Professional Documents
Culture Documents
Iron Deficiency Anaemia
Iron Deficiency Anaemia
Uploaded by
Riki KeiyaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Iron Deficiency Anaemia
Iron Deficiency Anaemia
Uploaded by
Riki KeiyaCopyright:
Available Formats
Iron Deficiency Anaemia in Pregnancy:
Developed Versus Developing Countries
Authors: *Avantika Gupta, Avanthi Gadipudi
Department of Obstetrics and Gynaecology, Jawaharlal Institute of Postgraduate
Medical Education and Research, Pondicherry, India
*Correspondence to dravantikagupta@gmail.com
Disclosure: The authors have declared no conflicts of interest.
Received: 15.02.18
Accepted: 13.06.18
Keywords: Anaemia, blood transfusion, intravenous iron, iron deficiency, iron
supplementation, pregnancy.
Citation: EMJ Hematol. 2018;6[1]:101-109.
Abstract
Anaemia is the most widespread of the haematological disorders, affecting about one-third of the
global population. Despite decades of public health interventions, anaemia in pregnancy remains a
major health problem worldwide, with an estimated 41.8% of pregnant women being diagnosed with
anaemia at some point in their gestation. At least half of the cases of anaemia in pregnant women
are assumed to be due to iron deficiency, with folate or vitamin B12 deficiency, chronic inflammatory
disorders, parasitic infections like malaria, and certain inherited disorders accounting for the
remaining cases. A considerable variation has been observed in the incidence and aetiology of
iron deficiency anaemia among developed and developing nations, warranting differences in
the screening protocols and management strategies used by clinicians in these countries.
This article highlights the differences in the management of iron deficiency anaemia among low
and high-income countries, with a detailed review of the policies followed in India.
DEFINING ANAEMIA IN PREGNANCY lower Hb and haematocrit levels among
black adults, the Institute of Medicine (IOM)
The definition of iron deficiency anaemia recommends lowering the Hb cut-off level
by 0.8 g/dL in this population.3 The British
(IDA) in pregnancy is imprecise as a result of
Committee for Standards in Haematology
pregnancy-induced changes in plasma volume
(BCSH)4 defines anaemia as a Hb value <2
and haematocrit, differences in haemoglobin (Hb)
standard deviations below the mean value for
concentration through the trimesters, differences
a healthy matched population, which amounts
in diagnostic tests, and ethnic variation. According
to Hb levels <11.0 g/dL in the first trimester,
to the World Health Organization (WHO), a
<10.5 g/dL in the second to third trimesters,
pregnant woman is considered to be anaemic if
and <10.0 g/dL in the postpartum period.
her Hb concentration is <11 g/dL,1 whereas Centers
for Disease Control and Prevention (CDC) Around three-quarters of anaemia-related
guidelines define anaemia as Hb <11 g/dL in the maternal mortality cases in south Asia occur in
first trimester and <10 g/dL in the second or India, and hence the Indian Council of Medical
third trimester.2 Based on the finding of typically Research (ICMR) further classifies anaemia
Creative Commons Attribution-Non Commercial 4.0 August 2018 • HEMATOLOGY 101
in pregnancy according to grades of severity INCIDENCE OF IRON DEFICIENCY
to aid in the triage of women requiring
ANAEMIA IN DEVELOPED VERSUS
early intervention:5 mild anaemia with Hb of
10.0–10.9 g/dL,moderate anaemia with Hb DEVELOPING COUNTRIES
of 9.9–7.0 g/dL, severe anaemia with Hb of
6.9–4.0 g/dL, and very severe anaemia with Hb IDA remains the most common nutritional
of <4.0 g/dL. deficiency globally, with about 32 million
pregnant women categorised as anaemic and
about 0.75 million pregnant women categorised
PATHOPHYSIOLOGY OF IRON as severely anaemic.8
DEFICIENCY ANAEMIA IN PREGNANCY
An analysis of National Health and Nutrition
Physiological or dilutional anaemia of pregnancy Examination Survey (NHANES) epidemiological
is observed in healthy pregnant women as a data from the USA from 1999–2006
result of a relatively greater expansion of demonstrated an overall prevalence of IDA
plasma volume by 30–40% in comparison to a of nearly 18.0%. Iron deficiency was shown to
20–25% raise in Hb mass and erythrocyte increase from 6.9% to 14.3% to 28.4% across
volume. This results in a modest decrease in the three trimesters during pregnancy.9
Hb levels, creating a low viscosity state, which A multicentre cross-sectional study in the UK
promotes oxygen transport to the placenta estimated a 24.4% prevalence of maternal
and fetus. Pregnancy significantly increases the anaemia at some stage of the antenatal period.10
demand for iron to balance the physiological A systematic analysis of population-
requirements of increased haematocrit, representative data of Hb concentration and
developing the fetoplacental unit, and for the prevalence of total and severe anaemia for
losses during delivery and lactation. The 1995–2011 reported the prevalence of anaemia in
Institute of Medicine (IOM) estimated that the pregnancy as 14.0% in high-income regions and
total iron loss associated with pregnancy and 23.0% in central and eastern Europe.11 In contrast
lactation is approximately 1,000 mg and has to these developed countries, about 53.0% of
recommended a daily dietary allowance for pregnant women in south Asia were diagnosed
iron in pregnancy of 27 mg instead of the 8 mg with anaemia, of whom 3.8% were found to
required for the nonpregnant adult population.6 be severely anaemic. Iron-amenable anaemia
If this recommended daily allowance of iron in represented >70.0% of these cases.11 Insufficient
pregnancy is not met, it results in women with quantity of iron-rich foods, poor environmental
depleted iron stores developing IDA. sanitation, unsafe drinking water, iron loss
due to parasite load (e.g., malaria or intestinal
Recent research into iron metabolism in humans
worms), and adolescent anaemia, along with
has paved the way for the discovery of a novel
teenage pregnancies and repeated pregnancies
peptide hormone, hepcidin, that acts as a
in low resource countries, are the predominant
homeostatic regulator of systemic iron
causes for the disproportionately increased
concentration by controlling iron efflux into the
prevalence of IDA in pregnancy in these nations.
