Professional Documents
Culture Documents
Bedside Ultrasound in The Diagnosis of Nonalcoholic Fatty Liver Disease
Uploaded by
Maru RLOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bedside Ultrasound in The Diagnosis of Nonalcoholic Fatty Liver Disease
Uploaded by
Maru RLCopyright:
Available Formats
Submit a Manuscript: http://www.wjgnet.
com/esps/ World J Gastroenterol 2014 June 14; 20(22): 6821-6825
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1007-9327 (print) ISSN 2219-2840 (online)
DOI:10.3748/wjg.v20.i22.6821 © 2014 Baishideng Publishing Group Inc. All rights reserved.
REVIEW
Bedside ultrasound in the diagnosis of nonalcoholic fatty
liver disease
Nancy Khov, Amol Sharma, Thomas R Riley
Nancy Khov, Department of Internal Medicine, Pennsylvania by clinicians from bedside ultrasound. The accessibility,
State Milton S. Hershey Medical Center and School of Medicine, ease of use, and low-side effect profile of ultrasound
Hershey, PA 17033, United States make bedside ultrasound an appealing imaging modali-
Amol Sharma, Thomas R Riley, Division of Gastroenterology ty in the detection of hepatic steatosis. When used with
and Hepatology, Department of Internal Medicine, Pennsylvania
appropriate clinical risk factors and steatosis involves
State Milton S. Hershey Medical Center and School of Medicine,
Hershey, PA 17033, United States greater than 33% of the liver, ultrasound can reliably
Author contributions: Khov N and Sharma A performed the diagnose NAFLD. Despite the ability of ultrasound in
literature search and wrote the paper; Riley TR participated in detecting moderate hepatic steatosis, it cannot replace
drafting the outline and revised the paper. liver biopsy in staging the degree of fibrosis. The pur-
Correspondence to: Nancy Khov, MD, Department of Internal pose of this review is to examine the diagnostic accura-
Medicine, Pennsylvania State Milton S. Hershey Medical Cen- cy, utility, and limitations of ultrasound in the diagnosis
ter and School of Medicine, 500 University Drive, Hershey, PA of NAFLD and its potential use by clinicians in routine
17033, United States. nkhov@hmc.psu.edu practices.
Telephone: +1-717-5315160 Fax: +1-717-5312034
Received: November 18, 2013 Revised: January 25, 2014
© 2014 Baishideng Publishing Group Inc. All rights reserved.
Accepted: March 19, 2014
Published online: June 14, 2014
Key words: Non-alcoholic fatty liver disease; Non-alco-
holic steatohepatitis; Liver fibrosis; Liver biopsy; Liver
disease; Liver cirrhosis; Steatosis; Bedside ultrasound
Abstract Core tip: Ultrasound is a non-invasive, widely available,
Non-alcoholic fatty liver disease (NAFLD) is the most and accurate tool in the detection of Non-alcoholic fatty
common liver disease in the United States. While the liver disease (NAFLD). Ultrasound should be used as
American Association for the Study of Liver Diseases the first-line diagnostic test in patients with abnormal
guidelines define NAFLD as hepatic steatosis detected liver enzymes when other causes are excluded. Clinical
either on histology or imaging without a secondary risk factors, when used with ultrasound findings, have
cause of abnormal hepatic fat accumulation, no imag- high accuracy in identifying NAFLD patients. We pres-
ing modality is recommended as standard of care for ent an algorithm for chronic abnormal liver enzymes
screening or diagnosis. Bedside ultrasound has been that illustrates the use of ultrasound in reducing the
evaluated as a non-invasive method of diagnosing need for liver biopsy in the diagnosis of NAFLD. Clini-
NAFLD with the presence of characteristic sonographic cians should be aware of the known limitations of ultra-
findings. Prior studies suggest characteristic sonograph- sound, including the inability to grade or stage fibrosis
ic findings for NAFLD include bright hepatic echoes, in NAFLD patients.
increased hepatorenal echogenicity, vascular blurring
of portal or hepatic vein and subcutaneous tissue thick-
ness. These sonographic characteristics have not been Khov N, Sharma A, Riley TR. Bedside ultrasound in the diag-
shown to aid bedside clinicians easily identify potential nosis of nonalcoholic fatty liver disease. World J Gastroenterol
cases of NAFLD. While sonographic findings such as 2014; 20(22): 6821-6825 Available from: URL: http://www.wjg-
attenuation of image, diffuse echogenicity, uniform net.com/1007-9327/full/v20/i22/6821.htm DOI: http://dx.doi.
heterogeneous liver, thick subcutaneous depth, and en- org/10.3748/wjg.v20.i22.6821
larged liver filling of the entire field could be identified
WJG|www.wjgnet.com 6821 June 14, 2014|Volume 20|Issue 22|
Khov N et al . Bedside ultrasound in the diagnosis of NAFLD
INTRODUCTION
The potential role of ultrasound by the clinician is in-
creasing. The estimated prevalence of non-alcoholic fatty
liver disease (NAFLD) is approximately 34%. Strongly
associated with metabolic syndrome, the incidence of
NAFLD will continue to rise with the projected progres-
sion of the obesity epidemic[1,2]. NAFLD includes a wide
spectrum of disease activity, from simple steatosis to
non-alcoholic steatohepatitis (NASH)[3,4]. Simple steatosis
has a benign and potentially reversible course, however,
NASH can progress to advanced fibrosis, cirrhosis, and
hepatocellular carcinoma[3,4]. The diagnosis of NAFLD
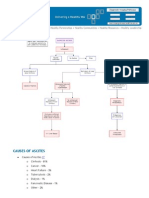
remains under recognized as most patients are asymp- Figure 1 Bedside ultrasound image displaying sonographic characteris-
tomatic until late stages of disease[5]. Liver biopsy is the tics on non-alcoholic fatty liver disease. Attenuation of image (green arrow),
gold standard in diagnosing NAFLD and the most accu- diffuse echogenicity, uniform heterogeneous liver, thick subcutaneous depth
(yellow arrow), and enlarged liver filling of the entire field as described by Riley
rate tool for grading fibrosis, however is invasive and car- et al[9].
