Professional Documents
Culture Documents
Hernia Inguinal
Uploaded by
Fernando BurgoaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hernia Inguinal
Uploaded by
Fernando BurgoaCopyright:
Available Formats
M u s c u l o s k e l e t a l I m a g i n g • R ev i ew
Jacobson et al.
Ultrasound of the Groin
Musculoskeletal Imaging
Review
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
FOCUS ON:
Ultrasound of the Groin:
Techniques, Pathology, and Pitfalls
Jon A. Jacobson1 OBJECTIVE. In a patient with symptoms referable to the groin, there can be a number of
Viviane Khoury 2 causes to consider and at times the cause of the symptoms is multifactorial. Although ultra-
Catherine J. Brandon1 sound can be effective in the evaluation of the groin, the depth and complexity of the anatomy
can be problematic. A protocol-driven approach for ultrasound evaluation of the groin will
Jacobson JA, Khoury V, Brandon CJ help to ensure an accurate and comprehensive evaluation. This article summarizes the ultra-
sound technique and protocol for evaluation of the groin to include evaluation of the hip joint,
anterior hip musculature, the iliopsoas bursa, the inguinal lymph nodes, the pubic symphys
eal region, and the inguinal region for hernias. Common pathologic conditions and pitfalls
related to ultrasound evaluation of the groin will be reviewed.
CONCLUSION. There are many potential pathologic conditions in a patient with groin
symptoms. Because symptoms may be multifactorial and history may be ambiguous or mis-
leading, a protocol-driven evaluation with ultrasound is recommended. The hip joint is evalu-
ated for effusion, synovitis, and labral abnormalities. The muscles and tendons, including the
common aponeurosis at the pubic symphysis, are evaluated for tendinosis and tears. Dynamic
evaluation should be considered to assess for snapping hip syndrome. Iliopsoas bursal dis-
tention and lymph node enlargement are other considerations. Last, inguinal region hernias
must be evaluated during the Valsalva maneuver and documented in two orthogonal planes to
avoid several important diagnostic pitfalls.
U
ltrasound has been used to effec- ner thigh; therefore, ultrasound of the groin
tively evaluate pathology of the should include evaluation of the hip joint,
musculoskeletal system [1–3]. anterior hip musculature, iliopsoas bursa, in-
When an abnormality involves the guinal lymph nodes, pubic symphyseal re-
distal extremity, ultrasound can accurately gion, and inguinal region for hernias. Dy-
show anatomy and pathology in detail with the namic evaluation is also an integral aspect
Keywords: groin, hernia, hip, joint, ultrasound benefit of directly correlating imaging and of a groin ultrasound examination. This arti-
physical examination findings [4]. Dynamic cle reviews a protocol-driven approach to the
DOI:10.2214/AJR.15.14523 evaluation of structures with muscle contrac- ultrasound evaluation of the groin, showing
tion, joint movement, or position change of the common pathologic conditions and discuss-
Received February 2, 2015; accepted after revision
April 15, 2015.
patient may also add significant information ing diagnostic pitfalls.
that may not be obtainable with static MRI [5].
1
Department of Radiology, University of Michigan, 1500 E In contrast to evaluation of the distal ex- Ultrasound Equipment
Medical Center Dr, TC-2910L, Ann Arbor, MI 48109-0326. tremities, evaluation of the groin and hip can Clinically available ultrasound units, both
Address correspondence to J. A. Jacobson
be more problematic. The added depth of the portable and cart-based, with variable fre-
(jjacobsn@umich.edu).
area being imaged results in lower resolu- quency transducers can be used to evaluate
2
Department of Radiology, University of Pennsylvania, tion, and there is more complex anatomy. It the groin and hip. For an examination of a
Philadelphia, PA. is often difficult to directly correlate imaging thin individual, a linear transducer of great-
Supplemental Data findings with patient symptoms and the clin- er than 10 MHz is effective. For larger pa-
Available online at www.ajronline.org. ical presentation may be ambiguous. To en- tients, a curvilinear transducer of less than
sure a comprehensive evaluation, one should 10 MHz is often needed to evaluate the hip.
AJR 2015; 205:513–523 follow a specific protocol when performing It is a misconception to presume that a curvi-
0361–803X/15/2053–513
an ultrasound examination (Table 1). linear transducer must be used, but often it is
The groin can be defined as the area at the necessary. The objective is to use the highest
© American Roentgen Ray Society junction of the lower abdomen and the in- frequency transducer possible to achieve the
AJR:205, September 2015 513
Jacobson et al.
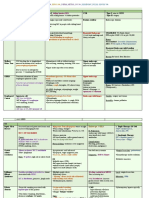
highest resolution given the constraints of a TABLE 1: Ultrasound Scanning Protocol of the Groin
patient’s body habitus.
Anatomic Region and Structures Pathology
Hip Joint Hip joint
Scanning Details Anterior recess Effusion, infection, synovial hypertrophy
For ultrasound examination of the hip Labrum Labral tear, paralabral cyst
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
joint, the transducer is placed in the sagittal
oblique plane long axis to the femoral neck. Femur Femoroacetabular impingement
The characteristic bone landmarks of the Anterior hip musculature
femoral head and neck should be identified Iliopsoas complex Snapping hip syndrome
(Fig. 1A). The femoral neck should be per-
Rectus femoris Tendinosis including calcific tendinosis
pendicular to the sound beam to eliminate
anisotropy of the overlying joint capsule. Sartorius Tendon tear
The hyperechoic fibrocartilage labrum is Iliopsoas bursa Distention, synovial hypertrophy, infection
also identified at the acetabulum. The trans- Inguinal lymph nodes
ducer is then rotated 90° to evaluate the ante-
Superficial and deep inguinal lymph nodes Hyperplasia, inflammation, primary neoplasia, metastases
rior hip in its short axis (Fig. 1B).
Pubic symphyseal region
Anatomy Rectus abdominis Common aponeurosis injury
The hip joint is evaluated for joint-relat- Pubic symphysis Adductor tendon tear or tendinosis
ed abnormalities, such as a joint effusion, in-
Adductor tendons Fracture
traarticular bodies, and synovial disorders.
When evaluating for a joint effusion, one Inguinal region hernias
should target the area over the anterior femo- Internal ring and inguinal canal Indirect inguinal hernia
ral neck. Normally, a hyperechoic layer mea- Hesselbach triangle Direct inguinal hernia
suring up to 7 mm is present, representing
Femoral canal Femoral hernia
the iliofemoral ligament and joint capsule
with its reflection [6] (Fig. 1A). If not imaged
perpendicular, this hyperechoic layer may Synovial Hypertrophy tear [16]. In the evaluation for a labral tear
appear artifactually hypoechoic from anisot- If a joint effusion is complex, the fluid may with ultrasound, sensitivity, specificity, and
ropy and may potentially simulate joint flu- appear hypoechoic rather than anechoic and accuracy have been shown to be 82%, 60%,
id. Regardless, the layer should measure less synovial hypertrophy should be considered. and 75%, respectively [16]; therefore, MRI,
than 7 mm if normal [7]. An additional pit- For assistance in the differentiation of a joint preferably MR arthrography, is indicated if
fall relates to leg positioning: Internal rota- effusion from synovial hypertrophy, a lack of there is concern for labral abnormalities [16].
