Professional Documents
Culture Documents
Varicella Zoster (Chickenpox) : Frequently Asked Questions
Uploaded by
Muhammad mukram0 ratings0% found this document useful (0 votes)
10 views2 pageskfkefj
Original Title
2.. 311271698-Referat-Osteoarthritis
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentkfkefj
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views2 pagesVaricella Zoster (Chickenpox) : Frequently Asked Questions
Uploaded by
Muhammad mukramkfkefj
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
COMPILED JUNE 2017
OUTBREAK RESPONSE, DIVISION OF PUBLIC HEALTH SURVEILLANCE AND RESPONSE
Varicella Zoster (Chickenpox)
Frequently Asked Questions
1. What is chickenpox?
Chickenpox is an infectious disease characterized by fever and a blister-like rash caused by
varicella-zoster virus (VZV). A first infection with VZV causes chickenpox. After recovery from
chickenpox, the virus can be dormant (inactive or latent) in a nerve root (specifically the dorsal
root ganglion of a sensory nerve). Reactivation of latent infection causes herpes zoster
(shingles) – a localized, painful blister-like rash, in the area supplied by that nerve. Typically
shingles occurs on the trunk, or face, on either the left or right side of the body, not both sides
2. Who can get chickenpox?
A person of any age can catch chickenpox if they have not had it previously, or if they have
not been vaccinated . The risk of catching chickenpox is higher in those who work in or attend
a school or child care facility or live with children.
3. Where does chickenpox occur in South Africa?
Chickenpox occurs across socio-economic groups and geographical regions in South Africa.
Almost 90% of adults in a seroprevalence study of HIV infected ART-naïve patients had
evidence of previous varicella infection. Globally almost 80% of persons are infected by 10
years of age.
4. How is chickenpox transmitted?
Varicella zoster virus is airborne and highly contagious. Approximately 90% of close contacts
who are non-immune will catch chickenpox after exposure to persons with disease. A person
with varicella is contagious from 1-2 days before rash onset until the sores have crusted. The
incubation period is approximately 10-21 (mean 14-16) days after exposure to the virus. VZV
can be spread from person to person by through infected respiratory secretions (coughing,
sneezing) that are aerosolized
5. What are the signs and symptoms of chickenpox?
Fever and malaise (feeling ill) may occur 1 to 2 days before rash onset, particularly in adults.
In children, the rash is often the first sign of disease. The rash usually appears first on the head,
chest, and back then spreads to the rest of the body. The rash is itchy and progresses rapidly
from flat sores to fluid-filled blisters before crusting. Asymptomatic infection (without rash,
or with very few blisters) may occur. Classically, lesions appear in crops, and are therefore
present in different stages of development – some at the papule, others at the blister and still
others at the crusted stage.
6. What are the complications of chickenpox?
Document FAQ_ Varicella Zoster (Chickenpox)_20170714 Page 1 of 2
In children, secondary bacterial infections of the skin lesions is the most common
complication, usually due to Staphylococcus aureus. In adults, pneumonia is a relatively
common complication. Severe complications are rare, but include septicaemia (blood stream
bacterial infection often due to Streptococcus pyogenes), toxic shock syndrome, infection of
soft tissues, bones or joints (necrotizing fasciitis, osteomyelitis septic arthritis), brain infection
(cerebellar ataxia, encephalitis). People at high risk for complications or severe infections
include immunocompromised persons, people with HIV or AIDS and pregnant women.
Infection during the 1st or early 2nd trimester of pregnancy may occasionally cause
complications in the baby called congenital varicella syndrome. Symptoms of congenital
varicella syndrome include scarring on the skin, smaller than usual limbs, a small head
(microcephaly) and low birth weight. Mortality following varicella is lowest for children
(1/100,000 cases) but higher for adults (25/100,000 cases)
7. How is chickenpox diagnosed?
Chicken pox is mostly diagnosed clinically without the need for laboratory testing. PCR for
varicella virus on a swab of vesicle fluid is confirmatory. A blood test for antibodies (serology)
can be positive. A rise in IgG titre is confirmatory. IgM testing is not recommended. The
differential diagnosis for varicella includes enteroviral infections, commonly due to coxsackie
A virus, unusual presentations of HSV1/2 or impetigo.
