Professional Documents
Culture Documents
European Journal of Obstetrics & Gynecology and Reproductive Biology
European Journal of Obstetrics & Gynecology and Reproductive Biology
Uploaded by
renatanurul0 ratings0% found this document useful (0 votes)
1 views6 pagesjurnal
Original Title
Carbetocin Rath2009
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1 views6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biology
European Journal of Obstetrics & Gynecology and Reproductive Biology
Uploaded by
renatanuruljurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Review
Prevention of postpartum haemorrhage with the oxytocin analogue carbetocin
Werner Rath*
Faculty of Medicine, Obstetrics and Gynecology, University of Aachen RWTH, Wendlingweg 2, 52074 Aachen, Germany
Contents
1. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
2. Pharmacological properties . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16
3. Efcacy in caesarean delivery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
4. Efcacy in vaginal delivery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
5. Tolerability and safety prole . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
5.1. Pharmacological studies in volunteers. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
5.2. Tolerability and safety prole in clinical trials in caesarean delivery . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
5.3. Tolerability and safety prole in clinical trials in vaginal delivery. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
6. Cost-effectiveness of carbetocin vs. other uterotonic agents . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
7. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
Acknowledgements . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520
A R T I C L E I N F O
Article history:
Received 12 March 2009
Received in revised form 13 May 2009
Accepted 18 June 2009
Keywords:
Postpartum haemorrhage
Prevention
Carbetocin
Efcacy
Safety prole
A B S T R A C T
Postpartumhaemorrhageis theleadingcauseof maternal mortalityworldwide: 6780%of cases arecaused
by uterine atony. Preventive measures include prophylactic drug use to aid uterine contraction after
delivery, thus avoiding severe blood loss and reducing maternal morbidity and mortality. Carbetocin is a
synthetic analogue of oxytocin with a half-life approximately 410 times longer than that reported for
oxytocin. It combines the safety andtolerabilityprole of oxytocinwiththe sustaineduterotonic activityof
injectable ergot alkaloids. Furthermore, carbetocin can be administered as a single dose injection either
intravenously or intramuscularly rather than as an infusionover several hours as is the case with oxytocin.
Carbetocin is currently indicated for prevention of uterine atony after delivery by caesarean section in
spinal or epidural anaesthesia. Data from three randomised controlled trials in caesarean delivery and a
meta-analysis indicate that carbetocin signicantly reduces the need for additional uterotonic agents or
uterine massage to prevent excessive bleeding compared with placebo or oxytocin. The risk of headache,
tremor, hypotension, ushing, nausea, abdominal pain, pruritus and feeling of warmth was similar in
womenwhoreceivedcarbetocin or oxytocin. The ndings fromtwomore recent double-blind randomised
trials and one retrospective study suggest that carbetocin may also represent a good alternative to
conventional uterotonic agents for prevention of postpartum haemorrhage after vaginal deliveries. A
reducedneedfor additional uterotonics was observedwithcarbetocinvs. oxytocininhigh-riskwomenand
carbetocin was at least as effective as syntometrine in low-risk women. In these studies of vaginal
deliveries, carbetocin was associated with a low incidence of adverse effects and demonstrated a better
tolerabilityprole thansyntometrine. Carbetocinhada long durationof actioncomparedwithintravenous
oxytocin alone and a better cardiovascular side effect prole compared with syntometrine. In addition to
being an effective treatment for the prevention of postpartumhaemorrhage following caesarean delivery,
carbetocin may also become the drug of choice for postpartum haemorrhage prevention after vaginal
delivery inhigh-riskwomenandthose whosuffer fromhypertensive disorders inpregnancy. Preeclampsia
is still a contraindication to the administration of carbetocin in the EU, and further studies would be
required to assess the cardiovascular effects of carbetocin before it can be advocated for routine use in
preeclamptic patients. Further researchis requiredtoassess whether prophylactic carbetocinis superior to
conventional uterotonic agents following vaginal delivery in low-risk women.
2009 Elsevier Ireland Ltd. All rights reserved.
* Tel.: +49 241 80 80 884; fax: +49 241 80 82 711.
E-mail address: wrath@ukaachen.de.
Contents lists available at ScienceDirect
European Journal of Obstetrics & Gynecology and
Reproductive Biology
j our nal homepage: www. el sevi er . com/ l ocat e/ ej ogr b
0301-2115/$ see front matter 2009 Elsevier Ireland Ltd. All rights reserved.
doi:10.1016/j.ejogrb.2009.06.018
1. Introduction
Postpartum haemorrhage occurs in up to 15% of vaginal
deliveries [1] and represents the most important cause of maternal
morbidity and mortality worldwide [26]. The risk of postpartum
haemorrhage is much higher for women undergoing caesarean
section [7], particularly in developing countries where the majority
of operations are carried out as an emergency procedure [8]. In
most cases, uterine atony is responsible for the occurrence of
excessive bleeding during or following childbirth [4,5]. Current
strategies for preventing postpartum haemorrhage include the
prophylactic use of uterotonic agents to enhance natural uterine
contraction and retraction following caesarean section and in the
third stage of labour for vaginal delivery [1,46]. Oxytocin is the
most widely used uterotonic agent [1,57], but only has a half-life
of 410 min [911] so must be administered as a continuous
intravenous infusion to achieve sustained uterotonic activity.
Another uterotonic drug frequently used in vaginal deliveries is
syntometrine, which contains 5 IU/ml oxytocin and 0.5 mg/ml
ergometrine [12,13]. Syntometrine combines the rapid onset of
action of oxytocin and the prolonged uterotonic effects of an ergot
alkaloid. Intramuscular syntometrine use in active management of
the third stage of labour is associated with a signicant reduction
in the risk of non-severe postpartum haemorrhage (<1000 ml of
blood loss) compared with intramuscular oxytocin [6,12,13].
Although intramuscular syntometrine is equally effective as
intravenous oxytocin [6,14], gastrointestinal and cardiovascular
side effects such as maternal nausea, vomiting and raised blood
pressure [6,1214] are more frequent due to stimulation of smooth
muscle contraction and vasoconstriction by ergometrine [15,16].
Oral and rectal administration of misoprostol, a synthetic analogue
of prostaglandin E1, have demonstrated lower efcacy than
injectable uterotonic agents in preventing excessive bleeding
following vaginal delivery [17,18] and are associated with a high
incidence of shivering, fever and a possible risk of severe
hyperthermia [1719]. These factors deem misoprostol unsuitable
for routine prevention of excessive postpartum bleeding in
developed countries, despite low cost and ease of use [6,17,18].
