Professional Documents
Culture Documents
Pediatric Nursing Assessment
Uploaded by
Danette Mae Roc0 ratings0% found this document useful (0 votes)
10 views7 pagesOriginal Title
11888509-Pediatric-Nursing-Assessment.doc
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views7 pagesPediatric Nursing Assessment
Uploaded by
Danette Mae RocCopyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 7
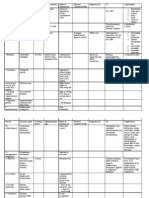
PEDIATRIC NURSING ASSESSMENT C.
Chief Concern (Narrative of Present Illness)
(Gordon’s Functional Health Pattern)
D. Wt
A. Name: Ht:
Preferred to be called: Temp: ____ (oral,axilla,rectal)
Age: Pulse _____ (regular/irregular)
Sex: Resp _____ (regular/irregular)
Time of Arrival to Unit: BP
Mode of Admission:
Mother’s Name: E. Past History
Occupation: 1. Birth History
Age: a. Mother’s health during pregnancy
Address: b. Labor and delivery
Tel. No.: c. Infant’s condition immediately after birth
Father’s Name: (APGAR)
Occupation:
Age: 2. Pregnancy, Labor and Delivery
Address: a. Obstetric history (GP, TPAL)
Tel. No: b. Crisis during pregnancy
Religion: c. Prenatal attitude toward fetus
Primary Language:
Nationality: 3. Perinatal History
a. Wt and Ht at birth
B. b. Loss of wt following birth and time of
1. Child’s Appearance & Behavior regaining birth wt
2. Parent-child interaction c. APGAR score, level of activity
3. Siblings and other family members d. Problem if any (birth injury, congenital
4. Home environment anomalies)
4. Dietary History (Feeding History) Has your child ever been in the hospital
before?
5. Immunization and boosters How was the hospital experience?
What things were important to you and
6. Developmental milestones (growth pattern) your child during that hospitalization? How
a. Approx wt at 6 mos, 1 yr, 2 yrs, 5 yrs can we be most helpful now?
b. Approx ht at 1 yr, 2 yrs, 3 yrs, 4 yrs What medications does your child take at
c. Dentition (including age of onset, home?
number of teeth and symptoms during Why are they given?
teething) When are they given?
d. Hold head steadily How are they given (if a liquid, with a
e. Sitting alone without support spoon, if a tablet, swallowed with water or
f. Walks without assistance other)?
g. Says first words Does he have any trouble taking
medication? If so, what helps?
F. Functional Health Pattern Assessment Does he have any allergies to
medications?
1. Health Perception-Health Management Pattern What does your child know about this
Why has your child been admitted? hospitalization?
How has your child’s general health been? Ask the child why he came to the hospital
What does your child know about this
hospitalization? 2. Nutritional and Metabolic Pattern
Ask the child why he came to the hospital What are the family’s usual meal times?
If answer is “For operation or for tests”, Do family members eat together or at separate
ask child to tell you about what had times?
happened before, during and after the What are your child’s favorite foods,
operation or tests beverages and snacks?
Average amounts consumed or usual size What is his usual pattern of elimination (bowel
positions movements)
Special cultural practices, such as family Do you have any concerns about elimination
eats only ethnic food (bed wetting, constipation, diarrhea)
What goods and beverages does your child What do you do for these problems?
dislike? Have you ever noticed that your child sweats a
What are his feeding habits (bottle, cup, lot?
spoon, eats by seld, needs assistance, any
special devices)? 4. Sleep-Rest Pattern
How dows the child like his food served What is your child’s usual hour of sleep and
(warm, cold, one at a time? awakening?
How would you describe his usual appetite? What is his schedule for naps/length of naps?
(hearty eater, picky eater) Is there a special routine before sleeping
Has his being sick affected your child’s (bottle, drink of water, bedtime story, nightlight,
appetite? favorite blanket, or toy or prayers)
Are there any feeding problems (excessive, Is there a special routine during sleep time
fussiness, spitting up, colic), any dental or such as walking to go to the bathroom?
gum problems that affect feeding? What type of bed does he sleep on?
What do you do with these problems? Does he have his own room or share a room:
if he shares a room, with whom?
3. Elimination Pattern What are the home sleeping arrangements
What are your child’s toilet habits? (diaper, (along or with others, such as sibling parent or
toilet trained [day only or day and night], use other person)?
of words to communicate urination and What is his favorite sleeping position?
defecation, potty chair, regular toilet, other Are there any problems awakening and getting
routines)? ready in the morning?
