Professional Documents
Culture Documents
Modified Rapidseq
Uploaded by
zaheermechOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Modified Rapidseq
Uploaded by
zaheermechCopyright:
Available Formats
AANA Journal/August 2001/Vol. 69, No.
4 291
Introduction
R
apid-sequence induction
(RSI) is a commonly used
anesthetic technique for
patients considered at risk
for regurgitation and pul-
monary aspiration. This technique con-
sists of preoxygenation, cricoid pressure,
and the avoidance of postive-pressure
ventilation until the airway has been
secured with an endotracheal tube.
Patients at risk for aspiration include
those with full stomachs and patients
with a history of gastrointestinal surgery,
hiatal hernia, gastroesophageal reflux
disease, esophageal motility disorders,
hyperchlorhydria, peptic ulcer, obesity,
or diabetes mellitus.
1
Although RSI is well established in
anesthetic practice, it is not without
possible risk to the patient. The most
alarming risk is the potential inability
to secure an airway or to ventilate a
patient who is unconscious and apneic.
The decision to use RSI needs to be
based on a thorough assessment of a
patients potential risk of aspiration and
the potential risks associated with RSI.
Potential risks of RSI include inability
to ventilate leading to hypoxia and
hypercarbia, alteration in heart rate and
blood pressure, and trauma to the air-
way. These risks may not be warranted
or appropriate for a patient at minimal
risk of regurgitation and aspiration. For
these cases, a modification of the stan-
dard RSI technique consisting of pre-
oxygenation, cricoid pressure, and gen-
tle positive-pressure ventilation before
tracheal intubation may be more appro-
priate. The purpose of this study was to
determine whether any such modifica-
tion of RSI technique is used currently
in clinical practice.
The primary objective of RSI is to
minimize the time between patient loss
of consciousness and tracheal intuba-
tion. RSI is a standard technique con-
sisting of preoxygenation and cricoid
pressure.
2
Positive-pressure ventilation
generally is avoided until the airway is
secured with an endotracheal tube,
unless attempts at intubation are
unsuccessful or desaturation occurs.
Considerable variation, however, exists
among anesthesia providers in the use
of this technique. Variability exists in
the duration of preoxygenation; the
selection, dosage, and timing of admin-
istration of the induction agent and
muscle relaxant; the use of adjunct
medications; the application of cricoid
pressure; and the management of a
failed intubation.
2
Preoxygenation is a standard com-
ponent of RSI.
2
According to basic
anesthetic texts, preoxygenation on
high fresh gas flows of 100% oxygen
via face mask with a good mask fit for
3 to 5 minutes is recommended. Alter-
natively, a series of 4 vital capacity
breaths of 100% oxygen may be used in
an emergency.
3,4
Sodium thiopental is selected most
frequently as the induction agent in
RSI.
2
Other agents used include keta-
mine,
5
etomidate,
6
and propofol.
7
Suc-
cinylcholine has long been considered
the gold standard muscle relaxant for
RSI, but adverse effects such as
arrhythmias, hyperkalemia, and fascic-
ulations may preclude its safe use in
certain situations such as burn injury
or spinal cord injury. Other muscle
relaxants that can be considered
include vecuronium
8-10
and rocuro-
nium.
6,10-12
Nondepolarizing muscle
relaxants, however, have a significantly
longer duration of action than suc-
The purpose of this study was to
identify the use of rapid-sequence
induction (RSI) and its hybrids. For
the study, 67 Certified Registered
Nurse Anesthetists at 1 hospital
completed a survey describing
their experience using a modified
technique for patients with a mod-
erately increased risk of regurgita-
tion and aspiration. Patient selec-
tion criteria and the use of
aspiration prophylaxis, preoxy-
genation, cricoid pressure, and
positive-pressure ventilation were
evaluated. In contrast with routine
induction and standard RSI tech-
niques, the modified RSI technique
consisted of aspiration prophy-
laxis, preoxygenation, application
of cricoid pressure, and positive-
pressure ventilation. The survey
revealed that a modification of
standard RSI is used commonly in
clinical practice. These modified
RSI techniques are not standard-
ized, as variation was noted in the
delivery of positive pressure venti-
lation. Further study is necessary
to identify widespread use of mod-
ified RSI techniques and to clarify
the risks and benefits of modified
RSI.
Key words: Modified rapid-se-
quence induction, preoxygenation,
cricoid pressure, positive-pressure
ventilation.
Modified rapid-sequence induction of
anesthesia: A survey of current
clinical practice
Stacey Schlesinger, CRNA, MSN,
MBA
Statesville, North Carolina
Diane Blanchfield, CRNA, MS
Charlotte, North Carolina
292 AANA Journal/August 2001/Vol. 69, No. 4
cinylcholine and could prove disastrous if a patient
could not be adequately ventilated or intubated. Non-
depolarizing muscle relaxants also may be undesir-
able for surgical procedures of short duration.
The timing of administration of the induction
agent in relation to the muscle relaxant in RSI also
seems to be variable. In 1 study of 210 anesthetists,
the muscle relaxant was administered immediately
after the induction agent by 46.5% of anesthetists,
after loss of lid reflex by 38% of anesthetists, and after
loss of verbal contact by 15% of anesthetists.
2
Other
descriptions of RSI include administration of muscle
relaxant 5 seconds after administration of the induc-
tion agent
5
or even before administration of the induc-
tion agent.
8,9
In any event, the rapid administration of
a barbiturate with an alkaline pH and a muscle relax-
ant with an acidic pH can result in immediate and
substantial precipitation and occlusion of the intra-
venous line.
13-15
The loss of intravenous access after a
patient loses consciousness and protective airway
reflexes might prove disastrous.
