Professional Documents
Culture Documents
Word
Uploaded by
Anastasia Lilian SuryajayaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Word
Uploaded by
Anastasia Lilian SuryajayaCopyright:
Available Formats
Medscape
Cryptococcosis is the most common fungal infection of the central nervous system and may present as a space-occupying lesion, meningitis, or meningoencephalitis. In addition, cryptococcosis is the most common fungal disease in HIV -infected persons, and it is the AIDS-defining illness for 60-70% of HIV-infected patients Cryptococcus neoformans spreads hematogenously to the CNS from pulmonary foci, which may be subclinical. No pneumonitis is found in more than 85% of patients with cryptococcal CNS disease. In addition to invading the lung and CNS, cryptococci also invade the skin, bone, and genitourinary tract, but meninges appear to be the preferred site. The reasons are not clear, but several suggestions have been made. For one, cryptococcal capsule antigens may have limited ability to induce an inflammatory response in the cerebrospinal fluid. Furthermore, the alternative pathway of complement is absent in the CSF. By contrast, CSF is a good growth medium for the organism in culture, possibly because of trophic properties of dopamine and other neurotransmitters in the CSF and the absence of cryptococcustoxic proteins.
Cryptococcal disease usually develops only when CD4+ lymphocyte counts fall below 100 cells/mL. At this stage, macrophage function also is impaired.
Immune reconstitution inflammatory syndrome occurs in some patients after treatment with highly active antiretroviral therapy (HAART). This syndrome is a paradoxical deterioration in the clinical status despite satisfactory control of viral replication and improvement of CD4+ counts as a result of an exuberant inflammatory response toward previously diagnosed or latent opportunistic pathogens
The annual incidence of cryptococcosis in the United States is 2-7 cases per 1000 HIV-infected patients, with up to 89% occurring as a CNS manifestation.[1] It is the fourth most common cause of opportunistic infections (after Pneumocystis jiroveci,
cytomegalovirus [CMV], and mycobacteria), and CNS manifestations (66-89%) are by far more common than manifestations in other organs. Its incidence has declined recently because of widespread use of antifungal and antiretroviral agents.[2]
Worldwide, it is estimated that approximately 1 million cases of HIV-associated cryptococcosis occur annually. In developed countries, the widespread use of highly active antiretroviral therapy (HAART) has lowered the incidence of cryptococcosis, but the incidence and mortality of the disease remain extremely high in areas with uncontrolled HIV disease and limited access to HAART or health care.[3]
Of patients with AIDS in the United States, cryptococcal meningitis occurs more commonly in African Americans than in whites.[2] However, a case-controlled study did not find an association between cryptococcal infection and race, suggesting that race may just be a surrogate for the presence of other conditions or exposures.
CNS cryptococcosis is rare in children with AIDS.
Cryptococcus neoformans is a round or oval yeast, 4-6 mm in diameter, surrounded by a 30-mm-thick capsule. Based on the polysaccharide wall serology, use of nutrients, and DNA sequence, it is subclassified into C neoformans neoformans and C neoformans gatii. Patients with AIDS typically are affected by C neoformans neoformans serotype A
CNS cryptococcosis is fatal unless treated. Several studies report acute mortality rates of 6-14%. A minority of patients die within the first 6 weeks after diagnosis, despite treatment. Those who survive usually live for longer than 18 months. In addition, the rate of relapse after treatment is high (30-50%).
Predictors of poor prognosis are controversial, but they have included the following:
REVIEW ARTICLE Year : 2007 | Volume : 55 | Issue : 3 | Page : 241-250 Imaging features of central nervous system fungal infections
Krishan K Jain, Shireesh K Mittal, Sunil Kumar, Rakesh K Gupta Department of Radiology, Sanjay Gandhi Post-Graduate Institute of Medical Sciences, Lucknow - 226 014, India
Date of Acceptance Correspondence Address: Rakesh K Gupta
26-May-2007
MR Section, Department of Radiology, SGPGIMS, Lucknow - 226 014 India
20 1
DOI: 10.4103/0028-3886.35685
PMID: 17921653
Abstract Fungal infections of the central nervous system (CNS) are rare in the general population and are invariably secondary to primary focus elsewhere, usually in the lung or intestine. Except for people with longstanding diabetes, they are most frequently encountered in immunocompromised patients such as those with acquired immunodeficiency syndrome or after organ transplantation. Due to the lack of inflammatory response, neuroradiological findings are often nonspecific and are frequently mistaken for tuberculous meningitis, pyogenic abscess or brain tumor. Intracranial fungal infections are being identified more frequently due to the increased incidence of AIDS patients, better radiological investigations, more sensitive microbiological techniques and better critical care of moribund patients. Although almost any fungus may cause encephalitis, cryptococcal meningoencephalitis is most frequently seen, followed by aspergillosis and candidiasis. The biology, epidemiology and imaging features of the common fungal infections of the CNS will be reviewed. The radiographic appearance alone is often not specific, but the combination of the appropriate clinical setting along with computed tomography or magnetic resonance may help to suggest the correct diagnosis.
Keywords: Acquired immunodeficiency syndrome, brain, central nervous system, computed tomography, diffusion weighted imaging, fungal infection, infection, magnetic resonance (MR), proton MR spectroscopy
How to cite this article: Jain KK, Mittal SK, Kumar S, Gupta RK. Imaging features of central nervous system fungal infections. Neurol India 2007;55:241-50
How to cite this URL: Jain KK, Mittal SK, Kumar S, Gupta RK. Imaging features of central nervous system fungal infections. Neurol India [serial online] 2007 [cited 2013 May 7];55:241-50. Available from: http://www.neurologyindia.com/text.asp?2007/55/3/241/35685
Fungal infections of the central nervous system (CNS) are rare and are invariably secondary to primary focus elsewhere, usually in the lung or intestine. Except for people with longstanding diabetes, these are most frequently encountered in immunocompromised patients such as those with acquired immunodeficiency syndrome (AIDS) or after organ transplantation. [1] Due to the lack of inflammatory response, neuroradiological findings are often nonspecific and are frequently mistaken for tuberculous meningitis, pyogenic abscess or brain tumor. [1],[2] Intracranial fungal infections are being identified more frequently due to the increased incidence of AIDS, better radiological investigations, more sensitive microbiological techniques and better critical care of moribund patients. [2] Although almost any fungus may cause encephalitis, cryptococcal meningoencephalitis is most frequently seen, followed by aspergillosis and candidiasis. [1]
The clinical and imaging features of the common fungal infections of the CNS will be reviewed. The radiographic appearance alone is usually nonspecific, however, when combined with appropriate clinical setting, may help in suggesting the correct diagnosis. [3]
Cranial Infection
Aspergillosis
Aspergillus is saprophytic opportunistic ubiquitous fungi found in soil, plants and grows as a mold on decaying vegetable matter. Aspergillus fumigatus is the most common human pathogen; however A. flavus, A. niger and A. oxyzae are also frequently seen. [2] They have septate hyphae with dichotomous branching and produce spores. Humans are infected by inhaling these spores, with the lungs and paranasal sinuses as the primary site of infection. [4]
CNS aspergillosis is a rare condition with worldwide distribution. [4] Most cases have been reported in adults, although the disease is also seen in children and neonates. [5] Infection reaches the brain directly from the nasal sinuses or is hematogenous from the lungs and gastrointestinal tract. Rarely, the infection may contaminate the operative field during a neurosurgical procedure. [2] In immunocompromised patients, aspergillosis usually occurs as part of a disseminated infection. [4]
The pathology of CNS aspergillosis can be classified into three forms: infarction, granulomas and meningitis. [5] The fungal hyphae block intracerebral blood vessels, resulting in thrombosis and subsequent infarction and hemorrhage. [4],[6] The fungus can then spread beyond the vessel walls and form abscesses in the altered brain tissue. [6] Purulent lesions may be chronic and have a tendency towards fibrosis and granuloma formation. [2] Erosion of vessel wall can also form mycotic aneurysms. Aspergillosis is the most common cause of mycotic aneurysm. [6],[7] Microscopically, the most striking feature is the presence of the vascular invasion with thrombosis. In purulent lesions, pus is seen in the center of the abscesses with abundant polymorphs at the periphery. Granulomas consist of lymphocytes, plasma cells and fungal hyphae. [2]
The clinical diagnosis of cerebral aspergillosis is difficult because of nonspecific symptoms and fever may be absent. [5] There may be clinical features of meningitis and subarachnoid hemorrhage. In patients with paranasal sinus disease orbital extension with proptosis, ocular palsies, visual deterioration and chemosis may occur. Aspergillosis should be considered in cases manifesting with acute onset of focal neurological deficits resulting from suspected vascular or space-occupying lesions, especially in immunocompromized hosts. [8],[9],[10]
The radiological appearance of Aspergillus infection of the CNS is variable and depends upon the immune status of the patients. Using computed tomography (CT) and magnetic resonance (MR), several patterns of cerebral aspergillosis have been reported: edematous lesions, hemorrhagic lesions, solid enhancing lesions referred to as aspergilloma or "tumoral form," [Figure - 1] abscess-like ring-like enhancing lesions [Figure - 2], infarction and mycotic aneurysm. [1] Multiple areas of hypodensity on CT or hyperintensity on T2-weighted images (T2WI) on MR, involving the cortex and/or subcortical white matter consistent with multiple areas of infarction is a common finding in Aspergillus infection. The superimposed hemorrhage may be identified as hyperdensity on CT and hyperintensity on T1weighted images (T1WI) on MR. On MR, lesions may show areas of isointensity or low signal intensity on T2WI, which is attributed to fungal hyphae containing paramagnetic elements like manganese, iron and magnesium, but may also be related to blood breakdown products. Dural enhancement is usually seen in lesions adjacent to infected paranasal sinuses, which represents direct extension of sinonasal disease [Figure - 3]. Recognition of these radiological patterns in patients with cerebral aspergillosis is helpful in establishing an early diagnosis. [1],[11]
Diffusion-weighted imaging (DWI) is valuable in early diagnosis of cerebral aspergillosis as it detects early infarction and can also be beneficial in differentiating these lesions from progressive multi-focal leukoencephalopathy and neoplasm. [12] Proton MR spectroscopy (PMRS) in an isolated case has shown elevation of glutamine-glutamate (2.1 ppm), lactate (1.3 ppm) and amino acids (0.9 ppm) at the central non-enhancing part of the aspergillus abscess which is significantly different from the spectra of cystic or necrotic brain tumors. [13]
Proton MR Spectroscopy in aspergilloma is nonspecific with high choline, low creatine and lactate with no N-acetyl aspartate (NAA) [Figure - 1]. [5]
Interestingly, lesions in perforating artery territories are more common in hematogenously disseminated aspergillosis involving the brain. This affinity for perforating artery is possibly related to the invasion of the walls of the involved larger arteries, subsequently compromising the origins of the perforating arteries. [14]
The CT appearance of aspergillosis sinusitis has been described as hypodense mass lesion with calcification and is separate from the wall of sinuses. In most cases, the adjacent bony structures show areas of erosion or sclerosis. [15] On MR, Aspergillus sinusitis appears as iso to hypointense on T1WI and hypointense (may be mistaken for air in the sinuses) on T2WI. This T2 shortening is due to by presence of iron, magnesium, as well as increased calcium contents. [5],[15]
Cryptococcosis
Cryptococcus neoformans , an encapsulated yeast-like fungus is the most common mycotic agent to affect the CNS. It is a ubiquitous organism found in mammal and bird feces, particularly in pigeon droppings. It causes disease primarily in patients with impaired immunity, particularly in those with AIDS. [16],[17] However, up to 30% of the patients have been reported with no predisposing condition. [18] Men are more commonly infected than women by cryptococcal infection. [5]
The infection is acquired through inhalation and spreads hematogenously to the CNS. The pathogenesis is remarkably similar to that of tuberculous meningitis. [19],[20] The central nervous system is the preferred site for cryptococcal infection, because soluble anticryptococcal factors present in serum are absent in cerebrospinal fluid (CSF) and the polysaccharide capsule of the fungus protects it from host inflammatory response. [16]
CNS infection can be either meningeal or parenchymal. [21] Meningitis is often the primary manifestation and is most pronounced at the base of the brain. Parenchymal involvement is seen as cryptococcomas, dilated Virchow-Robin spaces or enhancing cortical nodules. It is believed that the meningeal infection along the base of the skull may involve the adjacent brain parenchyma, giving rise to cryptococcomas or may extend along the Virchow-Robin spaces. The commonest parenchymal sites are the midbrain and the basal ganglia. The pseudocysts are formed due to dilatation of the Virchow-Robin spaces with mucoid gelatinous material produced by the capsule of the organism. [17],[21] The term cryptococcoma should be used for lesions in which the fungus has invaded the parenchyma, producing chronic granuloma composed of macrophages, lymphocytes and foreign body giant cells. [20] They may also arise within the choroid plexus resulting in obstructive hydrocephalus. [19] Cerebral infarctions, usually located in the basal ganglia, internal capsule and thalamus, may occur in 4% of patients with cryptococcal meningitis in the acute stage and during the treatment. [18]
Most patients with CNS cryptococcosis present with symptoms and signs of subacute meningitis or meningoencephalitis. Clinically, headache is the most common and sometimes the sole symptom. Meningeal features like photophobia and neck stiffness are uncommon. Other manifestations include symptoms and signs related to increased intracranial pressure due to hydrocephalus or related to encephalitis. [5],[20] Meningoencephalitis is associated with high morbidity and mortality, especially among immunocompromised hosts. [19],[20] Immunocompetent patients tend to present with localized, indolent neurological disease, more intense inflammatory responses but better clinical outcome. [22]
Cryptococcal disease may be diagnosed more readily than most other systemic fungal diseases for three reasons. The infection has a unique appearance on histopathology, the yeast can be seen in the CSF and the immunologic test for antigen in CSF and blood is highly sensitive and specific. [5]
The radiographic characteristics of CNS infection are protean and frequently minimal. [23] The spectrum of MR and CT abnormalities ranges from no abnormality to meningeal enhancement, abscesses, intraventricular or intraparenchymal cryptococcomas, gelatinous pseudocysts and/or hydrocephalus. [16],[23]
Hydrocephalus is the most common, although nonspecific finding. Intraparenchymal and intraventricular mass lesions are less common. [23] Pseudocysts are seen as wellcircumscribed, round to oval low-density lesions on CT and have CSF intensity on both T1WI and T2WI, which fail to enhance. [16] Demonstration of clusters of these cysts in the basal ganglia [Figure - 4] and thalami strongly suggest cryptococcal infection. [21]
Miliary lesions and cryptococcomas may present as variable density masses on CT and of low intensity on T1WI and high intensity on T2WI [Figure - 5]. [23] Granulomatous lesions are located preferentially on the ependyma of the choroid plexus and may enhance [Figure - 4]. [16],[23] However, contrast enhancement of cryptococcomas or meninges is uncommon in immunocompromised patients due to the underlying immunosuppression and non-immunogenic nature of the polysaccharide capsule of the cryptococcal organism. [17],[19],[21]
Immunocompetent patients are more likely to present with cryptococcomas. [23] Enhancement of these lesions might occur [Figure - 6] as a result of an immunologic reaction by the host. [21] Immediate and delayed imaging with a double dose of contrast has been reported to reduce the false negative studies by showing meningeal enhancement in immunocompromised patients. [24]
In vivo PMRS shows marked increase in lactate along with decrease in NAA, choline and creatine. [25] Spectroscopy results suggest neuronal injury and gliosis in CNS cryptococcosis with decreased ratio of metabolite to nonsaturated water signal. [26] Ex vivo PMRS has shown high concentration of alpha-trehalose and is considered as diagnostic of C. neoformans . [27]
On DWI, cryptococcoma shows hypointensity in the central cavity [Figure - 5] and mimics a necrotic brain tumor, rather than a pyogenic brain abscess. [28]
Mucormycosis
Mucormycosis is a life-threatening opportunistic fungal infection caused by one of the members of the mucoraceal family. [29] Rhizopus oryzae is the most common cause of infection. [30] The hyphae are broad and non-septated, with right-angle branching and are distinct from Aspergillus . When spores are converted into hyphae, they become invasive, involve blood vessels and disseminate hematogenously or may spread through the paranasal sinuses into the brain and orbits. [31],[32]
Diabetics comprise at least 70% of the reported cases and less than 5% occur in normal hosts. [5] Acidosis rather than hyperglycemia appears to be the important predisposing factor. [5],[30] Infection can also be seen in intravenous drug abusers, in patients of anemia, leukemia, uremia and severe burns and in those receiving corticosteroid or chemotherapy. [33]
The rhinocerebral form is the most common infection. [29],[30] The organism may spread directly through the cribriform plate, via retrograde proliferation along the vessels or via extension into the orbit and then through the optic canal or superior orbital fissure into the cavernous sinus. [5] The common presenting symptoms are headache, fever, sinusitis, facial swelling and unilateral orbital apex syndrome. [31] Neurological deficits may result secondary to intracerebral abscess formation and thrombosis of major intracranial vessels. [29] Prognosis is poor even after aggressive antifungal treatment and surgical debridement. [30]
Isolated CNS mucormycosis, a focal intracerebral infection, is rare and is mostly seen in drug abusers. It presents with acute onset and rapid development of
neurological symptoms. The suspected source of infection is spores in the injected substances. Infarcts and abscesses are found on imaging studies, most commonly in the basal ganglia. [31],[33] A study reported involvement of basal ganglia in 82% of drug abusers while non-drug abusers showed involvement in only 9% of cases. [34]
Findings on CT and MR images include dense opacification of paranasal sinuses with variable mucosal thickening and usually absence of fluid levels in the maxillary, ethmoid, frontal and sphenoid sinuses, in decreasing order of incidence. Sinus contents have variable MR imaging characteristics, from hypointensity to hyperintensity on T2WI, probably secondary to the presence of manganese, iron and calcium. [29],[31] When present, the finding of bony erosion of the sinuses is strongly suggestive of the diagnosis in the appropriate clinical context. It is uncommon to visualize an organized retro-orbital mass. Although CT may sometimes show evidence of infection of the orbital soft tissue, MR is more sensitive. [30]
Intracranial findings include infarcts related to vascular thrombosis, mycotic emboli and frontal lobe abscesses [Figure - 7]. [29] On MR, involvement of brain parenchyma by the fungus can be separated from bland infarction due to vascular involvement. Contrast-enhanced MR may help in distinguishing between these two possibilities. Involvement of cavernous sinuses, internal carotid and basilar artery in the form of abnormal vascular signal and abnormal enhancement has been shown secondary to thrombus formation in these vessels. [5] Immunocompetent patients show different pattern of disease with absence of calcification and a predilection for the ethmoid sinuses. However, contrast enhancement, intraorbital and intracranial extension and high mortality rates are similar among all patients regardless of the status of their immune system. [31]
Siegal et al. reported elevated lactate, depleted NAA and presence of succinate and acetate in mucormycosis, without the commonly seen resonances of valine, leucine and isoleucine observed in bacterial abscess on PMRS. [35]
Diffusion restriction has been reported in a case of fungal cerebritis due to mucormycosis with apparent diffusion coefficient (ADC) values in the range of that reported for pyogenic brain abscess. [36] In a case report of right-sided vision loss secondary to rhinocerebral mucormycosis, DWI demonstrated optic nerve infarction with restricted diffusion when regular MR was normal. Restricted diffusion may be the earliest detectable abnormality in acute ischemic optic neuropathy due to rhinocerebral mucormycosis. [37]
Blastomycosis
Blastomycosis, a thermally dimorphic fungus, is endemic in the southeastern and central United States. It is caused by Blastomyces dermatitidis . [38],[39] It is the yeast form that disseminates hematogenously, causing systemic disease. The fungus has been isolated from soil, which appears to be the reservoir for human infection. [5]
It is primarily a disease of the lung. Infection is usually acquired through inhalation of aerosolized conidia. [38],[40] Chronic pneumonia is the dominant clinical manifestation of blastomycosis, although extrapulmonary disease is also common, usually involving skin and subcutaneous tissue, bones and joints, prostate gland and CNS. [40] Central nervous system infection is the result of either direct extension from the sinus or orbital infection or hematogenous spread. [5] Central nervous system involvement occurs in ~4% of patients with blastomycosis. [41] It usually presents with meningitis, subdural focal leptomeningeal abscess or intraparenchymal abscess. [38]
It is surprising to know that blastomycosis does not have predilection for immunocompromised patients, as do other fungal organisms, such as Candida and cryptococcus. [42] Although it is not an AIDS-defining infection, reports of blastomycosis in individuals infected with the human immunodeficiency virus (HIV) are increasing. [43]
Findings on CT and MR are nonspecific. CT shows the presence of an isodense or hyperdense lesion with surrounding edema, which demonstrates variable enhancement on contrast administration. [5],[42] On MR, most granulomatous lesions are hyperintense on T2WI, however, dural lesions can be isointense or hypointense on both T1WI and T2WI. Contrast-enhanced study shows marked enhancement of granulomatous disease. [42] Dural enhancement may also occur with direct extension from paranasal sinuses. [5] The MR appearance of parenchymal blastomycosis abscess is indistinguishable from other causes of abscess. [5] Isolating the organism is required for the diagnosis of blastomycosis as serologic tests are typically negative and are not useful. [5],[39]
Coccidioidomycosis
Coccidioidomycosis is a systemic infection caused by a dimorphic fungus Coccidiodes immitis. [44] The organism is endemic to semiarid regions in the southwestern United States and northern Mexico. [45] It exists in the mycelial form within the soil and becomes infective when the airborne arthrospores are inhaled. [44] The heavier the inoculation, the more serious the resulting infection, as demonstrated by the increased incidence in endemic areas after severe dust storms or in members of archeologic expeditions who have disturbed the soil. [44],[45]
Approximately, 4-5% of symptomatic patients may develop disseminated disease with associated morbidity and mortality. [46],[47] Disseminated disease is even more common in immunocompromized patients. [5] Central nervous system involvement is usually secondary to hematogenous dissemination from the lungs with meninges as the most common site. [48]
Radiological findings in patients of CNS coccidioidomycosis on imaging are related to: (1) meningitis and ependymitis; (2) hydrocephalus; (3) solitary or multiple granulomas; (4) white matter disease; (5) vasculitis; and (6) spinal arachnoiditis. [44] Meningitis,
a potentially lethal complication of coccidioidomycosis may be associated with cerebritis. [5],[49] Hydrocephalus is seen in 68-93% of patients. [44],[50] Cerebral coccidioidal granulomas, either solitary or multiple, are less common than tuberculomas, but have been reported pathologically. [44] Vasculitis has been observed in up to 40% of cases of meningitis; however, this typically involves the small penetrating branches of the major cerebral vessels, resulting in deep ischemic infarction. [48] Ischemia has been reported in 58% of patients which may be related either to vasospasm or direct invasion of the vessel. [47],[50] Subarachnoid hemorrhage is a rare and fatal complication secondary to rupture of mycotic aneurysm. [51]