What do you do for these problems?
5. Activity-Exercise Pattern appliance, artificial elimination appliances,
What is your child’s schedule during the day? orthopedic devices)
(nursery school, daycare center, regular
school, extracurricular activities) Note: Use the following code to assess
What are his favorite activities or toys (both functional self care level for feeding,
active and quiet interests) bathing/hygiene, dressing/grooming, toileting:
What is his usual television-viewing schedule 0 – full self care
at home? 1 – requires use if equipment or device
What are his favorite programs? 2 – requires assistance or supervision
Are there any television restrictions? from another person and equipment or
Does your child have any illness or disabilities device
that limit his activity? If so, how? Is dependent and does not participate
What are his usual habits and schedule for
bathing? (bath in the tub or shower, sponge 6. Cognitive-Perceptual Pattern
bath, shampoo? Does your child have any hearing difficulty?
What are his dental habits (brushing, flossing, Does he use hearing aid?
fluoride supplements or rinses, favorite Have tubes been placed in your child’s
toothpaste, schedule of daily dental care) ears?
Does your child need help with dressing or Does your child have any vision problems?
grooming such as hair combing? Doe she wear eyeglasses or lenses?
Are there any problems with the above (dislike Does your child have any learning difficulties?
or refusal to bathe, shampoo hair or brush What is his grade in school?
teeth)
What do you do with these problems?
Are there special devices that your child
requires help in managing (eyeglasses,
contact lenses, hearing aid, orthodontic
7. Self Perception-Self-Concept Pattern Who usually takes care of your child during
How would you describe your child (takes time the day/night (especially if other than parent,
to adjust, settles in easily, shy, friendly, quiet, such as babysitter, relative)
talkative, serious, playful, stubborn, easy What are the parent’s occupations and work
going)? schedule?
What kinds of things make your child angry, Are there any special family considerations
annoyed, anxious or sad? What helps? (adoption, foster child, step parent, divorce,
How does your child act when he is annoyed single parent)?
or upset? Have any major changes in the family
What have been your child’s experiences with occurred lately? (death, divorce, separation,
and reactions to temporary separation from birth of a sibling, loss of job, financial strain,
you (parent)? mother beginning a career, other)? Explain
Does your child have any fears (places, child’s reaction.
objects, animals, people, situations)? How do Who are your child’s play companions or
you handle them? social group (peers, young or older children,
Do you think your child’s illness has changed adults, prefer to be alone)?
the way he thinks about himself (more shy, Do thing generally go well for your child in
embarrassed about appearance, less school or with friends?
competitive with friends, stays home more)? Does your child have security objects at home
(pacifier, thumb, bottle, blanket, stuffed animal
8. Role Relationship Pattern or doll)? Did you bring any of these to the
Does your child have a nickname he wishes to hospital?
be called? How do you handle discipline problems at
What are the names of other family members home? Are these methods always effective?
or others who live in the home (relatives, Does your child have any speech or hearing
friends, pets)? problems? If so, what are your suggestions for
communicating with him?
Will your child’s hospitalization affect family’s questions or talking about sex, nit respecting
financial support or care of other family others privacy, or wanting too much privacy)?
members, such as other children? Initiate a conversation about adolescent’s
What concerns do you have about your child’s sexual concerns with open-ended to more
illness and hospitalization? direct questions and using the terms “friends”
Who will be staying with your child while he is or “partners” rather than girlfriend or boyfriend
in the hospital? Tell me about your social life
How can we contact you or another close Who are your closest friends? (if one
family member outside of the hospital? friend is identified, could ask more about
that relationship, such as how much time
9. Sexuality-Reproductive Pattern they spend together, how serious they are
(Answer questions that apply to child’s age- about each other, if the relationship is
group) going that way the teenager hoped it
Has your child begun puberty (developing would)
physical, sexual characteristics, Might ask about dating and sexual issues,
menstruation)? Have you or your child had such as the teenager’s views on sex
any concerns? education, “going steady”, living together
Does your daughter know how to do BSE? or premarital sex
Does your child know how to do TSE? Which friends would you like to have visit
in the hospital?
Have you approached topics of sexuality with
your child? Do you feel you might need some
10. Coping Stress Tolerance Pattern
help with some topics?
If your child is tired or upset, what does he do?