Another key component of RSI is the application of
cricoid pressure. Cricoid pressure consists of com-
pression and occlusion of the esophagus in an attempt
to minimize the risk of regurgitation. Cricoid pressure
has been demonstrated to prevent air entry into the
stomach as long as a patent airway is maintained.
16
Excessive force applied to the cricoid cartilage can
obstruct the airway and interfere with successful tra-
cheal intubation. Possible complications of cricoid
pressure include difficult tracheal intubation, airway
obstruction, pulmonary aspiration, and esophageal
rupture.
17
Other unusual but reported complications
include bilateral subconjunctival hemorrhage from a
patient bucking against cricoid pressure
18
and cricoid
cartilage fracture.
19
Positive-pressure ventilation generally is avoided to
prevent aspiration and gaseous distention of the stom-
ach in RSI.
16
This, however, precludes the ability to
test the airway and verify that a patient can be ven-
tilated by mask before the administration of a muscle
relaxant. This also mandates a period of apnea that
may not be well tolerated by patients with compro-
mised respiratory status or increased baseline oxygen
requirements.
The use of a modified RSI technique would allow
for a patient to be gently ventilated by mask before the
insertion of an endotracheal tube. Positive-pressure
ventilation via a face mask could be provided before
administration of a muscle relaxant to test the airway
in patients with an airway assessed as marginal. Alter-
natively, positive-pressure ventilation via a face mask
could be provided before and after administration of a
muscle relaxant for patients unable to tolerate the
brief period of apnea associated with RSI. An exten-
sive review of the literature, however, has revealed no
descriptions of a modified RSI technique for these
patients.
Materials and methods
This descriptive study consisted of a survey of Certi-
fied Registered Nurse Anesthetists (CRNAs) em-
ployed at a large tertiary care hospital located in the
southeastern United States. The anesthetists were
asked to complete a survey describing their experi-
ence performing both RSI and modifications of RSI in
their clinical practice. CRNAs who reported having
used a modified RSI technique were asked additional
questions to determine how patients were selected
and whether preoxygenation, cricoid pressure, and
positive-pressure ventilation were used. One of the
investigators (S.S.) developed the data collection tool
for the sole purpose of this study.
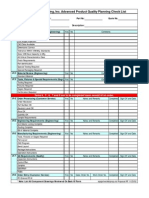
The survey (Figure 1) included 4 basic questions
on the anesthetists experience, practice setting, and
use of RSI and modified RSI techniques. CRNAs who
reported using a modified RSI technique in clinical
practice were asked 5 additional questions regarding
patient selection, provision of prophylaxis for aspira-
tion pneumonia, preoxygenation, cricoid pressure,
and positive-pressure ventilation.
Institutional review board approval was obtained
before the distribution of surveys to all employed
CRNAs in the inpatient and outpatient operating
rooms. Responses were compiled and analyzed to
identify the frequency of clinical use of RSI and mod-
ified RSI techniques, CRNA experience, and clinical
practice setting. For CRNAs who reported using a
modified RSI technique in clinical practice, further
review of the data identified patient selection consid-
erations and the anesthetists definition of the modi-
fied RSI technique.
Results
Of 84 surveys distributed, 67 were returned for an
overall response rate of 80%; 31 CRNAs (46%) had
more than 10 years of clinical experience, 21 (31%) had
5 to 10 years of experience, and 15 (22%) had fewer
than 5 years of experience. Of the 65 respondents who
answered question 2 (type of practice setting), 51
(78%) were employed primarily in the inpatient oper-
ating room, while 14 (22%) were employed primarily
in the outpatient department (Figures 2 and 3).
Nearly all respondents reported using both RSI and
modified RSI techniques in their clinical practice
(Figure 4). The reported use of a standard RSI tech-
AANA Journal/August 2001/Vol. 69, No. 4 293
Modified rapid-sequence induction (RSI) techniques
A Survey of Current Clinical Practice
RSI is a commonly used procedure in patients with full stomachs to minimize the risk of regurgitation and aspiration.
Standard components of RSI are preoxygenation, cricoid pressure and the avoidance of positive pressure ventilation via face
mask until an endotracheal tube is placed. In some circumstances, a modification of this rapid-sequence technique may be
warranted. The purpose of this questionnaire is to identify the clinical definition of modified RSI.
Please select the response that most closely reflects your current clinical practice.
1. Years anesthesia experience __< 5 years __5-10 years __> 10 years
2. Type of practice setting __ Inpatient operating room __ Outpatient operating room
3. In my clinical practice, I currently use RAPID-SEQUENCE INDUCTION (RSI)
__Never __ Rarely __Occasionally __Often __Always
4. In my clinical practice, I currently use MODIFIED RSI
__Never __Rarely __Occasionally __Often __Always
If you have NEVER used a modified RSI technique in your clinical practice, THANK YOU for your participation.
If you have used a MODIFIED RSI technique, please answer the following questions.
