Professional Documents
Culture Documents
female genital pathology
Uploaded by
Singitan Siyoum0 ratings0% found this document useful (0 votes)
2 views62 pagesFemale genital pathology 2024
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentFemale genital pathology 2024
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views62 pagesfemale genital pathology
Uploaded by
Singitan SiyoumFemale genital pathology 2024
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 62
Female genital pathology
Dr. Tafesse S. Hurisa( MD)
CERVICITIS
• Defn: inflammation of cervix
–can be subclassified as infectious or
noninfectious
• Causative agents of infectious cervicitis
–Chlamydia trachomatis accounts for 40% of
cases,
–Ureaplasma urealyticum,
–T. vaginalis, Neisseria gonorrhoeae,
–HSV-2 , and certain types of HPV.
• Clinical presentation
–leukorrhea.
–profuse, odorless, nonirritating, and white-to
yellow vaginal discharge.
–intermenstrual or postcoital vaginal bleeding.
• treated empirically with antibiotics that are
active against chlamydia and gonococcus.
NEOPLASIA OF THE CERVIX
• HPV, the causative
agent of cervical
neoplasia, has a
tropism for the
immature
squamous cells of
the transformation
zone.
concepts on HPV
• It is a double-stranded DNA virus with a protein capsid
unique to each viral type.
• Clinically classified as :
– high-risk (h.rHPV) :serotypes 16, 18, 31, 33, 35, 45, and
58,accounts for 95 percent of cervical cancer cases
worldwide.
– low-risk (lrHPV) : serotypes 6 and 11 cause nearly all
genital warts, laryngeal papillomas,
• transmitted by direct, usually sexual contact with
the genital skin, mucous membranes, or body
fluids of a person with HPV infection.
Possible consequences of HPV
infection.
HPV lnfection Prevention
• Sexual abstinence, delaying coitarche,
and limiting the number of sexual partners
• Vaccines
–The quadrivalent HPV vaccine for types 6, 11,
16, and 18, and Gardasil 9 is a nonavalent HPV
vaccine (9vHPV) against HPV types 6, 11, 16,
18, 31, 35, 45, 52, and 58.
– is recommended for all females age 9–45,
with target age 11–12.
Risk factors for CIN and
invasive carcinoma
• Early age at first intercourse
• Multiple sexual partners
• Male partner with multiple previous sexual
partners
• Persistent infection by high-risk strains of
papillomavirus
Risk factors...
• Multiple pregnancies
• Oral contraceptive use
• Smoking
• Immuno-suppression
cervical intra-epithelial
neoplasia (CIN)/SIL
• precancerous epithelial change
• common at the squamocolumnar junction
(transformation zone).
• peaks in incidence at about 30 years of age.
Classification of SIL
Screening
• Early detection of SIL is the rationale for
the Papanicolaou (Pap) test, in which
cells are scraped from the transformation
zone and examined microscopically.
• Age 21-65yrs @ 3ys interval
• CIN show a progression of changes on
histologic examination:
–Low grade SIL (squamous intraepithelial lesion
)
–High grade SIL
–Carcinoma insitu
–Superficially invasive squamous cell
carcinoma
–Invasive squamous cell carcinoma
INVASIVE CERVICAL
CANCER
• The most common cervical carcinomas
are :
–squamous cell carcinomas (75%), followed by
–adenocarcinomas and
–mixed adenosquamous carcinomas (20%)
and
–small cell neuroendocrine carcinomas (<5%).
Clinical Features
• peak age =45 years
• postcoital vaginal bleeding .
• unexpected vaginal bleeding, leukorrhea,
painful coitus (dyspareunia), or dysuria.
and lower extremity pain and edema.
• The primary treatment is hysterectomy
and lymph node dissection;
• small microinvasive carcinomas may be
treated with cone biopsy.
• Radiation and chemotherapy are also of
benefit in instances where surgery alone
is not curative.
ABNORMAL UTERINE
BLEEDING
• menorrhagia: profuse or prolonged
bleeding at the time of the period.
• metrorrhagia: irregular bleeding between
the periods.
• postmenopausal bleeding.
Causes of AUB
Leiomyoma/fibroids
• are the most common benign tumor in
females,
–affecting 30% to 50% of women of
reproductive age.