8. How is chickenpox treated?
Chickenpox typically requires no medical treatment and the disease is allowed to run its
course. Lotions, such as calamine lotion, can be applied to the skin to ease itching. Persons
with severe infection may be treated with an anti-viral medication acyclovir, or valacyclovir
9. How is chickenpox prevented?
Most adults in South Africa are immune (protected) to chicken pox because they have been
infected as children. Adults who do not recall having had chickenpox as a child may have a
test for antibodies (serology) to determine if they are immune. Vaccination against varicella is
not part of the Expanded Programme of Immunisation in South Africa, but is indicated for
children and adults in high risk categories. No official guidelines exist regarding vaccination. A
varicella vaccine is available in the private sector as a monovalent vaccine or co-formulated
with other live-attenuated vaccines measles, mumps and rubella. The ideal age of vaccination
is between 12-15 months.
10. Where can I find out more information
For the Public:
http://www.cdc.gov/chickenpox/index.html
For Healthcare Workers: http://www.cdc.gov/chickenpox/hcp/index.html
Contact the NICD hotline in emergency situations
For more information contact Center for Vaccines and Immunology:
Dr Villyen Motaze
Tel: +2711386640 Email: villyenm@nicd.ac.za
Document FAQ_ Varicella Zoster (Chickenpox)_20170714 Page 2 of 2
You might also like
- Interpretation: L55 - PSC Jayanagar Home Visit Municipal New No.42, Old No 825, Ground, W K P Road, 7Th Block, JayanagarDocument2 pagesInterpretation: L55 - PSC Jayanagar Home Visit Municipal New No.42, Old No 825, Ground, W K P Road, 7Th Block, JayanagardrmohangNo ratings yet
- Essay Claim of Policy HIV AIDSDocument2 pagesEssay Claim of Policy HIV AIDSdiary_anteNo ratings yet
- Chicken-Pox Concept MapDocument4 pagesChicken-Pox Concept MapElle0% (1)
- VaricellachickenpoxDocument6 pagesVaricellachickenpoxDedi SofyanNo ratings yet
- This Is A Document About Chicken PoxDocument24 pagesThis Is A Document About Chicken Poxarul100% (1)
- Signs and Symptoms: Chickenpox Is A HighlyDocument4 pagesSigns and Symptoms: Chickenpox Is A HighlysaaaraelleNo ratings yet
- Chickenpox Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With Varicella ZosterDocument12 pagesChickenpox Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With Varicella Zostersubbu2raj3372100% (2)
- Vaccinated Persons: Other Typical Symptoms That May Begin To Appear 1-2 Days Before Rash IncludeDocument5 pagesVaccinated Persons: Other Typical Symptoms That May Begin To Appear 1-2 Days Before Rash IncludePrimita Ayu DamayantiNo ratings yet
- ChickenpoxDocument16 pagesChickenpoxJeet ThuraiNo ratings yet
- Varicella/Herpes Zoster: Communicable Disease Management ProtocolDocument0 pagesVaricella/Herpes Zoster: Communicable Disease Management ProtocolJohn StenlyNo ratings yet
- Background: Pediatric Chickenpox Next Section: PathophysiologyDocument12 pagesBackground: Pediatric Chickenpox Next Section: PathophysiologyRachel Johann Aquinto100% (1)