plasma. Hepcidin levels in pregnant women are,
in general, lower than in nonpregnant healthy India is one of the countries with the highest
women, and decrease as pregnancy advances, prevalence of anaemia in the world. According
with the lowest levels of hepcidin observed in to the Indian National Family Health Survey, the
the third trimester.7 With decreasing expression prevalence of IDA in pregnancy ranges from
of hepcidin, there is an increased absorption of 23.6–61.4%.12 The incidence of IDA in India was
dietary iron and increased mobilisation of iron estimated at 60.0% in the urban population and
from body stores modulated by ferroportin. 69.0% in the rural population, and IDA resulted
Inflammatory states, including pre-eclampsia, in approximately 326,000 maternal deaths with
malaria infection, and obesity, have been an associated disability-adjusted life years of
associated with higher hepcidin during pregnancy 12,497,000.13 Diverse cultures, religions, food
compared to healthy controls, suggesting that habits, lifestyles, and traditions pose a challenge
maternal and fetal iron bioavailability could be to the implementation of various government
compromised in these conditions. health programmes in India.
102 HEMATOLOGY • August 2018 EMJ EUROPEAN MEDICAL JOURNAL
The situation is no different in other Asian Haider et al.18 demonstrated a dose–response
countries, like Pakistan, where in 2008 the relationship between increasing doses of iron
prevalence of anaemia among pregnant women supplements and reduction in the incidence of
was estimated at 90.5%; of these women, 75.0% low birth weight babies.
had mild anaemia and 14.8% had moderate
anaemia.14 In the year 2000, a community-based
SCREENING IN DEVELOPED
sample of 336 pregnant women in the plains
of Nepal showed that 72.6% of pregnant women
COUNTRIES VERSUS
were anaemic and 88.0% of cases of anaemia DEVELOPING COUNTRIES
were associated with iron deficiency.15
Strategies for anaemia screening may include
a routine screening of all expectant mothers or
MATERNAL AND FETAL
targeted screening based on established risk
EFFECTS OF IRON-DEPENDENT factors, diagnostic tests, or risk assessment
ANAEMIA IN PREGNANCY instruments. Though the need for antenatal
screening is well established, countries differ
The existing literature shows that failure to meet from one another in their screening policies
the increased iron requirements in pregnancy and criteria.
may result in adverse maternal and fetal
consequences. This is also supported by a The U.S. Department of Veterans Affairs/
comparative quantification of health risks by Department of Defence (VA/DoD) and
the WHO, which estimated that about 591,000 CDC2 recommend that all pregnant women
perinatal deaths and 115,000 maternal deaths should be screened for anaemia at some
worldwide can be attributed to IDA, either point during pregnancy, irrespective of their
directly or indirectly.16 Furthermore, it was risk stratification. The VA/DoD recommends
shown that correcting IDA of any severity screening during the first antenatal visit and is
reduces the risk of maternal death by about against routine repeat screening in asymptomatic
20% for each 1 g/dL increase in Hb. In light pregnant women.19 In comparison, the American
of these findings, newer health policies need College of Obstetricians and Gynaecologists
to focus on mild-to-moderate anaemia in (ACOG) recommends routine screening of all
pregnancy, in addition to severe anaemia, for a pregnant women for anaemia and implementing
greater public health impact. iron therapy if IDA is confirmed.20
Iron deficiency in pregnancy causes maternal Australian guidelines recommend the screening
morbidity with increased risk of abortion, of all pregnant women for anaemia at the
increased susceptibility to infection due to time of booking and at 28 weeks.21,22 If the
defective macrophage phagocytosis and pregnant woman is at risk of thalassaemia or
lymphocyte replication, physical weakness, haemoglobinopathy, she will require additional
pre-eclampsia, preterm labour, heart failure, investigations, such as Hb variant analysis and
increased risk of postpartum haemorrhage due iron studies.
to impaired myometrial contractility resulting
from hypoxia-induced enzymatic and cellular The IOM recommends that screening for
dysfunction, puerperal sepsis, and postnatal anaemia should be reserved for high-risk
depression. According to a study by Lone et al.,17 pregnant women only, who need to be followed
anaemia in pregnancy increases the risk up during each trimester and at 4–6 weeks
of preterm birth 4.0-fold, low birth weight postpartum.3 The U.S. Preventive Services Task
babies 2.2-fold, and low Apgar score in Force concluded that the current evidence is
newborn babies 1.8-fold in comparison to inadequate to assess the balance of benefits
nonanaemic women. Maternal iron depletion and harms of screening for IDA in pregnant
also reduces fetal iron stores and increases women to prevent adverse maternal and fetal
the risk of neonatal anaemia and perinatal outcomes. It also stated that although there is
morbidity. Correction of iron deficiency has insufficient evidence to prove the superiority of
proved to have beneficial effects on both the any screening tool, measurement of serum Hb
mother and the fetus. A meta-analysis by or haematocrit levels may often be considered
Creative Commons Attribution-Non Commercial 4.0 August 2018 • HEMATOLOGY 103
as the first step used in primary care practice. differentiating IDA from thalassaemia and
The Canadian Task Force on Preventive Health other haemoglobinopathies. The sensitivity and
Care, on the other hand, does not have a specificity, respectively, of red cell distribution
current recommendation for this topic.23,24 width in the diagnosis of IDA in pregnancy were
reported by Sultana et al.26 as 97.4% and 83.2%
With >80% of antenatal women diagnosed
and by Tiwari et al.27 as 72.8% and 82.4%.
