Professional Documents
Culture Documents
Obstructive Sleep Apnea: Prevalence
Obstructive Sleep Apnea: Prevalence
Uploaded by
Yess Filorio0 ratings0% found this document useful (0 votes)
17 views4 pagesOriginal Title
9ºsleepapnea.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views4 pagesObstructive Sleep Apnea: Prevalence
Obstructive Sleep Apnea: Prevalence
Uploaded by
Yess FilorioCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder that involves a
decrease or complete halt in airflow despite an ongoing effort to breathe. It occurs when
the muscles relax during sleep, causing soft tissue in the back of the throat to collapse and
block the upper airway. This leads to partial reductions (hypopneas) and complete pauses
(apneas) in breathing that last at least 10 seconds during sleep. Most pauses last between
10 and 30 seconds, but some may persist for one minute or longer. This can lead to
abrupt reductions in blood oxygen saturation, with oxygen levels falling as much as 40
percent or more in severe cases.
The brain responds to the lack of oxygen by alerting the body, causing a brief arousal
from sleep that restores normal breathing. This pattern can occur hundreds of times in
one night. The result is a fragmented quality of sleep that often produces an excessive
level of daytime sleepiness.
Most people with OSA snore loudly and frequently, with periods of silence when airflow
is reduced or blocked. They then make choking, snorting or gasping sounds when their
airway reopens.
A common measurement of sleep apnea is the apnea-hypopnea index (AHI). This is an
average that represents the combined number of apneas and hypopneas that occur per
hour of sleep.
Prevalence
OSA can occur in any ager group, but prevalence increases between middle and
older age.
OSA with resulting daytime sleepiness occurs in at least four percent of men and
two percent of women
About 24 percent of men and nine percent of women have the breathing
symptoms of OSA with or without daytime sleepiness.
About 80 percent to 90 percent of adults with OSA remain undiagnosed.
OSA occurs in about two percent of children and is most common at preschool
ages.
Types
Mild OSA: AHI of 5-15
Involuntary sleepiness during activities that require little attention, such as
watching TV or reading
Moderate OSA: AHI of 15-30
Involuntary sleepiness during activities that require some attention, such as
meetings or presentations
Severe OSA: AHI of more than 30
Involuntary sleepiness during activities that require more active attention, such as
talking or driving
Risk groups
People who are overweight (Body Mass Index of 25 to 29.9) and obese (Body
Mass Index of 30 and above)
Men and women with large neck sizes: 17 inches or more for men, 16 inches or
more for women
Middle-aged and older men, and post-menopausal women
Ethnic minorities
People with abnormalities of the bony and soft tissue structure of the head and
neck
Adults and children with Down Syndrome
Children with large tonsils and adenoids
Anyone who has a family member with OSA
People with endocrine disorders such as Acromegaly and Hypothyroidism
Smokers
Those suffering from nocturnal nasal congestion due to abnormal morphology,
rhinitis or both.
Effects
Fluctuating oxygen levels
Increased heart rate
Chronic elevation in daytime blood pressure
Increased risk of stroke
Higher rate of death due to heart disease
Impaired glucose tolerance and insulin resistance
Impaired concentration
Mood changes
Increased risk of being involved in a deadly motor vehicle accident
Disturbed sleep of the bed partner
Treatments
Sleep apnea must first be diagnosed at a sleep center or lab during an overnight sleep study,
or polysomnogram. The sleep study charts vital signs such as brain waves, heart beat and
breathing.
Continuous positive airway pressure (CPAP):
CPAP is the standard treatment option for moderate to severe cases of OSA and a
good option for mild sleep apnea. First introduced for the treatment of sleep apnea in
1981, CPAP provides a steady stream of pressurized air to patients through a mask
that they wear during sleep. This airflow keeps the airway open, preventing pauses in
breathing and restoring normal oxygen levels. Newer CPAP models are small, light
and virtually silent. Patients can choose from numerous mask sizes and styles to
achieve a good fit. Heated humidifiers that connect to CPAP units contribute to
patient comfort.