- Home Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentDocument50 pagesHome Visual Library Resources News Resources Mobile Subscribe Contact Skip To Main Page ContentAnastasia Lilian SuryajayaNo ratings yet
- Viral Infection: NAME-Rahul Pawar (Roll No.17) Sanket Joshi (Roll No.25)Document25 pagesViral Infection: NAME-Rahul Pawar (Roll No.17) Sanket Joshi (Roll No.25)aditya_aditya_mayekar199No ratings yet
- PAEDS 4 - 18.10.19 Viral InfectionDocument15 pagesPAEDS 4 - 18.10.19 Viral Infectionlotp12No ratings yet
- Chickenpox and SmallpoxDocument28 pagesChickenpox and SmallpoxFourth YearNo ratings yet
- Fwd. Epi 8Document40 pagesFwd. Epi 8Sumayya ChughtaiNo ratings yet
- Chickenpox, Shingles, and Herpes PathophysiologyDocument29 pagesChickenpox, Shingles, and Herpes PathophysiologyKim SunooNo ratings yet
- Kutis PorcelanaDocument34 pagesKutis Porcelanaapi-3743483No ratings yet
- Tuberculosis 1. Background of The Problem Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With VaricellaDocument6 pagesTuberculosis 1. Background of The Problem Chickenpox Is A Highly Contagious Disease Caused by Primary Infection With VaricellaFkrygeustobat Tikamarimunteupercaya TanyakeunkajalminaNo ratings yet
- Varicella/Herpes Zoster: Communicable Disease Management ProtocolDocument5 pagesVaricella/Herpes Zoster: Communicable Disease Management Protocolyuliyanto.efendiNo ratings yet
- Chickenpox (Varicella) : Questions and Answers: Information About The Disease and VaccinesDocument3 pagesChickenpox (Varicella) : Questions and Answers: Information About The Disease and VaccinesKailash NagarNo ratings yet
- Chickenpox: 2008/9 Schools Wikipedia Selection Health and MedicineDocument5 pagesChickenpox: 2008/9 Schools Wikipedia Selection Health and MedicinenvijaykanthNo ratings yet
- Varicella 1. Symptoms and SignsDocument3 pagesVaricella 1. Symptoms and SignsBahar KeyNo ratings yet
- Martinon TorresDocument4 pagesMartinon TorresFiqha RosaNo ratings yet
- Herpes 3, VSVDocument21 pagesHerpes 3, VSVCharles SainzNo ratings yet
- Mayores. Chicken Pox - Concept MapDocument3 pagesMayores. Chicken Pox - Concept MapAlvic Dy KowNo ratings yet
- Chickenpox and Shingles GuideDocument32 pagesChickenpox and Shingles GuideCharlz ZipaganNo ratings yet
- History of Chickenpox Disease and VaccineDocument2 pagesHistory of Chickenpox Disease and VaccineGunel AliyevaNo ratings yet
- Varicella by Siva MurugadossDocument34 pagesVaricella by Siva MurugadossPrakask BalanNo ratings yet
- Viral Meningitis Causes, Symptoms and TreatmentDocument4 pagesViral Meningitis Causes, Symptoms and TreatmentSam TagardaNo ratings yet
- MeaslesDocument4 pagesMeaslesKailash NagarNo ratings yet
- MeaslesDocument53 pagesMeaslestummalapalli venkateswara rao100% (1)
- Fever and Rash Differential DiagnosisDocument31 pagesFever and Rash Differential DiagnosisHannan AliNo ratings yet
- Varicella ZosterDocument41 pagesVaricella Zostertummalapalli venkateswara raoNo ratings yet
- Sketsa Case ReportDocument3 pagesSketsa Case ReportnikenseptiaNo ratings yet
- Measles Virus InfectionDocument20 pagesMeasles Virus Infectionsuryanto_malvinNo ratings yet