with IDA, routine screening of all pregnant
women is standard practice in India. Indian Serum Ferritin
National Rural Health Mission (NRHM) guidelines
recommend a compulsory Hb estimation for all Measurement of serum ferritin accurately
pregnant women by the cyanmethaemoglobin reflects iron stores and is commonly the first
method or by photocalorimeter at 14–16 weeks, laboratory test to become abnormal as iron
followed by at 20–24 weeks, 26–30 weeks, stores decrease. Serum ferritin values are
and 30–34 weeks of pregnancy (a minimum of not affected by recent iron ingestion and
four Hb estimations). The interval between are generally considered the best parameter
the Hb estimations should be a minimum of to assess deficient iron stores in pregnancy.
4 weeks. The trigger point for referral to a more A concentration <15 μg/L indicates iron depletion
specialised institution would be a Hb level of in all stages of pregnancy. Assessment of
≤7 g/dL at 14 weeks, 20–24 weeks, and 26–30 serum ferritin in pregnancy takes precedence
weeks, or a Hb level of ≤9 g/dL at 30–34 weeks.25 over other investigations in women with
suspected thalassaemia or haemoglobinopathy,
in women whose anaemia fails to respond
WORK-UP to a 2-week trial of oral iron, in women
with multifactorial anaemia, and before any
Clinical Symptoms and Signs parenteral iron replacement.
Symptoms and signs of IDA in pregnancy
Serum Iron, Total Iron Binding
are usually nonspecific and mimic normal
pregnancy changes, unless the anaemia is severe.
Capacity, and Transferrin Saturation
Fatigue is the most common symptom, Serum iron is an unreliable indicator of the iron
followed by varying degrees of pallor, lassitude, available at the tissue level because of wide
headache, palpitations, dizziness, dyspnoea, lack fluctuations in serum iron levels with recent
of concentration, and irritability. Pica develops ingestion of iron, infection, and diurnal rhythm.
in rare cases. Total iron binding capacity is increased with
iron deficiency and is an indirect measure
Full Blood Count, Blood Film, of obtainability of iron-binding sites and
and Red Cell Indices transferrin levels.
A complete blood count is usually the primary
Zinc Protoporphyrin
step in the diagnosis of IDA. It is simple, rapid
to perform, inexpensive, and helpful in the early Zinc protoporphyrin levels increase when iron
prediction of IDA. A full blood count provides availability decreases as zinc is incorporated
a complete blood picture, showing low Hb, into the protoporphyrin ring instead of iron.
mean cell Hb (MCH), mean cell volume (MCV), Serum zinc protoporphyrin has the advantage
and mean cell Hb concentration (MCHC); of not being influenced by the plasma dilution
a peripheral smear with presence of microcytic and hence has greater sensitivity and specificity
hypochromic red cells and characteristic ‘pencil for iron depletion; however, this test is rarely
cells’ or anisopoikilocytosis characterises IDA. performed because it is not readily available.
Red Cell Distribution Width Bone Marrow Iron
Increased red cell distribution width A bone marrow sample stained for iron with
implies variance in the red blood cell (RBC) Prussian blue has been considered the gold
volume distribution, similar to a peripheral standard for assessment of marrow iron stores.
blood smear anisocytosis, and helps in However, the invasive nature of this test restricts
104 HEMATOLOGY • August 2018 EMJ EUROPEAN MEDICAL JOURNAL
its use to the most complicated cases, in which Supplementation and Prophylaxis
the underlying cause of anaemia cannot be
identified by simpler means. All antenatal women must be given advice for
dietary modification to improve iron content
A Trial of Iron Therapy and its absorption. Iron-rich food items include
meat from cattle, fish, and poultry, and legumes
A trial of iron therapy has simultaneous and green leafy vegetables. The recommended
diagnostic and therapeutic applications in dietary intake of iron in the second half of
IDA. Microcytic hypochromic anaemia can pregnancy is 30 mg. Absorption of iron
be assumed to be due to iron deficiency increases 3-fold by the third trimester and
until proven otherwise. A rise in Hb level, the requirement increases from 1–2 mg to 6 mg
if demonstrable by 2 weeks, confirms iron per day.30 This increase cannot be taken care of
deficiency and is both cost and time-effective. by dietary modification alone and hence results
If the patient is at high risk of in anaemia during pregnancy in many women.
