratings yet
- Su 2023Document8 pagesSu 2023Toheeb LasisiNo ratings yet
- 21 - Telemedicine InrehabilitationDocument11 pages21 - Telemedicine InrehabilitationMariaNo ratings yet
- Bettger 2019Document9 pagesBettger 2019Ade Maghvira PutriNo ratings yet
- Week 2 - 410 NURDocument5 pagesWeek 2 - 410 NURCherie BoyerNo ratings yet
- The Perception and Knowledge About Episiotomy: A Cross-Sectional Survey Involving Healthcare Workers in A Low-And Middle-Income CountryDocument6 pagesThe Perception and Knowledge About Episiotomy: A Cross-Sectional Survey Involving Healthcare Workers in A Low-And Middle-Income Countrydior00No ratings yet
- 7 PubmedDocument12 pages7 PubmedNydia Isabel Ruiz AntonioNo ratings yet
- Hcin 540 - Finished Final Project PDFDocument12 pagesHcin 540 - Finished Final Project PDFapi-562816202No ratings yet
- Jurnal Telenursing Athiqah Syukri 2BDocument2 pagesJurnal Telenursing Athiqah Syukri 2BAthiqah SyukriNo ratings yet
- Perez Mengual, M. - s0134775 (Verslag)Document61 pagesPerez Mengual, M. - s0134775 (Verslag)Silvio MoralesNo ratings yet
- Patient Satisfaction With Telehealth Vs Inperson Hand Therapy A Retrospective Review of Results of An Online Satisfaction SurveyDocument7 pagesPatient Satisfaction With Telehealth Vs Inperson Hand Therapy A Retrospective Review of Results of An Online Satisfaction Surveyanita awNo ratings yet
- The Effects of Information Technology On Perioperative NursingDocument16 pagesThe Effects of Information Technology On Perioperative NursingBagus Adi PratamaNo ratings yet
- The Effects of A Structured Communication Tool in Patients Wit 2023 EClinicaDocument12 pagesThe Effects of A Structured Communication Tool in Patients Wit 2023 EClinicaronaldquezada038No ratings yet
- Electronic Hospital Information System Implemented Trincomaleean Experience Reengineering 2161 0711.S2 001Document7 pagesElectronic Hospital Information System Implemented Trincomaleean Experience Reengineering 2161 0711.S2 001Kite DireNo ratings yet
- Providing Higher Value Care Through Population Health Management: What Is The Radiologist 'S Role?Document2 pagesProviding Higher Value Care Through Population Health Management: What Is The Radiologist 'S Role?Camilo SotomayorNo ratings yet
- Benefits - and - Challenges - of - Ele 6Document7 pagesBenefits - and - Challenges - of - Ele 6silfianaNo ratings yet
- Digital Professionalism in Patient Care A Case Based Survey of PatientsDocument8 pagesDigital Professionalism in Patient Care A Case Based Survey of PatientsJane OrsalNo ratings yet
- Comparing Digital To Conventional Physical Therapy For ChronicDocument18 pagesComparing Digital To Conventional Physical Therapy For ChronickiranNo ratings yet
- Measuring Patient Satisfaction A Case StudyDocument5 pagesMeasuring Patient Satisfaction A Case Studyapouakone apouakoneNo ratings yet
- Ane Publish Ahead of Print 10.1213.ane.0000000000005208Document10 pagesAne Publish Ahead of Print 10.1213.ane.0000000000005208Ananth BalakrishnanNo ratings yet
- A Clinical Decision Support Framework For Heterogeneous Data SourcesDocument10 pagesA Clinical Decision Support Framework For Heterogeneous Data SourcesdineshshaNo ratings yet
- MDD1816 PDFDocument10 pagesMDD1816 PDFdineshshaNo ratings yet