• more frequent in black women.
• Their growth is estrogen dependent .
Clinical features
• often asymptomatic.
• menorrhagia, with or without metrorrhagia.
• abdominal mass, pelvic/back pain ,
• suprapubic discomfort , or infertility and
spontaneous abortion .
• Grossly , leiomyomas form well-
circumscribed, rubbery, white-tan masses
with a whorled, trabeculated appearance
on cut section.
• Leiomyomas are commonly multiple,and
may have subserosal, intramural, and
submucosal location .
Endometrial Carcinoma
• is the most frequent cancer occurring in
the female genital tract.
• It generally appears between the ages of
55 and 65 years
• endometrioid and serous carcinoma are
the 2 common histologic form.
Risk factors
• Endometrioid adenocarcinoma (most
common histological type): associated
with PTEN tumor suppressor gene
mutations
• Serous tumors: associated with TP53
tumor suppressor gene mutations
Clinical Features
• irregular or postmenopausal bleeding.
• With progression, the uterus enlarges and
may become affixed to surrounding
structures as the cancer infiltrates
surrounding tissues.
prognosis
• Stage is the major determinant of survival
in both types.
• Serous tumors tend to manifest more
frequently with extrauterine extension and
therefore have a worse prognosis than
endometrioid carcinomas.
Ovaries
• POLYCYSTIC OVARIAN SYNDROME
• TUMORS OF THE OVARY
PCOS/Stein-Leventhal
syndrome
• is a complex endocrine disorder
characterized by hyperandrogenism,
menstrual abnormalities, polycystic
ovaries, chronic anovulation, and
decreased fertility.
• This is due to high circulating androgens
and high circulating insulin levels causing
arrest of follicular development invarious
stages.
Clinical features
• irregular vaginal bleeding.
• infertility
• obesity and hirsutism.
• Bilateral Ovarian enlargement.
–On ultrasound the ovaries demonstrate the
presence of the necklace-like pattern of multiple
peripheral cysts (20–100 cystic follicles in each
ovary ).
• Histologic examination shows a thickened,
fibrotic ovarian capsule overlying
innumerable cystic follicles lined by
granulosa cells with a hyperplastic
luteinized theca interna.
• There is a conspicuous absence of
corpora lutea in the ovary.
Ovarian Tumors
Epithelial ovarian tumors
• are the most common form of ovarian
tumor (80%).
• occur predominantly in postmenopausal
women.
• These include serous, mucinous,Brenner,
endometrioid, and clear cell tumors.
• The most common malignant epithelial
cell type is serous cystadenocarcinoma.
RF
• Well-differentiated serous tumors show
psammoma bodies and a lining similar to
that of the fallopian tube.
• Mucinous tumors commonly have goblet
cells like intestinal mucosal cells.
–CA 125 can be used to follow treatment .
Psammoma Bodies (Concentric
Calcifications)
Ovarian Germ Cell
Tumors(15%)
• Teratoma (dermoid cyst )
–>95% of ovarian (but not testicular) teratomas
are benign;
–commonly occurs in early reproductive years
–Include elements from all 3 germ cell layers:
ectoderm (skin, hair, adnexa,neural tissue),
mesoderm (bone,cartilage),and endoderm
(thyroid, bronchial tissue)
–Complications include torsion,
rupture,and malignant transformation
–Can contain hair, teeth, and sebaceous
material
–The term struma ovarii is used when
there is a preponderance of thyroid tissue
–Immature teratoma is characterized by
histologically immature tissue
Dysgerminoma
• Malignant; commonly occurs in children
and young adults
• Risk factors include Turner syndrome and
disorders of sexual development
• Gross and microscopic features are similar
to seminomas
• Are radiosensitive; prognosis is good
Ovarian Sex Cord–Stromal
Tumors(5%)
• Ovarian fibroma
–Most common stromal tumor; forms a firm,
white mass
–Meigs syndrome refers to the combination of
fibroma, ascites, and pleural effusion .