ries the risk of complications[2,3]. Bedside ultrasound, as a
non-invasive and readily available tool, has an important
role in diagnosing NAFLD. In this paper we present a (1) attenuation of image quickly within 4-5 cm of depth,
review of current knowledge and literature on the utility making deeper structures difficult to decipher; (2) echo-
of beside ultrasound in the diagnosis of NAFLD by the genic diffusely but particularly important to note bright-
clinician. ness within the first 2-3 cm of depth; (3) liver uniformly
heterogeneous; (4) thick subcutaneous depth (> 2 cm);
and (5) liver fills entire field with no edges visible (viewed
CHARACTERISTIC SONOGRAPHIC as helpful but not necessary for diagnosis), as shown in
FEATURES OF NAFLD a prototypical bedside ultrasound image in Figure 1. Us-
ing these characteristic sonographic findings, bedside
High diagnostic accuracy can be achieved by the ultra- ultrasound yielded a sensitivity of 80% and specificity of
sound when sonographic features unique to NAFLD are 99%.
standardized and used to aid in diagnosis. Bright hepatic
echoes, increased hepatorenal echogenicity and vascular
blurring of portal or hepatic vein have been classified as EASE OF CLINICAL USE AND
unique sonographic features of NAFLD. In a prospec-
INTERPRETATION
tive study by Dasarathy et al[6], real time ultrasound was
performed followed by a liver biopsy to evaluate the ac- These typical sonographic features can be identified by
curacy of ultrasound in hepatic steatosis. When steatosis the clinician with the use of bedside ultrasound. Ultra-
was greater than 20% on biopsy, these sonographic fea- sound can result in an immediate diagnosis and devel-
tures were able to predict the presence of NAFLD with opment of a plan of care at the initial visit. Riley et al[9]
greater than 90% sensitivity. Lower levels of fat content demonstrated that clinical providers could be trained to
resulted in reduction of sensitivity[6]. A sonographic identify ultrasound images consistent with NAFLD after
scoring system used by Hamaguchi et al[7] was developed a brief 20-min session. Healthcare providers were subse-
based on similar pre-determined imaging findings. By quently able to reliably identify NAFLD using the proto-
using hepatorenal echo contrast, liver brightness, deep type image with substantial inter-observer agreement, κ
attenuation and vascular blurring, they were able to re- = 0.76[9].
port similar sensitivities in detecting histologically proven
NAFLD[7].
Subcutaneous tissue thickness, measured as the dis-
ULTRASOUND AS A DIAGNOSTIC TOOL
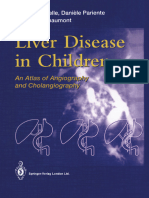
tance between the skin surface and the liver surface, has In patients with chronic hepatitis, an algorithm weighing
been shown to be another characteristic sonographic the relative importance between characteristic ultrasound
finding. When compared to other non-NAFLD liver dis- findings and clinical risk factors has been proposed for
eases, NAFLD patients had thicker subcutaneous tissue, the diagnosis of NALFD, as shown in Figure 2. To use
with a mean measurement of 25.6 ± 5.6 mm. In com- the algorithm, viral hepatitis, autoimmune liver disease,
parison, the non-NAFLD patients had a mean subcuta- alcoholic liver diseases, and genetic diseases must first
neous tissue thickness of 19.5 ± 5.2 mm. NAFLD was be excluded. Clinical risks include any of the follow-
unlikely when the subcutaneous tissue thickness was less ing: diabetes, body mass index (BMI) greater than 30,
than 20 mm[8]. Along with subcutaneous tissue thickness, hepatomegaly, and hyperlipidemia[10]. Ultrasound features
Riley et al[9] defined five characteristic sonographic find- include any 4 of the following 5 sonographic features:
ings for NAFLD that can be identified by the clinician: (1) attenuation of image quickly within 4-5 cm of depth;
WJG|www.wjgnet.com 6822 June 14, 2014|Volume 20|Issue 22|
Khov N et al . Bedside ultrasound in the diagnosis of NAFLD
Presence of chronically
abnormal liver enzymes
Are clinical risks
present?
Yes No
Are ultrasound features Proceed to liver
present? biopsy
Yes No
Is the AST/ALT > 1 or
Proceed to liver
has the BMI > 30 for
biopsy
more than 15 yr?
Yes No
Proceed to liver biopsy Initiate lifestyle changes
Figure 2 Diagnostic algorithm for suspected non-alcoholic fatty liver disease. The algorithm illustrates the use of ultrasound in reducing the need for liver biopsy
in the diagnosis of non-alcoholic fatty liver disease. BMI: Body mass index; AST/ALT: Aspartate aminotransferase/alanine aminotransferase.
