Professional Documents
Culture Documents
Good
Uploaded by
Yudistira PratamaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Good
Uploaded by
Yudistira PratamaCopyright:
Available Formats
12 AMJ March 2018 CASE REPORT AMJ.
2018;5(1):12–5
Superior Vena Cava Syndrome and Multiple Venous Thrombosis in a
Patient with B Cell Lymphoma
Mehmet Zahid Kocak, Gulali Aktas, Edip Erkus, Burcin Atak, Tuba Duman, Haluk Savli
Abant Izzet Baysal University Hospital, Department of Internal Medicine, Bolu, Turkey
Abstract
Background: Superior vena cava syndrome (SVCS) develops due to external mechanical pressure of superior
vena cava (SVC) by a mass lesion or by an enlarged lymph node, tumor invasion of the vessel wall, or venous
thrombosis resulting in intraluminal obstruction. Approximately 3,9% of lymphomas are complicated with
SVCS. This rate reaches to 7% in diffuse large B cell lymphoma. The objective of this article was to describe
a case report of a young woman with a diffuse large B cell lymphoma, complicated with pericardial-pleural
effusion and SVCS.
Methods: A 25 year old woman referred to the Internal Medicine Clinic of Abant Izzet Baysal University
Hospital with complaints of bloating in the neck and both arms. She had chest pain, dyspnea, cough, and
epigastric discomfort for 10 days. A thoracic magnetic resonance imaging (MRI) test and pathological
assessment were carried out.
Results: A mediastinal mass 64x112x82 mm in size, displaced the heart and main mediastinal structures to
posterior, was detected by thoracic magnetic resonance imaging (MRI) test. The result of the pathological
assessment of the biopsy specimen revealed large B cell lymphoma, stained strongly and diffusely with
CD20 and bcl-2. She was referred to the hematology unit and doing well after a chemotherapy.
Conclusions: Diagnosis of SVCS requires high level of clinical suspicion, detailed and complete physical
examination. Moreover, SVCS should be kept in mind in the differential diagnosis of patients presented with
edema in the neck and upper extremities.
Keywords: Lymphoma, mediastinal mass, superior vena cava syndrome
Introduction causes may also promote superior vena cava
syndrome.5 Generally, 3.9% of lymphomas
Superior vena cava syndrome (SVCS) develops complicate with SVCS. This rate reaches to 7%
due to external mechanical pressure of in diffuse large B cell lymphoma and 21% in
superior vena cava (SVC) by a mass lesion or lymphoblastic lymphoma.6
by an enlarged lymph node, tumor invasion of This article decribed a case report of a
the vessel wall, or venous thrombosis resulting 25-year-old woman with a diffuse large B
in intraluminal obstruction.1,2 Despite cell lymphoma, complicated with pericardial-
symptomatic relief is the rule in treatment of pleural effusion and SVCS.
the patients with SVCS3, cerebral edema may
develop.4 Case
The underlying etiologic cause is
malignancy in about 60–90% of SVCS cases. A 25-year-old woman referred to the
Bronchogenic carcinoma remains the most Internal Medicine Clinic of Abant Izzet Baysal
common malignant etiology in SVCS, but University Hospital with complaints of
lymphoma and germ cell tumors follow that bloating in the neck and both arms, recently.