Granulosa cell tumor
• Potentially malignant, estrogen-producing
tumor
• Presentation depends on age:
–Prepuberal patients with juvenile granulosa
cell tumor present with precocious puberty
–Reproductive age patients present with
irregular menses
–Postmenopausal patients present with vaginal
bleeding
• Complications include endometrial hyperplasia
and cancer
• Tumor forms a yellow-white mass that
microscopically shows polygonal tumor cells and
formation of follicle-like structures (Call-Exner
bodies)
• Primary sites for metastatic tumor to the ovary
include breast cancer,colon cancer,endometrial
cancer,and gastric “signet-ring cell” cancer
(Krukenberg tumor).
Breast Pathology
• The glandular portion of the breast is
composed of 12 to 15 independent ductal
systems that each drains approximately 40
lobules.
• Each lobule consists of 10 to 100 milk-
producing acini that empty into small
terminal ducts
• About 80–85% of normal breast tissue is
fat during the reproductive years.
BREAST FIBROADENOMA
• Fibroadenomas are the most common
breast tumors found in adolescents and
young women.
• In approximately 15% of patients they
occur as multiple lesions.
• Clinically, fibroadenomas are discrete,
smoothly contoured, rubbery, nontender,
freely moveable masses.
• The most distinctive gross feature of
fibroadenomas that allows them to be
distinguished from other breast lumps is
their mobility .
• Microscopically, the mass shows
proliferation of benign stroma,ducts,and
lobules.
FIBROCYSTIC CHANGES
• formerly called fibrocystic disease.
• divided into three groups, nonproliferative
disease, proliferative disease without
atypia, and proliferative disease with
atypia.
• primarily affect women in their
reproductive years.
• most often involve the upper outer
quadrant and may produce a palpable
mass or nodularity.
• Nonproliferative disease
–consists of three major morphologic changes:
cysts, fibrosis, and adenosis.
–It is termed “nonproliferative” because the
lesions contain single layers of epithelial cells.
–not associated with an increased risk of breast
cancer.
• Proliferative disease without atypia
–includes epithelial hyperplasia, sclerosing
adenosis, complex sclerosing lesion, and
papilloma.
–Each is associated with varying degrees of
epithelial cell proliferation.
–associated with a slightly increased risk of
breast cancer.
Proliferative disease with atypia
– includes atypical lobular hyperplasia (ALH)
and atypical ductal hyperplasia (ADH).
– ALH closely resembles lobular carcinoma in
situ (LCIS) and
– ADH closely resembles ductal carcinoma in
situ (DCIS) but are more limited in extent.
– The cells in ADH are uniform in appearance
and form sharply marginated spaces or rigid
bridges
– 13% to 17% of women with these lesions
develop breast cancer.
Breast Carcinoma
• is the most common cancer in women.
• Risk factors.
–Age(>50yrs)
–Unusually long / intense exposure to
estrogens (long length of reproductive
life,nulliparity, obesity, exogenous estrogens)
–Presence of proliferative fibrocystic changes,
especially atypical hyperplasia
–First–degree relative with breast cancer
• Hereditary influences are thought to be
involved in 5‒10% of breast cancers, with
important genes as follows:
–BRCA1 (error–free repair of DNA double-
strand breaks) chromosome 17q21
–BRCA2 (error–free repair of DNA double-
strand breaks) chromosome 13q12.3
–TP53 germline mutation (Li -Fraumeni
syndrome)
morphologic classifications
A.Noninvasive
1.Ductal carcinoma in situ
2.Lobular carcinoma in situ
B.Invasive
1.Invasive ductal carcinoma —70% to 80%
2.Invasive lobular carcinoma—~10% to 15%
3.Carcinoma with medullary features— ~5%
4.Mucinous carcinoma (colloid carcinoma) ~5%
5.Tubular carcinoma— ~5%
6.Other types
Triple assessment of breast
symptoms.
• Breast cancer is
most common in
the upper outer
quadrant .
• Gross examination of a breast cancer typically
shows a stellate, white-tan, gritty mass.
• Clinically, it can cause:
–Mammographic calcifications or architectural
distortion
–Palpable solitary painless mass
–Nipple retraction or skin dimpling
–Fixation of breast tissue to the chest wall
Inflammatory carcinoma
• Prognosis is dependent on the biologic
type of tumor, stage, and the availability of
treatment modalities.
