Professional Documents
Culture Documents
2011 Assessment Flowchart Vlu PDF
Uploaded by
jhogie afitnandriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2011 Assessment Flowchart Vlu PDF
Uploaded by
jhogie afitnandriCopyright:
Available Formats
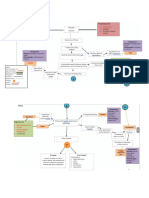
FLOW CHART FOR MANAGEMENT
FLOW CHART FOR ASSESSMENT OF
VENOUS LEG ULCERS OF VENOUS LEG ULCERS
Australian and New Zealand clinical practice guideline for
Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers
prevention and management of venous leg ulcers
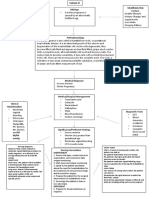
Patient presents with an ulceration on the lower leg Patient assessed as having a venous ulcer on the lower leg
1 Patient’s clinical history (page 20) Comprehensive assessment of the patient (page 20)
• Provide appropriate PAIN MANAGEMENT (page 28)
• medications • quality of life
•
1
venous disease varicose veins
• family history of leg ulceration • phlebitis
• psychosocial • nutrition
• decreased calf muscle pump • obesity
• comorbidities • pain Provide patient EDUCATION (Grade C, page 30)
HISTORY
function
• number of • Leg elevation • Compression therapy including use and care of hosiery
• surgery or trauma of affected pregnancies
Patient’s leg ulcer history (page 20)
• Nutrition • Exercise
leg
• previous or
• the duration of the current ulcer
• chest pain or pulmonary current DVT • previous ulcers and the time they have taken to heal
embolism
THE PATIENT
• prolonged standing or sitting
• time spent free of ulcers Provide access to appropriate PSYCHOSOCIAL support (page 31)
• strategies used to manage previous ulcers
Recommend ELEVATION of the lower limb to reduce oedema (Grade C, page 32)
Venous characteristics (page 22) Arterial characteristics
Associated changes in the leg Associated changes in the leg
PROGRESSIVE RESISTANCE EXERCISE to improve calf muscle function (Grade C, page 33)
• Firm (“brawny”) oedema • Oedema may be observed if infection present
• Haemosiderin deposit (reddish brown • Thin, shiny skin often with minimal hair growth
pigmentation)
• Leg shape is often straight with minimal shape
Encourage optimal NUTRITION AND HYDRATION to assist healing (page 34)
• Lipodermatosclerosis (skin hard and woody)
• Limb cool to touch
• Evidence of healed ulcers
•
• Dilated and torturous superficial veins
Elevated toes/leg become pale, dependent rub (+ve Beurger’s
test) 2 Prepare the surrounding skin:
• Hair is evident • Weak or absent pedal or leg pulses
• CLEANSE the leg at dressing changes (page 35)
• Atrophie blanche (white areas of intact skin) Ulcer location/characteristics
• MAINTAIN SKIN INTEGRITY of surrounding leg skin (page 36)
PREPARE THE LEG
ASSESSMENT
• • Ulcer margins well demarcated with “punched out” appearance
• CONTROL VENOUS ECZEMA (Grade C, page 36)
EXAMINATION
AND WOUND
Venous eczema (dry or wet itchy scaly skin)
• Altered shape – inverted “champagne
• Poorly perfused wound bed
bottle” • Necrotic tissue that may be tenacious (difficult to remove)
Wound bed preparation:
• Ankle flare (distended veins in foot arch or • Minimal wound exudate unless infected
ankle region) • CLEANSE the ulcer at dressing changes (page 35)
• Leaking oedema may result in maceration,
• Prone to infection • Consider DEBRIDEMENT of non-viable tissue (Grade C, page 37)
pruritis and scale
Pain • Consider treating CLINICAL INFECTION (page 38–47)
• Limb may be warm – heat and/or itch • Claudication or rest pain, may be worse at night or if leg is • Select appropriate PRIMARY DRESSING (Grade B, page 47)
elevated
Ulcer location and characteristics
• Anterior to medial malleolus
• Pretibial area (lower third of leg) Atypical ulcer characteristics
•
3 Graduated compression therapy (Grade B, page 53)
• Shallow with ragged, irregular edges None or minimal venous and arterial ulcers characteristics In the absence of arterial disease or diabetes mellitus