Although injectable prostaglandins such as prostaglandin 15-
methyl F2a or sulprostone can prevent excessive bleeding
following vaginal delivery, safety concerns and cost limit their
suitability for routine use in active management of the third stage
of labour. However, they remain useful therapeutic options for
postpartum haemorrhage treatment when other interventions
prove ineffective [6,17]. Recent interest has focused on the
prophylactic use of the oxytocin receptor agonist carbetocin
(DURATOCIN, PABAL, LONACTENE, Ferring Pharmaceuticals SA, St.
Prex, Switzerland) [2023]. Here we review the most recent
clinical data regarding the efcacy of carbetocin in the prevention
of postpartum haemorrhage following caesarean section and
vaginal delivery, and provide an update on the safety and
tolerability in comparison to conventional uterotonic agents.
2. Pharmacological properties
Carbetocin is a long-acting synthetic analogue of oxytocin
[24,25] that can be administered as a single-dose injection, either
intravenously or intramuscularly [26]. Intravenously administered
carbetocin has a half-life of approximately 40 min [26], around 4
10 times longer than that reported for oxytocin [911]. Following
intramuscular injection, carbetocin reaches peak plasma concen-
trations in less than 30 min and has 80% bioavailability [26]. The
effect of various intravenous and intramuscular doses of carbetocin
on the postpartum uterus has been evaluated by tocographic
recordings of uterine contractions 2448 h after vaginal delivery at
term in 40 women [27]. A single intravenous bolus of 830 mg
carbetocin or a single intramuscular injection of 1070 mg
carbetocin produced a tetanic uterine contraction within 2 min
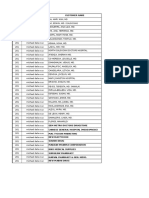
Table 1
Prevention of postpartum haemorrhage: summary of carbetocin vs. conventional uterotonic drugs in caesarean and vaginal delivery.
Study Population Intervention Main outcome
Caesarean delivery
RCT (29) n = 57 elective delivery 100 mg intravenous carbetocin
(n = 29) vs. 16-h intravenous
infusion 32.5 IU oxytocin
(n = 28) after placenta delivery
Mean intraoperative blood loss
was 158 vs. 188 ml, respectively
(p = 0.30). Signicantly fewer
women had blood loss 200 ml
with carbetocin (53%) vs. oxytocin (79%) (p = 0.041)
RCT (30) n = 694 elective delivery 100 mg intravenous carbetocin
(n = 317) vs. intravenous oxytocin
(5 IU bolus followed by infusion of 20 IU
over 8 h) (n = 318) after infant
(87%) or placenta (13%) delivery
Additional oxytocic intervention for uterine atony
(primary outcome) was 4.7% and 10.1%, respectively
(p < 0.05). Odds ratio for treatment failure requiring
oxytocic intervention was 2.03 times higher with
oxytocin vs. carbetocin (95% CI = 1.12.8)
Randomised pragmatic
clinical trial (32)
n = 152 at high risk of PPH 100 mg intravenous carbetocin
(n = 77) vs. 5 IU
intravenous oxytocin (n = 75)
Uterine atony evident in 8% vs. 19%, respectively
(p < 0.0001). Intraoperative blood loss 500 ml
only observed with oxytocin
Vaginal delivery
RCT (20) n = 160 at risk of PPH 100 mg carbetocin im + placebo
iv (n = 83) vs. 10 IU oxytocin in
a 2-h intravenous infusion + placebo
im (n = 77) administered immediately
after placental delivery
Uterine massage required in 43.4% vs. 62.3%,
respectively (p < 0.025). Uterotonic intervention
clinically indicated in 44.6% vs. 63.6%, respectively (p < 0.025)
RCT (21) n = 329 singleton
pregnancy,
delivery 34 weeks,
low PPH risk
100 mg intramuscular carbetocin
(n = 165) vs. intramuscular
syntometrine (5 IU oxytocin
and 0.5 mg ergometrine)
(n = 164) at the end of the second
stage of labour
No signicant difference in mean reduction in
haemoglobin concentration in rst 48 h
(1.4 vs. 1.5 g/dl, respectively) or need for additional
oxytocin injections (8.7% vs. 6.7%, respectively)
Retrospective
study (22)
n = 118 delivery
at term in
routine clinical
setting
100 mg intramuscular carbetocin
vs. intramuscular combination
of 5 IU oxytocin and 0.2 mg
ergometrine immediately
after infant delivery
Mean blood loss was 388 vs. 551 ml, respectively
(p = 0.01). Blood loss 500 ml was 21.4 vs. 43.5%,
respectively (p = 0.01) and blood loss 1000 ml
was 1.8% vs.14.5%, respectively (p = 0.02)
RCT, randomised controlled trial; PPH, postpartum haemorrhage.
W. Rath/ European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520 16
of drug administration [27]. Uterine activity persisted for an
average of 120 min following intramuscular injection and an
average of 60 min following intravenous injection [27]. Thus, these
data show that carbetocin onset of action is rapid irrespective of
administration route, but duration of action is longer following
intramuscular injection. The optimal carbetocin dose (intravenous
or intramuscular) is 100 mg [28].
3. Efcacy in caesarean delivery
Carbetocin is currently approved in 23 countries for prevention
of uterine atony and excessive bleeding following caesarean
delivery in spinal or epidural anaesthesia. This therapeutic
indication is supported by the results of two published controlled
clinical trials [29,30]. The rst study fromMontreal (Canada) was a
parallel-group, randomised, double-blind, double-dummy trial,
comparing uterotonic efcacy and safety of carbetocin and
oxytocin in 57 women undergoing elective caesarean section
[29]. A single 100 mg intravenous injection of carbetocin following
placental delivery was at least as effective as a 16-h intravenous
infusion of 32.5 IU oxytocin in controlling intraoperative blood
loss. No signicant differences in mean blood loss were observed
between treatment groups (Table 1). However, signicantly fewer
women in the carbetocin group (53%) than in the oxytocin group
(79%) had blood loss of 200 ml (p = 0.041) (Table 1). The second
study was a larger parallel-group, randomised, double-blind,
double-dummy, Canadian multi-centre trial, comparing the
efcacy and safety of carbetocin and oxytocin in 694 women
undergoing elective caesarean section [30]. A single 100 mg
intravenous injection of carbetocin was more effective at
preventing uterine atony than a 5 IU intravenous bolus of oxytocin
followed by intravenous infusion of 20 IU over 8 h; a signicantly
lower incidence of additional oxytocic interventions for treatment
failure was observed in the carbetocin arm (Table 1).
