Professional Documents
Culture Documents
Facial Protocol
Facial Protocol
Uploaded by
deepaliarnejaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Facial Protocol
Facial Protocol
Uploaded by
deepaliarnejaCopyright:
Available Formats
PHYSICAL THERAPY
MANAGEMENT FOR
FACIAL NERVE PARALYSIS
Prepared by:
Committee of Physical Therapy Protocols
Office of Physical Therapy Affairs
Ministry of Health Kuwait
2007
With collaboration of:
Physical Therapy Department
Kuwait University
ACKNOWLEDGEMENT
Our sincere thanks and gratitude to Ministry of Health for its
continuous support and encouragement that extended to us.
And, I extend my sincere thanks to all committee members of the
physical therapy protocol for their excellent work in preparation of this
scientific material and to the physical therapy department in Kuwait
University for their participation in this endeavor.
Lastly, I would like to dedicate this protocol to all colleagues with in
the profession, medical team members, and who are interested in
physical therapy profession, wishing that this booklet will be useful and
helpful toward improving physical therapy services in Kuwait.
With best wishes.
Director of physical therapy affairs
NABEEL Y. ALHUNAIF, P.T., B.Sc.
Committee of Physical Therapy Protocols
Ali Al-Mohanna M.Sc. P.T. (Farwaniya Hospital)
Khadijah Al-Ramezi, P.T. (Ibn Sina Hospital)
Lobna A. Abdulkareem, P.T. (Al-Adan Hospital)
Noura Al-Jwear, P.T. (Farwaniya Hospital)
Maali Al-Ajmi, P.T. (Maternity Hospital)
Dr. Surreya Mohomed B.Sc.; D.Ed. (Kuwait University)
Note: This protocol is a guideline only and it may vary from
patient to patient.
Definition:
It is a neurological condition that results from a lesion of the 7
th
cranial
nerve leading to an acute onset of weakness or total paralysis on the
ipsilateral side of the face.
Causes:
1) Bells palsy*
2) Ramsey-Hunt syndrome**
3) Middle ear infection
4) Trauma
5) Tumors
6) Post acoustic neuromas surgery
7) During surgery injuries.
* Although idiopathic facial paralysis ( Bells Palsy), is the most
common cause of unilateral facial paralysis accounting for
proximately 50% of the causes. its important for clinicians to
consider all causes to avoid overlooking potentially life-threatening
disease.
1,2,4
** A condition caused by herpes zoster of the geniculate ganglion
of the brain or neuritis of the facial nerve and characterized by
severe facial palsy and vesicular eruption in the pharynx, external
ear canal, tongue, and occipital area. Deafness, tinnitus, and vertigo
may be present.
3
Time of intervention: As soon as the patient reaches physiotherapy
department.
Physical Therapy Assessment:
- Assessment should be finished within the first 3 sessions.
(Appendix A for assessment sheet and guidelines).
- Documentation can be done by photo- and/or video recordings
for static and dynamic movement (eyes closed, blowing,
smiling, etc.) can be included.
Goals:
1) To educate / reassure the patient about the condition.
2) To relief pain.
3) To establish the bases for re-education of muscle and nerve
conduction.
4) To re-educate sensation if involved (sensory integration: touch,
2 point discrimination, temperature)
5) To facilitate / improve muscle contraction.
6) To facilitate / improve facial symmetry.
7) To prevent complications.
Frequency of treatment:
Frequency of treatment sessions differs according to the severity and
prognosis of each patient. However, by using the House classification
system for re-evaluating the patient, its suggested to have;
Month Session / Week
1
st
3 sessions per week
2
nd
twice per week
3
rd
once a week
Patient should then be referred to the physician for further evaluation if
no progression is noticed. A period of 14 months is allowed for
recovery.
4
Management:
Patient Education and Reassurance:
4,5,14
1) Explain the condition to the patient; its causes, incidence, prognosis
and treatment.
2) Re-assure the patient, but be realistic (dont give high expectations).
3) Advice the patient to take the prescribed medication from the
physician, and to avoid therapy given by non professionals. Explain
to the patient that taking medication and following the physical
therapy program are enough.
4) If eyes are involved, the patient should do the following:
a) Use eye drops ( as the physician prescribed)
b) Dont expose yourself to direct sunlight, being too close to TV
light, or strong room lighting
c) Wear sun glasses to protect eyes
d) Dont exhaust eyes by reading for long time
e) Avoid direct contact with air conditioners
5) Explain to the patient how the psychological state can affect the
treatment, so avoid any emotional conflict and seek family or friend
support to increase self awareness and self esteem.
6) Be aware of postural imbalance (especially for Ramsey-Hunt
syndrome).
