Professional Documents
Culture Documents
Braganza2011 PDF
Uploaded by
Amirullah AbdiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Braganza2011 PDF
Uploaded by
Amirullah AbdiCopyright:
Available Formats
Seminar
Chronic pancreatitis
Joan M Braganza, Stephen H Lee, Rory F McCloy, Michael J McMahon
Lancet 2011; 377: 1184–97 Chronic pancreatitis is a progressive fibroinflammatory disease that exists in large-duct (often with intraductal
Published Online calculi) or small-duct form. In many patients this disease results from a complex mix of environmental (eg, alcohol,
March 11, 2011 cigarettes, and occupational chemicals) and genetic factors (eg, mutation in a trypsin-controlling gene or the cystic
DOI:10.1016/S0140-
fibrosis transmembrane conductance regulator); a few patients have hereditary or autoimmune disease. Pain in
6736(10)61852-1
the form of recurrent attacks of pancreatitis (representing paralysis of apical exocytosis in acinar cells) or constant
Department of
Gastroenterology
and disabling pain is usually the main symptom. Management of the pain is mainly empirical, involving potent
(J M Braganza DSc) and analgesics, duct drainage by endoscopic or surgical means, and partial or total pancreatectomy. However, steroids
Department of Radiology rapidly reduce symptoms in patients with autoimmune pancreatitis, and micronutrient therapy to correct
(S H Lee FRCR), Manchester
electrophilic stress is emerging as a promising treatment in the other patients. Steatorrhoea, diabetes, local
Royal Infirmary, Manchester,
UK; Department of Education, complications, and psychosocial issues associated with the disease are additional therapeutic challenges.
Lancashire Teaching Hospitals,
Preston, UK (R F McCloy FRCS); Introduction Definition
and University of Leeds and
Chronic pancreatitis is a progressive inflammatory Traditionally, chronic pancreatitis has been classed as
Nuffield Hospital, Leeds, UK
(Prof M J McMahon FRCS) disorder in which pancreatic secretory parenchyma is fundamentally different from acute pancreatitis—the
Correspondence to:
destroyed and replaced by fibrous tissue, eventually latter is usually characterised by restoration of normal
Dr Joan M Braganza, leading to malnutrition and diabetes. Two forms are pancreatic histology after full clinical recovery.1 However,
c/o Mrs Jenny Parr, recognised—a large-duct calcifying type1 and a small-duct acute, recurrent acute, and chronic pancreatitis are now
Core Technology Facility,
variant.2–4 The disease is uncommon in Europe and the regarded as a disease continuum.9,10 There are several
3rd Floor, Grafton Street,
Manchester M13 9NT, UK USA; its prevalence in France is 26 per 100 000 people.5 reasons for this change: recurrent acute pancreatitis can
jenny.parr@manchester.ac.uk This prevalence is not dissimilar to the middle of three develop into chronic pancreatitis;10–12 there is an overlap
estimates from Japan,6,7 but considerably lower than the in causative factors, both genetic and environmental;10,13
figure of 114–200 per 100 000 in south India.7 experimental protocols can be modified to induce each
The main symptom of chronic pancreatitis is usually condition;14 and the pancreatitis attack is stereotyped—
pain, which occurs as attacks that mimic acute pancrea- patients have severe abdominal pain and increased blood
titis or as constant and disabling pain. Despite decades of amylase, lipase, and trypsinogen.
research, treatment of chronic pancreatitis remains
mostly empirical, and thus patients are repeatedly Pathophysiology and pathology
admitted to hospital and have interventional procedures, Experimental studies since the 1950s have shown that an
which strains medical resources.8 This absence of attack of pancreatitis begins as pancreastasis,13 prevention
progress in treatment is a sign of uncertainty about how of apical exocytosis in the pancreatic acinar cell (figure 1).15
the identified causative factors lead to the disease. The acinar cell quickly releases newly synthesised enzyme
Therefore, in this Seminar we focus on the patho- via the basolateral membrane into lymphatics, by way of
physiology and pathology of chronic pancreatitis before the interstitium, and directly into the bloodstream.16 Some
describing clinical management. zymogen granules also release their stored enzyme
basolaterally.15 These events result in inflammation.17
Findings from prospective clinical studies concur with
Search strategy and selection criteria this pancreastasis–pancreatitis sequence.13,17
We searched PubMed and the Cochrane library (to August, Experimental work has pinpointed a burst of reactive
2010) for reviews on chronic pancreatitis. We used Google oxygen species (ROS) as the trigger of so-called
scholar for specific searches, with “chronic pancreatitis” as the pancreastasis18 and as the potentiator of inflammation by
key phrase combined with “epidemiology”, “pathology”, activating signalling cascades that convert the damaged
“aetiology”, “gene mutations”, “pathogenesis”, acinar cell into a factory for chemokines and cytokines.19,20
“classification”, “diagnosis”, “pancreatic function tests”, ROS serve several physiological roles, including in signal
“pancreatic imaging tests”, “treatment of pain”, “pancreatic transduction,13,21 but an excess of ROS compared with
enzyme therapy”, “micronutrient therapy”, “antioxidant antioxidant capacity (electrophilic stress) is potentially very
therapy”, “endoscopic treatment”, or “surgical treatment”. We damaging. The exocytosis blockade seems to be caused by
selected the most up-to-date articles but did not disregard disruption of the methionine trans-sulphuration pathway
commonly referenced older publications. We also examined that produces essential methyl and thiol (principally
the reference lists of identified papers and selected those that glutathione) moieties.17,22 This problem also occurs in
we judged to be relevant. Review articles and book chapters clinical acute or acute-on-chronic pancreatitis.23–25
are cited to give readers more details and references than this In patients who develop large-duct chronic pancreatitis,
Seminar can accommodate. studies in the quiescent phase of the disease show that
the composition of pancreatic fluid changes in a manner
1184 www.thelancet.com Vol 377 April 2, 2011
Seminar
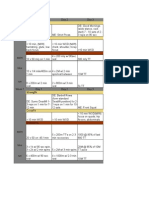
Normal Pancreastasis Pancreatitis
Constitutive
E pathways PAP/regIII
PSP/reg
ZG ZG ZG D
L ZG-L ZG-L
GC GC
RER RER ZG RER
Ph-elastase
Ph-PLA2
Nucleus Nucleus Nucleus
Constitutive MO
pathway
E
E E
MC PMN
Foci of gland digestion
Figure 1: Schematic representation of disturbances in the pancreatic acinar cell during experimental acute pancreatitis
See text for a full description. The constitutive pathway at the basolateral pole normally transports a small fraction of newly synthesised enzyme, as do two pathways at the
apical pole. E=amylase, lipase, trypsinogen, and other precursor proteases, and pro-phospholipase A2. RER=rough endoplasmic reticulum. GC=Golgi complex. ZG=zymogen
granules. L=lysosomes. ZG-L=miniscule fraction of zymogens activated by co-localisation with lysosomal enzymes. D=centripetal dissolution of granules.
PAP/regIII=pancreatitis associated protein. PSP/reg=pancreatic stone protein/islet regenerating protein. MC=mast cell. PMN=polymorphonuclear cell. MO=monocyte.
Ph-PLA2=phospholipase A2 from phagocytes and mast cell. Adapted from Braganza.13
that, for uncertain reasons, facilitates protein deposits— fibrosis.11 Nerves show breaching of the perineurium
the precursors to calcium carbonate stones.1 (1) There is adjacent to inflammatory foci, while the expression of
an early increase in secretion of enzyme and calcium, but nociceptive chemicals in nerve endings is increased.36
a decrease in the serine protease inhibitor Kazal type 1 Immunocytochemistry gives valuable insights into the
(SPINK 1), bicarbonate, and citrate.1 (2) Concentrations of development of chronic pancreatitis. Acinar cells,
free radical oxidation products are raised in the pancreatic which are hyperplastic at disease outset,2 show
fluid,26 which suggests ongoing electrophilic stress, and strong expression of cytochrome P450 (CYP) mono-
in an apparent attempt to compensate, concentrations of oxygenases,37–39 as do proliferated islets of Langerhans,37–39
the natural antioxidants27 lactoferrin and mucin are and hepatocytes (figure 2).37,38 After birth, CYP enzymes
increased.1,2,28 (3) Concentrations are altered of two are mainly located in the liver. CYP metabolises
secretory stress proteins29 (increased concentration of environmental lipophilic chemicals (xenobiotics). In the
pancreatitis associated protein [PAP]/regIII, which is first phase, the enzyme uses ROS to hydroxylate the
activated by electrophilic stress; and variable concentration substrate, which then usually undergoes second-phase
of pancreatic stone protein [PSP]/reg, formerly called conjugation reactions, often with glutathione and
lithostatin;1 figure 1) that tend to form fibrous lattices catalysed by glutathione transferases. So-called enzyme
upon partial digestion by trypsin. (4) There is an increase induction might be accompanied by expansion of the
of GP-2, which is a secreted component of zymogen endoplasmic reticulum so that, at least initially, the cell
granule membranes (analogous to the renal cast protein).30 secretes more of its normal products. However, this
(5) Concentrations of lysosomal enzymes are increased in defence reaction backfires if first-phase processing (eg, by
ductal fluid, and traces of trypsin appear.31 Moreover, the CYP2E1, CYP1A, and CYP3A1 isoforms) produces a
methionine metabolic pathway remains fractured.32–34 reactive xenobiotic metabolite. Cell injury depends on
On histology, the defining triad of stable disease whether or not there is enough by way of defences to
(irrespective of main causes or location)35 is acinar loss, ROS and reactive xenobiotic species: antioxidant enzymes
mononuclear cell infiltration, and fibrosis. The early (including the selenium-dependent glutathione peroxi-
lesions are distributed in patches; thus, normal findings dase), glutathione transferases, glutathione, and ascorbic
on needle biopsy are unreliable. An unusual form of so- acid (the bioactive form of vitamin C, which can substitute
called groove (paraduodenal) pancreatitis has been for glutathione).32,40 Immunochemistry shows that these
identified.11 Each inflammatory attack can cause foci of defence mechanisms are insufficient to meet the
fat necrosis that seem to lead to both pseudocysts and increased oxidant load in acinar cells,32,37 which therefore
www.thelancet.com Vol 377 April 2, 2011 1185
Seminar
show signs of electrophilic stress, such as excess lipo- progression resembles that from chronic active hepatitis
fuscin and cytoplasmic microvesiculation.41 to liver cirrhosis.2,12,47
Fibrosis is a sign that interstitial stellate cells are The table summarises the histological features of
activated in chronic pancreatitis; these cells play a ordinary chronic pancreatitis compared with features of
central part in disease progression by regulating the three variants in which the lesions are diffuse. The
synthesis and degradation of extracellular matrix pancreatic lesion in cystic fibrosis is a diffuse form of
proteins.42,43 Findings from histochemistry suggest a chronic pancreatitis wherein inflammatory stigmata
causal influence of two factors—an increase in lipid disappear by birth,48 except in patients with mild
peroxidation products caused by an excess of ROS in mutations in the cystic fibrosis transmembrane
adjacent acini,44 and the release of mast cell conductance regulator gene (CFTR), who might have
degranulation products,45 transforming growth factor β1 recurrent attacks.49 Uniform lesions also occur upstream
in particular.46 The two factors are linked in that ROS of an obstructed duct1,11,48 and in autoimmune
and their oxidation products are natural activators of pancreatitis.50,51 The latter can involve the whole or part
mast cells.17 Activation of stellate cells is increased by of the gland and has two subtypes. Characteristics of
cytokines from infiltrating leucocytes and the injured the more common type-1 autoimmune pancreatitis are
acinar cell.43 The end stage of chronic pancreatitis is a dense lymphoplasmacytic infiltrate with predominantly
identified by loss of all secretory tissue, disappearance IgG4+ cells, periductal swirling sclerosis, and obliterative
of inflammatory cells, and intense fibrosis. This venulitis. In the type-2, duct-destructive form, hordes
A B
D
H
H
D A
S
A
D
50 μm 50 μm
Figure 2: Immunolocalisation of cytochrome P4503A1 in surgical material from a 27-year-old woman with calcific chronic pancreatitis
The patient drank little alcohol, smoked 40 cigarettes a day, and worked as a forecourt attendant at a car and lorry-fuelling station. (A) The pancreatectomy fragment
shows that the enzyme (brown stain) is strongly expressed in acinar cells (A) but absent from epithelium of dilated ducts (D) or expanded stroma (S). (B) The needle
biopsy fragment of the liver showed that the enzyme is strongly expressed across the liver lobule (H) and weakly expressed in bile duct epithelium (D). Reproduced
with permission from Foster et al.37
Ordinary* Cystic fibrosis† Obstructive‡ Autoimmune§
Lesions
Distribution Patchy Diffuse Diffuse Diffuse
Extent of gland Variable Total Total Total or focal
Duct system
Main duct Irregularly dilated Minimally dilated Smoothly dilated Constricted
Protein plugs All ducts Intralobular and interlobular No No
Calcifying tendency Yes No No No
Epithelium destroyed (Groove form) No No Yes (type 2)
Neutrophils No No No Yes (type 2)
Inflammatory cells Mononuclear No No Plasmalymphacytic
Fibrosis Mainly perilobular Perilobular, intralobular Perilobular, intralobular Perilobular, intralobular, periductal
Pseudocyst Frequent No No No
*Excludes the small-duct variant (as in at least 30% of cases) wherein characteristic features are focal acinar cell damage and tubular complexes.3 Groove pancreatitis is similar
to the ordinary form, except for prominent destruction of ductal epithelium and cysts.1,11 †The earliest lesions occur in utero.48 ‡Diffuse lesions occur upstream from the
obstruction.1,11 §See text for subtypes.