(2) echogenic diffusely but particularly important to note known liver disease or significant alcohol use, they found
brightness within the first 2-3 cm of depth; (3) liver uni- non-alcoholic fatty liver disease to be more prevalent
formly heterogeneous; (4) thick subcutaneous depth (> 2 than previously reported. All individuals who had ultra-
cm); and (5) liver fills entire field with no visible edges[9]. sound findings suggestive of fatty liver had a liver biopsy
Characteristic features for NAFLD on ultrasound were to confirm their diagnosis. Using ultrasound as a screen-
found to be the strongest independent predictor on ing tool, they found NASH and NAFLD to be present at
multivariable analysis. Other clinical risk factors with sig- 12.2% and 46% of the population, respectively.
nificant correlation with the biopsy-proven diagnosis of Detection of NAFLD in potential living donor liver
NAFLD on multivariate analysis include the presence of transplantation is an important part of the routine pre-
diabetes, BMI > 30, hepatomegaly, female gender, age > transplant work-up[12]. During the evaluation of living
55, and triglyceride greater than 250[10]. The severity of donors, invasive procedures for healthy donors should be
hepatic steatosis on ultrasound in the presence of meta- minimized. It is well-recognized that the diagnostic accu-
bolic syndrome is a better non-invasive tool for monitor- racy of ultrasound diminishes with less than 20% hepatic
ing liver disease than liver enzymes[11]. Normal alanine steatosis. Identification of living donor candidates with
aminotransferase (ALT) level alone was not sufficient for a higher degree of hepatic steatosis by ultrasound may
exclusions of significant hepatic steatosis[12]. Aspartate allow them to forgo unnecessary liver biopsy needed for
aminotransferase (AST)/ALT ratio greater than 1, how- such assessment[15]. A study by Lee et al[12] evaluated 589
ever, has been associated to findings of advanced fibrosis living donor candidates with ultrasound, CT scan, and liv-
on liver biopsy[13]. The recognition of appropriate clinical er biopsy. They found a higher incidence than previously
factors in conjunction with characteristic ultrasound find- reported. In their study, 51.4% living donor candidates
ings can lead to an accurate diagnosis of NAFLD with- has greater than 5% steatosis and 10.4% had greater than
out the use of invasive testing, and also identify those 30% steatosis. Ultrasound had a sensitivity of 92.3%
individuals that should go onto have a liver biopsy. when steatosis was greater than 30% when screening this
population for a pre-transplant work-up.
In comparison to other non-invasive imaging tech-
ULTRASOUND AS A SCREENING TOOL niques, ultrasound has comparable sensitivities, greater
The prevalence of NAFLD and NASH may be higher ease of use, availability, and lower cost in screening for
than previously predicted creating the need for an ac- moderate to severe degrees of NAFLD. Although other
curate, non-invasive, and easily available modality for the modalities such as dual-gradient echo magnetic resonance
diagnosis of NAFLD in the asymptomatic patient[12,14]. imaging (DGE-MRI) is more accurate with sensitivity and
When Williams et al[14] used ultrasound to screen asymp- specificity greater than 90% when hepatic steatosis was
tomatic individuals in the general population without greater than 5%, the difference between DGE-MRI’s sen-
WJG|www.wjgnet.com 6823 June 14, 2014|Volume 20|Issue 22|
Khov N et al . Bedside ultrasound in the diagnosis of NAFLD
Table 1 Strength and weakness of ultrasound to diagnosis
ultrasound findings that could predict the presence of
non-alcoholic fatty liver disease steatosis. Although this score showed significant cor-
relation with metabolic derangements, the US-FLI had
Utility of ultrasound poor performance in predicting the presence of NASH.
Non-invasive Similarly, when Charatcharoenwitthaya and Lindor [23]
Ease of clinician use
evaluated various radiologic modalities in NASH, they
Ease of clinician interpretation
Widely available found that neither ultrasound, CT scan, nor MRI were
Low cost able to distinguish between NASH and other degrees of
Allows quick diagnosis NAFLD. Other studies have also shown that ultrasound
Limitations of ultrasound
cannot be used to grade degrees of fibrosis and cannot
Cannot grade degree of fibrosis
Limited use in pre-existing chronic liver disease
replace needle biopsy in distinguishing simple steatosis
Limited use in obese patients from steatohepatitis[24,25].
Low sensitivity when steatosis is less than 20%-30%
DISCUSSION
sitivity and ultrasound were statistically insignificant when Ultrasound represents a non-invasive, widely available,
steatosis was greater than 30%[1]. and accurate tool in the detection of NAFLD. Although
there is limited data available to support the use of ultra-
sound as a screening tool, ultrasound can be a powerful
LIMITATIONS OF ULTRASOUND
tool in the setting of known liver abnormality. Ultrasound
Ultrasound is limited in its utility in several settings, as should be used as the first-line diagnostic test in patients
shown in Table 1. As previously mentioned, multiple with abnormal liver enzymes. Standardized, characteristic
studies have shown that ultrasound underestimates the sonographic findings are able to reliably identify patients
prevalence of hepatic steatosis when less than 20% of with NAFLD. Clinical risk factors, when used with ultra-
steatosis is present. The sensitivity for detecting mild de- sound findings, have high utility in identifying NAFLD
grees of steatosis is low, ranging from 55%-90%[1,3,6,13,16,17]. patients and initiating an early plan of care. In a study by
Guajardo-Salinas et al[18] reported a low sensitivity in de- Riley et al[26], the risk of advanced fibrosis was increased
tecting all degrees of NASH in obese individuals (mean in patients with a BMI greater than 30 for over 15 years.
