Professional Documents
Culture Documents
Gds137 Slide Hyperthyroidism
Uploaded by
Louie Kem Anthony BabaranCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gds137 Slide Hyperthyroidism
Uploaded by
Louie Kem Anthony BabaranCopyright:
Available Formats
HYPERTHYROIDISM
GRAVES DISEASE
D HAKIMI S AK Dr HAKIMI SpAK
Dr MELDA DELIANA SpAK
Dr SISKA MAYASARI LUBIS SpA Dr SISKA MAYASARI LUBIS SpA
PHYSIOLOGY PHYSIOLOGY
Background g
Hyperthyroidism : overactivity of the
thyroid gland leading to excessive
synthesis of thyroid hormones and synthesis of thyroid hormones and
accelerated metabolism in the peripheral
tissues
Thyrotoxicosis : the clinical effects of an
unbound thyroid hormone, whether or
t th th id l d i th i not the thyroid gland is the primary
source
Causes of thyrotoxicosis in childhood y
Hyperthyroidism :
Diffuse toxic goiter (Graves' disease)
Nodular toxic goiter (Plummer disease)
TSH-induced hyperthyroidism:
TSH producing pituitary tumor
S l ti it it i t t th id h Selective pituitary resistance to thyroid hormone
Thyrotoxicosis without hyperthyroidism:
Chronic lymphocytic thyroiditis (CLT) Chronic lymphocytic thyroiditis (CLT)
Subacute thyroiditis
Thyroid hormone ingestion
Pathogenesis g
Genetic clonal lack of suppressor T cells T helper cells
multiply B cells produce TSH receptor antibodies:
TSH t tib di bi d t TSH t (Th id TSH receptor antibodies bind to TSH receptors (Thyroid
gland) T3 and T4 (Clinical presentation of hyperthyroidism)
(Pituitary gland) TSH
? TSH receptor antibodies bind to TSH receptors in retro-
orbital connective tissue T cells produce inflammatory
cytokines Glycosaminoglycans / Eye muscle antibodies?
Swelling in muscle and connective tissues behind eyes Swelling in muscle and connective tissues behind eyes
Ophthalmopathy
Frequency q y
In the US : because Graves' disease accounts for more than
95% of childhood cases of hyperthyroidism, the frequency of
Graves' disease approximates the frequency of all cases of
hyperthyroidism hyperthyroidism
Prevalence : 0,02% in childhood, accounting for fewer than 5%
of the total cases of Graves' disease
Associated with MHC locus (HLA-B8, HLA-DR-3, and possibly
HLA-DQA1*0501) and polymorphisms of cytotoxic lymphocyte
antigen (CTLA)-4 an immunoregulatory molecule that is antigen (CTLA) 4, an immunoregulatory molecule that is
expressed on the surface of activated lymphocytes and inhibits
T-lymphocyte activation
Frequency q y
Associations between Graves' disease and other
autoimmune diseases are well described and
include associations with DM Addisons disease include associations with DM, Addisons disease,
vitiligo, SLE, RA, myasthenia gravis, periodic
paralysis, ITP, and pernicious anemia
There is an increased risk of Graves' disease in
hild ith D d (t i 21) d children with Down syndrome (trisomy 21) and
DiGeorge syndrome (22q11 deletion)
Mortality / Morbidity y y
Excellent prognosis
Neonatal Graves' disease is self-limited, the prognosis is considerably
worse than that in older children The patients are prone to worse than that in older children. The patients are prone to
prematurity, airway obstruction and heart failure. The mortality rate :
as high as 16%
Hypercalcemia is occasionally seen in patients with hyperthyroidism Hypercalcemia is occasionally seen in patients with hyperthyroidism
Female to male ratio = 6 to 8 : 1
Prepubertal children tend to have more severe disease, require longer
medical therapy and achieve a lower rate of remission compared with