MR is superior to CT for detecting neuroimaging abnormalities in patients with coccidioidomycosis. [46] Typically, diffuse and intense leptomeningeal enhancement of basilar, sylvian and interhemispheric cisterns is seen on post-contrast MR studies in coccidioidomycosis meningitis. [47],[50] Leptomeningeal enhancement can also extend to the spinal canal. Occlusion of the anterior spinal artery due to meningeal inflammatory process has also been reported. [5],[50] Communicative or obstructive hydrocephalus develops after the granulomatous process about the fourth ventricle and basal meninges. [44] Deep cerebral infarcts can be seen as areas of hyperintensity on T2WI. Less commonly, focal white matter or deep grey matter enhancing lesions representing granulomas are identified. Uncommonly, focal abscesses have been reported in HIV patients. [52] Patients with documented neuroimaging abnormalities have a higher mortality. [46]
Histoplasmosis
Histoplasmosis, caused by a dimorphic fungus Histoplasma capsulatum , can range from subclinical infection to progressive disseminated disease. [53],[54] Infection is endemic in the upper Mississippi River and Ohio River valleys. [53] H. capsulatum grows as a mold in the soil and causes infection when microconidia or hyphal elements are inhaled and convert into yeasts in the lungs or when organisms in old foci reactivate during immunosuppression. [39] Disseminated disease is uncommon and
occurs primarily when cellular defenses are impaired. [53] Histoplasmosis represents the first manifestation of AIDS in 50-75% of patients. [39]
Clinical findings of progressive disseminated histoplasmosis are usually nonspecific. [53] Clinical syndromes include subacute or chronic meningitis, focal brain or spinal cord lesions, stroke and diffuse encephalitis. [53],[55]
CNS involvement is clinically recognized in 5-10% of cases of progressive disseminated histoplasmosis. However, in autopsy studies, it is reported in up to 25% of cases. [53],[55] Sites of CNS involvement include the basilar meninges, graywhite matter junction in the brain and rarely the spinal cord. [56] Isolated involvement of the thalamus and choroid plexus has also been described. [5],[57] Based on pathological correlation CNS histoplasmosis has been described in three forms: Meningitis, Cerebritis and Vasculitis. [56]
Imaging features of CNS histoplasmosis are nonspecific. CT is abnormal in ~90% of cases, usually showing enhancing mass lesions, cerebral atrophy or hydrocephalus. [53] On MR, the lesions are hyperintense on T2WI and hypointense on T1WI with perilesional edema and ring enhancement. In abscesses, the rim may be hypointense on T2WI due to the presence of paramagnetic free radicals in its wall. Diffuse leptomeningeal enhancement may also be present. [5] Rarely, the disease may present as a histoplasmoma, which appears as an expansile lesion in the thalamic, hypothalamic and chiasmatic regions, with ring enhancement. [58]
Candidiasis
Candida species are ubiquitous yeasts, found on plants and as normal flora of the alimentary tract and mucocutaneous membranes of humans. [59] Human candidiasis is most commonly caused by Candida albicans . The rapid multiplication in tissues, production of proteases, adhesions to extracellular matrix proteins and complement binding receptors are among the important factors contributing to its virulence. [60]
The clinical manifestations of candidiasis are primarily of three types: mucocutaneous, cutaneous and systemic or disseminated. Incidence of disseminated candidiasis is on the rise due to an increase in immunocompromised patients. Other risk factors include admission to intensive care units, total parenteral nutrition, multiple antibiotics, premature infants, corticosteroid use, chemotherapy and following organ transplantation, particularly during acute rejections. [61],[62]
Primary candidiasis of the brain and meninges is rare; however, CNS invasion is reported in 18-52% in disseminated candidiasis. [52],[63] Candida causes focal necrosis around the microcirculation mainly in the middle cerebral artery territory producing micro-abscesses. It can also cause vasculitis, intraparenchymal hemorrhage, aneurysms and thrombosis of small vessels with secondary infarction. [5],[63] Involvement of paranasal sinuses with extension to brain parenchyma with multiple abscess formation has also been reported [Figure - 8]. [5]
CT usually underestimates the extent of the disease. Microabcesses appear iso to hypodense on non-enhanced CT and show multiple punctate enhancing nodules on contrast study. Granuloma may appear as hyperdense nodule on CT with nodular or ring enhancement. On MR, granuloma formation and brain abscess may have hypointense signals on T2WI due to the magnetic susceptibility effect of hemorrhage. Lesions show ring-enhancement on contrast administration. MR also shows features of associated meningitis, vasculitis and infarction. [5],[63]
Common MR features of brain abscess secondary to fungal infection
Fungal abscesses are hypointense on T1WI and hyperintense on T2WI with welldefined rim enhancement on post-contrast images in immunocompetent patients. However, in immunocompromised patients, abscesses appear as patchy or punctate T2 hyperintense lesions with frequently absent enhancement. However, contrast enhanced imaging decreases the number of false negative studies. [1],[64],[65]
Fungal lesions are known to show lipids (1.2-1.3 ppm), lactate (1.3 ppm), alanine (1.5 ppm), acetate (1.9 ppm), succinate (2.4 ppm), choline (3.2 ppm) and unidentified resonance at 3.8 ppm on PMRS. [27],[35],[66] In a recent study conducted in our institution fungal abscesses were differentiated from non-fungal lesions by combining the conventional, DWI and PMRS features. [67] A ring-enhancing, T2heterointense lesion with irregular walls and non-enhancing intra-cavitary projections having low ADC carries a high probability of being a fungal abscess. These projections, directed centrally from the wall, are isointense to hypointense on T1WI and hypointense on T2WI [Figure - 9]. The identification of multiple signals seen between 3.6 and 3.8ppm assigned to trehalose sugars on PMRS may further add to the diagnostic confidence. [67]
Spinal Infections
Fungal infections of the spine are relatively uncommon. They have been reported with Candida , aspergillosis, cryptococcus, coccidioidomycosis and histoplasmosis. Candida and Aspergillus produce disease when they gain access to the vascular system through intravenous lines, during implantation of prosthetic devices or during surgery. For the other fungi, spinal involvement usually is the result of hematogenous or direct spread of organisms from an initial pulmonary source of infection. [68]
The vertebral body, posterior bony vertebral elements, epidural space and perispinal soft tissues may be involved in the infectious process. Occasionally, the intervertebral disc may be relatively spared early in the disease. [69]
Fungal spondylitis secondary to Candida and Aspergillus is characterized by low signal intensity on T1WI and high signal intensity on T2WI with intervening disc involvement [Figure - 10]. The bone marrow in the affected vertebral bodies may show low signal intensity on both T1WI and T2WI due to lack of inflammatory
response in immunocompromised patients. [5],[70] In some cases, hyperintensity of the vertebral disc is absent and rarely, intranuclear cleft may be preserved. [71] Epidural abscess may be seen in Aspergillus infection. There are reports of intradural abscess formation following epidural steroid injection in immunocompetent individuals. [5],[72]
Skeletal coccidioidomycosis is frequently multicentric. The axial skeleton is the most common site. [73] Spinal involvement is seen in approximately 25% of patients with disseminated disease. [74] Spinal lesions are usually well-demarcated but may be illdefined with permeative type of bone destruction. Plain radiographs are effective in the initial evaluation of bones and joints. CT and MR are useful in determining soft tissue involvement and spinal abnormalities. [73] The typical imaging features include disc involvement, heterogeneous marrow signal alteration and extensive extraosseous involvement with lack of bony deformity. [74] Other features include phlegmenous, enhancing non-liquefactive soft tissue abnormalities, cord compression and nerve root impingement. As the disease is multifocal, MR screening of the entire vertebral column often reveals occult areas of involvement. [74] The extensive soft tissue and marrow involvement with lack of bony deformities are the features that help to differentiate coccidiomycosis from other causes of infective spondylitis. [5] As the MR features are nonspecific, biopsy with culture is required to establish the diagnosis. [74]
Spinal cord disease is a rare presentation of cryptococcosis. [75] Bony involvement is seen in 5% of disseminated cryptococcosis. [76] Imaging findings are not specific and simulate spinal tuberculosis with involvement of the vertebral body along with posterior elements and paraspinous and perivertebral soft tissues with relative preservation of the disc. [77],[78] The vertebral body predominantly shows osteolytic lesions with discrete margins, absent surrounding sclerosis and periosteal reaction. [79] Meningoradiculitis and spinal cryptococcal granulomas are rare [Figure - 11]. [75],[77] In a case of spinal cryptococcus infection DWI shows hyperintensity of involved vertebral body, epidural space and posterior elements. [80]
Bone is the one of the frequent sites of disease in patients with blastomycosis, lower thoracic or lumbar vertebrae being most often affected. [81] MR reveals destructive vertebral changes, an epidural mass, psoas abscess and lack of involvement of the disc spaces. Sparing of the disc space is due to spread of infection by way of paravertebral structures and surrounding potential spaces. [82] Blastomycosis can rarely present as an isolated intramedullary lesion. [83]
Treatment of fungal spondylitis is often delayed because of difficulty with the diagnosis that results in poor prognosis. Performing fungal cultures whenever a spinal infection is suspected might hasten the diagnosis
High CSF cryptococcal antigen titer (>1:1024) Minimal CSF pleocytosis Altered mental status at presentation Positive India Ink preparation Hyponatremia Positive cultures from extrameningeal sites
Presentation Disease onset is usually insidious, which may be why the time from symptom onset to diagnosis is, on average, 30 days or more. The delay also may be due to the waxingand-waning course and the nonspecificity of symptoms.
Onset is rarely fulminant. Lung involvement is found in fewer than one third of patients with CNS cryptococcosis. Occasionally, evidence of unsuspected CNS cryptococcosis is detected on cerebrospinal fluid analysis done for other reasons. In almost half of patients, cryptococcosis in the CNS or elsewhere is the AIDSdefining illness.
Signs and symptoms at onset may be nonspecific and include the following:
Headache (73-81%) Fever (62-88%) Malaise (38-76%) Nausea and vomiting (8-42%) Stiff neck (22-44%) Visual disturbances (30%) Altered mental status with somnolence (18-28%) Photophobia (19%) Papilledema (10%) Cranial neuropathies, including nystagmus and amblyopia (6%) Occasionally, patients may experience focal neurologic symptoms or seizures. Focal signs may indicate that the infectious meningeal process has reached superficial layers of the cortex and cerebellum, or they may point to cryptococcomas (ie, cryptococcal abscesses), most commonly in the basal ganglia and cerebellum (see the images below).
Magnetic resonance imaging showing a cryptococcoma in the medulla.
Coronal section of brain showing a cryptococcoma in the basal ganglia. Mental status changes include confusion, psychomotor retardation, irritability, agitation, personality changes, and psychosis. Nuchal rigidity may be absent because of minimal inflammation.
Hydrocephalus must be suspected with new-onset impaired consciousness, motor signs, nausea, vomiting, or visual impairment. This usually occurs late in the course of cryptococcosis.
Bilateral visual loss also can result from arachnoiditis at the level of the optic nerves or cryptococcal invasion of the optic nerve. Occasionally, symptoms and signs of a radiculomyelopathy predominate because of spinal cord involvement. Patients may have radicular pain, stiffness or spasticity, limb weakness, sphincter disturbances, loss of sensation, and weakness.
CSF ANALYSIS Measurement of opening pressure is an important aspect of lumbar puncture. Opening pressure is elevated to greater than 200 mm H2 O in approximately two thirds of patients. CSF analysis may yield normal (ie, reference) results in 25% of patients and may be minimally abnormal in as many as 50%; therefore, identifying the organism via India Ink and serology is crucial.
CSF fluid appearance can be clear or turbid. Protein levels exceed 45 mg/dL in one third to two thirds of cases, ranging from normal to 300 mg/100 dL. The glucose level is usually normal and is less than 60% of the serum level in only 17-65%.
Mononuclear pleocytosis (>20 cells/mL) occurs in 13-31% of cases. Numbers vary between reports, but in one study, 55% of patients had fewer than 10 mononuclear cells/mL.
Close to 100% of CSF culture results are positive for Cryptococcus neoformans, whereas 66-80% of blood culture results are positive. India ink stain is positive in 74-88% of infected patients.
Test results for serum and CSF cryptococcal antigen may be positive. The initial diagnostic sensitivity of cryptococcal CSF antigen is 94.1%, followed by the serum antigen at 93.6%; this should not be used for discontinuing treatment.
A positive titer is sufficient to initiate therapy while cultures are pending in the appropriate clinical setting.
CT AND MRI CT scan is acceptable as a screening study, but MRI, with and without contrast, is the preferred diagnostic imaging modality. CT scan findings may be nonspecific or normal. Cryptococcal pseudocysts may appear as nonenhancing, hypodense lesions on CT scan.
With MRI, T1-weighted images may show low-intensity lesions in the basal ganglia, which are hyperintense on T2-weighted images and may enhance with gadolinium.
Twenty to thirty percent of patients show meningeal enhancement, parenchymal solid mass lesion without hemorrhage (granuloma), atrophy, cerebral edema, or hydrocephalus (see the image below). Commonly, in patients with increased intracranial pressure, the ventricles are small. If the imaging studies show a cryptococcal mass lesion (ie, cryptococcoma), toxoplasmosis and lymphoma must be considered in the differential diagnosis; brain biopsy may be indicated.
This image shows meningeal enhancement in a patient with cryptococcal meningitis.
HISTOLOGIC FINDING The meninges are opaque, and a capsular material may fill the subarachnoid space. Mixed meningeal infiltrates consisting of lymphocytes, eosinophils, plasma cells, multinucleated giant cells (containing phagocytized organisms), and neutrophils may surround clusters of organisms and sometimes form granulomas, but often the inflammatory response is scant.
Cryptococci extend along Virchow-Robin spaces into the brain. Parenchymal tubercles consisting of pseudocysts filled with organisms without significant inflammatory response, capsule formation, or gliosis are observed most often in the basal ganglia and cortical gray matter, but they may also be found elsewhere.
Primary Treatment If left untreated, cryptococcal CNS infections are fatal. Treatment with amphotericin B, flucytosine, fluconazole, and other antifungal agents greatly improves the prognosis, but a mortality rate of 6%, despite aggressive therapy, has been reported.
Current guidelines from the Infectious Diseases Society of America (IDSA) for primary therapy (induction and consolidation) of cryptococcal meningitis in HIVinfected patients recommend amphotericin B deoxycholate (0.7-1.0 mg/kg/day IV) plus flucytosine (100 mg/kg/day orally in 4 divided doses) for at least 2 weeks. This is followed by fluconazole (400 mg [6 mg/kg] per day orally) for a minimum of 8 weeks).[4]
Lipid formulations of amphotericin B (eg, liposomal amphotericin B [AmBisome], 6 mg/kg/day IV) can be substituted for amphotericin B. Liposomal amphotericin B may lead to quicker improvement with less renal toxicity. Flucytosine may be given intravenously in severe cases and in patients without oral intake.[4]
In a randomized study that compared 1 mg/kg versus 0.7 mg/kg of amphotericin B in HIV-infected patients with cryptococcal meningitis, the higher dose was more rapidly fungicidal; side effects were comparable.[5] Patients in both arms of the study also received flucytosine, 25 mg/kg 4 times daily.
Because amphotericin B treatment is not available in many centers in developing countries, oral therapy is an important alternative. Results of a randomized trial suggest that a 2-week course of high-dose fluconazole (1200 mg/day) combined with flucytosine (100 mg/kg/day) is the optimal oral therapy for cryptococcal meningitis. The combination proved more fungicidal than fluconazole alone and had a tolerable side-effect profile.[6]
In areas where flucytosine is unavailable, amphotericin B in combination with fluconazole (800-1200 mg/day) or voriconazole (300 mg twice daily) is an effective alternative in patients not receiving interacting medications.[7]
A double-blind, placebo-controlled phase II study suggested that adjunctive recombinant interferon-gamma 1b (rIFN- gamma 1b) may induce more rapid early sterilization of CSF in patients with HIV-associated Cryptococcus meningitis.[8] Patients in the treatment arm of this study received 100 or 200 g 3 times weekly for 10 weeks, plus standard antifungal therapy. IDSA guidelines suggest considering adjunctive rIFN- gamma 1b (100 g/m2 3 times weekly for 10 weeks) along with standard antifungal therapy, in cases of refractory infection. For patients who weigh less than 50 kg, consider giving 50 g/m2.[4]
Maintenance Therapy Maintenance therapy should be continued with fluconazole 200 mg/day. Amphotericin B (1 mg/kg/wk) is less effective than fluconazole, but it is an alternative for patients who experience relapse on fluconazole or for those who cannot tolerate it. Itraconazole 400 mg/day can be an alternative to fluconazole, but it is less effective.
Lifelong secondary prevention may be required. Relapses occur if secondary prevention is stopped or becomes ineffectual. Relapse rates without prevention range from 15-27%; this drops to 0-7% with prophylactic antifungal agents.
Consideration might be given to discontinuing secondary antifungal prophylaxis in selected patients who have responded well to highly active antiretroviral therapy (HAART), with 12-18 months of successful suppression of HIV viral replication. This remains controversial.
Criteria for discontinuing antifungal suppressive therapy during HAART, according to IDSA guidelines, are maintenance of a CD4+ cell count above 100 cells/L and an undetectable or very low HIV RNA level for 3 months or longer (minimum of 12 months of antifungal therapy).[4] The guidelines advise considering reinstitution of maintenance therapy if the CD4+ cell count falls below 100 cells/L.
Patients with cryptococcal disease who initiate HAART are at risk for cryptococcal immune reconstitution inflammatory syndrome (IRIS). Boulware et al found that in HAART-naive patients with AIDS and prior cryptococcal meningitis who developed IRIS after starting HAART, the cerebrospinal fluid tended to show less inflammation, with decreased CSF leukocytes (25 cells/mL or fewer), protein (50 mg/dL or less), interferon-gamma, interleukin-6, interleukin-8, and tumor necrosis factor-alpha, compared with patients who did not develop IRIS.[9]
Treatment of Relapse Patients who experience relapse should be restarted on induction-phase therapy. The susceptibility of the relapse isolate should be determined. A minimum inhibitory concentration (MIC) with a dilution difference of 3 or higher from the original isolate suggests development of direct drug resistance. Otherwise, an isolate with an MIC of 16 g/mL or more for fluconazole or 32 g/mL or more for flucytosine may be considered resistant, and alternative agents should be considered.[4]
Consider salvage consolidation therapy with fluconazole (8001200 mg/day orally), voriconazole (200400 mg twice daily orally), or posaconazole (200 mg orally 4 times daily or 400 mg orally twice daily) for 1012 weeks. If there are compliance issues and a susceptible isolate, prior suppressive doses of fluconazole may be reinstituted.[4]
Treatment of Increased Intracranial Pressure Increased intracranial pressure (>200 mm H2 O) occurs in over half of all patients with AIDS who have cryptococcal CNS infection, probably because of obstruction of the basal meninges or impaired CSF absorption. Since increased intracranial pressure is a prognostic factor whose correction leads to symptomatic improvement, this must be managed aggressively.
In the absence of obstructive hydrocephalus or risk of herniation, increased pressure (>250 mm H2 O) can be relieved by serial spinal taps or a lumbar-peritoneal shunt; in the presence of either of these, however, ventriculoperitoneal shunt is indicated. Decreasing intracranial pressure can rapidly improve headache, nausea, and vomiting. Mannitol has no proven benefit and is not routinely recommended.[4]
Treatment of Complications Seizures should be treated with standard therapy. Drugs that are less likely to affect bioavailability of highly active antiretroviral therapy (HAART) agents or anticryptococcal therapy are preferred.
Cognitive impairment may improve with successful anticryptococcal therapy. On a case-by-case basis, the presence of a cryptococcoma may lead to consideration of surgical intervention.
Rare visual loss due to local arachnoiditis or cryptococcal invasion of the nerves can be approached by nerve sheath decompression.
Overview Cryptococcus neoformans is a yeast that most commonly infects the central nervous system (CNS).[1] Most initial cryptococcal infections occur through inhalation of the yeast from the environment. Cryptococci have large polysaccharide capsules that strongly resist phagocytosis; the inflammatory reaction to the inhaled organisms produces a primary pulmonary-lymph node complex, which usually limits spread of the yeast from this site. C neoformans spreads from the lung and intrathoracic lymph nodes to circulate in the blood, especially if the host is immunocompromised.
Dissemination may occur during primary infection or during reactivation of the infection years later. The most commonly involved site is the CNS. In cases of cryptococcal meningoencephalitis that are not associated with human immunodeficiency virus (HIV) infection, the infection is often confined to the subarachnoid and perivascular Virchow-Robin spaces (see the image below).[2, 3]
Axial T2-weighted magnetic resonance image shows clustered hyperintensities in the left caudate; these are consistent with enlarged Virchow-Robin spaces caused by small cryptococcomas.
Preferred Examination Although the diagnosis of CNS cryptococcosis is made on the basis of a series of microbiologic investigations, computed tomography (CT) scanning and magnetic resonance imaging (MRI) are important diagnostic techniques in any patient with HIV infection or a patient with acquired immunodeficiency syndrome (AIDS) and neurologic dysfunction.
Several studies have shown that MRI is superior to CT in detecting abnormalities in patients with CNS cryptococcosis,[4] but with both imaging modalities, the number of lesions revealed is fewer than the number seen on pathologic examination.[5] Normal MRI findings do not exclude CNS cryptococcosis, because the typical features of this infection occur in only 40% of patients.
Computed Tomography CT scan findings are often nonspecific for CNS cryptococcosis. In a retrospective study, CT scans of 35 patients with intracranial cryptococcal infection demonstrated unremarkable findings in 43% of the patients.[6] However, positive findings included diffuse atrophy (34%), cryptococcomas (11%), hydrocephalus (9%), and diffuse cerebral edema (3%).
Cryptococcomas appear as round, hypoattenuating or isoattenuating lesions that occur less commonly as gelatinous pseudocysts (rather than as granulomas or abscesses). In immunologically intact hosts, the cryptococci usually induce a chronic granulomatous reaction; on CT scans, these cerebral cryptococcal granulomas appear as hypoattenuating or isoattenuating lesions, with or without enhancement.
Intracranial mass lesions occur frequently in patients with AIDS. The most common mass lesions detected by CT scanning or MRI are abscesses from toxoplasmosis, although lymphoma and less common infectious processes, such as cryptococcomas, must also be considered.[7]
Magnetic Resonance Imaging Cryptococcal meningitis is the most common CNS manifestation of cryptococcosis; the disease often has an insidious course (see the image below). In cases of AIDSrelated cryptococcal meningitis, leptomeningeal enhancement is not always seen on CT scans or MRIs.[5, 8, 9]
Axial contrast-enhanced T1-weighted magnetic resonance image shows diffuse, gyriform leptomeningeal enhancement. Enhancing lesions in the left basal ganglia, left temporal lobe, and left occipital lobe correspond to intraparenchymal cryptococcosis. The cryptococcal organism is surrounded by a polysaccharide capsule, which may protect it from the host inflammatory response even in immunocompetent patients. In response to the attack on the organisms by the host's immune system, the cryptococci produce a mucoid material. In a study by Arnder et al, of 3 patients were diagnosed with cryptococcal meningitis, 2 patients demonstrated thick enhancing subarachnoid spaces on postcontrast MRIs.[10] The diagnoses were confirmed at autopsy. In the postmortem MRI and pathologic examinations of the third patient, these areas of enhancement corresponded to the abundant mucoid material secreted by the organisms.[10]
Cryptococcal organisms spread from the basal cisterns through the Virchow-Robin spaces to the basal ganglia (as shown in the images below), internal capsule, thalamus, and brainstem.[3] The perivascular spaces may be enlarged as a result of the production of voluminous mucoid material. MRI is more sensitive than CT scanning in demonstrating abnormalities such as dilated perivascular spaces. These manifest on T2-weighted MRIs as punctate, hyperintense, round or oval lesions that are usually smaller than 3 mm. Enlarged perivascular spaces are not always a consequence of cryptococcosis; they may be the result of age-related changes or HIV-related atrophy.