Data from these two studies were pooled to determine overall
treatment effect in a recent meta-analysis [23]. The risk of
postpartumhaemorrhage, dened as a blood loss 500 ml, was not
signicantly decreased with carbetocin compared with oxytocin
(relative risk [RR] = 0.71 and 95% condence interval [CI] = 0.14
3.53). However, carbetocin signicantly reduced the need for
subsequent interventions with uterotonic drugs (RR = 0.44, 95%
CI = 0.250.78) or uterine massage (RR = 0.38, 95% CI = 0.180.80)
compared with oxytocin. The authors [23] also evaluated a
randomised controlled trial published in abstract form [31],
comparing a single 100 mg intravenous injection of carbetocin
(n = 62) vs. placebo (n = 57) following elective caesarean section.
Postpartum haemorrhage incidence was not reported as an
outcome measure and could not be assessed, but the requirement
for additional oxytocic therapy to prevent haemorrhage was
signicantly lower with carbetocin vs. placebo (RR = 0.18, 95%
CI = 0.090.35). Moreover, women in the carbetocin group
demonstrated a signicant increase in uterine tone for 20 min
following administration of study medication compared with
placebo (p < 0.05).
Another study, published in abstract form[32], investigated the
efcacy of carbetocin vs. oxytocin for prevention of uterine atony
in high-risk women undergoing delivery by caesarean section in
Mexico (Table 1). Risk factors included fetal macrosomia, poly-
hydramnios, lowplacental insertion, multiple gestation, prolonged
labour, uterine myomas and chorioamnionitis. The main efcacy
outcome measure was uterine atony incidence. A total of 77
women received carbetocin and 75 received oxytocin following
caesarean delivery. Signicantly fewer women experienced
uterine atony after caesarean delivery with carbetocin (8%) vs.
oxytocin (19%) (p < 0.0001). Blood loss 500 ml was only observed
in women who received oxytocin.
4. Efcacy in vaginal delivery
The efcacy of prophylactic carbetocin has also been investi-
gated in prevention of postpartum haemorrhage following vaginal
delivery. A randomised, double-blind, placebo-controlled study
has compared the efcacy of a single 100 mg intramuscular dose of
carbetocin with a 2-h intravenous infusion of 10 IU oxytocin [20]
(Table 1). The study was conducted in two hospital centres in
Canada and enrolled 160 women (83 in the carbetocin arm and 77
in the oxytocin arm) with 1 known risk factor including: history
of previous postpartum haemorrhage or retained placenta, grand
multiparity, uterine overdistension related to multiple gestation,
fetal macrosomia or polyhydramnios, chorioamnionitis, antepar-
tum haemorrhage, induction or augmentation of labour with
oxytocin for at least 4 h, prolonged labour or rapid excessive
labour. Treatment began immediately following placental delivery.
The primary outcome measure was the need for additional
uterotonic medications to prevent postpartum haemorrhage.
Other efcacy variables included the need for uterine massage,
change in haemoglobin and haematocrit over the initial 24 h
postpartum, estimated blood loss following study drug adminis-
tration to the end of delivery, uterine tone and amount/type of
lochia. The number of women requiring additional uterotonic
medication was comparable between treatment groups but
signicantly fewer women required at least one uterine massage
following treatment with carbetocin (43.4%) vs. oxytocin (62.3%)
(p < 0.025). Overall, uterotonic intervention (either additional
uterotonic agents or uterine massage) was required in 44.6% of
women who received carbetocin and in 63.6% of women who
received oxytocin, a statistically signicant difference (p < 0.025).
No signicant differences were observed between treatment
groups for other efcacy variables. The investigators concluded
that a single intramuscular injection of carbetocin is more likely to
prevent postpartum haemorrhage in high-risk women than a
continuous intravenous infusion of oxytocin.
Another randomised, double-blind, controlled trial has com-
pared efcacy and safety of intramuscular carbetocin with
intramuscular syntometrine in preventing primary postpartum
haemorrhage in low-risk women with singleton pregnancy
achieving vaginal delivery from 34 weeks [21] (Table 1). The
setting was the delivery suite of a university-based obstetric unit in
Hong Kong. A total of 329 women were randomised to receive
either a single intramuscular injection of 100 mg carbetocin
(n = 165) or a single intramuscular injection of 1 ml syntometrine
(5 IU oxytocin and 0.5 mg ergometrine) (n = 164) after the second
stage of labour (following anterior shoulder delivery). The primary
efcacy outcome was reduction in haemoglobin levels from
admission to the labour ward until 48 h after delivery. Secondary
efcacy outcomes included the need for additional oxytocin
injections, the incidence of 500 ml blood loss and the incidence of
retained placenta. The study did not demonstrate signicant
differences between treatment arms for any of the efcacy
outcomes. Thus, intramuscular carbetocin was considered as
effective as intramuscular syntometrine in preventing primary
postpartum haemorrhage following vaginal delivery in low-risk
women.
A recent retrospective study has also compared carbetocin
efcacy with combined use of oxytocin and ergometrine following
routine vaginal delivery in Macau, China [22] (Table 1). Women
(n = 118) received either a single intramuscular injection of 100 mg
carbetocin or a single intramuscular injection of 5 IU oxytocin and
0.2 mg ergometrine immediately following delivery. Signicantly
less blood loss was observed with carbetocin compared with
oxytocin and ergometrine (p = 0.01), with a mean difference
between treatment groups of 163 ml. Postpartum haemorrhage
incidence, dened as blood loss 500 ml, was signicantly lower in
W. Rath/ European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520 17
the carbetocin group (21.4%) than in the combination group
(43.5%) (p = 0.01). Notably, nine patients (14.5%) in the combina-
tion group experienced 1000 ml blood loss compared with one
patient (1.8%) in the carbetocin group (p = 0.02), and a signicantly
greater reduction in haematocrit was observed with oxytocin and
ergometrine compared with carbetocin. The authors concluded
that carbetocin should be considered a good alternative to
conventional uterotonics in preventing postpartum haemorrhage
after vaginal delivery. In this retrospective study, carbetocin
displayed signicantly better uterotonic activity than an oxytocin/
ergometrine combination containing less than half the ergome-
trine dose contained in syntometrine [21]. However, these ndings
are still of interest as these retrospective data more closely reect
everyday clinical practice.