Table: Main histological features of chronic pancreatitis subtypes (at diagnosis in stable disease)
1186 www.thelancet.com Vol 377 April 2, 2011
Seminar
of neutrophils infiltrate the wall of the duct, accompanied
by lymphocytes and plasma cells.51 Panel 1: Causative factors
Toxic
Causes Xenobiotics
Panel 1 lists causative factors of chronic pancreatitis. In • Alcohol
adults, excluding those with cystic fibrosis, 90–95% of • Cigarette smoke
patients are regarded as having alcoholic or idiopathic • Occupational volatile hydrocarbons
disease. Infective causes are rare.52 The connection between • Drugs: valproate, phenacitin, thiazide, oestrogen,
chronic pancreatitis and drugs (eg, valproate) is mostly and azathioprine
anecdotal. Studies from Italy,53 China, and Japan54 report
Endogenous
an association with gallstones in about 30% of patients.
• Hypercalcaemia, hyperparathyroidism
• Hyperlipidaemia, lipoprotein lipase deficiency
Alcoholic
• Chronic renal failure
Alcohol has long been regarded as the leading cause of
chronic pancreatitis in Europe, the USA, Brazil, Mexico, Infection or infestation
and South Africa, and is now regarded as the main cause • HIV, mumps virus, coxsackie virus
of the disease also in Australia and South Korea.7 • Echinococcus, Cryptosporidium
However, excess alcohol was the predominant factor in Genetic*
only 34% of cases of chronic pancreatitis in a recent • CFTR mutation
multicentre study from Italy53 and in 44% of cases in an • PRSS1 mutation
audit from the USA,55 with another study reporting that • SPINK1 mutation
African-Americans are at particular risk.56 Whether these
new data reflect differences in the definition of alcoholic Obstruction of main pancreatic duct
disease55 or a genuine change in the cause of chronic • Cancer
pancreatitis is not clear.57 • Post-traumatic scarring
Experimental studies have shown that, although the • Post-duct destruction in severe attack
pancreas processes ethanol efficiently (via a non-oxidative Recurrent acute pancreatitis
route that produces fatty acid ethyl esters, and by
oxidation via the acetaldehyde pathway), its metabolites Autoimmune
injure acinar cells and activate stellate cells in vitro.42,58
Miscellaneous
However, prolonged ethanol feeding does not induce
• Gall stones
chronic pancreatitis.58,59 Hence, the finding of a latent
• After transplant
interval of 15 years or more in patients who consumed
• After irradiation
150 g or more of ethanol per day—as most recently noted
• Vascular disease
in India60—is unsurprising. Moreover, less than 10% of
people who drink alcohol in excess develop the disease.61 Idiopathic
Collectively, these findings suggest that other factors • Early or late onset
interact to amplify ethanol toxicity in vivo. • Tropical
In animal models, small doses of ethanol induce
CFTR=cystic fibrosis transmenbrane conductance regulator. PRSS1=protease serine
CYP2E1, thus increasing the toxicity from other chemicals cationic trypsinogen. SPINK1=serine protease inhibitor Kazal. *Other, less common
to which the animal is simultaneously exposed.62,63 These mutations have been described.
results might rationalise the old observation that there is
no threshold for the pancreatic toxicity of ethanol,1 but
recent data suggest there is a threshold at 60 g per day.55 (manioc) were implicated. The classic description of
Moreover, CYP2E1 is the main pathway that metabolises tropical pancreatitis was from Kerala, south India;66
ethanol upon chronic excessive ingestion,63 but this however, hospital admission statistics revealed a decline
pathway releases ROS.64 in the disease by six times between 1962 and 1987,66
without a change in cassava consumption. Instead, the
Idiopathic decline coincided with the introduction of electricity in
60–70% of cases of chronic pancreatitis in India and this province, which removed the dependence on
China are labelled as idiopathic, as are around half the traditional lighting (see below). At present, tropical
cases in Japan.7 Tropical pancreatitis is a form of pancreatitis accounts for just 3·8 % of cases of chronic
idiopathic pancreatitis that affects young people and pancreatitis in India.60
has a propensity to diabetes and large calculi.65 This
disease is mainly reported in developing countries of Other toxic causes
Asia, Africa, and Central America, where severe Cigarette smoke has emerged as a strong independent
malnutrition and cyanogenic glycosides in cassava risk factor for chronic pancreatitis;55,67 the link was verified
www.thelancet.com Vol 377 April 2, 2011 1187
Seminar
by inhalation toxicology experiments.68,69 A case-control Idiopathic chronic pancreatitis is associated with a
study from the UK identified occupational volatile mutation in the CFTR gene.80,82,83 Patients can have one
hydrocarbons as another independent risk factor.70 This abnormal recessive allele, but possession of two confers
connection is upheld by descriptive studies from Chennai, a 40 times increased risk of developing idiopathic chronic
India,71 and Soweto, South Africa,72 which also reported pancreatitis, which rises to 500 times in patients who
regular contact with kerosene or paraffin, respectively, in also have a SPINK1 mutation.83 Some patients with
cookers, heaters, or lamps in patients with chronic apparent idiopathic chronic pancreatitis who have CFTR
pancreatitis (potentially relevant to Kerala, see above). mutations have an atypical form of cystic fibrosis.80 Three
Toxic damage to the pancreas by petrochemicals has been overlooked aspects of CFTR function have been reviewed
documented in lower vertebrates.40 Moreover, the simplest recently.32 CFTR is present in the luminal pole of acinar
animal model of chronic pancreatitis, which develops via cells where it might facilitate membrane recycling and
an acute phase, involves just one parenteral injection of exocytosis, like it does elsewhere. CFTR transports
dibutyltin (which has many industrial uses) and the injury bicarbonate and glutathione—which facilitate the
is amplified by alcohol.73 solubility of mucins in secretions—across the luminal
All these findings reinforce the pathological evidence membrane of ductal cells adjacent to the centroacinar
(figure 2) that the pancreas is a versatile but also space. CFTR is inactivated by electrophilic stress but is
vulnerable xenobiotic-metabolising organ.40 Inhaled protected by thiols and ascorbic acid. Moreover, CFTR is
xenobiotics that survive the pulmonary circulation would mislocalised to the cytoplasm of ductal cells in patients
pose the biggest threat (figure 2A) by striking the with chronic pancreatitis; this misplacement is corrected
pancreas directly via its rich arterial supply. in autoimmune disease by steroids, which also reduce
inflammation, restore bicarbonate and enzyme secretion,
Autoimmune and regenerate acinar cells.84
Autoimmune pancreatitis (2–4% of cases57) can be part Mutations in CFTR and SPINK1 have also been
of a multisystem disease (type 1) or can affect the described in patients with hypertriglyceridaemia or
pancreas alone (type 2).50,51 Aberrant human leucocyte hyperparathyroidism who develop pancreatitis.32 At
antigen DR-1 expression on pancreatic ductal cells present, molecular deficits that contribute to chronic
might present autoantigens to lymphocytes. Proposed pancreatitis have been identified in less than 10% of
pancreas-specific antigens include lactoferrin,28 carbonic alcoholic chronic pancreatitis and around 50% of
anhydrase, SPINK1, and a peptide that is present in cases overall.79
acinar cells that has homology to aminoacid sequences
in the plasminogen-binding protein of Helicobacter pylori74 Pathogenesis
(which might represent molecular mimicry)51 and also There is no agreement as to how these diverse causative
in ubiquitin–protein ligase74 (a cofactor for steroid factors lead to chronic pancreatitis. There are many
hormone receptors and an important peptide in the hypotheses about the pathogenesis of the disease,43 which
intracellular protein degradation pathway).75 fall into five main categories.
Genetic Ductal theory
Normally, if trypsinogen becomes prematurely activated One hypothesis suggests that ducts are the primary target
within the pancreas, it is inhibited by SPINK1 and then of the disease: theories centre on the primacy of calcifying
self-destructs or is degraded by trypsin-activated pro- protein deposits (protein plug hypothesis),1 stagnation of
teases;31 the potent inhibitor gluthathione is available if pancreatic juice, reflux of noxious bile and duodenal juice
all else fails.76 Hereditary pancreatitis is a rare condition (facilitated by passage of gallstones), and primary auto-
that is caused by a gain-of-function mutation (autosomal immune attack.
dominant, 80% penetrance) in the cationic trypsinogen
gene (PRSS1),9,10,42 which produces a degradation- Acinar theory
resistant form of trypsin.77 A transgenic mouse model Another hypothesis suggests that acini are the primary
of chronic pancreatic injury has proved this link.78 The target: alcohol is thought to injure acinar cells directly
PRSS1 mutation is not associated with alcoholic or (toxic metabolite hypothesis) or by increasing the cell’s
tropical chronic pancreatitis.79 By contrast, a loss-of- sensitivity to cholecystokinin (CCK) or via CYP2E1, while
function mutation in SPINK1 is strongly associated also activating stellate cells, especially in the presence of
with idiopathic disease79–82 but is thought to be a endotoxin.42,58 Another suggestion is that the disease is
predisposing or modifying factor rather than being caused by cyanide toxicity of the pancreas.
directly causative.42,79,80 Mutations in other genes that
could increase the threat from trypsin have also been Two-hits theory
described,79 as has a loss-of-function mutation in the Two so-called hits are additionally suggested as causing
PRSS2 gene (encoding anionic trypsinogen), which the disease: variations include a duct-to-acinar sequence,
protects against pancreatitis.79,80 vice versa, or double acinar hits. The last of these is the
1188 www.thelancet.com Vol 377 April 2, 2011
Seminar
most popular theory and incorporates the idea that constant pain; symptoms and signs of local complications
recurrent necrosis leads to periductal fibrosis.11 The first of the disease (eg, pseudocyst, obstruction of adjacent
attack of pancreatitis is taken to represent autodigestion organs, or vascular thrombosis); or complaints that suggest
caused by unregulated trypsin activity in the acinar cell. If exocrine or endocrine pancreatic failure, or both, by which
this attack is severe enough to recruit macrophages stage pancreatic calculi are often present. These features
(sentinel acute pancreatitis event hypothesis), subsequent form the basis for the most recent classification system
damage to the gland (by alcohol or electrophilic stress) (figure 3).47 In alcoholic disease, the interval from first
leads to fibrosis via macrophage-primed stellate cells. attack to steatorrhoea (signifying >95% loss of acini) is
around 13 years, which is substantially shorter than in
Electrophilic stress theory early-onset idiopathic disease12,86 or hereditary pancreatitis
The electrophilic stress theory is the pancreatic equivalent (≥26 years).12 Pancreatic calculi appear earliest in tropical
of paracetamol or carbon tetrachloride hepatotoxicity, pancreatitis,65 and earlier in alcoholic than idiopathic
which results from insufficient protection by glutathione disease.86 Diabetes might precede, begin at the same time
against electrophilic attack (via CYP) on key as, or start after steatorrhoea.65,88
macromolecules—not least, enzymes in the methionine Pain is the over-riding symptom in all but 10–15% of
trans-sulphuration pathway towards glutathione. How- cases of chronic pancreatitis; these cases are usually elderly
ever, in chronic pancreatitis electrophilic stress from patients with idiopathic disease12,86 or patients with
toxic metabolites—and, thereby, recurrent pancrea- autoimmune pancreatitis who might present with
stasis—develops over many years as a result of repetitive steatorrhoea, diabetes, or jaundice.50,51 The pain is wearying
exposures to multiple xenobiotics.41 Previous dietary and occurs in episodes that last about 1 week, or is constant.