tion of the hip may cause the anterior joint compressibility and internal flow on color or One cause for a labral tear is cam-type fem-
capsule to become convex anteriorly and to power Doppler imaging would indicate sy- oroacetabular impingement (FAI), in which
potentially measure greater than 7 mm. novial hypertrophy; however, this distinction an abnormal osseous contour of the proximal
may be difficult, and ultrasound-guided aspi- femur or abnormal femoral head-neck offset
Joint Effusion ration may be indicated. Because findings on can impinge on the acetabulum causing hy-
A joint effusion will appear as anechoic ultrasound cannot be used to exclude infec- aline cartilage and labral injuries [17]. Al-
distention of the joint capsule preferentially tion, joint aspiration, lavage and reaspiration, though ultrasound can show an anterosuperi-
around the femoral neck [6]. In the native hip, and synovial biopsy should be considered in or bony prominence and cam deformity of the
evaluation of the anterior recess provides an patients with any distention of the joint cap- proximal femur associated with FAI, alpha
adequate evaluation for a joint effusion. It is a sule if there is concern for septic joint [11–13]. angles cannot be reliably measured and ultra-
misconception to believe that fluid may be pre- In addition to infection, other possible causes sound is not recommended for FAI screening
sent only posteriorly; some degree of fluid is al- of synovial hypertrophy include systemic in- [18]. Related to a labral tear, a paralabral cyst
ways present anterior to the femoral neck in the flammatory arthritis, pigmented villonodular may also be identified on ultrasound as a lobu-
native hip with a joint effusion [8]. However, synovitis (Fig. 2), synovial chondromatosis, lar anechoic or hypoechoic fluid collection in
in the setting of a hip arthroplasty, a joint effu- and amyloid deposition [14]. contact with the labral tear [19] (Fig. 3). As a
sion may be loculated, which warrants a more potential pitfall, a paralabral cyst may be hy-
thorough evaluation of the lateral and posterior Labrum poechoic and difficult to delineate, although
femoral neck. As an additional pitfall after ar- Although the posterior aspect of the la- the lobular appearance and associated labral
throplasty, ultrasound can be inaccurate in the brum is difficult to visualize on ultrasound, tear suggest the appropriate diagnosis.
diagnosis of a small joint effusion [9]. An ex- the anterior aspect, which is the most com-
tensive evaluation of all areas of the hip is war- mon site for labral tears, can be easily eval- Anterior Hip Musculature
ranted when evaluating for complications relat- uated [15]. A hypoechoic or heterogeneous Scanning Details
ed to a hip arthroplasty, such as particle disease labrum indicates degeneration, whereas a For evaluation of the anterior hip muscula-
and pseudotumor formation [10]. more defined anechoic cleft indicates a labral ture, ultrasound scanning can begin over the
514 AJR:205, September 2015
Ultrasound of the Groin
femoral head and neck in the sagittal oblique fibers, and the medial iliacus becomes inter- tion with the hip joint is seen medial to the
plane using bone landmarks for orienta- posed between the psoas major tendon and psoas major tendon at the level of the femo-
tion (Fig. 1A). The transducer can then be superior pubic ramus [23]. As the patient re- ral head with the transducer positioned trans-
turned transverse to the body and centered turns the leg to a straight position, there is a verse to the body (Fig. 1B).
over the femoral head where the psoas major normal reversal in the rotational gliding of
tendon and iliopsoas complex can be iden- the psoas major around the medial iliacus Inguinal Lymph Nodes
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
tified (Fig. 1B). The transducer can then be muscle fibers. In patients with the abnormal Superficial inguinal lymph nodes are lo-
moved cephalad to the level of the ilium at condition, the medial component of the ilia- cated superficial to the femoral vessels in the
the anterior inferior iliac spine (AIIS) to vi- cus muscle becomes temporarily entrapped femoral triangle and are bordered by the in-
sualize the individual components of the il- between the psoas major tendon and superi- guinal ligament, sartorius, and adductor lon-
iopsoas complex (Fig. 1C). The transducer or pubic ramus [20]. As the iliacus muscle gus [27]. The deep inguinal lymph nodes
can be moved lateral at the level of the AIIS abruptly moves lateral, the psoas major ten- are located deeper and medial to the fem-
so that the rectus femoris can be identified. don also abruptly moves posterior and makes oral vessels [27]. It is common to identify
More cephalad, the sartorius origin can be contact with the superior pubic ramus [20]. multiple inguinal lymph nodes bilaterally in
identified at the anterior superior iliac spine. This contact results in an abnormal snap, asymptomatic individuals [27].
The anterior hip musculature can then be as- which is perceived by the patient and felt The average short-axis measurement of
sessed in both the long and short axes. through the transducer. an inguinal lymph node in asymptomatic in-
dividuals is 5.4 mm (range = 2.1–13.6 mm)
Iliopsoas Complex Rectus Femoris and Sartorius with a value of 8.8 mm at 2 SDs above the
The iliopsoas complex is composed of sev- For evaluation of the rectus femoris, assess- mean [27]. Because size criteria are simple
eral structures. In the transverse plane at the ment of both the direct (or straight) and indi- guidelines, the ultrasound characteristics
AIIS, the psoas major tendon is visible with rect (or reflected) heads is required [24]. With are important to determine whether a lymph
its muscle component located medial [20] the transducer’s short axis to the rectus fem- node is abnormal regardless of its size. For
(Fig. 1C). The psoas major tendon may be bi- oris over the AIIS, the direct head is visible example, a metastasis may cause focal asym-
fid with partial and complete splits [20]. An- (Fig. 1C). When the transducer is moved lat- metric enlargement without meeting the size
terolateral to the psoas major tendon are the eral and slightly inferior while the sound beam criterion for enlargement.
medial and lateral muscle fibers of the iliacus is being directed perpendicular to the later- A normal lymph node has an oval shape
with an interposed fascial layer [20]. Inferior al acetabular cortex to eliminate anisotropy, with a hyperechoic hilum, uniform thickness
to the AIIS, the ilioinfratrochanteric muscle the indirect head is visible. The transducer of the hypoechoic cortex, and a hilar pattern
component is present lateral to the iliacus; can then be turned 90° to evaluate the sepa- of blood flow on color and power Doppler
the rectus femoris is located directly lateral rate heads in the long axis. Possible pathologic imaging [28]. The normal hilum is echogen-
and the sartorius anterior to the ilioinfratro- findings includes tendinosis and a tendon tear. ic because of the reflective interfaces among
chanteric muscle [20]. An additional muscle This area is also a potential site for calcium hy- fat, sinusoids, and connective tissues [28].
component, composed of the inferior fibers droxyapatite crystal deposition as calcific ten- With hyperplastic lymph nodes, the normal
of the iliacus, is more difficult to visualize on dinosis (Fig. 4). Ultrasound-guided lavage and features of oval shape, echogenic hilum, uni-
ultrasound [20]. More distally, an accessory aspiration have been successfully used for per- form cortical thickness, and hilar blood flow
tendon from the medial iliacus fibers unites cutaneous treatment [25]. Similarly, the sarto- pattern persist, although the lymph node
with the psoas major tendon to form the il- rius is evaluated in the short and long axes for may be enlarged [28]. A neoplastic lymph
iopsoas tendon several centimeters proximal muscle and tendon abnormalities. node—either from metastases or primary
to the lesser trochanter. The lateral aspect of disease such as lymphoma—is characterized
the iliacus attaches to the proximal femoral Iliopsoas Bursa by a round or asymmetric shape, nonuniform
diaphysis as a direct muscle attachment [21]. The iliopsoas bursa is a normal structure cortical thickness, loss of the normal echo-
Ultrasound evaluation of the distal aspect of located medial and often deep to the ilio- genic hilum, and a peripheral or mixed pat-
the iliopsoas complex is improved with posi- psoas complex where the iliopsoas passes tern of blood flow [28, 29].