clinical entity.1 On the other hand, iatrogenic She also had chest pain, dyspnea, cough, and
Correspondence: Gulali Aktas M.D, Abant Izzet Baysal University Hospital, Department of Internal Medicine, Golkoy,
14280, Bolu, Turkey. Email: draliaktas@yahoo.com
ISSN 2337-4330 || doi: http://dx.doi.org/10.15850/amj.v5n1.1202 Althea Medical Journal. 2018;5(1)
Mehmet Zahid Kocak, Gulali Aktas, Edip Erkus, Burcin Atak, Tuba Duman, Haluk Savli: Superior Vena Cava 13
Syndrome and Multiple Venous Thrombosis in a Patient with B Cell Lymphoma
epigastric discomfort for 10 days. Although x-ray signed enlarged mediastinum. Besides
she had a history of cholecystectomy due bilateral pleural and pericardial effusions,
to cholelithiasis a month ago, she did not a heterogeneous malignant mass at the
complain of night sweats and 35 kg weight loss anterior mediastinum, 64x112x82 mm in
within two years. Additionally, she was not size, displaced the heart and main mediastinal
using medications regularly. The progressive structures to posterior was detected by the
dyspnea and edema in neck and arms lead to thoracic magnetic resonance imaging (MRI)
a preliminary diagnosis of SVCS. test. The mass surrounded the circumference
A physical examination revealed the of ascending aorta by 270 degrees, pulmonary
patient’s arterial blood pressure was 120/90 trunk and its branches by 180 degrees, and
mmHg, heart rate was 115 beats per minute, completely surrounded the circumferences of
body temperature was 36.9o Celsius and bilateral brachiocephalic veins and superior
respiratory rate was 20 per minute. The vena cava (figure 1). Then, a transthoracic
patient was comfortable only at sitting biopsy was performed.
position. Moreover, her face was plethoric and Additionally, aortocaval and para-aortic
the enlarged neck veins were notable along lymph nodes, of which the largest was 7.1mm
with the diffuse bulging in the neck and edema were visualized by the abdominal tomography.
in both arms. However, lymphadenopathy and No hepatomegaly or splenomegaly was noted.
splenomegaly were not detected. Based on these, Enoxaparin 60 mg twice a
Furthermore, blood test results were as day was prescribed. Dexamethasone 4mg four
follows: hemoglobin: 10.2g/dl, hematocrit: times a day was initiated due to progressive
32%, white blood cell count: 9,850/mm3, dyspnea and upper extremity edema. Dyspnea
platelet count: 412,000/mm3, erythrocyte and cough were ameliorated at the 2nd day of
sedimentation rate: 69mm/hour, lactate the treatment. While, pathological assessment
dehydrogenase: 911 U/l, uric acid: 4.8mg/ of the biopsy specimen revealed a large B cell
dl. The rest of the serum biochemistry was lymphoma, stained strongly and diffusely with
normal. Viral serology, including Ebstein-Barr CD20 and bcl-2.
virus, was negative. On the 5th day of treatment, the patient was
Furthermore, multiple lymphadenopathies doing well; her clinical signs and symptoms
of which the largest sized was 6mm and were improved. So she was referred to
sub-acute thrombi in left jugular vein were a hematology center for appropriate
detected in the neck sonography. The Doppler chemotherapy treatment.
ultrasonography of upper extremities revealed
sub-acute thrombi at the left axillary, brachial Discussions
and cephalic veins.
Moreover, a portable echocardiogram The main finding of the present report was
revealed a pericardial effusion and a chest that superior vena cava syndrome could be
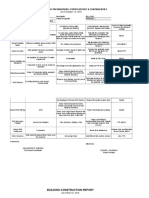
Figure 1 Mediastinal Lymphadenopathy in Magnetic Resonance Imaging
Althea Medical Journal. 2018;5(1)
14 AMJ March 2018
caused by lymphoma in young age despite the differentiated from DBBHL at the molecular
lack of palpable lymphadenopathies. Careful level by the absence of Bcl-2.11 On the other
history review, physical examination and hand, presentation with SVCS is a rare
imaging studies were needed to establish the condition in lymphomas, advanced cases may
underlying etiology in this syndrome. present this syndrome as seen in our patient.
The superior vena cava syndrome was first The SVCS treatment is largely dependent
described by William Hunter in 1757.7 It often on the underlying cause. Supportive
poses medical emergency. Approximately 60– and symptomatic treatments include
90% of SVCS cases are caused by malignancy, corticosteroids, diuretics and elevation of
which increases the incidence of thrombosis- head of the bed. However, there is no evidence-
associated SVCS due to increased venous based validation for any of these approaches
thrombosis in malignancies.1 Patients with that they are curative.2 Since lymphomas are
SVCS usually complain of cough, shortness steroid-sensitive malignancies, the steroid
of breath, voice disturbance and stridor.8,9 therapy provided symptomatic relief in the
Severity of the symptoms in SVCS is depended present case. The present patient responded
on the rate of progression, the degree of well to the standard chemotherapy for diffuse
obstruction, and the association between large B cell lymphoma.