insufficiency of micronutrients, especially methionine It starts in the epigastrium and moves through to the dorsal
and ascorbic acid, facilitates the problem.41,85 The diversion spine or localises to the left hypochondrium, radiating to
of free radical oxidation products into the interstitium the left infrascapular region. The pain is sometimes
causes mast cells to degranulate, leading to inflammation, associated with nausea and vomiting and can be partially
activation of nociceptive axon reflexes, and fibrosis.41 The eased by sitting up and leaning forward or by application of
realisation that compromised availability of methyl and local heat or other counterirritants to the dorsal spine or
thiol (glutathione) moieties underlies chronic pancreatitis epigastrium. The pain can be so severe that patients fear
has allowed an extension of the electrophilic stress food and lose weight. Most,12,86,89 but not all,88 studies have
concept to chronic pancreatitis that is associated with reported that pain diminishes markedly once the disease
gene mutations.32 Thus, the daily exposure of acinar cells burns out (which suggests that viable acini are a prerequisite
to traces of trypsin in people with PRSS1 or SPINK1 for pancreatic pain). However, by then patients often have
mutations is expected to strain glutathione reserves. Of become addicted to narcotic analgesics, which could cause
particular note, those with a CFTR mutation would be them to lose their jobs, homes, or families.88,90
left vulnerable not only to pancreastasis but also to Panel 2 lists factors that might contribute to pain in
intraductal calcifying protein plugs (large duct disease) patients with chronic pancreatitis:36 mast cell degranulation
when the residual CFTR protein is immobilised by products and hydrogen sulphide are plausible mediators
electrophilic stress.32 of the pancreatic component.91,92 The intensity of the pain
contrasts with the absence of specific signs in
Multiple-cause theory
The final hypothesis states that different causative factors
lead to damage via different pathways: this concept Attacks of apparent
acute pancreatitis A Early
incorporates the other theories while noting that Pain
pancreatic ischaemia can aggravate the disease.43
Complications
Clinical features • Bile duct stricture
• Duodenal stricture
Alcoholic chronic pancreatitis presents in the fourth or • Vascular stricture
fifth decade of life and mainly affects men.86 Idiopathic Clinical • Portal hypertension B Intermediate Cause
criteria • Pseudocyst
disease has early-onset (second decade) and late-onset • Pancreatic fistula
(sixth decade) forms, which have equal gender distri- • Pancreatic ascites
bution.12,86 Hereditary disease manifests at around 10 years87 • Rare, eg, colonic
stricture C End stage
and tropical pancreatitis at between 20 and 30 years,65 1 endocrine
whereas the more common type-1 form of autoimmune 2 exocrine
disease affects men in the sixth decade.51 Pancreatic failure 3 both
Presenting features of chronic pancreatitis usually fall
Figure 3: Proposal for a clinically based classification system for
into one of four groups: apparent acute or recurrent acute chronic pancreatitis
pancreatitis (the true diagnosis of chronic pancreatitis is For example, a patient may be described as having chronic pancreatitis
suspected when attacks recur after cholecystectomy); (idiopathic), stage B, bile duct.47
www.thelancet.com Vol 377 April 2, 2011 1189
Seminar
uncomplicated disease. Erythema ab igne is a useful Ordinary chronic pancreatitis has a high mortality
pointer for diagnosis of chronic pancreatitis in these rate—nearly 50% within 20–25 years of disease onset,12
patients, as is meteorism in patients whose pain has led to as a result of complications of an attack, coexisting
dependence on narcotic analgesics (figure 4). An epigastric disease, or the effects of alcoholism. Patients with
swelling suggests a pseudocyst, inflammatory mass, or chronic pancreatitis have an increased risk of pancreatic
cancer. Patients with multisystem involvement usually cancer,93 which accounts for 3% of deaths.86 Although
have the autoimmune form of chronic pancreatitis. the risk of pancreatic cancer is especially high in patients
with hereditary pancreatitis,87 they do not have a higher
mortality risk than the general population.94 Autoimmune
Panel 2: Pain in chronic pancreatitis pancreatitis also does not affect long-term survival.95
Caused by the disease
Diagnosis
Active inflammation*
Routine laboratory tests might reveal incipient diabetes,
Altered nociception type-1 hyperlipidaemia, or hypercalcaemia in patients
• Neurogenic inflammation* with suspected chronic pancreatitis. If type-1 auto-
• Visceral nerve sensitisation* immune disease is a possibility, serology will show
• Central nerve sensitisation raised concentrations of γ-globulin, IgG (IgG4 pre-
• Psychological dominantly), and various antibodies, including anti-
Hypertension lactoferrin, anti-carbonic anhydrase, rheumatoid factor,
• Ductal or tissue via increased cholecystokinin and anti-nuclear antibody.50,51 An abnormal liver function
profile suggests alcoholic liver disease, non-alcoholic
Tissue ischaemia
steatohepatitis,96 sclerosing cholangitis,50,51,96 metastases
Caused by complications from superimposed pancreatic cancer, gallstones, or,
• Inflammatory mass in head of gland most commonly, constriction of the intrapancreatic bile
• Obstruction of bile duct or duodenum duct, which occurs early in autoimmune pancreatitis,50,51
• Pseudocyst but is late otherwise.47
• Cancer of the pancreas Confirmation of the diagnosis of (non-calcific) chronic
pancreatitis is by histology of a wedge biopsy or resected
Caused by treatment specimen of pancreas. However, this is impractical. A
• Opiate gastroparesis or constipation reduction in bicarbonate with or without enzyme
Caused by unrelated problems content of duodenal aspirates after intubation and
• Peptic ulcer hormonal stimulation (by secretin with or without CCK
• Gall stones or its analogue caerulein), and abnormalities in the
• Mesenteric ischaemia pancreatic duct system on endoscopic retrograde
• Small-bowel stricture cholangiopancreatography (ERCP) are the most efficient
• Somatic (eg, surgical scar) alternative diagnostic techniques—with the former
substantially better at detecting small-duct disease than
*Mast cell degranulation products and hydrogen sulphide are potential mediators
(see text).
the latter.2,4 However, the secretory test is available in
only a few centres worldwide (and whether or not an
A B
Figure 4: Clinical features in chronic pancreatitis
(A) Erythema ab igne across the upper abdomen in a young patient with recurrent pancreatitis despite cholecystectomy for multiple gallstones (vertical scar). (B) Plain
abdominal radiograph shows heavy calcification in the pancreatic head (arrow) and a loaded colon in a patient with abdominal distension who was addicted to opiates.
1190 www.thelancet.com Vol 377 April 2, 2011
Seminar
endoscopic secretory test is as good is unclear).97
A B
Moreover, ERCP for diagnosis has largely been
abandoned in favour of magnetic resonance
cholangiopancreatography (MRCP) because ERCP can
precipitate pancreatitis in up to 4% of patients.9
There is no non-invasive test that can substitute for the
hormonal test for chronic pancreatitis.2 By contrast,
sophisticated imaging methods have rapidly developed,
such that the traditional ultrasound scan to visualise the
pancreas itself is virtually obsolete (but see figure 5). The
repertoire of imaging techniques is impressive:
multidetector CT (MDCT; figure 5); MRI;97 MRCP
(figure 6), which provides excellent images of the main
pancreatic duct98 but not always of the side-branch
changes as shown by ERCP; secretin-enhanced MRCP, Figure 5: Examples of ultrasound and multidetector images in patients with chronic pancreatitis
which also shows duodenal filling by pancreatobiliary (A) Transabdominal ultrasound scan showing a uniformly swollen, hypoechoic pancreas (arrowed), typical of
autoimmune pancreatitis. (B) Multidetector CT showing pancreatic calculi in an atrophic pancreas (long arrow)
secretions99 and is more accurate than standard MRCP in and a pseudocyst at the tail of the pancreas (short arrow).
identifying small-duct disease;100 endoscopic ultrasound
(EUS),101,102 which identifies both parenchymal and ductal A B
alterations (figure 6; now classified as the Rosemont
criteria),102 but which is observer-dependent and tends to
overdiagnose the disease;67 diffusion-weighted MRI;103
and PET.104 The last two imaging techniques have not
been properly assessed in chronic pancreatitis, whereas
the role of EUS continues to advance.
No investigation algorithm is suitable worldwide,
because much depends on available resources and
expertise, but a battery of tests should not be used for
diagnosis of suspected chronic pancreatitis because this Figure 6: Examples of three-dimensional magnetic resonance cholangiopancreatogram and endoscopic
will generate many false positive outcomes and cause ultrasound in patients with chronic pancreatitis
distress to the patient.2 Figure 7 presents a sequential (A) Three-dimensional magnetic resonance cholangiopancreatogram shows a minimally dilated biliary tree and
moderately dilated irregular main pancreatic duct. (B) Endoscopic ultrasound scan shows a minimally dilated
scheme for diagnosis of the disease, on the basis of pancreatic duct in the head of pancreas (arrowed) consistent with mild chronic pancreatitis: the distal common
whether or not the secretin test is available. This scheme bile duct appears normal (arrow head).
recognises that an abdominal radiograph will show
pancreatic calculi (nearly 100% specificity; figure 4) in at
least 30% of patients overall and in most patients with disease, for which there are no serum markers), a
tropical pancreatitis. This stepwise approach is therapeutic trial of steroids or histology (of core biopsy or
unnecessary in a patient who presents with fatty stools resected specimen), or both might be needed.50,51
after a long history of pancreatitis attacks or pain. In this There are two difficult diagnostic issues that must be
event, any of the following tests is probably sufficient for addressed. First, how can one distinguish between an
diagnosis: acid steatocrit (high value) on a spot stool inflammatory mass of ordinary chronic pancreatitis, focal
sample (which obviates the need for the traditional 3-day autoimmune disease, and pancreatic adenocarcinoma
faecal fat test);105 faecal elastase (low);105 recovery in expired with upstream chronic pancreatitis? Raised IgG
air of ¹³C (low) from a ¹³C-labelled mixed triglyceride concentrations can occur in all three settings and existing
load;106 or serum trypsinogen (low).4 However, a CT scan tumour markers are not specific enough to distinguish
is needed to identify the disease type. between them, although new molecular markers are being
Imaging tests show distinctive changes in type-1 developed.108 EUS or MDCT-guided core biopsy can be
autoimmune pancreatitis. Both ultrasound and MDCT used to confirm autoimmune pancreatitis, or a simple
typically show a diffusely enlarged sausage-shaped gland needle biopsy might identify tumour cells. ¹⁸F-fluoro-
(figure 5). ERCP shows long or multiple strictures of the deoxyglucose PET with CT facilitates the identification of
pancreatic duct and sometimes a long stricture in the cancer,104 but increased uptake is also a feature of
distal bile duct or sclerosing cholangitis.50,51 Findings autoimmune pancreatitis (as is increased uptake of
from one study suggest that MRCP cannot replace ERCP gallium).50,51 A pancreatectomy specimen might have to be
for the diagnosis of autoimmune disease.107 These used as the final diagnostic test, as it is for detecting an
imaging features are sufficient to make the diagnosis in a intraductal papillary mucinous tumour in a patient who
patient with an increased concentration of IgG4 in serum. has suspected idiopathic large-duct disease.109 Second,
If diagnostic doubt exists (as in a patient with type-2 should the clinician start a search for genetic mutations?
www.thelancet.com Vol 377 April 2, 2011 1191
Seminar
When providing treatment to control the pain
Suspected chronic associated with chronic pancreatitis, the patient’s fears
pancreatitis
and misconceptions about the disease should be
Positive
addressed sympathetically. Time should be spent
Plain radiograph for calculi
discussing the disease with the patient at the first clinic
Negative visit, with particular attention paid to circumstances
Positive
Multidetector CT surrounding the first attack. Patients should be advised
Negative to avoid alcohol and cigarettes, although there is no
Suspected small-duct Large-duct
evidence that abstinence from alcohol slows the disease
disease disease and the effect of alcohol on pain is debated.67,89 A dietary
assessment should be done (see later). Where warranted,
No Secretin test available? the help of a psychologist or pain therapy specialist
Yes should be sought, and the primary-care practitioner
Positive
must also be briefed on treatment strategy. Continuity of
Secretin test care is important to gain the patient’s trust and to
Negative
Positive minimise the risk of addiction to narcotics.