5. Tolerability and safety prole
5.1. Pharmacological studies in volunteers
In pharmacokinetic and dose-tolerance studies, up to 400 mg of
intravenous or intramuscular carbetocin was associated with the
occurrence of minimal adverse effects (mainly facial ushing and
feeling of warmth) in non-pregnant women [26]. After intramus-
cular administration of 400 and 800 mg, a signicant increase in
pulse rate was observed [26]. A study assessing uterotonic effects
of various doses of intramuscular or intravenous carbetocin on the
postpartumuterus 2448 h following vaginal delivery at term[27]
revealed that carbetocin produced mild abdominal cramping in
most women. Severe abdominal pain was reported by three
women who received doses of 50 or 100 mg intravenously or 70 mg
intramuscularly. Less frequently reported adverse events were
back pain, facial ushing and feeling of warmth. Similar to the
study previously mentioned [26] a transient increase in pulse rate
occurred 5 min after intramuscular administration of 70 mg
carbetocin (78.5 0.7 to 81.7 0.07 beats/min), not reaching the
level of tachycardia. A signicant decrease in blood pressure was not
observed. A mild increase in blood pressure (max. 140/80 mmHg)
that produced distressing abdominal pain was found in only two
patients following intravenous injection doses (50 and 100 mg).
In an ascending dose-tolerance study with intramuscular
carbetocin [28], a single injection of carbetocin (range 15
200 mg) was administered immediately after birth to healthy
women who delivered vaginally at term. There was no dose-
dependent effect on blood pressure, heart rate and respiratory rate
and no cases of nausea, vomiting or pruritus were reported.
Incidence of abdominal pain and tremor were 27% and 40%,
respectively. Abdominal pain was only severe enough to suggest a
possible link with carbetocin in one case (2%) [28]. There were six
cases of 1000 ml blood loss and four cases of retained placenta
[28]. Most of these serious adverse events occurred in women who
had received the highest dose of intramuscular carbetocin
(200 mg) and only the retained placenta cases were considered
to be possibly linked to carbetocin use by the investigators [28,33].
Lowest blood loss was recorded with 75125 mg carbetocin and
drug-related serious adverse events were not evident until at least
125 mg was administered. These ndings conrm that the
intramuscular dose of 100 mg carbetocin, effectively used for
prevention of uterine atony following vaginal delivery in all
recently published studies [2022], is the optimal dose with
respect to safety and tolerability.
Another study evaluated drug transfer to breast milk following
intramuscular injection of 70 mg carbetocin in ve healthy women
([714] weeks postpartum) [34]. The mean AUC of carbetocin
concentration in breast milk over 240 min following drug
administration was 50 times lower than plasma concentration
(18.6 and 29.0 pg/ml for the right and left breast, respectively,
compared with 1119.3 pg/ml in plasma). The small amounts
transferred from plasma into colostrum or breast milk following a
single injection of carbetocin presents little risk to breast-fed
infants [34]. Since carbetocin is a peptide, a small amount of drug
ingested by an infant is assumed to be rapidly degraded by gut
enzymes [33,34].
5.2. Tolerability and safety prole in clinical trials in caesarean
delivery
Adverse events reported by 10% of women who received
prophylactic intravenous carbetocin following caesarean delivery
were headache, tremor, hypotension, ushing, nausea, abdominal
pain, pruritus and feeling of warmth (Table 2) [33]. In the trial
comparing carbetocin with placebo, ushing, abdominal pain and
pruritus were more frequently observed with carbetocin and the
drug was associated with decreased blood pressure and transient
tachycardia [31]. Adverse events observed in the carbetocin vs.
oxytocin trials were similar in type and frequency between
treatment arms [2930,33] and the meta-analysis fromthese trials
conrmed that the risk of experiencing headache, tremor,
dizziness, ushing, shortness of breath, premature ventricular
contractions/tachycardia, abdominal pain, nausea, vomiting,
metallic taste, pruritus, back pain, feeling of warmth, chills or
sweating was similar with carbetocin or oxytocin [23].
5.3. Tolerability and safety prole in clinical trials in vaginal delivery
Use of carbetocin in vaginal delivery also revealed a similar
safety prole to oxytocin [20]. The incidence of dizziness, tremor
and vasodilation were comparable between treatment arms.
However, the incidence of headache was 2-fold lower with
carbetocin (7.2%) vs. oxytocin (14.3%), and vomiting (7.8%) and
pruritus (5.2%) were only reported in the oxytocin arm. Conversely,
abdominal pain was only reported in women who received
carbetocin (6%). Other adverse events previously reported (e.g.
increased pulse, decreased diastolic blood pressure and feeling of
warmth) were not observed in this trial [20].
Comparison of adverse events with carbetocin and syntome-
trine revealed that nausea and vomiting were signicantly reduced
with carbetocin [21]. Facial ushing and pain at the injection site
were only reported in the syntometrine arm (2% and 0.7%,
respectively). Hypertension (dened as blood pressure 140/
90 mmHg) at 30 and 60 min following delivery was 5.3% and 4% in
Table 2
Adverse events observed in clinical trials with carbetocin following caesarean section after administration under spinal or epidural anaesthesia [33].
System organ class disorders Very common (1/10) Common (1/100 and <1/10) Uncommon or sporadic (<1/100)
Blood and lymphatic system Anaemia
Nervous system Headache, tremor Dizziness
Vascular Hypotension, ushing
Respiratory, thoracic and mediastinal Chest pain, dyspnoea Tachycardia
Gastrointestinal Abdominal pain, nausea Metallic taste, vomiting
Skin and subcutaneous tissue Back pain
General and administration site conditions Feeling of warmth Chills, pain Sweating
W. Rath/ European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520 18
the syntometrine group, respectively, whereas hypertension was
not observed in the carbetocin group at either time point. However,
21.3% experienced tachycardia (dened as maternal pulse
100 beats/min) within 60 min of delivery with carbetocin,
compared with 12.7% in the syntometrine group. The duration
of tachycardia was not reported in this study. Only one out of 150
women (0.7%) in the carbetocin group required manual removal of
retained placenta compared with three out of 150 women (2%) in
the syntometrine group. The retrospective study comparing
carbetocin with the combination of oxytocin and ergometrine
did not report any safety and tolerability data [22].
6. Cost-effectiveness of carbetocin vs. other uterotonic agents
One study from Mexico has compared cost-effectiveness of
prophylactic carbetocin and oxytocin following caesarean section
[32]. Cost-effectiveness was modelled from the perspective of the
third party payer (Mexican Institute of Social Security) and
resource use was obtained from the clinical trial data (Table 1).
Costs were estimated using the nancial information provided by
the Mexican Institute of Social Security and were reported in USD.
Univariate and probabilistic sensitivity analyses were performed
using probability distribution data from the clinical trial and the
Monte Carlo Simulation technique [35]. The mean cost per woman
was signicantly lower following carbetocin treatment (3525 USD)
compared with oxytocin treatment (4054 USD) (p < 0.0001). The
mean cost-effectiveness ratio was 3874 USD for carbetocin and
4944 USD for oxytocin. The incremental cost-effectiveness ratio
revealed that carbetocin was dominant and the cost-effectiveness
acceptability curve and net health benets demonstrated that
carbetocin was superior to oxytocin independently of the will-
ingness-to-pay threshold.