Axial contrast-enhanced T1-weighted magnetic resonance image shows diffuse, gyriform leptomeningeal enhancement. Enhancing lesions in the left basal ganglia, left temporal lobe, and left occipital lobe correspond to intraparenchymal cryptococcosis.
T1-weighted magnetic resonance image demonstrates dilated perivascular spaces in the bilateral basal ganglia. Generalized atrophy is common in patients with AIDS; however, the observation of punctate hyperintensities is suggestive of cryptococcal disease, especially if other signs of diffuse atrophy (eg, ventricular and sulcal enlargement) are not present or if the patient has clinical signs or symptoms of meningitis.
By definition, cryptococcomas represent a collection of organisms, inflammatory cells, and gelatinous mucoid material in the brain parenchyma. Cryptococcomas may develop when organisms have extended directly from perivascular spaces into the parenchyma (see the following images) or, possibly, when they have invaded the parenchyma from other meningeal or ependymal surfaces.
T2-weighted axial magnetic resonance image demonstrates linear and punctate hyperintensities in the basal ganglia; these represent dilated perivascular spaces caused by small cryptococcomas. Cryptococcomas vary in size from several millimeters to several centimeters.
Axial T2-weighted magnetic resonance image shows clustered hyperintensities in the left caudate; these are consistent with enlarged Virchow-Robin spaces caused by small cryptococcomas.
T2-weighted axial magnetic resonance image demonstrates hyperintense cryptococcomas in the midbrain. Cryptococcomas are hyperintense on T2-weighted images. Although contrast enhancement of cryptococcomas is uncommon in cases of AIDS-related CNS cryptococcosis,[5] it has been reported.[10] The cryptococcal organism is surrounded by a polysaccharide capsule, which may protect it from the host inflammatory response, even in immunocompetent patients.
In immunologically intact hosts, the organisms usually induce a chronic granulomatous reaction. On MRI, the most common findings are punctate masses that demonstrate low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, without surrounding edema.
Choroid plexitis of the brain is a pathologic presentation of cryptococcosis. MRI demonstrates unilateral or bilateral enlargement and dense enhancement of the choroid plexus in the lateral and fourth ventricles.[11] These findings occur in association with clinical findings of leptomeningitis. The lesion may appear as an enhancing, intraventricular mass.
Unilateral cystic dilatation of the temporal horn of the lateral ventricle has also been described.[11] Cho et al believed this dilatation may be the result of entrapment of the temporal horn by inflamed choroid plexus, as well as extensive edema around the ipsilateral ventricle.[11]
Although MRI is useful as part of the initial investigation protocol for patients with suspected cryptococcal meningitis, serial imaging probably has a minimal role in monitoring response to therapy. However, magnetic resonance spectroscopy may detect changes in the metabolites that are related to inflammatory activity.
Treatment of acute cryptococcal meningitis in HIV infected adults, with an emphasis on resource-limited settings. Cochrane Database Syst Rev. 2008; (4):CD005647 (ISSN: 1469-493X)
Sloan D; Dlamini S; Paul N; Dedicoat M Hlabisa hospital, Private Bag x5001, Hlabisa, KwaZulu / Natal, South Africa, 3937. dereksloan@hotmail.com
BACKGROUND: Despite the advent and increasingly wide availability of antiretroviral therapy, cryptococcal meningitis (CM) remains a significant cause of mortality and morbidity amongst individuals with HIV infection in resource-limited settings. The ideal management of CM remains unclear. The aim of this review is to assess the evidence for deciding on which antifungal regimen to use as well as other modalities of management to utilise especially resource poor settings in order to achieve the best possible outcome and enable an individual with CM to survive their acute illness and benefit from antiretroviral therapy. OBJECTIVES: To determine the most effective initial and consolidation treatment strategy for CM in HIV infected adults. SEARCH STRATEGY: The Cochrane HIV/AIDS group search strategy was used. Key words in the search included, meningitis, cryptococcus neoformans, treatment, trial, human immunodeficiency virus, acquired immunodeficiency syndrome, antifungal agents, amphotericin, flucytosine, fluconazole, azole, lumbar puncture, cerebrospinal fluid (CSF) pressure and acetazolamide. SELECTION CRITERIA: Randomised of HIV-infected adults with a first episode of CM diagnosed on CSF examination, by India ink staining, CSF culture or cryptococcal antigen testing. DATA COLLECTION AND ANALYSIS: Data were extracted using standardised forms and analysed using Rev Man 4.2.7 software. MAIN RESULTS: Six studies are included in the review. Five of the studies
compared antifungal treatments and one study addressed lowering intracranial pressure. This study was stopped early due to excess adverse effects. The results of the other five studies as summarised as follows.Mayanja-Kizza 1998 compared fluconazole to fluconazole with 5 flucytosine. The dose of fluconazole used 200mg initially is lower than the recommended initial dose of 400mg. No survival advantage was found with the use of 5 flucytosine in addition to fluconazole.Two studies Brouwer 2004 and van der Horst 1997 compared Amphotericin (AmB) to AmB with 5 flucytosine. Both drugs were given at currently recommended doses for 2 weeks. No survival difference was found at 14 days or at 10 weeks (only recorded in Brouwer 2004). There were significantly more patients with sterile CSF cultures at 14 days in the group that received AmB with flucytosine.Brouwer 2004 compared AmB given alone to AmB given with flucytosine and fluconazole alone or in combination. This was a small study and no differences in mortality were noted between the groups.Bicanic 2008 compared high to standard dose AmB both with flucytosine. There was no difference in mortality between the two groups or adverse events.Leenders 1997 compared standard AmB to liposomal AmB. There was no difference in death rates between the two groups. But there were significantly fewer side effects in the group treated with liposomal AmB. AUTHORS' CONCLUSIONS: The main aim of this review was to determine the best treatment for cryptococcal meningitis in resourcelimited settings. In these settings usually only AmB and fluconazole are available. No studies suitable for inclusion in the review were found that compared these two drugs. Therefore we are unable to recommend either treatment as superior to the other. The recommended treatment for CM is a combination of AmB and flucytosine. The optimal dosing of AmB remains unclear. Liposomal AmB is associated with less adverse events than AmB and may be useful in selected patients where resources allow.Future research into the management of cryptococcal meningitis in resourcelimited settings should focus on the most effective use of medications that are available in these settings.Flucytosine in combination with AmB leads to faster and increased sterilisation of CSF compared to using AmB alone. As Flucytosine is often not available in developing countries, policy makers and national departments of heath should consider procuring this drug for HIV treatment programmes
Ann Indian Acad Neurol. 2010 Apr-Jun; 13(2): 112116.
doi: 10.4103/0972-2327.64635 PMCID: PMC2924508 Fungal infections of the central nervous system in HIV-negative patients: Experience from a tertiary referral center of South India K. N. Ramesha, Mahesh P. Kate, Chandrasekhar Kesavadas,1 V. V. Radhakrishnan,2 S. Nair,3 and Sanjeev V. Thomas Author information Article notes Copyright and License information Go to: Abstract Objective:
To describe the clinical, radiological, and cerebrovascular fluid (CSF) findings and the outcome of microbiologically or histopathologically proven fungal infections of the central nervous system (CNS) in HIV-negative patients.
Methodology and Results:
We identified definite cases of CNS mycosis by screening the medical records of our institute for the period 20002008. The clinical and imaging details and the outcome were abstracted from the medical records and entered in a structured proforma. There were 12 patients with CNS mycosis (i.e., 2.7% of all CNS infections treated in this hospital); six (50%) had cryptococcal infection, three (25%) had mucormycosis, and two had unclassified fungal infection. Four (33%) of them had diabetes as a predisposing factor. The common presentations were meningoencephalitis (58%) and polycranial neuritis (41%). Magnetic resonance imaging revealed hydrocephalus in 41% and meningeal enhancement in 25%, as well as some unusual findings such as subdural hematoma in the bulbocervical region, carpeting lesion of the base of the skull, and enhancing lesion in the cerebellopontine angle. The CSF showed pleocytosis (66%), hypoglycorrhachia (83%), and elevated
protein levels (100%). The diagnosis was confirmed by meningocortical biopsy (in three cases), paranasal sinus biopsy (in four cases), CSF culture (in three cases), India ink preparation (in four cases), or by cryptococcal polysaccharide antigen test (in three cases). Out of the ten patients for whom follow-up details were available, six patients recovered with antifungal medications (amphotericin B, 1 mg/kg/day for the minimum period of 6 weeks) and/or surgical treatment. Four patients expired (only one of them had received antifungal therapy).
Conclusions:
Most patients with CNS mycosis recover with appropriate therapy, but the diagnosis and management of these rare infections remains a challenge to clinicians.
Keywords: Amphotericin, central nervous system mycosis, outcome Go to: Introduction Fungal infections of the central nervous system (CNS) are relatively uncommon neuroinfections that are increasingly being recognized these days. This is mainly due to the increased awareness of clinicians about these conditions, the growing pool of immunocompromised host, the advances in imaging, and the availability of microbiological techniques to confirm the diagnosis from body fluids and specimens.[1,2] CNS mycosis can present as meningitis, encephalitis, stroke, intracranial mass lesions, spinal cord syndromes, or base of skull disorders.[2,3] The important conditions that predispose to CNS mycosis include AIDS, diabetes mellitus, use of immunosuppressants, organ transplantation, and hematological malignancies.[1-4] Though mortality and morbidity from CNS mycosis has improved over the decades, it remains high.[1,5] Against this background, we aimed to analyze the spectrum of CNS mycosis seen in HIV-negative patients treated in our institute over the last 8 years and to examine the outcome in these cases.
Go to: Materials and Methods This retrospective study was carried out at Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, a tertiary referral center for neurological and cardiac disorders. We defined 'CNS mycosis' as an infection of the central nervous system in a patient admitted with a neurological disorder, with the fungal etiology having been confirmed by histopathological or microbiological methods. We screened the case records of all admissions to the neurology services from January 2000 to December 2007 to identify all cases of CNS mycosis. During this period there were a total of 453 cases with neuroinfections and 12 (2.7%) of them satisfied our criteria for CNS mycosis. Their demographic data, clinical features, imaging findings, cerebrospinal fluid (CSF) picture, treatment details, and outcome were abstracted from the clinical records and entered into a structured proforma. For follow-up, patients and their caregivers were contacted either by telephone or by mail for details of current health status.
Go to: Results Twelve patients (six males and six females) with confirmed CNS mycosis were treated at our institute during the study period. Their mean age at presentation was 41.2 years (range 2366 years). The mean duration of symptoms at presentation was 73 days (range 13120 days). The various etiological agents were cryptococcus (six patients), mucormycosis (three), and aspergillus fumigatus (one). In the remaining two cases, the type of fungi could not be identified. Diabetes mellitus and long-term use of steroid for treatment of autoimmune disorders were the predisposing factors in four and two cases, respectively. Infection occurred in the setting of head injury and post neurosurgical procedure in one patient each. Four patients had no identifiable risk factors.
Patients presented with one of the two broad clinical presentations:
Meningitis syndrome: Seven patients had meningitis syndrome with fever and symptoms and signs of raised intracranial pressure and meningeal irritation. Two of them had hemiplegia due to vascular involvement and one had multiple cranial nerve palsies. Five had cryptococcal meningitis and one had postoperative meningitis due to aspergillus fumigatus. Cranial neuropathy syndromes: Five patients had polycranial neuritis, three with ocular motor involvements and two with lower cranial nerve palsies. Two each had cryptococcoma and mucormycosis. Routine hematological workup was unremarkable for most patients. Seven patients had leukocytosis, with a mean cell count of 18,857 cells/mm3 (range: 12,50032,000 cells/mm3), and nine had raised erythrocyte sedimentation rate of more than 50 mm in 1 h. MRI of the brain showed hydrocephalus in five patients and meningeal enhancement in three. Findings suggestive of choroid plexitis and vascular invasion of the middle cerebral artery was seen in one patient each. Other MRI findings included a carpeting lesion of the base of skull, an enhancing lesion in the cerebellopontine angle [Figure 1], and a subdural hematoma located in the bulbocervical location (this patient presented with spastic quadriparesis).
Figure 1 A 52-year-old lady presented with insidious onset, gradually progressive, right-sided trigeminal and facial nerve palsy of 4 months' duration. (a) Magnetic resonance imaging T2W axial sequence shows heterogeneously hyperintense lesion; (b, c) postcontrast ... All patients had undergone lumbar puncture for cerebrospinal fluid (CSF) study after cerebral imaging. The mean cell count in the CSF was 377 mm3 (range 51100 cells/mm3), eight had increased CSF cell count; only two had predominant polymorphonuclear leukocytosis. The mean CSF protein was 103.75 gm% (range 44 183 gm%) and mean CSF sugar was 33.91 mg% (range 365 mg%). Four patients had hypoglycorrhachia of less than 20% of the corresponding blood sugar. Cryptococcus was identified in the CSF by India ink preparation and was grown from the CSF in three patients. CSF smear was positive by PAS stain for mucor in one patient. The
paranasal sinus biopsy was positive for a specific fungus in three patients and unclassified in one. Cryptococcal polysaccharide antigen by latex agglutination method was positive in three out of the four patients in whom it was done. Meningocortical biopsy confirmed a specific fungus in three patients (cryptococcus, mucor, and Aspergillus fumigatus in one patient each). The workup carried out for bacterial meningitis and other chronic meningitides included CSF Gram's stain, polymerase chain reaction for Mycobacterium tuberculosis, cultures, and cytology for malignant cells; these tests were negative in all cases.
Seven patients were treated with 1 mg/kg/day of intravenous amphotericin B either for 6 weeks or till two sequential CSF cultures were negative (i.e., those that had been positive earlier). In addition, flucytosine at dose of 100 mg/kg/day for 2 weeks and fluconazole 400 mg/day for 8 weeks were given in one case each. Reversible renal failure and hepatorenal syndrome were noted in one patient each as complications of amphotericin treatment. Three patients underwent paranasal sinus debridement, two underwent resection of the intracranial/spinal mass, and one required ventriculoperitoneal shunt for hydrocephalus.
Follow-up data were available in ten cases; the mean duration of follow-up was 2.5 years. Five patients became asymptomatic and one made an incomplete recovery, with hydrocephalus as a sequel. Four patients expired (40%) in the hospital [hospital stay ranged from 336 days (mean 13 days)]. Three patients had cryptococcal infection and one had mucormycosis. Only one of the four patient who expired had received antifungal therapy. None of the surviving six patients had recurrence after the mean follow-up of 2.5 years. The clinicoradiological features and outcomes are summarized in Table 1.
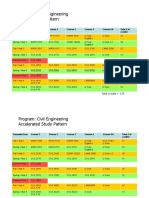
Table 1 Clinical features, investigation findings, and outcome of the study cohort Subgroup analysis
The majority of those with the meningitis syndrome (n = 7) had cryptococcus infection (71%). In those with the cranial neuropathy syndromes (n = 5), ocular motor involvement was seen only with mucormycosis (n = 2) and bulbar involvement/ lower cranial palsy was seen only with cryptococcus infection (n = 2). There was no statistically significant difference between those who survived (n = 6) and those who died (n = 4) with regard to age at presentation, presence of predisposing disorders, duration of symptoms, and specific MRI findings. However, only one of the four patients who died received any antifungal therapy, whereas all surviving patients had received antifungal therapy.
Go to: Discussion In this retrospective analysis, we have presented the clinicoradiological and CSF features and outcome of 12 consecutive patients with CNS mycosis. Fungal infection of the CNS was relatively rare in our experience (2.7% of all CNS infections). In other series that included patients with HIV and other immunocompromised patients, higher frequency of fungal meningitis (330% of all chronic meningitis) have been reported.[5,6] The risk factors for CNS mycosis in this series included diabetes mellitus, long-term steroid therapy, neurosurgery, and trauma. Other risk factors mentioned in the literature like HIV infection, organ transplantation, malignancy, etc. were not seen in our study cohort. This difference may be due to geographic and institutional referral bias. Cryptococcal meningitis is the most common clinical fungal infection of the CNS.[1,6,7] Certain syndromes are more common with some particular fungal type and this may guide further investigation and treatment. Signs of meningeal irritation occurred in 86% of cryptococcus infections, whereas focal neurological deficits were seen 50% of patients with aspergillosis in a series consisting of 57 autopsied patients with CNS fungal infections.[7] There are certain differences noted between immunocompetent and immunocompromised hosts in the clinical presentation: the duration of symptoms is likely to be longer and the incidence of neck rigidity is higher in immunocompetent individuals.[6]
Our patients presented with one of two broad syndromes: meningoencephalitis or cranial neuropathy. There was a distinct association between the fungal etiology and presentation. The majority of patients with cryptococcal infections presented with meningitis; two patients also had cryptococcoma. The other rare CNS manifestations described in cryptococcal infection are subdural effusion, dementia, and ischemic strokes, none of which were seen in our cohort.
We found lymphocytic pleocytosis in 6 patients (50%) and polymorphonuclear pleocytosis in two one in a cryptococcus infection and the other in an aspergillus infection. In the literature, polymorphonuclear pleocytosis said to be common in aspergillus and candida infection.[8] Immunocompromised patients, particularly those with HIV infection and AIDS, have higher a fungal load and tend to have higher yield with microbiological studies. In some series, India ink test was positive for cryptococcus in 80% cases, fungus culture was positive in 90%, cryptococcal polysaccharide antigen test (by latex agglutination or ELISA method) was positive in 90% cases.[8-10]
The radiological features of CNS mycosis tend to be nonspecific. They include hemorrhagic/edematous lesions, solid enhancing lesion, abscess, infarction, mycotic aneurysms, meningeal enhancement, hydrocephalus, sinusitis, etc.[11,12] MR imaging features in cryptococcal infections are cryptococcoma in basal ganglia and midbrain, hydrocephalus, and meningeal enhancement.[11,12]
Amphotericin B has poor penetration of the meninges, though it is a potent antifungal agent. Hence, it is often combined with flucytosine and fluconazole, which have better CSF penetration.[4] The mean treatment duration in those patients who completed treatment was 6.3 weeks. The recommended duration of treatment is 6 12 weeks or till culture becomes negative. The most important treatment-limiting toxicity reported with amphotericin is renal failure. This complication was seen in two out of seven of our patients, but the changes were reversible. Continuous infusion of conventional amphotericin is much cheaper and is probably as safe as treatment with the lipid-based formulation.[4]
Fungal infections of CNS often require surgical intervention for diagnosis (stereotactic biopsy) and therapy (CSF shunt procedures for hydrocephalus and resection of the fungal abscess or granuloma).[13] In our series, three patients underwent paranasal sinus debridement, two underwent resection of the intracranial/spinal mass, and one required a ventriculoperitoneal shunt for hydrocephalus. Debridement of sinuses is necessary in all forms of rhino-orbitocerebral mucormycosis.[14-17] It is important to carefully manage the predisposing conditions like diabetes while the patient is undergoing antifungal medications and surgery. Patients with AIDS require highly-active antiretroviral therapy (HAART) and long-term fluconazole maintenance therapy.[17]
The overall survival rate in this study was 60%, whereas the survival rate for those who received treatment was 86% (six out of seven patients). According to published literature, the survival rate varies between 40% and 92%.[1-4,6,7] In a study of 129 cases, the overall survival rate was 72%.[1] It was higher for cryptococcal and candida infection than for aspergillosis. In general, immunocompetent individuals with early diagnosis and treatment had better outcomes.[18] In a study of 38 patients with rhinocerebral mycosis, 47% died; the predictors of mortality were elderly age, intracranial extension, and immunocompromised state.[15] In view of the small number of cases in our study, we could not ascertain the prognostic factors.
In our small series, there were no specific clinical or imaging parameter that predicted higher mortality or complications. We observed that fungal etiology can be identified by a diligent search for fungi in the CSF by routine mycological tests in most cases. Stereotactic biopsy or biopsy of the any granuloma present in the paranasal sinuses are likely to provide accurate diagnosis. Since most of the patients who receive appropriate antifungal therapy recover, it is important to resort to biopsy if a definitive diagnosis is not readily available.
Fungal infections of the central nervous system: A review of fungal pathogens and treatment
Andrew Redmond1, Craig Dancer2, Marion L Woods3 1 Princess Alexandra Hospital, Department of Microbiology, Brisbane; University of Queensland, Adelaide, Australia 2 Institute of Veterinary and Medical Science, Adelaide, Australia 3 University of Queensland, Adelaide; The Royal Brisbane and Women's Hospital, Brisbane, Australia
Date of Acceptance Correspondence Address: Marion L Woods
18-Jun-2007
Department of Infectious Diseases, The Royal Brisbane and Women's Hospital, Herston 4029, Queensland Australia
8 2
DOI: 10.4103/0028-3886.35686
PMID: 17921654
Abstract Multiple factors influence the outcome of fungal infection of the central nervous system (CNS). The host and the pathogen in concert with drug delivery across the blood-brain barrier and drug activity are key factors in outcome. Drug costs can be prohibitively expensive. Drug toxicity with standard antifungal agents such as amphotericin B (infusion rate toxicity) can be reduced using simple techniques such as slower infusion and appropriate saline loading. Continuous infusion can allow relatively large doses of amphotericin B (up to 2 mg/kg/day, remaining below 0.08 mg/kg/hour) to be given with toxicity profiles comparable to expensive lipid formulations of amphotericin B. Dedicated peripherally inserted central catheters can remain in situ for weeks to months and are safe and relatively inexpensive. Correction of metabolic pathology in the case of mucormycosis and resolution of neutropenia are essential to effective treatment of filamentous fungal infections such as Mucor, Aspergillus and Scedosporium . The pharmacology and pharmacokinetics of the current major antifungal agents used to treat fungal infections of the CNS are reviewed. Tables that provide information about achievable CNS drug levels, antifungal susceptibilities and the likelihood of intrinsic drug resistance of significant fungal pathogens have been included to help the clinician with therapy. Treatment recommendations for Cryptococcal and Candida meningitis and for rhinocerebral infection with Mucor and Aspergillus have been included.
Keywords: Amphotericin B, antifungals, Candida , continuous infusion, Cryptococcus , meningitis, pharmacokinetics, toxicity
How to cite this article: Redmond A, Dancer C, Woods ML. Fungal infections of the central nervous system: A review of fungal pathogens and treatment. Neurol India 2007;55:251-9
How to cite this URL: Redmond A, Dancer C, Woods ML. Fungal infections of the central nervous system: A review of fungal pathogens and treatment. Neurol India [serial online] 2007 [cited 2013 May 7];55:251-9. Available from: http://www.neurologyindia.com/text.asp?2007/55/3/251/35686
Therapy of fungal central nervous system (CNS) infections is influenced by multiple factors including the pathogen and its drug susceptibility and by drug activity in the CNS, brain and spinal cord. Central nervous system drug levels are affected by the blood-brain barrier and the potential effect of efflux transporters that can modulate drug concentrations in the cerebrospinal fluid (CSF) and neural tissues. [1],[2] Also, efflux transporters have been identified in fungal pathogens that affect their susceptibility to antifungal agents. [3]
Although 70,000 to 1,500,000 fungal species exist and nearly 300 species have been associated with human infection, there are about a dozen yeasts and about 30 molds that are commonly identified as human pathogens. [4] Pathogens encountered in the CNS include yeasts ( Candida [neonates], Cryptococcus ), moniliaceous molds ( Aspergillus spp., Fusarium spp.), dimorphic fungi ( Blastomyces , Coccidioides , Histoplasma ), zygomycetes ( Mucor spp., Rhizopus spp.) and dematiaceous fungi ( Pseudallescheria [ Scedosporium ] spp.).
