Professional Documents
Culture Documents
Biphosphonate Therapy in Renal Osteodystrophy
Uploaded by
Satriyo Dwi SuryantoroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Biphosphonate Therapy in Renal Osteodystrophy
Uploaded by
Satriyo Dwi SuryantoroCopyright:
Available Formats
REVIEW JNEPHROL 2013; 26 ( 3 ) : 450-455
DOI: 10.5301/jn.5000188
Bisphosphonate therapy in renal osteodystrophy
– a review
Raoul Bergner Department of Internal Medicine A, Ludwigshafen General
Hospital, Ludwigshafen am Rhein - Germany
bisphosphonates. For this reason knowledge of the phar-
Abstract macokinetics of the various bisphosphonates is a manda-
Bisphosphonates have become a standard treatment tory precondition for their use in severe renal impairment or
for osteoporosis and malignant bone disease. Most dialysis dependence.
are contraindicated in severe renal insufficiency be- Bone disease is a frequent finding in severe renal im-
cause they are eliminated exclusively by the kidneys. pairment (Kidney Disease: Improving Global Outcomes
However, the marked impairment of bone metabo- [KDIGO] stages IV & V). Most forms are subsumed un-
lism in many dialysis patients provides a rationale der the terms renal osteopathy or renal osteodystrophy.
for their judicious use in this setting. Animal stud- However, they do not form a homogeneous syndrome but
ies reveal that bisphosphonates inhibit hyperpara- encompass a whole complex of bone changes charac-
thyroid bone changes. Clodronate, pamidronate and terized on the one hand by chronic vitamin D deficiency
ibandronate are also readily dialyzable, enabling and reduced 1-α-hydroxylase activity and on the other by
them to be used in dialysis patients. Initial pilot stud-
secondary hyperparathyroidism (1). Other critical deter-
ies in dialysis patients have confirmed the positive
minants of bone metabolism include chronic metabolic
effect on hyperparathyroid bone disease observed in
acidosis, raised ß2-microglobulin levels (2, 3) and regu-
animal models. However, large randomized placebo-
controlled trials are required before the use of lar heparin treatment in dialysis (4) (Fig. 1). Most current
bisphosphonates in renal osteopathy can be gener- treatments in dialysis patients aim to lower parathyroid
ally recommended. hormone (PTH) levels into the guideline range (Kidney Dis-
ease Outcome Quality Initiative [KDOQI]) (5). Additional
Key words: Bisphosphonate, Dialysis, High turnover os- aims are to lower calcium and phosphate levels into their
teopathy, Hyperparathyroidism, Renal osteodystrophy predefined target ranges. But since this barely influences
the critical determinants just mentioned, such therapy
often has a limited impact on bone. Approaches aimed
Introduction at treating bone metabolism directly are only in their
infancy and to be viewed in the main as experimental.
Bisphosphonates have become a standard treatment for Nevertheless, patients in stage IV or V chronic renal fail-
osteoporosis and malignant bone disease. Their mecha- ure are known to be at above-average fracture risk even
nism of action − osteoclast inhibition − makes them a after their PTH levels have been lowered into the KDOQI
valuable treatment option in all forms of bone disease as- guideline range (Tab. I) (6). Hence the need to elucidate
sociated with increased osteoclast activity. Since bisphos- the feasibility of bisphosphonate use in severe renal im-
phonates are either bound to bone or excreted intact via the pairment or dialysis dependence.
kidney, there has been reluctance to consider their use in
renal impairment. In addition, some bisphosphonates have Pharmacokinetics
become notorious for nephrotoxic complications, although
this has been confined almost exclusively to their use in ma- The only bisphosphonates for which targeted pharmacoki-
lignant bone disease, in particular multiple myeloma. There netic studies are available in dialysis-dependent renal failure
have been no reports as yet of nephrotoxic complications in are clodronate (7, 8), an early non-aminobisphosphonate,
the treatment of osteoporosis. Even so, a creatinine clear- and ibandronate (9) and pamidronate (10), both among the
ance below 30-35 mL/min contraindicates the use of most newer aminobisphosphonates.
450 © 2012 Società Italiana di Nefrologia - ISSN 1121-8428
JNEPHROL 2013; 26 ( 3 ) : 450-455
alysis, ibandronate 2 mg was administered at the end of a
dialysis session and bone binding equated with non-renal
clearance (12). Unlike clodronate, ibandronate was 95% to
99% cleared from the circulation (= bound to bone), but
independently of PTH or other bone metabolism markers.
This naturally carries the risk of the near-total ibandronate
dose being taken up in bone, even in low turnover bone.