tioning the hip in flexion, abduction, and ex- over the ilium. Communication between the
ternal rotation [22]. iliopsoas bursa and the hip joint is present in Pubic Symphyseal Region
approximately 15% of individuals, although The pubic symphyseal region has many
Snapping Hip Syndrome this number increases in the presence of in- anatomic structures that may be the source
To evaluate for snapping iliopsoas, the flammatory arthritis and after arthroplasty of groin symptoms, especially in the athlete
transducer is placed short axis to the psoas [26]. When distended, the iliopsoas bursa is [30]. One method for ultrasound evaluation
major tendon of the iliopsoas complex at the identified medial and deep to the iliopsoas is to begin scanning the rectus abdominis
level of the ilium superior to the AIIS and is complex and may extend proximal along the muscle in short axis inferior to the umbilicus
positioned in the oblique axial plane parallel psoas musculature in the abdomen to poten- and then to turn the transducer 90° so that the
to the inguinal ligament. The patient is then tially simulate a psoas abscess. In this situa- muscle is viewed in the long axis. The trans-
asked to flex, abduct, and externally rotate tion, identification of hip joint communica- ducer is moved inferior to the pubis, where a
the hip. During this maneuver, the psoas ma- tion is essential to confirm iliopsoas bursal common aponeurosis is formed between the
jor tendon normally rotates anterolateral rel- distention, which is most often related to a insertion of each rectus abdominis and the
ative to and around the medial iliacus muscle chronic hip joint process. This communica- origin of each adductor longus tendon [30].
AJR:205, September 2015 515
Jacobson et al.
The transducer can then be moved more in- tion findings to improve accuracy in the set- artery. The transducer can then be angled par-
ferior and oblique toward the knee to main- ting of an unclear clinical diagnosis [34]. Ul- allel to the inguinal canal to assess for an indi-
tain the long axis with the adductor muscu- trasound for the diagnosis of a nonpalpable rect inguinal hernia during the Valsalva ma-
lature; external rotation of the hip assists in or clinically occult hernia has proven more neuver. The transducer is turned 90° over the
this evaluation. The transducer can then be difficult [35], with a sensitivity and specific- inguinal canal, and the Valsalva maneuver is
repositioned over the symphysis pubis in the ity of 86% and 77%, respectively [36], and repeated. This latter evaluation short axis to
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
transverse plane on the body to evaluate for another study showing a sensitivity of 33% the inguinal canal is essential and important
a joint abnormality. Alternatively, the pubic and specificity of 0% [37]. These results to avoid diagnostic pitfalls, which we discuss
symphyseal region can be examined begin- likely reflect the difficulty in performing an later. The transducer is then moved medial in
ning over the adductor muscles and can then ultrasound examination for inguinal hernias the transverse plane between the inferior epi-
be moved proximal to visualize the common and further indicate the need for a clear un- gastric artery and the lateral border of the rec-
aponeurosis and the symphysis pubis. derstanding of sonographic anatomy and the tus abdominis to evaluate for a direct ingui-
One of the most common abnormalities use of a comprehensive protocol. nal hernia in Hesselbach triangle during the
in the symphysis pubis region in athletes in- Valsalva maneuver, and the transducer is also
volves the common aponeurosis between the Anatomy turned 90° in the sagittal plane. Finally, the
rectus abdominis and the adductor muscula- There are three essential soft-tissue land- transducer is positioned short axis to the fem-
ture [30, 31] (Fig. 5). Although the cause of marks for orientation: the lateral margin of oral vasculature inferior to the inguinal liga-
and the term “sports hernia” is often debat- the rectus abdominis, the inferior epigastric ment to assess for a femoral hernia during the
ed, abnormality of the common aponeurosis artery, and the inguinal ligament (Fig. 6A) Valsalva maneuver. We must emphasize the
has been described as the predominant im- [38]. These three boundaries outline Hessel- importance of documenting any hernia in two
aging feature in patients with athletic pub- bach triangle (i.e., the location of a direct in- orthogonal planes: Visualization in the sagit-
algia symptoms [31]. At the common apo- guinal hernia) (Fig. 6). Just superior to the tal plane is important to avoid diagnostic pit-
neurosis, hypoechoic swelling and anechoic origin of and lateral to the inferior epigastric falls for all inguinal region hernias.
clefts may be seen with cortical irregular- artery is the location of the deep or internal
ity [32]. Less commonly, isolated tears of inguinal ring (i.e., the origin of an indirect Indirect Inguinal Hernia
the adductor compartment may be present: inguinal hernia) (Fig. 6). The region distal to The characteristic finding of an indirect
A full-thickness tear is characterized by ten- the inguinal ligament and medial to the fem- inguinal hernia is abnormal movement of in-
don retraction and interposed heterogeneous oral vasculature is the femoral canal (i.e., the traabdominal contents (fat, bowel, or both)
but predominantly hypoechoic hemorrhage origin of a femoral hernia) (Fig. 6). through the deep inguinal ring and through
in the acute and subacute setting [31]. Oth- the inguinal canal [38–40] (Fig. 7 and Vid-
er proposed causes for athletic pubalgia, or Valsalva Maneuver eos S1 and S2 [supplemental videos that can
sports hernia, include a medial bulge in the An adequate Valsalva maneuver (defined be viewed in the AJR electronic supplement
posterior wall of the inguinal canal, obtura- as forced expiratory effort against a closed to this article available at www.ajronline.
tor nerve entrapment, osteitis pubis, tendon glottis) is essential during ultrasound exami- org]). On ultrasound, this abnormality ap-
tear, and inguinal hernias [31, 33]. nation for hernias. One method to increase pears as tissue of variable echogenicity mov-
Abnormalities of the pubic symphysis, intraabdominal pressure is to have the pa- ing through the deep inguinal ring, which
which include hypoechoic capsular disten- tient “puff the cheeks out” while blowing on originates lateral to the inferior epigastric ar-
tion, anechoic joint fluid, synovial hypertro- the back of the hand. To ensure an adequate tery. This tissue then moves medial, parallel
phy, and cortical irregularity, may also be Valsalva maneuver, the femoral vein dis- to the skin surface within the inguinal canal
detected with ultrasound [32]. The superi- tal to the inguinal ligament should distend. and parallel to the plane of the inguinal liga-
or pubic ramus should also be evaluated for Of note, some hernias are not visible during ment. An extensive hernia may extend medi-
cortical step-off or callus to indicate frac- routine Valsalva maneuvers and may require al to and potentially through the external or
ture. A cortical irregularity of the symphysis scanning with the patient standing. superficial inguinal ring into the scrotum or
pubis may be physiologic, related to the un- labia majora and may present as a mass [41].