congestion and azygos vein.1 In this case report, In conclusion, diagnosis of SVCS requires
the patient was presented with chest pain, high level of clinical suspicion, detailed and
dyspnea, cough, facial plethora and edema complete physical examination. SVCS should
in both upper extremities and in the neck. In be kept in mind in the differential diagnosis of
addition to these findings, bilateral pleural the patient whom is presented with edema in
and pericardial effusions were detected in our neck and upper extremities.
patient.
The enlarged paratracheal lymph nodes, References
lymphomas and thymomas located in the
mediastinum or anterior mediastinum caused 1. Owens Cd, Rapp JH, Gasper WJ, Johnson
SVCS via the external compression of the MD. Superior vena caval obstruction.
superior vena cava. However, bronchogenic Blood vessels and lymphatic disorders.
carcinoma has the highest association with In: Papadakis MA, McPhee SJ, editors.
SVCS development.8,9 Yu et al.10 classified Current medical diagnosis and treatment
SVCS as asymptomatic, mild, moderate, (Lange). 54th ed. San Fransisco: McGraw
serious, life-threatening, and fatal according Hill Education; 2015. p. 481–2.
to the symptoms and findings of patients 2. Shenoy S, Shetty S, Lankala S, Anwer F,
and concluded that the most common form Yeager A, Adigopula S. Cardiovascular
of SVCS is moderate SVCS (50%) and least oncologic emergencies. Cardiology.
common is fatal SVCS (<1%). According to 2017;138(3):147–58.
this classification, our phenomenon is in 3. Friedman T, Quencer KB, Kishore SA,
accordance with the moderate class SVCS. Winokur RS, Madoff DC. Malignant venous
The contrast-enhanced thoracic computed obstruction: superior vena cava syndrome
tomography is the most useful diagnostic and beyond. Semin Intervent Radiol.
method for evaluating.1 In patients with 2017;34(4):398–408 .
contrast allergy, thoracic MRI is a good 4. Talapatra K, Panda S, Goyle S, Bhadra K,
alternative with an equal sensitivity.1 Biopsy Mistry R. Superior vena cava syndrome:
is needed to confirm the underlying cause of A radiation oncologist’s perspective. J Can
SVCS in patients presented with undiagnosed Res Ther. 2016;12(2):515–9.
mass. 5. Thapa S, Terry PB, Kamdar BB.
Although the younger age of the patient Hemodialysis catheter-associated superior
along with pericardial and pleural effusions vena cava syndrome and pulmonary
and multiple sub-acute venous thrombi embolism: a case report and review of the
suggested the possibility of mediastinal large literature. BMC Res Notes. 2016;9:233.
B cell lymphoma, we detected diffuse B cell 6. Ferhanoğlu B. Diffuse Large B cell
lymphoma in our case. According to the World Lymphomas- Clinical findings and
Health Organization (WHO) classification, Treatment. 2006. [cited 2018 January 28].
MBBHL (mature large B cell lymphoma) is Available from: http://www.thd.org.tr/
classified under the title of diffuse large B-cell thdData/userfiles/file/diffuz_buyuk_b.
lymphoma (DBBHL) and the average age of pdf.)
onset is between 35-40 years. The MBBHL is 7. Stajnic M, Canji T, Panić G, Tomić N, Jelkić
Althea Medical Journal. 2018;5(1)
Mehmet Zahid Kocak, Gulali Aktas, Edip Erkus, Burcin Atak, Tuba Duman, Haluk Savli: Superior Vena Cava 15
Syndrome and Multiple Venous Thrombosis in a Patient with B Cell Lymphoma
N, Kovacević B. The superior vena cava 10. Yu JB, Wilson LD, Detterbeck FC. Superior
syndrome as a manifestation of dissection vena cava syndrome—a proposed
of the ascending aorta. Med Pregl. classification system and algorithm
2001;54(7–8):380–2. for management. J Thorac Oncol.