Fungal cell wall components (ergosterol, chitin, 1,3 and 1,6-glucan) have been the major targets of the five classes of antifungal agents in use currently, with the exception of flucytosine (antimetabolic effects). [3] Drugs that affect uniquely
occurring fungal cell wall components such as ergosterol (ergosterol binding polyenes or ergosterol synthesis inhibition-azoles, allylamines) and glucan synthesis inhibitors (echinocandins) are in current use.
Amphotericin B has been in use for decades and remains an effective agent for most yeasts and molds [Table - 1]. The main toxicity is renal impairment via reduction in blood flow to both the renal tubules and glomeruli. Toxicity is infusion rate-related and may be ameliorated by continuous infusion of amphotericin B deoxycholate through a dedicated line such as a peripherally inserted central catheter (PICC) or by use of a lipid-based amphotericin B product. Continuous infusion of amphotericin B deoxycholate may provide an economically preferable alternative to more expensive lipid-based amphotericin B agents (double lumen PICC lines cost about $100 USD and last for weeks to months). Renal toxicity associated with continuous 24-h infusion (up to 2 mg/kg/day, less than 0.08 mg/kg/h) is roughly equivalent to that associated with lipid-based amphotericin B products. [5],[6],[7],[8],[9],[10] Saline infusion prior to amphotericin B infusion is recommended to additionally reduce renal toxicity. [11] Azoles such as fluconazole and voriconazole have been shown to be effective with acceptable toxicity profiles. Newer agents such as the echinocandins are effective antifungals but are expensive [Table - 1].
This review will discuss the pharmacology and pharmacokinetics of these agents to treat fungal infections of the CNS. We include a table for likely intrinsic drug resistance to antifungal agents [Table - 2], as well as minimal inhibitory concentration data for the most common human fungal pathogens in conjunction with achievable CSF drug levels [Table - 3],[Table - 4],[Table - 5]. We will highlight treatment of Cryptococcal meningitis, Candida meningitis and invasive molds (rhinocerebral mucormycosis).
Mode of Action
Amphotericin B is a polyene antibiotic that is derived from Streptomyces nodosus a soil actinomycete. Amphotericin B binds to ergosterols in the cell wall of fungi and by doing so, disrupts the cell wall integrity leading to increased permeabilty, K + leakage and death of the cell. [3]
Flucytosine is a cytosine analog that enters fungal cells via cytosine permease. It is converted to 5-fluorouracil within the cell. Further enzymatic activity converts this molecule to 5-fluorouridine triphosphate which inhibits thymidylate synthetase (affecting DNA synthesis) or to 5-fluorouridine monophosphate that inhibits proteins' synthesis by interfering with mRNA synthesis.
Allylamines (terbinafine) inhibit squalene epoxidase in the ergosterol pathway. Accumulation of squalene is thought to be toxic to fungal cells. The role for terbinafine in systemic fungal infection is anecdotal. It is used in combination with azoles in the setting of difficult to treat Aspergillus or Scedosporium infections.
Azoles ([imidazoles- ketoconazole, miconazole], [triazoles- fluconazole itraconazole, voriconazole, posaconazole, ravuconazole]) inhibit lanosterol 14 a-demethylase, a cytochrome P-450-dependent fungal enzyme that is necessary for ergosterol production.
Glucan synthesis inhibitors ([echinocandins -caspofungin, anidulafungin and micafungin]) interfere with glucan synthesis leading to osmotically unstable cells (analogous to the effects of penicillin on susceptible gram-positive bacteria). [3],[12]
Pharmacokinetics
Amphotericin B
Amphotericin B is highly protein-bound to human serum albumin and to human a1-acid glycoprotein in vitro (95-99.2%), with the maximum predicted concentration of unbound amphotericin B being 0.774 mg/ml. [13],[14] In vitro experiments suggest that non-protein-bound (free) amphotericin B is the component with antifungal activity. [13],[15],[16] Despite low CSF levels achieved in the rabbit model, sufficient conventional amphotericin B can be detected in brain tissue to have an equivalent anti- Candida effect to liposomal amphotericin B that is dosed at fivefold greater doses. [17] This difference appears to be related to free amphotericin B levels. Lipid-based amphotericin B compounds have less than one-tenth (1/10) the amount of free unbound amphotericin B available compared with the level of free unbound amphotericin B associated with the use of conventional amphotericin B, [13] although a clinical study of the treatment of cryptococcal meningitis found equivalence between lipid and non-lipid-based amphotericin. [18] A recent trial has shown that 10 mg/kg dosing of liposomal amphotericin B is not superior to 3 mg/kg in the treatment of invasive mold infection. [19]
The half-life of conventional amphotericin B is 5.3 days 1.25 days, with a volume of distribution at steady state of 1807 ml/kg (virtually all tissue distributed). [15] It appears that conventional amphotericin B is eliminated largely unchanged in urine (20.6%) and feces (42.5%) (via biliary secretion probably) very slowly over a week. Amphotericin B clearance is 50-fold lower than plasma flow to either kidneys or the liver. [15]
Azoles
Fluconazole is a widely used agent with activity against yeasts, particularly species of Candida and Cryptococcus . It has no activity against filamentous fungi. It is available in intravenous and oral preparations. The oral bioavailability is very high and
is unaffected by gastric pH or food. Only a small fraction is protein-bound and its elimination is mostly by renal excretion of unchanged drug. The half-life in healthy volunteers is approximately 29.7h, making it suitable for daily dosing. Fluconazole is widely distributed through body tissues, including the CSF.
Fluconazole CSF levels are available from studies in healthy controls and in the setting of CNS infection with Coccidioides, Scedosporium and Cryptococcus in HIVinfected patients. Achieved CSF levels vary between 1.12 -6.2 mg/ml (52-89% of serum levels) and occur within 4h of oral dosing [Table - 2]. The CSF half-life appears to be prolonged. Persisting CSF levels between 2.16 - 4.44 mg/ml have been detected in humans with fungal meningitis up to 24h after administration and are higher than concomitant serum levels. [20],[21] The doses used in these studies were lower than the 400 to 800 mg daily which is recommended for CNS infections. The CSF levels are comparable to the levels achieved in a rabbit model. [22] The elimination half-life in the CSF in a rabbit model is approximately 9h. [23] In human studies the ratio of CSF to blood levels appears to be higher in the setting of infection, suggesting increased permeability of the blood-brain barrier related to inflammation.
Itraconazole has a wider spectrum of activity than fluconazole but is more difficult to use due to a complex pharmacokinetic profile. The drug is highly water-insoluble and extensively protein-bound. Oral bioavailability is limited and affected by fasting state and gastric pH. Bioavailability can be improved by administration with food or acids or in capsules or cyclodextrin vehicles and is reduced by H-2 receptor antagonists. Itraconazole has a very high volume of distribution and levels in tissues have been shown to be higher than in plasma. The half-life is long allowing daily dosing. [24]
Although itraconazole has been reported in case series to be successful for some CNS infections, particularly Aspergillus , its penetration into CSF is poor. In rabbit studies peak CSF levels achieved were 0.156 mg/l and the CSF: serum ratio was 9%. Inflammation of the meninges made no difference to the CSF levels. [22]
Voriconazole is a triazole agent with a broader spectrum of activity including yeasts and also filamentous molds Aspergillus spp., Scedosporium spp. and Fusarium spp. Oral bioavailability is reported to be almost 90% and an intravenous preparation is also available. Absorption is affected by fatty meals but not gastric pH. The plasma half-life is 6h allowing for twice daily oral administration. In healthy subjects the volume of distribution is high, suggesting good tissue penetration. In contrast to fluconazole up to 60% of voriconazole is protein-bound and the drug undergoes extensive hepatic metabolism. It is both a substrate and inhibitor of the cytochrome P450 isoenzymes CYP2C19, CYP2C9 and CYP3A4 and has significant interactions with other drugs. The pharmacokinetics are non-linear due to saturation of metabolism. With appropriate loading doses, steady state concentrations can be achieved at 24h. The intravenous preparation contains a vehicle, SBECD, which accumulates in moderate to severe renal impairment, GFR<50 mls/min. [25],[26]
Cerebrospinal fluid and brain tissue penetration by voriconazole has been reported in human studies of meningitis patients [Table - 2]. High CSF levels are achievable rapidly. CSF levels from 0.08 to 3.93 g/ml are reported (CSF: serum ratios of 0.221) [27],[28],[29],[30],[31] and levels of up to 0.72 g/ml and 2.41 g/ml have been reported within 2h of intravenous and oral administration respectively. [30] Brain tissue levels appear to be higher than plasma levels and peak tissue levels of 58.3 g/mg have been reported. [30]
Posaconazole is a broad-spectrum triazole drug that is currently available only as an oral suspension. Less information is available about this agent than the older agents. Its absorption is improved when taken with fatty food. It has a large volume of distribution (Vd=486L) and is extensively protein-bound. It undergoes glucuronidation in the liver to inactive metabolites. [32],[33] It is a substrate for the cytochrome P450 isoenzyme CYP3A4 and is expected to have significant interactions with drugs such as the rifamycins and calcineurin inhibitors. It has a broad spectrum of antifungal activity in vitro including most pathogenic yeasts, Aspergillus spp. and promising activity against zygomycetes and Fusarium spp. Reports and case series demonstrate its clinical activity against Candida spp.
(including fluconazole-resistant species), Aspergillus , zygomycetes and Fusarium . The little information available about CNS penetration of this agent suggests that levels are below the limit of detection, [34] but case series suggest that the agent is active against CNS fungal infections. [35],[36]
Ravuconazole is a broad-spectrum triazole drug undergoing evaluation. A rabbit study has shown that the drug penetrates into brain tissue, [37] but no human data are available at this time.
Echinocandins
Echinocandins are not orally bioavailable and are given by intravenous infusion. All are significantly protein-bound with half-lives compatible with once daily dosing [caspofungin (96.5%, t 1/2 10 hours, Cmax 12 mg/ml), micafungin (99.5%, t 1/2 13 hours, Cmax 7.1 mg/ml), anidulafungin (80%, t 1/2 25.6h, Cmax 7.5 mg/ml)]. Each of these echinocandins achieves maximum concentrations in serum that exceed the MICs of many Candida species and some Aspergillus spp. Clinical studies show efficacy of echinocandins against Candida and some Aspergillus spp. The current role of echinocandins is for salvage therapy of Candida and Aspergillus infections. [12]
Clinical Use of Antifungal Agents
Therapy of cryptococcal meningitis is aimed at CSF sterilization and reduction of intracranial pressure to less than 200 mmH 2 O. Elevated CSF pressures > 350 mmH 2 O can be associated with the clinical signs of papilloedema, decreased visual acuity, decreased hearing, headache and confusion. Focal neurological signs may indicate mass lesions (cryptococcoma).
Therapy is usually given as induction followed by a maintenance course. In HIVinfected individuals, amphotericin B (0.7-1 mg/kg/day) plus flucytosine (100 mg/kg/day divided into four oral doses) is given for two weeks or until the yeast is cleared from the CSF. [38] This is followed by oral fluconazole 400-800 mg/day for up to 10 weeks (until CSF sterile). [39] Chronic suppression follows with fluconazole 200 mg/day. Cessation of therapy may be considered if there has been sufficient immune reconstitution and complete suppression of HIV replication. [40] In HIVuninfected individuals therapy may be the same or with the combination of amphotericin B and flucytosine being given for 6-10 weeks. In this setting therapy is usually curative without a requirement for further treatment.
Cerebrospinal fluid pressure symptoms can be managed by lumbar puncture to reduce the pressure to < 200 mmH 2 O (as often as needed). Ventriculo-peritoneal shunts may be required in patients with sustained increased pressures.
HIV-infected patients with a history of cryptococcosis are at risk for development of immune restoration disease on introduction of antiretroviral therapy. This has been described with lymphadenitis [41],[42],[43],[44],[45] or CNS disease with recurrent meningitis [46],[47],[48],[49] or cryptococcoma. [50] The pathogenesis of this disease process is still being clarified. Optimal therapy has not been defined but case series have reported success with varied management strategies.
Candida meningitis is uncommon, but occurs predominantly in three groups of patients: neonates, neurosurgical patients and immunosuppressed patients. The disease occurs most commonly as a complication of fungemia, but may follow direct inoculation, e.g., after the placement of CNS prostheses. There are no randomized trials to guide therapy. Neonatal Candida meningitis may present in a nonspecific fashion; is a particular risk in extremely low birthweight infants; and series report mortality up to 37.5%. [51],[52],[53],[54]
In neurosurgical patients Candida meningitis occurs after placement of a device such as a shunt or external drain. [55-58] Symptoms vary but usually include lethargy, fever and meningism. Focal neurological abnormalities and seizures may occur. Cerebrospinal fluid pleocytosis is usually observed, however positive gram stains and hypoglycorrhachia are uncommon.
Candida meningitis has been described in a variety of immune deficiency states: chronic granulomatous disease, myeloperoxidase deficiency, IgA deficiency, severe combined immunodeficiency, HIV infection, solid organ transplantation and lymphoma. [59],[60],[61],[62],[63],[64],[65],[66],[67] In the reported HIV-infected patients CSF pleocytosis was universal and hypoglycorrhachia common. In this group of patients all presented with either fever or headache or both.
Amphotericin B and flucytosine in combination are recommended for treatment. [68],[69] Monitoring of flucytosine levels has been recommended, aiming for serum levels 40-60 g/ml. [70],[71] Fluconazole and flucytosine are known to achieve high levels in the central nervous system. [72],[73],[74] In vitro evidence suggests that amphotericin B and flucytosine act synergistically [75] but no studies confirm clinical superiority of combination therapy for Candida meningitis. Animal data suggest amphotericin B may be more rapidly fungicidal than fluconazole for Candida [76] and there are reports of therapeutic failure of fluconazole in neonatal Candida meningitis. [77],[78] In neurosurgical patients, removal of prosthetic devices is recommended. Duration of therapy is not well defined, but generally a minimum of four to six weeks is suggested. Intravenous amphotericin with oral flucytosine is commonly employed until the signs and symptoms have resolved, then completion of therapy is with oral fluconazole. The echinocandins and extended-spectrum azoles have been shown to be efficacious in candidemia, and voriconazole is known to penetrate well into the CNS. These agents may be expected to be useful for the treatment of Candida meningitis.
Rhinocerebral infections with Aspergillus spp. or zygomycetes are conditions with high rates of morbidity and mortality. The basis of treatment is to correct the underlying metabolic (ketoacidosis) and hematologic (neutropenia) pathology. These
fungal pathogens are angioinvasive and commonly cause tissue infarction (brain/paranasal sinus mucosa/cavernous sinus) by clotting blood vessels. This angioinvasive characteristic promotes tissue invasion at the same time impairing delivery of drugs to the site of infection. Surgical debridement in combination with high-dose amphotericin B (up to 2 mg/kg/day by continuous 24-h infusion or lipidbased alternatives) or voriconazole/posaconazole/echinocandins (if Aspergillus ) are the treatments that may alter outcome in an otherwise 100% mortality in untreated patients. These patients usually require multiple surgical procedures that combine otolaryngological and neurosurgical expertise. [31],[79],[80],[81]
Conclusion
A vast amount of literature has been published dealing with treatment of CNS yeast infections such as Cryptococcus neoformans and Candida albicans . Clinical guidelines such as those published by the Infectious Diseases Society of America are a ready reference and clinical guide to therapy and are freely accessible on the internet (http://www.idsociety.org/). MIC tables for the 30 most common fungal species that cause disease in humans are intended as a guide to clinicians. Individual local susceptibility testing is essential in choosing appropriate therapy. Treatment of CNS infections with zygomycetes, on the other hand, is largely based on anecdotal series of cases. Cost of antifungal therapy remains a crucial issue worldwide. Whereas lipid-based formulations of amphotericin B offer lower rates of renal toxicity, their costs may not be affordable. Amphotericin B deoxycholate given as a continuous infusion, with appropriate saline loading, through a dedicated line remains a safe and affordable option with similar toxicity profiles compared with expensive lipid-based compounds. Because it is the free (non-protein-bound) amphotericin B that has antifungal effect, the advantage gained by liposome/lipid formulations (an order of magnitude lower free amphotericin B concentrations) in terms of renal toxicity, can be matched by continuous infusion amphotericin B. More clinical trials that appropriately administer continuous infusions of amphotericin B and measure free amphotericin B concentrations by HPLC (high performance liquid chromatography)
could potentially be of great economic and clinical benefit. (Animal models such as the rabbit model of Candida infection [13],[15] have inexplicably not reported or tested continuous infusion amphotericin B treatment arms to date)[95].
REVIEW ARTICLE Year : 2007 | Volume : 55 | Issue : 3 | Page : 267-273 Surgical management of intracranial fungal masses
Vedantam Rajshekhar Department of Neurological Sciences, Christian Medical College, Vellore, India
Date of Acceptance Correspondence Address: Vedantam Rajshekhar
11-Apr-2007
Department of Neurological Sciences, Christian Medical College, Vellore - 632 004 India
2 3
DOI: 10.4103/0028-3886.35688
PMID: 17921656
Abstract Background: Intracranial fungal masses (IFMs, granulomas and abscesses) are uncommon lesions, infrequently encountered by neurosurgeons. There is no conclusive evidence on the ideal surgical management of these lesions. Aims: To summarize the recent literature on the prevalence, presentation, surgical management and outcome of patients with IFMs. Materials and Methods: The recent published literature was searched using standard search engines (PubMed and Google) for articles reporting on the databases and surgical management of IFMs. A special effort was made to include publications from Indian centers. Results: Intracranial fungal masses were rarely seen even in major neurosurgical centers in India with a prevalence of around one to two per year. While most patients with IFM have immunosuppressed states, nearly 50% of patients with IFMs (especially in India) have no obvious predisposing causes and are apparently immunocompetent. The clinical presentation could be categorized into three groups: 1. Involvement of the cranial nerves 1 to 6 with orbital and nasal symptoms. 2. Focal neurological deficits due to involvement of any part of the neuraxis; and 3. "Stroke-like" presentation with sudden onset of hemiparesis. Based on the presence or absence of radiological evidence of paranasal sinus disease, IFMs were classified into two types: 1. Rhinocerebral type; 2. Purely intracranial type that was further divided into a. intracerebral or b. extracerebral forms. Aspergillus species was the commonest fungal organism causing IFMs but a number of other fungi have been reported to cause IFMs. Surgery for IFMs can be of different types, namely 1. Stereotactic procedures; 2. Craniotomy; 3. Shunt surgery; and 4. Treatment of fungal aneurysms. Generally, radical surgery is advocated for IFMs but there is no unanimity regarding the radicality of the excision especially for the rhinocerebral form of the disease. Surgery should always be followed by antifungal therapy for prolonged periods. Mortality and morbidity in
patients with IFMs is very high and ranges from 40-92%. Immunosuppressed patients with IFMs and those in whom the diagnosis is delayed have the highest mortality rates, with immunocompetent patients with the rhinocerebral form of the disease having the best outcome. Conclusions: There should be a high index of suspicion for IFMs not only in patients with known risk factors for the development of fungal infections but also in immunocompetent patients in India. Intraoperative pathological diagnosis should be obtained in any patient suspected to have an IFM and tissue should be processed for fungal cultures. Prompt diagnosis, radical and safe surgery and aggressive and prolonged treatment with anti-fungal agents may lead to a better outcome especially in immunocompetent patients.
Keywords: Brain, fungal abscess, fungal granuloma, outcome, stereotactic surgery, surgery
How to cite this article: Rajshekhar V. Surgical management of intracranial fungal masses. Neurol India 2007;55:267-73
How to cite this URL: Rajshekhar V. Surgical management of intracranial fungal masses. Neurol India [serial online] 2007 [cited 2013 May 7];55:267-73. Available from: http://www.neurologyindia.com/text.asp?2007/55/3/267/35688
Intracranial fungal masses (IFMs, granulomas and abscesses) are uncommon entities, although, they are being increasingly recognized in recent years. The largest case series reported to date has 40 patients gathered over 22 years from two centers,
one in India and the other in the United States. [1] It is speculated that their increasing incidence is attributable to the rising incidence of human immunodeficiency virus (HIV) infections, increased used of immunosuppresants, increased survival amongst patients undergoing organ transplants and cancer chemotherapy and the rising incidence of diabetes mellitus (DM) especially in India. Intracranial fungal infections including meningitis are quite commonly seen in the group of patients mentioned above but IFMs are relatively infrequently reported. The management of patients with IFM has not been standardized although it is agreed that medical management with antifungal agents is the mainstay of therapy. The role of surgery (biopsy versus partial excision versus radical excision) and the duration of antifungal antibiotic therapy have not been clearly elucidated in the literature. This article attempts to review the literature on the role of surgery in the management of patients with IFM and to determine prognostic factors if any reported in the literature. The recent published literature was searched using standard search engines (PubMed and Google) for articles reporting on the surgical management of IFMs. A special effort was made to include publications from Indian centers.
Prevalence
In a neurosurgical service, one would only rarely encounter IFMs. This is borne out by the sparse reports of IFMs from several large neurosurgical centers in India. There were 32 IFMs in a 14-year period in PGI, Chandigarh. [2] In a study spanning 22 years, 40 patients with IFMs were seen in NIMHANS, Bangalore and another center in the United States. [1] From NIMS, Hyderabad, 21 patients with aspergillomas were reported over a period of seven years. [3] In our center, we encountered 13 patients with intracranial aspergillomas over a 12- year period. [4] Mehta et al. [5] from AIIMS, New Delhi, reported 14 patients with an IFM over a 17 year period. In a review of cerebral aspergillomas, Nadkarni et al. [6] from KEM Hospital, Mumbai collected 18 patients over a 38-year period. It is, therefore, likely that even in large neurosurgical centers in India, the caseload of IFMs would not
exceed two per year. Surgery for IFMs would constitute about one per 1000 neurosurgical procedures performed at these centers. With these prevalence rates, it is not surprising that IFMs are rarely suspected in patients with isolated intracranial masses.
One could conversely study the prevalence of IFMs in patients who undergo transplant procedures. During a three-year period, 17 cases of IFMs (abscesses) were diagnosed in a cohort of 1620 patients who had undergone liver, heart, lung, renal and stem cell transplants in a center in the United States. [7] In another series from Pittsburgh, over a 14 year period, involving 2380 liver transplants, 1650 kidney transplants and 598 heart and heart-lung transplants, IFMs were diagnosed in 24 patients (0.5%). [8] These were most often seen within the first 3 months of the transplant. Another series from a major center for bone marrow transplantation in the United States reported 53 patients with fungal brain abscess over an 8.5 year period. [9] In a prospective study from our center, 1476 primary renal transplant recipients were evaluated for systemic mycoses and eight (0.5%) were diagnosed with IFMs. [10] The cumulative prevalence of IFMs in transplant recipients thus varies between 0.5 and 1%.