fused growth plates, and may persist in pa- Scanning Details There is a significant pitfall if one relies on
tients until their mid-20s [32]. To begin ultrasound evaluation for ingui- imaging long axis to the inguinal canal. If the
nal hernias, the transducer is placed short axis intraabdominal contents shift inferiorly dur-
Inguinal Region Hernias to one of the rectus abdominis muscles infe- ing the Valsalva maneuver, the inguinal canal
Inguinal region hernias should be consid- rior to the umbilicus [38]. As the transducer region can move inferior also and can move
ered as a primary or potentially contributing is moved inferior, the inferior epigastric ar- out of view of the ultrasound imaging. This
cause for groin symptoms, which include in- tery is identified deep to the rectus abdominis is why the short-axis view of the inguinal ca-
direct inguinal, direct inguinal, and femoral and is followed moving laterally. Color Dop- nal (in the sagittal oblique plane) is essential
hernias. With regard to the imaging diag- pler imaging may assist in the identification and is necessary to avoid misdiagnosis. In the
nosis of hernias, one meta-analysis showed of the inferior epigastric artery, which is then short axis, the indirect inguinal hernia can
a sensitivity of 92.7–100% and specificity followed inferiorly to its origin at the external be seen moving in and out of the plane ad-
of 22.2–100% using ultrasound [34]. The iliac artery. If the transducer is moved slightly jacent to the spermatic cord (in males) and is
authors stressed that the imaging findings cephalad, this area is the location of the deep visible even if the inguinal canal shifts inferi-
should be correlated with physical examina- inguinal ring lateral to the inferior epigastric orly (Figs. 7B and 7C and Video S2). When
516 AJR:205, September 2015
Ultrasound of the Groin
reporting an indirect inguinal hernia, one size of the direct hernia, which includes the References
should measure the hernia short axis in cross cephalocaudad, mediolateral, and antero- 1. Jacobson JA. Musculoskeletal sonography and
section or two dimensions and also indicate posterior dimensions, should be described MR imaging: a role for both imaging methods.
the medial extent. during the Valsalva maneuver. Radiol Clin North Am 1999; 37:713–735
Additional diagnostic pitfalls exist when 2. Klauser AS, Tagliafico A, Allen GM, et al. Clini-
using ultrasound to evaluate for an indi- Femoral Hernia cal indications for musculoskeletal ultrasound: a
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
rect inguinal hernia. One consideration is a The characteristic finding of a femoral Delphi-based consensus paper of the European
spermatic cord lipoma, which may appear hernia is abnormal intraabdominal contents Society of Musculoskeletal Radiology. Eur Radi-
similar to an indirect inguinal hernia on ul- moving in an inferior direction through the ol 2012; 22:1140–1148
trasound [42]. Movement of the abnormal femoral canal [38–40]. On ultrasound, tis- 3. Jacobson JA. Fundamentals of musculoskeletal
tissue during the Valsalva maneuver can- sue of variable echogenicity will be seen ultrasound, 1st ed. Philadelphia, PA: Saunders
not be used for this distinction because both extending inferiorly, most commonly me- Elsevier, 2007:2
spermatic cord lipomas and indirect ingui- dial to the femoral vein, potentially causing 4. Jamadar DA, Jacobson JA, Caoili EM, et al. Mus-
nal hernias may display minimal movement. compression of the femoral vein (Fig. 10 and culoskeletal sonography technique: focused versus
To distinguish between these two patholog- Videos S7 and S8). The abnormal inferior comprehensive evaluation. AJR 2008; 190:5–9
ic entities, one can evaluate the deep ingui- movement of tissue should be seen in two or- 5. Jacobson JA. Musculoskeletal ultrasound and
nal ring: A true indirect inguinal hernia will thogonal planes—both in the short axis and MRI: which do I choose? Semin Musculoskelet
show abnormal tissue extending through this in the long axis. Radiol 2005; 9:135–149
ring. Another diagnostic pitfall is round lig- 6. Robben SG, Lequin MH, Diepstraten AF, den Hol-
ament varicosities seen in pregnant women, Reporting lander JC, Entius CA, Meradji M. Anterior joint
which should not be misinterpreted as a vas- Most inguinal region hernias involve ab- capsule of the normal hip and in children with tran-
cular malformation [43, 44]. An uncommon normal movement of isoechoic or hyper- sient synovitis: US study with anatomic and histo-
finding that can be seen in the inguinal canal echoic intraabdominal fat. Bowel showing logic correlation. Radiology 1999; 210:499–507
in women is a cyst of the canal of Nuck due the characteristic circular echotexture with 7. Koski JM, Anttila PJ, Isomaki HA. Ultrasonogra-
to a patent processus vaginalis [45]. possible peristalsis may also be visible. The phy of the adult hip joint. Scand J Rheumatol
size of a hernia should be described in all di- 1989; 18:113–117
Direct Inguinal Hernia mensions rather than using ambiguous terms 8. Moss SG, Schweitzer ME, Jacobson JA, et al. Hip
The characteristic finding of a direct in- such as “small” or “large.” It is also impor- joint fluid: detection and distribution at MR imag-
guinal hernia is focal intraabdominal tis- tant to describe what is in the hernia (fat, ing and US with cadaveric correlation. Radiology
sue moving anteriorly through the Hessel- bowel, or both) and if the contents are reduc- 1998; 208:43–48
bach triangle [38–40] (Fig. 8 and Videos ible or irreducible. In the situation of an in- 9. Weybright PN, Jacobson JA, Murry KH, et al.
S3 and S4). On ultrasound, this tissue of carcerated hernia with ischemia, ultrasound Limited effectiveness of sonography in revealing
variable echogenicity will move character- is often ineffective given the patient’s symp- hip joint effusion: preliminary results in 21 adult
istically in a posterior-to-anterior direction toms and CT may be indicated. patients with native and postoperative hips. AJR
and should be documented in two imaging 2003; 181:215–218
planes. Relying on only transverse imaging Summary 10. Ostlere S. How to image metal-on-metal prostheses
(relative to the body) in an assessment for a There are many potential pathologic con- and their complications. AJR 2011; 197:558–567
direct inguinal hernia is a significant pitfall ditions in a patient with groin symptoms. Be- 11. Fink B, Gebhard A, Fuerst M, Berger I, Schafer P.
that may result in diagnostic inaccuracy. In cause symptoms may be multifactorial and High diagnostic value of synovial biopsy in peri-
some individuals, the normal intraabdomi- history may be ambiguous or misleading, a prosthetic joint infection of the hip. Clin Orthop
nal contents move inferior with the Valsal- protocol-driven evaluation with ultrasound is Relat Res 2013; 471:956–964
va maneuver (Fig. 9 and Videos S5 and S6). recommended. The hip joint is evaluated for 12. Kung JW, Yablon C, Huang ES, Hennessey H, Wu
Movement of this tissue under the Hessel- effusion, synovitis, and labral abnormalities. JS. Clinical and radiologic predictive factors of
bach triangle can simulate a direct ingui- The muscles and tendons, including the com- septic hip arthritis. AJR 2012; 199:868–872
nal hernia when imaged in the transverse mon aponeurosis at the pubic symphysis, are 13. Strouse PJ, DiPietro MA, Adler RS. Pediatric hip
plane; however, if the transducer is turned evaluated for tendinosis and tears. Dynamic effusions: evaluation with power Doppler sono-
90° into the sagittal plane, this pitfall can be evaluation should be considered to assess for graphy. Radiology 1998; 206:731–735
avoided. In patients without a hernia, it be- snapping hip syndrome. Iliopsoas bursal dis- 14. Pai VR, van Holsbeeck M. Synovial osteochon-
comes clear that there is no focal movement tention and lymph node enlargement are oth- dromatosis of the hip: role of sonography. J Clin
of abdominal tissue but rather just broad in- er considerations. Last, inguinal region her- Ultrasound 1995; 23:199–203
ferior displacement. This displacement is nias must be evaluated during the Valsalva 15. Blankenbaker DG, De Smet AA, Keene JS, Fine
unlike a true direct inguinal hernia where maneuver and documented in two orthogo- JP. Classification and localization of acetabular
there is focal anterior movement of the in- nal planes to avoid several important diag- labral tears. Skeletal Radiol 2007; 36:391–397
traabdominal contents through the Hessel- nostic pitfalls. 16. Jin W, Kim KI, Rhyu KH, et al. Sonographic
bach triangle. A true direct inguinal hernia evaluation of anterosuperior hip labral tears with
should appear as focal movement of the in- Acknowledgment magnetic resonance arthrographic and surgical
traabdominal contents through the Hessel- Illustrations courtesy of Danielle Dobbs, correlation. J Ultrasound Med 2012; 31:439–447
bach triangle in two orthogonal planes. The Ann Arbor, MI. 17. Bedi A, Kelly BT. Femoroacetabular impinge-
AJR:205, September 2015 517
Jacobson et al.