pubertal children. This appears to be particularly true in children who
present at < 5 years of age
Age g
Incidence increases throughout childhood,
with a peak incidence in children aged 10 -
15 years
Predisposing factors p g
Genetic susceptibility (including HLA alleles)
Stress
Smoking (especially associated with ophthalmopathy)
Female sex (sex steroid) Female sex (sex steroid)
Postpartum period
Iodine (including amiodarone)
Lithium
Rare factors : Interferon- therapy Rare factors : Interferon therapy
Highly active antiretroviral therapy
(HAART) for HIV infection
Campath 1-H monoclonal antibody (for multiple sclerosis)
Clinical features
*Symptoms* Symptoms
Hyperthyroidism :
Heat intolerance, sweating, palpitations, pruritus,
dyspnea on exertion (exacerbation of asthma) dyspnea on exertion (exacerbation of asthma),
weight loss (with hyperphagia), weight gain (rarely),
hyperdefecation, tremulousness and tremor,
weakness fatigue urinary frequency nocturia weakness, fatigue, urinary frequency, nocturia,
thirst, anxiety, emotional lability, insomnia,
restlessness, inability to concentrate,
oligomenorrhea/amenorrhea errectile oligomenorrhea/amenorrhea, errectile
dysfunction/gynecomastia, dyspepsia, nausea,
vomiting (rare)
Clinical features
*Symptoms* *Symptoms*
Ophthalmopathy :
Eye irritation, dryness, excessive tearing,
visual blurring, diplopia, retro-orbital
discomfort, pain on eye movement, visual
loss
Clinical features
*Signs* g
Hyperthyroidism :
Warm, smooth, moist skin, onycholisis
(loosening of the nail bed, Plummers nails),
palmar erythema, thinning of the hair, stare,
lid retraction (and lag) bright shiny eyes lid retraction (and lag), bright, shiny eyes,
tachycardia, atrial fibrilation, widened pulse
pressure, hyperdynamic circulation, tremor
(fi ) h ti fl i l (fingers), hyperactive reflexes, proximal
myopathy
Clinical features
*Signs* *Signs*
O hth l th Ophthalmopathy :
Periorbital edema, conjunctival erythema,
chemosis (conjunctival edema) proptosis chemosis (conjunctival edema), proptosis,
ophthalmoplegia, loss of colour vision (optic
neuropathy) papilledema (optic neuropathy) neuropathy), papilledema (optic neuropathy)
Laboratory evaluation
Patients with Graves' disease have elevated levels of T4 T3 and Patients with Graves disease have elevated levels of T4, T3, and
T3RU and low or undetectable levels of TSH
If the diagnosis of Graves disease is unclear, TSH receptor Abs
should be measured should be measured
Tg and / or TPO Abs are often present but are less sensitive and
specific than TSH receptor Abs in the diagnosis of Graves disease in
childhood childhood
Radioactive iodine uptake and scan are necessary to confirm the
diagnosis of Graves disease only in atypical cases (for example, if
meas rement of TSH receptor Abs is negati e and if the th roto ic measurement of TSH receptor Abs is negative and if the thyrotoxic
phase of either CLT or subacute thyroiditis or functioning thyroid
nodule is suspected). In Graves disease, the uptake is elevated and
diffuse
Laboratory evaluation y
Obtaining a CBC before the initiation of
antithyroid medications may be valuable for
separating patients with underlying
Leukopenia or thrombocytopenia from
ti t h d l d t i it patients who develop drug toxicity
Therapy py
The choice of which of the three therapeutic options
(medical th/, radioactive iodine, or surgery) to use
should be individualized and discussed with the