5. Patients that I have utilized a MODIFIED RSI technique upon include: (check all that apply)
__ Moderately obese patients
__ Morbidly obese patients
__ Diabetic patients with no clinical symptoms of reflux disease
__ Patients with a history of prior esophageal surgery
__ Patients with a history of GERD but with no recent symptoms
__Other. Please explain:__________________________________________________
6. Based on your definition of modified RSI, is aspiration prophylaxis appropriate?
___ No ___ Yes If Yes, your usual management is: (check all that apply)
__Premedication with sodium citrate
__Premedication with metoclopramide
__Premedication with H
2
antagonist
__Other: _____________________________ (please specify)
7. Based on your definition of Modified RSI, is preoxygenation required prior to induction?
___ No ___ Yes If Yes, for how long? (select the best answer)
__PreO
2
on 100% > 5 min
__PreO
2
on 100% 3-5 min
__PreO
2
on 100% < 3 min
__PreO
2
on 100% 4 vital capacity breaths
8. Based on your definition of modified RSI, is the application of cricoid pressure necessary?
___ No ___ Yes If yes, when is it applied? (select the best answer)
__Prior to induction agent
__At the same time as induction agent
__After loss of lid reflex
__After loss of verbal contact
9. Based on your definition of modified RSI, is an attempt to ventilate via face mask appropriate?
___ No ___ Yes If yes, when do you attempt to ventilate? (select the best answer)
__PRIOR to administration of a muscle relaxant
__FOLLOWING administration of muscle relaxant
__BOTH before and after administration of muscle relaxant
Figure 1. Survey*
*GERD indicates gastroesophageal reflux disease; PreO
2
indicates preoxygenation.
294 AANA Journal/August 2001/Vol. 69, No. 4
nique was described as often by 45 (67%) and
occasional by 20 (30%). Only 2 respondents (3%)
reported never or rarely having used a standard
RSI technique. No CRNA reported always using a
standard RSI technique.
Of the respondents, 65 (97%) reported they have
used a modified RSI technique in their clinical prac-
tice. The use of this technique was described as occa-
sional by 42 (63%), often by 19 (28%), and
always by 1 (1%). Only 3 (4%) reported rarely
using a modified RSI technique.
The 65 CRNAs who reported using a modified RSI
technique were asked to answer 5 additional ques-
tions on the survey. Five patient scenarios were
described, and the anesthetists were asked to identify
those in which they had used a modified RSI tech-
nique for the induction of general anesthesia. A total
of 57 respondents (88%) reported they had used a
modified RSI technique for patients with moderate
obesity, while 23 (35%) reported its use for patients
with morbid obesity. In addition, 43 respondents
(66%) reported they had used modified RSI for
patients with diabetes who had no current signs and
symptoms of reflux disease. For patients with a his-
tory of esophageal surgery, 18 (28%) responded they
had used a modified RSI technique. For patients with
a history of gastroesophageal reflux disease but no
recent symptoms, 48 respondents (74%) reported
using a modified RSI technique. These findings are
summarized in Figure 5.
CRNAs also were asked to identify any other
patient situations in which they had used a modified
RSI technique (Table).
The remaining survey questions addressed the spe-
cific components of a modified RSI technique. The
0
25
50
75
100
> 10 5-10 < 5
Years of clinical experience
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
21(31%)
15(22%)
31(46%)
Figure 2. Reported experience of Certified Registered
Nurse Anesthetists (N=67)*
Inpatient
operating room
Outpatient
operating room
Clinical practice setting
14(22%)
51(78%)
Figure 3. Reported primary employment setting
(n=65)
0
10
20
30
40
50
60
70
80
90
100
Modified
RSI
RSI
Always Often Occasion-
ally
Rarely Never
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
1% 0%
67%
28%
63%
30%
4%
1%
3%
1%
How often technique is used
Figure 4. Use of standard rapid-sequence induction
(RSI) and modified RSI techniques in clinical practice
(N=67)*
0
10
20
30
40
50
60
70
80
90
100
History of
gastroesophageal
reflux disease but
no current signs
and symptoms
Prior
esoph-
ageal
surgery
Diabetes,
no signs
and
symptoms
of reflux
Morbid
obesity
Moderate
obesity
Indication
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
88%
35%
66%
28%
74%
Figure 5. Modified rapid-sequence induction
indications (n=65)
*Due to rounding, percentages may not add up to 100%.
*Due to rounding, percentages may not add up to 100%.
AANA Journal/August 2001/Vol. 69, No. 4 295
preoperative administration of medication to alter
gastric pH and/or gastrointestinal motility (aspiration
pneumonia prophylaxis) was reported by 55 (85%) of
the CRNAs who reported using a modified RSI tech-
nique. Regarding their choice of drug administration,
52 (95%) of these 55 respondents administered H
2
receptor antagonists, 49 (89%) administered metoclo-
pramide, and 2 (4%) administered sodium citrate.
These data are summarized in Figure 6. No other
medications were identified as being administered as
part of a modified RSI.
Preoxygenation is another key component of stan-
dard RSI and possibly of modified RSI. Of the CRNAs
who have used a modified RSI technique, 63 (97%)
reported that preoxygenation is required before
induction. Of those respondents, 61 reported meth-
ods (Figure 7), which included preoxygenation on
100% FIO
2
(fraction of inspired oxygen) for 3 to 5
minutes (31 [51%]), for 4 vital capacity breaths (13
[21%]), for fewer than 3 minutes (11 [18%]), and for
more than 5 minutes (6 [10%]).
Cricoid pressure is another usual component of
both standard and modified RSI. A total of 62 CRNAs
(95%) who have used a modified RSI technique
reported that the application of cricoid pressure is
necessary. Of the respondents (n=57) who reported
when cricoid pressure is applied, 40 (70%) reported
that cricoid pressure was applied at the same time as
administration of the induction agent. Other re-
sponses included before administration of the induc-
tion agent (11 [19%]), after loss of lid reflex (3 [5%]),
and following loss of verbal contact (3 [5%]). These
data are summarized in Figure 8.
In standard RSI, positive-pressure ventilation is
avoided until the airway is secured. Of those using a
modified RSI technique, 61 (94%) reported that an
attempt to ventilate via a face mask is appropriate. Of
Patient at risk for desaturation but RSI is indicated
Trauma patient who has been NPO for 8 h
End-stage renal disease without symptoms of GERD
Patient for heart surgery with GERD
Consistent history of reflux
Patient >24 h postpartum
Patient who is >5 mo pregnant
Inhalation induction
Table. Other proposed indications for modified
rapid-sequence induction (RSI)*
*GERD indicates gastroesophageal reflux disease; NPO indicates nothing by
mouth.