7) Follow the given home program.
Treatment options:
The options available for physical therapy management to achieve
the mentioned goals are as follows.
A. Electrotherapy
B. Neuromuscular retraining
C. Manual massage
D. Kabat rehabilitation.
A) Electrotherapy:
6
(Appendix B)
According to reviewed studies about the effect of
electrotherapy modalities used for treatment of facial nerve
paralysis it was found that neither modalities had a superior
effect; (electrotherapy modalities can be used as an adjunct
therapy)
The electrotherapy modalities reviewed included: electrical
stimulation (ES), electromyography biofeedback (EMG
bio), ultrasound, laser, and short-wave diathermy (SWD).
a) Electrotherapy still lacking evidence due to inappropriate
research methodology, small sample size, inadequate
treatment parameter, inconsistent follow up
b) No evidence support electrical stimulation benefit for acute
facial paralysis but it's effective for chronic condition
c) Biofeedback is more effective when muscle activity presents
d) No evidence supports the benefit of using continues mode of
short wave diathermy, while pulse mode can facilitate healing
process in acute condition
e) Lazar still has no study supporting to use it with acute or
chronic condition
f) Ultrasound can be beneficial for acute conditions, but there
is lack of statistical support since research still not
investigating it's long effect
g) ES & EMG bio are efficient to be use with chronic
condition.
15
other studies consider ES as contraindicated due
to its interruption of re-innervations
4,16
Therapist has to use his/her clinical judgment and skills to
determine the best modality to be used according to the clinical
presentation of the condition
Considering the Physiological effects of electrotherapy
modalities & the stage of the disease can help in facial
paralysis management
Lesion recovery depend on type of lesion, age, nutritional &
metabolic status of the patient
Effect of electrotherapy in relation to classification of lesion
6, 7
1. Neuropraxia: nerve conduction is block temporary with
preserve axon, it's response to electrical stimuli, and usually has
a complete recovery
Ultrasound effective to reduce edema & provide normal
healing environment (still no appropriate parameter
recommended)
Studies prefer to delay use ES unless poor prognosis factors
present, also galvanic current still not prove it's beneficial.
Pulsed SWD used to facilitate healing & reduce edema (no
study review found, but according to physiological affect)
Lazar increases the energy of the inflammatory area, also
consider as anti inflammatory, recommended to use it for
elderly with poor metabolic or nutrition
EMG bio is not effective due to absent of muscle
contraction
2. Axonotmesis: axon is interrupted but with intact nerve sheath
and axon regenerated 1mm/day, potential has a complete
recovery
Research
6
mention that using the ES for 3 h/day, can lead to
change capillary density
EMG bio will be effective as voluntary movement present,
help to prevent synkinesis
Ultrasound & heat have a poor efficiency, while Laser can
be effective at this phase
(Further studies need to prove relevance of modalities on
healing process)
3. Endoneurotmesis: endoneurium & axon are destroy while
perineurium is intact, axon regenerate with scar lead to partial
re-innervation & synkinesis therefore incomplete recovery
4. Perineurotmesis: only epineurium is intact while other nerve
tissues destroyed, lead to abnormal regeneration, synkinesis &
incomplete recovery
5. Neurotmesis: complete nerve rupture with little or no
regeneration & recovery option, can develop painful neuromas
beside the nerve
ES & EMG bio may maintain muscle tone
ES is significant with nerve or muscle grafting, according to
its physiological affect such as improving circulation
B) Neuromuscular retraining:
4, 7, 16
Neuromuscular retraining is applied using selective motor
training to facilitate symmetrical movement and control
undesired gross motor activity (synkinesis*).
Patient re-education is the most important aspect of the
treatment process. EMG feedback and/or specific mirror
exercises will provide a sensory feedback to promote learning.
When each muscle group is being assessed, the patient observes
the action of these muscles in the mirror and instructed to
perform small symmetrical specific movements on the sound
side to identify the right response. Each patient presents with
different functional disability, so there are no general list of
exercises.
As patient identifies the specific area of dysfunction, patient can
begin to perform exercise to improve facial movements' guided
by the affected side so isolated muscle response is preserved
and coordination improved. Repetitions & frequency of
exercises can be modified according to improvement status
(appendix C)
The movements should be initiated slowly and gradually so that
the patient can observe the angle, strength, and speed of each
movement, because rapid movements can't help the patient in
controlling the abnormal movement (synkinesis).
The patient can apply a manual resistance as isolated facial
movement improved in affected side to be obvious without
synkinesis.
Synkinesis:
The site of synkinesis should be identified in order to teach the
patient how to control abnormal movement pattern.