ment. J Bone Joint Surg Am 2013; 95:82–92 Cejna M, Turetschek K, Kainberger F. Imaging atic review and meta-analysis of the role of radiol-
18. Buck FM, Hodler J, Zanetti M, Dora C, Pfirrmann features of iliopsoas bursitis. Eur Radiol 2002; ogy in the diagnosis of occult inguinal hernia.
CW. Ultrasound for the evaluation of femoroace- 12:409–415 Surg Endosc 2013; 27:11–18
tabular impingement of the cam type: diagnostic 27. Bontumasi N, Jacobson JA, Caoili E, Brandon C, 37. Miller J, Cho J, Michael MJ, Saouaf R, Towfigh S.
performance of qualitative criteria and alpha an- Kim SM, Jamadar D. Inguinal lymph nodes: size, Role of imaging in the diagnosis of occult hernias.
gle measurements. Eur Radiol 2011; 21:167–175 number, and other characteristics in asymptomat- JAMA Surg 2014; 149:1077–1080
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
19. Mervak BM, Morag Y, Marcantonio D, Jacobson ic patients by CT. Surg Radiol Anat 2014; 38. Jamadar DA, Jacobson JA, Morag Y, et al. Sono-
J, Brandon C, Fessell D. Paralabral cysts of the 36:1051–1055 graphy of inguinal region hernias. AJR 2006;
hip: sonographic evaluation with magnetic reso- 28. Esen G. Ultrasound of superficial lymph nodes. 187:185–190
nance arthrographic correlation. J Ultrasound Eur J Radiol 2006; 58:345–359 39. Brandon CJ, Jacobson JA, Fessell D, et al. Groin
Med 2012; 31:495–500 29. Roberto S, Valeria B, Roberto del V, Raffaella M, pain beyond the hip: how anatomy predisposes to
20. Guillin R, Cardinal E, Bureau NJ. Sonographic Chiara FA, Leopoldo R. Analysis by high resolu- injury as visualized by musculoskeletal ultra-
anatomy and dynamic study of the normal ilio- tion ultrasound of superficial lymph nodes: ana- sound and MRI. AJR 2011; 197:1190–1197
psoas musculotendinous junction. Eur Radiol tomical, morphological and structural variations. 40. Stavros AT, Rapp C. Dynamic ultrasound of her-
2009; 19:995–1001 Clin Imaging 2014; 38:96–99 nias of the groin and anterior abdominal wall.
21. Polster JM, Elgabaly M, Lee H, Klika A, Drake R, 30. Omar IM, Zoga AC, Kavanagh EC, et al. Athletic Ultrasound Q 2010; 26:135–169
Barsoum W. MRI and gross anatomy of the iliopsoas pubalgia and “sports hernia”: optimal MR imag- 41. Patel B, Zivin S, Panchal N, Wilbur A, Bresler M.
tendon complex. Skeletal Radiol 2008; 37:55–58 ing technique and findings. RadioGraphics 2008; Sonography of female genital hernias presenting
22. Balius R, Pedret C, Blasi M, et al. Sonographic 28:1415–1438 as labia majora masses. J Ultrasound Med 2014;
evaluation of the distal iliopsoas tendon using a new 31. Zoga AC, Kavanagh EC, Omar IM, et al. Athletic 33:155–159
approach. J Ultrasound Med 2014; 33:2021–2030 pubalgia and the “sports hernia”: MR imaging 42. Rosenberg R, Williamson MR. Lipomas of the
23. Deslandes M, Guillin R, Cardinal E, Hobden R, findings. Radiology 2008; 247:797–807 spermatic cord and testis: report of two cases.
Bureau NJ. The snapping iliopsoas tendon: new 32. Robinson P, Bhat V, English B. Imaging in the as- J Clin Ultrasound 1989; 17:670–674
mechanisms using dynamic sonography. AJR sessment and management of athletic pubalgia. 43. Polat AV, Aydin R, Polat AK, Kececi IS, Karahan
2008; 190:576–581 Semin Musculoskelet Radiol 2011; 15:14–26 G, Taskin GO. Round ligament varicosities: a rare
24. Gyftopoulos S, Rosenberg ZS, Schweitzer ME, 33. Garvey JF, Read JW, Turner A. Sportsman her- cause of groin swelling in pregnancy. Abdom Im-
Bordalo-Rodrigues M. Normal anatomy and nia: what can we do? Hernia 2010; 14:17–25 aging 2013; 38:1178–1181
strains of the deep musculotendinous junction of 34. Robinson A, Light D, Nice C. Meta-analysis of 44. Ryu KH, Yoon JH. Ultrasonographic diagnosis of
the proximal rectus femoris: MRI features. AJR sonography in the diagnosis of inguinal hernias. round ligament varicosities mimicking inguinal
2008; 190:[web]W182–W186 J Ultrasound Med 2013; 32:339–346 hernia: report of two cases with literature review.
25. Park SM, Baek JH, Ko YB, Lee HJ, Park KJ, Ha 35. Robinson P, Hensor E, Lansdown MJ, Ambrose Ultrasonography 2014; 33:216–221
YC. Management of acute calcific tendinitis NS, Chapman AH. Inguinofemoral hernia: accu- 45. Ozel A, Kirdar O, Halefoglu AM, et al. Cysts of
around the hip joint. Am J Sports Med 2014; racy of sonography in patients with indeterminate the canal of Nuck: ultrasound and magnetic reso-
42:2659–2665 clinical features. AJR 2006; 187:1168–1178 nance imaging findings. J Ultrasound 2009;
26. Wunderbaldinger P, Bremer C, Schellenberger E, 36. Robinson A, Light D, Kasim A, Nice C. A system- 12:125–127
A B
Fig. 1—24-year-old woman with normal anterior hip.
A, Ultrasound image with transducer in sagittal oblique plane long axis to femoral neck (N) shows femoral head (H), acetabulum (A), labrum (curved arrow), and anterior
capsule (arrowhead). Note reflected capsule (straight arrow) over femoral neck.
B, Ultrasound image with transducer in transverse plane over femoral head (H) shows iliopsoas muscle (IP) and tendon (arrow). S = sartorius.