8. Lepper PM, Ott SR, Hoppe H, Schumann 2008;3(8):811–4.
C, Stammberger U, Bugalho A, et 11. Arlindo EM, Marcondes NA, Fernandes
al. Superior vena cava syndrome in FB, Faulhaber GAM. Quantitative flow
thoracic malignancies. Respir Care. cytometric evaluation of CD200, CD123,
2011;56(5):653–66. CD43 and CD52 as a tool for the differential
9. Wan JF, Bezjak A. Superior vena cava diagnosis of mature B-cell neoplasms. Rev
syndrome. Emerg Med Clin North Am. Bras Hematol Hemoter. 2017;39(3):252–8.
2009;27(2):243–55.
Althea Medical Journal. 2018;5(1)
You might also like
- Superior Vena Cava Syndrome: GroundbreakersDocument6 pagesSuperior Vena Cava Syndrome: GroundbreakersJuli IsmailNo ratings yet
- Proceedings From The 2010 Annual Meeting of The American College of Physicians, Wisconsin ChapterDocument15 pagesProceedings From The 2010 Annual Meeting of The American College of Physicians, Wisconsin ChapterHarold FernandezNo ratings yet
- Superior Vena Cava Syndrome Case ReportDocument8 pagesSuperior Vena Cava Syndrome Case ReportBenjamin VegaNo ratings yet
- Superior Vena Cava Syndrome Causes and TreatmentDocument13 pagesSuperior Vena Cava Syndrome Causes and TreatmentFuji Seprinur HidayatNo ratings yet
- Reversible Cerebral Vasoconstriction Syndrome Following Blood Transfusion in The Setting of Possible Rheumatoid-Associated Vasculitis: A Case Report and Review of LiteratureDocument4 pagesReversible Cerebral Vasoconstriction Syndrome Following Blood Transfusion in The Setting of Possible Rheumatoid-Associated Vasculitis: A Case Report and Review of LiteratureasclepiuspdfsNo ratings yet
- Recurrent Ischaemic Stroke Unveils Polycythaemia Vera - BMJ Case ReportsDocument9 pagesRecurrent Ischaemic Stroke Unveils Polycythaemia Vera - BMJ Case ReportsancillaagraynNo ratings yet
- AML Case Study AnalysisDocument14 pagesAML Case Study AnalysisIssaiah Nicolle CeciliaNo ratings yet
- TMP 69 E9Document7 pagesTMP 69 E9FrontiersNo ratings yet
- 2020 case report DLBCL CD56Document9 pages2020 case report DLBCL CD56maomaochongNo ratings yet
- Large Vessel Occlusion Secondary To COVID-19 Hypercoagulability in A Young Patient: A Case Report and Literature ReviewDocument6 pagesLarge Vessel Occlusion Secondary To COVID-19 Hypercoagulability in A Young Patient: A Case Report and Literature Reviewdevi ramadiantiNo ratings yet
- Vachani Oncolink SVCSDocument2 pagesVachani Oncolink SVCSarmitadewiNo ratings yet
- Exacerbation of Antiphospholipid Antibody Syndrome After Treatment of Localized Cancer-A Report of Two CasesDocument5 pagesExacerbation of Antiphospholipid Antibody Syndrome After Treatment of Localized Cancer-A Report of Two Casesloshaana105No ratings yet
- TMP 155 BDocument7 pagesTMP 155 BFrontiersNo ratings yet
- YessDocument5 pagesYessalingh98No ratings yet
- Chronic Myeloid Leukemia Presenting With Priapism 2329 6917 1000171Document5 pagesChronic Myeloid Leukemia Presenting With Priapism 2329 6917 1000171SalwiyadiNo ratings yet
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseFrom EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseNo ratings yet
- Oncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdyDocument14 pagesOncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdySandra PargaNo ratings yet