Has your child’s illness affected the way he or
If he is upset, doe she have a special
she feels about being a male or female? If so,
person or object he wants?
how?
If your child has temper tantrums, what causes
Do you have any concerns with behaviors in
them and how do you handle them?
your child such as masturbation, asking many
Who does your child talk to when something is Nose – nasal flaring, epistaxis, stuffy nose
worrying him? Throat – dental condition, pharyngitis
How does your child usually handle problems Mouth – mouth breathing, gum bleeding
or disappointments? NECK – pain, limitation of movement
Has there been any big changes or problems CHEST – breast enlargement, masses
un your family recently? How did you handle RESPIRATORY – chronic cough, frequent colds
them? (#/yr)
Has your child ever ha d a problem with drugs CARDIOVASCULAR – cynosis, fatigue on
or alcohol or tried suicide? exertion, anemia, blood type, CBC, rate and rythim
Do you think your child is accident prone? If of heart
so, explain? GUT – frequency, dysuria, descent of testes
GIT – food intolerance, eating and elimination
11. Value-Belief Pattern habits, vomiting
What us your religion? GYNECOLOGIC – menarche, regularity, vaginal
How is religion or faith important in your child’s discharge
life? MUSCULOSKELETAL – weakness, clumsiness,
What religious practices would you have lack of coordination, abnormal gait, deformities,
continued in the hospital such as prayers fractures
before meals/bedtime, visit by minister, priest, NEUROLOGICAL – head, fontanels, sutures,
or rabbi, prayer group? circumference, orientation to time place and
alertness, responsiveness to reflexes
G. Physical Assessment
INTEGUMENT – intact, hygiene, rashes, H. Current Developmental Level
abrasions 1. Gross Motor Skills
EENT 2. Frame Motor Adoptive Skills
Eyes – pale, conjuctiva, PERLA 3. Language Skills
Ears – hearing, symmetry, discharge, pain 4. Personal-Social
You might also like
- Jehovah's Witnesses and Child Sex AbuseDocument178 pagesJehovah's Witnesses and Child Sex Abusesirjsslut0% (1)
- Sex and Context - Hormones and Primate Sexual MotivationDocument19 pagesSex and Context - Hormones and Primate Sexual MotivationbobbyNo ratings yet
- 11 Gordon's Functional Assessment PatternDocument2 pages11 Gordon's Functional Assessment PatternJan Christian Dayto83% (6)
- SchizophreniaDocument3 pagesSchizophreniamiss RN100% (2)
- MMDSTDocument50 pagesMMDSTmongosie60% (5)
- PVDDocument7 pagesPVDmiss RNNo ratings yet
- Performance AnxietyDocument30 pagesPerformance Anxietyhunghl9726No ratings yet
- Review of SystemsDocument2 pagesReview of SystemsDiane Gabriel100% (1)
- Benjamin BrittenDocument91 pagesBenjamin BrittenSergio Miguel MiguelNo ratings yet
- Criminal Background Checks For Prospective Foster and Adoptive Parents-2011Document65 pagesCriminal Background Checks For Prospective Foster and Adoptive Parents-2011Rick ThomaNo ratings yet
- Pedia Comprehensive Questionaire GuideDocument14 pagesPedia Comprehensive Questionaire GuideMarimiel PagulayanNo ratings yet
- Functions of Female OrgasmDocument6 pagesFunctions of Female OrgasmRamanasarmaNo ratings yet
- Abruptio PlacentaDocument13 pagesAbruptio Placentamiss RN92% (12)
- Charting Examples For Physical AssessmentDocument6 pagesCharting Examples For Physical AssessmentFerdos Adem90% (10)
- NCM119ClinicalLab Pediatric Ward Pneumonia Case Study Group 4Document40 pagesNCM119ClinicalLab Pediatric Ward Pneumonia Case Study Group 4Allysa MacalinoNo ratings yet
- Discharge PlanningDocument3 pagesDischarge PlanningAlex Marie100% (2)
- Nursing Health HistoryDocument9 pagesNursing Health HistoryJajangNo ratings yet