(Fig. 1 continues on next page)
518 AJR:205, September 2015
Ultrasound of the Groin
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
C
Fig. 1 (continued)—24-year-old woman with normal anterior hip. Fig. 2—19-year-old woman with pigmented
C, Ultrasound image with transducer in transverse oblique plane over ilium shows villonodular synovitis. Ultrasound image with
psoas major muscle (Pm) and tendon (Pt) and rectus femoris direct head (RF). Note transducer in oblique sagittal plane long axis to
lateral (Im-L) and medial (Im-M) muscle fibers of iliacus with interposed septation femoral neck (N) shows heterogeneous hypoechoic
(arrowhead). AIIS = anterior inferior iliac spine, V = femoral vein. synovial hypertrophy (arrows) that predominantly
distends anterior recess. Note bone erosion
(arrowheads). H = femoral head.
Fig. 3—17-year-old girl with labral detachment and paralabral cyst. Ultrasound Fig. 4—38-year-old woman with rectus femoris calcific tendinosis. Ultrasound
image with transducer in oblique sagittal plane long axis to femoral neck shows image in sagittal plane shows calcium hydroxyapatite deposition (arrow) within
labrum (asterisk) that is detached (arrow) from acetabulum (A) and associated direct head of rectus femoris (arrowheads). Note close proximity of calcium
paralabral cyst (arrowheads). H = femoral head. hydroxyapatite to femoral head (H). AIIS = anterior inferior iliac spine.
Fig. 5—40-year-old man with common aponeurosis injury. Ultrasound image with
transducer in sagittal oblique plane over pubis (P) shows hypoechoic thickening of
common aponeurosis (straight arrows) associated with cortical irregularity. Note
adductor longus tendon (arrowheads) and rectus abdominis (curved arrow).
AJR:205, September 2015 519
Jacobson et al.
Fig. 6—Illustrations of inguinal region without and with
hernias. (Drawing by Dobbs D, used with permission)
A, Illustration of anterior inguinal region shows rectus
abdominis (R), inferior epigastric vessels (arrowhead),
and inguinal ligament (curved arrow), which outlines
Hesselbach triangle (H). Note deep inguinal ring
(straight arrow) at origin of inguinal canal.
B, Illustration shows direct inguinal hernia at
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
Hesselbach triangle (arrowhead); indirect inguinal
hernia with bowel extending through deep ring,
inguinal canal, and superficial ring (curved arrow);
and femoral hernia extending through femoral canal
(straight arrow). Note direction of specific hernias
during Valsalva maneuver, with direct inguinal hernia
moving anterior, indirect inguinal hernia moving
medial and to lesser extent inferior, and femoral
hernia moving inferior.
A B
A B
Fig. 7—31-year-old man with right-sided indirect inguinal hernia.
A, Ultrasound image with transducer in axial oblique plane long axis to inguinal
canal during Valsalva maneuver shows fat-containing indirect inguinal hernia
(white arrows) traversing internal ring (arrowheads) lateral to epigastric and
external iliac vessels (V) and coursing medial parallel to skin surface within
inguinal canal; left side of image is lateral. Black arrow indicates direction of
movement. See Video S1, a supplemental video; it can be viewed in AJR electronic
supplement to this article, available at www.ajronline.org.
B and C, Ultrasound image (B) and illustration (C) in sagittal oblique plane short
axis to inguinal canal during Valsalva maneuver show indirect hernia in short axis
(straight arrows) adjacent to spermatic cord (curved arrow) in inguinal canal; left
side of image is cephalad. Wavy arrow points to normal intraabdominal contents.
See Video S2. (Drawing by Dobbs D, used with permission)
C
520 AJR:205, September 2015
Ultrasound of the Groin
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
A B
C D
Fig. 8—63-year-old man with right-sided direct inguinal hernia.
A, Ultrasound image in transverse plane over Hesselbach triangle shows direct inguinal hernia (white arrows)
extending in posterior-to-anterior direction during Valsalva maneuver, medial to inferior epigastric and external
iliac vessels (V); left side of image is lateral. Black arrow indicates direction of movement. See Video S3 in AJR
electronic supplement to this article, available at www.ajronline.org.
B and C, Axial MR images obtained during rest (B) and Valsalva maneuver (C) show direct inguinal hernia (white
arrows, C) medial to vasculature (V) extending anterior (arrowhead, C) during Valsalva maneuver with black
arrow indicating direction of hernia. Note bowel-containing left direct inguinal hernia with gas (black arrow, C).
D, Ultrasound image in sagittal plane over Hesselbach triangle shows focal direct inguinal hernia (straight
white arrows) and adjacent spermatic cord (curved arrow); left side of image is cephalad. Straight black arrow
indicates posterior-to-anterior direction of hernia in continuity with intraabdominal contents (wavy arrow). See
Video S4.
E, Sagittal MR image obtained during Valsalva maneuver shows focal anterior movement (black arrow) of
intraabdominal contents through Hesselbach triangle (straight white arrows). Note spermatic cord (curved arrow).
E (Fig. 8 continues on next page)
AJR:205, September 2015 521
Jacobson et al.
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
F G
Fig. 8 (continued)—63-year-old man with right-sided direct inguinal hernia.
F and G, Illustrations in sagittal plane obtained during rest (F) and Valsalva maneuver (G) show focal and anterior movement of direct inguinal hernia (straight arrows, G) in
continuity with intraabdominal contents (wavy arrow). Curved arrow = spermatic cord. (Drawings by Dobbs D, used with permission)
Fig. 9—42-year-old man with right-sided pseudodirect inguinal hernia.
A, Ultrasound image with transducer in transverse plane over Hesselbach triangle
during Valsalva maneuver shows normal intraabdominal contents (arrows), medial to
inferior epigastric and external iliac vessels (V); left side of image is lateral. See Video
S5 in AJR electronic supplement to this article, available at www.ajronline.org.
B and C, Ultrasound image (B) and illustration (C) in sagittal plane over
Hesselbach triangle during Valsalva maneuver show diffuse movement of normal
intraabdominal contents without focal anterior movement, bulge, or hernia (wavy
arrows); left side of image is cephalad. Curved arrow = spermatic cord. See Video
S6. (Drawing by Dobbs D, used with permission)
A
B C
522 AJR:205, September 2015
Ultrasound of the Groin
Downloaded from www.ajronline.org by 190.189.5.219 on 10/26/17 from IP address 190.189.5.219. Copyright ARRS. For personal use only; all rights reserved
A B
Fig. 10—59-year-old woman with right-sided femoral hernia.
A, Ultrasound image in transverse plane inferior to inguinal ligament with transducer over femoral canal shows focal femoral hernia (arrows)
compressing femoral vein (V) during Valsalva maneuver. A = femoral artery; left side of image is lateral. See Video S7 in AJR electronic
supplement to this article, available at www.ajronline.org.
B, Ultrasound image in sagittal plane with transducer over femoral canal and medial to femoral vasculature shows focal femoral hernia
(white arrows) during Valsalva maneuver. Black arrow indicates inferior direction of movement during Valsalva maneuver; left side of image
is cephalad. See Video S8.
F O R YO U R I N F O R M AT I O N
A data supplement for this article can be viewed in the online version of the article at: www.ajronline.org.