- Varicella Zooster VirusDocument9 pagesVaricella Zooster VirusChikita Artia SariNo ratings yet
- Chickenpox What Is Chickenpox?Document19 pagesChickenpox What Is Chickenpox?s.khan9211rediffmail.comNo ratings yet
- ANTIVIRAL DRUGSDocument3 pagesANTIVIRAL DRUGSJoshua MendozaNo ratings yet
- Small PoxDocument12 pagesSmall Poxnn1216100% (1)
- Answers For MICI 1100 Final ReviewDocument16 pagesAnswers For MICI 1100 Final Reviewashley.danielngenegboNo ratings yet
- Preliminary (Pendahuluan) A. BackgroundDocument5 pagesPreliminary (Pendahuluan) A. BackgroundAbadiNo ratings yet
- Viral DiseasesDocument54 pagesViral Diseasesapi-19916399No ratings yet
- Varicella, Meningitis and DHFDocument7 pagesVaricella, Meningitis and DHFdebaynNo ratings yet
- Herpes Zoster Vaccine Fact SheetDocument8 pagesHerpes Zoster Vaccine Fact SheetsDamnNo ratings yet
- Patho Unit 5Document37 pagesPatho Unit 5Shafiya ShaikNo ratings yet
- Varicella ZosterDocument10 pagesVaricella ZosterVu Nhat KhangNo ratings yet
- Indonesian VaricellaDocument18 pagesIndonesian VaricellaWahyu FathurrachmanNo ratings yet
- Signs and SymptomsDocument6 pagesSigns and SymptomsKajim SharibiNo ratings yet
- Clinical Features of Varicella-Zoster Virus Infection - Chickenpox - UpToDateDocument16 pagesClinical Features of Varicella-Zoster Virus Infection - Chickenpox - UpToDatevotuyetdongtrinhNo ratings yet
- Varicella-Zoster Virus (Chickenpox) : Click The Icon To See An X-Ray of Pneumonia Following Exposure To ChickenpoxDocument4 pagesVaricella-Zoster Virus (Chickenpox) : Click The Icon To See An X-Ray of Pneumonia Following Exposure To ChickenpoxerfinaNo ratings yet
- Varicella: Immunization, Vaccines and BiologicalsDocument1 pageVaricella: Immunization, Vaccines and BiologicalsRozakNo ratings yet
- Varicella-Zoster Virus: (Chickenpox / Shingles)Document15 pagesVaricella-Zoster Virus: (Chickenpox / Shingles)walkrogNo ratings yet
- Chicken PoxDocument15 pagesChicken PoxQareeb KhanNo ratings yet
- Infection Case 45 - HIV & AIDSDocument2 pagesInfection Case 45 - HIV & AIDSkabal321No ratings yet
- ChickenpoxDocument3 pagesChickenpoxEdward McSweegan, PhDNo ratings yet
- Hypothesis: Andal, Darwin F. Sec. 1 1-8 Formative Assessment On Ecologic ModelDocument2 pagesHypothesis: Andal, Darwin F. Sec. 1 1-8 Formative Assessment On Ecologic ModelDarwin AndalNo ratings yet
- Herpes Zoster in Older Adults: Risk Factors, Diagnosis and ManagementDocument15 pagesHerpes Zoster in Older Adults: Risk Factors, Diagnosis and ManagementNadia Desanti RachmatikaNo ratings yet
- Assignment 3Document3 pagesAssignment 3EurydiceNo ratings yet
- The Coronavirus Pandemic: Essential Guide to Understand & Protect Yourself from COVID-19From EverandThe Coronavirus Pandemic: Essential Guide to Understand & Protect Yourself from COVID-19No ratings yet
- Somatic Complaints in Depression Psikosomatik Untad 2012Document19 pagesSomatic Complaints in Depression Psikosomatik Untad 2012Muhammad mukramNo ratings yet
- PIIS0140673620310424Document10 pagesPIIS0140673620310424JohnStrowskyNo ratings yet