- Labor Room and DNC Chart BeghDocument3 pagesLabor Room and DNC Chart BeghTeanu Jose Gabrillo TamayoNo ratings yet
- Feminist Literary Theory A Reader by Mary Eagleton PDFDocument12 pagesFeminist Literary Theory A Reader by Mary Eagleton PDFKim MacRae33% (6)
- EDD & AOG Computation: Expected Date of Delivery & Age of GestationDocument3 pagesEDD & AOG Computation: Expected Date of Delivery & Age of GestationRam AugustNo ratings yet
- The Ritual, or Intellectual Decompression, ChamberDocument1 pageThe Ritual, or Intellectual Decompression, Chamberbroscuta23No ratings yet
- Peripheral Vascular DiseaseDocument3 pagesPeripheral Vascular Diseasemiss RN100% (4)
- Peripheral Vascular DiseaseDocument3 pagesPeripheral Vascular Diseasemiss RN100% (4)
- Children's Functional Health Pattern Assessment - Student-3Document7 pagesChildren's Functional Health Pattern Assessment - Student-3Anonymous a6mRz7WH88% (8)
- This Study Resource Was: Head-To - Toe Assessment Documentation SampleDocument2 pagesThis Study Resource Was: Head-To - Toe Assessment Documentation SampleA Sung100% (3)
- Gordon S Functional Health Pattern Assessment ToolDocument17 pagesGordon S Functional Health Pattern Assessment Toolmiss RN96% (45)
- Gordon S Functional Health Pattern Assessment ToolDocument17 pagesGordon S Functional Health Pattern Assessment Toolmiss RN96% (45)
- Stages of LaborDocument3 pagesStages of Labormiss RN100% (8)
- 125.6 (Medicine) DISCHARGE PLANDocument1 page125.6 (Medicine) DISCHARGE PLANNadja Jamilah100% (1)
- DischargeDocument3 pagesDischargeHeather100% (1)
- MMDST: Metro Manila Development Screening Test (MMDST) 4 SectorsDocument5 pagesMMDST: Metro Manila Development Screening Test (MMDST) 4 SectorsJennifer Davis Condiman100% (1)
- Chapter 24: Nursing Care of A Family During A Surgical Intervention For BirthDocument22 pagesChapter 24: Nursing Care of A Family During A Surgical Intervention For BirthAlyssaGrandeMontimorNo ratings yet
- Initial Data Base For Family Nursing PracticeDocument12 pagesInitial Data Base For Family Nursing Practicemiss RN67% (18)
- Case Study Ob WardDocument41 pagesCase Study Ob WardIan Mizzel A. Dulfina0% (2)
- IVF Color CodingDocument2 pagesIVF Color CodingLabs Mendoza100% (2)
- Soapie ChartingDocument2 pagesSoapie ChartingMica Omotsosirc100% (1)
- Gordon's Functional Pattern PneumoniaDocument6 pagesGordon's Functional Pattern PneumoniaLei Ortega86% (14)
- Compilation of Pedia NotesDocument56 pagesCompilation of Pedia Notestempter_10100% (2)
- NCP Ineffective ThermoregulationDocument4 pagesNCP Ineffective ThermoregulationCharmae Navea100% (1)
- Instruments in The Delivery RoomDocument6 pagesInstruments in The Delivery RoomRenea Joy Arruejo0% (1)
- DischargeDocument4 pagesDischargePatricia Franco100% (1)
- Gordons Functional Health PatternDocument8 pagesGordons Functional Health PatterniamjenivicNo ratings yet
- Focus Data ChartingDocument3 pagesFocus Data ChartingcattleyaNo ratings yet
- Gordons PediaDocument2 pagesGordons PediaRachell SamsonNo ratings yet
- Head To Toe AssessmentDocument2 pagesHead To Toe AssessmentBen0% (1)
- Psychoanalysis of ChildrenDocument407 pagesPsychoanalysis of ChildrenHCami2100% (1)
- Gordon's 11 Functional Health PatternsDocument4 pagesGordon's 11 Functional Health PatternsRenalyn LalanganNo ratings yet
- Gordon S Health AssessmentDocument13 pagesGordon S Health AssessmentMaria Visitacion100% (3)
- Gordon's Bisaya VersionDocument2 pagesGordon's Bisaya VersionDanielle Valerie100% (1)
- Placenta PreviaDocument6 pagesPlacenta Previamiss RN93% (14)
- Gordon's Functional Health Pattern SampleDocument4 pagesGordon's Functional Health Pattern SampleSheila_Marie_L_45075% (4)