Magnetic resonance
cholangiopancreatography
after secretin stimulation Analgesics
Regular analgesics are superfluous in patients with
Negative
sporadic attacks but are needed in those with background
Positive pain. Use of analgesics should broadly follow WHO
Endoscopic ultrasound
guidelines for cancer pain.110 Briefly, analgesic
Negative
Reconsider other diagnoses Chronic
treatment begins with paracetamol or a non-steroidal
Re-test at intervals pancreatitis anti-inflammatory drug, or both, followed by a mild
Therapeutic trial of opioid such as tramadol, perhaps coupled with a
micronutrients?
neuroleptic antidepressant. Narcotic analgesics should
Figure 7: Algorithm for the diagnosis of chronic pancreatitis
be avoided if possible. A simple pain diary with a 10 cm
visual analogue scale is useful, as is a baseline quality-of-
life assessment. Analgesia devices to deliver morphine
A recent review gives valuable guidance.80 PRSS1 mutation that are controlled by the patient should not be used,
testing for diagnostic purposes is acceptable in even in an attack. Such drugs can worsen pain by
symptomatic young individuals or in those with a family inducing mast cell degranulation111 and (possibly thereby17)
history of pancreatitis, but counselling and clinical follow- cause gastroparesis4 and constipation (figure 4).
up are needed if the result is positive. There is no indication
for SPINK1 mutation testing. At present there is no Steroids and enzyme therapy
rationale for CFTR mutation testing in the setting of Treatment with steroids is associated with rapid relief
pancreatitis alone. Instead, a sweat test should be done if of symptoms in autoimmune pancreatitis.50,51 The
atypical cystic fibrosis is suspected, and patients should be starting dose is 30–40 mg per day of prednisolone,
referred to a specialist clinic when sweat chloride which is tapered over 3 months while monitoring
concentration is borderline (40–59 mmol/L) or abnormal serum IgG concentrations and imaging findings. Long-
(>60 mmol/L). However, the vulnerability of CFTR to term maintenance with 5·0–7·5 mg per day of
electrophilic stress potentially explains both false positive prednisolone is recommended to prevent relapses.50
sweat tests and abnormal nasal potential difference studies Recurrences, which typically occur in type-1 disease,95
in a variety of conditions (eg, severe malnutrition).32 favour the development of pancreatic calculi.112
In patients with small-duct disease, pancreatic acinar
Treatment cells are suggested to be under constant stimulation by
Treatment goals CCK because subnormal delivery of pancreatic proteases
The goals of treatment for chronic pancreatitis are to into the duodenum allows improved survival of a CCK-
relieve acute or chronic pain, calm the disease process to releasing peptide from the duodenal mucosa.4 Hence,
prevent recurrent attacks, correct metabolic consequences the following potential treatments have been successfully
such as diabetes or malnutrition, manage complications tested:4 oral pancreatic enzymes (non-enteric coated, two
when they arise, and address psychosocial problems. trials), subcutaneous octreotide (one trial), and oral
Endoscopic treatment, surgery, or both, are only needed dosing with the CCK-A receptor antagonist loxiglumide
when optimum medical treatment fails to relieve pain (one trial). However, this issue is contentious,113,114 and the
(figure 8) and to deal with specific complications (figure 3). explanation that these measures “allow the pancreas to
A detailed discussion of complications is beyond the rest”4 is at odds with the finding that the exocytosis
scope of this Seminar. apparatus is already paralysed in an attack (figure 1) and
1192 www.thelancet.com Vol 377 April 2, 2011
Seminar
hindered thereafter.32 Other explanations might be that
such treatments act by blunting an effect of CCK on pain Painful chronic pancreatitis
pathways in the CNS36 or by ameliorating electrophilic
stress (see later).115 Non-narcotic analgesia
Alcohol and cigarette avoidance
Dietary assessment Exclude non-pancreatic pain Treatment
Micronutrient therapy Psychosocial issues Conservative treatment for 10 weeks effective
Micronutrient therapy is designed to supply methyl and Micronutrient treatment
Pancreatic enzyme treatment Treatment
thiol moieties that are essential for the exocytosis not
apparatus (figure 1) while protecting it against effective
electrophilic attack, as by CYP-derived ROS or reactive
xenobiotics species (figure 2).32 Findings from six
Large–duct disease Small–duct disease
clinical trials have reported that micronutrient therapy
controls pain and curbs attacks in patients with chronic
pancreatitis.116–122 Of these trials, three were Pancreatic mass No mass
descriptive116–118 and three were placebo-controlled.119–122
However, the different ways of expressing outcome
precludes a meta-analysis.123 The study with the highest Treatment
Cyst or pseudocyst Solid mass Endoscopic or surgical
power (80%) to detect a difference between treatment duct drainage effective
and placebo was from Delhi:122 after 6 months’ treatment
(which included pancreatic enzymes in all patients)
Treatment
there was a greater reduction in the number of painful Suspected Suspected not
days per month and in the use of analgesic tablets in autoimmune cancer effective
pancreatitis
the treatment group than in the placebo group;
Treatment
substantially more patients became pain free, and not effective Neural Treatment
biochemical markers of electrophilic stress were Trial of steroids manipulation* effective
lowered by active treatment.
Studies from Manchester, UK, suggested that the Endoscopic CT guided or endoscopic Treatment
drainage ultrasound-guided biopsy not
micronutrient therapy formulation should include effective
methionine and vitamin C,124 with the need for selenium
assessed by measuring blood concentrations. Vitamin E
Treatment Treatment Cancer Doubt
and β carotene were included in the first trial because effective effective confirmed persists
Pancreatectomy
there was no commercial preparation that did not include
them,119 and three of the other five trials also used this Figure 8: Algorithm for the management of painful chronic pancreatitis
protocol.116,121,122 Improvement, as judged by the number of Note that the solid mass in autoimmune pancreatitis is often in the head of pancreas and suggests cancer,
attacks, admission episodes, pain diaries, pain intensity, but that ducts are usually constricted. *Procedures include thoracic splanchnicectomy, coeliac plexus block,
and neurostimulation.
or permutations and combinations of these factors,
occurred by 10–12 weeks.119,121,122 In the UK, the micro-
nutrient therapy preparation Antox (Pharma Nord, glutathione levels have increased and that concentrations
Morpeth, UK) is a convenient means of dosing because it of the prescribed micronutrients are not excessive,
contains all the desired items. A starting regimen of two because this would compromise the physiological roles of
tablets of Antox three times per day provides daily doses ROS.127,128 Very recent reports indicate the need to keep
of 2·88 g methionine (but up to 4 g might initially be track of blood homocysteine, and concentrations of
needed in some patients),125 720 mg vitamin C, 300 μg vitamins (B6, B12, folic acid) that serve as cofactors of
organic selenium, and 210 mg vitamin E (which is enzymes that govern homocysteine removal—either by
unnecessary until steatorrhoea develops).126 This treat- facilitating its transmethylation back to methionine, or by
ment has no significant side-effects now that β carotene ensuring its passage along the transsulphuration pathway
has been withdrawn because of cosmetic problems:125 towards glutathione.32,34,41,129 Of particular interest, elevated
one patient (of >300) developed schizophrenia when on homocysteine has been recorded in people at Soweto
4 g of methionine daily but, of note, this patient had a (South Africa) who drank more than 100 g alcohol per day
strong family history of psychiatric disease.125 for many years130—a group that is traditionally regarded
Patients should also be given dietary advice on as being at high risk of chronic pancreatitis.55
antioxidant-rich foods to aid the long-term management Treatment for 10 weeks is recommended before any
of the disease. It should be stressed that culinary invasive procedure in patients with chronic pancreatitis,
practices—eg, frying vegetables at high temperature (as to calm the disease process. Full treatment is usually
in south India41)—could compromise the bioavailability of needed for 6 months, followed by a gradual dose reduction
antioxidants, notably of ascorbic acid.32 Blood monitoring guided by biochemical data and patients’ symptoms.125 We
is essential to ensure that plasma and erythrocyte recorded treatment failure in 10% of patients, usually
www.thelancet.com Vol 377 April 2, 2011 1193
Seminar
because of non-compliance (eg, in patients who misuse 2 years in patients with intraductal calculi;138 however,
alcohol) or a large cyst or pseudocyst;125 otherwise, lithotripsy can occasionally precipitate acute pancrea-
symptom control was achieved by choline supplements to titis.133 Thoracoscopic splanchnicectomy can provide good
boost methyl supply.32 Moreover, micronutrient therapy initial pain relief, but pain recurs by 15 months in more
has no effect on painful conditions that might be than 50% of patients.139
misdiagnosed as chronic pancreatitis (unpublished); once
validated, this finding could form the basis for a therapeutic Surgery
trial when the diagnosis remains equivocal after full Historically, around 50% of patients with chronic
testing (figure 7). Finally, there is increasing evidence to pancreatitis referred to surgical clinics require an operation
support the idea that a daily micronutrient supplement compared with around 25% on long-term follow-up in a
might abort the development of chronic pancreatitis in specialist medical clinic.88 Micronutrient treatment seems
groups or even populations at risk of the disease.32,130 to substantially reduce the need for surgery.82,125,132 The
Micronutrient treatment is better at controlling pain objectives of surgery are to decompress obstructed ducts
and improving quality of life than conventional (to relieve pain) and at the same time to preserve pancreatic
treatment.131 Moreover, long-term micronutrient tissue as well as adjacent organs (to preserve function),
treatment might curb disease progression.82 Excluding while recognising that the head of the pancreas constitutes
typical autoimmune pancreatitis, which can be treated the so-called pacemaker of chronic pancreatitis. The
with steroids, micronutrient treatment has been effective simplest operation—lateral pancreaticojejunostomy—
irrespective of cause (including mutations in PRSS1,118 provides immediate pain relief in many patients but pain
CFTR,82 and SPINK182), disease duration,131 or ductal tends to recur with the passage of time. Distal pancrea-
anatomy (large-duct calcifying or small-duct disease), tectomy, like pancreaticojejunostomy, does not address the
and also when there is an inflammatory calcified mass.132 problem of disease in the head of the pancreas, which can
By contrast, the antioxidants allopurinol and curcumin continue to deteriorate. Moreover, distal pancreatectomy
have been ineffective for treatment of chronic pancreatitis can result in removal of the functionally most active part of
in clinical trials.32 Two multicentre trials of Antox are the gland. Pancreaticoduodenectomy gives good pain
in progress (Current Controlled Trials numbers relief, but is a major operation. It is indicated in groove
ISRCTN21047731 and ISRCTN44912429). pancreatitis if there is duodenal obstruction or when
neoplasia cannot be ruled out preoperatively.140
Treatment of steatorrhoea and diabetes Duodenum-preserving head resection combined, when
The treatment of pancreatic steatorrhoea usually begins appropriate, with lateral pancreaticojejunostomy has
with 30 000 IU of lipase per meal in an acid-resistant been a major advance: only 8·7% of patients continued to
enzyme preparation. In patients who do not respond to have pancreatic pain at a median of 5·7 years follow-up,
this treatment, a low-fat diet (50–75 g per day), dose whereas 93% of patients had pancreatic pain
increase, gastric proton-pump inhibitor, or a combination preoperatively.141 The operation was simplified by carving
thereof should be recommended.67 A check on fat-soluble out an inverted cone from the pancreatic head, allowing
vitamin status is advisable.126 The main aim in the the cavity and the distal duct to drain into a jejunal loop,
treatment of diabetes in patients with chronic pancreatitis thus removing the complex mass of obstructed ducts and
is to prevent hypoglycaemia caused by deficiency of inflammatory tissue that frequently lies within the head
glucagon; simple insulin regimens are preferable. of the gland.142 A further simplification made this
operation suitable for patients in whom there was little in
Endoscopic treatment the way of duct dilatation: a so-called ice-cream scoop is
Of the many potential indications for endoscopic taken out of the pancreatic head to leave a thin rim of
treatment of chronic pancreatitis,133 two are undisputed. pancreas laterally and posteriorly. Pain improved in
First, EUS can be used to facilitate transmural drainage of 55% of patients after 41 months of follow-up.143
pseudocysts that are not connected to the pancreatic duct A precise assessment of the merits of the different
system, and endoscopically placed transpapillary stents in operations for painful chronic pancreatitis has been
the duct are useful when they do134 or when a duct leak confounded by an absence of agreement about
leads to pancreatic ascites or pleural effusion.135 Second, indications for surgery, details of the surgical
endoscopic stenting of the bile duct is a useful temporary techniques, and methods used to measure outcomes.144
measure in patients with a distal duct stricture. However, there is no doubt that the safety of conser-
Limited comparative data suggest that surgery is more vative operations (eg, lateral pancreaticojejunostomy
effective136 and has a more durable effect in controlling combined with limited excision of the head of the
pain137 than endoscopic dilatation or stenting of the gland) has improved: operative mortality, about 5% with
pancreatic duct. Findings from a randomised clinical traditional resection of the head of pancreas, has fallen
trial showed that extracorporeal shock-wave lithotripsy to 0–3% and morbidity has been halved.145 There seems
with or without endoscopic clearance of stone fragments to be little if any advantage to be gained from total
was equally effective at reducing pain over the subsequent pancreatectomy with islet transplant.146
1194 www.thelancet.com Vol 377 April 2, 2011
Seminar
Conclusions 22 Capdevila A, Decha-Umphai W, Song K-H, Borchardt RT,
Chronic pancreatitis remains a challenging disease. Wagner C. Pancreatic exocrine secretion is blocked by inhibitors
of methylation. Arch Biochem Biophys 1997; 345: 47–55.