Clinical Presentation
Intracranial fungal masses can be seen in any age group but most patients are in the third, fourth and fifth decades of life. They have been reported even in neonates, infants and young children. [11] The duration of symptoms can vary from a few days to several months or even years. [1],[2],[3],[4],[5],[6],[12],[13] The illness generally has a shorter duration in patients with an IFM without sinus disease. [12] The disease can be indolent especially in those in whom the disease spreads from the sinuses to the brain and such patients may present with symptoms of several years duration. The clinical presentation is not specific but can be divided into three distinct types depending on the nature of the disease. [2],[3],[4] The three types of
clinical presentation are: 1. Involvement of the cranial nerves 1 to 6 with orbital and nasal symptoms. These symptoms/signs are common in patients with fungal infections that originate in the paranasal sinuses (PNS) and spread to the intracranial compartment by the contiguous route.; 2. Focal neurological deficits due to involvement of any part of the neuraxis; and 3. "Stroke-like" presentation with sudden onset of hemiparesis. Additionally, patients with any of these presentations might manifest features of raised intracranial pressure, seizures and altered sensorium. The altered sensorium can result from raised intracranial pressure, ischemia due to the vasculitis associated with the concomitant fungal meningitis and fungal meningoencephalitis. "Stroke-like" presentation is not common and has been reported in 6-10% of patients. [2],[3],[4] It results from fungal arteritis involving the cerebral vessels in the cavernous sinus or the circle of Willis. Rarely, patients with fungal aneurysms present with subarachnoid hemorrhage. [14],[15] Interestingly, fever is an infrequent symptom in patients with IFM and is seen in only 10 - 31% of patients. [1],[2],[5],[6],[12]
Predisposing Illnesses
DM is a frequent predisposing illness in patients with IFM especially that associated with PNS involvement. Several other diseases and conditions that are reported as risk factors in patients with IFM include, HIV infection organ transplantation, cancer chemotherapy, prolonged steroid therapy, autoimmune disorders such as systemic lupus erythromatosis and tuberculosis. In recent years there have been several reports of IFMs in large numbers of immunocompetent patients with no obvious focus of infection. Intracranial fungal masses in immunocompetent patients have been predominantly reported from India, Pakistan, Saudi Arabia, Africa and California in the United States. [12],[13] It is postulated that a hot, dry climate with a high content of aspergillus spores in the atmosphere due to agriculture dust may be a probable cause for the occurrence of IFMs in persons residing in these regions. Nearly 50% of patients with IFMs have no overt predisposing illness or evidence of
immunosuppression. [1],[2],[4],[11],[12] It is possible that in some of these patients, there might be subclinical impairment of cell-mediated immunity.
Rarely, fungal infection may follow direct inoculation of the brain during intracranial or transsphenoidal surgery or following trauma. [15],[16] Sharma et al. [2] reported two patients who developed IFMs following intracranial surgery.
Associated systemic fungal infections
Intracranial fungal masses usually develop by the spread of fungal infection to the intracranial compartment from a systemic source of infection. The commonest focus of such infection is the PNS and the mastoid sinuses. The other systemic sources of infection include the lungs and heart especially in the presence of artificial heart valves. The disease is usually spread through the hematogenous route but invasion of contiguous tissues and spread into the intracranial compartment is also common in the case of PNS and mastoid infections. In a proportion of patients with IFM, however, no obvious systemic source for the fungal infection is discernible in spite of an extensive search for the same.
Causative Organisms
The fungi that cause IFMs are dealt with in detail in other articles in this issue. Only the common organisms will be mentioned here. The commonest fungus that produces an IFM is the Aspergillus spp. Aspergillus flavus is generally implicated as the causative organism in patients who are immunocompetent whereas A . fumigatus is more frequently reported in immunocompromised individuals. [6],[12] The other fungi causing IFMs include cryptococcus , mucormycosis, Candida , cladosporium and dematiaceous fungi. [1],[2],[5],[7],[8],[9],[10],[17],[18],[19],[20] Reports of several
other fungi producing IFMs are available in the literature but most are individual case reports. [21],[22] Fungal aneurysms are caused usually by Aspergillus or mucormycosis. The angioinvasive nature of these organisms leads to the digestion of the elastic lamina of the vessels by the production of the enzyme elastase. [14]
Imaging Diagnosis
Imaging diagnosis of IFMs is dealt with in another article in this issue and only some salient features will be mentioned here. Contrast enhanced computerized tomography (CT) and magnetic resonance imaging (MRI) of the head are the investigations of choice. Unfortunately, neither of these tests provides a definitive diagnosis of an IFM. CT and MRI only reveal intracranial mass or masses that enhance with contrast and can also provide evidence of involvement of the paranasal sinuses and the mastoid sinus. Careful attention should be paid to the sinuses in any patient suspected to have an IFM. The masses are contrast enhancing with perilesional edema. [1],[2],[4],[6] It has been postulated that MR appearances are characteristic for IFMs caused by different fungal agents. Cryptococcomas appear as hypointense masses on T2W images whereas aspergillomas have an intermediate signal intensity on T2W sequences. [1] Siddiqui et al. [12] reported that IFMs caused by aspergillus were extremely hypointense on T2-weighted MR images and were hypointense to isointense on T1-weighted sequences and suggested that MR features of an intracranial aspergilloma are characteristic enough to initiate empiric antifungal therapy without microbiological confirmation of the diagnosis, prior to definitive surgery. While this strategy might be acceptable as an interim measure prior to surgery, imaging diagnosis should not be considered as a replacement for pathological or microbiological diagnosis as anti-fungal agents are generally toxic and should not be administered on a long-term basis to any patient without definitive diagnosis of a fungal infection.
As the imaging features of IFM are non-specific, several differential diagnoses are generally considered prior to surgery except in patients with easily identifiable risk factors. The commonly considered imaging differential diagnoses are tuberculomas, metastasis, lymphoma, glioma and meningioma if the mass is dural based. In the case of rhino-cerebral disease a common differential diagnosis would be sinonasal malignancy.
Classification of IFMs
Based on the presence or absence of the involvement of the paranasal sinuses (PNS), IFMs can be classified into 1. Rhinocerebral or sinocranial group (when PNS disease is identifiable on the CT/MR imaging); or 2. Primary intracranial group (when PNS disease is absent). Primary intracranial IFMs can be further classified as a. Extracerebral (extra-axial); or b. intracerebral (intra-axial) group based on the relationship of the IFM to the brain parenchyma. [2] The rhino-cerebral form of the disease is the most common presentation of IFMs and accounts for 40 to 80% of most large series of IFMs from India. [1],[2],[3],[4],[5],[6] Although in patients with the extracerebral form of the disease, no PNS involvement is evident on initial imaging, this may become manifest later in the course of the disease. [1],[2],[4] It is therefore possible that even at initial presentation PNS involvement was present but occult.
The rhinocerebral form of the disease presents most often in the anterior skull base or the sellar and parasellar regions. If the focus of infection is in the mastoid air cells then the spread of the disease is to the petrous bone and subsequently to the middle or posterior fossa. The commonest location for a primary intracranial IFM is the supratentorial compartment with the majority of lesions being present in the frontal lobes. There are two reasons for the predilection of the frontal lobes for IFMs. First, the frontal lobes account for nearly a third of the cerebral hemispheres and hence receive a major portion of the blood supply to the brain and second, the frontal lobes being in close proximity to the frontal and ethmoidal PNS present an obvious target for the spread of infection from the sinuses. The other common location for an IFM is the temporal lobe. Because of its proximity to the
petrous temporal bone fungal infections from the mastoid air cells can spread to the temporal lobe. Kumar et al. [23] reported one patient with an IFM in the lateral ventricle, this location being extremely rare.
The posterior fossa structures are very infrequently involved especially by isolated infections and may only be occasionally involved when there are several IFMs. Mastoid sinus fungal infections can, however, spread to the cerebellar hemispheres through contiguous spread. In their series of 25 patients with craniocerebral aspergillomas, Siddiqui et al , [12] did not have a single patient with a posterior fossa lesion. Dubey et al , [1] who reported one of the largest series of IFMs with 40 patients, did not have a single patient with a posterior fossa lesion. In the series of IFMs reported by Sharma et al. , [2] five of the 32 patients had posterior fossa lesions (three in the cerebellopontine angle and two in the cerebellum) but all of these lesions were in association with either parasellar or temporal lobe fungal masses and were not seen in isolation. Therefore, isolated cerebellar fungal masses are rare and may not be suspected pre-operatively.
The consistency of the IFMs differs based on the type of cerebral involvement. [2] In the rhinocerebral form, the IFMs are firm to hard in consistency and are difficult to cut into. On the other hand, the IFMs in the intracerebral form of the disease are soft and suckable and may have pockets of pus within them. This difference is also evident in the pathological examination with marked fibrosis being a prominent feature of the rhinocerebral form of the disease. [3]
Fungal aneurysms are rare entities with only about 15 cases reported till 2001. [14] Most of the these aneurysms involve the proximal intracranial vessels typically involving the intradural portion of the internal carotid artery. They are fusiform and involve longer segments of the artery when compared with bacterial aneurysms which are globular and small. [14] They result from invasion of the vessel wall either from hematogenous spread of infection or direct invasion of the vessel wall from outside.
Surgical management
Surgical management of IFMs is primarily directed at achieving a definitive diagnosis but may involve other objectives as detailed below. Whatever surgical approach is used, there should be a high index of intra-operative suspicion of a fungal etiology for an inflammatory mass. Only with this approach will the tissue be sent for fungal cultures. If this opportunity is missed then the diagnosis might become doubtful and exact speciation will be impossible even if fungal hyphae are recognized in the histopathological samples.
Stereotactic procedures
Stereotactic biopsy/aspiration is resorted to when the IFM is deep seated (e.g. ganglionic, brain stem, thalamus), located in an eloquent region of the brain (e.g. motor regions) or when the masses are multiple and the object of surgery is to arrive at a diagnosis and obtain pus/tissue for culture studies. Although the procedure only achieves a diagnosis and obtains tissue/pus for microbiological studies, there are reports of successful management of patients with IFMs using stereotactic biopsy/aspiration along with appropriate medical therapy. [24],[25],[26],[27],[28] It is suggested that both the periphery and the center of the mass be targeted as the fungal hyphae may only be present in the periphery of the mass. [12] Stereotactic procedures are, attractive as they are minimally invasive procedures and are especially appropriate in those patients with IFMs whose general condition precludes major cranial surgery. Stereotactic biopsy/aspiration can be performed under local analgesia in most adults and thus helps avoid the additional morbidity of general anaesthesia in moribund patients. [27] Stereotactic craniotomies might also be done in patients with IFMs to reduce the morbidity of a craniotomy procedure and shorten the duration of the surgery. [29]
Amphotericin can be injected directly into the IFM and has been reported to provide a better outcome in isolated cases. [30] Ommaya reservoirs may be placed stereotactically into IFMs and amphotericin B can be injected directly into the IFM.
[31] This has been reported to yield good outcomes in isolated cases. The rationale for local therapy with amphotericin B is that it avoids the high systemic toxicity of the drug and also bypasses the blood brain barrier. [12],[13]
Craniotomy
Open craniotomy is performed for suspected IFMs that are in relatively accessible regions of the brain and when it is perceived that a radical excision is feasible and safe. Open surgery is also done often when the diagnosis of IFM is not suspected eg. when the mass is present in the subfrontal region and an imaging diagnosis of an olfactory groove meningioma is made. Radical excision of the IFM can rapidly reduce the mass effect and might improve penetration of the antifungal agents into the infected tissue. [2] While it is generally agreed that aggressive surgical management of IFMs leads to a better outcome, [1],[2],[4],[6],[13],[28],[29],[31],[32] radical surgery might not be feasible due to the location of IFMs in eloquent regions of the brain or not advisable in some patients due to their poor general condition. Siddiqui et al. [12] suggested that a less than radical approach should be taken in the surgical management of IFMs. The author would not advocate the use of radical approaches such as skull base approaches to excise IFMs as these procedures are associated with higher morbidity even in otherwise well-preserved patients. From the literature, there is no conclusive evidence that radical and aggressive surgery improves outcome in patients with IFMs but a reasonably radical approach would be advisable whenever it is feasible without severe morbidity or additional neurological deficits. In some patients, repeated craniotomies are required to eradicate residual or recurrent disease. [2] Local antifungal therapy with amphotericin B soaked in gelatin sponge has been used successfully in a patient with an IFM, following open surgical debridement. [33]
Shunt surgery
Hydrocephalus that develops in some patients with IFMs requires the placement of a ventriculoperitoneal (VP) shunt. Several authors have documented the need for VP
shunts in patients with IFMs either as primary procedures or as a secondary procedure when patients with IFMs on medical therapy develop hydrocephalus. [1],[2],[5],[12],[13],[31] It is presumed that hydrocephalus in these patients is the result of arachnoiditis of the basal cisterns producing a communicating type of hydrocephalus.
Management of fungal aneurysms
There are reports of clipping of fungal aneurysms. [1],[2] More recently endovascular techniques have been used to obliterate these aneurysms. [14] However, the ultimate outcome for patients with fungal aneurysms is poor and almost uniformly fatal. [14]
Surgery for PNS disease
Whenever IFMs are associated with PNS disease, surgical eradication of the PNS disease should be attempted. In recent years, functional endoscopic sinus surgery (FESS) has been the mainstay of PNS surgery and is used frequently in the radical excision of fungal disease in the PNS. [12] Besides removal of the diseased mucosal tissues, FESS also restores the aeration of the sinuses which in itself prevents reestablishment of the fungal infection in the PNS.
Antifungal Therapy
As antifungal therapy including the dose and duration of antifungal therapy will be discussed in a separate article, only some relevant aspects of the medical management of IFMs will be discussed here. Amphotericin B remains the mainstay of
therapy in patients with IFMs. Due to its high systemic toxicity, patients undergoing therapy with amphotericin B require careful monitoring. Liposomal amphotericin B is a safer alternative with lower toxicity but is very expensive and many patients in our country might not be able to afford the drug. Oral antifungal agents such as flucytosine and itraconazole might be used in the long-term maintenance therapy. It has been suggested that itraconazole administered pre-operatively for a week might improve outcome in patients with IFMs. [12] Patients undergoing transplant procedures who are at high risk for developing IFMs might be given a trial of prophylactic amphotericin B but whether this strategy is effective in preventing IFMs is still unclear. [8]
Prognosis and Outcome
High mortality and morbidity have been uniformly reported in almost all series of patients with IFMs. The mortality rates range from around 40% in immunocompetent patients to 92% in transplant recipients. Unfortunately, newer drugs and more aggressive surgical procedures have not made a significant dent in the mortality and morbidity rates of patients with IFMs. Young et al. [31] reported a mortality rate of 43.6%; it was higher when the diagnosis was delayed (64%) and lower if the diagnosis was made early and treatment initiated promptly (39%). A mortality rate of 63% was reported by Dubey et al. [1] in their series of 40 patients with IFMs. Two-thirds of their patients had predisposing illnesses (diabetes, tuberculosis, renal transplant, lymphoma and HIV infection). Mortality in immunocompetent patients with intracerebral aspergillosis was 66.7% in the series reported by Siddiqui et al. [12] Jamjoom et al. [13] and Sharma et al. [2] reported a mortality of 41% and 50% respectively. Rhinocerebral mucormycosis has a high mortality associated with it. In immunocompetent patients, the survival is 75% but it decreases to 60% in patients with diabetes mellitus and to only 20% in those with other systemic disorders. [34]
Prognosis for IFMs is better in patients who are immunocompetent as opposed to those who are immunocompromized. In immunocompromized patients, the prognosis depends largely on the control of the underlying condition and not on the IFM alone. Patients with the rhinocerebral form of the disease have a better survival than those with the primary intracranial form. The longer survival, however, is associated with significant morbidity.
The other major cause of mortality and morbidity is the involvement of major cerebral blood vessels by the fungi leading to major strokes. Vasculitis seems to be a frequent sequel to surgery for IFMs in the skull base region and several authors have recorded mortality due to stroke following surgery for such lesions. [2],[6],[12],[13] For some reason, patients who undergo surgery for IFMs, even distant from the skull base, seem to be at risk for the development of arteritis and subsequently develop morbidity due to the cerebral ischemia.
One of the major reasons for poor outcome in immunocompetent patients with IFMs is the delay in diagnosis. Several patients with primary intracranial IFMs in India are treated with empiric anti-tuberculous therapy (ATT) on the basis of an imaging diagnosis. [1],[2] This causes a delay of eight to 12 weeks in most patients as a repeat imaging is performed only after this interval and a possibility of a misdiagnosis recognized when the intracranial mass is not responding to ATT. Hydrocephalus due to a fungal infection can be misdiagnosed as being due to tuberculous meningitis and treated with empiric ATT after a VP shunt. Mehta et al. [5] reported such a patient in whom the diagnosis of a fungal meningitis was only made post-mortem.
Finally, some of the mortality and morbidity in patients with IFMs is also attributable to the antifungal agents. Amphotericin B is notorious for causing renal and liver failure and has other serious side effects.
Conclusions
Intracranial fungal masses are uncommon lesions in most neurosurgical centers but are being increasingly diagnosed in not only immunocompromized but also immunocompetent patients especially in India. There should be a high index of suspicion for these lesions and whenever an inflammatory mass is encountered at surgery, the tissue from the intracranial mass should be subjected to fungal cultures in addition to cultures for bacteria. Stereotactic procedures might yield a good outcome in selected patients but whenever feasible safe radical excision of the IFM along with normal nervous tissue around it should be done. Medical therapy with antifungal agents is required for prolonged periods following surgery in patients with IFM. In spite of several advances in imaging and surgical techniques and the advent of some newer antifungal agents, the prognosis for patients with IFM continues to remain grim and mortality rates range between 40 and 90%. In immunocompromized patients with IFM the mortality rates are very high and the control of the underlying condition usually determines the outcome in these patients.
e 21, Issue 4, pp 293-318 Fungal Infections of the CNS Dr Katharine E. Black, Lindsey R. Baden Infections with fungi cause significant morbidity in the immunocompromised host and invasion of the CNS may lead to devastating consequences. Vulnerable individuals include those with haematological malignancies, transplant recipients, and those infected with HIV. Potential pathogens include yeasts, Aspergillus spp., other moulds of an increasing variety, and a range of dimorphic fungi, often associated with particular geographical locations. Antifungal treatments include polyenes such as amphotericin B and its lipid formulations, azoles such as fluconazole and itraconazole, and the more recent voriconazole and posaconazole. The new antifungal class of echinocandins, such as caspofungin, micafungin and anidulafungin, typically
lack CNS penetration. Amphotericin B and flucytosine are used to initiate treatment for CNS yeast infections caused by Candida and Cryptococcus neoformans. Voriconazole is preferred for aspergillus, although amphotericin B, particularly in lipid formulation, is also useful. Reliable treatment data are lacking for CNS infections with most of the non-aspergillus moulds; posaconazole holds promise for the zygomycetes and perhaps some of the rarer pigmented fungi, but amphotericin B preparations are still recommended. Oral fluconazole is effective for the CNS manifestations of coccidioides, while histoplasmosis and blastomycoses typically require amphotericin B therapy. Effective treatment requires a definitive diagnosis, which is often challenging in the population at risk of CNS fungal infections.
Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario
SK Shankar1, A Mahadevan1, C Sundaram2, Chitra Sarkar3, Geeta Chacko4, DN Lanjewar5, Vani Santosh1, TC Yasha1, VV Radhakrishnan6 1 Department of Neuropathology, National Institute of Mental Health and Neurosciences, Bangalore, India 2 Department of Pathology, Nizam's Institute of Medical Sciences, Hyderabad, India 3 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India 4 Department of Pathology, Christian Medical College, Vellore, India 5 Department of Pathology, Grant Medical College and Sir JJ Group of Hospitals, Mumbai, India
6 Department of Pathology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvanathapuram, India
Date of Acceptance Correspondence Address: S K Shankar
07-Jul-2007
Department of Neuropathology, National Institute of Mental Health and Neurosciences, Bangalore - 560 029 India
8 2
DOI: 10.4103/0028-3886.35680
PMID: 17921648
Abstract Ubiquitously present fungi in the environment find a nidus in the human body and adopt its metabolic machinery to be in symbiosis or become pathogenic. Immunocompromised states like human immunodeficiency virus (HIV) / acquired immunodeficiency syndrome (AIDS), systemic neoplasia and organ transplantation have enhanced the frequency of fungal infections. High-risk behavior, IV drug abuse
and air travel have led to the emergence of new fungal infections hitherto geographically localized. The pathology in the central nervous system (CNS) is dictated largely by the size of the fungus - the yeast forms, by virtue of their small size enter the microcirculation to cause meningitis and microabscesses, while hyphal forms invade the vasculature to manifest as large pale or hemorrhagic infarcts. The growth kinetics of fungi, the antigenic character of the capsule. the proteases secreted by the mycelial forms and the biochemical milieu in the host also determine clinical manifestations. A hospital-based analysis of the available information from India suggests that in the non-HIV patient population, hyphal forms like Aspergillosis and Zygomycosis are the most common pathogens, while yeast forms like Cryptococcus and Candida are the prime pathogens in cases of HIV/AIDS, the altered macrophage function acting in synergy with suppressed cell-mediated immunity. In Northeastern states, systemic infection by Penicillium marneffei is reported in association with HIV though CNS involvement is not recorded. Although fungal infections of the CNS are reported from various hospitals in India, studies are limited by non-availability of relevant microbiological studies and the reported prevalence data is biased by the surgical practices, availability of postmortem and microbiology and laboratory support. Detailed clinical and mycological investigations related to the interaction between the fungus and host environment is a fertile area of research to understand the basic pathogenetic mechanisms.
Keywords: Aspergillosis, central nervous system, cryptococcosis, dimorphic fungi, mycotic infections, pathogenesis, penicilliosis, pheohyphomycosis, zygomycosis
How to cite this article: Shankar S K, Mahadevan A, Sundaram C, Sarkar C, Chacko G, Lanjewar D N, Santosh V, Yasha T C, Radhakrishnan V V. Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurol India 2007;55:198-215
How to cite this URL: Shankar S K, Mahadevan A, Sundaram C, Sarkar C, Chacko G, Lanjewar D N, Santosh V, Yasha T C, Radhakrishnan V V. Pathobiology of fungal infections of the central nervous system with special reference to the Indian scenario. Neurol India [serial online] 2007 [cited 2013 May 7];55:198-215. Available from: http://www.neurologyindia.com/text.asp?2007/55/3/198/35680
Fungi are ubiquitous in nature, but the distribution of fungal infections in a community depends on the environment, the climatic conditions, socioeconomic status of the human hosts, their habits and genetic factors. The ability of fungi to adapt to the elevated body temperature and reduced redox state of the tissues and overcome defense mechanisms of the human host alone can cause disease of varying severity. In the soil they are saprophytes producing mycelia and airborne conidia. Normally fungal infections are of low virulence and confined to local infections. In immunocompromised states, however, the same fungus tends to produce invasive infection with devastating consequences. Certain body sites like the brain and meninges are preferentially invaded by specific groups of fungi like Cryptococcus , Candida species. Patients with the acquired immunodeficiency syndrome (AIDS) appear to be more prone to infections by Candida , Cryptococcus , Nocardia, Histoplasma and Pneumocystis carinii while aspergillosis is uncommon. In cases of hematological malignancies, solid organ transplantation, renal failure or autoimmune disorders with prolonged steroid therapy, candidiasis and aspergillosis are common. This reflects the preferential selectivity of the fungus for host metabolic state and immune status favorable for survival and growth. A wide variety of fungi now isolated from neutropenic patients like Pheohyphomycetes , Trichosporum and Penicillium marneffei were not recognized as human pathogens before. Some of the fungi like coccidioidomycosis and histoplasmosis show gender preference, the chronic progressive disease being more common in males. In pregnant women the dissemination rate is equal to or exceeds that in males, reflecting the hormonal influence on the growth of fungi. Worldwide travel has increased the exposure of many communities to formally geographically limited fungal infections.