haemoglobinopathy and the status is unknown, The WHO strongly recommends daily oral iron
they can be evaluated with ferritin and iron and folic acid supplementation as a part of
therapy can be started while screening is being antenatal care to reduce the risk of low birth
performed. If there has been no improvement weight babies, maternal anaemia, and iron
in Hb by 2 weeks, referral should be made deficiency. The International Nutritional Anemia
to more specialised centres to consider other Consultative Group (INACG), as well as the
causes of anaemia. WHO, recommends that 60 mg elemental iron
has to be given as prophylaxis to all antenatal
WHO and CDC technical guidance is that, in the
women in countries where the prevalence of
absence of infection, measuring serum ferritin
anaemia is >40%.1
or serum transferrin receptor in association
with Hb provides the best assessment of iron In the UK and Australia, routine administration
status in the general population.28 However, of iron supplementation to all pregnant women
in low-resource settings like India, the majority is not recommended. However, in India, where
of these tests are either not easily affordable prevalence is as high as 58%, the Ministry
or not available. Therefore, the RBC indices hold of Health and Family Welfare (MOHFW)
great value for primary diagnosis, which can recommends iron supplementation in the form
reduce unnecessary investigative costs. Of all of 100 mg elemental iron for 100 days along
the available indices, the Meltzer index with 500 μg of folic acid starting from
(MCV:RBC ratio) has been shown to be the most 14–16 weeks. However, the problem with
reliable indicator with the highest sensitivity.29 100 mg elemental iron compared to 60 mg
is increased incidence of gastrointestinal side
According to Indian National Rural Health effects like nausea, vomiting, and constipation.
Mission guidelines,25 management of IDA in For nonanaemic patients with iron deficiency,
pregnancy includes: the dose can be as low as 20–60 mg.
>> Hb estimation by cyanmethemoglobin method According to a recent Cochrane review,31 iron
using a semiautoanalyser or photocalorimeter, supplementation reduces the risk of anaemia
which is mandatory in all institutions. in full-term mothers by 70% and the risk of
>> Peripheral smear, MCV:RBC ratio, serum iron iron deficiency by 57%. However, there was no
binding capacity, and Hb electrophoresis significant effect on preterm birth and neonatal
performed in medical colleges, District death. The fetus is relatively protected from
Headquarter hospitals, and other secondary the effects of iron deficiency by upregulation of
care institutions with facilities for these tests. placental iron transport proteins.31 To improve
>> Urine assessment for albumin, sugar, and acceptability of adherence to supplementation,
deposits, and a urine culture if pus cells are a behavioural change communication strategy
detected, to rule out refractory anaemia. should be implemented to communicate the
benefits of oral iron supplementation. This is
consolidated by the provision of an information
leaflet in the patient’s language in the UK.
Creative Commons Attribution-Non Commercial 4.0 August 2018 • HEMATOLOGY 105
Table 1: Elemental iron content and dose per tablet of oral iron preparations.
Iron salt Dose per tablet Elemental iron
Ferrous sulphate 300 mg 60 mg
Ferrous sulphate (dried) 200 mg 65 mg
Ferrous fumarate 322 mg 100 mg
Ferrous gluconate 300 mg 35 mg
Ferrous succinate 100 mg 35 mg
In India, nutrition counselling is provided at TREATMENT
antenatal check-ups during the monthly village
health and nutrition day. Accredited social health National Institute for Health and Care Excellence
workers are given incentives for providing (NICE), British Society of Haematology (BSH),
iron folic acid supplements to patients at and Australian Guidelines all recommend a trial
their doorstep. of oral iron for 2 weeks in women diagnosed
with anaemia during the antenatal period.4
The available ferrous salts include ferrous
This treatment can be started at the
fumarate, ferrous sulphate, ferrous gluconate,
community level and an adequate rise in Hb
and succinate. The amount of elemental iron
is considered to be diagnostic of IDA.21,22,34
varies in each salt and hence the number of
If the haemoglobinopathy state is unknown,
tablets to be taken daily varies; for instance, iron therapy should be started and a
if a woman takes ferrous gluconate she needs haemoglobinopathy screen should be organised
to take two tablets per day, as compared to simultaneously. Duration of therapy should be
ferrous sulphate or ferrous fumarate (one tablet the time until the patient’s Hb rises to normal
per day), as shown in Table 1. and then a further 3 months or until 6 weeks
postpartum in order to replenish stores. If Hb is
Oral iron supplementation should be taken on an
<10 g/dL in the postpartum period, 100–200 mg
empty stomach along with vitamin C-containing
elemental iron should be given for a further
food items and women should be informed not
3 months. Nonanaemic iron-deficient women
to have tea, coffee, or antacids when taking should be given 65 mg elemental iron and Hb
iron tablets. test should be repeated after 8 weeks.
Supplementation with oral iron is continued for Supplementation compliance has to be ensured
3 months, and a therapeutic dose of iron in patients. For example, women should be
is started if the anaemia is not corrected. asked about the colour of their stools, which
In populations with endemic hookworm should be black while on oral iron treatment,
(a prevalence of ≥20–30%), antihelminthic or they can be asked to return the empty
therapy should be given to any patient with supplement packaging. Gastrointestinal side
severe anaemia because treatment is safer effects can be as high as 40% with oral iron
and cheaper than diagnosing a hookworm therapy, and include nausea and vomiting,
infection. After the first trimester, mebendazole constipation, and diarrhoea. Particularly if the
or albendazole can be safety administered to mother is near term, the indications of referral
pregnant women. In India, all pregnant women to secondary care in the UK are:
are given one tablet of 400 mg albendazole
>> No rise in Hb during 2 weeks of treatment.
at 14–16 weeks. In malaria endemic areas,
>> Hb <7 g/dL.
provision of iron folic acid supplementation
should be implemented in addition to measures >> Symptoms of iron supplementation.
for prevention, diagnosis, and treatment >> >34 weeks into pregnancy.
of malaria.32
106 HEMATOLOGY • August 2018 EMJ EUROPEAN MEDICAL JOURNAL
Absorption of oral iron can be increased by taking the next 5 days. Hb testing is repeated after
a source of vitamin C along with the supplement 2–3 weeks and a second dose can be planned
on an empty stomach. Parenteral iron should be if required. A single dose should not exceed
considered from the second treatment month 1,000 mg of iron per week. A general
onwards in patients with: practitioner has to be notified if continued iron
therapy is needed.