• Ruddy granulation tissue • Pain is extreme aim for > 30 mmHg (elastic) or high stiffness system (inelastic)
COMPRESSION
• Caution: Compression should be applied by a trained health professional
• Wound exudate moderate to high Oedema
and according to manufacturer’s guidelines
• May be odorous • Ulcer has an unusual appearance or atypical distribution
Pain • Suspicion of malignancy
• Patients receiving compression therapy should be MONITORED CLOSELY to ensure they
Varying from nil, to mild or extreme • Deterioration in ulcer or necrotic tissue present
• are able to tolerate compression and to monitor signs of healing
May be relieved by elevation of leg • Ulcer that has not healed in three months
Non-invasive diagnostic tests may be ordered: (page 24) Invasive diagnostic tests may be ordered:
INVESTIGATIONS
•
•
Pedal and leg pulses • Arterial and/or venous duplex scanning
(page 24)
• Blood profiles 4 Review and consider referral (page 26)
ABPI • Photoplethysmography
•
• TBPI • TCPO2
Wound tissue biopsy Ulcers not reduced in size by 25% in four weeks or failing to heal in
• • MRI
REVIEW
12 weeks should be considered for specialist referral
X-ray • Pulse oximetry
• Wound swab
3 Referral to 4 Refer to other
2 ABPI < 0.8 or > 1.2 or specialist side for
Prevention of recurrence
5
Atypical or arterial characteristics health management
MANAGEMENT
REFERRAL
professional of the Venous Measure and fit compression hosiery providing 18–40 mmHg (Grade B, page 62)
DIAGNOSIS
ulcer
(page 26)
ABPI 0.8–1.2 or
RECURRENCE
Characteristics of venous aetiology Ongoing encouragement should be given related to exercise, leg elevation and nutrition
PREVENT
Use CEAP classification
Hosiery should be renewed at least annually
SUMMARY OF RECOMMENDATIONS
Table 3.1: Recommendation grades15 Prepare the leg and ulcer
Evidence-based gradings developed from critical appraisal of the research Cleanse the leg and ulcer when dressings and bandages are changed. CBR
A Excellent evidence — body of evidence can be trusted to guide practice Treat venous eczema and impaired peri-ulcer skin promptly. CBR
B Good evidence — body of evidence can be trusted to guide practice in most situations Consider using topical barrier preparations to reduce peri-ulcer erythematous maceration in patients C
with VLU.
C Some evidence — body of evidence provides some support for recommendation(s) but care should
be taken in its application Enzymatic debriding agents have no effect in promoting healing in VLUs. C
D Weak evidence — body of evidence is weak and recommendation must be applied with caution Consider other debridement methods to prepare the ulcer bed for healing. CBR
Consensus-based recommendation (CBR) Treat clinical infection
Consensus evidence — a graded recommendation could not be made due to a lack of evidence Cadexomer iodine could be used to promote healing in VLUs when there is known increased microbial B
CBR from SRs or RCTs in populations with VLUs. The CBRs are supported by all members of the Expert burden.
Working Committee. Silver products offer no benefit over standard care in reducing the healing time of VLUs. C
Honey offers no benefits over standard care in promoting healing in VLUs. A
PREVENTING INITIAL OCCURRENCE OF VLUs Grade Topical antimicrobial agents should not be used in the standard care of VLUs with no clinical signs of B
Prevent and manage venous hypertension by: CBR infection.
• providing deep vein thrombosis (DVT) prophylaxis There may be a role for judicious use of topical antimicrobials when there is known or suspected increased CBR
• detecting and managing DVT early microbial burden.
• promoting access to venous surgery and phlebology interventions.
Use topical antibiotics judiciously in managing VLUs as there is a concern that their use is associated with CBR
When there are no contraindications, apply compression therapy to prevent the initial development of CBR antibiotic resistance and sensitivities.
a VLU in those at risk.