The treatment of synkinesis depends on inhibition of the
unwanted movements that occur during volitional &
spontaneous movements; by perform facial movement slowly
without triggering the abnormal movement. Stretching is
recommended here to prevent muscles tightness.
C) Manual Massage:
17
Massage can be performed in conjunction with other treatment
options. It can be done to improve perceptual awareness.
Massage manipulations on the face include:
1. Effleurage
2. Finger or thumb kneading
3. Wringing
4. Hacking
5. Tapping
6. Stroking
* An involuntary movement of one part occurring simultaneously with
reflex or voluntary movement of another part
3
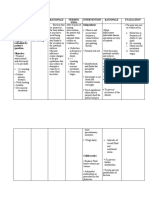
D) Kabat Rehabilitation
12
Kabat rehabilitation is type of motor control rehabilitation
technique based on proprioceptive neuromuscular facilitation
(PNF).
During Kabat, therapist facilitate the voluntary contraction of
the impaired muscle by applying a global stretching then
resistance to the entire muscular section and motivate action by
verbal input and manual contact. (table 1)
When performing Kabat, 3 regional are considered: the upper
(forehead and eyes), intermediate (nose), and lower (mouth).
Prior to Kabat, ice stimulation has to perform to a specific
muscular group, in order to increase its contractile power.
Table 1: Kabat Rehabilitation
Resistance Stretch Muscle
O
r
b
i
c
u
l
a
r
i
s
O
r
i
s
Z
y
g
o
m
a
t
i
c
m
a
j
o
r
L
e
v
a
t
o
r
L
a
b
i
i
S
u
p
e
r
i
o
r
i
s
D
i
l
a
t
o
r
N
a
r
e
s
a
n
d
N
a
s
a
l
e
s
P
r
o
c
e
r
u
s
Resistance Stretch Muscle
O
r
b
i
c
u
l
a
r
i
s
O
c
u
l
i
C
o
r
r
u
g
a
t
o
r
S
u
p
e
r
c
e
l
l
i
F
r
o
n
t
a
l
i
s
M
e
n
t
a
l
i
s
Prognosis:
2,4,8,11,18,
19
The majority of patients with facial nerve paralysis (about 85%)
begin to recover within the first 3 weeks after onset.
While about 15% of patients, recovery begins after 2 to 3
months from onset.
Satisfactory recovery of facial paralysis was reported to achieve
grade 1 or 2 on the House-Brackmann Grading System.
Poor recovery is usually determined after 6 months of onset.
Poor recovery notice for patients with history of diabetes,
hypertension and obesity
Table 2: Risk Factors that may lead to poor prognosis:
High Risk
Factors
NET* response
Significant worse recovery seen in (83%)
of patients who showed poor or no
response to NET on the affected side.
Recovery after
a month of
onset
79% of Patients who exhibit grade 4 and
above after 1 month will have poor
prognosis than patients with grade 3 or
less.
Moderate
Risk
Factors
Severity of
facial paralysis
47% of Patients with severe paralysis
(grade 5 and above) had poor prognosis
than patients with incomplete paralysis
(grade 4 and below).
Age 26% of patients above 50 years old had
significant poor prognosis.
Low Risk
Factors
Cause of facial
paralysis
24% of patients with VZV** cause had
significant poor prognosis than other
causes.
Stapedial
reflex***
If the stapedial muscle reflex is absent,
only 20% will have poor prognosis.
* Nerve excitability test, examined by ENT specialist
** varicella-zoster virus
*** examined by ENT specialist.
Appendix (A)
MINISTRY OF HEALTH
HOSPITAL: _______________________
Physical Therapy Department
Facial Paralysis Assessment
Patients Name: ___________________________
File No: __________ Telephone: ____________
Age: __________ Gender: M F
Nationality: ________ Occupation:___________
Date of Referral: __________________________
Referring Physician: _______________________
D.O. Admission: / / . OP Ward: Room: Bed:
D.O. Assessment: / / . Diagnosis: __________________________________________
PRESENT HISTORY (D.O. Onset: ___________________________)
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
Receiving Traditional Treatment: ______________________________________________________________
PAST MEDICAL HISTORY (include number of years):
Heart Disease Prior CVA / TIA DM Type: Cancer
Hypertension Lung Disease Previous Episode Other:
Details: ___________________________________________________________________________________
SOCIAL HISTORY
______________________________________________________________________________________________
____________________________________________________________________________________________
PSYCHOLOGICAL IMPACT Anxious Depressed Concerned Other:
__________________________________________________________________________________________
MEDICATION Analgesic Corticosteroids Antibiotic Antiviral
_______________________________________________________________________________________________
PATIENT'S CONCERN: ____________________________________________________________________
__________________________________________________________________________________________
OBSERVATION / ASSOCIATED CONDITIONS
Facial asymmetry Synkinesis Otorrhea Headache
Blurred vision Drooling Otalgia Vertigo
Lacrimation Taste disturbance Tinnitus Hearing impairment
Bell's phenomenon Parathesthesis Other: ________________________________________
PAIN (location, description, intensity)
_______________________________________________________________________________________________
__________________________________________________________________________________________
SENSATION
_______________________________________________________________________________________________
__________________________________________________________________________________________
FUNCTIONAL STATUS
_____________________________________________________________________________________ _____ _____
_______________________________________________ __ _ ____________________ _________________ ___
_.=. \ _=,,= _>= ,,,. == \= -=\ ,
F
A
C
I
A
L
P
A
R
A
L
Y
S
I
S
A
S
S
E
S
S
M
E
N
T
P
.