>> Severe gastrointestinal side effects.
>> Intolerance to oral iron malabsorption. In India, oral iron therapy is initially trialled in
all women with Hb ≤9 g/dL. In patients with Hb
>> IDA unresponsive to oral iron.
7–9 g/dL, parental iron should be considered
>> Absolute noncompliance, particularly if mother after 32–34 weeks for an early rise, ensuring
is near term. 100% compliance. In patients with Hb <7 g/dL,
Among the various parenteral iron preparations, parenteral iron should be considered. The
iron carboxymaltose is the most preferred drug, government of India recommends the use of
and there is no need to give a test dose because intravenous iron sucrose since it is available
it is rarely associated with anaphylaxis. This readily and cheaper than alternatives.26 It is
drug can be given as total drug infusion and is available at a concentration of 20 mg/mL
available at the concentration of 50 mg/mL and is given as a slow intravenous injection of
of elemental iron. The dose is calculated on 100 mg or infusion of 200 mg. The U.S. Food
the basis of pre-pregnancy or booking weight, and Drug Administration (FDA) approves a
aiming for a target Hb of 11 g/dL. maximum dose of parenteral iron of 600 mg per
week. Unlike ferric carboxymaltose, it cannot be
Infused over 15 minutes, 1,000 mg in 20 mL given as a total dose infusion. Contraindications
is diluted in 250 mL of 0.9% sodium chloride. for parenteral iron are hypersensitivity to iron
The patient is observed for 30 minutes after or any cause other than IDA.
administration and oral iron is avoided for
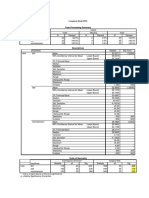
At booking appointment
IDA Hb <11 g/dL in first Iron deficiency alone
Nonanaemic
trimester or <10.5 g/dL in serum ferritin <30 μg/L
(Hb >11 g/dL)
second or third trimester Hb >11 g/dL
180–200 mg elemental
High risk Low risk iron with folic acid
400 µg as trial
No further
Normal Low serum intervention. Low dose iron; i.e.,
Hb after 2–3 weeks
serum ferritin Repeat Hb 65 mg elemental iron
ferritin (<30 μg/L) at 28 weeks
Hb improves No change
Oral iron
Continue until Check ferritin, serum B12, and serum folate
3 months after
Hb normalises
Serum ferritin <30 μg/L
Start parenteral iron
Figure 1: Management of iron deficiency anaemia in pregnancy in accordance to Royal College of Obstetricians and
Gynaecologists (RCOG) Green-top Guidelines.
Hb: haemoglobin; IDA: iron deficiency anaemia.
Adapted from Blood Transfusion in Obstetrics: Green-top Guideline No. 4731
Creative Commons Attribution-Non Commercial 4.0 August 2018 • HEMATOLOGY 107
Among intramuscular preparations, the only transfusion guideline33 recommends blood
one available in the UK is low molecular weight transfusion in labour or the immediate
iron dextran. In India, the most popular iron postpartum period if Hb is <7 g/dL. In Western
preparation is iron sorbitol citrate complex; countries, provision of cell salvage should be
however, these injections tend to be painful considered at the time of caesarean section.
and cause permanent skin staining. Their use is
therefore generally discouraged and no longer CONCLUSION
recommended in the UK. If one is to be given,
the Z-track injection technique should be used. IDA during pregnancy continues to be a
Women who are still anaemic at the time of major health problem in the developing world.
birth may require additional precautions, such as: This warrants certain steps at the individual
and community levels, such as education of
>> Birth in a hospital setting. pregnant women about anaemia, its causes,
>> Group and save of blood. and health implications. Nutritional education,
>> Active management of the third stage. with a special emphasis on strategies based on
locally available foodstuffs, administration of
>> A plan to deal with postpartum haemorrhage.
appropriate iron and folate supplements while
The need for blood transfusion can arise in the ensuring maximum compliance, treatment of
following situations: chronic disease like malaria deworming, and
universal antenatal care to pregnant women will
>> Severe anaemia in the last trimester for help in combatting this serious health hazard.
immediate improvement in Hb status. Long-term governmental policies should be
>> Severe anaemia with signs of cardiac failure directed towards formulation of effective plans
or hypoxia. to eradicate anaemia in children and adolescent
>> Haemoglobinopathy or bone marrow girls. Owing to the significant heterogeneity
failure syndromes. in screening, diagnosis, and treatment of IDA
>> Acute haemorrhage: if Hb <6 g/dL or if the across nations, more research is needed to
patient becomes haemodynamically unstable understand the clinical effects of routine
due to ongoing haemorrhage. screening, the ideal screening tools,
and the most effective treatment of IDA
The recent Royal College of Obstetricians during pregnancy.
and Gynaecologists (RCOG) (Figure 1) blood
References
1. World Health Organization. childbearing age,” (1994) Earl R, hepatocytes is mediated by the
Haemoglobin concentrations for the Woteki CE (eds.), Washington (DC): prohormone convertase furin. Blood
diagnosis of anaemia and assessment National Academies Press. Cells Mol Dis. 2008;40(1):132-8.
of severity. Vitamin and Mineral
4. Pavord S et al.; British Committee 8. Stevens GA et al.; Nutrition Impact
Nutrition Information System. 2011.
for Standards in Haematology. UK Model Study Group (Anaemia).