- MMDST Output.Document7 pagesMMDST Output.Jhen JhenNo ratings yet
- Childrens Functional Health Pattern AssessmentDocument5 pagesChildrens Functional Health Pattern AssessmentAnonymous d7DpEo3100% (4)
- Health Teaching PlanDocument2 pagesHealth Teaching Plankristel_nicole18yahoNo ratings yet
- Gordon's 11 Functional Health PatternDocument3 pagesGordon's 11 Functional Health Patternbladimer_ria100% (3)
- Metro Manila Development Screening TestDocument4 pagesMetro Manila Development Screening TestKath100% (6)
- Cephalocaudal and System ApproachDocument22 pagesCephalocaudal and System ApproachitsmeayaNo ratings yet
- Osteogenesis ImperfectaDocument6 pagesOsteogenesis Imperfectamiss RN100% (2)
- MMDST FormDocument3 pagesMMDST FormJulianne B. Dela CruzNo ratings yet
- Gordons 11 Functional Patterns..QuestionsDocument1 pageGordons 11 Functional Patterns..Questionsmiss RN81% (32)
- Cast and TractionsDocument6 pagesCast and Tractionsmiss RN100% (12)
- Questionnaire On The Perception of College Students Toward Sogie Equality BillDocument1 pageQuestionnaire On The Perception of College Students Toward Sogie Equality BillHaesoo Shii100% (1)
- Hepatic EncephalopathyDocument10 pagesHepatic Encephalopathymiss RN100% (1)
- Functional Health Pattern AssessmentDocument3 pagesFunctional Health Pattern Assessmentsheinelle82% (11)
- RatirahasyaDocument3 pagesRatirahasyaIoan-ovidiu Cordis100% (1)
- Nurses NotesDocument2 pagesNurses NotesAvyel Kram100% (3)
- PrioritizationDocument9 pagesPrioritizationmiss RN100% (4)
- FDARDocument7 pagesFDARCatherine Casas Borbon50% (2)
- 8 Point Postpartum Assessment WorksheetDocument2 pages8 Point Postpartum Assessment WorksheetSoni Ali100% (2)
- Nursing Diagnosis and Nursing Interventions For HirschsprungDocument5 pagesNursing Diagnosis and Nursing Interventions For HirschsprungAhmed Altrafe100% (2)
- MMDSTDocument70 pagesMMDSTIrwan M. IskoberNo ratings yet
- Date/Time Focus Progress Notes: October 8, 2020 11:00 PMDocument1 pageDate/Time Focus Progress Notes: October 8, 2020 11:00 PMRyll Johnson50% (2)
- Fdar UTIDocument2 pagesFdar UTINickaela CalalangNo ratings yet
- Nursing Health History of ReyDocument3 pagesNursing Health History of ReyElaine Joy Calma Canlas100% (1)
- Risk For Hypothermia of New BornDocument2 pagesRisk For Hypothermia of New BornjenspryNo ratings yet
- FdarDocument1 pageFdarEloisa Claire DayananNo ratings yet
- Cephalocaudal Assessment (Cen)Document4 pagesCephalocaudal Assessment (Cen)Kristine Young100% (1)
- n320 Peds NCP wk3Document2 pagesn320 Peds NCP wk3api-301826049No ratings yet
- 870 Nursing Admission History According To Functional Health PatternsDocument2 pages870 Nursing Admission History According To Functional Health PatternsBooz ChannelNo ratings yet
- Nursing Assessment - Pediatric Clients in The Community New 1 1Document7 pagesNursing Assessment - Pediatric Clients in The Community New 1 1Ugalde AlyssakyleNo ratings yet
- Functional Health Pattern AssessmentDocument3 pagesFunctional Health Pattern AssessmentDanette Mae RocNo ratings yet
- Interview QsDocument15 pagesInterview Qsjae jaeNo ratings yet
- Gordons 11 Functional Health PatternsDocument2 pagesGordons 11 Functional Health PatternsCathryn luv QuisidoNo ratings yet
- INTAKE FORM From Parents Ver 2022Document4 pagesINTAKE FORM From Parents Ver 2022Reymart PalaganasNo ratings yet
- Interview Guide For Nursing Health HistoryDocument3 pagesInterview Guide For Nursing Health HistoryDersly LaneNo ratings yet
- Peripheral Arterial DseDocument2 pagesPeripheral Arterial Dsemiss RNNo ratings yet