Fungi like Blastomyces dermatitides, Paracoccidioides brasiliensis, Pseudoallescheria boydii and Coccidioides immitis are capable of eliciting disease in the absence of known predisposing factors and are hence labeled pathogenic fungi. It is essential to realize that any fungus is potentially a central nervous system (CNS) pathogen and patients with fungal infections have some degree of immunosuppression. Classification as pathogenic and opportunistic fungi is more for ease of understanding of the pathology as overlap in pathogenesis and invasive patterns exists in both forms.
The morphology and size of the organism determine the evolution and phenotype of CNS lesions. The small yeast forms, up to 20 m in diameter ( Blastomyces , Coccidioides , Paracoccidioides , Sporotrichum , Histoplasma , Cryptococcus and Candida ) reach the small arterioles and capillaries producing leptomeningitis and subpial ischemic lesions as they have access to the microcirculation from which they seed the subarachnoid space. Intermediate-sized pseudohyphae such as those of Candida occlude small vessels in the microcirculation to produce local areas of tissue necrosis that transform into abscesses. The large hyphal forms of variable size (Septate- Aspergillus , Cephalosporium , Cladosporium etc; non-septate- Zygomyces ) obstruct large and intermediate size arteries and occasionally veins, giving rise to large infarcts. Routine histology, special stains and morphological characteristics indicate the type of fungus, but speciation needs culturing and biochemical characterization. Tissue fungal infection burden of less than 10 CFU/gm of tissue usually proves to be histologically negative. [1]
The phenomenon of resistance to fungal infection is poorly understood and most of the data available is extrapolation from animal models. Immunity to fungal infections is related to the tissue reaction elicited by the fungi and their products. [2],[3],[4] Unlike superficial fungi, the deep mycosis has diverse antigens with different activities. Fungi like Histoplasma and Blastomyces exist as dimorphic forms having different antigens, (H and M antigens) each specific in their molecular features and pathogenic potentials. [5],[6],[7] Humoral responses are induced by producing circulatory antibodies to polysaccharides and glycoprotein fractions of the fungal cell wall. The quantitation of the circulating antibodies does not reflect the immune status of the individual and are not protective. In some, profound antigenemia can be
found instead of antibody response indicating deficient/indifferent humoral immunity to the antigen. The fungal antigens are highly cross-reactive with even quite unrelated fungal antigens. [5],[8] In deep tissue mycosis, the antigen of the infective yeast is quite different from that found in cultures with spores and mycelium. Both humoral and cell-mediated immunity take part to contain the fungus and a high degree of overlap in immune response is exhibited. The immunity against fungi is not long-lasting unlike in bacteria and viruses, the antigenic potential being variable, highly nonspecific and relatively poor to elicit response. This makes the host prone for reinfection by the same fungus at the previously infected site, despite healing of the existing infection in the individual.
Nonspecific (innate) defense mechanisms to fungal infections include skin and mucosa behaving as mechanical barriers and cytokines facilitating emigration of phagocytic cells (polymorphs and macrophages) to ingest and destroy the microbes. Neutrophils, the first line of defense against microbes are short-lived cells that have powerful antifungal and bactericidal mechanisms. Macrophages are long-lived and form the first line of defense against inhaled microbial pathogens, like Aspergillus spores. T lymphocytes in conjunction with macrophages are important in conferring specific resistance to fungal infection.
Fatal fugal infections are uncommon among patients with intact immunological defense and are caused by restricted number of 'pathogenic' fungi. In immunocompromised patients, the protective mechanisms are deficient or absent making them prone to infections from saprophytic fungi that are generally nonpathogenic in immunocompetent hosts. Disseminated and progressive infection caused by Penicilliosis marneffei is an emerging opportunistic infection in AIDS patients and is endemic in Southeast Asia and Southern China.
The following presentation centers more on the patholobiology of common fungal infections of CNS relevant to India while rare and emerging fungi invading the brain are dealt with briefly. Though fungal infections of the nervous system are reported from various centers in India [Table - 1], the studies are limited by non-availability of relevant mycological studies. The prevalence data of fungal infections from
various centers [Table - 1] is to a certain extent biased because of the surgical practices and limited availability of postmortem studies. In view of the large number of autopsies from AIDS cases, the National Institute of Mental Health and Neurosciences (NIMHANS) at Bangalore has the highest number of cases of cryptococcosis followed by aspergillosis. On the other hand, academic institutions from Hyderabad, [9] Chandigarh [10] and Bangalore reported large series of aspergillosis derived from surgical material. The low numbers of cryptococcosis reported by other centers may therefore not be a true reflection of low prevalence. The advent of organ transplantation with immunosuppressive therapy and HIV/AIDS has altered the prevalence data of systemic fungal infections in many centers reflecting the vulnerable population than changes in the environmental ecosystems. Newer forms of fungal infections are emerging as a result of global travel.
Cryptococcosis
Cryptococcosis is a deep visceral, systemic cutaneous mycosis with reports from worldwide and in all races. Male predominance can be explained partly by greater outdoor exposure and partly by the fact that hormonal, estrogen inhibits the growth of Cryptococcus . [11] For reasons not clear, person to person transmission of this illness is not reported. More than 50% of patients with disseminated disease are immunocompromised. On the other hand, patients with cryptococcomas, a granulomatous mass lesion, are not immunocompromised. Patients with AIDS or other immunocompromised states are almost exclusively infected with C. neoformans variety neoformans (Serotypes A,D, A/D) while C. neoformans var gatti (Serotypes B and C) has a propensity to cause disease in immunocompetent hosts, suggesting that genetic and phenotypic differences are responsible for the different severity of the disease. [12],[13]
The fungus is most frequently isolated from pigeon droppings, but also from soil, wood and trees. [14],[15] Cryptococcus var gatti is mostly limited to tropical and
subtropical regions. Molecular epidemiology of C. neoformans has revealed genetic variation between isolates. High degree of heterogeneity is noted among isolates from USA, while isolates from most areas of the world, including Australia, show limited genetic diversity, with possible clonality. [16],[17],[18]
Cryptococcus produces capsular antigen glucoronoxylomannan in large quantities, which is heat-stable and pronase-resistant and its half life is 24h. [19] False positive tests by latex agglutination tests (RPLA) for cryptococcosis may occur by crossreactivity with heat-stable components of Trichosporon bigelii , malignancy, septicemia and contamination of talc from latex gloves into cerebrospinal fluid (CSF). [20] Non-capsular exoantigens from both encapsulated and unencapsulated isolates of C. neoformans like species-specific 34-38 kDA glycoprotein [21] and 115 kDA exoantigen react strongly with sera of patients with cryptococcosis and are thus useful in diagnosis of cryptococcosis in AIDS patients. [22] Antigen titer levels in HIV patients with cryptococcal infection remain elevated for a longer time and these patients may require a longer duration of treatment.
Majority of C. neoformans isolates identified before AIDS epidemic in Thailand belonged to Serotype B and C ( C. neoformans var gatti ) while most of the isolates now are Serotype A and D ( Cryptococcus neoformans var neoformans ). In contrast to relatively uniform colony characteristics of Candida species, variation in colony characters has been reported in cases of cryptococcosis. Melanin positive cryptococci are pathogenic while melanin negative albino isolates are considered nonpathogenic. [23] However, Banerjee [23] isolated melanin negative albino strains and melanin positive and negative strains of C. neoformans ( var grubii ) in patients with HIV, suggesting a molecular genetic variation. Most of the isolates from HIV positive patients from India are serotype A, var grubbi . In a study by Rajendran et al. from south India [24] of the 12 isolates from HIV positive individuals, 10 were VNI (Serotype A) molecular type. In previous studies in immunocompromised patients, strains of variety neoformans , particularly Serotype A were isolated. [23] Identification of var gatti is essential as this variety is relatively refractory to treatment and needs prolonged or increased dose of antifungal therapy and shows long-term sequelae.
Most commonly Cryptococcus initiates as a primary pulmonary infection. Approximately 5-10% of HIV infected patients develop cryptococcal meningitis (CM) as an AIDS defining illness [25] and in about 40%, it may be the initial manifestation. [26] Of the 588 patients with HIV/AIDS analyzed (1990-2002) at NIMHANS, Bangalore, south India, cryptococcosis was the opportunistic infection in 25% and cryptococcosis and tuberculosis with coexisting toxoplasmosis in 12% (Satishchandra P, Unpublished data). A clinical study from western India reported cryptococcal meningitis in 67.4% of cases. [27] In an autopsy study of 134 cases of HIV/AIDS from NIMHANS between 1990-2004, cryptococcal infection accounted for 31.3% of monomicrobial infections, toxoplasmosis for 20.8% and tuberculous meningitis for 20.1%. [28] This discrepancy between clinical and autopsy data may be related to misdiagnosis of systemic cryptococcal infection as tuberculous infection because of close clinical and radiological similarities and also tuberculosis being highly endemic in India. It is likely that cryptococcal meningitis in cases of HIV could be reactivation of the dormant lesion in the lung similar to Ghon's focus of pulmonary tuberculosis. The systemic infection of Cryptococcus from the primary pulmonary and cutaneous focus is essentially hematogenous. The spread to the brain most often results in leptomeningitis similar to tuberculosis. CSF low in complement and immunoglobulins facilitates establishment of infection in the basal meninges and choroid plexus. Cryptococcal CNS infections can be meningitis, meningoencephalitis or rarely cryptococcomas, as localized granulomatous masses. Cryptococcosis in childhood AIDS has been diagnosed more frequently than in pre-AIDS era. [29]
Grossly, the pathological lesions can be minimal and overlooked, mistaking the slightly opaque meninges as pooling of CSF in subarachnoid space [Figure - 1]A. On occasion, small nodules 2-3 mm in size, adjacent to the vessels on the surface may be seen, mistaken for tuberculous lesion. Cryptococcal meningitis tends to be subacute or chronic and may be associated with hydrocephalus in patients with longer survival due to chronic fibrosing leptomeningitis along the base. In less than 10% of cases, one finds multiple, cystic, non-granulomatous, mucoid intraparenchymal lesions in the basal ganglia [Figure - 1]B, thalamus, cortical ribbon and ventral brainstem, suggesting hematogenous spread of the fungus and entrapment around the endarteries of the pial, lenticulostriate and thalamostriate vessels. Rarely, large
demyelinating lesions resembling demyelinating plaques on imaging and gross pathology, are seen, reflecting dispersal of the organism along the medullary arteries and veins traversing the white matter following blockage of the superior sagittal sinus. In rare instances in immunocompetent individuals, masses of fungi aggregate in granulomatous exudate producing firm, dry mass lesions in the parenchyma, ependymal surface or choroid plexus.
Histologically, the tissue reaction in cryptococcosis is variable. In meningitis the subarachnoid space is widened by the cryptococci floating in pools of mucin, aggregating around the vessels, but rarely found in the lumen or the vessel wall. The inflammatory reaction is minimal constituted by lymphocytes, plasma cells and foamy histiocytes, which have ingested the organisms. In the gelatinous cystic lesions the neuropil is pushed around the cavity filled by a colony of organisms, usually around a vessel visualized as hypodense areas of widened Virchow Robin space on magnetic resonance imaging (MRI). Gliosis and inflammatory components are conspicuous by their absence in the cystic lesions and when present, the cellular response is restricted to sparse foamy histiocytes.
In case of cryptococcomas, the mass is discernable on imaging. These form circumscribed masses with tiny cystic spaces along the margin [Figure - 1]C or lobulated septate mucoid masses with variable number of giant cells containing the yeast forms devoid of their capsule and zones of necrosis. Rarely, one may find granulomatous arteritis, resembling tuberculous pathology, but PAS stain unmasking the organism in giant cells [Figure - 2]A-E. The giant cell response is prominent in immunocompetent hosts [Figure - 2]D while in immunocompromised hosts as in HIV/AIDS, the immune response is poor and numerous extracellular yeast forms floating in pools of mucin are seen in the subarachnoid [Figure - 2]E and Virchow Robin spaces within the parenchyma.
The polysaccharide capsule sensitive to hyalase, is essential for virulence, inhibiting phagocytosis and antigen presentation. The polysaccharide antigen released during the infection, may spread in the interstitial space of the nervous system and depress the function of immune effector cells, inhibit leukocyte migration, elicit
suppressor responses, resulting in antibody unresponsiveness and facilitate invasion of T lymphocytes by the HIV virus. Radhakrishnan et al ., [30] demonstrated in an in vivo experimental study that hyaluronidase administration depolymerizes the capsular mucopolysaccharide and elicits a granulomatous response. In addition, endogenous nitric oxide (NO) produced by macrophages and activated astrocytes (activated by IL-1 produced by activated microglia and IFN by T cells) inhibit the growth of cryptococci in vitro . The role of this mechanism in vivo is unclear, especially in the absence of reactive astrocytosis in the CNS lesions. The paucity of inflammation and compression of the vessels in the cystic lesions accounts for relatively nonspecific imaging findings except for widened Virchow Robin spaces. Severe headache and elevated intracranial pressure without accompanying hydrocephalus or cerebral edema are reported in more than 50% cases of cryptococcal meningitis in association with HIV infection. [31] A preliminary pathological study of the brain and the dural venous sinuses in our autopsied cases revealed plugging of the arachnoidal villi by myxoid capsule-rich cryptococci, at places almost occluding the venous sinuses. [28] Lee and colleagues by immunohistochemistry showed tissue deposits of capsular antigen dissociated from the organisms. [32] This obstruction to venous drainage and impedance to CSF circulation could be leading to 'dynamic hydrocephalic attacks' unrecognized on cranial computerized tomography scan or MRI in the majority of instances. Relief obtained by draining off the CSF gives further credence to the idea of dynamic hydrocephalus. Poor CSF inflammatory cell response, positive culture of cryptococci from extraneural sites and systemic dissemination were found to be common in association with HIV and indicated poor prognosis. [33]
Cryptococcus neoformans infection though has significant affinity for CNS, rarely results in infarction. Till date six known cases of cerebral infarction and two cases of transient neurological deficit related to cryptococcal meningitis in HIV infected individuals have been reported. Tjia et al. , reported 4% incidence of cerebral infarction secondary to cryptococcal meningitis in HIV seronegative patients. [34] Evidence of arteritis on angiography has been observed in a patient with cryptococcal meningitis. Cryptococcal vasculitis in chronic cases, immune-mediated vasospasm and dilated ventricles stretching the already compressed vessels in the parenchyma by the cryptococcal deposits have been considered as the pathogenetic
events leading to infarcts. [35] A case of verterbrobasilar stroke presumably caused by basilar artery occlusion by cryptococcal infection has been described. [36]
With the advent of HAART, the incidence of C. neoformans infection in HIV infected patients has declined and immunocompromised organ transplant recipients are at a higher risk. Hussain et al. reported that transplant recipients receiving tacrolimus were significantly less likely to have CNS involvement and more likely to have cutaneous, soft tissue and osteoarticular involvement compared to patients receiving non-tacrolimus-based immunosuppressive therapy. [18] Tacrolimus, a natural macrolide antifungal agent is toxic to C. neoformans in vitro by inhibiting calcineurin, at 37 o C, but not at 24 o C. Thus temperature-dependent inhibition of cryptococci by tacrolimus which crosses the blood brain barrier may prevent CNS infection, but allow growth of fungus at cooler body sites like skin, soft tissues and bone.
Indian literature [Table - 2]
Cryptococcal meningitis has been reported as the most common opportunistic infection of the CNS in patients with HIV/AIDS in India. [27],[28],[37],[38] It accounted for 2-7% of all opportunistic infections in three large cohorts of HIV patients from Mumbai (4.7-7%), Chennai (2%) and Delhi (3.7%). [39],[40],[41],[42],[43] A review of CNS cyrptococcosis in the Indian subcontinent in 2001 [44] noted peculiarly higher incidence from north India as compared to the south despite high prevalence of HIV in the south as compared to the north Indian states, probably due to under-reporting of cases.
At NIMHANS, cryptococcal meningitis was the most common opportunistic infection in AIDS patients at autopsy [Table - 2] seen in 31.3% of cases. [28] Among the 78 cases of cryptococcal meningitis diagnosed by autopsy/biopsy, Cryptococcus neoformans was the common isolate. In south Indian patients, diagnosis of cryptococcal meningitis was associated with a sevenfold increase in mortality. [39] The mean CD4 count at presentation was 91 cells/l, median survival after diagnosis
being 22 months. In a study that included HIV positive and negative cases, those with HIV had poorer CSF cell response and higher mortality. [33] Other poor prognostic factors identified included altered mental status, positive blood cultures, CSF antigen titer above 1:1024, positive CSF India ink, CSF white cell count below 20 cell/mm 3 and elevated CSF pressures.
Sporadic reports of cryptococcal meningitis in apparently healthy hosts are reported from different parts of India. [45],[46],[47] A single case of cryptococcoma in an immunocompetent host in the absence of cryptococcal meningitis was reported from Mumbai. [48] Besides HIV/AIDS, renal transplantation, diabetes mellitus [47],[49] following long-term steroid therapy for polymyositis [50] and acute lymphoblastic leukemia [51] are emerging as risk factors.
The majority of isolates from HIV positive patients from India are Serotype A var grubbi consistent with the serotype prevalent worldwide [14],[52],[53] and a few reports of var gatti . [54]
Candidiasis
Candida is an endogenous pathogen, its usual habitat being the gastrointestinal tract. Most cases of candidiasis arise in immunocompromised hosts. Phagocytosis is the principal nonspecific mechanism protecting the host against Candida albicans infection. The hyphal form of candida is more pathogenic as it can resist digestion by both polymorphs and macrophages. The Candida albicans mannan is chemotactic to neutrophils and induces complement activation via alternate complement pathway. High incidence of candidiasis is seen in neutropenic patients (cancer patients on chemotherapy), in those with defects in neutrophil/macrophage function (long-term steroid therapy) or depletion of complement (e.g. systemic lupus erythematosis). Role of T-cell mediated immunity in host protection is unclear but is derived from
the knowledge that patients with chronic mucocutaneous candidiasis have functional defects in T-cells. Its role in deep-seated infection is less clear.
Mucocutaneous candidiasis is probably one of the commonest manifestations of HIV positive status worldwide, its reported incidence in India being 50-100%. [55],[56],[57],[58] Common agents isolated from India are C. albicans while C. dubliniensis is one of the important species reported as an opportunistic organism from western countries [59] and is not seen in the Indian HIV positive population. During the past two decades, a significant shift in the epidemiology of candidemia due to different Candida species has occurred, probably related to antifungal prophylaxis. In the 1960s and 1970s Candida albicans accounted for 90% of candidemia, while after 1988 Candida tropicalis, C. parapsidosis, C. krusei and C. glabrata became more frequent. [60],[61] Candida species colonizing mucocutaneous areas as saprophytes may invade the CNS by blood stream infection, following IV administration of therapeutic drugs or IV drug abuse or during open heart surgery. A wide variety of conditions like prolonged antibiotics, steroids, immunosuppressive agents, chemotherapeutic treatment, indwelling catheters, parenteral nutrition, abdominal surgery, burns, malignancies, neutropenia and HIV/AIDS promote hematogenous spread. [62],[63] Candida meningitis can manifest spontaneously as a complication of accidental inoculation during neurosurgery, [64] head injury [65] or ventriculostomies, [66] the severity dictated by the dose of inoculum. [67]
The involvement of the CNS is in the form of microabscesses, usually in the territory of the anterior and middle cerebral arteries. [68] With occlusion of small vessels by the pseudohyphae, colonies of yeast enmeshed in fibrin and acute polymorph reaction may present as small hemorrhagic infarcts, progressing to microabscess and later granulomatous reaction. On histology, unless suspected and looked for, the Candida organisms may be overlooked.
Candida cell wall mannans (carbohydrate homopolymer with mannose and small amount of protein and phosphate) is a heat-stable antigen, resistant to cooking, protease treatment and acidic pH. The greatest limitation of mannan detection for diagnosis is the transient antigenemia [69] and binding of mannan to immune complexes.
Presence of candidal cytoplasmic enzyme, enolase (48kDa) appears to be a marker for deep tissue invasion even in the absence of detectable fungemia, especially hepato-splenic candidiasis. [70] Aspartyl protease is an important virulence factor expressed by invading C. albicans allowing penetration of the anatomical barrier and escape from phagolysosomes. [71] Development of diagnostic tests based on protease detection is of limited value as different species of Candida secrete antigenically distinct proteases.
Indian literature
Indian literature on CNS candidiasis is sparse. Sundaram et al. [9] reported six patients [Table - 1] while Radhakrishnan and co-workers reported two patients presenting with multiple intracerebral abscesses [72] and neither had any detectable form of immunocompromised state. In a study from Indore, examining the causes of fungal meningitis in HIV positive and negative subjects, candida was found to be second most common cause of fungal meningitis in both groups after cryptococcal meningitis. [49] In the HIV negative group, diabetes, renal transplantation and small for date and premature neonates have been recognized as causes of immunosuppression. At NIMHANS, candidiasis was seen as a co-infection with A. fumigatus and Zygomycetes in two cases. Both had uncontrolled diabetes and one had undergone renal transplantation but no case of isolated CNS candidiasis was seen.
Aspergillosis
Aspergillus is a ubiquitous fungus in soil, water, decaying vegetation and organic debris that was first recognized to be pathogenic in humans in 1847, [73] common pathogenic species being Aspergillus fumigatus or Aspergillus flavus . The asexually produced conidia on aerial hyphal stalk are the infective form of the organism that
is inhaled through the respiratory route. Its germination into filamentous forms results in tissue destruction and disease.
The clinical manifestations are produced by both tissue invasion and the host immune response. The first line of cellular defense against conidia that escape entrapment by bronchial mucus are macrophages which ingest the conidia, kill germinating cells and secrete cytokines and chemokines. Alveolar macrophages prevent spores from germinating but are not eliminated. Steroid prevents fusion of phagosome containing aspergillus spores with lysosomes predisposing to profuse germination and dissemination of the infection. Germinating hyphae that escape macrophage surveillance are destroyed by neutrophils and monocytes. Importance of neutrophils in host defense against aspergillus infection is derived from its occurrence in patients with leukemia, neutropenic states and chronic granulomatous disease. Tcells play a role in the resolution of chronic forms by modulating the function of macrophages.