Available at: http://www.who.int/
guidelines on the management of Global, regional, and national trends
vmnis/indicators/haemoglobin/en/.
iron deficiency in pregnancy. Br J in haemoglobin concentration and
Last accessed: 14 June 2018.
Haematol. 2012;156(5):588-600. prevalence of total and severe
2. Centers for Disease Control (CDC). anaemia in children and pregnant and
5. Ezzati M et al. Comparative Risk
CDC criteria for anemia in children non-pregnant women for 1995-2011:
Assessment Collaborating Group.
and childbearing-aged women. A systematic analysis of population-
Selected major risk factors and global
MMWR Morb Mortal Wkly Rep. representative data. Lancet Glob
and regional burden of disease. The
1989;38(22):400-4. Health. 2013;1(1):e16-25.
Lancet. 2002;360(9343):1347-60.
3. Institute of Medicine (US) Committee 9. Mei Z et al. Assessment of iron
6. Trumbo P et al. Dietary reference
on the Prevention, Detection, and status in US pregnant women from
intakes: Vitamin A, vitamin K, arsenic,
Management of Iron Deficiency the National Health and Nutrition
boron, chromium, copper, iodine, iron,
Anemia Among U.S. Children and Examination Survey (NHANES), 1999-
manganese, molybdenum, nickel,
Women of Childbearing Age, “Iron silicon, vanadium, and zinc. J Am Diet 2006. Am J Clin Nutr. 2011;93(6):
deficiency anemia: Recommended Assoc. 2001;101(3):294-301. 1312-20.
guidelines for the prevention,
detection, and management 7. Valore EV, Ganz T. Posttranslational 10. Barroso F et al. Prevalence of
among US children and women of processing of hepcidin in human maternal anaemia and its predictors:
108 HEMATOLOGY • August 2018 EMJ EUROPEAN MEDICAL JOURNAL
A multi-centre study. Eur J Obstet States and Canada. Am J Clin Nutr. deficiency anemia. Mymensingh Med
Gynecol Reprod Biol. 2011;159(1): 2017;106(Suppl 6):1647S-54S. J. 2013;22(2):370-6.
99-105.
20. American College of Obstetricians 27. Tiwari M et al. Correlation of
11. Balarajan Y et al. Anaemia in low- and Gynecologists. ACOG Practice haemoglobin and red cell indices
income and middle-income countries. Bulletin No. 95: Anemia in pregnancy. with serum ferritin in Indian women
Lancet. 2011;378(9809):2123-35. Obstet Gynecol. 2008;112(1):201-7. in second and third trimester of
pregnancy. Med J Armed Forces
12. Lokare PO. A study of prevalence 21. RANZCOG 2009. Prepregnancy
India. 2013;69(1):31-6.
of anemia and sociodemographic counselling. 2017. Available at:
factors associated with anemia https://www.ranzcog.edu.au/ 28. World Health Organization
among pregnant women in RANZCOG_SITE/media/RANZCOG- (WHO), “Assessing the iron
Aurangabad city, India. Annals of MEDIA/Women%27s%20Health/ status of populations: Including
Nigerian Medicine. 2012;6(1):30-4. Statement%20and%20guidelines/ literature reviews: Report of a
Clinical-Obstetrics/Pre-pregnancy- joint World Health Organization/
13. Toteja GS et al. Prevalence of Counselling-(C-Obs-3a)-review- Centers for Disease Control and
anemia among pregnant women and July-2017.pdf?ext=.pdf. Last accessed: Prevention Technical Consultation
adolescent girls in 16 districts of India. 9 July 2018. on the assessment of iron status
Food Nutr Bull. 2006;27(4):311-5. at the population level, Geneva,
22. RANZCOG 2009. Routine antenatal
14. Baig-Ansari N et al. Anemia Switzerland,” (2004) 2nd edition.
assessment in the absence of
prevalence and risk factors in pregnancy complications. 2012. 29. Urrechaga E, Hoffmann JJML. Critical
pregnant women in an urban Available at: http://www.testingportal. appraisal of discriminant formulas
area of Pakistan. Food Nutr Bull. ashm.org.au/resources/C-Obs_3_ for distinguishing thalassemia from
2008;29(2):132-9. (b)_Routine_Antenatal_Assessment_ iron deficiency in patients with
in_the_Absence_of_Pregnancy_ microcytic anemia. Clin Chem Lab
15. Dreyfuss ML et al. Hookworms, Complications_NEW_Mar_13.pdf. Last Med. 2017;55(10):1582-91.
malaria and vitamin A deficiency accessed: 9 July 2018.
contribute to anemia and iron 30. Bothwell TH. Iron requirements in
deficiency among pregnant women 23. International Nutritional Anemia pregnancy and strategies to meet
in the plains of Nepal. J Nutr. Consultative Group (INACG), World them. Am J Clin Nutr. 2000;72(1
2000;130(10):2527-36. Health Organization (WHO), United Suppl):257S-64S.
Nations Childrens Fund (UNICEF),
16. Stoltzfus RJ et al., “Iron deficiency “Guidelines for the use of iron 31. Peña-Rosas JP et al. Daily oral iron
anaemia,” Ezzati et al. (eds.), supplements to prevent and treat supplementation during pregnancy.