- Adding Insult To Injury Journal CritiqueDocument1 pageAdding Insult To Injury Journal Critiqueapi-357707616No ratings yet
- A Study of Patient Satisfaction Level in Inpatient Spine Department of A Tertiary Care Multi-Speciality HospitalDocument6 pagesA Study of Patient Satisfaction Level in Inpatient Spine Department of A Tertiary Care Multi-Speciality Hospitalimran_chaudhryNo ratings yet
- Clinical Decision Support SystemDocument13 pagesClinical Decision Support SystemUdit Kheterpal100% (1)
- In Telehealth, Physiotherapists Can Triage Orthopedic Waiting Lists: Pilot StudyDocument7 pagesIn Telehealth, Physiotherapists Can Triage Orthopedic Waiting Lists: Pilot StudyIJAR JOURNALNo ratings yet
- CAA - Alterações CognitivasDocument21 pagesCAA - Alterações CognitivasMaria JoãoNo ratings yet
- 2022 - Educational Nursing Intervention in Reducing Hospital Readmission A Systematic ReviewDocument15 pages2022 - Educational Nursing Intervention in Reducing Hospital Readmission A Systematic ReviewArthurNo ratings yet
- Patient Acceptance For Computer Use in Outpatient DepartmentDocument9 pagesPatient Acceptance For Computer Use in Outpatient DepartmentEarl RomanosNo ratings yet
- Olalekan Et Al. 2019Document12 pagesOlalekan Et Al. 2019karamabbaskeremNo ratings yet
- Acute Care For The Elderly: A Literature Review: Mary Ann Liebert, IncDocument9 pagesAcute Care For The Elderly: A Literature Review: Mary Ann Liebert, IncWatson AbatNo ratings yet
- Development of Common Data Elements To Provide Tele Self-Care ManagementDocument5 pagesDevelopment of Common Data Elements To Provide Tele Self-Care Managementvovinda rujianaNo ratings yet
- CDSSDocument16 pagesCDSSMartinus CiputraNo ratings yet
- J Ajem 2019 158384Document9 pagesJ Ajem 2019 158384Zira RizkaNo ratings yet
- A Class Based Approach For Medical Classification of Chest PainDocument5 pagesA Class Based Approach For Medical Classification of Chest Painsurendiran123No ratings yet
- Time For A Patient-Driven Health Information Economy?: PerspectiveDocument4 pagesTime For A Patient-Driven Health Information Economy?: PerspectiveanggiNo ratings yet
- Socko Low 2014Document8 pagesSocko Low 2014Tri Monarita JohanNo ratings yet
- Article 1Document15 pagesArticle 1Mart Joseph SenoNo ratings yet
- International Journal of Pharmacy Practice AbstractsDocument40 pagesInternational Journal of Pharmacy Practice AbstractsFabiola NogaNo ratings yet
- Hassling2003 Article AWeb-BasedPatientInformationSyDocument12 pagesHassling2003 Article AWeb-BasedPatientInformationSyddineshkumar51144No ratings yet
- HCE-Medicina GeneralDocument9 pagesHCE-Medicina GeneralSimon RojasNo ratings yet
- 1-10 Commandments of Effective CDS ElecSept2021Document8 pages1-10 Commandments of Effective CDS ElecSept2021TTJNo ratings yet
- Introduction:-: Journal HomepageDocument6 pagesIntroduction:-: Journal HomepageIJAR JOURNALNo ratings yet
- Valuing Variance: The Importance of Variance Analysis in Clinical Pathways UtilisationDocument6 pagesValuing Variance: The Importance of Variance Analysis in Clinical Pathways Utilisationismail ajiNo ratings yet
- IntroductionDocument7 pagesIntroductionshadrack mutindaNo ratings yet
- 2011 ICTD DecisionSupport Paper PDFDocument12 pages2011 ICTD DecisionSupport Paper PDFNurrochman FerdiansyahNo ratings yet
