Professional Documents
Culture Documents
Neoplasia
Neoplasia
Uploaded by
fgdhgfrh0 ratings0% found this document useful (0 votes)
17 views2 pagesOriginal Title
Neoplasia.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views2 pagesNeoplasia
Neoplasia
Uploaded by
fgdhgfrhCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
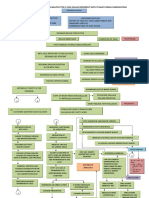
Appearance - Gross Morphology Pathogenesis
Neoplasia Video/mindmap: Six characteristics of cancer cells:
https://pathweb.nus.edu.sg/pathology-demystified/neoplasia/i-what- 1. Self-sufficient in growth factors
Clinical workflow for cancer diagnosis: is-neoplasia/ 2. Insensitive to inhibitory signals
1. Biopsy performed tissue sent to patho lab pathologist 3. Resistant to apoptosis
ascertains if malignant clinician decides on treatment 4. Immortal
2. After surgical excision (if done) pathologist examines the removed 5. Angiogenesis
tumour to decide on grade and local stage multidisciplinary team 6. Able to invade and metastasize
decides on further treatment (e.g. chemotherapy) Requires multi-step genetic alterations to overcome multiple
protective mechanisms:
Definition (1) Cell cycle regulatory checkpoints
Neoplasm: An abnormal mass of tissue, the growth of which exceeds, (2) Tumour suppressing mechanisms
and is uncoordinated with that of the normal tissues and persists in the (3) Apoptosis (cell death) &
same excessive manner after cessation of the stimuli which evoked the (4) DNA repair mechanisms
change. Pathogenesis Video/Mindmap: https://pathweb.nus.edu.sg/pathology-
demystified/neoplasia/ii-how/
Characteristics of Benign VS Malignant tumours
Benign Malignant Examples of genes involved:
Appearance and behaviour
Gross and microscopic features Gross and microscopic features
“innocent” abnormal
Remains localized – does NOT Locally invasive
invade. Appearance – Microscopic (often related to tumour grade)
No metastasis Metastasis (e.g. via vessels) (More: Papa Robbins 9th edition page 268-272)
Treatment
Amenable to local surgical Requires surgical
removal excision/radio/chemo
Prognosis/Outcome
Patient generally survives. Death and morbidity, cachexia.
However can cause significant (often)
morbidity through local effects
e.g. brain tumour compression
Nomenclature on tumours – how to name tumours
Mechanisms of genetic aberrations – Prognosis (Malignant tumours)
Kindly refer to notes/robbins textbook for more details. Video/Mindmap: https://pathweb.nus.edu.sg/pathology-
Inherited genetic aberration demystified/neoplasia/iii-clinical-effects-of-neoplasms/
- Inherited cancer syndromes, familial cancers
“Acquired” genetic aberration Stage and Grade are parameters used to assess clinical aggressiveness.
- Aging – Accumulation of gene mutations over the years
- Physical injury – Radiation / radiotherapy Stage - size and/or extent of the tumour growth
- Chemical carcinogens – Tobacco, Asbestos etc Tumour stage essentially refers to the size and/or extent of the tumour
- Biological – Chronic inflammation (Chronic liver cirrhosis: growth. Clinical findings, radiological imaging (CT scans, MRI, PET scans
Hepatocellular carcinoma) etc), intra-operative surgical findings and pathology reports of excised
- Viral integration into host genome can cause: oncogene expression, tumours are used to stage tumours. The AJCC TNM (American Joint
tumour suppressor gene inhibition, drive polyclonal proliferation of Committee on Cancer) staging system is widely used. Different
lymphocytes leading to increased risk of acquiring genetic mutations tumours have different TNM staging systems according to site and /or
which contribute to neoplastic transformation. tissue of origin.
Ebstein-Barr Virus – Hodgkin lymphoma, Burkitt lymphoma,
Nasopharyngeal CA; Grade - reflects the degree of differentiation of the tumour
Human Papilloma Virus – Squamous cell carcinoma of the uterine How well the tumour cells resemble the tissue of origin. The closer the
cervix resemblance, the lower the grade. In high grade tumours, the tumour
- Bacterial (Helicobactor pylori: Gastric lymphoma) cells appear very abnormal and are hard recognise as a certain cell
type.