Comparative quantification of health iron deficiency anemia,” Stoltzfus Cochrane Database Syst Rev.
risks: Global and regional burden of RJ, Dreyfuss ML (eds.), (1998), 2015;(7):CD004736.
disease attributable to selected major Washington, DC: Ilsi Press.
risk factors: Volume 1 (2004), Geneva: 32. Orton LC, Omari AA. Drugs for
World Health Organisation. 24. Siu AL; Preventive Services Task treating uncomplicated malaria in
Force. Screening for iron deficiency pregnant women. Cochrane Database
17. Lone FW et al. Maternal anaemia and anemia and iron supplementation Syst Rev. 2008;(4):CD004912.
its impact on perinatal outcome. Trop in pregnant women to improve
Med Int Health. 2004;9(4):486-90. 33. Royal College of Obstetricians and
maternal health and birth outcomes:
Gynaecologists. Blood Transfusion in
U.S. Preventive Services Task Force
18. Haider BA et al; Nutrition Impact Obstetrics: Green-top Guideline No.
Recommendation Statement. Ann
Model Study Group (anaemia). 47. 2015. Available at: https://www.
Intern Med. 2015;163(7):529-36.
Anaemia, prenatal iron use, and risk rcog.org.uk/globalassets/documents/
of adverse pregnancy outcomes: 25. Kapil U, Bhadoria AS. National iron- guidelines/gtg-47.pdf. Last accessed:
Systematic review and meta-analysis. plus initiative guidelines for control of 21 June 2018.
BMJ. 2013;346:f3443. iron deficiency anaemia in India, 2013.
Natl Med J India. 2014;27(1):27-9. 34. NICE. Antenatal care for
19. O'Brien KO, Ru Y. Iron status of uncomplicated pregnancies. 2017.
North American pregnant women: 26. Sultana GS et al. Value of red cell Available at: https://www.nice.org.uk/
An update on longitudinal data and distribution width (RDW) and RBC Guidance/cg62. Last accessed:
gaps in knowledge from the United indices in the detection of iron 9 July 2018.
Creative Commons Attribution-Non Commercial 4.0 August 2018 • HEMATOLOGY 109
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- CAT-6020B IntroductionDocument17 pagesCAT-6020B IntroductionAhmad RidhaNo ratings yet
- User'S Manual: June 2006 T.O. #33D7-22-32-1Document194 pagesUser'S Manual: June 2006 T.O. #33D7-22-32-1Pierpaolo AparoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Questionnaire Organic FoodDocument4 pagesQuestionnaire Organic FoodYuvnesh Kumar50% (2)
- Radio Data Reference Book Jessop 1967Document148 pagesRadio Data Reference Book Jessop 1967Cubelinho ResuaNo ratings yet
- MA5600T&MA5603T&MA5608T V800R016C10 Feature Guide 02 PDFDocument2,232 pagesMA5600T&MA5603T&MA5608T V800R016C10 Feature Guide 02 PDFMonowarul Alam MonirNo ratings yet
- Blendsbrochure 03 11 11Document20 pagesBlendsbrochure 03 11 11Valentina NistorNo ratings yet
- Renoir: Brushstrokes of A GeniusDocument4 pagesRenoir: Brushstrokes of A GeniuschrissypbshowNo ratings yet
- GMR 6939Document6 pagesGMR 6939Alfa FebriandaNo ratings yet
- Poster Session IV: ObjectiveDocument2 pagesPoster Session IV: ObjectiveAlfa FebriandaNo ratings yet
- Rizka Arsil, Syahredi SA, Hafni BachtiarDocument3 pagesRizka Arsil, Syahredi SA, Hafni BachtiarAlfa FebriandaNo ratings yet
- Antenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Document4 pagesAntenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Alfa FebriandaNo ratings yet
- Leptin rs2167270 G A (G19A) Polymorphism May Decrease The Risk of Cancer: A Case Control Study and Meta Analysis Involving 19 989 SubjectsDocument10 pagesLeptin rs2167270 G A (G19A) Polymorphism May Decrease The Risk of Cancer: A Case Control Study and Meta Analysis Involving 19 989 SubjectsAlfa FebriandaNo ratings yet
- Single Nucleotide Polymorphisms of Follicle-Stimulating Hormone Receptor Promoter and Their Impacts To The Promoter ActivitiesDocument10 pagesSingle Nucleotide Polymorphisms of Follicle-Stimulating Hormone Receptor Promoter and Their Impacts To The Promoter ActivitiesAlfa FebriandaNo ratings yet
- Pregnancy, The Postpartum Period and Prothrombotic Defects: Risk of Venous Thrombosis in The MEGA StudyDocument6 pagesPregnancy, The Postpartum Period and Prothrombotic Defects: Risk of Venous Thrombosis in The MEGA StudyAlfa FebriandaNo ratings yet
- Success of External Cephalic Version With Terbutaline As Tocolytic AgentDocument4 pagesSuccess of External Cephalic Version With Terbutaline As Tocolytic AgentAlfa FebriandaNo ratings yet
- Corticotrophin Releasing Hormone As A Useful Marker To Identify The Pre-EclampsiaDocument4 pagesCorticotrophin Releasing Hormone As A Useful Marker To Identify The Pre-EclampsiaAlfa FebriandaNo ratings yet