Oral appliances:
An oral appliance is an effective treatment option for people with mild to moderate
OSA who either prefer it to CPAP or are unable to successfully comply with CPAP
therapy. Oral appliances look much like sports mouth guards, and they help maintain
an open and unobstructed airway by repositioning or stabilizing the lower jaw,
tongue, soft palate or uvula. Some are designed specifically for snoring, and others
are intended to treat both snoring and sleep apnea. They should always be fitted by
dentists who are trained in sleep medicine.
Surgery: Surgery is a treatment option for OSA when noninvasive treatments such
as CPAP or oral appliances have been unsuccessful. It is most effective when there is
an obvious anatomic deformity that can be corrected to alleviate the breathing
problem. Otherwise, surgical options most often address the problem by reducing or
removing tissue from the soft palate, uvula, tonsils, adenoids or tongue. More
complex surgery may be performed to adjust craniofacial bone structures. Surgical
options may require multiple operations, and positive results may not be permanent.
One of the most common surgical methods is uvulopalatopharyngoplasty (UPPP),
which trims the size of the soft palate and may involve the removal of the tonsils and
uvula. Adenotonsillectomy, the surgical removal of the tonsils and adenoids, is the
most common treatment option for children with OSA. Other children with sleep
apnea may benefit from CPAP.
Behavioral changes:
Weight loss benefits many people with sleep apnea, and changing from back-
sleeping to side-sleeping may help those with mild cases of OSA.
Over-the-counter remedies:
Although some external nasal dilator strips, internal nasal dilators, and lubricant
sprays may reduce snoring, there is no evidence that they help treat OSA. They may
even mask the problem by muting the loud snoring that is a warning sign for sleep
apnea.
Position Therapy:
A treatment used for patients suffering from mild OSA. Patients are advised to stay
off of the back while sleeping and raise the head of the bed to reduce symptoms.
2510 North Frontage Road
Darien, IL 60561
(630) 737-9700
www.aasmnet.org AASM 2008
You might also like
- Baptism EventDocument37 pagesBaptism Eventsharmaine ella guittap68% (19)
- Sleep ApneaDocument23 pagesSleep Apneahams100% (1)
- Acupuncture Treatment For Sleep ApneaDocument11 pagesAcupuncture Treatment For Sleep Apneataoacu2000100% (1)
- TMJ Ankylosis Case PresentationDocument60 pagesTMJ Ankylosis Case PresentationbasharakmNo ratings yet
- Sleep Apnea JournalDocument4 pagesSleep Apnea JournalShamini ShanmugalingamNo ratings yet
- Obstructive Sleep Apnoea Sept 2014Document4 pagesObstructive Sleep Apnoea Sept 2014Desak PratiwiNo ratings yet
- Information Supplement: Obstructive Sleep ApnoeaDocument4 pagesInformation Supplement: Obstructive Sleep ApnoeaNgaire TaylorNo ratings yet
- Sleep Medicine: Devi Farida UtamiDocument105 pagesSleep Medicine: Devi Farida UtamimufiNo ratings yet
- ResearchDocument3 pagesResearchapi-380517264No ratings yet
- Patient Information Brochure: What Is Obstructive Sleep Apnea?Document2 pagesPatient Information Brochure: What Is Obstructive Sleep Apnea?Muhammad SyammNo ratings yet