The clinical manifestations and disease severity are dictated by the immunologic state of the patient. Lowered host resistance caused by underlying debilitating diseases such as bronchiectasis, carcinoma, sarcoid and tuberculosis, neutropenia, collagen vascular disorders, organ transplantation, chemotherapy, hepatic failure, disruption of normal flora by use of antimicrobial agents and steroids predispose the patient to colonization and invasive disease. [74],[75],[76],[77],[78],[79],[80],[81]
Infection of the CNS by Aspergillus follows hematogenous seeding (lungs and heart being the most common primary sites) [74],[75] or direct inoculation into the CNS during surgical procedures or spread from contiguous structures like paranasal sinuses, mastoid and middle ear. A spectrum of diseases with more than one pathological process can be present at any given time. The morphological changes observed in aspergillosis of CNS depends on the mode of acquisition, whether by hematogenous dissemination or local spread from contiguous anatomical structures. The former leads to multiple lesions involving the middle or anterior cerebral arterial territory with acute necrotizing and purulent lesions (cerebrovascular aspergillosis). In the latter event, the resultant lesions are chronic granulomas
eliciting dense fibrosis. The infection in the nervous system can be found in the cerebral parenchyma, meninges or the vascular system.
Aspergillus fumigatus is the most common species to cause invasive disease, the variation in epidemiology, pathogenicity and antifungal susceptibility patterns dictating important differences in the clinical manifestations, therapy and outcome of disease caused by the Aspergillus species. Aspergillus flavus has been implicated as the cause of a large proportion of paranasal sinus infections [82] and Aspergillus nidulans in chronic granulomatous disease. Acquisition of the type of organism also differs with the environmental source, for instance Aspergillus niger , a frequent colonizer of the gastrointestinal tract is recovered from hospital water distribution systems [83] while A. terreus is acquired through nosocomial exposure to plants. [84] Aspergillis terreus though an uncommon cause of invasive disease, is resistant to amphotericin B and therefore associated with high mortality. [85] Therefore mycological identification of Aspergillus spp. in making therapeutic decisions cannot be overemphasized.
Intracranial aspergillomas are solid, firm intracerebral lesions that exhibit florid granulomatous inflammation without suppuration [Figure - 3]A, B observed in otherwise immunocompetent individuals and those with chronic granulomatous disease, following hematogenous seeding or extension from contiguous paranasal sinuses. The chronic indolent form of paranasal sinus aspergillosis becomes invasive to involve the orbit, base of skull, anterior, middle and posterior cranial fossae and the parasellar regions to produce intracranial granulomas, usually termed the sinocranial or rhinocerebral form. Extension from the sinuses via the orbital apex is the most common route presenting as orbital apex syndrome and radiological abnormalities lead to early biopsy and diagnosis. [86],[87],[88],[89],[90],[91] Vascular invasion is not a prominent feature, hence necrosis is rare and vessels are sclerosed. The pathogenetic mechanism of intense fibrosis has been attributed to 'fumigalin' produced by A. fumigatus . [92] However, most cases of sinonasal aspergillosis are caused by A. flavus that predominates in the nasal polyps and hence pathogenesis of characteristic fibrosis remains obscure.
The frontal and temporal lobes are the most common sites for intracerebral granuloma formation [93],[94],[95],[96] presenting as space-occupying lesions. [87],[97],[98] Those located at the basifrontal or basitemporal regions are invariably mistaken for meningioma or tuberculoma both on imaging and at surgery. The extracerebral variety could represent the rhinocerebral form wherein the paranasal sinus involvement was not detectable at initial presentation but found on MRI or on follow-up scans. The rare purely intracerebral granulomas are those in which no contiguous extension from paranasal sinuses was detectable [98],[99] and the diagnosis is often delayed until histopathology. [100]
An abscess caused by Aspergillus species of fungus contains a central area of liquefactive necrosis surrounded by a wall of hemorrhagic necrosis with acute inflammation interspersed with numerous hyphal elements. Cerebral abscess results from hematogenous seeding in immunocompromised individuals, as in HIV/AIDS, solid organ transplantation, chronic granulomatous disease and patients on corticosteroid therapy.
Cerebrovascular aspergillosis [Figure - 3]C, D, E denotes a well-recognized syndrome of cerebral infarction and necrosis and/or hemorrhage without suppuration resulting from vascular invasion and thrombosis [Figure - 3]C secondary to endovascular infection from a septic embolus or direct invasion of the vessel wall causing vasculitis. Less commonly it can follow meningitis [101],[102] or post-surgical clipping of aneurysms. [103] The ability of Aspergillus spp. to produce enzyme elastase confers direct angioinvasive property to this fungus [92] leading to cerebral hemorrhage or aneurysm formation [Figure - 3]D, E. Inflammatory response is usually scarce, lesions occurring within the territory of affected vessels essentially in the cerebral cortex, subcortical regions and less commonly the brainstem, cerebellum and spinal cord. This form is most frequent in immunocompromised patients with hematopoietic stem cell or solid organ transplants and occasionally following corticosteroid therapy.
Although vascular invasion is common in Aspergillus lesions, true mycotic aneurysms are rare [104] and result from direct invasion of the wall, from the luminal or
adventitial side. In contrast to bacterial mycotic aneurysm, these are fusiform and involve longer and more proximal segments of intracranial vessels like basilar, middle and posterior cerebral arteries. The vessel is friable and infiltrated by hyphae. The lumen may be thrombosed leading to cerebral infarction or may serve as a source of emboli. Isolated meningitis due to Aspergillus spp. is extremely unusual, being more often a complication of other aspergillus-related lesions.
Though Aspergillus has a predilection for the CNS, spinal cord involvement has been reported very rarely. [105],[106],[107],[108] Most cases present as epidural mass or through involvement of thoracic vertebrae to cause cord compression and paraplegia. Upper thoracic level of the spinal cord is most commonly affected, caused by contiguous spread from lung. [107],[108],[109]
Indian literature [Table - 3]
In India, sinocranial aspergillosis accounts for a significant proportion of histologically verified cases reported [10],[96], [110],[111],[112],[113],[114],[115],[116],[117],[118],[119] in otherwise normal hosts in contrast to the disseminated forms that account for the majority of cases from Western countries. [75],[120],[121] Young men, otherwise normal, from rural areas are most commonly affected. [122],[123],[124] Similarly high incidence of fungal keratitis is reported from India in apparently normal hosts. [125] The high incidence of fungal sinusitis and keratitis is related to the spore content of pathogenic Aspergillus spp. in the environment colonizing sinuses, nasopharynx, mastoid and middle ear. In moldy environment, Aspergillus spore concentrations exceeding 12x10 6 m 3 are recorded. [126] Compromised sinus aeration, altered immune response to fungi including poor nutritional status could facilitate growth of the organism and eventual contiguous spread into cranial cavity. [115],[127] Diamond and Bennett observed that though patients appeared free from overt immunological compromise, subclinical impairment of cell-mediated immunity might be present. [128]
Despite aggressive use of amphotericin B and 5-flurocytosine, the prognosis is poor as adequate tissue concentrations may not be achieved as to reach the fungi embedded deep within the tissue. [116],[118] Intracavitary instillation of amphotericin B has been recommended to achieve higher tissue concentrations. [129] Radical surgical debridement is believed to be curative if the extent of surgical resection extends into the uninvolved tissue and can reduce mortality from 64% to 39%. [99],[130],[131] The stress of surgery and steroid therapy to control cerebral edema in the immediate postoperative phase could be contributory factors in the fungal growth.
True mycotic aneurysms caused by direct invasion of Aspergillus hyphae into vessel wall and rupture causing subarachnoid hemorrhage is rarely reported in the Indian literature. [132],[133] The possibility of iatrogenic fungal meningitis with fungi being introduced into the subarachnoid space during spinal anesthesia is suggested in some of the cases. [133]
Other forms of CNS aspergillosis including invasive form, [134] brain abscess [111],[135] are reported rarely from India. Uppin et al. in this same issue report rare occurrence of pale infarcts resulting from angioinvasion and thrombosis. A single case involving thoracic vertebra and forming a paraspinal mass by contiguous extension from pulmonary aspergillosis is reported from Mumbai [136] and two other cases from NIMHANS [111] causing spinal cord compression.
In a large series of 456 samples of Aspergillus spp. cultured from clinical samples, A. flavus (46.93%) was the most common isolate followed by A. fumigatus (37.72%) and A. niger (15.35%). A. fumigatus was the predominant species isolated from the blood and respiratory tract specimens and A. flavus from nasal polyps whereas A. niger predominated in nail specimens. [137]
The high prevalence of A. flavus in nasal polyps could explain the high incidence of the sinocranial form of aspergillosis from India. [116]
Zygomycosis (Mucormycosis)
Zygomycosis is a worldwide polymorphic disease caused by the fungi of the class zygomycetes-order mucorales and entomophthorales. Members of the order mucorales grow profusely on decaying vegetables, seeds, fruits, compost piles, animal excreta and bread rich in carbohydrates. The disease is an opportunistic infection and the distribution of the various clinical forms is based on the predisposing factor rather than on age, gender, race or geography. Zygomycosis is caused by several genera belonging to the family Mucoraceas such as Rhizopus, Mucor and Absidia. Rhizopus is the offending organism in 95% of cases ( Rhizopus arrhizus and Rhizopus oryzae ). The fungus in culture consists of broad, branching, non-septate hyphae measuring 6-15 mm in diameter and up to 200 mm in length, from the base of which root-like structures (rhizoids) grow. From the rhizoids, sprouts (sporangiospores) bearing asexual fruiting heads (sporangia) develop, which are frequently airborne. Some of the major predisposing factors to zygomycosis are: diabetic ketoacidosis, hematological malignancies, neutropenia, immunosuppressive medication, renal failure, bone marrow or solid organ transplantation, septicemia, trauma, burns, starvation, IV drug abuse, premature babies and Hepatitis A - a feature common to the majority of these being high tissue catabolism and ketoacidosis. Rarely, nosocomial infections from contaminated elastoplast bandages [138] and catheters [139] are recorded.
Clinically, the manifestations of zygomycosis are protean but can be classified into six distinct clinical syndromes: rhino-orbito-cerebral, pulmonary, gastrointestinal, cutaneous, disseminated and miscellaneous. [140]
Unlike most other mycoses in which cerebral involvement is secondary to a primary focus in the lung (aerosol entry), this mycosis establishes most frequently from an infection of the facial skin, nasal and paranasal sinus mucosa or nasopharynx and
spreads to the arteries in the rhino-maxillary-orbital territory and the internal carotid artery with eventual thrombosis. The basifrontal area is involved by direct venous invasion through the orbital plate and cavernous sinus [Figure - 4]A. Brain involvement results from hematogenous dissemination resulting in venous thrombosis and hemorrhagic lesions, involving diencephalic areas, usually sparing the infratentorial structures [Figure - 4]B. The main pathological feature of acute invasive cerebral zygomycosis is invasion of the vessels leading to thrombosis and necrosis of the vessel wall, [Figure - 4]C,D the fungus coursing through the lumen. In the chronic invasive form of the disease in immunocompetent individuals, chronic inflammatory exudate is seen admixed with polymorphs and eosinophils as small microabscesses surrounded by epitheloid and giant cells. The hyphal elements coursing through the tissue are surrounded by a eosinophilic sleeve encrusted with polymorphs (Splendore-Hoeppli phenomenon). The fungus is essentially extravascular after it reaches the brain through larger veins or arteries, resulting in hemorrhagic infarcts with cavitation involving the white matter or diencephalic nuclei. Although these fungi have been considered opportunistic, the cerebral form of the disease has been recorded in previously healthy individuals. [141] In diabetic ketoacidosis there is substantially reduced binding of iron to transferrin, leading to freely available iron promoting the growth of Rhizopus oryzae . [142] However, the mechanism of susceptibility to zygomycosis in patients with other predisposing factors is not clear though enhanced metabolism, acidosis and neoglucogenesis could be contributing. Though the fungus readily invades the vessel wall, no definite virulence factor has been identified.
Zygomycosis fungi, though can be cultured easily on routine mycological media, are often difficult to recover from clinical samples, as during biopsy procedure or processing in the laboratory the hyphal elements get damaged and are rendered nonviable. No standard rapid serological method for diagnosis of zygomycosis is available, as unlike other fungi, zygomycosis does not contain D-glucan (DG) cell wall component and is antigenically relatively non-reactive. However, specific antisera produced against hyphal forms are effective in reducing pathology in mice with zygomycosis, suggesting a protective role of humoral response. Interestingly, reports of co-infection with two fungal pathogens along with zygomycete are reported in the literature, indicating pathological succession of the fungal pathogens in the host's necrotizing tissue and emergence of synergistic infections influencing
the clinical course. [143] Although prognosis is considered poor, aggressive surgical debridement and antifungal therapy have increased the survival.
Indian literature [Table - 4]
The largest series of 129 cases of zygomycosis from a single center from India is reported from Chandigarh [144] followed by Nizam's Institute of Medical Sciences (NIMS), Hyderabad and NIMHANS, Bangalore. [145],[146] Rhino-orbito-cerebral type was the most common presentation, uncontrolled diabetes mellitus (50%) being the significant risk factor in the rhinocerebral form. Rhizopus arrhizus was the most common isolate followed by Apophysomyces elegans . A. elegans has been reported only rarely from other centers. [147],[148] Infection of cutaneous and subcutaneous tissue with local invasion to neighboring structures is by far the most common by A. elegans . Weinberg et al. suggested higher isolation of A. elegans from patients living in warm climates as the fungus is a thermophile. [147]
High survival rate of 70.8% was reported by Chakrabarti et al. [144] in the rhinoorbito-cerebral form of zygomycosis following timely medical and/or surgical intervention.
Pheohyphomycosis
This is a term used to describe infections caused by pigmented fungi that contain melanin in their cell walls. These incite a variety of clinical syndromes ranging from subcutaneous nodules to brain abscesses and disseminated disease. The unique feature of this fungal infection is that it causes pathology in immunocompetent individuals. Most species are considered as opportunists though some may be true pathogens.
Agents of pheohyphomycosis that include the genera Cladosporium, Hormodendrum and Phialophora are common saprophytes found in soil and decaying vegetation. They cause a chronic cutaneous mycosis in adult males involving predominantly the lower extremities in agricultural and forest workers walking barefoot and are exceptionally rare in children. Cladophialophora bantiana is the most common species isolated. Interestingly, virulent infections due to Ramichloridium mackenziei have only been seen in the Middle East region and there are no documented survivors till date. [149]
Cerebral pheohyphomycosis arises from an extracranial infected site and spreads to the brain hematogenously. Revankar et al. [149] in their extensive review of 101 cases of primary CNS pheohyphomycosis found that except for one case with contralateral sinusitis, no patient had sinusitis or otitis making local extension unlikely. The hematogenous route is the most likely source of CNS infection from a primary subclinical pulmonary focus or cutaneous lesions. An intriguing possibility of neurotropism is that of metabolic tropism to melanin that may be responsible for CNS localization. Receptors that recognize melanin or its biochemical byproducts could allow these fungi to cross the blood-brain barrier and enter the brain parenchyma. However, human melanin (derived from tyrosine) and fungal melanin (mostly derived from acetate) are different biochemically although they share the same physicochemical properties. This notion is therefore speculative as it does not explain why so few are infected when many more individuals are exposed to this mycosis. Melanin is a known virulence factor in many fungi and has been extensively studied in Cryptococcus neoformans and Wangiella dermatiditis . [150],[151],[152],[153],[154],[155],[156],[157] It is believed to confer protection from scavenging free radicals produced by phagocytic cells in their oxidative outburst that would normally kill organisms. [153] In addition, melanin binds to hydrolytic enzymes thereby preventing their action on the plasma membrane. These multiple functions of melanin, may help explain the pathogenic potential of some dematiaceous fungi, even in immunocompetent hosts.
An unusual manifestation of brain involvement is abscess formation without meningitis. [158],[159] Alternatively, meningitis may be the sole manifestation. [160] The CNS may be the only site of infection as in other mycoses, [161] the frontal lobe being the most commonly involved site. Single or multiple abscesses may enlarge to produce leptomeningitis or ventriculitis. The characteristic brown color of the mycelium can sometimes be recognized macroscopically. [162]
Histologically the lesions are primarily intraparenchymal abscesses. They are larger than the microabscesses caused by pseudohyphae of Candida spp . Granulomatous response has also been described, the fungus located within the giant cells walled in by fibrosis and reactive gliosis. The pigmented fungal hyphae are slender (2-3 m thick) with constrictions occurring at every 3-15 m interval. Sometimes the pigment may not be apparent in stained sections with PAS and methenamine silver. The melanin-specific Masson-Fontana stain has been used to confirm the presence of dematiaceous hyphae in tissues.
Clinical management of these primary CNS pheohyphomycoses is problematic due to their poor response to standard antifungals and mortality rates are high regardless of immune status of the host. Treatment with a combination of Amphotericin B, 5flucytosine and itraconazole was associated with improved survival.
Indian data [Table - 4]
Pheohyphomycosis appears uncommon in India. The largest number of cases is reported from NIMHANS (14 cases, 7.65%). [163] Most presented with cerebral abscesses involving the frontal lobes [Figure - 5]A, although rare presentation with cerebral infarction [Figure - 5]B was also seen. Histology revealed characteristic pigmented hyphal forms with constrictions in the necrotic wall of the abscess or the infarcted tissue [Figure - 5]C. Cladosporium trichoides was the most common isolate. Outcome was uniformly fatal where details were available with no survivors documented [Table - 5]. Four cases are reported from NIMS, Hyderabad (unpublished data) and two cases each from the All India Institute of Medical
Sciences, New Delhi and Christian Medical College, Vellore. The first report of this clinical entity from India was by Bagchi et al. [164] and the first culture-proven case was by Dastur et al . [165] This was followed by sporadic reports from other centers with no predilection for race or geographic location. [166],[167],[168],[169] A cerebral abscess caused by Fonsecaea pedrosoi , a rare chromomycotic infection was reported from NIMHANS, Bangalore. [170] Most infections of pheohyphomycosis occurred in the second and third decade, the youngest case documented was in a sixday-old neonate. [171] Almost all cases involved immunocompetent hosts except for an occasional report in a renal transplant recipient. [172] High mortality was seen in almost all reported cases mainly due to delay in surgical resection and treatment with less effective antifungal agents like amphotericin B. Vyas et al. report survival following early and complete surgical resection with flucytosine therapy. [173]
Penicilliosis marnefei
Penicilliosis marneffei is a facultative, intracellular pathogen, the only thermally dimorphic fungus, growing as mould at 25 o C on Saboraud's Dextrose agar and converts to yeast form at 37 o C on enriched medium. The unique feature of the fungus is the presence of a soluble red pigment diffusing into the agar. The cell wall has mannoprotein which is antigenic. No definite virulence determinant of this fungus has been identified.
This fungus is the third most common opportunistic infection in HIV infected patients of South East Asia, following pulmonary tuberculosis and cryptococcosis. [174],[175] It causes progressive infection in both immunocompetent and immunocompromised hosts. The organism invades the reticuloendothelial system, intracellular and extracellular basophilic, elliptical yeast forms with a clear central septation seen in macrophages. Differentiation between Peniciliosis marneffei and H. capsulatum is important because both are intracellular pathogens. Histopathologically, penicilliosis causes granulomatous reaction in immunocompetent
patients. In immunosuppressed individuals it causes necrotizing abscesses with neutrophils and fibrin and macrophages engorged with proliferating yeast cells in tissues, heralding signs of disseminated infection. The organism can be isolated from blood and the CSF, suggesting involvement of the nervous system. The clinical symptoms are nonspecific and resemble closely other fungal infections like histoplasmosis and cryptococcosis in HIV infected patients.
Indian data
This fungal infection is recognized in HIV infected individuals from the northeastern state of India, Manipur and the majority of the patients were IV drug abusers sharing unsterilized needles but not a single pathologically confirmed brain lesion has been recorded from that state. [176],[177] However, in the literature, successful isolation of the fungus from meninges has been reported. [178] In a follow-up study of 36 cases of Penicilliosis marneffei from Jawaharlal Nehru Medical College Hospital, Imphal, Manipur, other coexisting opportunistic infections like pulmonary/extrapulmonary tuberculosis, oral candidiasis, cryptococcal meningitis, mucocutaneous Herpes simplex and multidermatomal Herpes zoster infections have been reported. Cell-mediated immunity plays a central role in the host defense mechanism against this infection. Response to itraconzole and fluconazole was found to be good.
Other Uncommon Dimorphic Fungi Involving the CNS
These are geographically restricted mycoses, corresponding to the areas in the world where warm temperature and dry conditions exist. The fungi belonging to this group are Coccidioides immitis, Paracoccidioides braziliensis, Histoplasma capsulatum, Sporotrichum schenkii, Blastomyces dermatitides . The organisms live in the soil and in vegetation. These fungi penetrate the oral, pharyngeal and nasal
mucosa by ingestion or inhalation causing focal lesions and then are carried hematogenously to other viscera like lungs and reticuloendothelial organs and rarely to CNS. The pulmonary and lymph node lesions can be self-limiting, the primary focus undergoing calcification. The central nervous system involvement usually becomes apparent one to three months after the primary infection. The disseminated disease develops in less than 0.2% of cases [179] and occurs more often in pregnant, diabetic and immunocompromised individuals.
These fungi manifest chiefly as acute, subacute or chronic symptomatic meningitis or with meningoencephalitic symptoms. Blockage of the CSF pathway may result in hydrocephalus. Extensive spinal meningitis may cause adhesive arachnoiditis and spinal cord compression. The pathological changes observed on gross, microscopic examination and changes in the CSF closely resemble those of tuberculous meningitis. The organisms can be located in the histiocytes and giant cells by methenamine silver stain. However, the lesions may be overlooked, being mistaken for cryptococcal or mycobacterial infection in view of the close similarity in pathogenesis and pathology. Awareness of the geographic pathology, culture or antigenic characterization are the key to recognition.
Pseudoallescheria boydii infection presenting as a mycetoma is a very rare cerebral mycosis. The organisms are present in the soil and water as thin septate hyphae. When the organism infects the nervous system, it causes meningoencephalitis with microabscesses and rarely, mass lesions and hemorrhagic infarcts. With persistence of the infection, the suppurative lesion may become granulomatous in nature. Histological examination not only establishes the diagnosis but also allows specific identification of the causative agent.
Madurella mycetoma usually involves subcutaneous tissues of the lower extremities and involvement of CNS and cranial bones is extremely rare and sporadic cases are reported from India. [9],[180] The organisms reach the brain following local trauma. The black grains of Madurella mycetomatis found in the midst of neutrophilic abscesses contain uniform rust brown cement and hyphae with expanded terminal
cells. Surgical management and amphotericin B are found useful in mycetoma of lower limbs.
Therapeutic Rationale of CNS Fungal Infections
Parallel to the increase in the incidence of opportunistic fungal infections, especially following immunosuppressive states like post transplantation, and metabolic derangement like diabetes and HIV/AIDS, there has been introduction of new antifungal agents to combat the disease. Though both superficial and systemic fungal infections elicit cell-dependent immune reaction, the host immunity is not strong enough to eradicate and the fungus can remain dormant for long periods, waiting for an opportune moment to get reactivated. The relative uniqueness of the fungal cell wall antigens in contrast to the human host is exploited to develop antifungal pharmacological agents. Both yeast and hyphal forms, because of their size and thick cell wall can reach the nervous system only through circulation. Various proteases secreted by the fungi help in reaching a conducive nidus in the brain, breaching the vasculature. The presence of glucose and serum proteins and absence of complement system and inflammatory cells facilitate the growth of the fungi once they reach the CSF pathway and brain parenchyma. The recognition of these characteristics formed the bedrock for developing antifungal agents and understanding the mechanism of antifungal therapy at the bedside.