patient and his/her family
Medical therapy with one of the thiouracil derivates py
(PTU or MMI) is the initial choice of most
pediatricians, although radioiodine is gaining
increasing acceptance, particularly in non-compliant
d l t i hild h t ll t d d adolescents, in children who are mentally retarded,
and in those about to leave home
Therapy py
PTU, MMI, and carbimazole (converted to MMI)
exert their antithyroid effect by inhibiting the
organification of iodine and the coupling of organification of iodine and the coupling of
iodotyrosine residues on the Tg molecule to
generate T3 and T4
PTU but not MMI, inhibits the conversion of T4 to the
ti i T3 t ti l d t if th more active isomer T3, a potential advantage if the
thyrotoxicosis is severe
Therapy py
The usual initial dosage of MMI is 0.5 mg/kg/day
given once or twice daily and that of PTU is 5
mg/kg/day given thrice daily Carbimazole is best mg/kg/day given thrice daily. Carbimazole is best
given in a dose of 10-20 mg twice or thrice daily
depending on the concentration of free T4
In severe cases, a beta-adrenergic blocker
(propranolol, 0.5-2.0 mg/kg/day given every 8 h) can
b dd d t t l th CV ti it til be added to control the CV overactivity until a
euthyroid state is obtained
Therapy py
The serum concentrations of T4 and T3
normalize in 3-6 weeks, but TSH
t ti t t t l til concentration may not return to normal until
several months later
Approximately 50% of children will go into
long-term remission within 4 years, with g y
continuing remission rate of 25% every 2
years for up to 6 years of treatment
Therapy py
Lower initial degree of hyperthyroxinemia
(T4 < 20 ug/dL or 257.4 nmol/L, T3/T4 ratio
< 20), BMI, and older age have been
associated with an increased likelihood of
t i i permanent remission
P i t f TSH t Ab i di t Persistance of TSH receptor Abs indicates a
high likelihood of relaps
Therapy py
Many authors also recommend checking the
white blood cell count and liver function tests
before therapy because Graves disease
itself can be associated with abnormalities in
th t these parameters
Therapy py
Radioactive iodine therapy should be used
with caution in children < 10 years of age
and particularly in those 5 years of age or
less because of the increased susceptibility
f th th id l d i th t th of the thyroid gland in the young to the
proliferative effects of ionizing radiation
Therapy Therapy
Although a dose of 50-200 uCi of 131 I /
ti t d f th id ti h b d estimated gram of thyroid tissue has been used,
the higher dosage is recommended, particularly
in younger children, in order completely to ablate in younger children, in order completely to ablate
the thyroid gland and thereby reduce the risk of
future neoplasia
The formula used is: (estimated thyroid weight in
grams) x 50 200 uCi 131 I / fractional 131 I 24 h grams) x 50-200 uCi 131 I / fractional 131 I 24-h
uptake)
Therapy py
One usually sees a therapeutic effect within
6 weeks to 3 months
If significant ophthalmopathy is present, RAI g p p y p
therapy should be used with caution, and
treatment with corticosteroid for 6-8 weeks
ft RAI d i i t ti b i after RAI administration may be wise
Therapy Therapy
Surgery is appropriate for patients who have failed
di l t th h h k dl medical management, those who have markedly
enlarged thyroid, those whom refuse RAI, and for
the rare patient with significant eye disease in whom
RAI is contraindicated
The child must be euthyroid before surgery Iodides The child must be euthyroid before surgery. Iodides