- Pulmonary Embolism - European Heart Journal 2012Document12 pagesPulmonary Embolism - European Heart Journal 2012Andreas IoannouNo ratings yet
- 2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CDocument4 pages2014 Kabir Et Al. - Chronic Eosinophilic Leukaemia Presenting With A CPratyay HasanNo ratings yet
- Q2 GPA Diseases of WBCs Lymph Nodes Spleen and ThymusDocument7 pagesQ2 GPA Diseases of WBCs Lymph Nodes Spleen and ThymusAdrian CaballesNo ratings yet
- Non Hodgkin Lymphoma NasofaringDocument4 pagesNon Hodgkin Lymphoma Nasofaringsuci triana putriNo ratings yet
- Subclavian Thrombosis in A Patient With Advanced Lung Cancer: A Case ReportDocument5 pagesSubclavian Thrombosis in A Patient With Advanced Lung Cancer: A Case Reportah1976No ratings yet
- Management of Chronic Venous Disease: 7th Annual Women's Heart & Vascular SymposiumDocument3 pagesManagement of Chronic Venous Disease: 7th Annual Women's Heart & Vascular Symposiumatika5No ratings yet
- Med Oncology MCQDocument109 pagesMed Oncology MCQdrzika100% (8)
- WBC Usmle QuestionsDocument17 pagesWBC Usmle Questionssplinter594100% (1)
- Oncologic Mechanical Emergencies 2014 Emergency Medicine Clinics of North AmericaDocument14 pagesOncologic Mechanical Emergencies 2014 Emergency Medicine Clinics of North AmericamarcosjuniormutucaNo ratings yet
- Priapism - A Rare Presentation in Chronic Myeloid Leukemia: Case Report and Review of The LiteratureDocument5 pagesPriapism - A Rare Presentation in Chronic Myeloid Leukemia: Case Report and Review of The LiteratureSalwiyadiNo ratings yet
- Infective EndocarditisDocument5 pagesInfective Endocarditismustafa malvi100% (1)
- Early - Stage Hodgkins Lymphoma in A Child A CaseDocument6 pagesEarly - Stage Hodgkins Lymphoma in A Child A CaseХарш Навнітбхаі НімаватNo ratings yet
- Lymphoma Involving The Heart: A Case ReportDocument5 pagesLymphoma Involving The Heart: A Case ReportRanda TabbahNo ratings yet
- NCM 112 OR Notes CaseDocument6 pagesNCM 112 OR Notes CaseSureen RegularNo ratings yet
- A Case Report On Sickle Cell Disease With Hemolyti PDFDocument4 pagesA Case Report On Sickle Cell Disease With Hemolyti PDFAlhaji SwarrayNo ratings yet
- Insuficiencia Por EndocarditisDocument4 pagesInsuficiencia Por EndocarditisKatherin TorresNo ratings yet
- Chronic Venous InsufficiencyDocument29 pagesChronic Venous InsufficiencyariNo ratings yet
- Acute Lower Limb Ischemia As The Initial Symptom of Acute Myeloid LeukemiaDocument4 pagesAcute Lower Limb Ischemia As The Initial Symptom of Acute Myeloid LeukemiaekanovicaNo ratings yet
- Oncologic EmergenciesDocument163 pagesOncologic EmergenciesGeorge BoaduNo ratings yet
- Krok2 - Medicine - 2016Document25 pagesKrok2 - Medicine - 2016ashighaNo ratings yet
- Superior Vena Cava Syndrome Due To Right Anterior Mediastinal Hematoma: A Case ReportDocument3 pagesSuperior Vena Cava Syndrome Due To Right Anterior Mediastinal Hematoma: A Case ReportDr. Usman HashmiNo ratings yet
- JCM 11 06258Document13 pagesJCM 11 06258deja234No ratings yet
- Sepsis Parte 2Document12 pagesSepsis Parte 2Maria AlejandraNo ratings yet
- Clinical Examination: A Trigger But Not A Substitute For Hemodynamic EvaluationDocument3 pagesClinical Examination: A Trigger But Not A Substitute For Hemodynamic EvaluationGdfgdFdfdfNo ratings yet