0
25
50
75
100
Metoclopramide H
2
receptor
antagonist
Sodium citrate
Method
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
52 (95%)
2 (4%)
49 (89%)
Figure 6. Methods of prophylaxis for aspiration
pneumonia in modified rapid-sequence induction
(n=55)
0
25
50
75
100
4 vital
capacity
breaths
< 3
minutes
3-5
minutes
> 5
minutes
Duration
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
31 (51%)
6 (10%)
11 (18%)
13 (21%)
Figure 7. Duration of preoxygenation in modified
rapid-sequence induction (n=61)
0
25
50
75
100
After loss
of verbal
contact
After loss
of lid
reflex
Same time
as induction
agent
Before
induction
agent
Timing of cricoid pressure
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
40 (70%)
11 (19%)
3 (5%) 3 (5%)
Figure 8. Timing of the application of cricoid pressure
in modified rapid-sequence induction (n=57)
296 AANA Journal/August 2001/Vol. 69, No. 4
the respondents who reported when they attempt to
ventilate (n = 60), 30 (50%) reported that they did so
both before and after administration of a muscle
relaxant. An additional 13 (22%) reported providing
positive-pressure ventilation before administration of
a muscle relaxant, and 17 (28%) reported providing
positive-pressure ventilation following administration
of a muscle relaxant. These data are summarized in
Figure 9.
Discussion
The analysis of the data confirms that a modified RSI
technique often is used by CRNAs in clinical practice
at 1 institution. As shown in Figure 10, the modified
RSI technique most often consists of pharmacological
prophylaxis, preoxygenation, cricoid pressure, and
positive-pressure ventilation. This differs from a stan-
dard RSI technique, which does not include positive-
pressure ventilation, and from a routine induction,
which does not include aspiration prophylaxis or
cricoid pressure.
Although survey respondents were CRNAs with
varying experience from inpatient and outpatient set-
tings, the reported use of standard RSI and modified
RSI was consistent among all practioners (Figures 11
and 12). It is important to note that most of the anes-
thetists surveyed graduated from the same nurse anes-
thesia training program.
Patients selected for the modified RSI technique
included those in whom the relative risks of regurgi-
tation and aspiration seemed to be less than the risks
associated with the use of standard RSI. These include
moderately obese patients and patients with underly-
ing gastroesophageal reflux disease or a disease
process (diabetes, renal failure) associated with gas-
troesophageal reflux disease but who have no current
symptoms. The low reported use of modified RSI for
patients with morbid obesity or who have undergone
esophageal surgery most likely reflects a tendency to
select a standard RSI technique for these patients.
There were some differences among clinicians in
the specific application of each component of modi-
fied RSI. Variation was demonstrated in the duration
of preoxygenation, the timing of application of cricoid
pressure, and the choice of preoperative medications
to alter gastrointestinal motility and gastric pH. There
was wide variation in the timing of positive-pressure
ventilation in modified RSI.
Aspiration prophylaxis was reported by most
CRNAs as part of a modified RSI. This most com-
monly consisted of the administration of an H
2
recep-
tor antagonist, metoclopramide, or both.
Preoxygenation with 100% oxygen was provided
most often for 3 to 5 minutes and was followed by the
application of cricoid pressure. Cricoid pressure gen-
erally was applied at the same time as administration
of an induction agent. The use of cricoid pressure was
reported by nearly all anesthetists as part of a modi-
fied RSI technique.
Positive-pressure ventilation is used as part of a
modified RSI technique by most CRNAs surveyed.
This represents the most substantial difference of
modified RSI with standard RSI, in which positive-
pressure ventilation generally is avoided. The timing
of positive-pressure ventilation in relation to the
administration of a muscle relaxant in modified RSI,
however, is variable. Some anesthetists reported that
they administered positive-pressure ventilation both
before and after administration of a muscle relaxant.
0
25
50
75
100
Before
and after
administration
of muscle
relaxant
Following
administration
of muscle
relaxant
Before
administration
of muscle
relaxant
Timing of positive-pressure ventilation
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
17 (28%)
13 (22%)
30 (50%)
Figure 9. Use of positive-pressure ventilation via face
mask in modified rapid-sequence induction (n=60)
0
25
50
75
100
Positive-
pressure
ventilation
Cricoid
pressure
Preoxy-
genation
Aspiration
prophylaxis
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
63 (97%)
55 (85%)
62 (95%)
61 (94%)
Components of rapid-sequence induction
Figure 10. Reported components of modified rapid-
sequence induction (n=65)
AANA Journal/August 2001/Vol. 69, No. 4 297
Other anesthetists provided positive-pressure ventila-
tion only before or only after administration of a mus-
cle relaxant. A few anesthetists reported that they did
not provide positive-pressure ventilation at any time
during modified RSI. It is unclear to the investigators
how this modified RSI technique differed from stan-
dard RSI.
The variability in the use of positive-pressure ven-
tilation may represent different objectives for individ-
ual patients in the selection of a modified RSI tech-
nique. During standard RSI, patients are made apneic
and unconscious without establishing that they can
be ventilated by mask. This theoretically avoids
gaseous distention of the stomach and subsequent
possible regurgitation and aspiration. However, if the
anesthetist subsequently is unable to intubate or ven-
tilate, results could prove disastrous. During modified
RSI, the provision of positive-pressure ventilation via
a face mask allows the anesthetist to affirm the ability
to ventilate before administering a muscle relaxant.