BMI 46-49) by ultrasound. In his retrospective chart In this clinical setting, with abnormal liver enzymes and
review of ultrasound reports, the right upper quadrant ultrasound findings suggestive of NAFLD, these patients
ultrasound was an unreliable tool for screening fatty liver, would benefit from a liver biopsy to identify the degree
with a sensitivity of 40%. In another study evaluating the of fibrosis.
diagnosis of NAFLD by ultrasound in obese patients un- Bedside ultrasound can be incorporated into the
dergoing bariatric surgery, de Moura Almeida et al[19] also
training of clinicians and used in hepatology practices at
found a low sensitivity of 64.9%. In this study, patients
outpatient visits. There is also potential use of ultrasound
had an average BMI of 43.8. Low sensitivities in both
when screening liver donor candidates. Ultrasound can
these studies may be a result of the lack of clearly de-
be used to exclude candidates with existing hepatic ste-
fined characteristic sonographic findings for the diagnosis
atosis without putting them through liver biopsy. An early
of NAFLD. Nonetheless, severe obesity may also limit
the ability to reliably detect liver echogenicity due to thick ultrasound and diagnosis will allow a potential liver donor
layers of subcutaneous fat[19,20]. candidate with hepatic steatosis to initiate early interven-
When used in the setting of other chronic liver dis- tion and re-evaluation at a later date.
eases, such as chronic hepatitis C, ultrasound had unac- In conclusion, the bedside ultrasound is a powerful
ceptably low sensitivity and specificity in identifying and useful diagnostic tool in the detection of NAFLD.
hepatic steatosis[2,21]. Perez et al[21] revealed in their chronic It is an accurate and reliable method that can reduce the
hepatitis C patients that ultrasound had only a sensitiv- need for liver biopsy in the appropriate clinical setting.
ity of 32% for detecting fat on biopsy in these patients. Clinicians should be aware of the known limitations
These low sensitivities suggest that ultrasound should when interpreting ultrasound, most importantly the in-
not be the only modality used in detecting co-existing ability to grade or stage degree of fibrosis in NAFLD
NAFLD in patients with chronic hepatitis C. patients. While bedside ultrasound cannot replace liver
Perhaps the most important limitation of using ul- biopsy in monitoring the progression from simple steato-
trasound alone is its inability to correlate with the degree sis to NASH, its accessibility, ease of use, and low-side
of fibrosis[20]. Ultrasound scoring systems fall short of effect profile make it an appealing diagnostic tool when
distinguishing between progressive NASH and benign used in the appropriate clinical setting. As the incidence
steatosis. Studies have shown poor correlation between of NAFLD continues to rise, we expect an increase in
sonographic findings and the histological stage of fibrosis the use of bedside ultrasound by clinicians as it becomes
on biopsy[2,20]. Ballestri et al[22] developed the ultrasound integrated into the routine practices of gastroenterolo-
fatty liver indicator (US-FLI), a scoring system based on gists and hepatologists.
WJG|www.wjgnet.com 6824 June 14, 2014|Volume 20|Issue 22|
Khov N et al . Bedside ultrasound in the diagnosis of NAFLD
treras M, Landt CL, Harrison SA. Prevalence of nonalcohol-
REFERENCES ic fatty liver disease and nonalcoholic steatohepatitis among
1 Lee SS, Park SH, Kim HJ, Kim SY, Kim MY, Kim DY, Suh a largely middle-aged population utilizing ultrasound and
DJ, Kim KM, Bae MH, Lee JY, Lee SG, Yu ES. Non-invasive liver biopsy: a prospective study. Gastroenterology 2011; 140:
assessment of hepatic steatosis: prospective comparison of 124-131 [PMID: 20858492 DOI: 10.1053/j.gastro.2010.09.038]
the accuracy of imaging examinations. J Hepatol 2010; 52: 15 Yamashiki N, Sugawara Y, Tamura S, Kaneko J, Matsui
579-585 [PMID: 20185194 DOI: 10.1016/j.jhep.2010.01.008] Y, Togashi J, Ohki T, Yoshida H, Omata M, Makuuchi M,
2 Chen CH, Lin ST, Yang CC, Yeh YH, Kuo CL, Nien CK. The Kokudo N. Noninvasive estimation of hepatic steatosis in
accuracy of sonography in predicting steatosis and fibrosis living liver donors: usefulness of visceral fat area measure-
in chronic hepatitis C. Dig Dis Sci 2008; 53: 1699-1706 [PMID: ment. Transplantation 2009; 88: 575-581 [PMID: 19696642
17939048 DOI: 10.1007/s10620-007-0048-2] DOI: 10.1097/TP.0b013e3181b11c19]
3 Baršić N, Lerotić I, Smirčić-Duvnjak L, Tomašić V, Duvnjak 16 Festi D, Schiumerini R, Marzi L, Di Biase AR, Mandolesi D,
M. Overview and developments in noninvasive diagnosis Montrone L, Scaioli E, Bonato G, Marchesini-Reggiani G,