Systemic antibiotics should not be used in the standard care of VLUs that show no clinical signs of infection. B
ASSESSMENT, DIAGNOSIS AND REFERRAL Grade
Select a dressing and topical treatment
A health professional trained in the assessment and management of VLUs should conduct a CBR
No specific dressing product is superior for reducing healing time in VLUs. Select dressings based on B
comprehensive assessment of all patients presenting with a leg ulcer.
clinical assessment of the ulcer, cost, access and patient/health professional preferences.
A comprehensive assessment should include:
• clinical, pain and leg ulcer history Consider using dressings or bandages impregnated with zinc oxide to provide comfort and promote CBR
• examination of the leg and ulcer epithelialisation of a healthy granulated, superficial VLU.
• investigations to support diagnosis. Topical, pale, sulphonated shale oil could be used to promote healing in VLUs. C
A comprehensive assessment of the leg ulcer should be made on initial presentation and at regular CBR Apply compression
intervals thereafter to guide ongoing management.
When there are no contraindications, apply compression therapy to promote healing in VLUs. B
Use CEAP classification to evaluate and classify venous disease. CBR
Other interventions
Refer patients with a non-healing or atypical leg ulcer for consideration of biopsy. CBR
Consider bi-layered, bioengineered skin grafts to promote healing in persistent VLUs. B
Local guidelines should provide clear indication of appropriate criteria for referral to specialist health CBR
professionals. Health professionals benefit from education on VLUs and their management. Patient outcomes may be C
superior when ulcer care is conducted by a trained health professional.
MANAGING PAIN ASSOCIATED WITH VLUs Grade
When there are no contraindications, pentoxifylline could be used to promote healing in VLUs. B
Provide adequate pain management to promote QOL and VLU healing. CBR
When there are no contraindications, micronised, purified flavanoid fraction may be used to decrease C
When there are no contraindications, apply EMLA® cream to reduce pain associated with the A the healing time for VLUs.
debridement of VLUs.
Rural and remote populations
Electrotherapy could be considered for reducing pain from VLUs. C
Where access to specialist services is limited, health professionals could contact a VLU specialist via CBR
MANAGEMENT OF VLUs Grade telecommunications for advice and support in assessing and managing a patient with a VLU.
Managing the patient PREVENTING RECURRENCE OF VLUs Grade
Provide patients with appropriate education on their condition and its management. C Maintaining practices that promote the health of the legs may reduce the risk of VLU recurrence. CBR
Provide psychosocial assessment and support as an essential component in the patient’s management CBR Consider the continued use of compression therapy to reduce the risk of VLUs recurrence. B
plan.
Elevate the patient’s leg to promote changes in microcirculation and decrease lower limb oedema. C
Progressive resistance exercise may improve calf muscle function. C
Optimise the patient’s nutrition and hydration to promote healing in patients with VLUs. CBR
You might also like
- William Boericke. Homoeopat PDFDocument475 pagesWilliam Boericke. Homoeopat PDFAbhishek Kumar Upadhyay100% (1)
- Nattokinase - Optimum Health Vitamins PDFDocument13 pagesNattokinase - Optimum Health Vitamins PDFAnonymous SQh10rG100% (1)