7. Conclusion
Carbetocin is a long-acting synthetic analogue of oxytocin that
combines the safety and tolerability prole of oxytocin with the
sustained uterotonic activity of ergometrine and is currently
indicated for the prevention of uterine atony following caesarean
delivery. Evidence from three randomised controlled trials
indicates that a single intravenous injection of 100 mg carbetocin
signicantly reduces the need for additional uterotonic interven-
tions to maintain adequate uterine tone and prevent/treat
excessive bleeding following caesarean delivery vs. placebo or
intravenous oxytocin. Furthermore, the administration of a single
injection of carbetocin is more convenient than an oxytocin
infusion, which requires an intravenous line and is time-
consuming. In high-risk women, carbetocin is superior to oxytocin
in preventing 500 ml of blood loss following caesarean section
and may represent the most cost-effective uterotonic drug in
developing countries with low resources, as suggested by the
results of the clinical trial conducted in Mexico.
Two recent randomised controlled clinical trials and one
retrospective study have indicated that carbetocin may also
represent a good alternative to conventional uterotonic agents
for prevention of postpartum haemorrhage after vaginal delivery.
When administered as a single 100 mg dose, carbetocin has
demonstrated longer duration of action compared with intrave-
nous oxytocin, as indicated by the reduced need for additional
uterotonic interventions in high-risk women with carbetocin.
Carbetocin is also at least as effective as syntometrine for
management of the third stage of labour in low-risk women.
Carbetocin has been associated with a low incidence of adverse
effects, with a similar tolerability prole to intravenous oxytocin. It
has also been associated with a lower incidence of gastrointestinal
side effects compared with the combination of oxytocin and
ergometrine. A higher rate of tachycardia has been reported with
carbetocin vs. syntometrine. Tachycardia duration was not
reported, but based on available data fromother trials, a transitory
and slight increase of no clinical relevance would be expected. In
this context it must be taken into account that the denition of
physiological tachycardia in pregnancy ranges from 100 to
120 beats/min. Carbetocin appears to have a better cardiovascular
side-effect prole than oxytocin or syntometrine. However, data
from the hitherto published literature are limited. The effect of
carbetocin on blood pressure needs further investigation, and
preeclampsia remains a contraindication to the use of carbetocin.
Available data are encouraging to suggest carbetocin could become
useful for prevention of postpartum haemorrhage even in
preeclamptic pregnant women.
Nevertheless, the careful assessment of the patients history
and close blood pressure monitoring are mandatory in each patient
treated with carbetocin, in particular in those with suspected pre-
existing cardiovascular disease.
The promising ndings from these studies suggest that
carbetocin may become the drug of choice for prevention of
postpartum haemorrhage after vaginal delivery in high-risk
women. More trials in low-risk women who undergo vaginal
delivery are needed to assess whether carbetocin is superior to
conventional uterotonic drugs for the majority of pregnant
women. Also, further studies could be conducted to determine if
single intramuscular administration of carbetocin is advantageous
in settings where prophylactic use of intravenous uterotonics is
unsafe or impracticable, like in domiciliary practice or in third
stage of labour management in developing countries.
Acknowledgments
The author is grateful to Ferring Pharmaceuticals who provided
funding through an unrestricted educational grant.
References
[1] Prendiville W, Elbourne D, Chalmers I. The effects of routine oxytocic admin-
istration in the management of the third stage of labor: an overview of the
evidence from controlled clinical trials. Br J Obstet Gynecol 1988;95:316.
[2] Rochat RW, Koonin LM, Atrash HK, Jewett JF, the Maternal Mortality Colla-
borative. Maternal mortality in the United States: report from the Maternal
Mortality Collaborative. Obstet Gynecol 1988;72:917.
[3] Li XF, Fortney JA, Kotelchuck M, Glover LH. The postpartum period: the key to
maternal mortality. Int J Gynecol Obstet 1996;54:110.
[4] World Health Organization. Global estimates of maternal mortality for 1995:
results of an in-depth review analysis and estimation strategy (statement).
Geneva: World Health Organization; 2001.
[5] Bouwmeester FW, Boltc AC, van Geijn HP. Pharmacological and surgical
therapy for primary postpartum haemorrhage. Curr Pharm Des 2005;11:
75973.
[6] Chong Y-S, Su L-L, Arulkumaran S. Current strategies for the prevention of
postpartum haemorrhage in the third stage of labour. Curr Opin Obstet
Gynecol 2004;16:14350.
[7] Wedisinghe L, Macleod M, Murphy DJ. Use of oxytocin to prevent haemorrhage
at caesarean sectiona survey of practice in the United Kingdom. Eur J Obstet
Gynecol Reprod Biol 2008;137:2730.
[8] Ozumba BC, Ezegwui HU. Blood transfusion and caesarean section in a
developing country. J Obstet Gynecol 2006;26:7468.
[9] Ryden G, Sjoholm J. Half-life of oxytocin in blood of pregnant and non-
pregnant women. Acta Endocrinol (Copenh) 1969;61:42531.
[10] Fabian M, Forsling M, Jones J. The clearance and antidiuretic potency of
neurohypophysal hormones in man, and their plasma binding and stability.
J Physiol 1969;204:6538.
[11] Chard T, Boyd N, Forsling M. The development of a radioimmunoassay for
oxytocin: the extraction of oxytocin fromplasma, and its measurement during
parturition in human and goat blood. J Endocrinol 1970;48:22334.
[12] McDonald S, Abbott JM, Higgins SP. Prophylactic ergometrine-oxytocin versus
oxytocin for the third stage of labour. Cochrane Database Syst Rev; 2004 [Issue
I. Art. No: CD000201].
[13] Liabsuetrakul T, Choobun T, Peeyanajarassri K, Islam QM. Prophylactic use of
ergot alkaloids in the third stage of labour. Cochrane Database Syst Rev; 2007
[Issue 2. Art. No: CD005456].
W. Rath/ European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520 19
[14] Choy CM, Lau WC, Tam WH, Yuen PM. A randomized controlled trial of
intramuscular syntometrine and intravenous oxytocin in the management
of the third stage of labour. BJOG 2002;109:1737.
[15] Dumoulin JG. A reappraisal of the use of ergometrine. J Obstet Gynecol
1981;1:17881.
[16] Carey M. Adverse cardiovascular sequelae of ergometrine. Br J Obstet Gynecol
1993;100:865.
[17] Gu lmezoglu AM, Forna F, Villar J, Hofmeyr GJ. Prostaglandins for prevention of
Postpartum haemorrhage. Cochrane Database Syst Rev; 2004 [Issue I. Art. No:
CD000494].