of nonalcoholic fatty liver disease. World J Gastroenterol Colecchia A. Review article: the diagnosis of non-alcoholic
2012; 18: 3945-3954 [PMID: 22912545 DOI: 10.3748/wjg.v18. fatty liver disease -- availability and accuracy of non-
i30.3945] invasive methods. Aliment Pharmacol Ther 2013; 37: 392-400
4 Ahmed MH, Barakat S, Almobarak AO. Nonalcoholic fatty [PMID: 23278163 DOI: 10.1111/apt.12186]
liver disease and cardiovascular disease: has the time come 17 Mottin CC, Moretto M, Padoin AV, Swarowsky AM, Toneto
for cardiologists to be hepatologists? J Obes 2012; 2012: MG, Glock L, Repetto G. The role of ultrasound in the diag-
483135 [PMID: 23320150] nosis of hepatic steatosis in morbidly obese patients. Obes
5 Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Surg 2004; 14: 635-637 [PMID: 15186630 DOI: 10.1381/09608
Guallar E, Clark JM. Diagnostic accuracy and reliability 9204323093408]
of ultrasonography for the detection of fatty liver: a meta- 18 Guajardo-Salinas GE, Hilmy A. Prevalence of nonalcoholic
analysis. Hepatology 2011; 54: 1082-1090 [PMID: 21618575 fatty liver disease (NAFLD) and utility of FIBROspect II to
DOI: 10.1002/hep.24452] detect liver fibrosis in morbidly obese Hispano-American
6 Dasarathy S, Dasarathy J, Khiyami A, Joseph R, Lopez patients undergoing gastric bypass. Obes Surg 2010; 20:
R, McCullough AJ. Validity of real time ultrasound in 1647-1653 [PMID: 19957049 DOI: 10.1007/s11695-009-0027-0]
the diagnosis of hepatic steatosis: a prospective study. J 19 de Moura Almeida A, Cotrim HP, Barbosa DB, de Athayde
Hepatol 2009; 51: 1061-1067 [PMID: 19846234 DOI: 10.1016/ LG, Santos AS, Bitencourt AG, de Freitas LA, Rios A, Alves
j.jhep.2009.09.001] E. Fatty liver disease in severe obese patients: diagnostic
7 Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Na- value of abdominal ultrasound. World J Gastroenterol 2008;
kajima T, Kato T, Takeda N, Okuda J, Ida K, Kawahito Y, 14: 1415-1418 [PMID: 18322958 DOI: 10.3748/wjg.14.1415]
Yoshikawa T, Okanoue T. The severity of ultrasonographic 20 Mishra P, Younossi ZM. Abdominal ultrasound for diagno-
findings in nonalcoholic fatty liver disease reflects the meta- sis of nonalcoholic fatty liver disease (NAFLD). Am J Gastro-
bolic syndrome and visceral fat accumulation. Am J Gastro- enterol 2007; 102: 2716-2717 [PMID: 18042105 DOI: 10.1111/
enterol 2007; 102: 2708-2715 [PMID: 17894848 DOI: 10.1111/ j.1572-0241.2007.01520.x]
j.1572-0241.2007.01526.x] 21 Perez NE, Siddiqui FA, Mutchnick MG, Dhar R, Tobi M,
8 Riley TR, Bruno MA. Sonographic measurement of the Ullah N, Saksouk FA, Wheeler DE, Ehrinpreis MN. Ultra-
thickness of subcutaneous tissues in nonalcoholic fatty liver sound diagnosis of fatty liver in patients with chronic liver
disease versus other chronic liver diseases. J Clin Ultrasound disease: a retrospective observational study. J Clin Gastro-
2005; 33: 439-441 [PMID: 16281268 DOI: 10.1002/jcu.20164] enterol 2007; 41: 624-629 [PMID: 17577120 DOI: 10.1097/01.
9 Riley TR, Mendoza A, Bruno MA. Bedside ultrasound can mcg.0000225680.45088.01]
predict nonalcoholic fatty liver disease in the hands of clini- 22 Ballestri S, Lonardo A, Romagnoli D, Carulli L, Losi L, Day
cians using a prototype image. Dig Dis Sci 2006; 51: 982-985 CP, Loria P. Ultrasonographic fatty liver indicator, a novel
[PMID: 16783524 DOI: 10.1007/s10620-006-9343-6] score which rules out NASH and is correlated with meta-
10 Riley TR, Kahn A. Risk factors and ultrasound can predict bolic parameters in NAFLD. Liver Int 2012; 32: 1242-1252
chronic hepatitis caused by nonalcoholic fatty liver disease. [PMID: 22520641 DOI: 10.1111/j.1478-3231.2012.02804.x]
Dig Dis Sci 2006; 51: 41-44 [PMID: 16416209 DOI: 10.1007/ 23 Charatcharoenwitthaya P, Lindor KD. Role of radiologic
s10620-006-3082-6] modalities in the management of non-alcoholic steatohepa-
11 Kim HC, Choi SH, Shin HW, Cheong JY, Lee KW, Lee HC, titis. Clin Liver Dis 2007; 11: 37-54, viii [PMID: 17544971 DOI:
Huh KB, Kim DJ. Severity of ultrasonographic liver steatosis 10.1016/j.cld.2007.02.014]
and metabolic syndrome in Korean men and women. World 24 Lupsor M, Badea R. Imaging diagnosis and quantification
J Gastroenterol 2005; 11: 5314-5321 [PMID: 16149138] of hepatic steatosis: is it an accepted alternative to needle bi-
12 Lee JY, Kim KM, Lee SG, Yu E, Lim YS, Lee HC, Chung YH, opsy? Rom J Gastroenterol 2005; 14: 419-425 [PMID: 16400362]
Lee YS, Suh DJ. Prevalence and risk factors of non-alcoholic 25 Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP,
fatty liver disease in potential living liver donors in Korea: a Hurley M, Mullen KD, Cooper JN, Sheridan MJ. The utility
review of 589 consecutive liver biopsies in a single center. J of radiological imaging in nonalcoholic fatty liver disease.