Conventional amphotercin B, a polyene macrolide heptane, binds to the ergosterol in the cell membrane causing direct membrane toxicity, partly by oxidative damage. Though human cell membrane lacks ergosterol, amphotericin B, a polyene binds to the cell membrane cholesterol of the mammalian cells, resulting in toxicity to metabolically active cells in the liver and kidney. Amphotericin B is unstable when exposed to heat, light and acidic pH. Lipid formations of the drug increase the efficiency and reduce toxicity, while treating deep mycosis.
The azole group of drugs inhibit the fungal cytochrome p450-dependent enzymes, thereby impairing ergosterol synthesis. Ketoconazole is orally effective but penetrates CSF poorly. Itraconazole and fluconazole are active orally and less toxic, because of their more specific binding to fungal cell wall cytochrome p450. Fluconazole, because of relatively small molecular size is water-soluble, minimally protein-binding, excreted in urine as an active drug, penetrates well into the CSF and has prolonged half life (25h in humans), thus is effective for CNS mycosis caused by Cryptococcus , Candida and hyphal forms.
5-Flurocytosine, a competitive antimetabolite for uracil in the synthesis of yeast RNA interfering with thymidilate synthetase, is a water-soluble, stable fungi static compound, used orally. It works synergistically with amphotericin B, in the treatment of cryptococcal meningitis. As the human cells lack the enzyme system to synthesize fungal cell wall glycans and chitin, drugs like Echinocandin and Nikkomycin are developed exploiting this biochemical selectivity and are entering the clinical trails. Though the antifungal therapy is used extensively and favorable clinical response is noted, how it alters the host tissue response is unclear, especially following longterm therapy.
Epilogue
Despite significant advances in taxonomy, cultural characters and molecular biology of fungi, critical gaps still remain in understanding their pathobiology. Important questions like how the fungi survive in the host cell, particularly in granulomas, how long and where they persist during sub-clinical infections and how they exploit the host defenses for their survival and pathogenicity remain unanswered. The newly emerging branch of comparative genomics will provide insight into the synergistic and antagonistic influence of fungi and bacteria on their respective growth in the
"microbial ecosystem" in the host causing manifest diseases. Many of the fungi retain their pathogenic potential and virulence in diverse animal hosts without this being a requirement for replication and survival. Passage of a virulent strain of H. capsulatum in the presence of soil ameba ( A. castellani ) results in selection of variants that are pathogenic in mice indicating that the virulence in the pathogen can be amplified by interaction with an amoeboid host. [181] The replication and acquisition of the polysaccharide capsule by C. neoformans in the amoeba is a feature similar to interaction between macrophages and ingested yeast forms of fungi. Similarly, non-pathogenic cryptococci are killed by nematodes while wild strain of C. neoformans is lethal to the worms. [182] It is plausible that in tropical developing countries the intestinal nematodes may be involved in modulating the survival and virulence of systemic fungi. The study of the interaction between the fungi and their potential host in the environment is a rich area of investigation to explore the fundamental question related to pathogenesis in clinical medicine.
Acknowledgments
We thank the clinicians, the microbiologists and resident staff of different centers for their assistance in establishing the diagnosis. Patient secretarial assistance provided by Mrs. Kanakalakshmi, data retrieval by Ms. Neema Susan Monteiro and Mr. Shivaji and photographic work by Mr. K. Manjunath are gratefully acknowledged.
Fig. 1. Characteristic findings of cryptococcal CNS infection. (A) Brain biopsy (hematoxylin and eosin, 400) shows multiple Cryptococci (black arrow) and inflammatory cells. The clear, mucoid appearance of the thick capsule (red arrow) results in a halo around the organism. (Courtesy of Dr Gretchen Johns, Mayo Clinic.) (B) MRI reveals dilated ventricles from communicating hydrocephalus in a patient with cryptococcal meningitis. (C) Multiple small gelatinous pseudocysts are evident in the basal ganglia. (Courtesy of Dr Beth Levy, Saint Louis University, St Louis, MO.)
Fig. 2. Necrosis of the inferior frontal lobe was found in a patient with mucormycosis. (Courtesy of Dr Beth Levy, Saint Louis University, St Louis, MO.)
Fig. 3. In a patient with mucormycosis of the ethmoid and cancer of the lung, invasion of a thrombosed infraorbital artery is reflected in the development of an erythematous cheek (A) and necrotic eschar several days later (B).
Fig. 4. A necrotic palate was observed in a diabetic woman with an acute cellulitis of the orbit from Rhizopus.
Fig. 5. (A) GMS stain (600) shows Aspergillus with septated hyphae that typically branch no more than 45 degrees. (Courtesy of Department of Pathology, Saint Louis University, St Louis, MO.) (B) Hemorrhagic necrosis in the thalamus was caused by infection with Aspergillus. (Courtesy of Dr Beth Levy, Saint Louis University, St Louis, MO.)
INFEKSI FUNGAL PADA S.S.P
Fungi adalah organisme yang terdapat dimana-mana dengan virulensi rendah yang menjadi patogenik pada lingkungan tertentu seperti depresi immunitas bermedia sel, neutro penia, dan terapi antibiotika sistemik jangka lama. Tidak jarang menginvasi otak.
Infeksi fungal kini didiagnosis lebih sering karena bertambahnya kewaspadaan atas setiap infeksi, biopsi dan tehnik diagnostik lebih baik, bertambahnya pasien yang mendapat antibiotika jangka lama, dan bertambahnya perjalanan ke, dan immigrasi dari, daerah infeksi endemik. Misdiagnosis dan terlambatnya diagnosis umum dilakukan. Masalah ini secara umum berperan atas kegagalan mengejar diagnosis laboratori dan jaringan. Kompetensi sistema immun adalah faktor yang penting dalam preseleksi patogen fungal spesifik: Cryptococcus, Coccidioides, Histoplasma, dan Blastomyces dapat menginfeksi orang sehat, sedang infeksi fungal lain terjadi hampir selalu pada pasien dengan immunitas seluler yang terganggu. Terkenanya SSP mungkin disseminata, menyebabkan meningitis atau meningoensefalitis; atau fokal, menyebabkan abses granulomatosa. Berbeda dengan infeksi bakterial, meningitis fungal cenderung dimulai ringan dengan perburukan bertahap. Nyeri kepala, kaku kuduk, demam, letargi, status mental depresi, dan palsi saraf kranial mungkin tampak. Cryptococcus, Coccidioides, Candida, dan Aspergillus umum tampil sebagai meningitis atau meningoensefalitis. Tanda dan gejala klinis tak bisa dibedakan dari semua bentuk meningitis kronik lain. Pleositosis CSS adalah limfositik, protein CSS sedikit meninggi, dan glukosa CSS biasanya berkurang. Umumnya
fungi sulit dibiak dari darah dan CSS, serta tes serologis kurang sensitif, sebagian karena terganggunya immunitas seluler umum terjadi pada pasien ini. CT scan tidak selalu membantu pada meningitis fungal, tapi mungkin memperlihatkan hidrosefalus, komplikasi dari meningitis kronik. MRI dapat efektif memperlihatkan penguatan basiler dan inflamasi. Abses otak tunggal atau multipel mungkin tampil dengan kejang, nyeri kepala, status mental depresi, atau defisit neurologis fokal, sering bersamaan dengan pneumonia. Patogen yang umum adalah Cryptococcus, Aspergillus, Nocardia, Blastomyces, Actinomyces, dan Histoplasma.
CRYPTOCOCCOSIS
Cryptococcus neoformans, organisme tanah yang umum, adalah meningitis fungal terbanyak yang terjadi di USA. Abses granulomatosa kriptokokal juga telah dikenal baik, namun jarang terjadi. Cryptococcosis terjadi baik pada orang sehat maupun dengan sistema immun yang terganggu. Ia penyebab kematian dan kesakitan yang bermakna pada pasien AIDS, infeksi terjadi pada sekitar 10 % pasien. Saluran respirasi adalah daerah infeksi primer, dan disseminasi hematogen adalah sumber infeksi SSP tersering. Apus tinta india dari CSS hanya positif
pada 50 % kasus; namun antigen kapsuler dapat dilacak dengan fiksasi komplemen pada sekitar 90 % kasus. Dua regimen terapi saat ini dipakai untuk menindak meningitis kriptokokal, berdasar penelitian pada pasien AIDS: amfoterisin B IV (0.3-0.7 mg/kg/hari) dikombinasi dengan flusitosin (150 mg/kg/hari) dan flukonazol oral (150-400 mg/hari). Proporsi responder masing-masing 50 % dengan mortalitas 25 %; namun pasien yang diterapi flukonazol lebih lambat mancapai CSS yang bersih dan mempunyai mortalitas yang tinggi selama minggu pertama terapi. Karenanya amfoterisin B dengan atau tanpa flusitosin dianjurkan untuk minggu awal terapi. Flukonazol yang kurang toksik yang diberikan per oral, dibedakan karena waktu paruh yang lebih panjang, pemberian oral sekali sehari, dan penetrasi CSS tinggi, lebih disukai untuk pemakaian terapi kronis.
COCCIDIOIDES
Coccidioides immitis biasa terdapat pada tanah setengah kering di Amerika. Bisa menginvasi tanpa adanya kelainan lain yang menyertai; hampir selalu melalui saluran nafas. Walau kelainan ini dapat tampil sebagai infeksi SSP saja, biasanya didahului riwayat keluhan respirasi. Pada pasien dengan gangguan immunitas, meningitis bisa terjadi sebagai infeksi diseminata
sistemik letal. Coccidiomycosis sering tidak ditemukan hingga penyakit telah menetap dengan eksudat sisterna basal proteinaseosa tebal; jadi hidrosefalus dan palsi saraf kranial mungkin timbul. Hidrosefalus dapat sangat mempersulit terapi. Tes fiksasi komplemen atas antibodi CSS positif pada setengah kasus. Sebelum dikenal amfoterisin B, mortalitas meningitis coccidioidal mencapai 100 %. Pengobatan dengan pemberian amfoterisin B IV dan intratekal atau intrasisternal menurunkan mortalitas hingga 30-50 %. Namun amfoterisin B memiliki efek buruk yang jelas hingga membatasi penggunaan kllinis dan pemberian intratekal berbulan-bulan menjadi sulit. Karenanya dianjurkan pemasangan reservoir CSS subkutan. Efek samping amfoterisin B yang diberikan CSS adalah meningitis kemikal, arakhnoiditis, infarksi kord tulang belakang, perdarahan intrasisternal, dan superinfeksi bakterial pada reservoir. Relaps, sering beberapa tahun setelah terapi yang berhasil, sering dijumpai pada coccidiomycosis. Azol diketahui sangat efektif dalam menindak coccidiomycosis sistemik, namun penelitian awal atas meningitis dengan mikonazol dan ketokonazol tidak menjanjikan. Flukonazol diketahui efektif dalam pengobatan meningitis, digunakan sebagai terapi tunggal atau kombinasi dengan amfoterisin atau mikonazol intratekal.
CANDIDIASIS
Candidiasis jarang pada orang sehat, walau biasa didapat pada flora orofaringeal. Berbeda dengan meningitis fungal lainnya, sumber infeksi SSP sering primer bukan pada pernafasan, namun penyebaran dari intestinal, uriner atau kateter vaskuler. Candidiasis sering merupakan komplikasi lambat atas tindakan berbagai keadaan kelemahan, dan insidens yang tinggi infeksi SSP ditemukan pada autopsi. Walau meningitis lebih sering, juga ditemukan abses otak granulomatosa candidal. Candida albicans serta spesies lain dijumpai pada meningitis pasien AIDS dan infeksi alat pintas. Tindakan dengan mikonazol, IV dan IV dikombinasi intratekal, memperlihatkan hasil memuaskan. Reseksi bedah atas granuloma diikuti terapi anti mikrobial memberikan hasil akhir memuaskan.
ASPERGILLOSIS
Aspergillus adalah fungi paling banyak dilingkungan. Semula dijelaskan sebagai infeksi fokal yang jarang akibat dari perluasan infeksi sinus, aspergillosis adalah infeksi diseminata dengan prevalensi meningkat,
kedua setelah C. neoformans sebagai infeksi fungal tersering pada SSP pada pasien dengan gangguan immunitas. Infeksi SSP opportunistik oleh Aspergillus biasanya didahului infeksi pulmoner dan dikira melalui penyebaran hematogen. Meningitis, ensefalitis, abses otak soliter atau multipel, dan vaskulitis telah diketahui. Invasi vaskuler dengan vaskulitis nekrotik dan embolisasi sering terjadi pada kelainan diseminata SSP, hal yang khas pada Phycomyces. Aneurisma mikotik serebral bisa terjadi. Ditemukan kelainan yang didapat dari komunitas pada pasien immunokompeten berupa lesi massa soliter pada apeks orbit, dan menjadi diseminata setelah reseksi; karenanya hal ini harus dipikirkan pada pasien yang immunologis tak terganggu. Infeksi aspergillus pada ruang diskus pada pasien yang terganggu sistema immunnya juga dijumpai. Amfoterisin B dengan atau tanpa flusitosin atau rifampin, adalah terapi medikal optimal. Dosis kumulatif amfoterisin B 450-2300 mg dilaporkan berhasil dengan baik. Bila terjadi massa yang diskreta, dilakukan kraniotomi reseksi atau aspirasi stereotaktik. Bahkan dengan terapi agresif, prognosis buruk dan survival jarang.
PHYCOMYCYTES
Walaupun penyebaran hematologis adalah jalur primer kebanyakan infeksi SSP, terkadang abses fungal terjadi setelah kontaminasi langsung pada otak dari infeksi berdekatan. Ini umum tampak pada infeksi Zygomyces, terutama mucormycosis, agen yang lebih agresif yang sering menyebabkan serebritis difusa. Mucormycosis adalah contoh ensefalitis fungal difusa, terjadi paling sering pada pasien dengan diabetes mellitus dan immunitas terganggu. Organisme ini lebih menyukai mengenai vaskulatur serebral dengan akibat iskemia, trombosis, dan infarksi sebagai tambahan atas inflamasi. Jaringan orbit dan sinus paranasal sering terkena. Tindakan termasuk debridemen jaringan terinfeksi dan devital, perawatan kelainan yang mendasari, dan amfoterisin B sistemik. Prognosis buruk walau dengan tindakan, kecuali diagnosis ditegakkan dini.
ACTINOMYCOSIS
Actinomyces israelii adalah suatu bakteri anaerob gram positif yang biasa dijumpai pada flora oral normal. Dibicarakan dibab ini karena riwayatnya yang mengkategorikannya kedalam infeksi fungal. Actinomycosis tampil sebagai abses otak tunggal, dan secara jarang sebagai meningitis basiler purulen, dan biasanya penyebaran
langsung dari infeksi telinga atau mandibula walau penyebaran hematogen dari kelainan pulmoner menjadi lebih utama. Tindakannya terdiri dari drainasi serta penisilin IV untuk 3-4 bulan.
NOCARDIOSIS
Nocardia adalah aerob gram positif yang juga sejarahnya dikategorikan kedalam bakteri 'fungus-like'. Nocardiosis SSP biasanya sekunder atas penyebaran hematogen dari infeksi pulmoner, dan biasanya tampil sebagai abses, walau meningitis purulen juga terjadi. Abses biasanya multipel dan multilokuler. Pembentukan kapsul terjadi dengan buruk. berbeda dengan actinomycetes, nocardia cenderung resisten penisilin. Tindakan yang dianjurkan adalah sulfametoksazol 4-8 gr/ hari untuk 612 bulan. Drainasi diindikasikan untuk abses yang terjangkau; namun pengelolaan non bedah pernah dilaporkan.
You might also like
- Guidelines For The Prevention and Management of Mycobacterium Tuberculosis Infection and Disease in Adult Patients With Chronic Kidney DiseaseDocument12 pagesGuidelines For The Prevention and Management of Mycobacterium Tuberculosis Infection and Disease in Adult Patients With Chronic Kidney DiseaseAnastasia Lilian SuryajayaNo ratings yet
- Typhoid HepatitisDocument2 pagesTyphoid HepatitisAnastasia Lilian SuryajayaNo ratings yet
- Doa UmatDocument2 pagesDoa UmatAnastasia Lilian SuryajayaNo ratings yet
- Iavt 03 I 2 PDocument3 pagesIavt 03 I 2 PAnastasia Lilian SuryajayaNo ratings yet
- Tuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghDocument3 pagesTuberculosis in Liver Cirrhosis: Rajesh Upadhyay, Aesha SinghAnastasia Lilian SuryajayaNo ratings yet
- For Practitioner: Tuberculosis and Chronic Renal Failure Therapy PatternsDocument3 pagesFor Practitioner: Tuberculosis and Chronic Renal Failure Therapy PatternsAnastasia Lilian SuryajayaNo ratings yet
- Pulmonary Tuberculosis in Patients With Chronic Renal Failure at Zagazig University HospitalsDocument6 pagesPulmonary Tuberculosis in Patients With Chronic Renal Failure at Zagazig University HospitalsAnastasia Lilian SuryajayaNo ratings yet
- Treatment STHDocument3 pagesTreatment STHAnastasia Lilian SuryajayaNo ratings yet
- Leptin 180212Document22 pagesLeptin 180212Anastasia Lilian SuryajayaNo ratings yet
- File 40Document37 pagesFile 40Anastasia Lilian SuryajayaNo ratings yet
- DiliDocument18 pagesDiliKharisma Rizqiah WahyuniNo ratings yet
- RespirologyDocument8 pagesRespirologyAnastasia Lilian SuryajayaNo ratings yet
- Treatment of Tuberculosis DiseaseDocument41 pagesTreatment of Tuberculosis DiseaseAnastasia Lilian SuryajayaNo ratings yet
- Jurnal MiraDocument1 pageJurnal MiraAnastasia Lilian SuryajayaNo ratings yet
- Lumbal PungsiDocument11 pagesLumbal PungsiAnastasia Lilian SuryajayaNo ratings yet
- Tugas Hiv CihuiiDocument2 pagesTugas Hiv CihuiiAnastasia Lilian SuryajayaNo ratings yet
- Treatment STHDocument3 pagesTreatment STHAnastasia Lilian SuryajayaNo ratings yet
- Leptin 180212Document22 pagesLeptin 180212Anastasia Lilian SuryajayaNo ratings yet
- Leptin WikipediaDocument14 pagesLeptin WikipediaAnastasia Lilian SuryajayaNo ratings yet
- LiesDocument7 pagesLiesAnastasia Lilian SuryajayaNo ratings yet
- Leptin EditDocument50 pagesLeptin EditAnastasia Lilian SuryajayaNo ratings yet
- Leptin 190212Document24 pagesLeptin 190212Anastasia Lilian SuryajayaNo ratings yet
- Leptin BaruuDocument3 pagesLeptin BaruuAnastasia Lilian SuryajayaNo ratings yet
- Breast AbscessDocument56 pagesBreast AbscessAnastasia Lilian Suryajaya0% (1)
- Tambahann INF SSPDocument28 pagesTambahann INF SSPAnastasia Lilian SuryajayaNo ratings yet
- Home Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentDocument50 pagesHome Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentAnastasia Lilian SuryajayaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- EC 2012 With SolutionsDocument50 pagesEC 2012 With Solutionsprabhjot singh1No ratings yet
- ABHA Coil ProportionsDocument5 pagesABHA Coil ProportionsOctav OctavianNo ratings yet
- Acer Globalisation ProcessDocument10 pagesAcer Globalisation ProcesscrosstheevilNo ratings yet
- Reaction PaperDocument3 pagesReaction PaperLois DolorNo ratings yet
- Sage TutorialDocument115 pagesSage TutorialChhakuli GiriNo ratings yet
- Written Report SampleDocument16 pagesWritten Report Sampleallanposo3No ratings yet
- Glossary of Blasting TermsDocument13 pagesGlossary of Blasting TermsNitesh JainNo ratings yet
- City Limits Magazine, December 1981 IssueDocument28 pagesCity Limits Magazine, December 1981 IssueCity Limits (New York)No ratings yet
- Densha: Memories of A Train Ride Through Kyushu: By: Scott NesbittDocument7 pagesDensha: Memories of A Train Ride Through Kyushu: By: Scott Nesbittapi-16144421No ratings yet
- 8 X 56 M.-SCH.: Country of Origin: ATDocument1 page8 X 56 M.-SCH.: Country of Origin: ATMohammed SirelkhatimNo ratings yet
- GrenTech Express Communication System Introduction 1.0Document30 pagesGrenTech Express Communication System Introduction 1.0Son NguyenNo ratings yet
- Citibank CaseDocument6 pagesCitibank CaseLalatendu Das0% (1)
- Answer: C: Exam Name: Exam Type: Exam Code: Total QuestionsDocument26 pagesAnswer: C: Exam Name: Exam Type: Exam Code: Total QuestionsMohammed S.GoudaNo ratings yet
- Chapter 13 Current Liabilities Test Bank Versi 2Document72 pagesChapter 13 Current Liabilities Test Bank Versi 2Slamet Tri PrastyoNo ratings yet
- Worked Solution Paper5 A LevelDocument8 pagesWorked Solution Paper5 A LevelBhoosan AncharazNo ratings yet
- Exclusive GA MCQs For IBPS Clerk MainDocument136 pagesExclusive GA MCQs For IBPS Clerk MainAnkit MauryaNo ratings yet
- Zero Tolerance 2010Document16 pagesZero Tolerance 2010Adrian KozelNo ratings yet
- Properties of WaterDocument23 pagesProperties of WaterNiken Rumani100% (1)
- HR Practices in Public Sector Organisations: (A Study On APDDCF LTD.)Document28 pagesHR Practices in Public Sector Organisations: (A Study On APDDCF LTD.)praffulNo ratings yet
- Celula de CargaDocument2 pagesCelula de CargaDavid PaezNo ratings yet
- Prediction of CBR From Index Properties of Cohesive Soils: Magdi ZumrawiDocument1 pagePrediction of CBR From Index Properties of Cohesive Soils: Magdi Zumrawidruwid6No ratings yet
- Nat Steel BREGENEPD000379Document16 pagesNat Steel BREGENEPD000379Batu GajahNo ratings yet
- CHN Nutri LabDocument4 pagesCHN Nutri LabMushy_ayaNo ratings yet
- HKUST 4Y Curriculum Diagram CIVLDocument4 pagesHKUST 4Y Curriculum Diagram CIVLfrevNo ratings yet
- S-Sapfico-Satyanarayanamaterial 121212Document183 pagesS-Sapfico-Satyanarayanamaterial 121212mpsing1133No ratings yet
- Managing Errors and ExceptionDocument12 pagesManaging Errors and ExceptionShanmuka Sreenivas100% (1)
- WSD M1a283 B50Document9 pagesWSD M1a283 B50'Lampa'No ratings yet
- Joomag 2020 06 12 27485398153Document2 pagesJoomag 2020 06 12 27485398153Vincent Deodath Bang'araNo ratings yet
- HDO OpeationsDocument28 pagesHDO OpeationsAtif NadeemNo ratings yet
- QAU TTS Form Annual AssessmentDocument6 pagesQAU TTS Form Annual AssessmentsohaibtarikNo ratings yet