[18] Villar J, Gu lmezoglu AM, Hofmeyr GJ, Forna F. Systematic review of rando-
mized controlled trials of misoprostol to prevent postpartum haemorrhage.
Obstet Gynecol 2002;100:130112.
[19] Chong YS, Chua S, Arulkumaran S. Severe hyperthermia following oral mis-
oprostol in the immediate postpartumperiod. Obstet Gynecol 1997;90:7034.
[20] Boucher M, Nimrod CA, Tawagi GF, Meeker TA, Rennicks White RE, Vann J.
Comparison of carbetocin and oxytocin for the prevention of postpartum
haemorrhage following vaginal delivery: a double-blind randomized trial. J
Obstet Gynecol Can 2004;26:4818.
[21] Leung SW, Ng PS, Wong WY, Cheung TH. A randomized trial of carbetocin
versus syntometrine in the management of the third stage of labour. BJOG
2006;113:145964.
[22] Ngan L, Keong W, Martins R. Carbetocin versus a combination of oxytocin and
ergometrine in control of postpartum blood loss. Int J Gynecol Obstet
2007;97:1523.
[23] Su LL, Chong YS, Samuel M. Oxytocin agonists for preventing postpartum
haemorrhage. Cochrane Database Syst Rev; 2007 [Issue 3. Art. No: CD005457].
[24] Atke A, Vilhardt H. Uterotonic activity and myometrial receptor afnity of I-
deamino-I-carba-2-tyrosine (O-methyl)-oxytocin. Acta Endocrinol (Copenh)
1987;19:9716.
[25] Norstro m A, Andersson A, Vilhardt H. Contractile effect of oxytocin and I-
deamino-l-carba-2-tyrosine (O-methyl)-oxytocin in myometrial tissue from
non-pregnant and term pregnant women. Acta Endocrinol (Copenh)
1990;122:5668.
[26] Sweeney G, Holbrook AM, Levine M, et al. Pharmacokinetics of carbetocin, a
long-acting oxytocin analogue, in nonpregnant women. Curr Ther Res
1990;47:52040.
[27] Hunter DJ, Schulz P, Wassenaar W. Effect of carbetocin, a long-acting oxytocin
analogue in the postpartum uterus. Clin Pharmacol Ther 1992;52:607.
[28] van Dongen PW, Verbruggen MM, de Groot ANJA, van Roosmalen J, Sporken
JMJ, Schulz M. Ascending dose tolerance study of intramuscular carbetocin
administered after normal vaginal birth. Eur J Obstet Gynecol Reprod Biol
1998;77:1817.
[29] Boucher M, Horbay GLA, Grifn P, Deschamps Y, Desjardins C, Schulz M,
Wassenar W. Double-blind, randomized comparison of the effect of carbetocin
and oxytocin on intraoperative blood loss and uterine tone of patients under-
going cesarean section. J Perinatol 1998;18:2027.
[30] Dansereau J, Joshi AK, Helewa ME, et al. Double-blind comparison of carbe-
tocin versus oxytocin in prevention of uterine atony after cesarean section. Am
J Obstet Gynecol 1999;180:6706.
[31] Barton SR, Jackson A. The safety and efciency of carbetocin to control
uterine bleeding following caesarean section. Prenat Neonatal Med
1996;1:185.
[32] Del Angel-Garcia G, Garcia-Contreras F, Constantino-Casas P, et al. Economic
evaluation of carbetocine for the prevention of uterine atony in patients with
risk factors in Mexico. Value Health 2006;9(6):A254.
[33] Ferring Pharmaceuticals: Global Pharmacovigilance. Periodic safety update
report for carbetocin. 17 July 2006. On le at Ferring Pharmaceutical A/S,
Copenhagen. Denmark.
[34] Silcox J, Schulz P, Horbay GLA, Wassenaar W. Transfer of carbetocin into
human breast milk. Obstet Gynecol 1993;82:4569.
[35] Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity
analysis using Monte Carlo Simulation. A practical approach. Med Decis
Making 1985;5:15777.
W. Rath/ European Journal of Obstetrics & Gynecology and Reproductive Biology 147 (2009) 1520 20
You might also like
- Avatar Neytiri 1Document48 pagesAvatar Neytiri 1Jheix Diniz100% (5)
- Evarrest MonographDocument24 pagesEvarrest MonographbasakerpolatNo ratings yet
- Roller Sakai R2H-2 Shop ManualDocument151 pagesRoller Sakai R2H-2 Shop ManualQuang Tuan100% (4)
- The Potential Role of Sunitinib in Gastrointestinal Cancers Other Than GISTDocument8 pagesThe Potential Role of Sunitinib in Gastrointestinal Cancers Other Than GISTcesarjbcNo ratings yet
- Molecular and Cellular EndocrinologyDocument8 pagesMolecular and Cellular Endocrinologyapi-25984300No ratings yet
- Laboratory Diagnosis of Parasites From The Gastrointestinal TractDocument81 pagesLaboratory Diagnosis of Parasites From The Gastrointestinal TractMariam Mata100% (1)
- Background Paper 6.16 Postpartum HaemorrhageDocument35 pagesBackground Paper 6.16 Postpartum HaemorrhageAkrm Al-komimNo ratings yet
- Aftryp SWG PDFDocument182 pagesAftryp SWG PDFij EducationNo ratings yet
- Diagnosis and Managment of Gaynecologic CancersDocument1,067 pagesDiagnosis and Managment of Gaynecologic CancersarisNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument7 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyfujimeisterNo ratings yet
- Farmacocinetica y Farmacodinami de MMF Clin Pharmacokinet 2007 46 1 13-58Document46 pagesFarmacocinetica y Farmacodinami de MMF Clin Pharmacokinet 2007 46 1 13-58Maria Marina Papaginovic LeivaNo ratings yet
- Multiple Myeloma Patient Education Manual: October 2007 EditionDocument85 pagesMultiple Myeloma Patient Education Manual: October 2007 EditionKareem WaheedNo ratings yet
- Treatment of Vaginal Bleeding Irregluarities Induced by Progestin Only ContraceptivesDocument67 pagesTreatment of Vaginal Bleeding Irregluarities Induced by Progestin Only ContraceptivesAlejandro VillalpandoNo ratings yet
- Intrathecal Antibacterial and Antifungal TherapiesDocument24 pagesIntrathecal Antibacterial and Antifungal TherapiesntnquynhproNo ratings yet