Hepatol 2007; 47: 239-244 [PMID: 17400323] Gastroenterology 2002; 123: 745-750 [PMID: 12198701 DOI:
13 Grandison GA, Angulo P. Can NASH be diagnosed, graded, 10.1053/gast.2002.35354]
and staged noninvasively? Clin Liver Dis 2012; 16: 567-585 26 Riley TR, Taheri M, Schreibman IR. Does weight history
[PMID: 22824481] affect fibrosis in the setting of chronic liver disease? J Gastro-
14 Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Con- intestin Liver Dis 2009; 18: 299-302 [PMID: 19795023]
P- Reviewers: Chen JL, Chen GY, Wang JG, Zhu F
S- Editor: Qi Y L- Editor: A E- Editor: Ma S
WJG|www.wjgnet.com 6825 June 14, 2014|Volume 20|Issue 22|
Published by Baishideng Publishing Group Inc
8226 Regency Drive, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx
http://www.wjgnet.com
I S S N 1 0 0 7 - 9 3 2 7
2 2
9 7 7 1 0 0 7 9 3 2 0 45
© 2014 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- Steketee Master-ClinicianDocument101 pagesSteketee Master-Clinicianrgr4321100% (2)
- Course - Fundamentals of Traditional Chinese Medicine - Center For True HealingDocument49 pagesCourse - Fundamentals of Traditional Chinese Medicine - Center For True HealingAry Nogueira100% (1)
- Health and Safety Environmental ManagementakistanDocument40 pagesHealth and Safety Environmental ManagementakistanAminullah01No ratings yet
- GREEN Manual - 2021Document157 pagesGREEN Manual - 2021Bon Ber Amad Orofeo100% (2)
- Psychiatry EmergencyDocument121 pagesPsychiatry EmergencyDr. Jayesh Patidar67% (6)
- Reproductive Health: Presented byDocument22 pagesReproductive Health: Presented byJulie RodelasNo ratings yet
- Ultrasound Imaging of The AbdomenDocument224 pagesUltrasound Imaging of The AbdomenAsztalos Attila100% (9)
- NCCN Antiemesis Guideline 2018 v3 PDFDocument68 pagesNCCN Antiemesis Guideline 2018 v3 PDFholdonpainendsNo ratings yet
- WJG 20 7392 PDFDocument12 pagesWJG 20 7392 PDFTarraNo ratings yet
- Gurevic@zg Htnet HRDocument22 pagesGurevic@zg Htnet HRNam LeNo ratings yet
- AscitesDocument5 pagesAscitescaomanhthau37No ratings yet
- Us Elastography in Hepatic Fibrosis Radiology in TrainingDocument8 pagesUs Elastography in Hepatic Fibrosis Radiology in TrainingValentina IorgaNo ratings yet
- Aresia de Vias Biliares UltrasonidoDocument14 pagesAresia de Vias Biliares UltrasonidoArturo GarciaNo ratings yet
- Background: Open Access Original Article DOI: 10.7759/cureus.10987Document5 pagesBackground: Open Access Original Article DOI: 10.7759/cureus.10987hengkyNo ratings yet
- The Comparative Advantage of Plain Radiography in Diagnosis of Obstruction of The Small Intestine in DogsDocument10 pagesThe Comparative Advantage of Plain Radiography in Diagnosis of Obstruction of The Small Intestine in DogsLara LampertNo ratings yet
- The Value of Ultrasound in Previously Undiagnosed Renal FailureDocument3 pagesThe Value of Ultrasound in Previously Undiagnosed Renal FailureAnonymous V5l8nmcSxbNo ratings yet
- IntJMedPublicHealth32111-7924347 220043Document0 pagesIntJMedPublicHealth32111-7924347 220043budi_26690No ratings yet
- Liver Disease in Children - An Atlas of Angiography and CholangiographyDocument151 pagesLiver Disease in Children - An Atlas of Angiography and Cholangiographyedo opanovicNo ratings yet
- 2-Value of Renal Cortical Thickness As A Predictor of RenalDocument5 pages2-Value of Renal Cortical Thickness As A Predictor of Renaljeb faqNo ratings yet
- The Role of Ultrasonography in The Evaluation of Diffuse Liver DiseaseDocument13 pagesThe Role of Ultrasonography in The Evaluation of Diffuse Liver Disease{Phantom}No ratings yet
- 2 D SWE DD Fibrosis Non Fibrosis - 240416 - 190701Document6 pages2 D SWE DD Fibrosis Non Fibrosis - 240416 - 190701bella friscaamaliaNo ratings yet
- Precision Diagnostica y Confiabilidad Del Us en Higado GrasoDocument9 pagesPrecision Diagnostica y Confiabilidad Del Us en Higado GrasoDavidNo ratings yet
- Relationship of Serum Uric Acid Level With Non-Alcoholic Fatty Liver Disease and Its in Ammation Progression in Non-Obese AdultsDocument9 pagesRelationship of Serum Uric Acid Level With Non-Alcoholic Fatty Liver Disease and Its in Ammation Progression in Non-Obese AdultssyifaNo ratings yet
- 04mos PDFDocument10 pages04mos PDFMarcelitaTaliaDuwiriNo ratings yet
- Advances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewDocument7 pagesAdvances in Understanding The Progression of Non-Alcoholic Fatty Liver Disease To Non-Alcoholic Steatohepatitis: A Comprehensive ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Wiles2017 Article ManagementAndFollow-upOfGallblDocument11 pagesWiles2017 Article ManagementAndFollow-upOfGallblTrần Quốc KhánhNo ratings yet