- Name: Ericka Vanessa MoránDocument6 pagesName: Ericka Vanessa MoránLitopez YepezNo ratings yet
- Sleep Disorders (Diasomnia) : Diasomnia - Difficulties Falling Asleep or WakingDocument11 pagesSleep Disorders (Diasomnia) : Diasomnia - Difficulties Falling Asleep or Wakingfunny-arianNo ratings yet
- The Facts On Sleep Apnea SecretsDocument63 pagesThe Facts On Sleep Apnea SecretsClariceikoNo ratings yet
- Sleep Apnoea - Prof - DR K.K.PDocument44 pagesSleep Apnoea - Prof - DR K.K.PjialeongNo ratings yet
- Obstructive Sleep Apnea SyndromeDocument44 pagesObstructive Sleep Apnea SyndromeSantiNo ratings yet
- Sleep Apnea - Could It Be Robbing You of Rest?Document4 pagesSleep Apnea - Could It Be Robbing You of Rest?Saya MenangNo ratings yet
- Sleep ApnoeaDocument2 pagesSleep Apnoeaapi-338840258No ratings yet
- Obstructive Sleep Apnoea SyndromeDocument72 pagesObstructive Sleep Apnoea SyndromeArjun SainiNo ratings yet
- Obstructive Sleep Apnea and Analgesia - SJH PowerpointDocument29 pagesObstructive Sleep Apnea and Analgesia - SJH PowerpointAbd ZouhierNo ratings yet
- Case Study 20Document5 pagesCase Study 20yjones39100% (3)
- Sleep Apnea: Name - Bharvi Yadav Roll No. - 200BSCCP015Document8 pagesSleep Apnea: Name - Bharvi Yadav Roll No. - 200BSCCP015Bharvi YadavNo ratings yet
- Sleep Apnea Syndrome &Document28 pagesSleep Apnea Syndrome &Sumit PuloriaNo ratings yet
- Management of Obstructive Sleep Apnea: A Dental Perspective: Eview RticleDocument9 pagesManagement of Obstructive Sleep Apnea: A Dental Perspective: Eview RticleFourthMolar.comNo ratings yet
- Obstructive Sleep Apnea in AdultsDocument2 pagesObstructive Sleep Apnea in AdultsElaine CristinaNo ratings yet
- Nasal Obstruction and Obstruction During Sleep - Pausanos and GoDocument10 pagesNasal Obstruction and Obstruction During Sleep - Pausanos and GoPowell TabogocNo ratings yet
- Obstructive Sleep ApnoeaDocument69 pagesObstructive Sleep ApnoeaPrasanna Datta100% (1)
- OSCE Sleep ApneaDocument2 pagesOSCE Sleep ApneaNadia AlmahalawiNo ratings yet
- Obstructive Sleep ApneaDocument15 pagesObstructive Sleep ApneaMushee01No ratings yet
- SnoringDocument12 pagesSnoringa3llamNo ratings yet
- Adenoids and TonsilsDocument12 pagesAdenoids and TonsilsUsama FadhulNo ratings yet
- Sleep Disordered Breathing (Part 4) : Obstructive Sleep Apnea in ChildrenDocument5 pagesSleep Disordered Breathing (Part 4) : Obstructive Sleep Apnea in ChildrenSuprit SnNo ratings yet
- Sleep Disordered Breathing/ Obstructive Sleep Apnea: Jhansi Nalamati MDDocument53 pagesSleep Disordered Breathing/ Obstructive Sleep Apnea: Jhansi Nalamati MDRabie MeramNo ratings yet
- Leep Pnea: Reporters: Desdechado, Niellan Ferrer, Jessa Magkilat, Hanzarri Palmes, Kamillah Sabat, ChristianDocument27 pagesLeep Pnea: Reporters: Desdechado, Niellan Ferrer, Jessa Magkilat, Hanzarri Palmes, Kamillah Sabat, ChristianEira LopezNo ratings yet
- Sleep Apnea Term PaperDocument8 pagesSleep Apnea Term Paperf1gisofykyt3100% (1)
- 152 Obstructive Sleep Apnoea and Anaesthesia 1Document6 pages152 Obstructive Sleep Apnoea and Anaesthesia 1Echo WahyudiNo ratings yet
- Cure Sleep ApneaDocument5 pagesCure Sleep ApneaAdelyn Bebz AchiengNo ratings yet