T
.
FACIAL MUSCLE STRENGTH
Date
Muscle Grade
Frontalis
Corrugator
Orbi. oculi
Procerus
Dialator Nasalis
Risorius
Zygomaticus major
Orbi. oris
Levator labii superioris
Levator anguli oris
Key: F: Functional, WF: Weak Functional, NF: Non Functional, O: Absent
HOUSE-BRACKMANN CLASSIFICATION OF FACIAL FUNCTION
Date
Grade
Key: 1: Normal, 2: Slight, 3: Moderate, 4: Moderately severe, 5: Severe, 6: Total paralysis
PRECAUTIONS _______________________________________________________________________________
PROBLEM LIST TREATMENT GOALS
Pain:
Difficulty closing eye or dry eye
Difficulty with facial expressions
Face feels stiff
Impairment of sensation
Difficulty eating & drinking (items fall out of
the weak corner of the month)
Other:
TREATMENT PLAN:
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
______________________________________________________________________________________________
P.T. Name & Signature: _____________________
Database for Facial Paralysis Assessment
Present History: progression of disease and date of onset
Receiving Traditional Treatment: if yes, list the type of traditional treatment patient
received
Past Medical History: other relevant medical problems / conditions (CVA:
cerebrovascular accident, TIA: transient ischemic
attacks, DM: diabetic mellitus), previous episode and
treatment
Social History: marital status, living situation, occupation and hobbies
Psychological Impact: patient emotional status e.g. anxious, depressed or concerned
(worried) .etc.
Medication: list of current medications, dose and times of day
Patient Concern: what the patient wants to achieve
Observation / Associated Conditions: description of observations of patient on 1
st
assessment and any
associated problems or
conditions e.g.:
o Synkinesis: abnormal regeneration of the facial nerve resulting in a cross-wiring in the
muscle motor end plates. e.g.: when the patient smiles, his eyelid closes on the
affected side
o Lacrimation: an outflow of tears, weeping
o Otorrhea: discharge from the external auditory meatus
o Otologia: pain in the ear
o Tinnitus: a buzzing, thumping or ringing sound in the ear
o Bell's phenomenon: rolling of the eyeball upward & outward when an attempt is made
to close the eye on the side of the face affected in peripheral facial paralysis
Pain: site (mastoid, facial nerve exit or cervical), type and grade of pain (use Visual
Analogue Scale or Numerical Analogue Scale )
Sensation: test light touch, temperature and any abnormal sensory feelings
Functional Status: picture of present lifestyle, and limitation in self care activities e.g.
feeding
Facial Muscle Strength: muscle test as per Oxford grading (key illustrated)
House-Brackmann Classification of Facial Function: describe the facial functional status
Grade Degree Description
Gross At rest At motion
1 Normal Normal facial
function in all
nerve branches
Normal facial
function in all
nerve branches
Normal facial function
in all nerve branches
2 Slight Slight weakness
on close
inspection,
slight
asymmetry
Normal tone &
symmetry
Forehead: good to
moderate movement
Eye: complete closure
with minimum effort
Mouth: slight
asymmetry
3 Moderate Obvious but not
disfiguring facial
asymmetry.