- Performance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseDocument8 pagesPerformance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseChausarPutraBenagilNo ratings yet
- A Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionDocument6 pagesA Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionSantosh BabuNo ratings yet
- Systematic Review: The Epidemiology and Natural History of Non-Alcoholic Fatty Liver Disease and Non-Alcoholic Steatohepatitis in AdultsDocument12 pagesSystematic Review: The Epidemiology and Natural History of Non-Alcoholic Fatty Liver Disease and Non-Alcoholic Steatohepatitis in AdultsLays RosalNo ratings yet
- Document From KagiDocument3 pagesDocument From KagiFarras Ghanikagi SutediNo ratings yet
- Pi Is 0002934399803544Document3 pagesPi Is 0002934399803544Muhammad Kholid FirdausNo ratings yet
- Hepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andDocument15 pagesHepatology Communications - 2022 - Vieira Barbosa - Fibrosis 4 Index As An Independent Predictor of Mortality andjim.palmarbNo ratings yet
- Original ArticleDocument5 pagesOriginal ArticlehengkyNo ratings yet
- EBCR USG SirosisDocument16 pagesEBCR USG Sirosisindra_strongNo ratings yet
- The Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisDocument5 pagesThe Role of Abdominal X-Rays in The Investigation of Suspected Acute AppendicitisFitri RachmadaniNo ratings yet
- ACHALASIADocument9 pagesACHALASIASacad SuleimanNo ratings yet
- Acute Renal Colic: An Imaging Update: Dr. Kin-Shing TaiDocument2 pagesAcute Renal Colic: An Imaging Update: Dr. Kin-Shing TaiJenry Reyes TrispaNo ratings yet
- 4.gheonea Ionut Final PRDocument8 pages4.gheonea Ionut Final PRNicoleta Popa-FoteaNo ratings yet
- Journal Reading RadiologyDocument33 pagesJournal Reading RadiologyBrian HallNo ratings yet
- Medical Ultrasonography July 2009 Vol 11 No 2 Page 15 18Document4 pagesMedical Ultrasonography July 2009 Vol 11 No 2 Page 15 18roxitanaNo ratings yet
- PIIS0749073923000184Document14 pagesPIIS0749073923000184Allende Tellechea CarrilloNo ratings yet
- Preferred Examination: Right Ureteral Calculus With Periureteral StrandingDocument26 pagesPreferred Examination: Right Ureteral Calculus With Periureteral StrandingErrina YustiraNo ratings yet
- Diagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosDocument6 pagesDiagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosWingga Chrisna AjiNo ratings yet
- Radiologic Evaluation of Nonalcoholic Fatty Liver DiseaseDocument12 pagesRadiologic Evaluation of Nonalcoholic Fatty Liver DiseasePuputNo ratings yet
- Bmri2019 3951574Document10 pagesBmri2019 3951574Anonymous 1EQutBNo ratings yet
- Ferraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundDocument12 pagesFerraioli Et Al 2022 Us Attenuation For Liver Fat Quantification An Aium Rsna Qiba Pulse Echo Quantitative UltrasoundThesisaurus IDNo ratings yet
- Accuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureDocument4 pagesAccuracy of Ultrasonography in The Diagnosis of Acute Calculous Cholecystitis: Review of The LiteratureAnasriNstNo ratings yet
- 22 Iajps22102020Document6 pages22 Iajps22102020iajpsNo ratings yet
- Histopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisDocument18 pagesHistopathology of Nonalcoholic Fatty Liver Disease - Nonalcoholic SteatohepatitisLaia BertranNo ratings yet
- Non Alcoholic Liver Disease PhilippinesDocument5 pagesNon Alcoholic Liver Disease PhilippinesMara Benzon-BarrientosNo ratings yet
- Clinical and Endoscopic Study of Dysphagia: A Prospective Crossectional Study at A Tertiary Care Centre at North - Eastern IndiaDocument3 pagesClinical and Endoscopic Study of Dysphagia: A Prospective Crossectional Study at A Tertiary Care Centre at North - Eastern IndiaInternational Organization of Scientific Research (IOSR)No ratings yet
- Evaluation of Liver Fibrosis and Cirrhosis On TheDocument7 pagesEvaluation of Liver Fibrosis and Cirrhosis On TheeugeniaNo ratings yet
- US Elastography in Liver Frulio DX Interv Im 2013Document20 pagesUS Elastography in Liver Frulio DX Interv Im 2013gatoflacoNo ratings yet
- Pancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyDocument4 pagesPancreatic Head Mass: What Can Be Done ? Diagnosis: UltrasonographyMolla WariNo ratings yet
- Elastografia Hepatica Transitoria Higado Graso No AlcoholicoDocument5 pagesElastografia Hepatica Transitoria Higado Graso No Alcoholicoalan obeth hipolito seguraNo ratings yet