- Sleep Apnea and Sleep-Disordered BreathingDocument64 pagesSleep Apnea and Sleep-Disordered Breathing李丞永No ratings yet
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Obstructive Sleep Apnea - Dr.M.M.varadharaja / Orthodontic Courses by Indian Dental AcademyDocument168 pagesObstructive Sleep Apnea - Dr.M.M.varadharaja / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Apnea Obstructiva Del SueñoDocument22 pagesApnea Obstructiva Del SueñoRaul SotoNo ratings yet
- Obstructive Sleep ApnoeaDocument43 pagesObstructive Sleep Apnoeachunshienwc6833100% (3)
- Obstructive Sleep ApneaDocument80 pagesObstructive Sleep ApneaAamir Yousuf100% (2)
- ANESTHESIA For OTLARYNGOLOGIC SurgeryDocument64 pagesANESTHESIA For OTLARYNGOLOGIC SurgeryKelvin TuazonNo ratings yet
- Obesity and Obstructive Sleep ApnoeaDocument26 pagesObesity and Obstructive Sleep ApnoeaMagdi PienaarNo ratings yet
- LaryngitisDocument9 pagesLaryngitisjonna casumpangNo ratings yet
- Adult and Pediatric Obstructive Sleep ApneaDocument44 pagesAdult and Pediatric Obstructive Sleep ApneaSwastik SatpathyNo ratings yet
- PrintDocument65 pagesPrintLý TưởngNo ratings yet
- Sleep ApneuDocument22 pagesSleep ApneuAnonymous 8Jlc7aTs90No ratings yet
- Nclex (1301) (1) (1315)Document43 pagesNclex (1301) (1) (1315)Elizabeth SharmaNo ratings yet
- 2 Respiratory ObstructionDocument8 pages2 Respiratory ObstructionLulu MushiNo ratings yet
- RPS - BLS (Dr. Bindo)Document38 pagesRPS - BLS (Dr. Bindo)Krmilla KumillNo ratings yet
- Cure Sleep Apnea: Everything About Sleep Apnea And Sleep Apnea TreatmentFrom EverandCure Sleep Apnea: Everything About Sleep Apnea And Sleep Apnea TreatmentRating: 3.5 out of 5 stars3.5/5 (3)
- OSA Obstructive Sleep Apnea Fact SheetDocument4 pagesOSA Obstructive Sleep Apnea Fact SheetChoche Luis Jodon100% (1)
- Sleep Disorders Presented by Group 4Document30 pagesSleep Disorders Presented by Group 4Praise ToluwalaseNo ratings yet
- 18sleep Apnea and Sleep DisordersDocument23 pages18sleep Apnea and Sleep Disordersnikita ester100% (1)
- LaryngospasmDocument3 pagesLaryngospasmbalab2311No ratings yet
- Obstructive Sleep Apnea, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandObstructive Sleep Apnea, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 3 out of 5 stars3/5 (2)
- Obstructive Sleep Apnea: SS Visser Lung Unit Pah and UpDocument23 pagesObstructive Sleep Apnea: SS Visser Lung Unit Pah and UpMuhammad NuruddinNo ratings yet
- Sleep Disorders Treatment GuideDocument16 pagesSleep Disorders Treatment GuideNestor BalboaNo ratings yet
- OSA UpdatesDocument64 pagesOSA UpdatesRosmadi IsmailNo ratings yet
- Treating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of LifeDocument8 pagesTreating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of Life'ArifahAhmadNo ratings yet
- Samsung Scholarship Application 2013Document8 pagesSamsung Scholarship Application 2013Alex CarricoNo ratings yet
- Bukh DV 36 SmeDocument5 pagesBukh DV 36 SmeTullio OpattiNo ratings yet
- NCEPOD / CEPOD National Confidential Enquiry Into Post Operative DeathsDocument23 pagesNCEPOD / CEPOD National Confidential Enquiry Into Post Operative DeathsdrschethanNo ratings yet