For patients who cannot be ventilated safely via a face
mask during modified RSI, a decision can be made
before the administration of a muscle relaxant to
reawaken the patient and proceed with an awake intu-
bation. This may be of added importance for patients
in whom succinylcholine is contraindicated, since the
resulting period of paralysis with a nondepolarizing
muscle relaxant can be substantially longer.
The modified RSI technique also may be valuable
for patients who may not tolerate even brief periods of
apnea, because careful, low-peak airway pressure ven-
tilation can be provided throughout the induction
period. The use of positive-pressure ventilation before
and after the administration of a muscle relaxant
allows the anesthetist to test the airway and avoid
desaturation.
Modified RSI seems to be an acceptable and com-
mon clinical technique for the induction of general
anesthesia in selected patients at this institution. Fur-
thermore, the modified technique seems to be well-
defined as the sequence of aspiration prophylaxis with
an H
2
receptor antagonist and metoclopramide, pre-
oxygenation with 100% oxygen for 3 to 5 minutes or
4 vital capacity breaths, application of cricoid pressure
at the same time as administration of the induction
agent, and provision of positive-pressure ventilation
before and after administration of a muscle relaxant.
As with standard RSI, there seems to be variation in
the specific application of each of these components.
The purpose of the present study was to determine
whether a modified RSI technique is used in clinical
practice for the induction of general anesthesia. Fur-
ther study is warranted to evaluate the use of a modi-
fied RSI technique in other clinical settings and to
determine the safety and efficacy of the technique.
REFERENCES
1. Mallampati SR. Airway management. In: Barash PG, Cullen BF,
Stoelting RK, eds. Clinical Anesthesia. Philadelphia, Pa: Lippincott-
Raven; 1997:573-594.
2. Thwaites AJ, Rice CP, Smith I. Rapid sequence induction: a ques-
tionnaire survey of its routine conduct and continued manage-
ment during a failed intubation. Anaesthesia. 1999;54:376-381.
3. Santos AC, Pederson H, Finster M. Obstetric anesthesia. In: Barash
PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. Philadelphia
PA: Lippincott-Raven; 1997:1061-1090.
4. Chipas A. Airway management. In: Nagelhout JJ, Zaglaniczny KL,
eds. Nurse Anesthesia. Philadelphia PA: WB Saunders; 1997:708-
725.
5. Baraka AS, Sayyid SS, Assaf BA. Thiopental-rocuronium versus ket-
amine-rocuronium for rapid-sequence intubation in parturients
0
25
50
75
100
> 10 y (n=31)
5-10 y (n=21)
< 5 y (n=15)
Always Often Occasion-
ally
Rarely Never
Frequency of RSI
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
Figure 11. Reported use of standard rapid-sequence
induction (RSI) by length of Certified Registered
Nurse Anesthetist experience
0
25
50
75
100
>10y (n=31)
5-10 y (n=21)
<5 y (n=15)
Always Often Occasion-
ally
Rarely Never
Frequency of modified RSI
P
e
r
c
e
n
t
a
g
e
o
f
r
e
s
p
o
n
s
e
s
Figure 12. Reported use of modified rapid-sequence
induction (RSI) by length of Certified Registered
Nurse Anesthetist experience
298 AANA Journal/August 2001/Vol. 69, No. 4
undergoing cesarean section. Anesth Analg. 1997;84:1104-1107.
6. Fuchs-Buder T, Sparr HJ, Ziegenfub T. Thiopental or etomidate for
rapid sequence induction with rocuronium. Br J Anaesth. 1998;
80:504-506.
7. Wright PMC, Caldwell JE, Miller RD. Onset and duration of
rocuronium and succinylcholine at the adductor pollicis and
laryngeal adductor muscles in anesthetized humans. Anesthesiol-
ogy. 1994;81:1110-1115.
8. Cicala R, Westbrook L. An alternative method of paralysis for
rapid sequence induction. Anesthesiology. 1988;69:983-986.
9. Silverman SM, Culling RD, Middaugh RE. Rapid-sequence orotra-
cheal intubation: a comparison of three techniques. Anesthesiology.
1990;73:244-248.
10. Magorian T, Flannery KB, Miller RD. Comparison of rocuronium,
succinylcholine, and vecuronium for rapid-sequence induction of
anesthesia in adult patients. Anesthesiology. 1993;79:913-918.
11. McCourt KC, Salmela L, Mirakhur RK, et al. Comparison of
rocuronium and suxamethonium for use during rapid sequence
induction of anaesthesia. Anaesthesia. 1998;53:867-871.
12. Mazurek AJ, Rae B, Hann S, et al. Rocuronium versus succinyl-
choline: are they equally effective during rapid-sequence induc-
tion of anesthesia? Anesth Analg. 1998;87:1259-1262.
13. Njoku DB, Lenox WC. Use care when injecting rocuronium and
thiopental for rapid sequence induction and tracheal intubation
[letter]. Anesthesiology. 1995;83:222.
14. Brandom BW. Use care when injecting rocuronium and thiopental
for rapid sequence induction and tracheal intubation [letter].
Anesthesiology. 1995;83:222.
15. Molbegott L. The precipitation of rocuronium in a needleless intra-
venous injection adaptor [letter]. Anesthesiology. 1995; 83:223.
16. Lawes EJ, Campbell I, Mercer D. Inflation pressure, gastric insuffla-
tion and rapid sequence induction. Br J Anaesth. 1987;59:315-318.
17. Vanner RG, Asai T. Safe use of cricoid pressure. Anesthesia. 1999;
54:1-3.
18. Putland J. Subconjunctival haemmorrhage following rapid
sequence induction in pregnancy [letter]. Anaesthesia. 1998;
53:313.