(Lugols solution, 5-10 drops twice a day, or
potassium iodide, 2-10 drops daily) are added for 7-
14 days before surgery in order to decrease the 14 days before surgery in order to decrease the
vascularity of the gland
THANK YOU THANK YOU
You might also like
- Hyperthyroidsm: EpidemiologyDocument6 pagesHyperthyroidsm: EpidemiologyEllieNo ratings yet
- Thyroid DX PXLDocument62 pagesThyroid DX PXLabduljebarNo ratings yet
- Thyroid Disorders During PregnancyDocument25 pagesThyroid Disorders During PregnancyA.H.ANo ratings yet
- Therapeutics: Thyroid DisordersDocument24 pagesTherapeutics: Thyroid DisordersSharas FarhadNo ratings yet
- Hyperthyroidism: A Practical Approach To Diagnosis and ManagementDocument70 pagesHyperthyroidism: A Practical Approach To Diagnosis and ManagementMutiara Manuella TambaNo ratings yet
- Drug Management of Thyroid DiseaseDocument22 pagesDrug Management of Thyroid DiseaseHassan.shehri100% (6)
- Hyperthyroidism in PregnancyDocument29 pagesHyperthyroidism in PregnancyLavina JainNo ratings yet
- Grave'S Disease: Farida Ulfa 1510211057Document11 pagesGrave'S Disease: Farida Ulfa 1510211057farida ulfaNo ratings yet
- Abnormal Thyroid Function in PregnancyDocument54 pagesAbnormal Thyroid Function in Pregnancyasri khazaliNo ratings yet
- Graves' Hyperthyroidism in Pregnancy: A Clinical ReviewDocument22 pagesGraves' Hyperthyroidism in Pregnancy: A Clinical ReviewAnisa Dinda NurlianaNo ratings yet
- Endocrine 160110083024Document65 pagesEndocrine 160110083024Ryan CracknellNo ratings yet
- Pemeriksaaan Laboratorium Kelainan Thyroid: DR - Budi Dermawan Lubis, SPPK DR - Siti Hajar, M.Ked, SPPKDocument12 pagesPemeriksaaan Laboratorium Kelainan Thyroid: DR - Budi Dermawan Lubis, SPPK DR - Siti Hajar, M.Ked, SPPKBonitavanyNo ratings yet
- Week 3 Pharmaco Part 2Document34 pagesWeek 3 Pharmaco Part 2Tiko JomidavaNo ratings yet
- Biol 460 Case StudyDocument11 pagesBiol 460 Case Studyapi-353888678No ratings yet
- TPO in PregnancyDocument18 pagesTPO in PregnancyRoxana TudorNo ratings yet
- FunctionTests Brochure PDFDocument2 pagesFunctionTests Brochure PDFArslan SaleemNo ratings yet
- The Role of Maternal Thyroid Status On Pregnancy Outcome For Motherand NewbornDocument36 pagesThe Role of Maternal Thyroid Status On Pregnancy Outcome For Motherand NewbornRahmayantiYuliaNo ratings yet
- CHN1 Health Care Delivery System2Document22 pagesCHN1 Health Care Delivery System2MicaNo ratings yet
- Variations, Errors, and QualityDocument46 pagesVariations, Errors, and QualityJohn Reden RomeroNo ratings yet
- Hypothyroidism in PregnancyDocument14 pagesHypothyroidism in PregnancyShajia ZafarNo ratings yet
- Conference Brochure With Link7Document16 pagesConference Brochure With Link7Shrutik AshiyaniNo ratings yet
- Thyroid Drug and Calcium Homeostasis - PHD332 - 30112017Document62 pagesThyroid Drug and Calcium Homeostasis - PHD332 - 30112017Alisa BoonsukNo ratings yet
- Clinical Practice Guidelines For Hypothyroidism in Adults: AACE and ATA 2012Document63 pagesClinical Practice Guidelines For Hypothyroidism in Adults: AACE and ATA 2012Nur Rakhma AkmaliaNo ratings yet
- Critical Aspect Analytical Test Review: Jakarta 14 December 2017 Speaker: Heru Purnomo, STDocument24 pagesCritical Aspect Analytical Test Review: Jakarta 14 December 2017 Speaker: Heru Purnomo, STMohammad Naufal AliefNo ratings yet