Synkinesis is
noticeable but not
severe. may have
hemi- facial spasm or
contracture
Normal tone &
symmetry
Forehead: slight to
moderate movement
Eye: complete closure
with effort
Mouth: slight weakness
with maximum effort
4 Moderately
severe
Asymmetry is
disfiguring &/or
obvious facial
weakness
Normal tone &
symmetry
Forehead: no movement
Eye: incomplete closure
Mouth: asymmetrical
with maximum effort
5 Severe Only slight,
barely
noticeable
movement
Asymmetrical
facial
appearance
Forehead: no movement
Eye: incomplete closure
Mouth: slight movement
6 Total
paralysis
No facial
function
No facial
function
No facial function
Precaution: an action done to avoid possible danger, discomfort, etc
Problem List: concise summary of main problems observed from assessment, which require
intervention
Treatment Goals: specific, achievable, objective goals with time frame
Treatment Plan: specific outline of treatment plan, essential details of treatment procedures
with specific treatment techniques
Appendix (B)
Appendix (C)
References
1. Bleicher JN, Hamiel BS, Gengler JS. A survey of facial paralysis:
etiology and incidence. Ear Nose Throat J 1996; 75:355-8.
2. Brach JS, VanSwearingen JM. Not all facial paralysis is Bell's palsy:
a case report. Arch Phys Med Rehabil 1999; 80: 857-9.
3. Thomas CL (1997): Taber's cyclopedic medical dictionary. F.A.Davis
Company. Philadelphia.
4. Brach JS, VanSwearingen. Physical therapy for facial paralysis: a
tailored treatment approach. Phys Ther. 1999; 79:397-404.
5. Carlson DS, Pfadt E. When your patient has acute facial paralysis:
learn to distinguish between Bell's palsy and Ramsy Hunt syndrome.
Nursing 2005; 35: 54-55.
6. Quinn R, Cramp F. The efficacy of electrotherapy for Bell's palsy: a
systematic review. Phys Ther Reviews 2003; 8: 151-164.
7. Cronin GW, Steenerson RL. The effectiveness of neuromuscular
facial retraining combined with electromyography in facial paralysis
rehabilitation. Otolaryngology-Head and Neck Surgery 2003; 128:
534-538.
8. Petruzzelli G, Hirsch B. Bell's palsy: a diagnosis of exclusion.
Postgrad Med 1991; 90:115-23.
9. Li J, Goldberg G, Munin MC, Wagner A, and Zafonte R. Post-
traumatic bilateral facial palsy: a case report and literature review.
Brain Injury 2004; 18: 315-320.
10. Van Gelder RS, Phillippart SMM, and Bernard BGES. Effects of
myofeedback and mime-therapy on peripheral facial paralysis.
Internat J of Psycho 1990; 25: 191-211.
11. Ikeda M, Abiko Y, Kukimoto N, Omori H, Nakazato H, and Ikeda K.
Clinical factors that influence the prognosis of facial nerve paralysis
and the magnitude of influence. Laryngoscope 2005; 115: 855-860.
12. Barbara M, Monini S, Buffoni A, Cordier A, Ronchetti F, Harguindey
A, Di Stadio A, Cerruto R, and Filipo R. Early rehabilitation of facial
nerve deficit after acoustic neuroma surgery. Acta Otolaryngol 2003;
123: 932-935.
13. Shafshak TS. The treatment of facial palsy from the point of view of
physical and rehabilitation medicine. Eura Medicophys 2006; 42: 41-
47.
14. Sugiura M, Niina R, Ikeda M, Nakazato H, Abiko Y, Kukimoto N,
and Ohmae Y. An assessment of Psychological stress in patients with
facial palsy. Nippon Jibiinkoka Gakkai Kaiho 2003; 106:491-8.
15. Targan RS, Alon G, and Kay SL. Effect of long term electrical
stimulation on motor recovery and improvement of clinical residuals
in patients with unresolved facial nerve palsy. Otolaryngol Head
Neck Surg 2000; 122:246-52.
16. Diels HJ. Facial paralysis: is there a role for a therapist?. Facial Plast
Surg 2000; 16:361-4
17. Margaret Hollis (1992): Massage for Therapists. Blackwell Scientific
Publications. Oxford.