19. Heath KJ, Palmer M, Fletcher, SJ. Fracture of the cricoid cartilage
after Sellicks manoeuvre. Br J Anaesth. 1996;76:877-878.
AUTHORS
Stacey Schlesinger, CRNA, MSN, MBA, is a nurse anesthetist for Uni-
four Anesthesia Associates in Hickory, NC.
Diane Blanchfield, CRNA, MS, is a clinical coordinator at Carolinas
Health System in Charlotte, NC.
You might also like
- Critical Care Review: Airway Management of The Critically Ill PatientDocument16 pagesCritical Care Review: Airway Management of The Critically Ill PatientNikita ShakyaNo ratings yet
- Secuencia de Intubación RápidaDocument16 pagesSecuencia de Intubación Rápidaalis_maNo ratings yet
- Rapid Sequence Intubation and Cricoid PressureDocument16 pagesRapid Sequence Intubation and Cricoid PressureErlin IrawatiNo ratings yet
- 1 s2.0 S0733862722000384 MainDocument13 pages1 s2.0 S0733862722000384 Maincoca12451No ratings yet
- 4.-Rapid Sequence Intubation in Adults - Uptodate PDFDocument14 pages4.-Rapid Sequence Intubation in Adults - Uptodate PDFkendramura100% (1)
- Obesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaDocument8 pagesObesity and Anticipated Difficult Airway - A Comprehensive Approach With Videolaryngoscopy, Ramp Position, Sevoflurane and Opioid Free AnaesthesiaIJAR JOURNALNo ratings yet
- 2022 Preoperative Assessment Premedication Perioperative DocumentationDocument38 pages2022 Preoperative Assessment Premedication Perioperative DocumentationMohmmed Mousa100% (1)
- AARC Clinical Practice GuidelineDocument7 pagesAARC Clinical Practice GuidelineXime GonzálezNo ratings yet
- Ventilatorweaningand Extubation: Karen E.A. Burns,, Bram Rochwerg, Andrew J.E. SeelyDocument18 pagesVentilatorweaningand Extubation: Karen E.A. Burns,, Bram Rochwerg, Andrew J.E. Seelyأركان هيلث Arkan healthNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Smith 2001Document19 pagesSmith 2001PaulHerreraNo ratings yet
- Freid 2005Document14 pagesFreid 2005PaulHerreraNo ratings yet
- Airway Management in The Obese Patient: William A. LoderDocument6 pagesAirway Management in The Obese Patient: William A. LoderTapas Kumar SahooNo ratings yet
- Rapid Sequence Intubation For Adults Outside The Operating RoomDocument12 pagesRapid Sequence Intubation For Adults Outside The Operating Roomjohnsam93No ratings yet
- Evid TT 2200305Document4 pagesEvid TT 2200305Muthia Farah AshmaNo ratings yet
- Anesthesia in Prehospital Emergencies and in The Emergency DepartmentDocument7 pagesAnesthesia in Prehospital Emergencies and in The Emergency DepartmentIvan TapiaNo ratings yet
- Practice Guidelines For Preoperative FastingDocument18 pagesPractice Guidelines For Preoperative FastingTaufik RachmanNo ratings yet
- Physiotherapy in The ICUDocument10 pagesPhysiotherapy in The ICUakheel ahammedNo ratings yet
- Effect of Smoking On Intraoperative Sputum and Postoperative Pulmonary Complication in Minor Surgical PatientsDocument7 pagesEffect of Smoking On Intraoperative Sputum and Postoperative Pulmonary Complication in Minor Surgical PatientsfellaniellaNo ratings yet
- Pediatric Rapid Sequence Intubation - An In-Depth ReviewDocument12 pagesPediatric Rapid Sequence Intubation - An In-Depth ReviewDiego LatorreNo ratings yet
- Rapid Sequence Intubation in Adults For Emergency Medicine and Critical Care - UpToDateDocument41 pagesRapid Sequence Intubation in Adults For Emergency Medicine and Critical Care - UpToDateFabio FreitasNo ratings yet
- 2015 LeeuwenbergDocument10 pages2015 LeeuwenbergPaulHerreraNo ratings yet
- Maximizing Success With Rapid Sequence IntubationsDocument11 pagesMaximizing Success With Rapid Sequence IntubationsRaymond RosarioNo ratings yet
- Prehospital Rsi ManualDocument20 pagesPrehospital Rsi ManualMiguel XanaduNo ratings yet
- Articulo de Indice de SecrecionesDocument7 pagesArticulo de Indice de Secrecionesmariam.husseinjNo ratings yet
- The Physiologically Difficult Airway: Eview RticleDocument9 pagesThe Physiologically Difficult Airway: Eview RticleEdson Llerena SalvoNo ratings yet
- Farmacologia en SIRDocument19 pagesFarmacologia en SIRFranklin Correa PrietoNo ratings yet
- Greater Sydney Area Hems Prehospital Rsi Manual: Version 2.1 Oct 2012Document20 pagesGreater Sydney Area Hems Prehospital Rsi Manual: Version 2.1 Oct 2012Juan Antonio GarcíaNo ratings yet
- Enhancing Pulmonary Function and Arterial Blood GaDocument12 pagesEnhancing Pulmonary Function and Arterial Blood Gaاحمد العايديNo ratings yet
- Module 1 Case StudyDocument7 pagesModule 1 Case StudyDivine ParagasNo ratings yet
- Secuencia Rapida GuiasDocument29 pagesSecuencia Rapida GuiasToñoGomezNo ratings yet