THANK YOU
You might also like
- Deped Teachers Health CardDocument8 pagesDeped Teachers Health CardMarjorie Jacinto-Tañala100% (1)
- Germ Cell Tumor Ovary PDFDocument70 pagesGerm Cell Tumor Ovary PDFmelysaNo ratings yet
- Molly's Case StudyDocument10 pagesMolly's Case StudyYounas BhattiNo ratings yet
- Cancer in Reproductive Tract.ppt.Document29 pagesCancer in Reproductive Tract.ppt.Muskan TiwariNo ratings yet
- Endometrial Malignancies 1Document41 pagesEndometrial Malignancies 1jerrydanfordfxNo ratings yet
- Benign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDocument83 pagesBenign & Precancerous Tumors of Female Genital Organs: by Assist. O.V.BakunDian Permata PutraNo ratings yet
- BreastDocument50 pagesBreastعلي عليNo ratings yet
- Benign Ovarian Tumors-1Document45 pagesBenign Ovarian Tumors-1abdulghani100% (1)
- 1.female Genital SystemDocument114 pages1.female Genital Systemأسود / BlackNo ratings yet
- Genetalia Wanita: Tuti Andayani, SppaDocument60 pagesGenetalia Wanita: Tuti Andayani, SppaFariz Auliadi KhalilNo ratings yet
- Ovarian TumoursDocument41 pagesOvarian TumoursVlad RazvanNo ratings yet
- Ovarian TumorDocument59 pagesOvarian Tumorapi-1991639980% (5)
- Path Pathology of The Ovaries and Fallopian Tubes Part 1 2020-2021Document12 pagesPath Pathology of The Ovaries and Fallopian Tubes Part 1 2020-2021JohnNo ratings yet
- Pathology of The OvaryDocument7 pagesPathology of The OvaryLorMD34No ratings yet
- PA Genitalia WanitaDocument100 pagesPA Genitalia WanitaBNo ratings yet
- Benign Neoplasms of The Genital 2Document22 pagesBenign Neoplasms of The Genital 2ugonna nwokeNo ratings yet
- Narag, MarkDocument64 pagesNarag, MarkChristian PasicolanNo ratings yet
- Benign and Malignant Cervical LesionsDocument46 pagesBenign and Malignant Cervical LesionsRohitNo ratings yet
- FGTDocument248 pagesFGTAmanuel MaruNo ratings yet
- Click Here For Video: Pathology of The Uterus, Part 2 Cheryl A. Hanau, M.DDocument11 pagesClick Here For Video: Pathology of The Uterus, Part 2 Cheryl A. Hanau, M.DJohnNo ratings yet
- Disordered of The Breast: Abdelkarim BarqawiDocument63 pagesDisordered of The Breast: Abdelkarim BarqawiRazan HaimounyNo ratings yet
- Surgical Posting - Testicular TumoursDocument16 pagesSurgical Posting - Testicular TumoursDiyana ZatyNo ratings yet
- 11 - SurgpathDocument22 pages11 - Surgpathemely p. tangoNo ratings yet
- OvariantumoursDocument56 pagesOvariantumoursArwa QishtaNo ratings yet
- Ovarian TumDocument69 pagesOvarian TumFangNo ratings yet
- Benign Breast DisordersDocument30 pagesBenign Breast DisordersShams Nadeem AlamNo ratings yet
- Breast Cancer Presentation FinalDocument69 pagesBreast Cancer Presentation Finalakinpe1100% (1)
- Endometrial Cancer: Manuela RussuDocument38 pagesEndometrial Cancer: Manuela RussuAnonymous 0XqZUl06PmNo ratings yet
- Box-07. (FGT+MGT) PDFDocument11 pagesBox-07. (FGT+MGT) PDFfoisaliffatNo ratings yet
- Different Pathologies of The UterusDocument74 pagesDifferent Pathologies of The UterusAmal100% (1)
- Carcinoma Vulva - FinalDocument70 pagesCarcinoma Vulva - FinalAastha Jain100% (1)
- 11 BreastDocument22 pages11 Breastluckyswiss7776848No ratings yet
- Cervical Intraepithelial Neoplasia and Cervical CancerDocument28 pagesCervical Intraepithelial Neoplasia and Cervical CancerNatnael100% (1)
- Female Path 93013Document135 pagesFemale Path 93013Kelompok BelajarNo ratings yet