- Assessment of Patient Satisfaction in Public Hospitals in Cyprus A Descriptive StudyDocument13 pagesAssessment of Patient Satisfaction in Public Hospitals in Cyprus A Descriptive StudyerwhuanNo ratings yet
- CDSS NotesDocument6 pagesCDSS NotesShreeja SPNo ratings yet
- Impact of Technology in Better Dispersal of HealthDocument4 pagesImpact of Technology in Better Dispersal of Healthvasthu broto ariyoNo ratings yet
- Kruse2018 TheUseOfElectronicHealthRecordDocument16 pagesKruse2018 TheUseOfElectronicHealthRecordalNo ratings yet
- Matic Pablo Pantig Patungan Peralta Nursing Informatics Final Requirement Conduct of Research Writing Thru Scoping ReviewDocument11 pagesMatic Pablo Pantig Patungan Peralta Nursing Informatics Final Requirement Conduct of Research Writing Thru Scoping ReviewYuuki Chitose (tai-kun)No ratings yet
- Demographic and Clinical Predictors of ResponseDemographic and Clinical Predictors of ResponseDocument8 pagesDemographic and Clinical Predictors of ResponseDemographic and Clinical Predictors of ResponseDara Mayang SariNo ratings yet
- Musculoskeletal Science and PracticeDocument7 pagesMusculoskeletal Science and PracticeShaun TylerNo ratings yet
- Capstone PaperDocument25 pagesCapstone Paperapi-512644800No ratings yet
- Translate AnakDocument12 pagesTranslate AnakAndikNo ratings yet
- Running Title: Digital Vs Conventional Implant Impressions: DDS, MS, PHDDocument41 pagesRunning Title: Digital Vs Conventional Implant Impressions: DDS, MS, PHDÁł ÃăNo ratings yet
- Envisioning A Learning Healthcare SystemDocument6 pagesEnvisioning A Learning Healthcare SystemOmWawanNo ratings yet
- The Effect of Early Ambulation On Patient Outcomes For Total Joint ReplacementDocument4 pagesThe Effect of Early Ambulation On Patient Outcomes For Total Joint ReplacementAris PurnomoNo ratings yet
- Clinical Decision Support System: Fundamentals and ApplicationsFrom EverandClinical Decision Support System: Fundamentals and ApplicationsNo ratings yet
- Draft 12 - PosterDocument1 pageDraft 12 - Posterapi-286232866No ratings yet
- 5Document1 page5api-286232866No ratings yet
- Relieving Anxiety in Patients Undergoing Cataract SurgeryDocument1 pageRelieving Anxiety in Patients Undergoing Cataract Surgeryapi-286232866No ratings yet
- Methodology: CCS Research Champions Programme: Evaluating The Impacts On ParticipantsDocument1 pageMethodology: CCS Research Champions Programme: Evaluating The Impacts On Participantsapi-286232866No ratings yet
- Identifying Barriers To Mobilisation of Patients in The Queen Elizabeth Hospital King's LynnDocument1 pageIdentifying Barriers To Mobilisation of Patients in The Queen Elizabeth Hospital King's Lynnapi-286232866No ratings yet
- Kate NichollsDocument1 pageKate Nichollsapi-286232866No ratings yet
- CRNM Census Report Final 2023Document45 pagesCRNM Census Report Final 2023api-286232866No ratings yet
- Whywedoresearch How Are You 07Document3 pagesWhywedoresearch How Are You 07api-286232866No ratings yet
- Racheal Crane Babyloss Awareness Case Studies 20th March 2023Document1 pageRacheal Crane Babyloss Awareness Case Studies 20th March 2023api-286232866No ratings yet
- Edp 070817 Infant Formula Research 1Document1 pageEdp 070817 Infant Formula Research 1api-286232866No ratings yet