18. Peitersen E. Natural history of Bell's Palsy. Am J Otol 1982; 4: 107-
11
19. Zgorzalewicz M, Laksa B. Physical therapy in peripheral facial
paresis. Neurol Neurochir Pol 2001; 35: 111-24
You might also like
- B14 Facial Electrical NewDocument8 pagesB14 Facial Electrical NewDan ManoleNo ratings yet
- QuizzesDocument13 pagesQuizzesmonggokaburNo ratings yet
- G8 Develop and Maintain Effectiveness at WorkDocument4 pagesG8 Develop and Maintain Effectiveness at WorkcarmenNo ratings yet
- Microneedling Consent Aftercare FormDocument5 pagesMicroneedling Consent Aftercare FormMalgorzata wojtowiczNo ratings yet
- Beauty Therapy-L1 (Cur) PDFDocument154 pagesBeauty Therapy-L1 (Cur) PDFImtiyaz67% (3)
- Elleebana Lash Lift TrainingDocument2 pagesElleebana Lash Lift TrainingOlivia JordanNo ratings yet
- What Are Extremes of IntelligenceDocument4 pagesWhat Are Extremes of IntelligenceNikki Flores80% (5)
- Facial Aftercare AdviceDocument2 pagesFacial Aftercare AdvicerobertNo ratings yet
- Beauty TherapyDocument20 pagesBeauty TherapyMeor Muhammad Shukri100% (1)
- Health and SpaDocument6 pagesHealth and SpaJeremy Jasper CembranoNo ratings yet
- Spa BodyworksDocument450 pagesSpa BodyworksAdriano Barbir100% (3)
- Start and Run A Successful Beauty Salon - A Comprehensive Guide To Managing or Acquiring Your Own SalonDocument273 pagesStart and Run A Successful Beauty Salon - A Comprehensive Guide To Managing or Acquiring Your Own Salondeepankar100% (5)
- CIDESCO CertificationDocument1 pageCIDESCO CertificationSandip PatilNo ratings yet
- BodyWrap PDFDocument24 pagesBodyWrap PDFm100% (2)
- Mckenzie ExtDocument4 pagesMckenzie ExtmohamedwhateverNo ratings yet
- The Unicorn Patient PDFDocument130 pagesThe Unicorn Patient PDFAmanda TrebianoNo ratings yet
- Skin Cleansing-Wps OfficeDocument4 pagesSkin Cleansing-Wps OfficeAngela AlejandroNo ratings yet
- Massage Business ProposalDocument21 pagesMassage Business ProposalJunarNo ratings yet
- Spa Manager or Spa Consultant or Spa Training AmbassadorDocument2 pagesSpa Manager or Spa Consultant or Spa Training Ambassadorapi-77404779No ratings yet
- Dermabrasion Micro DermabrasionDocument5 pagesDermabrasion Micro DermabrasionMalek AmamouNo ratings yet
- Basic Model User'S ManualDocument4 pagesBasic Model User'S ManualDokterYolanda100% (1)
- Starting An Ecd CentreDocument28 pagesStarting An Ecd CentreJoseph OyomNo ratings yet
- Spa Treatment MenuDocument32 pagesSpa Treatment MenuEmelia Jugdav100% (1)
- Peeling and Microdermabrasion Changes HystologicalsDocument6 pagesPeeling and Microdermabrasion Changes HystologicalsBrian MacíaNo ratings yet
- Contra-Indications: NVQ Level 2 Beauty TherapyDocument24 pagesContra-Indications: NVQ Level 2 Beauty TherapyUzma Khan100% (1)
- Esthetician/paramedical AestheticianDocument2 pagesEsthetician/paramedical Aestheticianapi-121459287No ratings yet
- Creative Short Courses and Master ClassesDocument32 pagesCreative Short Courses and Master ClassesNHCollege0% (1)
- Student HandbookDocument2 pagesStudent Handbookapi-305903882No ratings yet
- Provide Facial Electrotherapy TreatmentsDocument23 pagesProvide Facial Electrotherapy TreatmentsrobertNo ratings yet
- What Is Facial Massage PDFDocument1 pageWhat Is Facial Massage PDFlisniskytherapiesNo ratings yet
- CIDESCO Model Consent Form For Eyelash TintingDocument1 pageCIDESCO Model Consent Form For Eyelash Tintingmatina papaspyrouNo ratings yet
- What Are The Benefits of Dermaplaning and How Much Does It Cost?Document2 pagesWhat Are The Benefits of Dermaplaning and How Much Does It Cost?Daniel CalderonNo ratings yet
- CosmetologyDocument11 pagesCosmetologymhslanguagesNo ratings yet
- Salon Safety OERDocument83 pagesSalon Safety OERRishabh MishraNo ratings yet
- 16 A P Integumentary HandoutDocument19 pages16 A P Integumentary Handoutapi-300931855No ratings yet
- Spa Menu PDFDocument14 pagesSpa Menu PDFFrankNo ratings yet