- Obstructive Jaundice Aetiological SpectrDocument8 pagesObstructive Jaundice Aetiological Spectrvvwaghmare30No ratings yet
- Prevalence of Anaemia in Decompensated Chronic Liver DiseaseDocument5 pagesPrevalence of Anaemia in Decompensated Chronic Liver DiseaseElang SudewaNo ratings yet
- SWE in HAIDocument15 pagesSWE in HAIValentina IorgaNo ratings yet
- Gambaran Hasil Ultrasonografi Urologi Pada Pasien Dengan Klinis NefrolitiasisDocument9 pagesGambaran Hasil Ultrasonografi Urologi Pada Pasien Dengan Klinis NefrolitiasisNabila JuliantyNo ratings yet
- SC 2015242Document7 pagesSC 2015242resi ciruNo ratings yet
- Evaluation and Management of Obesity-Related Nonalcoholic Fatty Liver DiseaseDocument10 pagesEvaluation and Management of Obesity-Related Nonalcoholic Fatty Liver DiseaseVíctor V MayoralNo ratings yet
- 5 Advanced Ultrasound TechniquesDocument7 pages5 Advanced Ultrasound Techniquesjefaturaimagenologia Hospital NogalarNo ratings yet
- Contrast-Enhanced Ultrasound Imaging of Hepatic NeoplasmsFrom EverandContrast-Enhanced Ultrasound Imaging of Hepatic NeoplasmsWen-Ping WangNo ratings yet
- Evaluation and Management of Dysphagia: An Evidence-Based ApproachFrom EverandEvaluation and Management of Dysphagia: An Evidence-Based ApproachDhyanesh A. PatelNo ratings yet
- Endoscopy in Liver DiseaseFrom EverandEndoscopy in Liver DiseaseJohn N. PlevrisNo ratings yet
- Thyroid Ultrasound and Ultrasound-Guided FNAFrom EverandThyroid Ultrasound and Ultrasound-Guided FNAH. Jack Baskin, Sr.No ratings yet
- The SAGES Manual of Flexible EndoscopyFrom EverandThe SAGES Manual of Flexible EndoscopyPeter NauNo ratings yet
- Hesr 51 352Document26 pagesHesr 51 352Naja nigricollisNo ratings yet
- Medical Terminology Chapter 3 Verified AnswersDocument8 pagesMedical Terminology Chapter 3 Verified AnswersGregg ProducerNo ratings yet
- Apps For Paediatric Dosing - An Evaluation - Vonbach PriskaDocument1 pageApps For Paediatric Dosing - An Evaluation - Vonbach PriskaSara KreboldNo ratings yet
- BAQUIRAN - HUME 124 Activity 2.2. Hazards at HomeDocument8 pagesBAQUIRAN - HUME 124 Activity 2.2. Hazards at HomeMa.angeli BaquiranNo ratings yet
- Glucagon Stimulation Test For Adults v1 Nhs UkDocument2 pagesGlucagon Stimulation Test For Adults v1 Nhs UkNavojit ChowdhuryNo ratings yet
- Food Products Advertisement Regulation 2019Document12 pagesFood Products Advertisement Regulation 2019ILABESHI GABRIELNo ratings yet
- Pazoki Et Al. 2022 - Efficacy and Safety of Saffron As Adjunctive Therapy in Adults With ADHDDocument7 pagesPazoki Et Al. 2022 - Efficacy and Safety of Saffron As Adjunctive Therapy in Adults With ADHDLaura DecockNo ratings yet
- (New & Improved) TDEE Calculator (Insanely Accurate)Document11 pages(New & Improved) TDEE Calculator (Insanely Accurate)LaraNo ratings yet
- PharmDos LAB - M2.2Document7 pagesPharmDos LAB - M2.2Gianna LingadNo ratings yet
- Blinded Study Synopsis FormatDocument9 pagesBlinded Study Synopsis FormatSok YeeNo ratings yet
- Hazardous Materials Storage GuidelinesDocument4 pagesHazardous Materials Storage Guidelinesclinton sampsonNo ratings yet
- OSH Manual Medium Risk EntitiesDocument122 pagesOSH Manual Medium Risk EntitiesNitika SinhaNo ratings yet
- DOTSLong 5.4Document2 pagesDOTSLong 5.4JAY JR. APONNo ratings yet
- Registration at AWC-EnglishDocument2 pagesRegistration at AWC-EnglishSamtha MasineniNo ratings yet
- Buku Murid Bahasa Inggris - Work in Progress - Sports and Health Buku Panduan Guru Bahasa Inggris SMA Kelas X Unit 3 - Fase EDocument26 pagesBuku Murid Bahasa Inggris - Work in Progress - Sports and Health Buku Panduan Guru Bahasa Inggris SMA Kelas X Unit 3 - Fase ENurul WildaNo ratings yet
- NursingDocument9 pagesNursingIlie SmarandacheNo ratings yet
- 1 SMDocument10 pages1 SMsatuA keslingNo ratings yet
- Novilyn C. Pataray BSN - Ii Pharyngitis: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Pharyngitis: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- Review Article: Common Periodontal Diseases of Children and AdolescentsDocument8 pagesReview Article: Common Periodontal Diseases of Children and AdolescentsGea Akalili SabrinaNo ratings yet
- T I O F P P: M S P: Journal of Southwest Jiaotong UniversityDocument10 pagesT I O F P P: M S P: Journal of Southwest Jiaotong UniversityNeanderthalNo ratings yet
- Iowa DHS LetterDocument2 pagesIowa DHS LetterThe GazetteNo ratings yet
- MGT-404Document10 pagesMGT-404Amna KhalidNo ratings yet
- CIRCI Guidelines 2015Document6 pagesCIRCI Guidelines 2015Wissam SleimanNo ratings yet