- Blog Doc 2Document2 pagesBlog Doc 2api-286232866No ratings yet
- Meet Hilda... : Special Edition!Document6 pagesMeet Hilda... : Special Edition!api-286232866No ratings yet
- Blog DocumentDocument1 pageBlog Documentapi-286232866No ratings yet
- Nursing Times Article 2015Document2 pagesNursing Times Article 2015api-286232866No ratings yet
- The Impact of Step-Down Unit Care On Patient Outcomes After ICU DischargeDocument7 pagesThe Impact of Step-Down Unit Care On Patient Outcomes After ICU DischargeJHNo ratings yet
- Product Information - DHA Plans Table of BenefitsDocument8 pagesProduct Information - DHA Plans Table of BenefitsAhmedNo ratings yet
- Noor Medical Complex - Erbil, IRAQDocument2 pagesNoor Medical Complex - Erbil, IRAQNoor DoctorsNo ratings yet
- ICAI HS360 WithoutDuductibleDocument52 pagesICAI HS360 WithoutDuductiblepadiNo ratings yet
- Resident Physician (MedicineDocument7 pagesResident Physician (MedicineEngr Md. Mamun RassalNo ratings yet
- The Brooklyn Cancer Center Welcomes Asmat Ullah, MDDocument2 pagesThe Brooklyn Cancer Center Welcomes Asmat Ullah, MDPR.comNo ratings yet
- MSQH 5th Edition Draft Standard 1 - Governance Leadership DirectionDocument40 pagesMSQH 5th Edition Draft Standard 1 - Governance Leadership DirectionEsmar A. Hamid KenohNo ratings yet
- Procedure Checklist Hot and Cold Application: Camarines Sur Polytechnic CollegesDocument2 pagesProcedure Checklist Hot and Cold Application: Camarines Sur Polytechnic CollegesElaine Frances IlloNo ratings yet
- Session 1. Drug and Therapeutics Committee-OverviewDocument12 pagesSession 1. Drug and Therapeutics Committee-OverviewNunik Dewi KumalasariNo ratings yet
- Residency Manual 2020 28-Dec-2020Document127 pagesResidency Manual 2020 28-Dec-2020Asif KhanNo ratings yet
- Ao 2020-0047Document41 pagesAo 2020-0047D Alfz EinsTein JDNo ratings yet
- BENEFICENCE MEaningDocument2 pagesBENEFICENCE MEaningcyrene gabaoNo ratings yet
- Topic 7 JOB DESCRIPTIONDocument20 pagesTopic 7 JOB DESCRIPTIONSimon JosanNo ratings yet
- Test Bank For Understanding The Essentials of Critical Care Nursing 2nd Edition Kathleen PerrinDocument26 pagesTest Bank For Understanding The Essentials of Critical Care Nursing 2nd Edition Kathleen PerrinRoger Enriquez100% (26)
- MHC PMS OverviewDocument2 pagesMHC PMS OverviewArbias Gashi0% (1)
- Experiences:: Personal DataDocument2 pagesExperiences:: Personal DataMariel NaborNo ratings yet
- Caring Situation Paper 2 - Nurs 452Document8 pagesCaring Situation Paper 2 - Nurs 452api-558100249No ratings yet
- Assignment Sheet PDFDocument13 pagesAssignment Sheet PDFعبدالرحمن علىNo ratings yet
- Egypt Approved Medical Providers PharmaciesDocument115 pagesEgypt Approved Medical Providers PharmaciesAhmed AliNo ratings yet
- Paradigm Shift EssayDocument10 pagesParadigm Shift Essayapi-456202876No ratings yet
- AAOS Code of ConductDocument187 pagesAAOS Code of ConductongchenguanNo ratings yet
- Letter OxygenDocument2 pagesLetter OxygenMarco BaltazarNo ratings yet
- LM First Chapter SampleDocument11 pagesLM First Chapter SampleNikita JacobsNo ratings yet
- Professional ReferenceDocument2 pagesProfessional ReferenceFrancis ContaoiNo ratings yet
- AH102 Module 3Document50 pagesAH102 Module 3leona edwardsNo ratings yet