- Superior Vena Cava Syndrome Secondary To Adult T-Cell Lymphoblastic LymphomaDocument3 pagesSuperior Vena Cava Syndrome Secondary To Adult T-Cell Lymphoblastic LymphomaIJAR JOURNALNo ratings yet
- Cric2018 7237454Document4 pagesCric2018 7237454Muhammad Nur Ardhi LahabuNo ratings yet
- Pancytopenia Secondary To Bacterial SepsisDocument16 pagesPancytopenia Secondary To Bacterial Sepsisiamralph89No ratings yet
- 2021 Large-Vessel Vasculitis NatureDocument23 pages2021 Large-Vessel Vasculitis NatureRooyNo ratings yet
- How I Treat and Manage Strokes in Sickle Cell DiseaseDocument10 pagesHow I Treat and Manage Strokes in Sickle Cell DiseaseNinaNo ratings yet
- Wudel-Nesbitt2001 Article SuperiorVenaCavaSyndromeDocument15 pagesWudel-Nesbitt2001 Article SuperiorVenaCavaSyndromeFernandoNo ratings yet
- Varicocele A ReviewDocument5 pagesVaricocele A ReviewLiaApprilia Kartinii Cupcupcuap ElvenadoNo ratings yet
- VASCULITIS by Dr. AJ. 1Document34 pagesVASCULITIS by Dr. AJ. 1Abira KhanNo ratings yet
- 080508-148 Syphilitc Aneurys Case Report PDFDocument4 pages080508-148 Syphilitc Aneurys Case Report PDFCarol SantosNo ratings yet
- Spontaneous Intracerebral HaemorrhageDocument3 pagesSpontaneous Intracerebral Haemorrhageselvie87No ratings yet
- Catheter-Directed Thrombolysis of Iliocaval Thrombosis in Patients With COVID-19Document13 pagesCatheter-Directed Thrombolysis of Iliocaval Thrombosis in Patients With COVID-19oscarNo ratings yet
- Case 17378: Unicentric Intra-Abdominal Castleman's Disease Mimicking MalignancyDocument8 pagesCase 17378: Unicentric Intra-Abdominal Castleman's Disease Mimicking MalignancyPedro Luis Almeyda RamírezNo ratings yet
- MCQ 5Document85 pagesMCQ 5Kailash KhatriNo ratings yet
- Patho SGD: Cardiovascular Module Case 1Document4 pagesPatho SGD: Cardiovascular Module Case 1carmina_guerreroNo ratings yet
- Saddle Pulmonary Embolism: A Rare Case of Proximal Pulmonary EmbolismDocument3 pagesSaddle Pulmonary Embolism: A Rare Case of Proximal Pulmonary EmbolismIJAR JOURNALNo ratings yet
- Simon 2016Document12 pagesSimon 2016yoNo ratings yet
- Acute Presentation of Third Ventricular Cavernous Malformation - Saberi2021Document4 pagesAcute Presentation of Third Ventricular Cavernous Malformation - Saberi2021Bruno Diaz LlanesNo ratings yet
- Ijvm2014 531689 PDFDocument6 pagesIjvm2014 531689 PDFReka HariskianaNo ratings yet
- Splenectomy - A Therapeutic Option in Splenic Marginal Zone Cell LymphomaDocument11 pagesSplenectomy - A Therapeutic Option in Splenic Marginal Zone Cell LymphomaFlorin IliescuNo ratings yet
- Jadwal Vaksinasi Gratis LEbakDocument9 pagesJadwal Vaksinasi Gratis LEbakYudistira PratamaNo ratings yet
- Isolation Guidelines HealthDocument204 pagesIsolation Guidelines HealthGrace Datu100% (1)
- DokumenDocument1 pageDokumenYudistira PratamaNo ratings yet
- GoodDocument4 pagesGoodYudistira PratamaNo ratings yet
- BAB II Penting Makalah PersenticionDocument6 pagesBAB II Penting Makalah PersenticionYudistira PratamaNo ratings yet
- Proposed Panel Antenna: Globe Telecom ProprietaryDocument2 pagesProposed Panel Antenna: Globe Telecom ProprietaryJason QuibanNo ratings yet
- Project Report Software and Web Development Company: WWW - Dparksolutions.inDocument12 pagesProject Report Software and Web Development Company: WWW - Dparksolutions.inRavi Kiran Rajbhure100% (1)