- Inguinal Hernia EcaaDocument36 pagesInguinal Hernia EcaaElsha ZaskiaNo ratings yet
- Hemorrhoids: Presented By-Stuti Rastogi BSC Nursing 2 YearDocument25 pagesHemorrhoids: Presented By-Stuti Rastogi BSC Nursing 2 YearStuti RastogiNo ratings yet
- Home Care RN Skills ChecklistDocument2 pagesHome Care RN Skills ChecklistGloryJaneNo ratings yet
- IGCSE Biology Notes Updated April 2016Document94 pagesIGCSE Biology Notes Updated April 2016Adi101010101010101100% (1)
- Nursing Care Plan Abruptio PlacentaeDocument2 pagesNursing Care Plan Abruptio Placentaederic93% (29)
- Nursing Care Plan Ectopic PregnancyDocument2 pagesNursing Care Plan Ectopic PregnancyLei Ortega94% (36)
- Varicose Veins Endovenous Laser TreatmentDocument17 pagesVaricose Veins Endovenous Laser TreatmentaillNo ratings yet
- A Detailed Lesson Plan in Science 9Document5 pagesA Detailed Lesson Plan in Science 9GRACE LABATA0% (1)
- Communication in Nursing PracticeDocument3 pagesCommunication in Nursing PracticeOllian30050% (2)
- Uterovaginal ProlapseDocument52 pagesUterovaginal ProlapseAmeera K Khan75% (4)
- Nursing Care Plan Ectopic PregnancyDocument2 pagesNursing Care Plan Ectopic Pregnancyderic90% (39)
- Medical Terminology Systems A Body Systems Approach 8Th Edition Gylys Test Bank Full Chapter PDFDocument46 pagesMedical Terminology Systems A Body Systems Approach 8Th Edition Gylys Test Bank Full Chapter PDFkhuyentryphenakj1100% (9)
- NCC-SickleCellAnemiaManagement ConceptMap InteractivePDFDocument2 pagesNCC-SickleCellAnemiaManagement ConceptMap InteractivePDFLoggerz Arck100% (1)
- Diabetic UlcerDocument56 pagesDiabetic UlcermucfhsinNo ratings yet
- Deep Vein ThrombosisDocument9 pagesDeep Vein ThrombosisitdocNo ratings yet
- Nursing Care Plan Abrubtio PlacentaDocument2 pagesNursing Care Plan Abrubtio PlacentaLei Ortega0% (1)
- Medical Surgical NursingDocument31 pagesMedical Surgical Nursingsingireddi1revathi100% (3)
- NURSING CARE PLAN - Hepatitis ADocument2 pagesNURSING CARE PLAN - Hepatitis Aderic74% (19)
- KNGF Evidence Statement: Anal IncontinenceDocument2 pagesKNGF Evidence Statement: Anal IncontinencesilkofosNo ratings yet
- Evidence Statement Anal Incontinence Flowchart PDFDocument2 pagesEvidence Statement Anal Incontinence Flowchart PDFsilkofosNo ratings yet
- CS45385 NHS Abdo Pain Pathway Management - Primary Care Nov 17Document2 pagesCS45385 NHS Abdo Pain Pathway Management - Primary Care Nov 17Dinno PradanaNo ratings yet
- Ectopic PregnancyDocument13 pagesEctopic PregnancyJonielyn LagunaNo ratings yet
- Acute Abdominal Pain Pathway: Management - Primary Care and Community SettingsDocument2 pagesAcute Abdominal Pain Pathway: Management - Primary Care and Community Settingsshella1selinaNo ratings yet
- Peritonitis Sek UnderDocument2 pagesPeritonitis Sek UnderAnonymous eF8cmVvJaNo ratings yet
- Clinical PathwayDocument5 pagesClinical Pathwaychenri1318No ratings yet
- Prolapse Class 2020Document110 pagesProlapse Class 2020Vani BallaNo ratings yet
- 111 PDFDocument2 pages111 PDFswapnilazarusNo ratings yet
- Nursingcrib Com NURSING CARE PLAN Hepatitis A PDFDocument2 pagesNursingcrib Com NURSING CARE PLAN Hepatitis A PDFswapnilazarusNo ratings yet
- Unit Ix: Nursing Management of Patients With Gi Disorders: Topic: AppendicitisDocument16 pagesUnit Ix: Nursing Management of Patients With Gi Disorders: Topic: Appendicitisayushi rainaNo ratings yet
- Clinica de Chirurgie Caritas Clinica de Chirurgie CaritasDocument9 pagesClinica de Chirurgie Caritas Clinica de Chirurgie Caritaslordsith2004No ratings yet