- Guidelines of The American Thyroid Association PREGNANCY PDFDocument47 pagesGuidelines of The American Thyroid Association PREGNANCY PDFIqra AnugerahNo ratings yet
- Thyroid and InfertilityDocument36 pagesThyroid and InfertilitySairindri SahooNo ratings yet
- Hypothyroid in Pregnancy Andi CakraDocument32 pagesHypothyroid in Pregnancy Andi CakraCakraEkkyNo ratings yet
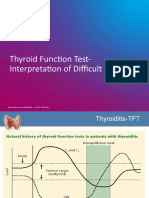
- TFT Interpretation of Difficult CasesDocument51 pagesTFT Interpretation of Difficult CasesAditya GautamNo ratings yet
- Thyroid Emergencies-Dr. AM IyagbaDocument13 pagesThyroid Emergencies-Dr. AM IyagbaDr. Amb. Monday ZaccheausNo ratings yet
- '3'hyperthyroid and HypothyroidDocument42 pages'3'hyperthyroid and Hypothyroidafriskha bulawanNo ratings yet
- Thyroid Emergencies: Abrar AlharbiDocument35 pagesThyroid Emergencies: Abrar AlharbiabrarNo ratings yet
- Surgical Pathology For Dentistry Students - Surgical Pathology of Thyroid and Adrenal GlandsDocument38 pagesSurgical Pathology For Dentistry Students - Surgical Pathology of Thyroid and Adrenal Glandssorin niky mocanu100% (1)
- Laboratory Diagnostics of (Selected) Endocrine DisordersDocument48 pagesLaboratory Diagnostics of (Selected) Endocrine DisordersPaulina PaskeviciuteNo ratings yet
- Parathyroid-Hormone Calcium HomeostasisDocument58 pagesParathyroid-Hormone Calcium HomeostasisSudhakar LakavathNo ratings yet
- Hormon GDSDocument23 pagesHormon GDSBRI KUNo ratings yet
- Thyroid DisordersDocument67 pagesThyroid DisordersMA 09No ratings yet
- HyperthyroidDocument12 pagesHyperthyroidChristine Joy PepitoNo ratings yet
- 1-Good Health Gold Package - PO2257496339-951Document1 page1-Good Health Gold Package - PO2257496339-951Aafaq BhuttoNo ratings yet
- Hypothalamic Pitutary Axis and Thyroid Hormone SynthesisDocument5 pagesHypothalamic Pitutary Axis and Thyroid Hormone Synthesis78 shivangi mauryaNo ratings yet
- Hormones and Related DrugsDocument42 pagesHormones and Related DrugsRamya PrabhuNo ratings yet
- Thyroid PathophysiologyDocument7 pagesThyroid PathophysiologyS RiarNo ratings yet
- Thyroid Panel-1 (T3/T4/TSH) : Investigation Observed Value Unit Biological Reference IntervalDocument2 pagesThyroid Panel-1 (T3/T4/TSH) : Investigation Observed Value Unit Biological Reference IntervalShashikantNo ratings yet
- Thyroid HormonesDocument7 pagesThyroid HormonesAbdullah EssaNo ratings yet
- Thyroiddisease 190216062020Document42 pagesThyroiddisease 190216062020Manikandan Vp100% (1)
- Pathophysiology of Endocrine SystemDocument64 pagesPathophysiology of Endocrine SystemTess MohamedNo ratings yet
- Hypothyroidism in PregnancyDocument29 pagesHypothyroidism in PregnancyhanaddulNo ratings yet
- Lecture 29 30 Thyroid TherapeuticsDocument3 pagesLecture 29 30 Thyroid TherapeuticsAhmed MashalyNo ratings yet
- Thyroid Profile (Total T3, Total T4, TSH), Serum: EcliaDocument3 pagesThyroid Profile (Total T3, Total T4, TSH), Serum: EcliaRoopa gowdaNo ratings yet
- Thyroid Diseases in Pregnancy (Fereidoun Azizi, Fahimeh Ramezani Tehrani)Document252 pagesThyroid Diseases in Pregnancy (Fereidoun Azizi, Fahimeh Ramezani Tehrani)tesis indraparmadityaNo ratings yet
- Thyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneDocument41 pagesThyroid Disease: Presentation By: Pimundu Vicent Audo Ritah Tutor: Dr. Fualal JaneEsther AumaNo ratings yet
- Fertility: Assessment and Treatment For People With Fertility ProblemsDocument4 pagesFertility: Assessment and Treatment For People With Fertility ProblemsPatrick CoghlanNo ratings yet