Effects of Neoplasia Tumour grade is thus always assessed MICROSCOPICALLY (by the
Clinical Effects Video/Mindmap: pathologist)
https://pathweb.nus.edu.sg/pathology-demystified/neoplasia/iii-
clinical-effects-of-neoplasms/ Important Resources – do not forget:
Quizzes and Media Gallery: https://pathweb.nus.edu.sg/pathology-
demystified/neoplasia/1249-2/
- Know how to describe POTS/tumours grossly, distinguish grossly
between benign and malignant, and appreciate the histological
characteristics of benign and malignant tumours.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- MedicalBooks PDFDocument80 pagesMedicalBooks PDFfgdhgfrh50% (8)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Gourmet FinalDocument33 pagesGourmet Finalrizwanhafsa50% (4)
- Cell Damage and DeathDocument1 pageCell Damage and DeathfgdhgfrhNo ratings yet
- Glasgow Coma ScaleDocument4 pagesGlasgow Coma ScalefgdhgfrhNo ratings yet
- Embryology 10Document5 pagesEmbryology 10fgdhgfrhNo ratings yet
- The Probe Level Monitor: Instruction Manual PL-517 January 2001Document20 pagesThe Probe Level Monitor: Instruction Manual PL-517 January 2001horacio mondragon100% (1)
- GHVGHDocument3 pagesGHVGHINDAH IKA SARININGRUMNo ratings yet
- Before Domination: The History of Jollibee in The PhilippinesDocument22 pagesBefore Domination: The History of Jollibee in The PhilippinesChestineErikhaUmagatNo ratings yet
- Detector arc-LAD - HS 2019Document11 pagesDetector arc-LAD - HS 2019kryo195No ratings yet
- AlmeidaDocument8 pagesAlmeidaNicole TristanchoNo ratings yet
- Supplier Evalution & Control ProcedureDocument4 pagesSupplier Evalution & Control ProcedurePrime Cap100% (1)
- Code - 2216 - Congenital EventrationDocument5 pagesCode - 2216 - Congenital EventrationHumaida Hasan SamiraNo ratings yet
- Pathophysiology of Diabetes Mellitus Type Ii With ComplicationsDocument4 pagesPathophysiology of Diabetes Mellitus Type Ii With ComplicationsEricka Genove100% (1)
- Developmental Stages of Middle and Late AdolescenceDocument17 pagesDevelopmental Stages of Middle and Late AdolescenceFRED100% (1)
- Oncology McqsDocument115 pagesOncology McqsSyed NoorNo ratings yet
- Solid Recovered Fuels - Specifications andDocument8 pagesSolid Recovered Fuels - Specifications andLaraCarralNo ratings yet
- Aerial View of CII-Godrej GBC, Hyderabad Showing Wind Towers, Solar Photovoltaic Panels and Green Roofs. (Sourced)Document11 pagesAerial View of CII-Godrej GBC, Hyderabad Showing Wind Towers, Solar Photovoltaic Panels and Green Roofs. (Sourced)Happie SinghNo ratings yet
- Alpha Series Workshop Manual: Lpa, LPW, LPWT, Lpws and LPWGDocument109 pagesAlpha Series Workshop Manual: Lpa, LPW, LPWT, Lpws and LPWGAndres Huertas100% (1)
- Pat Bahasa Inggris Kelas IiDocument3 pagesPat Bahasa Inggris Kelas Iiwiwik widajatiNo ratings yet
- TSB SolventDocument9 pagesTSB SolventMaythee SaisriyootNo ratings yet
- Concept of Prana Vayu & Shat Chakras in Marma Chikitsa (मममम मममममममम)Document4 pagesConcept of Prana Vayu & Shat Chakras in Marma Chikitsa (मममम मममममममम)VestigeKamleshNo ratings yet
- PDS Benefit Overview - Dentist 2019Document4 pagesPDS Benefit Overview - Dentist 2019jentotheskyNo ratings yet
- When God Himself Was A StudentDocument2 pagesWhen God Himself Was A StudentSagar SharmaNo ratings yet
- Jds Journal of Syiah Kuala Dentistry SocietyDocument5 pagesJds Journal of Syiah Kuala Dentistry SocietyDewa Ayu Kumara DewiNo ratings yet
- Form No. 16: Details of Salary Paid and Any Other Income and Tax DeductedDocument2 pagesForm No. 16: Details of Salary Paid and Any Other Income and Tax DeductedSundaresan ChockalingamNo ratings yet
- Will The Real Sex Slave Please Stand UpDocument20 pagesWill The Real Sex Slave Please Stand Upabiwilkinson90No ratings yet
- RapeDocument34 pagesRapeGurpreet Singh Mandair100% (1)
- Erp SSTDocument32 pagesErp SSTAzmi Nurse OfficialNo ratings yet
- Statistics Mcqs Paper 2013Document2 pagesStatistics Mcqs Paper 2013zeb4019100% (1)
- Hooter - 72x72mm: Terminal ConnectionDocument1 pageHooter - 72x72mm: Terminal ConnectionImran TambatNo ratings yet
- Emission Calculation 2Document12 pagesEmission Calculation 2myungkwan haNo ratings yet
- Pico LL Very Fast-Acting Fuse 251/253 SeriesDocument4 pagesPico LL Very Fast-Acting Fuse 251/253 SeriesElhadj OualiNo ratings yet
- Brown Aluminium Oxide: AlcabDocument1 pageBrown Aluminium Oxide: AlcabIssam TrikiNo ratings yet
- Intro To First Aid and Basic Life SupportDocument31 pagesIntro To First Aid and Basic Life SupportLance BaraquielNo ratings yet