- Bacaan Setelah Shalat Fardhu PDFDocument4 pagesBacaan Setelah Shalat Fardhu PDFMuhammad mukramNo ratings yet
- Bacaan Setelah Shalat Fardhu PDFDocument4 pagesBacaan Setelah Shalat Fardhu PDFMuhammad mukramNo ratings yet
- Miliaria Pustulosa (Infetrop)Document11 pagesMiliaria Pustulosa (Infetrop)Muhammad mukramNo ratings yet
- Early Detection of Psychosomatic - UNTAD - 2012Document12 pagesEarly Detection of Psychosomatic - UNTAD - 2012Muhammad mukramNo ratings yet
- Anxiety and Surgery UNTAD 2012Document35 pagesAnxiety and Surgery UNTAD 2012Muhammad mukramNo ratings yet
- Anxiety and Surgery UNTAD 2012Document22 pagesAnxiety and Surgery UNTAD 2012Arief Munandar AndiNo ratings yet
- Nejmsr2005760 PDFDocument7 pagesNejmsr2005760 PDFeuaiciNo ratings yet
- Coping Mechanism in Psychosomatic - UNTAD - 2012Document12 pagesCoping Mechanism in Psychosomatic - UNTAD - 2012Muhammad mukramNo ratings yet
- Anticonvulsants for Special PopulationsDocument56 pagesAnticonvulsants for Special PopulationsMuhammad mukramNo ratings yet
- Early Detection of Psychosomatic - UNTAD - 2012Document12 pagesEarly Detection of Psychosomatic - UNTAD - 2012Muhammad mukramNo ratings yet
- Gestational Diabetes and Ketoacidosis LectureDocument24 pagesGestational Diabetes and Ketoacidosis LectureMuhammad mukramNo ratings yet
- Anticonvulsants for Special PopulationsDocument56 pagesAnticonvulsants for Special PopulationsMuhammad mukramNo ratings yet
- Checklist Anatomy OsteologyDocument20 pagesChecklist Anatomy OsteologyGraffita BaktiNo ratings yet
- No No RM Nama JK UmurDocument45 pagesNo No RM Nama JK UmurMuhammad mukramNo ratings yet
- Drug For Allergy and Route PDFDocument92 pagesDrug For Allergy and Route PDFMuhammad mukramNo ratings yet
- Kuliah Sinkop UntadDocument35 pagesKuliah Sinkop UntadMuhammad mukramNo ratings yet
- Bab 370 Tatalaksana Infark Miokard Akut Tanpa Elevasi ST PDFDocument6 pagesBab 370 Tatalaksana Infark Miokard Akut Tanpa Elevasi ST PDFMuhammad mukramNo ratings yet
- Bab 334 Radiologi Jantung PDFDocument4 pagesBab 334 Radiologi Jantung PDFMuhammad mukramNo ratings yet
- Chickenpox (Varicella) : What Is Chickenpox? What Are The Symptoms of Chickenpox?Document3 pagesChickenpox (Varicella) : What Is Chickenpox? What Are The Symptoms of Chickenpox?Muhammad mukramNo ratings yet
- Anticonvulsants for Special PopulationsDocument56 pagesAnticonvulsants for Special PopulationsMuhammad mukramNo ratings yet
- Bab 335 EKG Pada Uji Latih Jantung PDFDocument3 pagesBab 335 EKG Pada Uji Latih Jantung PDFMuhammad mukramNo ratings yet
- AbortusDocument8 pagesAbortusMuhammad mukramNo ratings yet
- Urticaria 2014Document8 pagesUrticaria 2014Beny RaNo ratings yet
- Somatic Complaints in Depression Psikosomatik Untad 2012Document19 pagesSomatic Complaints in Depression Psikosomatik Untad 2012Muhammad mukramNo ratings yet
- Bab 384 Penyakit Jantung Dan Operasi Non Jantung PDFDocument8 pagesBab 384 Penyakit Jantung Dan Operasi Non Jantung PDFMuhammad mukramNo ratings yet
- Comparative Efficacy and Safety of Ebastine 20 MG, Ebastine 10 MG and Levocetirizine 5 MG in Acute UrticariaDocument4 pagesComparative Efficacy and Safety of Ebastine 20 MG, Ebastine 10 MG and Levocetirizine 5 MG in Acute UrticariaMuhammad mukramNo ratings yet