- Antifungicos y Antibioticos IntratecalesDocument24 pagesAntifungicos y Antibioticos IntratecalesRu MNo ratings yet
- 2019 ELSO Meeting Abstracts.1Document109 pages2019 ELSO Meeting Abstracts.1Luis Rubén MirandaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument7 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyDiana Carolina di Filippo VillaNo ratings yet
- A and Lactation: Safe Vitamin Dosage During PregnancyDocument46 pagesA and Lactation: Safe Vitamin Dosage During PregnancyastrimentariNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument9 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologyrolla_hiraNo ratings yet
- Impact of Cows' Milk Estrogen On Cancer RiskDocument12 pagesImpact of Cows' Milk Estrogen On Cancer RiskCHRISTIAN BENJAMIN CHANG CORNEJO100% (1)
- GoserelinDocument9 pagesGoserelinbibiutzNo ratings yet
- Cancer Preventive and Therapeutic Effects of EGCG The Major Polyphenol in Green TeaDocument24 pagesCancer Preventive and Therapeutic Effects of EGCG The Major Polyphenol in Green TeaEmanuela MerticariuNo ratings yet
- Iron Deficiency and Anaemia in Women in the Gynaecological and Obstetrical Practice (with Case Reports)From EverandIron Deficiency and Anaemia in Women in the Gynaecological and Obstetrical Practice (with Case Reports)No ratings yet
- Middle East Fertility Society Journal: Maryam Eftekhar, Nasim Tabibnejad, Afsar Alsadat TabatabaieDocument7 pagesMiddle East Fertility Society Journal: Maryam Eftekhar, Nasim Tabibnejad, Afsar Alsadat TabatabaieDrAstha GuptaNo ratings yet
- Pharmaceuticals and Women: Priority Medicines For Europe and The World "A Public Health Approach To Innovation"Document22 pagesPharmaceuticals and Women: Priority Medicines For Europe and The World "A Public Health Approach To Innovation"Rifael Satrio AdinugrohoNo ratings yet
- Antepartum Haemorrhage - CTM Guideline 2020Document20 pagesAntepartum Haemorrhage - CTM Guideline 2020Kvy OngNo ratings yet
- 2018 Vaccine Confidence en PDFDocument77 pages2018 Vaccine Confidence en PDFRobert EnteenNo ratings yet
- Critical Reviews in Oncology/HematologyDocument10 pagesCritical Reviews in Oncology/HematologyAndrea RangelNo ratings yet
- Ofirmev Monograph FinalDocument40 pagesOfirmev Monograph FinalDrFarah Emad AliNo ratings yet
- European Evidence-Based Consensus On The Management of Ulcerative Colitis: Current ManagementDocument39 pagesEuropean Evidence-Based Consensus On The Management of Ulcerative Colitis: Current ManagementPriyatna NhaNo ratings yet
- Etizolam Article1 Who 2016Document22 pagesEtizolam Article1 Who 2016Stiven DestNo ratings yet
- Management of Postpartum Haemorrhage PPHDocument19 pagesManagement of Postpartum Haemorrhage PPHamanabduwahabNo ratings yet
- Ezx 314Document29 pagesEzx 314Adventa 91No ratings yet
- ''Sangrado Perioperatorio Severo GuiaDocument113 pages''Sangrado Perioperatorio Severo GuiaHECTOR ESTRADANo ratings yet
- FDA Sientra Briefing PackageDocument50 pagesFDA Sientra Briefing PackageMaresNo ratings yet
- Treatment For Primary Postpartum Haemorrhage (Review) : Mousa HA, Alfirevic ZDocument27 pagesTreatment For Primary Postpartum Haemorrhage (Review) : Mousa HA, Alfirevic ZDownloadNo ratings yet
- Cuscuta Chinensislam. - A Systematic Review On PDFDocument17 pagesCuscuta Chinensislam. - A Systematic Review On PDFDintakurthi PrasanthNo ratings yet
- CD 005646Document21 pagesCD 005646Pool Chavez CernaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument9 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyJose Alfredo Juarez VelazquezNo ratings yet
- Abortion Care Thrombose ProfylaxeDocument22 pagesAbortion Care Thrombose ProfylaxeambiebieNo ratings yet
- Full Text 03Document49 pagesFull Text 03Shandy Suwanto PutraNo ratings yet
- Clinical Microbiology Reviews-2017-Garcia-e00025-17.fullDocument81 pagesClinical Microbiology Reviews-2017-Garcia-e00025-17.fullJoshua ElbanbuenaNo ratings yet
- Demicheli Et Al - 2000 - Prevention and Early Treatment of Influenza in Healthy AdultsDocument74 pagesDemicheli Et Al - 2000 - Prevention and Early Treatment of Influenza in Healthy AdultsМихаил РайцисNo ratings yet
- Hyponatraemia in Cancer PatientDocument11 pagesHyponatraemia in Cancer Patientfahadrock2002No ratings yet
- 1 s2.0 S2468784720303457 MainDocument7 pages1 s2.0 S2468784720303457 MainsandrakucabaNo ratings yet
- BST Obstetrics Gynaecology Curriculum 2018 19 Years 23 Printable Version PDFDocument78 pagesBST Obstetrics Gynaecology Curriculum 2018 19 Years 23 Printable Version PDFshruthi mzmcNo ratings yet
- (Lippincott Manual Series) Canan Avunduk - Manual of Gastroenterology - Diagnosis and Therapy-LWW (2008)Document528 pages(Lippincott Manual Series) Canan Avunduk - Manual of Gastroenterology - Diagnosis and Therapy-LWW (2008)Nguyễn Võ Anh Tiến100% (1)
- NHBPEPDocument52 pagesNHBPEPjofizamNo ratings yet
- CisPt TOP Dasari2014 PDFDocument15 pagesCisPt TOP Dasari2014 PDFJuanita Pulido TeutaNo ratings yet
- CisplatinDocument15 pagesCisplatinJaya Semara PutraNo ratings yet
- Catheter-Associated UrinaryDocument78 pagesCatheter-Associated UrinaryFaozan FikriNo ratings yet
- C Ovid 19 Treatment GuidelinesDocument459 pagesC Ovid 19 Treatment GuidelinesRamya RSNo ratings yet
- 0 Pfizer-BioNTech Information For VaccinatorsDocument27 pages0 Pfizer-BioNTech Information For VaccinatorsCan O.No ratings yet
- Hernia CCDocument50 pagesHernia CCEddy Romario Vilcanqui JiménezNo ratings yet