- 19 TahnyDocument14 pages19 Tahnyheba abd elazizNo ratings yet
- Hernias: Mata, Francisco Casio A. Group 1Document56 pagesHernias: Mata, Francisco Casio A. Group 1Francisco Casio MataNo ratings yet
- Hiatal Hernia: BY MR, Vinay KumarDocument27 pagesHiatal Hernia: BY MR, Vinay KumarVinay KumarNo ratings yet
- PathopysiologyDocument14 pagesPathopysiologyAbigail Faith PretestoNo ratings yet
- Complete Denture Diagnosis & Treatment PlanningDocument40 pagesComplete Denture Diagnosis & Treatment PlanningAbdul KaderNo ratings yet
- UGIBDocument34 pagesUGIBChe Ainil ZainodinNo ratings yet
- AppendicitisDocument2 pagesAppendicitisjustinekaye diongsonNo ratings yet
- Nursing Management of Git Problems: Oral and Esophageal DisordersDocument18 pagesNursing Management of Git Problems: Oral and Esophageal Disorderslcpot_se7en7505100% (2)
- Nursing Care in Patient With Post Stroke: Erfin Firmawati, NS., MNSDocument33 pagesNursing Care in Patient With Post Stroke: Erfin Firmawati, NS., MNSAyu NawangiNo ratings yet
- Emergenze Addome RXDocument9 pagesEmergenze Addome RXBrovazzo PieroNo ratings yet
- NCP FinalDocument10 pagesNCP FinalAlessandro MadrigalNo ratings yet
- HemorrhoidsDocument9 pagesHemorrhoidsHimaniNo ratings yet
- Non-Modifiable Risk Factors: Modifiable Risk Factors: EtiologyDocument1 pageNon-Modifiable Risk Factors: Modifiable Risk Factors: EtiologyDenise FranciscoNo ratings yet
- 876knee Disorders - 4Document19 pages876knee Disorders - 4Umut YücelNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Urological RefferalDocument12 pagesUrological Refferalmichelle octavianiNo ratings yet
- Congenital Talipes Equinovarus (CTEV) : Nur Farhanah Binti Ariffin BJPA2019-0016 HSIDocument31 pagesCongenital Talipes Equinovarus (CTEV) : Nur Farhanah Binti Ariffin BJPA2019-0016 HSIfarhanah ariffinNo ratings yet
- Gs Toronto Nots PdaDocument34 pagesGs Toronto Nots PdaAhmed AttiaNo ratings yet
- Ob NCP 2Document2 pagesOb NCP 2Kimberly Mondala (SHS)No ratings yet
- 112 MS Lec Mod 3 CompleteDocument9 pages112 MS Lec Mod 3 CompleteANNE DOMINIQUE STA. ANANo ratings yet
- Cesarean SectionDocument11 pagesCesarean SectionChristine SaliganNo ratings yet
- Prevention of DVT & PE-1Document12 pagesPrevention of DVT & PE-1arongeremewNo ratings yet
- Vi. Nursing Care Plan Cues Analysis Nursing Diagnosis Goal / Plan Intervention Rationale EvaluationDocument2 pagesVi. Nursing Care Plan Cues Analysis Nursing Diagnosis Goal / Plan Intervention Rationale EvaluationRaisa Robelle QuichoNo ratings yet
- Compression Stockings CviDocument5 pagesCompression Stockings CviRafael CiresDrouetNo ratings yet
- Lumley Acute Abdomen 590 627Document38 pagesLumley Acute Abdomen 590 627zeek powerNo ratings yet
- MED Diseases of The EsophagusDocument4 pagesMED Diseases of The EsophagusJulie Anne AciertoNo ratings yet
- Stoma CareFrom EverandStoma CareJennie BurchNo ratings yet
- Essentials of Mini ‒ One Anastomosis Gastric BypassFrom EverandEssentials of Mini ‒ One Anastomosis Gastric BypassMervyn DeitelNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- Laparoscopic Sleeve GastrectomyFrom EverandLaparoscopic Sleeve GastrectomySalman Al-SabahNo ratings yet
- Gastrointestinal Interventional Endoscopy: Advanced TechniquesFrom EverandGastrointestinal Interventional Endoscopy: Advanced TechniquesMihir S. WaghNo ratings yet
- Medical Emergency ServiceDocument5 pagesMedical Emergency Servicejhogie afitnandriNo ratings yet
- CTEVDocument46 pagesCTEVjhogie afitnandriNo ratings yet
- Medical Emergency ServiceDocument5 pagesMedical Emergency Servicejhogie afitnandriNo ratings yet