Resective surgery continues to be the definitive treatment 23 Mårtennson J, Bolin T. Sulphur amino acid metabolism in chronic
for persistent pain, but is not ideal in a chronic relapsing pancreatitis. Am J Gastroenterol 1986; 81: 1179–84.
inflammatory process. Micronutrient treatment might 24 Braganza JM, Scott P, Bilton D, et al. Evidence for early oxidative
stress in acute pancreatitis. Int J Pancreatol 1995; 17: 69–81.
offer a viable alternative.
25 Rahman SH, Srinivasan AR, Nicolaou A. Transsulfuration defects
Contributors and increased glutathione degradation in severe acute pancreatitis.
All authors participated in writing this Seminar. All authors saw and Dig Dis Sci 2009; 54: 675–82.
approved the final manuscript. 26 Santini SA, Spada C, Bononi F, et al. Enhanced lipoperoxidation
products in pure pancreatic juice: evidence for organ-specific
Conflicts of interest oxidative stress in chronic pancreatitis. Dig Liver Dis 2003;
We declare that we have no conflicts of interest. 35: 888–92.
Acknowledgments 27 Gutteridge JMC. Lipid peroxidation and antioxidants as biomarkers
We thank Prof J R Foster for the microphotographs (figure 2). of tissue damage. Clin Chem 1995; 41: 1819–28.
28 Jin CX, Hayakawa T, Kitagawa M, Ishiguro H. Lactoferrin
References in chronic pancreatitis. JOP 2009; 10: 237–41.
1 Sarles H. Etiopathogenesis and definition of chronic pancreatitis.
29 Graf R, Schiesser M, Reding T, et al. Exocrine meets endocrine:
Dig Dis Sci 1986; 11 (suppl): S91–107.
pancreatic stone protein and regenerating protein—two sides
2 Braganza JM. The pancreas. Recent Adv Gastroenterol 1986; of the same coin. J Surg Res 2006; 133: 113–20.
6: 251–80.
30 Freedman SD, Sakamoto K, Venu RP. GP2, the homologue to the
3 Walsh TN, Rode J, Theis BA, Russell RCG. Minimal change renal cast protein uromodulin is a major component of intraductal
chronic pancreatitis. Gut 1992; 33: 1566–71. plugs in chronic pancreatitis. J Clin Invest 1993; 92: 83–90.
4 Gupta V, Toskes PP. Diagnosis and management of chronic 31 Rinderknecht H. Pancreatic secretory enzymes. In: Go VLW,
pancreatitis. Postgrad Med J 2005; 81: 491–97. DiMagno EP, Gardner JD, Lebenthal E, Reber HA, Scheele GA, eds.
5 Lévy P, Barthet M, Mollard BR, Amouretti M, The pancreas. Biology, pathobiology, and disease. 2nd edition.
Marion-Audibert AM, Dyard F. Estimation of the prevalence New York: Raven Press, 1993: 219–52.
and incidence of chronic pancreatitis and its complications. 32 Braganza JM, Dormandy TL. Micronutrient therapy for chronic
Gastroenterol Clin Biol 2006; 30: 838–44. pancreatitis: rationale and impact. JOP 2010; 11: 99–112.
6 Otsuki M. Chronic pancreatitis in Japan: epidemiology, prognosis, 33 Syrota A, Dop-Ngassa M, Paraf A. ¹¹C-L-methionine for evaluation
diagnostic criteria, and future problems. J Gastroenterol 2003; of pancreatic exocrine function. Gut 1981; 22: 907–15.
38: 315–26.
34 Girish BN, Vaidyanathan K, Rao NA, Rajesh G, Reshmi S,
7 Garg PK, Tandon RK. Survey on chronic pancreatitis in the Balakrishnan V. Chronic pancreatitis is associated with
Asia–Pacific region. J Gastroenterol Hepatol 2004; 19: 998–1004. hyperhomocysteinemia and derangements in transsulfuration
8 Spanier BWM, Dijkgraaf MGW, Bruno MJ. Trends and forecasts and transmethylation pathways. Pancreas 2010; 39: e11–16.
of hospital admissions for acute and chronic pancreatitis in the 35 Shrikhande SV, Martignoni ME, Shrikhande M, et al. Comparison
Netherlands. Eur J Gasroenterol Hepatol 2008; 20: 653–58. of histological features and inflammatory cell reaction in alcoholic,
9 Mitchell RMS, Byrne MF, Baillie J. Pancreatitis. Lancet 2003; idiopathic and tropical chronic pancreatitis. Br J Surg 2003;
361: 1447–55. 90: 1565–72.
10 Whitcomb DC. Mechanisms of disease: advances in understanding 36 Lieb II JG, Forsmark CE. Pain and chronic pancreatitis.
the mechanisms leading to chronic pancreatitis. Aliment Pharmacol Ther 2009; 29: 706–19.
Nat Clin Pract Gastroenterol Hepatol 2004; 1: 46–52. 37 Foster JR, Idle JR, Hardwick JP, Bars R, Scott P, Braganza JM.
11 Klöppel G. Chronic pancreatitis, pseudotumors and other Induction of drug-metabolising enzymes in human pancreatic
tumor-like lesions. Mod Pathol 2007; 20: S113–31. cancer and chronic pancreatitis. J Pathol 1993; 169: 457–63.
12 Ammann RW. Diagnosis and management of chronic 38 Wacke R, Kirchner A, Prail F, et al. Up-regulation of cytochrome
pancreatitis: current knowledge. Swiss Med Wkly 2006; P450 1A2, 2C9 and 2E1 in chronic pancreatitis. Pancreas 1998;
136: 166–74. 16: 521–28.
13 Braganza JM. Evolution of pancreatitis. In: Braganza JM, ed. 39 Standop J, Schneider M, Ulrich A, Büchler MW, Pour PM.
The pathogenesis of pancreatitis. Manchester: Manchester Differences in immunohistochemical expression of
University Press, 1991: 19–33. xenobiotic-metabolizing enzymes between normal pancreas, chronic
14 Wallig M. Xenobiotic metabolism, oxidant stress and chronic pancreatitis and pancreatic cancer. Toxicol Pathol 2003; 31: 506–13.
pancreatitis: focus on glutathione. Digestion 1998; 40 Foster JR. Toxicology of the exocrine pancreas. In: Ballantyne B,
59 (suppl 4): 13–24. Marrs T, Syversen T eds. General and applied toxicology, 3rd edn.
15 Gaisano HY, Gorelick FS. New insights into the mechanisms Chichester: John Wiley and Sons, 2009: 1411–55.
of pancreatitis. Gastroenterology 2009; 136: 2040–44. 41 Braganza JM. A framework for the aetiogenesis of chronic
16 Cook LJ, Musa OA, Case RM. Intracellular transport of pancreatic pancreatitis. Digestion 1998; 58 (suppl 4): 1–12.
enzymes. Scand J Gastroenterol 1996; 219 (suppl): 1–5. 42 Witt H, Apte MV, Keim V, Wilson JS. Chronic pancreatitis:
17 Braganza JM. Towards a novel treatment strategy for acute challenges and advances in pathogenesis, genetics, diagnosis,
pancreatitis: 1: reappraisal of the evidence on aetiogenesis. and therapy. Gastroenterology 2007; 132: 1557–73.
Digestion 2001; 63: 69–91. 43 Stevens T, Conwell DL, Zuccaro G. Pathogenesis of chronic
18 Sanfey H, Bulkley B, Cameron JL. The role of oxygen-derived free pancreatitis: an evidence-based review of past theories and recent
radicals in the pathogenesis of acute pancreatitis. Ann Surg 1984; developments. Am J Gastroenterol 2004; 99: 2256–70.
200: 405–13. 44 Casini A, Galli A, Pignalosa P, et al. Collagen type 1 synthesised
19 Dabrowski A, Boguslowicz C, Dabrowska M, Tribillo I, by pancreatic periacinar stellate cells (PSC) co-localizes with lipid
Gabryelewicz A. Reactive oxygen species activate mitogen-activated peroxidation-derived aldehydes in chronic alcoholic pancreatitis.
protein kinases in pancreatic acinar cells. Pancreas 2000; J Pathol 2000; 192: 81–89.
21: 376–84. 45 Zimnoch L, Szynaka B, Puchalski Z. Mast cells and pancreatic
20 Leung P, Chan YC. Role of oxidative stress in pancreatic stellate cells in chronic pancreatitis with differently intensified
inflammation. Antioxid Redox Signal 2009; 11: 135–65. fibrosis. Hepatogastroenterology 2002; 49: 1135–38.
21 Chavnov M, Petersen OH, Tepikin A. Free radicals and 46 Lindstedt KA, Wang Y, Shiota N, et al. Activation of paracrine
the pancreatic acinar cells: role in physiology and pathology. TGF-beta1 signaling upon stimulation and degranulation of rat serosal
Philos Trans R Soc Lond B Biol Sci 2005; 360: 2273–84. mast calls: a novel function for chymase. FASEB J 2001; 15: 1377–88.
www.thelancet.com Vol 377 April 2, 2011 1195
Seminar
47 Buchler MW, Martigone ME, Friess H, Malfertheiner P. A proposal 75 Ramamoorthy S, Nawaz Z. E6-associated protein is a dual
for a new clinical classification of chronic pancreatitis. function coactivator of steroid hormone receptors.
BMC Gastroenterol 2009; 9: 93. Nucl Recept Signal 2008; 6: e006.
48 Longnecker DS. Pathology and pathogenesis of diseases 76 Steven FS, Al-Habib A. Inhibition of trypsin and chymotrypsin
of the pancreas. Am J Pathol 1982; 107: 103–21. by thiols. Biochim Biophys Acta 1979; 568: 408–15.
49 O’Sullivan BP, Freedman SD. Cystic fibrosis. Lancet 2009; 77 Halangk W, Krüger B, Ruthenbürger M, et al. Trypsin activity is
373: 1891–904. not involved in premature, intrapancreatic trypsinogen activation.