- Thyroid Hormones and AntiDocument2 pagesThyroid Hormones and AntiNishaHasanNo ratings yet
- HYPOTHYROIDISMDocument30 pagesHYPOTHYROIDISMTopeNo ratings yet
- Dneerajalaxmi 20220611120615333Document1 pageDneerajalaxmi 20220611120615333Donthula SripathiNo ratings yet
- Thyroid Function TestDocument28 pagesThyroid Function TestDhinesh Muthusamy100% (1)
- Lab Report NewDocument2 pagesLab Report Newnsdh5v5v5sNo ratings yet
- Thyrotoxicosis: Presenter: Emiacu Kenneth Facilitator: Dr. Freddie KibengoDocument35 pagesThyrotoxicosis: Presenter: Emiacu Kenneth Facilitator: Dr. Freddie KibengoNinaNo ratings yet
- Presentation SlideDocument63 pagesPresentation SlideJENNIFER ENEKWECHINo ratings yet
- Thyroid Disorders: A Practical ApproachDocument26 pagesThyroid Disorders: A Practical ApproachSadashivayya SoppimathNo ratings yet
- Hyperthyroid Is Med ItDocument31 pagesHyperthyroid Is Med ItJuliana Sanjaya VocNo ratings yet
- Pork Binagoongan RecipeDocument1 pagePork Binagoongan RecipeLouie Kem Anthony BabaranNo ratings yet
- BEC-1A June 19, 2016Document134 pagesBEC-1A June 19, 2016Louie Kem Anthony BabaranNo ratings yet
- The Moral Issue of Paternalism and Truth TellingDocument4 pagesThe Moral Issue of Paternalism and Truth TellingLouie Kem Anthony Babaran0% (2)
- Fundamentals in NursingDocument2 pagesFundamentals in NursingLouie Kem Anthony BabaranNo ratings yet
- Downloaded From Perfect Notes and Guitar Tabs SearcherDocument30 pagesDownloaded From Perfect Notes and Guitar Tabs SearcherLouie Kem Anthony BabaranNo ratings yet
- Kahit Maputi Na Ang Buhok KoDocument13 pagesKahit Maputi Na Ang Buhok KoLouie Kem Anthony Babaran100% (1)
- Pie Details Fact or FictionDocument2 pagesPie Details Fact or FictionLouie Kem Anthony BabaranNo ratings yet
- Borrelia SPP Are Gram Negative Helical Bacteria: Rickketsia Tsutsugamushi Is The CausativeDocument1 pageBorrelia SPP Are Gram Negative Helical Bacteria: Rickketsia Tsutsugamushi Is The CausativeLouie Kem Anthony BabaranNo ratings yet
- Pathophysiology of Rheumatic Heart DiseaseDocument3 pagesPathophysiology of Rheumatic Heart DiseaseLouie Kem Anthony Babaran50% (8)
- I Wont Give UpDocument9 pagesI Wont Give UpRose AnnNo ratings yet
- AtherosclerosisDocument11 pagesAtherosclerosisLouie Kem Anthony BabaranNo ratings yet
- Or InstrumentDocument1 pageOr InstrumentLouie Kem Anthony BabaranNo ratings yet
- Pathophysiology PP FinalDocument2 pagesPathophysiology PP FinalLouie Kem Anthony Babaran0% (1)
- Perioperative NursingDocument9 pagesPerioperative NursingLouie Kem Anthony BabaranNo ratings yet
- Mental Health and Mental DisordersDocument24 pagesMental Health and Mental DisordersLouie Kem Anthony BabaranNo ratings yet
- On Pies and PastriesDocument44 pagesOn Pies and PastriesLouie Kem Anthony Babaran100% (2)
- Jamica L. Ramirez Bsn-4 Set2Document44 pagesJamica L. Ramirez Bsn-4 Set2Louie Kem Anthony BabaranNo ratings yet
- Cake Decorating RubricDocument1 pageCake Decorating RubricLouie Kem Anthony BabaranNo ratings yet
- Who Am IDocument30 pagesWho Am ILouie Kem Anthony BabaranNo ratings yet
- Sites of An Ectopic Pregnancy AreDocument11 pagesSites of An Ectopic Pregnancy AreLouie Kem Anthony BabaranNo ratings yet
- Single-Crust Pie Demo FormDocument2 pagesSingle-Crust Pie Demo FormLouie Kem Anthony BabaranNo ratings yet
- Case Presentation On CholelithiasisDocument24 pagesCase Presentation On CholelithiasisLouie Kem Anthony Babaran100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationLouie Kem Anthony BabaranNo ratings yet