AJR:205, September 2015 523
You might also like
- Transabdominal Sonography in Assessment of The Bowel in AdultsDocument16 pagesTransabdominal Sonography in Assessment of The Bowel in AdultsСергей СадовниковNo ratings yet
- Inguinal Hernia Ultrasound 2Document6 pagesInguinal Hernia Ultrasound 2savingtaviaNo ratings yet
- Probyn L. 2023. High-Resolution US in Evaluation Adult Hip.Document16 pagesProbyn L. 2023. High-Resolution US in Evaluation Adult Hip.Javier MartinNo ratings yet
- VALUE OF SONOGRAPHY IN Determining The Nature of Pleural EFUSION 1991Document5 pagesVALUE OF SONOGRAPHY IN Determining The Nature of Pleural EFUSION 1991waldemar russellNo ratings yet
- Examen Fisico RodillaDocument10 pagesExamen Fisico RodillaURGENCIAS HUSRTNo ratings yet
- Radiological Anatomy of The Colon and Rectum in Children: Gastroenterology & Hepatology: Open AccessDocument5 pagesRadiological Anatomy of The Colon and Rectum in Children: Gastroenterology & Hepatology: Open AccesseugeniaNo ratings yet
- Jum 2004 23 1 73 PDFDocument11 pagesJum 2004 23 1 73 PDFNam LeNo ratings yet
- Mesenteric Cyst in InfancyDocument27 pagesMesenteric Cyst in InfancySpica AdharaNo ratings yet
- Deal Arcon 2012Document7 pagesDeal Arcon 2012Alif BareizyNo ratings yet
- Ajr 17 19378Document13 pagesAjr 17 19378heryanggunNo ratings yet
- Ultrasonographic Evaluation of The Coxofemoral Joint Region in Young FoalsDocument6 pagesUltrasonographic Evaluation of The Coxofemoral Joint Region in Young FoalsNathalia PedrazaNo ratings yet
- Original Report: Sonographic and MR Imaging Findings of Testicular Epidermoid CystsDocument6 pagesOriginal Report: Sonographic and MR Imaging Findings of Testicular Epidermoid CystsWildaHanimNo ratings yet
- Usg 17008Document15 pagesUsg 17008Aldo VictoriaNo ratings yet
- Elasto Mama - JUm 2009Document8 pagesElasto Mama - JUm 2009cjijcNo ratings yet
- Chapter 34Document12 pagesChapter 34Haba HenrikNo ratings yet
- 07 RJR 08 Particularities of Anesthesia in ENT Endoscopic SurgeryDocument8 pages07 RJR 08 Particularities of Anesthesia in ENT Endoscopic SurgeryAyuAnatrieraNo ratings yet
- Ellenbogen Et Al 2012 Sensitivity of Gray Scale Ultrasound in Detecting Urinary Tract ObstructionDocument3 pagesEllenbogen Et Al 2012 Sensitivity of Gray Scale Ultrasound in Detecting Urinary Tract ObstructionAli AlSowaidiNo ratings yet
- Ultrasound of The Abdominal Wall and GroinDocument11 pagesUltrasound of The Abdominal Wall and Groinfahmi rosyadiNo ratings yet
- Hyperostosis CranialisDocument5 pagesHyperostosis CranialisDayang SayalamNo ratings yet
- Muscloskeletal UsDocument9 pagesMuscloskeletal UsJERAM SINKONDENo ratings yet
- ARM UltrasoundDocument3 pagesARM Ultrasoundghnd4rkjwxNo ratings yet
- Sonego 2014Document6 pagesSonego 2014Isabella WilkeNo ratings yet
- Proposal of Measurement of Vertical Larynx Position at RestDocument5 pagesProposal of Measurement of Vertical Larynx Position at RestianekinNo ratings yet
- Ultrasonographic Appearance and Histopathological Findings of The Genital Tract in Healthy Nulliparous Female RabbitsDocument10 pagesUltrasonographic Appearance and Histopathological Findings of The Genital Tract in Healthy Nulliparous Female RabbitsAkın SeverNo ratings yet
- Accuracy of Physical Examination in Subacromial Impingement SyndromeDocument5 pagesAccuracy of Physical Examination in Subacromial Impingement SyndromeClaudia BuitragoNo ratings yet
- Archives of Oral Biology: ArticleinfoDocument6 pagesArchives of Oral Biology: Articleinfoمحمد عبدالرحمنNo ratings yet
- US LumbarDocument11 pagesUS LumbarNAOMI ZAVALA LENDOSNo ratings yet
- Ultrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Document9 pagesUltrasound Imaging of Bowel Pathology - Technique and Keys To Diagnosis in The Acute Abdomen, 2011Сергей СадовниковNo ratings yet
- Ultrasonography of Soft Tissue - Oops LesionsDocument9 pagesUltrasonography of Soft Tissue - Oops LesionsMauricio RuizNo ratings yet
- The Anteroposterior Pelvic RadiographDocument10 pagesThe Anteroposterior Pelvic Radiographharo.r9524No ratings yet
- Imaging of Postpartum Complications: A Multimodality ReviewDocument12 pagesImaging of Postpartum Complications: A Multimodality ReviewGabriela Serra del CarpioNo ratings yet
- Muscle Misuse Voice Disorder Description and ClassificationDocument7 pagesMuscle Misuse Voice Disorder Description and Classificationmaya_15_128403No ratings yet
- Science - Adf8009 Genetic ArchitectureDocument13 pagesScience - Adf8009 Genetic ArchitectureHua Hidari YangNo ratings yet
- Facial UltrassomDocument7 pagesFacial UltrassomcarlosNo ratings yet
- Diagnostic Procedures in Gynecology (2023)Document3 pagesDiagnostic Procedures in Gynecology (2023)RONALDO CUANo ratings yet
- Urologie - Bencherki Youssef - Giant Abscessed Urachal in AdultDocument1 pageUrologie - Bencherki Youssef - Giant Abscessed Urachal in AdultYoussef BencherkiNo ratings yet
- Skill Paper 3Document1 pageSkill Paper 3SHAHBAZ AHMADNo ratings yet
- Skeletal Development of The Proximal Humerus in The Pediatric Population: MRI FeaturesDocument10 pagesSkeletal Development of The Proximal Humerus in The Pediatric Population: MRI Featuresahmed doweidarNo ratings yet
- Sonography of Shoulder Impingement SyndromeDocument5 pagesSonography of Shoulder Impingement Syndromeapi-263772125No ratings yet
- Cervical AuscutationDocument18 pagesCervical AuscutationCristian Camilo HERNANDEZ PEREZNo ratings yet
- Feline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Document14 pagesFeline Abdominal Ultrasonography: What'S Normal? What'S Abnormal?Ветеринарная хирургия Dvm Тозлиян И. А.No ratings yet
- AOCC IUS Primer Training Module Chapter 7Document14 pagesAOCC IUS Primer Training Module Chapter 7chengyucheung92No ratings yet
- Vocal Fold Insuf Ficiency: Medialization Laryngoplasty Vs Calcium Hydroxylapatite Microspheres (Radiesse Voice)Document6 pagesVocal Fold Insuf Ficiency: Medialization Laryngoplasty Vs Calcium Hydroxylapatite Microspheres (Radiesse Voice)Dr. Hilder HernandezNo ratings yet