- Diagram KimiaDocument6 pagesDiagram KimiaMuhammad mukramNo ratings yet
- Viral Exanthems and EnanthemsDocument2 pagesViral Exanthems and Enanthemsclark146No ratings yet
- Cuestionario de Evaluación. Unit 1: Revisión Del IntentoDocument1 pageCuestionario de Evaluación. Unit 1: Revisión Del IntentoPetraNo ratings yet
- Mumps Guide: Causes, Symptoms, Treatment & PreventionDocument14 pagesMumps Guide: Causes, Symptoms, Treatment & PreventionChristian JonathanNo ratings yet
- Arboviruses: Characteristics, Transmission and DiseasesDocument2 pagesArboviruses: Characteristics, Transmission and DiseasesDapoy PeraltaNo ratings yet
- Drug MOAs Uses Forms AEs Resistance CharacteristicsDocument2 pagesDrug MOAs Uses Forms AEs Resistance CharacteristicsKate Sarah GabasaNo ratings yet
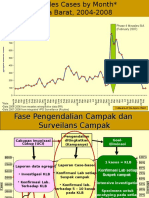
- Campak Dan RubelaDocument9 pagesCampak Dan RubelaAstin Nur FitriaNo ratings yet
- Diseases by time, place and personDocument10 pagesDiseases by time, place and personReah Jayzel AlkuinoNo ratings yet
- Chicken Pox: By: Ari & JennDocument12 pagesChicken Pox: By: Ari & JennEzekiel ArtetaNo ratings yet
- TB Test ResultsDocument5 pagesTB Test ResultsSanNo ratings yet
- SBI Reporting Forms New 2019 1Document7 pagesSBI Reporting Forms New 2019 1Salagmaya ES100% (1)
- Machupo VirusDocument15 pagesMachupo VirusiggyNo ratings yet
- Treatment of Herpes Zoster With Botanical.13Document4 pagesTreatment of Herpes Zoster With Botanical.13sesiaNo ratings yet
- Data Quality ReportDocument1 pageData Quality Reportamrudin yakobNo ratings yet
- Science DengvaxiaDocument2 pagesScience DengvaxiaJan Den Saul DalanNo ratings yet
- MMR NotesDocument2 pagesMMR NotesrotiNo ratings yet
- Corona Virus (Covid 19)Document13 pagesCorona Virus (Covid 19)Daffa JNo ratings yet
- Antiviral AgentsDocument14 pagesAntiviral Agentsalishba100% (1)
- Daftar PustakaDocument2 pagesDaftar PustakaAnonymous 65zjdAVNo ratings yet
- Company Profile Ayulia 2023Document13 pagesCompany Profile Ayulia 2023Willia HospitalNo ratings yet
- Tarlac State University Graduate StudiesDocument4 pagesTarlac State University Graduate StudiesL.J. SantosNo ratings yet
- Orange and Green Sustainability and Environment Minimalist InfographicDocument1 pageOrange and Green Sustainability and Environment Minimalist InfographicIvan Albert AguitasNo ratings yet
- Kualitas Hidup ODHADocument13 pagesKualitas Hidup ODHAAchmad VindoNo ratings yet
- Herpes Simplex PDFDocument28 pagesHerpes Simplex PDFAnggi Tridinanti PutriNo ratings yet
- 1425 25 2628 1 10 20200518 DikonversiDocument7 pages1425 25 2628 1 10 20200518 DikonversiErna YulianaNo ratings yet
- SeqdumpDocument7 pagesSeqdumpAnayantzin AyalaNo ratings yet
- DengueDocument15 pagesDengueLilibeth Ramos AnieteNo ratings yet
- Govt. medical college Kannauj MCQ's on measlesDocument27 pagesGovt. medical college Kannauj MCQ's on measlesnikhil73% (11)
- MAY 28, 2020 - FINAL Dashboard CovidDocument59 pagesMAY 28, 2020 - FINAL Dashboard CovidIrish Mae JovitaNo ratings yet