- Types of Nonverbal CommunicationDocument11 pagesTypes of Nonverbal CommunicationPrince Charlie F. AquinoNo ratings yet
- Pride 18-19 FinalDocument3 pagesPride 18-19 FinalSushant PatilNo ratings yet
- Generic Name: Phytonadione Brand Name:: Mechanism of ActionDocument3 pagesGeneric Name: Phytonadione Brand Name:: Mechanism of ActionJay VillasotoNo ratings yet
- Military Chaplain Review Medical EthicsDocument196 pagesMilitary Chaplain Review Medical EthicsToaction100% (3)
- GCQRI Lit ReviewDocument18 pagesGCQRI Lit ReviewgcqriNo ratings yet
- Effective MicroorganismsDocument8 pagesEffective MicroorganismswawahalimNo ratings yet
- Imperforate Anus PDFDocument3 pagesImperforate Anus PDFNajwaNo ratings yet
- Ananya Basu Internal Medicine Clinical CaseDocument4 pagesAnanya Basu Internal Medicine Clinical Caseavnikasharma4889No ratings yet
- Emkarate Rl220h Msds v1.5Document11 pagesEmkarate Rl220h Msds v1.5luanacompany954No ratings yet
- Spaces On The Spectrum How Autism Movements Resist Experts and Create Knowledge Tan All ChapterDocument67 pagesSpaces On The Spectrum How Autism Movements Resist Experts and Create Knowledge Tan All Chaptercorrie.thompson187100% (2)
- Maria Umar - Entrepreneurship Assignment 1Document3 pagesMaria Umar - Entrepreneurship Assignment 1Faizan AhmedNo ratings yet
- F2 IS Exam 1 (10-11)Document7 pagesF2 IS Exam 1 (10-11)羅天佑No ratings yet
- 1158 PDFDocument7 pages1158 PDFankitaNo ratings yet
- How To Do Logic Checks During Plant Pre-CommissioningDocument2 pagesHow To Do Logic Checks During Plant Pre-CommissioningVraja KisoriNo ratings yet
- Nikita Final Paper 1Document4 pagesNikita Final Paper 1Nikita BhagadkarNo ratings yet
- Nike CSR !!!!!!!!!!!!!!!!!!!!!!!!!!Document5 pagesNike CSR !!!!!!!!!!!!!!!!!!!!!!!!!!charlotteNo ratings yet
- Oligo Analyzer SEC PRIMER 2Document1 pageOligo Analyzer SEC PRIMER 2divillamarinNo ratings yet
- Todd Harris JBAM.2009Document19 pagesTodd Harris JBAM.2009Kiran KarkiNo ratings yet
- EAS 69 2006 Pasteurized Milk SpecificationDocument8 pagesEAS 69 2006 Pasteurized Milk SpecificationFelix MwandukaNo ratings yet
- Levall 28: Product Data SheetDocument2 pagesLevall 28: Product Data SheetEfereonNo ratings yet
- Best Ref QuestionnaireDocument18 pagesBest Ref QuestionnaireMarvin M PulaoNo ratings yet
- Heart MattersDocument39 pagesHeart MattersGerry OshNo ratings yet
- ICS501 RevQDocument9 pagesICS501 RevQreteversiliaNo ratings yet
- Cyclone and Bangladesh A Historical and Environmental Overview From 1582 To 2020Document21 pagesCyclone and Bangladesh A Historical and Environmental Overview From 1582 To 2020Ibnath Nabiha/MF/BRACNo ratings yet
- E. Development of Nanocomposite Based Antimicrobial Cotton FabricsDocument11 pagesE. Development of Nanocomposite Based Antimicrobial Cotton FabricsAbreham BekeleNo ratings yet
- Concepts of Community CHN2 090120Document62 pagesConcepts of Community CHN2 090120Pucha MorinNo ratings yet
- WaterproofingDocument5 pagesWaterproofingAkhilesh KumarNo ratings yet
- ABB VFD CatalogesDocument25 pagesABB VFD CatalogesadehriyaNo ratings yet
- Audit NDT BasicsDocument41 pagesAudit NDT BasicsAnonymous B7pghh100% (3)
- Ảnh hưởng của hệ thống sưởi Ohmic đến sự phân hủy của các thành phần hoạt tính sinh học trong thực phẩm 2020 PDFDocument18 pagesẢnh hưởng của hệ thống sưởi Ohmic đến sự phân hủy của các thành phần hoạt tính sinh học trong thực phẩm 2020 PDFĐoanNo ratings yet