- Manual MicrodermabrasionDocument56 pagesManual MicrodermabrasionÁlvaro RubioNo ratings yet
- Hair Growth Treatment Programv2Document3 pagesHair Growth Treatment Programv2Ryan RiyyanNo ratings yet
- Introduction To Body WrapsDocument28 pagesIntroduction To Body WrapsRely Emmanuel FloresNo ratings yet
- Effectiveness of SOP For SPADocument20 pagesEffectiveness of SOP For SPASafi abd rahman100% (1)
- Desk Receptionist Manual: East Stroudsburg UniversityDocument22 pagesDesk Receptionist Manual: East Stroudsburg UniversityTuấn PhápNo ratings yet
- Skincare Pt1Document6 pagesSkincare Pt1Anna StacyNo ratings yet
- Facials Techniques & MoreDocument199 pagesFacials Techniques & Morekrystalortiz111820No ratings yet
- Beauty Guide Skin Care PDFDocument129 pagesBeauty Guide Skin Care PDFnguyen ba trungNo ratings yet
- Abnormal Bleeding Anxiety/Depression High Blood Pressure Diabetes Autoimmune Disease Mood Swings Migraines SeizuresDocument2 pagesAbnormal Bleeding Anxiety/Depression High Blood Pressure Diabetes Autoimmune Disease Mood Swings Migraines SeizuresAnna Croox ReschNo ratings yet
- 7chapter 2 - Hair Conditioning & ApplicationsDocument6 pages7chapter 2 - Hair Conditioning & ApplicationsGupta Shekhar SulabhNo ratings yet
- Section 1 Seat 9: Precious & Royal SpaDocument187 pagesSection 1 Seat 9: Precious & Royal SpaBlue BööNo ratings yet
- Galvanic Intructions PDFDocument4 pagesGalvanic Intructions PDFFuh Ken ChinNo ratings yet
- Acne Scars and Chemical PeelsDocument2 pagesAcne Scars and Chemical Peelsnlr253100% (1)
- Muhammad-Best Eyelash Extension GlueDocument2 pagesMuhammad-Best Eyelash Extension Gluearticle writerNo ratings yet
- CSBBTH0052A - Provide Facial TreatmentsDocument9 pagesCSBBTH0052A - Provide Facial TreatmentsDean WrightNo ratings yet
- Bridal Makeup Course in AsansolDocument3 pagesBridal Makeup Course in AsansolmakeupartisttriptiNo ratings yet
- Curriculum of Competency Unit (Cocu)Document15 pagesCurriculum of Competency Unit (Cocu)Saravanan Palanisamy100% (1)
- The Benefits of Dermaplaning With Feel SynergyDocument2 pagesThe Benefits of Dermaplaning With Feel SynergyDaniel CalderonNo ratings yet
- WRBSS302BDocument80 pagesWRBSS302BIon Logofătu Albert50% (2)
- 6.face Treatment (Yg Sahih)Document15 pages6.face Treatment (Yg Sahih)Saravanan PalanisamyNo ratings yet
- Beauty Care Wellness Massage CompenduimDocument35 pagesBeauty Care Wellness Massage CompenduimImena SeseNo ratings yet
- The Dermatologists' Prescription for a New You!From EverandThe Dermatologists' Prescription for a New You!Rating: 5 out of 5 stars5/5 (1)
- A Systematic Review On Physical Therapy Interventions For Patients With Binge Eating DisorderDocument1 pageA Systematic Review On Physical Therapy Interventions For Patients With Binge Eating DisordermohamedwhateverNo ratings yet
- Effects of Exercise and Diet On Weight Loss Maintenance in Overweight and Obese Adults: A Systematic ReviewDocument1 pageEffects of Exercise and Diet On Weight Loss Maintenance in Overweight and Obese Adults: A Systematic ReviewmohamedwhateverNo ratings yet
- Weight-Management Interventions For Pregnant or Postpartum WomenDocument1 pageWeight-Management Interventions For Pregnant or Postpartum WomenmohamedwhateverNo ratings yet
- Verbal Descriptor Scale (Pain Thermometer)Document1 pageVerbal Descriptor Scale (Pain Thermometer)mohamedwhateverNo ratings yet
- Physiotherapy Treatment Approaches For The Recovery of Postural Control and Lower Limb Function Following StrokeDocument2 pagesPhysiotherapy Treatment Approaches For The Recovery of Postural Control and Lower Limb Function Following StrokemohamedwhateverNo ratings yet
- Lifestyle Interventions To Reduce Raised Blood Pressure: A Systematic Review of Randomized Controlled TrialsDocument1 pageLifestyle Interventions To Reduce Raised Blood Pressure: A Systematic Review of Randomized Controlled TrialsmohamedwhateverNo ratings yet