- Chest - Diaphragmatic Motion Studied by M-Mode Ultrasonography Methods, Reproducibility, and Normal Values PDFDocument10 pagesChest - Diaphragmatic Motion Studied by M-Mode Ultrasonography Methods, Reproducibility, and Normal Values PDFnirchennNo ratings yet
- Basic Investigations: Endoscopy, X-Ray, Mri, EcgDocument6 pagesBasic Investigations: Endoscopy, X-Ray, Mri, EcgAndrei DragosNo ratings yet
- Journal of Oral Biology and Craniofacial ResearchDocument4 pagesJournal of Oral Biology and Craniofacial ResearchRafika OljNo ratings yet
- The Fetal Cerebellar Vermis Assessmentfor Abnormal Developmentby Ultrasonographyand Magnetic Resonance ImagingDocument14 pagesThe Fetal Cerebellar Vermis Assessmentfor Abnormal Developmentby Ultrasonographyand Magnetic Resonance ImagingThienMinhCaoNo ratings yet
- Ultrasonographic Atlas of Splenic LesionsDocument14 pagesUltrasonographic Atlas of Splenic LesionsFlavio RojasNo ratings yet
- Heary RF Bebawee RS The History and Overview of Spinal Deformity Heary RF Albert TJ Editors Spinal Deformities The Essentials Thieme 2014 p2-13 PDFDocument12 pagesHeary RF Bebawee RS The History and Overview of Spinal Deformity Heary RF Albert TJ Editors Spinal Deformities The Essentials Thieme 2014 p2-13 PDFCesar SosaNo ratings yet
- Percutaneous Computed-Tomography-Guided Biopsy of The Spine: 229 ProceduresDocument6 pagesPercutaneous Computed-Tomography-Guided Biopsy of The Spine: 229 ProceduresMarcelo MudoNo ratings yet
- Lin 2017Document11 pagesLin 2017Ibnu CaesarNo ratings yet
- Female Perineal Diseases: Spectrum of Imaging FindingsDocument20 pagesFemale Perineal Diseases: Spectrum of Imaging FindingsBayar A. AhmedNo ratings yet
- S DI 07052019 BoneDensityMeasurementsDocument22 pagesS DI 07052019 BoneDensityMeasurementsDian Angraeni WidiastutiNo ratings yet
- Practical Approach To Linear Endoscopic Ultrasound Examination of The Rectum and Anal CanalDocument10 pagesPractical Approach To Linear Endoscopic Ultrasound Examination of The Rectum and Anal CanalERICSON ARCANANo ratings yet
- J Ultrasmedbio 2014 12 509Document1 pageJ Ultrasmedbio 2014 12 509Mahatria RajNo ratings yet
- High Grade Infective Spondylolisthesis oDocument4 pagesHigh Grade Infective Spondylolisthesis oyaneemayNo ratings yet
- USG Hernia ScrotalisDocument4 pagesUSG Hernia ScrotalisStevent RichardoNo ratings yet
- Ultrasound Guided Caudal Epidural Injection.9Document2 pagesUltrasound Guided Caudal Epidural Injection.9Jevi Wahyoe NouviyantiNo ratings yet
- How Did Paul Nogier Establish The Map of The Ear PDFDocument9 pagesHow Did Paul Nogier Establish The Map of The Ear PDFHolística SarasvatiNo ratings yet
- Hernia BibleDocument24 pagesHernia BibleKevin ReyesNo ratings yet
- Clinical Examination - Karen Notes - SHIRI For BD DoctorsDocument11 pagesClinical Examination - Karen Notes - SHIRI For BD DoctorsHelp LineNo ratings yet
- 4.2 Abdominal Wall Hernia (Jerome Villacorta's Conflicted Copy 2014-03-22)Document7 pages4.2 Abdominal Wall Hernia (Jerome Villacorta's Conflicted Copy 2014-03-22)Miguel C. DolotNo ratings yet
- Pediatrics Final2021Document165 pagesPediatrics Final2021TayaNo ratings yet
- Abdominal Wall Hernias - Gastrointestinal Emergencies - Merck Manual Home EditionDocument4 pagesAbdominal Wall Hernias - Gastrointestinal Emergencies - Merck Manual Home EditionAdreiTheTripleANo ratings yet
- GIT DisordersDocument161 pagesGIT DisordersAddisu SertsuNo ratings yet
- Development Reproductive SystemsDocument59 pagesDevelopment Reproductive SystemsAli AbdElnaby SalimNo ratings yet
- 100 Gross Anatomy ConceptionsDocument231 pages100 Gross Anatomy ConceptionsChris Kristofferson100% (1)
- Iguinal Hernia Examination-1Document16 pagesIguinal Hernia Examination-1Jamshaid AhmedNo ratings yet
- HERNIADocument171 pagesHERNIATonyScaria0% (1)
- Recurrent Groin HerniaDocument6 pagesRecurrent Groin HerniaJohn-adewaleSmithNo ratings yet
- 3-Inguinal Canal PDFDocument58 pages3-Inguinal Canal PDFN A0% (1)
- HerniaDocument13 pagesHerniabugoy_bugoyNo ratings yet
- ABDOMEN124Document25 pagesABDOMEN124Ashraf Alamin AhmedNo ratings yet
- Hernia Overview of Treatment OptionsDocument5 pagesHernia Overview of Treatment OptionsKhristine Ruth De GraciaNo ratings yet
- 06 Inguinal Hernia SrsDocument10 pages06 Inguinal Hernia SrslowhillNo ratings yet
- Case Study Indirect Inguinal Hernia Left IncauceratedDocument6 pagesCase Study Indirect Inguinal Hernia Left Incauceratedstudent_019No ratings yet
- World Guidelines For Groin Hernia ManagementDocument43 pagesWorld Guidelines For Groin Hernia ManagementDaniel OctavianusNo ratings yet
- Hernia in ChildrenDocument5 pagesHernia in Childrensusheewa100% (1)
- Surgery EORDocument76 pagesSurgery EORAndrew BowmanNo ratings yet
- Tumescent TAPP Laparoscopic Inguinal Hernia RepairDocument6 pagesTumescent TAPP Laparoscopic Inguinal Hernia RepairUmer KhanNo ratings yet
- Hernia - Hernioplasty With Bilayer Polypropylene Mesh PDFDocument4 pagesHernia - Hernioplasty With Bilayer Polypropylene Mesh PDFAnonymous YLmmme4XX0No ratings yet
- PACES 3 - AbdomenDocument14 pagesPACES 3 - AbdomenDrShamshad KhanNo ratings yet
- Hernia FinalDocument21 pagesHernia FinalYeoh Shu TingNo ratings yet
- MSQ's Pediatric SurgeryDocument28 pagesMSQ's Pediatric Surgeryrohit0% (1)
- Case Hernia Inguinalis LateralisDocument15 pagesCase Hernia Inguinalis LateralisnabilahfajriahNo ratings yet
- All PackageRates (ABPMJAY) PDFDocument300 pagesAll PackageRates (ABPMJAY) PDFSumit Soni0% (1)
- 10.male Reproductive System 2 BlocksDocument220 pages10.male Reproductive System 2 BlocksANA CAROLINE ANDRADE DE MELONo ratings yet
- Hernias: Riza Pahlevi, DR., M.Si - Med., SP.B SMF Bedah Rsud MuntilanDocument34 pagesHernias: Riza Pahlevi, DR., M.Si - Med., SP.B SMF Bedah Rsud MuntilanMuhammad RizkyNo ratings yet
- HERNIIDocument4 pagesHERNIISeceleanu MarianNo ratings yet