- Islam Et Al. - 2015 - Cancer Stem Cells in Oesophageal Squamous Cell Carcinoma Identification, Prognostic and Treatment PerspectivesDocument11 pagesIslam Et Al. - 2015 - Cancer Stem Cells in Oesophageal Squamous Cell Carcinoma Identification, Prognostic and Treatment PerspectivesCarly LeungNo ratings yet
- A Review of The Literature On The Effects of Acetaminophen On Pregnancy OutcomeDocument13 pagesA Review of The Literature On The Effects of Acetaminophen On Pregnancy OutcomeJack AndreasNo ratings yet
- Biochemical Pharmacology: Prabhavathi Fernandes, Evan MartensDocument12 pagesBiochemical Pharmacology: Prabhavathi Fernandes, Evan MartensMarco OliveiraNo ratings yet
- Oncologic Results of Fertility Sparing Surgery of Cervical Cancer - An Updated Systematic ReviewDocument15 pagesOncologic Results of Fertility Sparing Surgery of Cervical Cancer - An Updated Systematic Reviewdelapm22No ratings yet
- PlacentaDocument102 pagesPlacentaHazel MarananNo ratings yet
- Chart Booklet 2 Months To 5 YearsDocument59 pagesChart Booklet 2 Months To 5 YearsCaptain MesencephalonNo ratings yet
- Acute Otitis Media FaridDocument13 pagesAcute Otitis Media Fariddr.cintaNo ratings yet
- Report of A Case Treated With Acetylbetah (Ethylcholine Broi IdeDocument8 pagesReport of A Case Treated With Acetylbetah (Ethylcholine Broi IdeKartika AnggakusumaNo ratings yet
- Carbetocin For The Prevention of Postpartum Hemorrhage: D. Cordovani, J. C. A. Carvalho, M. Boucher and D. FarineDocument8 pagesCarbetocin For The Prevention of Postpartum Hemorrhage: D. Cordovani, J. C. A. Carvalho, M. Boucher and D. FarineKartika AnggakusumaNo ratings yet
- Osteoporosis: Pathophysiology and Clinical ManagementDocument628 pagesOsteoporosis: Pathophysiology and Clinical ManagementKartika AnggakusumaNo ratings yet
- Obstetrics 2Document6 pagesObstetrics 2Kartika AnggakusumaNo ratings yet
- PCOS InsulineDocument14 pagesPCOS Insulinet3klaNo ratings yet
- WHO Grow Chart TB+U Girl 5-19Document1 pageWHO Grow Chart TB+U Girl 5-19Kartika AnggakusumaNo ratings yet
- Posyandu LansiaDocument9 pagesPosyandu LansiaKartika AnggakusumaNo ratings yet
- AbstractDocument18 pagesAbstractKartika AnggakusumaNo ratings yet
- Unit 4 Qk Qktd Bài TậpDocument4 pagesUnit 4 Qk Qktd Bài TậpNguyễn Hoàng Thanh NgânNo ratings yet
- Finish WRDocument2 pagesFinish WRTejinder KumarNo ratings yet
- 82-01.54.455696-1.4 C3, C6, C6 HD Video Colposcope Service Manual-ESDocument88 pages82-01.54.455696-1.4 C3, C6, C6 HD Video Colposcope Service Manual-ESВалентина Кудаева100% (1)
- Run To Failure / Breakdown Maintenance. - Planned / Calendar Based Preventive' Maintenance (PM) - Predictive Maintenance (PDM)Document30 pagesRun To Failure / Breakdown Maintenance. - Planned / Calendar Based Preventive' Maintenance (PM) - Predictive Maintenance (PDM)Chetan PatilNo ratings yet
- Class-10 Termi QPDocument5 pagesClass-10 Termi QPvishal kumarNo ratings yet
- PsychologicaldisorderprojectDocument18 pagesPsychologicaldisorderprojectapi-273867984No ratings yet
- User Manual: 4Kw/6Kw Twin Solar Inverter / ChargerDocument64 pagesUser Manual: 4Kw/6Kw Twin Solar Inverter / ChargerCristobal GutierrezNo ratings yet
- Service Manual: TransformerDocument18 pagesService Manual: TransformerPierre EyebeNo ratings yet
- PROBLEM: An Undisturbed: Properties of Soil Related ProblemsDocument2 pagesPROBLEM: An Undisturbed: Properties of Soil Related ProblemsAldrin LampareroNo ratings yet
- 5minuteflowcompanionguide 2 PDFDocument29 pages5minuteflowcompanionguide 2 PDFNachoVillaverdeNo ratings yet
- Echoupal S PresentationDocument24 pagesEchoupal S PresentationPrabhat KumarNo ratings yet
- Housekeeping Maid's Cart Is A Trolley (Also Referred As A Housekeeper'sDocument4 pagesHousekeeping Maid's Cart Is A Trolley (Also Referred As A Housekeeper'sAsher LeitonNo ratings yet
- GE 24inch Front Load Washer: ModelsDocument99 pagesGE 24inch Front Load Washer: Modelsdan themanNo ratings yet
- Resume 5Document1 pageResume 5api-518171117No ratings yet
- PFH 120 V0.0 Portside and Starboard SideDocument93 pagesPFH 120 V0.0 Portside and Starboard SideDouglas David SilvaNo ratings yet
- EFT Religija A)Document3 pagesEFT Religija A)emofreeNo ratings yet
- RA9165 - Comprehensive Dangerous Drugs Act of 2002Document24 pagesRA9165 - Comprehensive Dangerous Drugs Act of 2002Mikhael Glen LatazaNo ratings yet
- Drainage Condition in Water Logged Areas of Central Part in Chittagong City CorporationDocument6 pagesDrainage Condition in Water Logged Areas of Central Part in Chittagong City CorporationinventionjournalsNo ratings yet
- 34 - G R - No - 213486-DigestDocument2 pages34 - G R - No - 213486-DigestNaomi InotNo ratings yet
- Motor Es CatDocument42 pagesMotor Es CatfelixezamoraNo ratings yet
- UNIT - 2 Human Resource PlanningDocument19 pagesUNIT - 2 Human Resource PlanningEshaan ChadhaNo ratings yet
- CaMaNaVaTon 201Document12 pagesCaMaNaVaTon 201guaporicNo ratings yet
- Research Paper On Neonatal NursingDocument7 pagesResearch Paper On Neonatal Nursinggvxphmm8100% (1)
- BeneficenceDocument4 pagesBeneficenceArnulfo ArmamentoNo ratings yet
- 20-Chapter 23 IndicatorsDocument26 pages20-Chapter 23 IndicatorsAliyah SajaNo ratings yet
- Mind Mapping Form 1 OPSDocument18 pagesMind Mapping Form 1 OPShoneym69457667% (3)
- 3.2 NSS Application Form For NSS VolunteerDocument1 page3.2 NSS Application Form For NSS VolunteerAbcd EfgNo ratings yet
- Coney CovenantDocument27 pagesConey CovenantEnokmanNo ratings yet