- Aavs 7 1 17-23 PDFDocument7 pagesAavs 7 1 17-23 PDFAlfa FebriandaNo ratings yet
- 1 PDFDocument7 pages1 PDFAlfa FebriandaNo ratings yet
- Haplotype AnalysisDocument5 pagesHaplotype AnalysisAlfa FebriandaNo ratings yet
- Antenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Document4 pagesAntenatal Care of Preeclampsia: From The Inverted Pyramid To The Arrow Model?Alfa FebriandaNo ratings yet
- Anaemia Pregnancy: (Dieckmann 1944 I960)Document13 pagesAnaemia Pregnancy: (Dieckmann 1944 I960)Alfa FebriandaNo ratings yet
- A Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesDocument2 pagesA Rare Case of Meigs Syndrome in Pregnancy With Bilateral Ovarian MassesAlfa FebriandaNo ratings yet
- Meigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsDocument6 pagesMeigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsAlfa FebriandaNo ratings yet
- Lock 1941Document3 pagesLock 1941Alfa FebriandaNo ratings yet
- Aogs 13082Document9 pagesAogs 13082Alfa FebriandaNo ratings yet
- Transfusion-Related Acute Lung Injury Risk Mitigation: An UpdateDocument10 pagesTransfusion-Related Acute Lung Injury Risk Mitigation: An UpdateAlfa FebriandaNo ratings yet
- Lampiran Hasil SPSS Klasifikasi Case Processing SummaryDocument5 pagesLampiran Hasil SPSS Klasifikasi Case Processing SummaryAlfa FebriandaNo ratings yet
- Huppert Z 2008Document7 pagesHuppert Z 2008Alfa FebriandaNo ratings yet
- Pi Is 0015028215018762Document11 pagesPi Is 0015028215018762Alfa FebriandaNo ratings yet
- Aogs 13082Document8 pagesAogs 13082Alfa FebriandaNo ratings yet
- Placenta: J. Patel, K. Landers, R.H. Mortimer, K. RichardDocument7 pagesPlacenta: J. Patel, K. Landers, R.H. Mortimer, K. RichardAlfa FebriandaNo ratings yet
- Ni Hms 672407Document19 pagesNi Hms 672407Alfa FebriandaNo ratings yet
- Maternal Serum Leptin As A Marker of PreeclampsiaDocument6 pagesMaternal Serum Leptin As A Marker of PreeclampsiaAlfa FebriandaNo ratings yet
- International Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary Syndrome 2018Document16 pagesInternational Evidence-Based Guideline For The Assessment and Management of Polycystic Ovary Syndrome 2018Alfa FebriandaNo ratings yet
- Enerpac Bolting ToolsDocument25 pagesEnerpac Bolting ToolsmichNo ratings yet
- HeliintDocument24 pagesHeliintCyntia OteyNo ratings yet
- Lecture Notes: Metric Spaces - Sergey MozgovoyDocument41 pagesLecture Notes: Metric Spaces - Sergey MozgovoyNúñezNo ratings yet
- Stieber Clutch Bearings CatalogueDocument96 pagesStieber Clutch Bearings CatalogueCardoso MalacaoNo ratings yet
- ISOVER Saint Gobain - Technical CatalogueDocument40 pagesISOVER Saint Gobain - Technical CatalogueBeng RosalesNo ratings yet
- 1º ESO - Inglés Vocabulary SEP PDFDocument13 pages1º ESO - Inglés Vocabulary SEP PDFKruveKruveNo ratings yet
- Bus Stop Guidelines Brochure PDFDocument26 pagesBus Stop Guidelines Brochure PDFWahyuBudiPrakosoNo ratings yet
- Armavia Flight 967 AccidentDocument3 pagesArmavia Flight 967 AccidenttherosantibadNo ratings yet
- Annual Curriculum Plan Science 2ndDocument2 pagesAnnual Curriculum Plan Science 2ndmarjorie conradeNo ratings yet
- Let's BeginDocument38 pagesLet's Begincrizziemaginationph2No ratings yet
- Shall I Use Zones or LDOMsDocument3 pagesShall I Use Zones or LDOMsplou0404No ratings yet
- Financial Performance Through Ratio Analysis of Rahimafrooz CIC Agro LimitedDocument58 pagesFinancial Performance Through Ratio Analysis of Rahimafrooz CIC Agro LimitedChemistry SoniaNo ratings yet
- Patent KarpenDocument2 pagesPatent KarpenErin MckinneyNo ratings yet
- Lucía Bustos Vázquez - CLASSWORKDocument9 pagesLucía Bustos Vázquez - CLASSWORKJesús Miguel Elías OsunaNo ratings yet
- Shadow BadmintonDocument9 pagesShadow Badmintonkuku93No ratings yet
- S/N Category Sub-Category Items NamesDocument9 pagesS/N Category Sub-Category Items NamesMIMOH80No ratings yet
- 6-Egyptian Code For LoadsDocument13 pages6-Egyptian Code For Loadsebrahimmousa9999No ratings yet
- Lesson PlanDocument11 pagesLesson PlanJean AmocapNo ratings yet
- Jenkins Ward 1965Document17 pagesJenkins Ward 1965franciscoNo ratings yet
- Geometry in The Real WorldDocument20 pagesGeometry in The Real Worldapi-279385232No ratings yet
- Chp. 2. Addressing Pollution (E.v.S)Document6 pagesChp. 2. Addressing Pollution (E.v.S)yastimewada2008No ratings yet
- 3.7 Organ Transplantation PDFDocument3 pages3.7 Organ Transplantation PDFbrownieallennNo ratings yet
- c09 Aeb D Sta B ST Al Az 0001Document1 pagec09 Aeb D Sta B ST Al Az 0001Ryan De Vera PagalNo ratings yet