- 4 Efektivitas Ambulasi DiniDocument6 pages4 Efektivitas Ambulasi DiniRifqi Daffa KurniaNo ratings yet
- Clinical Use of BloodDocument221 pagesClinical Use of BloodRizma Adlia100% (1)
- Jurnal PeneltianDocument3 pagesJurnal Peneltianjhogie afitnandriNo ratings yet
- Yg Ny Jop314 PDFDocument4 pagesYg Ny Jop314 PDFjhogie afitnandriNo ratings yet
- Yg Ny IJCP-69-1257 PDFDocument11 pagesYg Ny IJCP-69-1257 PDFjhogie afitnandriNo ratings yet
- Family Caregiving For Persons With Heart Failure at The Intersection of Heart Failure and Palliative Care: A State-of-theScience RevieDocument30 pagesFamily Caregiving For Persons With Heart Failure at The Intersection of Heart Failure and Palliative Care: A State-of-theScience Reviejhogie afitnandriNo ratings yet
- Ethics For The Information Age 7th Edition Quinn Solutions ManualDocument34 pagesEthics For The Information Age 7th Edition Quinn Solutions Manualoutcourt.unownedqagy100% (35)
- F3 Workbook p45-47Document3 pagesF3 Workbook p45-47jnieeeNo ratings yet
- ALL Clinicals OF LOWER LIMB (Anatomy)Document22 pagesALL Clinicals OF LOWER LIMB (Anatomy)Abdullah NasrullahNo ratings yet
- Cardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101Document26 pagesCardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101bagasNo ratings yet
- Chapter 1 - Respiratory and Circulatory Systems Working With The Other Organ SystemsDocument60 pagesChapter 1 - Respiratory and Circulatory Systems Working With The Other Organ SystemsPatricia Sofia DizonNo ratings yet
- Circulatory SystemDocument5 pagesCirculatory SystemTan XiangNo ratings yet
- Central Venous PressureDocument10 pagesCentral Venous PressureAngelo ArquizaNo ratings yet
- Diosmin + Hisperidin: DaflonDocument10 pagesDiosmin + Hisperidin: DaflonMark Anthony Mabini LlanosNo ratings yet
- Circulatory SystemDocument18 pagesCirculatory SystemRussiel DagohoyNo ratings yet
- Blue Phantom Customer CatalogueDocument43 pagesBlue Phantom Customer Cataloguedgina8800No ratings yet
- Norcet 17 Sep 2023-1Document28 pagesNorcet 17 Sep 2023-1Neutral Body NursingNo ratings yet
- Bab 20 PDFDocument43 pagesBab 20 PDFFuad AssodiqiNo ratings yet
- English For MedicineDocument52 pagesEnglish For MedicineRoya NaderiNo ratings yet
- Upsc Cms One Liner DR Varun AgarwalDocument13 pagesUpsc Cms One Liner DR Varun AgarwalSubhro ChatterjeeNo ratings yet
- Cardiovascular System Test Study GuideDocument26 pagesCardiovascular System Test Study GuideEstherThompsonNo ratings yet
- Propanolol Dan Hipertensi PortalDocument6 pagesPropanolol Dan Hipertensi PortalIndah LestariNo ratings yet
- New Zealand Data Sheet: Primolut N® Qualitative and Quantitative CompositionDocument13 pagesNew Zealand Data Sheet: Primolut N® Qualitative and Quantitative CompositionMohammed ShakilNo ratings yet
- Final Guidance Document For Donor HaemovigilanceDocument60 pagesFinal Guidance Document For Donor HaemovigilanceShiva ChandrakarNo ratings yet
- VascularDocument40 pagesVascularOmar MohammedNo ratings yet
- Coronary CirculationDocument33 pagesCoronary CirculationAayushman YadavNo ratings yet
- Anatomi Organ DR - Siti Rafiah HusainDocument73 pagesAnatomi Organ DR - Siti Rafiah HusainfitrahfajrianihamingNo ratings yet
- Lesson 6-Cardiovascular System PDFDocument10 pagesLesson 6-Cardiovascular System PDFRichard John IslaNo ratings yet
- II. Blood Vessels Physiology By: Dr. Abdulrahman Aqra MD MSCDocument12 pagesII. Blood Vessels Physiology By: Dr. Abdulrahman Aqra MD MSCapi-290338101No ratings yet