- Anesthesia For Bariatric Surgery Practice Guideline - Approved 4 - 9 - 2018 - KAPC - PDF PDFDocument4 pagesAnesthesia For Bariatric Surgery Practice Guideline - Approved 4 - 9 - 2018 - KAPC - PDF PDFHIRANGERNo ratings yet
- Myasthenia Gravis Multiple Sclerosis Case FileDocument3 pagesMyasthenia Gravis Multiple Sclerosis Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Atracurio Vs CisatracurioDocument6 pagesAtracurio Vs CisatracurioEdisonANo ratings yet
- Trends in Anasthesia and Critical CareDocument6 pagesTrends in Anasthesia and Critical CareNurLatifah Chairil AnwarNo ratings yet
- Acute Life-Threatening Hypoxemia During Mechanical VentilationDocument8 pagesAcute Life-Threatening Hypoxemia During Mechanical VentilationCesar Rivas CamposNo ratings yet
- Rapid Sequence Intubation: BackgroundDocument8 pagesRapid Sequence Intubation: Backgroundmarsh86No ratings yet
- RCT of Aprv Vs LPV in Ards PtsDocument11 pagesRCT of Aprv Vs LPV in Ards PtsOldriana Prawiro HapsariNo ratings yet
- Airway Covid - 19Document37 pagesAirway Covid - 19Monica Herdiati Rukmana NaibahoNo ratings yet
- Oral and Maxillofacial Surgery Clinics of North America Office Based Anesthesia 45 57Document13 pagesOral and Maxillofacial Surgery Clinics of North America Office Based Anesthesia 45 57Max FaxNo ratings yet
- Symposium Papers: Emergency Airway ManagementDocument10 pagesSymposium Papers: Emergency Airway Managementdewin21No ratings yet
- 37 Iajps37112017 PDFDocument4 pages37 Iajps37112017 PDFBaru Chandrasekhar RaoNo ratings yet
- Kali Bichromicum 30C For COPD 2005Document8 pagesKali Bichromicum 30C For COPD 2005Dr. Nancy MalikNo ratings yet
- Mechanical Ventilator Discontinuation Process: Lingye Chen,, Daniel Gilstrap,, Christopher E. CoxDocument7 pagesMechanical Ventilator Discontinuation Process: Lingye Chen,, Daniel Gilstrap,, Christopher E. CoxGhost11mNo ratings yet
- Determinants of Time-To-Weaning in A Specialized Respiratory Care UnitDocument10 pagesDeterminants of Time-To-Weaning in A Specialized Respiratory Care UnitClaudia IsabelNo ratings yet
- Determinants of Time-To-Weaning in A Specialized Respiratory Care UnitDocument10 pagesDeterminants of Time-To-Weaning in A Specialized Respiratory Care UnitClaudia IsabelNo ratings yet
- Comparative Study of Breathing Techniques After Coronary Artery by Pass GraftingDocument12 pagesComparative Study of Breathing Techniques After Coronary Artery by Pass GraftingJulenda CintarinovaNo ratings yet
- 2 DiaphragmaticExcursionDocument5 pages2 DiaphragmaticExcursionTiago XavierNo ratings yet
- Masoomeh Adib, Atefeh Ghanbari, Cyrus Emir Alavi and Ehsan Kazemnezhad LeyliDocument9 pagesMasoomeh Adib, Atefeh Ghanbari, Cyrus Emir Alavi and Ehsan Kazemnezhad LeyliBoy MadNo ratings yet
- Should Patients Be Able To Follow Commands Prior To IonDocument10 pagesShould Patients Be Able To Follow Commands Prior To IonjuliasimonassiNo ratings yet
- Extubation With or Without Spontaneous Breathing TrialDocument9 pagesExtubation With or Without Spontaneous Breathing TrialPAULA SORAIA CHENNo ratings yet
- Maggiore 2013Document10 pagesMaggiore 2013oman hendiNo ratings yet
- NCM 112 (FINALS) Chap 1Document2 pagesNCM 112 (FINALS) Chap 1MikasaNo ratings yet
- ERAS Protocols in TB EmpyemaDocument6 pagesERAS Protocols in TB EmpyemaMohan VenkateshNo ratings yet
- Ards Prone PositionDocument9 pagesArds Prone PositionAnonymous XHK6FgHUNo ratings yet
- Jerath2020 Article InhalationalVolatile-basedSedaDocument4 pagesJerath2020 Article InhalationalVolatile-basedSedasncr.gnyNo ratings yet
- Webinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020Document95 pagesWebinar Kuliah Umum Anestesi Joglo Semar 17 Juni 2020izaNo ratings yet
- Terapia Adjunta en SdraDocument23 pagesTerapia Adjunta en SdraMarcoNo ratings yet
- RSI - Children 2 PDFDocument6 pagesRSI - Children 2 PDFAbdul RachmanNo ratings yet
- Voisard Manufacturing, Inc. Advanced Product Quality Planning Check ListDocument1 pageVoisard Manufacturing, Inc. Advanced Product Quality Planning Check ListzaheermechNo ratings yet
- Total Quality Management Must Know" Concepts For EngineersDocument28 pagesTotal Quality Management Must Know" Concepts For EngineerszaheermechNo ratings yet
- Training Schedule PWIDocument1 pageTraining Schedule PWIzaheermechNo ratings yet
- Cswip 3.1 Welding Inspector - Multiple Choice Question, Dec 7, 2007Document43 pagesCswip 3.1 Welding Inspector - Multiple Choice Question, Dec 7, 2007claytoninf87% (30)
- CSWIP Plate Tr5. WPK Rev2Document4 pagesCSWIP Plate Tr5. WPK Rev2razormeback100% (1)