- Tuberculosis PathophysiologyDocument1 pageTuberculosis Pathophysiologymiss RN100% (15)
- Subdural HematomaDocument7 pagesSubdural Hematomamiss RN50% (2)
- Respiratory Anatomy Physiology and Dse DefinitionDocument4 pagesRespiratory Anatomy Physiology and Dse Definitionmiss RN100% (2)
- Coxa Plana PathophysiologyDocument1 pageCoxa Plana Pathophysiologymiss RN100% (4)
- NCP Quadriplegia ParaplegiaDocument3 pagesNCP Quadriplegia Paraplegiamiss RN50% (2)
- DysphagiaDocument1 pageDysphagiamiss RN100% (1)
- A. Community Structure, Characteristics and Dynamics: 5 6 A B C D E F G HDocument7 pagesA. Community Structure, Characteristics and Dynamics: 5 6 A B C D E F G Hmiss RNNo ratings yet
- Figure 1. Number of Students Studying Before An ExamDocument8 pagesFigure 1. Number of Students Studying Before An Exammiss RNNo ratings yet
- Case Presentation Lab ResultsDocument2 pagesCase Presentation Lab Resultsmiss RNNo ratings yet
- Communicable DiseaseDocument3 pagesCommunicable Diseasemiss RNNo ratings yet
- Case Presentation Lab ResultsDocument2 pagesCase Presentation Lab Resultsmiss RNNo ratings yet
- BJ - Spears: Loaded 1676 TweetsDocument65 pagesBJ - Spears: Loaded 1676 Tweetsbibob3ab dsNo ratings yet
- Human Reproduction Class 12 Notes Biology - MyCBSEguide - CBSE Papers & NCERT SolutionsDocument11 pagesHuman Reproduction Class 12 Notes Biology - MyCBSEguide - CBSE Papers & NCERT SolutionsMansiMalhotra0% (1)
- Part 1 Exam in UtsDocument9 pagesPart 1 Exam in UtsWOOD VNo ratings yet
- Nirvana/ Deleuze: Bodies Without OrgansDocument11 pagesNirvana/ Deleuze: Bodies Without OrgansLeandros CorieltauvorumNo ratings yet
- Pomegranate Flower TypeDocument10 pagesPomegranate Flower TypeAki FujikawaNo ratings yet
- Advantages of Co EducationDocument17 pagesAdvantages of Co EducationafzalNo ratings yet
- Massachusetts Alliance On Teen Pregnancy ReportDocument16 pagesMassachusetts Alliance On Teen Pregnancy ReportGreg SaulmonNo ratings yet
- German Modern Architecture Adn The Modern WomanDocument24 pagesGerman Modern Architecture Adn The Modern WomanUrsula ColemanNo ratings yet
- 20 Ways To Avoid SexualDocument3 pages20 Ways To Avoid SexualO Allen Boane100% (1)
- Notes lt-ms-ls3-2Document4 pagesNotes lt-ms-ls3-2api-420503879No ratings yet
- Final Report On The Safety Assessment of 2-PhenoxyethanolDocument19 pagesFinal Report On The Safety Assessment of 2-PhenoxyethanolF4ARNo ratings yet
- Kylie - Andrealphus GamesDocument1 pageKylie - Andrealphus GamesNyan ThutaNo ratings yet
- Homeroom ActivityDocument8 pagesHomeroom ActivityClarence HubillaNo ratings yet
- Iud Contraception: MK: Bahasa Inggris Terapan Dosen Pengampu: I Made Rai Jayawidanta, SS., M.HumDocument4 pagesIud Contraception: MK: Bahasa Inggris Terapan Dosen Pengampu: I Made Rai Jayawidanta, SS., M.HumMilla ArtiniNo ratings yet
- Marks Wise Questions CH-1Document27 pagesMarks Wise Questions CH-1lakshshah5116No ratings yet
- Public Toilets Remain One of The Few Sex-Segregated Spaces LeftDocument15 pagesPublic Toilets Remain One of The Few Sex-Segregated Spaces LefthillelNo ratings yet
- 172nd Report Law Commission of IndiaDocument54 pages172nd Report Law Commission of IndiaKrishna PratapNo ratings yet
- Efectos de La Exposición A La Pornografía en Las Tendencias de Comportamiento Agresivo en HombresDocument10 pagesEfectos de La Exposición A La Pornografía en Las Tendencias de Comportamiento Agresivo en HombresMaria Del Carmen Chavez LamasNo ratings yet
- Domesticating The Yogyakarta Principles in Kenya Human Rights Training ManualDocument62 pagesDomesticating The Yogyakarta Principles in Kenya Human Rights Training ManualRyan Ubuntu OlsonNo ratings yet