- Cryolipolysis For Targeted Fat Reduction and Improved Appearance of The Enlarged Male BreastDocument1 pageCryolipolysis For Targeted Fat Reduction and Improved Appearance of The Enlarged Male BreastmohamedwhateverNo ratings yet
- Weight Management Interventions Targeting Young Women: A Systematic ReviewDocument1 pageWeight Management Interventions Targeting Young Women: A Systematic ReviewmohamedwhateverNo ratings yet
- Evidence-Based Practice Fact SheetDocument3 pagesEvidence-Based Practice Fact Sheetmohamedwhatever100% (2)
- Lumbar StenosisDocument104 pagesLumbar StenosismohamedwhateverNo ratings yet
- Kinesio PDFDocument4 pagesKinesio PDFmohamedwhateverNo ratings yet
- MeaslesDocument23 pagesMeaslesadwait marhattaNo ratings yet
- 2nd Patho Exam QDocument17 pages2nd Patho Exam QSaleh RazickNo ratings yet
- Painless Diabetic Motor NeuropathyDocument12 pagesPainless Diabetic Motor NeuropathyHamza JubranNo ratings yet
- Assess For Signs of HyperglycemiaDocument9 pagesAssess For Signs of HyperglycemiaSheril Sularte CasanesNo ratings yet
- LicenseSPC PA0002-009-002 16122008220131Document5 pagesLicenseSPC PA0002-009-002 16122008220131abdelaziz_ismail685662No ratings yet
- Dermatological Toxicities of Bruton's Tyrosine Kinase InhibitorsDocument14 pagesDermatological Toxicities of Bruton's Tyrosine Kinase InhibitorsabdullahNo ratings yet
- Cues Problem Physiologic Behavioral: Nutrition: Less Than Body Requirements Acute Pain Altered ADLDocument3 pagesCues Problem Physiologic Behavioral: Nutrition: Less Than Body Requirements Acute Pain Altered ADLAya BolinasNo ratings yet
- Pancreatic and Periampullary Carcinoma (Nonendocrine) : Host FactorsDocument26 pagesPancreatic and Periampullary Carcinoma (Nonendocrine) : Host Factorsjuan jose velascoNo ratings yet
- Cardiac Coarctation of The Aorta CoA Management Following Surgical RepairDocument6 pagesCardiac Coarctation of The Aorta CoA Management Following Surgical RepairMohammed IbrahimNo ratings yet
- MeaslesDocument14 pagesMeaslesCHALIE MEQUNo ratings yet
- Vital Signs QUIZDocument3 pagesVital Signs QUIZJeyser T. GamutiaNo ratings yet
- TRIAZOLAMDocument4 pagesTRIAZOLAMEzequiel RosalesNo ratings yet
- Orthopaedic Blunder: - Ward 5F - Edendale HospitalDocument28 pagesOrthopaedic Blunder: - Ward 5F - Edendale Hospitalaya kafeelNo ratings yet
- Hematopoiesis: RbcsDocument27 pagesHematopoiesis: Rbcsjamba juiceNo ratings yet
- 2014.panduan Layanan Klinis Dokter Spesialis Dermatologi Dan Venereologi Dr. RetnoDocument47 pages2014.panduan Layanan Klinis Dokter Spesialis Dermatologi Dan Venereologi Dr. RetnoBoby ShéNo ratings yet
- Patient History GastroDocument249 pagesPatient History GastroMatto RajputNo ratings yet
- Types of WoundsDocument4 pagesTypes of WoundsHanarisha Putri AzkiaNo ratings yet
- Lecture 9 Guidelines For Application of Stretching InterventinsDocument4 pagesLecture 9 Guidelines For Application of Stretching InterventinsMarwa MehmoodNo ratings yet
- PSB Introduction To DisabilityDocument26 pagesPSB Introduction To Disabilityapi-261503220100% (2)
- Renal QuizDocument2 pagesRenal QuizJune Dumdumaya75% (4)
- Pedia+smiley Block7Document7 pagesPedia+smiley Block7tej0331No ratings yet
- LP KEHAMILAN NORMAL Zaii - Id.enDocument5 pagesLP KEHAMILAN NORMAL Zaii - Id.enMuhammad ZainuddinNo ratings yet
- Management of Patients With Special NeedsDocument4 pagesManagement of Patients With Special NeedsSophia MolinaNo ratings yet
- NCP LeptospirosisDocument6 pagesNCP LeptospirosisJean Marie DavidNo ratings yet
- Paediatric Podiatry Clinical Framework 2019 FinalDocument23 pagesPaediatric Podiatry Clinical Framework 2019 FinalMahmoud A KhatabNo ratings yet
- Imse Finals Reviewer - Pacate, Joyce C.Document9 pagesImse Finals Reviewer - Pacate, Joyce C.jcpacate1178qcNo ratings yet
- Module 2Document47 pagesModule 2HUTALLA CezanneNo ratings yet
- USMLE Step 2 CK Bible 2nd EdDocument435 pagesUSMLE Step 2 CK Bible 2nd Edgabe_babe001086% (21)