50 Shimosegawa T, Kanno A. Autoimmune pancreatitis in Japan: Am J Physiol Gastrointest Liver Physiol 2002; 282: G367–74.
overview and perspective. J Gastroenterol 2009; 44: 503–17. 78 Archer H, Jura N, Keller J, Jacobson M, Bar-sag D. A mouse
51 Park DH, Kim M-H, Chari S. Recent advances in autoimmune model of hereditary pancreatitis generated by transgenic
pancreatitis. Gut 2009; 58: 1680–89. expression of R122H trypsinogen. Gastroenterology 2006;
52 Wagner ACC. Serological tests to diagnose chronic pancreatitis. 131: 1844–55.
In: Buchler MW, Friess H, Uhl W, Malfertheiner P, eds. Chronic 79 Chen JM, Férec C. Chronic pancreatitis: genetics and
pancreatitis: novel concepts in biology and therapy. London: pathogenesis. Annu Rev Genomics Hum Genet 2009; 10: 63–87.
Blackwell, 2002: 217–22. 80 Ooi CY, Gonska T, Durie PR, Freedman SD. Genetic testing
53 Frulloni L, Gabrielli A, Pezzilli R, et al. Chronic pancreatitis: report in pancreatitis. Gastroenterology 2010; 138: 2202–06.
from a muticenter Italian survey (PanCronfAISP) on 893 patients. 81 Mahurkar S, Nageshwar Reddy D, Rao GV, Chandak GR. Genetic
Dig Liver Dis 2009; 41: 311–17. mechanisms underlying the pathogenesis of tropical calcific
54 Yan M-X, Li Y-Q. Gall stones and chronic pancreatitis: the black box pancreatitis. World J Gastroenterol 2009; 21: 256–69.
in between. Postgrad Med J 2006; 82: 254–58. 82 Midha S, Khaguria R, Shastri S, Kabra M, Garg PK. Idiopathic
55 Yadav D, Whitcomb DC. The role of alcohol and smoking chronic pancreatitis in India: phenotypic characterization and
in pancreatitis. Nat Rev Gastroenterol Hepatol 2010; 7: 131–45. strong genetic susceptibility due to SPINK1 and CFTR mutations.
56 Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of Gut 2010; 59: 800–07.
alcohol-related liver and pancreatic disease in the United States. 83 Cohn JA. Reduced CFTR function and the pathobiology of
Arch Intern Med 2008; 168: 649–56. idiopathic pancreatitis. J Clin Gastroenterol 2005; 39: S70–77.
57 Pezzilli R. Etiology of chronic pancreatitis: has it changed in the last 84 Ko SB, Mizumo N, Yatabe Y, et al. Corticosteroids correct aberrant
decade? World J Gastroenterol 2009; 15: 4737–40. CFTR localization in the duct and regenerate acinar cells in
58 Pandol SJ, Rarity M. Pathobiology of alcoholic pancreatitis. autoimmune pancreatitis. Gastroenterology 2010; 138: 1988–96.
Pancreatology 2007; 7: 105–14. 85 Segal I. Pancreatitis in Soweto, South Africa: focus on alcohol.
59 Li J, Guo M, Liu R, Wang R, Tang C. Does chronic ethanol intake Digestion 1998; 59 (suppl 4): 25–35.
cause chronic pancreatitis?: evidence and mechanism. Pancreas 86 Layer P, Yamamoto H, Kalthoff L, Clain JE, Bakken LJ,
2008; 37: 189–95. DiMagno EP. The different courses of early and late-onset
60 Balakrishnan V, Unnikrishnan AG, Thomas V, et al. Chronic idiopathic and alcoholic chronic pancreatitis. Gastroenterology
pancreatitis: a prospective nationwide study of 1086 subjects from 1994; 107: 1481–87.
India. JOP 2008; 9: 593–600. 87 Rosendahl J, Bödeker H, Mössner J, Teich N. Hereditary chronic
61 Dufour MC, Adamson MD. The epidemiology of alcohol-induced pancreatitis. Orphanet J Rare Dis 2007; 2: 1.
pancreatitis. Pancreas 2003; 27: 286–90. 88 Lankisch PG, Löhr-Happe A, Otto J, Creutzfeldt W. Natural course
62 Strubelt O. Interaction between ethanol and other hepatotoxic in chronic pancreatitis. Digestion 1993; 54: 148–55.
agents. Biochem Pharmacol 1980; 29: 1445–49. 89 Bornman PC, Girdwood AH, Marks IN, Hatfield ARW, Kottler RE.
63 Lieber CS. The discovery of the microsomal ethanol oxidizing The influence of continued alcohol intake, pancreatic duct
system and its physiological and pathological role. Drug Metab Rev hold-up, and pancreatic insufficiency on the pain pattern in
2004; 36: 511–12. chronic noncalcific and calcific pancreatitis: a comparative study.
Surg Gastroenterol 1982; 1: 5–9.
64 Gonzalez FJ. Role of cytochromes P450 in chemical toxicity and
oxidative stress: studies with CYP2E1. Mutat Res 2005; 569: 101–10. 90 Gardner TB, Kennedy AT, Gelrud A, et al. Chronic pancreatitis
and its effect on employment and health care experience: results
65 Barman KK, Premalatha G, Mohan V. Tropical chronic pancreatitis.
of a prospective American multicenter study. Pancreas 2010;
Postgrad Med J 2003; 79: 606–15.
39: 498–501.
66 Balakrishnan V. Tropical pancreatitis—epidemiology, pathogenesis
91 Hoogerwerf WA, Gondesen K, Xiao SY, Winston JH, Willis WD,
and aetiology. In: Balakrishnan V, ed. Chronic pancreatitis in India.
Pasricha PJ. The role of mast cells in the pathogenesis of pain in
Trivandrum: St Joseph’s Press, 1987: 81–85.
chronic pancreatitis. BMC Gastroenterol 2005; 5: 8.
67 Di Magno MJ, Wamsteker E-J, Lee A. Chronic pancreatitis.
92 Nishimura S, Fukushima H, Takahashi T, et al. Hydrogen sulfide
BMJ Best Practice 2010. http://bestpractice.bmj.com/best-practice/
as a novel mediator for pancreatic pain in rodents. Gut 2009;
monograph/67/highlights.html (accessed Feb 12, 2011).
58: 762–70.
68 Wittel UA, Hopt UT, Batra SK. Cigarette smoke-induced pancreatic
93 Lowenfels AB, Maisonneuve P, Cavallini G, et al. Pancreatitis
damage: experimental data. Langenbecks Arch Surg 2008;
and the risk of pancreatic cancer. N Engl J Med 1993; 328: 1433–37.
393: 581–88.
94 Rebours V, Boutron-Ruault M-C, Jooste V, et al. Mortality rate
69 Hao J-Y, Li G, Pang B. Evidence for cigarette smoke-induced
and risk factors in patients with hereditary pancreatitis: uni- and
oxidative stress in the rat pancreas. Inhalation Toxicol 2009;
multidimensional analyses. Am J Gastroenterol 2009; 104: 2312–17.
21: 1007–12.
95 Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile
70 McNamee R, Braganza JM, Hogg J, Leck I, Rose P, Cherry N.
and relapse rate of type 1 versus type 2 autoimmune pancreatitis.
Occupational exposure to hydrocarbons and chronic pancreatitis:
Gastroenterology 2010; 139: 140–48.
a case-referent study. Occup Environ Med 1994; 51: 631–37.
96 Braganza JM. The role of the liver in exocrine pancreatic disease.
71 Braganza JM, John S, Padmayalam I, et al. Xenobiotics and tropical
Int J Pancreatol 1988; 3: S19–42.
pancreatitis. Int J Pancreatol 1990; 7: 231–45.
97 Balci NC, Smith A, Momtahen AJ, et al. MRI and S-MRCP
72 Jeppe CY, Smith MD. Transversal descriptive study of xenobiotic
findings in patients with suspected chronic pancreatitis:
exposures in patients with chronic pancreatitis and pancreatic
Correlation with endoscopic pancreatic function testing (Epft).
cancer. JOP 2008; 9: 235–39.
J Magn Reson Imaging 2010; 31: 601–06.
73 Merkord J, Weber H, Jonas L, Nizze H, Henninghausen G.
98 Tamura R, Ushibashi T, Takahashi S. Chronic pancreatitis: MRCP
The influence of ethanol on long-term effects of dibutyltin
versus ERCP for quantitative caliber measurement and qualitative
dichloride (DBTC) in pancreas and liver of rats. Hum Exp Toxicol
evaluation. Radiology 2006; 238: 920–28.
1998; 17: 144–50.
99 Czako L. Diagnosis of early-stage chronic pancreatitis by
74 Frulloni L, Lunardi C, Simone R, et al. Identification of a novel
secretin-enhanced magnetic resonance cholangiopancreatography.
antibody associated with aotuimmune pancreatitis. N Engl J Med
J Gastroenterol 2007; 42 (suppl 17): 113–17.
2010; 361: 2135–42.
1196 www.thelancet.com Vol 377 April 2, 2011
Seminar
100 Sai JK, Suyama M, Kubokawa Y, Watanabe S. Diagnosis of mild 123 Monfared SSMS, Vahidi H, Abdolghaffari AH, Nikfar S,
chronic pancreatitis (Cambridge classification): comparative study Abdollahi M. Antioxidant therapy in the management of acute,
using secretin injection-magnetic resonance chronic and post-ERCP pancreatitis: a systematic review.
cholangiopancreatography and endoscopic retrograde World J Gastroenterol 2010; 15: 4481–90.
pancreatography. World J Gastroenterol 2008; 14: 1218–21. 124 Bilton D, Schofield D, Mei G, Kay PM, Bottiglieri T, Braganza JM.
101 Kahl S, Glasbrenner B, Leodolter A, Pross M, Schulz HU, Placebo-controlled trials of antioxidant therapy in patients with
Malfertheiner P. EUS in the diagnosis of early chronic pancreatitis: recurrent pancreatitis. Drug Invest 1994; 8: 10–20.
a prospective follow-up study. Gastrointest Endosc 2002; 55: 507–11. 125 McCloy RF. Chronic pancreatitis at Manchester, UK. Focus
102 Catalano MF, Sahai A, Levy M, et al. EUS-based criteria for the on antioxidant therapy. Digestion 1998; 59 (suppl 4): 36–48.
diagnosis of chronic pancreatitis: the Rosemont classification. 126 Dominguez-Muňoz JE, Iglesias-Garcia J. Oral pancreatic enzyme
Gastrointest Endosc 2009; 169: 1251–61. substitution therapy in chronic pancreatitis: is clinical response an
103 Balci NC, Perman WH, Saglam S, Akisik F, Fattahi R, Bilgin M. appropriate marker for evaluation of therapeutic efficacy? JOP 2010;
Diffusion-weighted magnetic resonance imaging of the pancreas. 11: 158–62.
Top Magn Reson Imaging 2009; 20: 43–47. 127 Li T-S, Marbán E. Physiological levels of reactive oxygen species are
104 Kumar R, Kumari A, Garg P, et al. Role of F18-FDG PET-CT required to maintain genomic stability in stem cells. Stem Cells
imaging in differentiating benign and malignant pancreatic lesions 2010; 28: 1178–85.
and its comparison with CT/MRI/EUS. J Nucl Med 2009; 128 Gutteridge JMC, Halliwell B. Antioxidants: molecules, medicines,
50 (suppl 2): 1755. and myths. Biochim Biophys Res Commun 2010; 393: 561–64.
105 Girish BN, Rajesh G, Vaidyanathan K, Balakrishnan V. Fecal 129 Braganza JM, Odom N, McCloy RF, Ubbink JB. Homocysteine
elastase1 and acid steatocrit estimation in chronic pancreatitis. and chronic pancreatitis. Pancreas 2010; 39: 1303–04.
Indian J Gastroenterol 2009; 28: 201–05. 130 Segal I, Ally R, Hunt LP, Sandle LN, Ubbink JB, Braganza JM.
106 Nakamura H, Morifuji M, Murakami Y, et al. Usefulness of a Insights into the development of alcoholic chronic pancreatitis at
13C-labeled mixed triglyceride breath test for assessing exocrine Soweto, South Africa: a controlled cross-sectional study. Pancreas
function after pancreatic surgery. Surgery 2009; 145: 168–75. (in press).