- Physical Configuration Audit (PCA) ChecklistDocument2 pagesPhysical Configuration Audit (PCA) ChecklistzaheermechNo ratings yet
- Preventive Maintenance of MachinesDocument6 pagesPreventive Maintenance of MachineszaheermechNo ratings yet
- ISO Standards Collection - CranesDocument4 pagesISO Standards Collection - CranesJosé Rezende0% (1)
- Functional Configuration Audit (FCA) Checklist: RequirementsDocument2 pagesFunctional Configuration Audit (FCA) Checklist: RequirementszaheermechNo ratings yet
- Passive and Low Frequency RadarDocument11 pagesPassive and Low Frequency RadarzaheermechNo ratings yet
- Pca Checklist: RestrictedDocument3 pagesPca Checklist: RestrictedzaheermechNo ratings yet
- FCA Checklist (NASA)Document2 pagesFCA Checklist (NASA)zaheermechNo ratings yet
- Guide To Insulation Product Specifications: ASTM Guides, Practices and Test MethodsDocument24 pagesGuide To Insulation Product Specifications: ASTM Guides, Practices and Test MethodszaheermechNo ratings yet
- A Powerpoint Training Presentation: by Keith H. CooperDocument38 pagesA Powerpoint Training Presentation: by Keith H. CooperzaheermechNo ratings yet
- ACCP Professional Level III Initial Qualification RequirementsDocument1 pageACCP Professional Level III Initial Qualification RequirementszaheermechNo ratings yet
- EXAMPLE CalculationsDocument4 pagesEXAMPLE CalculationszaheermechNo ratings yet
- Gant ChartDocument2 pagesGant ChartzaheermechNo ratings yet
- Denso HP4Document87 pagesDenso HP4Abraham Janco Janco100% (2)
- Thesis TopicsDocument9 pagesThesis TopicsInayath AliNo ratings yet
- dnd3 Character Sheet STD 105cDocument2 pagesdnd3 Character Sheet STD 105cGerry MaloneyNo ratings yet
- PRP RationaleDocument12 pagesPRP Rationalemarquezjayson548No ratings yet
- ReflectionDocument2 pagesReflectionBảo HàNo ratings yet
- A Crude Awakening Video NotesDocument3 pagesA Crude Awakening Video NotesTai NguyenNo ratings yet
- Individual Ability in SoftwareDocument9 pagesIndividual Ability in Softwaredhana0809100% (4)
- CREW Whitaker Recusal Letter DOJ 11-8-2018Document9 pagesCREW Whitaker Recusal Letter DOJ 11-8-2018Beverly TranNo ratings yet
- Airplus CDF3 Technical SpecsDocument38 pagesAirplus CDF3 Technical Specssadik FreelancerNo ratings yet
- Distortion of The Ecclesiological Views of Metropolitan Chrysostomos of PhlorinaDocument11 pagesDistortion of The Ecclesiological Views of Metropolitan Chrysostomos of PhlorinaHibernoSlavNo ratings yet
- Name: - Date: - Week/s: - 2 - Topic: Examining Trends and FadsDocument3 pagesName: - Date: - Week/s: - 2 - Topic: Examining Trends and FadsRojelyn Conturno100% (1)
- Kindergarten ArchitectureDocument65 pagesKindergarten ArchitectureAnushka Khatri83% (6)
- Report End of Chapter 1Document4 pagesReport End of Chapter 1Amellia MaizanNo ratings yet
- Proofreading: Basic Guide (Research)Document34 pagesProofreading: Basic Guide (Research)Mary Christelle100% (1)
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- SwahiliDocument7 pagesSwahiliMohammedNo ratings yet
- Content Kartilya NG Katipunan: Kataastaasan, Kagalanggalangang Katipunan NG Mga Anak NG Bayan)Document6 pagesContent Kartilya NG Katipunan: Kataastaasan, Kagalanggalangang Katipunan NG Mga Anak NG Bayan)AngelaNo ratings yet
- CPP CheatsheetDocument10 pagesCPP CheatsheetPrakash GavelNo ratings yet
- RagragsakanDocument6 pagesRagragsakanRazel Hijastro86% (7)
- Implementasi Fault Management (Manajemen Kesalahan) Pada Network Management System (NMS) Berbasis SNMPDocument11 pagesImplementasi Fault Management (Manajemen Kesalahan) Pada Network Management System (NMS) Berbasis SNMPIwoncl AsranNo ratings yet
- Natural Gas DistributionDocument46 pagesNatural Gas DistributionscribdmisraNo ratings yet
- The Spokesman Weekly Vol. 32 No. 39 May 30, 1983Document12 pagesThe Spokesman Weekly Vol. 32 No. 39 May 30, 1983SikhDigitalLibraryNo ratings yet
- Small Incision Cataract SurgeryDocument249 pagesSmall Incision Cataract SurgeryAillen YovitaNo ratings yet
- My Kindergarten BookDocument48 pagesMy Kindergarten BookfranciscoNo ratings yet
- Detergent For Auto DishWashing Machine EDocument5 pagesDetergent For Auto DishWashing Machine EkaltoumNo ratings yet
- Pale ExamDocument4 pagesPale ExamPatrick Tan100% (1)
- Material Safety Data Sheet: Manufacturer Pt. Bital AsiaDocument3 pagesMaterial Safety Data Sheet: Manufacturer Pt. Bital AsiaediNo ratings yet
- E9d30c8 4837smartDocument1 pageE9d30c8 4837smartSantoshNo ratings yet
- Exercise No. 2 (DCC First and Second Summary)Document3 pagesExercise No. 2 (DCC First and Second Summary)Lalin-Mema LRNo ratings yet
- Literature ReviewDocument7 pagesLiterature Reviewapi-353923446No ratings yet