- Event Report Insights Into HackathonDocument7 pagesEvent Report Insights Into HackathonSujoy SarkarNo ratings yet
- Knit Free by JojiDocument8 pagesKnit Free by JojipaulaNo ratings yet
- Universal Preschool Is No Golden Ticket: Why Government Should Not Enter The Preschool Business, Cato Policy Analysis No. 333Document31 pagesUniversal Preschool Is No Golden Ticket: Why Government Should Not Enter The Preschool Business, Cato Policy Analysis No. 333Cato InstituteNo ratings yet
- AbductedDocument160 pagesAbductedSoni Mishra TiwariNo ratings yet
- Bridge 3 Deck DesignDocument16 pagesBridge 3 Deck DesignMd MamroseNo ratings yet
- Bab 2Document13 pagesBab 2Teguh Novri YansyahNo ratings yet
- PLC Timers and CountersDocument16 pagesPLC Timers and CountersTristan Jeff BautistaNo ratings yet
- NCM 210 RLE - 10 Herbal Plants Approved by DOHDocument6 pagesNCM 210 RLE - 10 Herbal Plants Approved by DOHLYRIZZA LEA BHEA DESIATANo ratings yet
- Trumpet Auditions Spring 2023Document7 pagesTrumpet Auditions Spring 2023JeffNo ratings yet
- MIT 103 Assignment-1Document9 pagesMIT 103 Assignment-1Rachna BhatnagarNo ratings yet
- No Homework Policy Counter ArgumentDocument2 pagesNo Homework Policy Counter ArgumentRafael Silva Medina100% (1)
- Questioner For The Long Quiz (Grade 8)Document3 pagesQuestioner For The Long Quiz (Grade 8)Novie Mae ReambonanzaNo ratings yet
- BGM User ManualDocument48 pagesBGM User ManualAlgebra92No ratings yet
- Verification and Validation in CFD and Heat Transfer: ANSYS Practice and The New ASME StandardDocument22 pagesVerification and Validation in CFD and Heat Transfer: ANSYS Practice and The New ASME StandardMaxim100% (1)
- Ccna Interview Ques-2Document11 pagesCcna Interview Ques-2Sarath Chandra GupthaNo ratings yet
- Nursing Dissertation SmokingDocument8 pagesNursing Dissertation SmokingCustomPapersOnlineSingapore100% (1)
- 6.2.3.7 Packet Tracer - Configuring Multiarea OSPFv3 Instructions IGDocument3 pages6.2.3.7 Packet Tracer - Configuring Multiarea OSPFv3 Instructions IGana100% (1)
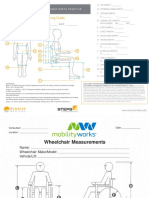
- Attachemnt A - Body and Wheelchair MeasurementDocument2 pagesAttachemnt A - Body and Wheelchair MeasurementNur Adila MokhtarNo ratings yet
- AICTE 360 Degree Feedback Implementation Manual 20210123Document31 pagesAICTE 360 Degree Feedback Implementation Manual 20210123pradeephmkumarNo ratings yet
- Therapist Driven ProtocolsDocument3 pagesTherapist Driven ProtocolsPaoly PalmaNo ratings yet
- Action of Catalase On Hydrogen PeroxideDocument4 pagesAction of Catalase On Hydrogen PeroxideRuchie Ann Pono BaraquilNo ratings yet
- Nanoscience and Nanotechnology in ArgentinaDocument84 pagesNanoscience and Nanotechnology in ArgentinaMaterials Research InstituteNo ratings yet
- MOS Structure Lifting PlanDocument15 pagesMOS Structure Lifting Planmuiqbal.workNo ratings yet
- Grand Case Study V7 Final 030310Document49 pagesGrand Case Study V7 Final 030310Jemimah Ruth Madayag ValenzuelaNo ratings yet
- Big Dams, Development Aid and World BankDocument24 pagesBig Dams, Development Aid and World BankMushtaq GaadiNo ratings yet
- Activity Based CostingDocument26 pagesActivity Based CostingVishal BabuNo ratings yet