107 Kamisawa T, Tu Y, Egawa N, Okamoto A, Kodama M, Kamata N. 131 Shah NS, Makin AJ, Sheen AJ, Siriwardena AK. Quality of life
Can MRCP replace ERCP for the diagnosis of autoimmune assessment in patients with chronic pancreatitis receiving
pancreatitis? Abdom Imaging 2009; 34: 381–84. antioxidant therapy. World J Gatroenterol 2010; 16: 4066–71.
108 Mendieta Zerón H, Garcia Flores JR, Romero Prieto ML. 132 Sharer NM, Taylor PM, Linaker BD, Gutteridge JMC, Braganza JM.
Limitations in improving detection of pancreatic adenocarcinoma. Safe and successful use of vitamin C to treat painful calcific chronic
Future Oncol 2009; 5: 657–68. pancreatitis despite iron overload from primary haemochromatosis.
109 Pezzilli R. Intraductal papillary-mucinous tumor of the pancreas: Clin Drug Invest 1995; 10: 310–15.
the clinical research continues. JOP 2004; 5: 53–55. 133 Heyries L, Sahel J. Endoscopic treatment of chronic pancreatitis.
110 WHO. Cancer pain relief and palliative care: report of a WHO World J Gastroenterol 2007; 13: 6127–33.
expert committee. Geneva: World Health Organization, 1990: 134 Rosso E, Alexis N, Ghanesh P, et al. Pancreatic pseudocyst in
technical report series 804. chronic pancreatitis: endoscopic and surgical treatment. Dig Surg
111 Di Bello MG, Masini E, Ioannides C, et al. Histamine release from 2003; 20: 397–406.
rat mast cells induced by the metabolic activation of drugs of abuse 135 Pai CG, Suvana D, Bhat G. Endoscopic treatment as first-line
into free radicals. Inflamm Res 1998; 47: 122–30. therapy for pancreatic ascites and pleural effusion.
112 Kawa S, Hamano H, Ozaki Y, et al. Long-term follow-up of J Gastroenterol Hepatol 2009; 24: 1198–202.
autoimmune pancreatitis: characteristics of chronic disease and 136 Cahen DL, Gouma DJ, Nio Y, et al. Endoscopic versus surgical
recurrence. Clin Gastroenterol Hepatol 2009; 7 (suppl 11): S18–22. drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med
113 Winstead NS, Wilcox CM. Clinical trials of pancreatic enzyme 2007; 356: 676–84.
replacement for painful chronic pancreatitis—a review. 137 Kowalczyk LM, Draganov PV. Endoscopic therapy for chronic
Pancreatology 2009; 9: 344–50. pancreatitis: technical success, clinical outcomes, and
114 Shafiq N, Rana S, Bhasin D, et al. Pancreatic enzymes for chronic complications. Curr Gastroenterol Rep 2008; 11: 111–18.
pancreatitis. Cochrane Database Syst Rev 2009; 4: CD006302. 138 Dumonceau J-M, Costamagna G, Tringali A, et al. Treatment for
115 Kotzampassi K, Paramythiotis D, Makedou A, Eleftheriadis E. painful calcified chronic pancreatitis: extracorporeal shock wave
Octreotide improves oxidative stress in sodium lithotripsy versus endoscopic treatment: a randomized controlled
taurocholate-induced pancreatic injury. Annals Gastroenterol 2004; trial. Gut 2007; 56: 545–52.
17: 402–06. 139 Baghdadi S, Abbas MH, Albouz F, Ammori BJ. Systematic review
116 De las Heras-Castano G, Garcia de la Paz A, Fernandez MD, of the role of thoracoscopic splanchnicectomy in palliating the pain
Fernández Forcelledo JL. Use of antioxidants to treat pain in of patients with chronic pancreatitis. Surg Endosc 2008; 22: 580–88.
chronic pancreatitis. Rev Esp Enferm Dig 2000; 92: 381–85. 140 Laverick JM, Gordon SR, Sutton JE, Suriawinata A, Gardner TB.
117 Dítě P, Prěcechtelová M, Novotný I, Soška V, Źaková A, Lata J. A comprehensive, case-based review of groove pancreatitis. Pancreas
Changes of reactive oxidative substances in patients with 2009; 38: e169–75.
morphologically different degrees of chronic pancreatitis 141 Beger HG, Büchler M, Bittner RR, Oettinger W, Roscher R.
and effects of long-term therapy with natural antioxidants. Duodenum-preserving resection of the head of the pancreas in
Gastroenterologia Polska 2003; 10: 379–83. severe chronic pancreatitis: early and late results. Ann Surg 1989;
118 Uomo G, Talamini G, Rabitti PG. Antioxidant treatment in 209: 273–78.
hereditary pancreatitis: a pilot study on three young patients. 142 Ho HS, Frey CF. The Frey procedure: local resection of pancreatic
Dig Liver Dis 2001; 33: 58–62. head combined with lateral pancreaticojejunostomy. Arch Surg 2001;
119 Uden S, Bilton D, Nathan L, Hunt LP, Main C, Braganza JM. 136: 1353–58.
Antioxidant therapy for recurrent pancreatitis: placebo-controlled 143 Müller MW, Friess H, Leitzbach S, et al. Perioperative and follow-up
trial. Aliment Pharmacol Ther 1990; 4: 357–71. results after central pancreatic head resection (Berne technique) in
120 Uden S, Schofield D, Miller PF, Day JP, Bottiglieri T, Braganza JM. a consecutive series of patients with chronic pancreatitis. Am J Surg
Antioxidant therapy for recurrent pancreatitis: biochemical profiles 2008; 196: 364–72.
in a placebo-controlled trial. Aliment Pharmacol Ther 1992; 6: 229–40. 144 Shah NS, Siriwardena AK. Variance in elective surgery for chronic
121 Kirk GR, White JS, McKie L, et al. Combined antioxidant therapy pancreatitis. JOP 2009; 10: 30–36.
reduces pain and improves quality of life in chronic pancreatitis. 145 Andersen DK, Frey CF. The evolution of the surgical treatment
J Gastrointest Surg 2006; 10: 499–503. of chronic pancreatitis. Ann Surg 2010; 251: 18–32.
122 Bhardwaj P, Garg PK, Maulik S, Saraya A, Tandon RK, Acharya SK. 146 Garcea G, Weaver J, Phillips J, et al. Total pancreatectomy with and
A randomized controlled trial of antioxidant supplementation for without islet cell transplantation for chronic pancreatitis: a series of
pain relief in patients with chronic pancreatitis. Gastroenterology 85 consecutive patients. Pancreas 2009; 38: 1–7.
2009; 136: 149–59.
www.thelancet.com Vol 377 April 2, 2011 1197
You might also like
- A Survey of English and American Literature Module 1 3Document80 pagesA Survey of English and American Literature Module 1 3Jathalia VillaNo ratings yet
- Platelet Rich Plasma in Musculoskeletal PracticeDocument10 pagesPlatelet Rich Plasma in Musculoskeletal PracticeAmirullah AbdiNo ratings yet
- Nicola Maffulli (Eds.) - Platelet Rich Plasma in Musculoskeletal Practice-Springer-Verlag London (2016) PDFDocument256 pagesNicola Maffulli (Eds.) - Platelet Rich Plasma in Musculoskeletal Practice-Springer-Verlag London (2016) PDFedbraga-1No ratings yet
- Week 1-12 strength and conditioning programDocument6 pagesWeek 1-12 strength and conditioning programBrian Michael CarrollNo ratings yet
- Feminist Criticism in Frankenstein, Equus and The Turn of The ScrewDocument4 pagesFeminist Criticism in Frankenstein, Equus and The Turn of The ScrewLucia ToledoNo ratings yet
- GROWTH ASSESSMENT FOR 10-YEAR-OLD SCHOOLERDocument4 pagesGROWTH ASSESSMENT FOR 10-YEAR-OLD SCHOOLERYashoda SatputeNo ratings yet
- Югоизточна Европа под османско владичество 1354-1804Document531 pagesЮгоизточна Европа под османско владичество 1354-1804auroradentataNo ratings yet
- Roke TsanDocument53 pagesRoke Tsanhittaf_05No ratings yet
- Woody Plant Seed Manual - CompleteDocument1,241 pagesWoody Plant Seed Manual - CompleteJonas Sandell100% (1)
- Nursing Theories: Nightingale, Johnson, Abdellah & MoreDocument8 pagesNursing Theories: Nightingale, Johnson, Abdellah & More3amabelle arevaloNo ratings yet
- Kulkarni 2010Document11 pagesKulkarni 2010Amirullah AbdiNo ratings yet
- Fluid Resuscitation in Acute PancreatitisDocument7 pagesFluid Resuscitation in Acute PancreatitisRicardo Isique SantillanNo ratings yet
- Flgastro 2018 101102Document8 pagesFlgastro 2018 101102carolina pulidoNo ratings yet
- Practical Guide To The Management of Acute Pancreatitis: George Goodchild, Manil Chouhan, Gavin J JohnsonDocument8 pagesPractical Guide To The Management of Acute Pancreatitis: George Goodchild, Manil Chouhan, Gavin J JohnsonRene CordovaNo ratings yet
- Acute Pancreatitis: Review ArticleDocument4 pagesAcute Pancreatitis: Review ArticleFifin m saidNo ratings yet
- Acute PancreatitisDocument10 pagesAcute PancreatitisAndrés Menéndez RojasNo ratings yet
- pancreatitis-frontline-gastro-reviewDocument8 pagespancreatitis-frontline-gastro-reviewlaurentiu.ducuta12No ratings yet
- Pancreatitis AgudaDocument12 pagesPancreatitis AgudaWILLIAM RICARDO CASTAÑEDA VARGASNo ratings yet
- New Insights of Acute PancreatitisDocument18 pagesNew Insights of Acute Pancreatitispruebaprueba321765No ratings yet
- Acute Pancreatitis: SeminarDocument12 pagesAcute Pancreatitis: SeminarKaren JboNo ratings yet
- New Insights Into Acute Pancreatitis: Peter J. Lee and Georgios I. PapachristouDocument18 pagesNew Insights Into Acute Pancreatitis: Peter J. Lee and Georgios I. PapachristouandreaNo ratings yet
- Drug Induced PancreatitisDocument7 pagesDrug Induced PancreatitisHanine UsamahNo ratings yet
- Chronic PancreatitisDocument7 pagesChronic PancreatitisMr. LNo ratings yet
- Pancretitis AgudaDocument12 pagesPancretitis Agudapruebaprueba321765No ratings yet
- Pancreatitis RevDocument14 pagesPancreatitis Revbmoreno78No ratings yet
- Autoimmune PancreatitisDocument7 pagesAutoimmune PancreatitisWinstonNo ratings yet
- The Acinar-Ductal Tango in The Pathogenesis of Acute PancreatitisDocument10 pagesThe Acinar-Ductal Tango in The Pathogenesis of Acute Pancreatitispruebaprueba321765No ratings yet
- Pancreatitis Cronica Dog-CatDocument14 pagesPancreatitis Cronica Dog-CatSamantha Orozco PinedaNo ratings yet
- 2015 Article 1362Document17 pages2015 Article 1362Radityo Budi LeksonoNo ratings yet
- Jurnal: Acute PancreatitisDocument11 pagesJurnal: Acute Pancreatitisahmad fachryNo ratings yet
- Diagnosis and Management of Chronic PancreatitisDocument8 pagesDiagnosis and Management of Chronic PancreatitiscarmenNo ratings yet
- Acute Pancreatitis (Annals of IM)Document16 pagesAcute Pancreatitis (Annals of IM)Jorge Armando Arrieta GalvanNo ratings yet
- Chronic PancreatitisDocument8 pagesChronic PancreatitisSanjaya SenevirathneNo ratings yet
- Jurnal DhaDocument11 pagesJurnal DhasiydahNo ratings yet
- Chronic PancreatitisDocument14 pagesChronic PancreatitisAgus GarciaNo ratings yet
- BanksFreemanACGpancGuidelines PDFDocument23 pagesBanksFreemanACGpancGuidelines PDFJairo AndréNo ratings yet