- Ovarian TumorsDocument69 pagesOvarian Tumorskarin02No ratings yet
- Learning Unit 8 - Neoplasia of The FGT Part 3Document15 pagesLearning Unit 8 - Neoplasia of The FGT Part 3Marelize ErasmusNo ratings yet
- The Male Genital SystemDocument57 pagesThe Male Genital Systembessan alfqeatNo ratings yet
- Breast CancerDocument32 pagesBreast Cancerjames garcia100% (1)
- Carcinoma Breast GuideDocument8 pagesCarcinoma Breast GuideYeshvi s100% (1)
- Neoplasms of Testis NishDocument54 pagesNeoplasms of Testis NishRamesh ReddyNo ratings yet
- Neoplastic Diseases of The OvaryDocument61 pagesNeoplastic Diseases of The Ovaryea013No ratings yet
- Malignant Diseases of The OvaryDocument64 pagesMalignant Diseases of The OvaryGÖKSU SAYGILINo ratings yet
- NTU Breast Pathology 2024Document72 pagesNTU Breast Pathology 2024Chen HouyuNo ratings yet
- Disease of Female Reproductive System: Maria Picu, MDDocument66 pagesDisease of Female Reproductive System: Maria Picu, MDAbanoub AwadallaNo ratings yet
- Etiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsDocument33 pagesEtiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsNatasya Ayusandra MahersaputriNo ratings yet
- Benign Ovarian MassDocument39 pagesBenign Ovarian MassVidhi Chaudhary100% (1)
- Breast PathologDocument51 pagesBreast Pathologjusttin779No ratings yet
- Cervical Cancer Screening and DiagnosisDocument137 pagesCervical Cancer Screening and DiagnosisBhattarai ShrinkhalaNo ratings yet
- 3.diseases of The BreastDocument87 pages3.diseases of The Breastأسود / BlackNo ratings yet
- Septiya Agestin Cahyaningrum - Malignancy in Reproductive Health System - WordDocument30 pagesSeptiya Agestin Cahyaningrum - Malignancy in Reproductive Health System - WordSepty KawaiNo ratings yet
- Endometrial Cancer Diagnosis and TreatmentDocument9 pagesEndometrial Cancer Diagnosis and TreatmentAhmed Butt100% (1)
- Ovary PDFDocument62 pagesOvary PDFBatool SherbiniNo ratings yet
- Neoplastic Diseases of The OvaryDocument61 pagesNeoplastic Diseases of The Ovarysandeepv08No ratings yet
- Salivary Glands TumoursDocument102 pagesSalivary Glands TumoursSokna SyNo ratings yet
- Xv. Ultrasound Evaluation of The AdnexaDocument13 pagesXv. Ultrasound Evaluation of The AdnexajamiladeguzmanabcdefghijklmNo ratings yet
- Pre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5Document147 pagesPre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5FarazNo ratings yet
- Endometrial NeoplasiaDocument48 pagesEndometrial NeoplasiaBONI M.WoyessaNo ratings yet
- Benign Salivary Gland Tumors - Dr. Nermine El Bahey (2019-2020)Document13 pagesBenign Salivary Gland Tumors - Dr. Nermine El Bahey (2019-2020)MOHAMED AMINNo ratings yet
- Uterine Body Carcinoma - DRJDocument35 pagesUterine Body Carcinoma - DRJJyoti MishraNo ratings yet
- Endometrial Cancer: A Comprehensive Resource for Patients and FamiliesFrom EverandEndometrial Cancer: A Comprehensive Resource for Patients and FamiliesNo ratings yet
- EDEMADocument12 pagesEDEMASingitan SiyoumNo ratings yet
- hypertensive disorders of pregnancyDocument32 pageshypertensive disorders of pregnancySingitan SiyoumNo ratings yet
- inflammation and tissue repairDocument55 pagesinflammation and tissue repairSingitan SiyoumNo ratings yet
- Endocrine PathologyDocument60 pagesEndocrine PathologySingitan SiyoumNo ratings yet