- Time Table Semester II 2019-2020Document18 pagesTime Table Semester II 2019-2020Shiv Kumar MeenaNo ratings yet
- Useful Relations in Quantum Field TheoryDocument30 pagesUseful Relations in Quantum Field TheoryDanielGutierrez100% (1)
- GastrectomyDocument19 pagesGastrectomyCyrus GarciaNo ratings yet
- Sample QuestionsDocument70 pagesSample QuestionsBushra MaryamNo ratings yet
- How Do I Prepare For Public Administration For IAS by Myself Without Any Coaching? Which Books Should I Follow?Document3 pagesHow Do I Prepare For Public Administration For IAS by Myself Without Any Coaching? Which Books Should I Follow?saiviswanath0990100% (1)
- AIOUDocument2 pagesAIOUHoorabwaseemNo ratings yet
- Class Opening Preparations Status ReportDocument3 pagesClass Opening Preparations Status ReportMaria Theresa Buscato86% (7)
- Request For Proposal Construction & Phase 1 OperationDocument116 pagesRequest For Proposal Construction & Phase 1 Operationsobhi100% (2)
- Body Shaming Among School Going AdolesceDocument5 pagesBody Shaming Among School Going AdolesceClara Widya Mulya MNo ratings yet
- OMR Sheet Has Been Attached at The End: EST Erial ODocument8 pagesOMR Sheet Has Been Attached at The End: EST Erial OSangeeta BansalNo ratings yet
- 2nd QUARTER EXAMINATION IN P. E 2019-2020Document3 pages2nd QUARTER EXAMINATION IN P. E 2019-2020Lyzl Mahinay Ejercito MontealtoNo ratings yet
- WEEK 8. - Gen Math-PortfolioDocument12 pagesWEEK 8. - Gen Math-PortfolioOreo ProductionsNo ratings yet
- Eportfile 4Document6 pagesEportfile 4api-353164003No ratings yet
- CURRICULUM AUDIT: GRADE 7 MATHEMATICSDocument5 pagesCURRICULUM AUDIT: GRADE 7 MATHEMATICSjohnalcuinNo ratings yet
- Daily Assessment RecordDocument4 pagesDaily Assessment Recordapi-342236522100% (2)
- A Summer Internship Project ON " To Study The Supply Chain Management On Amul Fresh Products" AT GCMMF, AmulDocument19 pagesA Summer Internship Project ON " To Study The Supply Chain Management On Amul Fresh Products" AT GCMMF, AmulweetrydhNo ratings yet
- 3 - Content - Introduction To Java, JVM, JDK PDFDocument8 pages3 - Content - Introduction To Java, JVM, JDK PDFAnonymous zdY202lgZYNo ratings yet
- Fjords Blue Web ENG PDFDocument20 pagesFjords Blue Web ENG PDFMoldovan MirceaNo ratings yet
- Lineapelle: Leather & Non-LeatherDocument16 pagesLineapelle: Leather & Non-LeatherShikha BhartiNo ratings yet
- Guitar Chords:: Chorus: CF CF FCFC CFGC Verse: CF CF FCFC CFGCDocument17 pagesGuitar Chords:: Chorus: CF CF FCFC CFGC Verse: CF CF FCFC CFGCKhuanZumeNo ratings yet
- City MSJDocument50 pagesCity MSJHilary LedwellNo ratings yet
- GRP Product CatalogueDocument57 pagesGRP Product CatalogueMulyana alcNo ratings yet
- Business StrategiesDocument2 pagesBusiness Strategiesthristanlexter694No ratings yet
- Simulia Abaqus Standard DatasheetDocument3 pagesSimulia Abaqus Standard Datasheetuser923019231831No ratings yet
- INVENTORY MANAGEMENT TechniquesDocument24 pagesINVENTORY MANAGEMENT TechniquesWessal100% (1)
- AnhvancDocument108 pagesAnhvancvanchienha7766No ratings yet
- ElectricalDocument30 pagesElectricalketerNo ratings yet
- ChromosomesDocument24 pagesChromosomesapi-249102379No ratings yet