- Management of Chronic Pancreatitis - BMJ (2024)Document16 pagesManagement of Chronic Pancreatitis - BMJ (2024)sancolaNo ratings yet
- NCDD 04272009 ResearchPlan DiseasesofPancreasDocument10 pagesNCDD 04272009 ResearchPlan DiseasesofPancreasGmail JONo ratings yet
- Pancreatitis PDFDocument10 pagesPancreatitis PDFEmilio' 'BatistaNo ratings yet
- Word Antes de Traducir Yo PDFFFDocument9 pagesWord Antes de Traducir Yo PDFFFSonia Tacuri SolanoNo ratings yet
- Pancreatite AgudaDocument8 pagesPancreatite AgudaGabriel MouraNo ratings yet
- Pharmacologic Management and Prevention of Acute PancreatitisDocument8 pagesPharmacologic Management and Prevention of Acute PancreatitisarnoldNo ratings yet
- Seminar: Definition of Chronic PancreatitisDocument14 pagesSeminar: Definition of Chronic PancreatitisCarlos Alberto Torres LópezNo ratings yet
- 10 1056@NEJMra1505202 PDFDocument10 pages10 1056@NEJMra1505202 PDFFiorella ChambiNo ratings yet
- Liver, Pancreas and Biliary Tract Problems: Research JournalDocument13 pagesLiver, Pancreas and Biliary Tract Problems: Research JournalElaine Frances IlloNo ratings yet
- Acute Pancreatitis in Dogs: Advances in Understanding, Diagnostics, and TreatmentDocument10 pagesAcute Pancreatitis in Dogs: Advances in Understanding, Diagnostics, and TreatmentLaura Tatiana CarreroNo ratings yet
- AcutePancreatitis PDFDocument22 pagesAcutePancreatitis PDFharnellaNo ratings yet
- 8a Acute PancreatitisDocument12 pages8a Acute PancreatitisTony SswwNo ratings yet
- 1 s2.0 S0140673620313106 MainDocument9 pages1 s2.0 S0140673620313106 MainEdwin Fabian Usaquen KairuzNo ratings yet
- The Revised Atlanta Classification For Acute Pancreatitis: Updates in Imaging Terminology and GuidelinesDocument12 pagesThe Revised Atlanta Classification For Acute Pancreatitis: Updates in Imaging Terminology and Guidelinesjaider luis saurith monterrosaNo ratings yet
- Acute Pancreatitis. Lancet Seminar Sept 5, 2020Document9 pagesAcute Pancreatitis. Lancet Seminar Sept 5, 2020Luis Henrique SalesNo ratings yet
- Management of Acute Pancreatitis in DogsDocument13 pagesManagement of Acute Pancreatitis in Dogsluufer19No ratings yet
- Lipase Vs AmylaseDocument6 pagesLipase Vs AmylaseLuis AcevedoNo ratings yet
- Current Advances in The Management of Chronic Pancreatitis: Disease-a-MonthDocument34 pagesCurrent Advances in The Management of Chronic Pancreatitis: Disease-a-MonthNandaNo ratings yet
- PA - Gastroenterology - 2013 - Jun - 144 (6) - 1272Document10 pagesPA - Gastroenterology - 2013 - Jun - 144 (6) - 1272Lourianne NcNo ratings yet
- Clinical ManagementDocument10 pagesClinical Managementpruebaprueba321765No ratings yet
- Acute Pancreatitis-A Clinical Update: Review ArticleDocument6 pagesAcute Pancreatitis-A Clinical Update: Review ArticleDương Ngọc DiệpNo ratings yet
- Acute Pancreatitis: Clinical PR ActiceDocument9 pagesAcute Pancreatitis: Clinical PR ActicesanthiagoschneiderNo ratings yet
- Clinical-Liver, Pancreas, and Biliary TractDocument8 pagesClinical-Liver, Pancreas, and Biliary TractKirsten HartmanNo ratings yet
- Diagnosis Biomarkers in Acute Intestinal Ischemic InjuryDocument13 pagesDiagnosis Biomarkers in Acute Intestinal Ischemic InjuryrizkyNo ratings yet
- Diagnosis and Treatment of Sclerosing CholangitisDocument17 pagesDiagnosis and Treatment of Sclerosing CholangitisjonasNo ratings yet
- Pancreatitis Aguda para Emergencia PDFDocument11 pagesPancreatitis Aguda para Emergencia PDFJudithzaloNo ratings yet
- ColangiopatiasDocument10 pagesColangiopatiasInes MendonçaNo ratings yet
- Postendoscopic Retrograde Cholangiopancreatography PancreatitisDocument7 pagesPostendoscopic Retrograde Cholangiopancreatography PancreatitisErnest Ang GrekNo ratings yet
- Laroche 1998Document9 pagesLaroche 1998takechi takechiNo ratings yet
- Chronic Pancreatitis: Review and Update of Etiology, Risk Factors, and Management (Version 1 Referees: 2 Approved)Document11 pagesChronic Pancreatitis: Review and Update of Etiology, Risk Factors, and Management (Version 1 Referees: 2 Approved)Nur FakhirahNo ratings yet
- Pankreatitis 2017Document13 pagesPankreatitis 2017GitarefinaNo ratings yet
- Diseases of the Liver and Biliary TreeFrom EverandDiseases of the Liver and Biliary TreeAnnarosa FloreaniNo ratings yet
- Pancreatitis: Medical and Surgical ManagementFrom EverandPancreatitis: Medical and Surgical ManagementDavid B. AdamsNo ratings yet
- The Pancreas: An Integrated Textbook of Basic Science, Medicine, and SurgeryFrom EverandThe Pancreas: An Integrated Textbook of Basic Science, Medicine, and SurgeryNo ratings yet
- Cardiac Myxoma Case Series 1Document2 pagesCardiac Myxoma Case Series 1Amirullah AbdiNo ratings yet
- Cardiac Myxoma Case Series 1Document2 pagesCardiac Myxoma Case Series 1Amirullah AbdiNo ratings yet
- Koran Digestive 05 Maret Kamar 2 & 3Document4 pagesKoran Digestive 05 Maret Kamar 2 & 3Amirullah AbdiNo ratings yet
- Poster Cardiac Myxoma Case Series GambarDocument2 pagesPoster Cardiac Myxoma Case Series GambarAmirullah AbdiNo ratings yet
- Cardiac Myxoma Case SeriesDocument1 pageCardiac Myxoma Case SeriesAmirullah AbdiNo ratings yet
- Salinan Salinan Terjemaha 37-70Document19 pagesSalinan Salinan Terjemaha 37-70Amirullah AbdiNo ratings yet
- Cover LetterDocument3 pagesCover Lettert3guhku2hNo ratings yet
- Properties of NMBAsDocument1 pageProperties of NMBAsAmirullah AbdiNo ratings yet
- Braganza 2011Document7 pagesBraganza 2011Amirullah AbdiNo ratings yet
- Science of The Total Environment: Lei Zhu, Wugao Zhang, Wei Liu, Zhen HuangDocument9 pagesScience of The Total Environment: Lei Zhu, Wugao Zhang, Wei Liu, Zhen HuangAmirullah AbdiNo ratings yet
- Fisiologi DefekasiDocument9 pagesFisiologi DefekasiAmirullah AbdiNo ratings yet
- Serum Prolactin and Cognitive Outcome in PsychosisDocument2 pagesSerum Prolactin and Cognitive Outcome in PsychosisAmirullah AbdiNo ratings yet
- Case Penetrating Keratoplasty in Bullous KeratopathyDocument3 pagesCase Penetrating Keratoplasty in Bullous KeratopathyAmirullah AbdiNo ratings yet
- Cardiopulmonary Resuscitation: Unusual Techniques For Unusual SituationsDocument10 pagesCardiopulmonary Resuscitation: Unusual Techniques For Unusual SituationsAmirullah AbdiNo ratings yet
- Ehp 7059Document6 pagesEhp 7059Amirullah AbdiNo ratings yet
- Anticoagulants AwalDocument16 pagesAnticoagulants AwalAmirullah AbdiNo ratings yet
- Surviving Sepsis Campaign Hour 1 Bundle 2018Document12 pagesSurviving Sepsis Campaign Hour 1 Bundle 2018Amirullah AbdiNo ratings yet
- The Natives Who Lost Their LivesDocument2 pagesThe Natives Who Lost Their LivesAmirullah AbdiNo ratings yet
- The Surviving Sepsis Campaign Bundle 2018 UpdateDocument4 pagesThe Surviving Sepsis Campaign Bundle 2018 UpdateYo MeNo ratings yet
- Do We Need A New Definition of Sepsis?: Intensive Care Medicine February 2015Document4 pagesDo We Need A New Definition of Sepsis?: Intensive Care Medicine February 2015Amirullah AbdiNo ratings yet
- Poster DR TatiDocument1 pagePoster DR TatiAmirullah AbdiNo ratings yet
- Ipi 106521Document14 pagesIpi 106521chanssickNo ratings yet
- Poster DR TatiDocument3 pagesPoster DR TatiAmirullah AbdiNo ratings yet
- Wagenlehner2007 2 PDFDocument15 pagesWagenlehner2007 2 PDFAmirullah AbdiNo ratings yet
- The Natives Who Lost Their LivesDocument2 pagesThe Natives Who Lost Their LivesAmirullah AbdiNo ratings yet
- MeiDocument3 pagesMeiAmirullah AbdiNo ratings yet
- Analisis Semiotika Pada Cover Novel Trilogi Karya Vira SafitriDocument9 pagesAnalisis Semiotika Pada Cover Novel Trilogi Karya Vira SafitridedydoankNo ratings yet
- LLM Thesis On Human RightsDocument7 pagesLLM Thesis On Human Rightswssotgvcf100% (2)
- POMR Satiti Acute CholangitisDocument30 pagesPOMR Satiti Acute CholangitisIka AyuNo ratings yet
- Court Documents - Purdue Pharma CaseDocument236 pagesCourt Documents - Purdue Pharma CaseHung LeNo ratings yet
- Ritual and Religion Course at University of EdinburghDocument10 pagesRitual and Religion Course at University of EdinburghRenata DC MenezesNo ratings yet
- CCNA Security Instructor Lab Manual v1 - p8Document1 pageCCNA Security Instructor Lab Manual v1 - p8MeMe AmroNo ratings yet
- BIG-IP Access Policy Manager CustomizationDocument118 pagesBIG-IP Access Policy Manager CustomizationDhananjai SinghNo ratings yet
- German UnificationDocument40 pagesGerman UnificationJosephlangeloNo ratings yet
- Siemens: Building A Structure To Drive Performance and Responsibility - CaseDocument6 pagesSiemens: Building A Structure To Drive Performance and Responsibility - CaseBitopan SonowalNo ratings yet
- 40 Inventive Principles Applied to Service OperationsDocument16 pages40 Inventive Principles Applied to Service Operationssina yadegariNo ratings yet
- Lesson 1 G8Document11 pagesLesson 1 G8Malorie Dela CruzNo ratings yet
- CẤU TẠO TỪ VÀ TỪ LOẠIDocument15 pagesCẤU TẠO TỪ VÀ TỪ LOẠIccnsdNo ratings yet
- Biology 1090 Exam 1 Study GuideDocument5 pagesBiology 1090 Exam 1 Study GuideAmandaNo ratings yet
- Abstract & Concrete NounsDocument2 pagesAbstract & Concrete NounsSitifatimah92No ratings yet
- Logistic Growth Rate Functions Blumberg1968Document3 pagesLogistic Growth Rate Functions Blumberg1968Jonnathan RamirezNo ratings yet
- Analysis of A Refrigeration Cycle With Coolprop PDFDocument6 pagesAnalysis of A Refrigeration Cycle With Coolprop PDFewan_73No ratings yet
- Recommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Document2 pagesRecommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Maja MudriNo ratings yet
- Slings CatalogDocument152 pagesSlings CatalogtaNNertaroNo ratings yet
- Tulsi Ka Kavya Aur Samanvay Ki ChestaDocument6 pagesTulsi Ka Kavya Aur Samanvay Ki Chestaaman singhNo ratings yet
- Presentation On Indian Railways-03Document18 pagesPresentation On Indian Railways-03Shweta SinghNo ratings yet
- Effect of Grain Boundary Thermal Expansion on Silicon Nitride Fracture ToughnessDocument8 pagesEffect of Grain Boundary Thermal Expansion on Silicon Nitride Fracture Toughnessbrijesh kinkhabNo ratings yet
- Samantha Serpas ResumeDocument1 pageSamantha Serpas Resumeapi-247085580No ratings yet