- Hypertensive Disorder in Pregnancy-5-19-2015-ZimbabweDocument39 pagesHypertensive Disorder in Pregnancy-5-19-2015-ZimbabwedanielNo ratings yet
- Case Study: Acute GlomerulonephritisDocument19 pagesCase Study: Acute GlomerulonephritisKuruma Maricar SorianoNo ratings yet
- Congenital Anomaly 15-09-2015Document116 pagesCongenital Anomaly 15-09-2015gibranNo ratings yet
- Cognitiveimpairmentand Dementiainparkinson Disease: Jennifer G. Goldman,, Erica SiegDocument13 pagesCognitiveimpairmentand Dementiainparkinson Disease: Jennifer G. Goldman,, Erica SiegJuan Carlos Carbajal SilvaNo ratings yet
- Stroke Disease Risk Factors and TreatmentDocument3 pagesStroke Disease Risk Factors and TreatmentHardianti YahyaNo ratings yet
- Tatsumi 1997Document9 pagesTatsumi 1997dad dzd adaNo ratings yet
- Klubsybear Additional Recalls: Hematology A.karyolysisDocument2 pagesKlubsybear Additional Recalls: Hematology A.karyolysisMartin ClydeNo ratings yet
- Anatomy and Physiology of The ThoraxDocument6 pagesAnatomy and Physiology of The ThoraxdocaliNo ratings yet
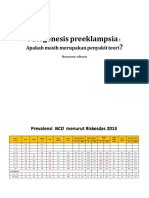
- Patogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFDocument49 pagesPatogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFFellita Ratri ANo ratings yet
- Acute PancreatitisDocument23 pagesAcute PancreatitisBibaswan ChakrabartyNo ratings yet
- The Corsi Block-Tapping Task Standardization and Normative DataDocument7 pagesThe Corsi Block-Tapping Task Standardization and Normative DataLidio ClementeNo ratings yet
- ICD 10 Penyakit KardiovaskularDocument20 pagesICD 10 Penyakit KardiovaskularMaya ShofiaNo ratings yet
- Impact of Excessive Mobile Phone Usage On Human JCSB 1000235Document5 pagesImpact of Excessive Mobile Phone Usage On Human JCSB 1000235nidNo ratings yet
- Cleft Lip and Palate GuideDocument29 pagesCleft Lip and Palate Guideمحمد محمود القحيفNo ratings yet
- Confidential Client Health HistoryDocument3 pagesConfidential Client Health HistoryHelen A. AmoraNo ratings yet
- Blood Transfusion Guide: Types, Storage, Indications & ComplicationsDocument61 pagesBlood Transfusion Guide: Types, Storage, Indications & ComplicationsshikhaNo ratings yet
- Gingival Tissue Management Methods for Dental RestorationsDocument20 pagesGingival Tissue Management Methods for Dental RestorationsSriram PugalenthiNo ratings yet
- Secondary GlaucomaDocument57 pagesSecondary GlaucomaBasudev chNo ratings yet
- Acute Abdominal Pain MCQs and ManagementDocument4 pagesAcute Abdominal Pain MCQs and ManagementAsim NiazNo ratings yet
- Stroke: Dr. Fidha Rahmayani, M.SC, SP.S Fakultas Kedokteran Universitas Lampung RS Abdul MulukDocument45 pagesStroke: Dr. Fidha Rahmayani, M.SC, SP.S Fakultas Kedokteran Universitas Lampung RS Abdul Mulukdhea nadhiaNo ratings yet
- Skin LayersDocument3 pagesSkin LayersCrackmcat CrackmcatNo ratings yet
- DocumentDocument128 pagesDocumentHardi OtoyNo ratings yet
- Art Dolor GeriátricoDocument9 pagesArt Dolor GeriátricoarrlyNo ratings yet
- Magnesium sulfate medicationDocument2 pagesMagnesium sulfate medicationAndrea ANo ratings yet
- Choose The Correct Answer For Questions (1 - 90)Document12 pagesChoose The Correct Answer For Questions (1 - 90)حمزة الفنيني100% (3)
- Review - SurgeryDocument40 pagesReview - SurgerymedstudNo ratings yet
- Pterygium - EyeWikiDocument1 pagePterygium - EyeWikiPaudel SujanNo ratings yet
- Related LiteratureDocument16 pagesRelated LiteratureivahcamilleNo ratings yet