Appropriate caution is thus recommended in therapy.
Pamidronate
Clearance of 1 mg radiolabeled pamidronate was 69 ±
17 mL/min (10). No bone-binding data are available for
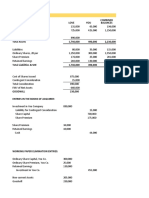
Fig. 1 - Four major mechanisms causing sustained stimula- pamidronate in dialysis patients.
tion of osteoclast (OC) activity: in addition to the most impor-
Thus, all bisphosphonates studied to date have proven to
tant stimulating factor, parathyroid hormone (PTH), chronic
metabolic acidosis, increased β2microglobulin (β2MG) and be readily dialyzable: four-hour dialysis clears 35% to 40%
elevated fibroblast growth factor 23 (FGF 23) also have OC- of the administered dose (Tab. II), which is approximately
activating activity. Heparin administration at each dialysis
session likewise causes OC activation by inhibiting osteopro-
equivalent to renal bisphosphonate elimination in normal
tegerin (OPG). OB = osteoblasts; RANK-L = receptor activator renal function. In the case of pamidronate, however, there
of nuclear factor kappa B ligand (RANKL). is some uncertainty as to whether the clearance of 1 mg is
extrapolable to a standard clinical dose of 60-90 mg. With
the other bisphosphonates the doses were in each case
Clodronate relatively close to those in clinical use.
Two studies used a similar design to determine the dialyz- Continuous ambulatory peritoneal dialysis (CAPD)
ability of clodronate, infusing 300 mg over two hours prior to
four-hour dialysis (7, 8). Calculated clodronate clearances, Because bone metabolism in CAPD has only been studied
86 ± 10 mL/min and 88 ± 16 mL/min, were largely similar to with methylene-bisphosphonate (13), no figures for bisphos-
those for normal renal function. A study of clodronate up- phonate clearance via CAPD can be provided.
take into bone found a clear dependency on PTH levels and
bone metabolism: the higher the PTH, the greater the bone Animal studies
uptake (11).
Initial models of bisphosphonate therapy for hyperparathy-
Ibandronate roid bone disease were explored in animals using ibandro-
nate (14), olpadronate (15), and pamidronate (16).
Clearance of ibandronate 1 mg administered at the start of Ibandronate 1.25 µg/kg or placebo was administered sub-
fourhour hemodialysis was 92 ± 19 mL/min, a value like- cutaneously (sc) weekly for three weeks to 2/3 nephrecto-
wise virtually identical to that for normal renal function (9). mized rats and the results compared with sham-operated
To quantify bone binding in the absence of subsequent di- controls with normal renal function (14). Ibandronate com-
Table I
Target parathormone, calcium and phosphate values according to National Kidney Foundation
Kidney Disease Outcome Quality Initiative (KDOQI) guidelines (5)
Parathyroid hormone 150-300 pg/mL 16.5-33.0 pmol/L Evidence
Calcium 8.4-9.5 mg/dL 2.1-2.37 mmol/L Opinion
Phosphate 3.5-5.5 mg/dL 1.13-1.78 mmol/L Evidence
Calcium × phosphate < 55 mg2/dL2 Evidence
© 2012 Società Italiana di Nefrologia - ISSN 1121-8428 451
Bergner: Bisphosphonate therapy in renal osteodystrophy
pletely abolished the bone effects of developing hyper- use of the various bisphosphonates in this setting. The first
parathyroidism in nephrectomized rats. Bone resorption trial of clodronate in dialysis patients dates from 1990 (17).
parameters (deoxypyridinoline) and bone volume to total However, this was a very brief study in nine patients with
volume (BV/TV) in the ibandronate group were almost identi- severe hyperparathyroid bone disease who received an
cal to those in the rats with normal renal function. infusion of clodronate 300-600 mg at the end of five con-
A near-identical study design in 5/6 nephrectomized rats secutive dialysis sessions. A significant fall was observed
administered olpadronate 1.6 µg sc weekly for five weeks in bone resorption parameters (hydroxyproline) and calcium
found a similar effect (15). After an initial increase in de- and phosphate levels. Alkaline phosphatase (AP) and PTH
oxypyridinoline in nephrectomized animals, levels in the ac- values, on the other hand, increased. While some of the pa-
tive treatment group subsequently declined to those in the tients were simply followed up, others received clodronate
sham-operated animals versus marked bone resorption in 1.6 g orally daily for a further two weeks. Only these longer-
the placebo controls. Olpadronate significantly reduced the treated patients showed sustained benefit in terms of their
tartrate-resistant acid phosphatase (TRAP) positive osteo- laboratory parameters.
clast count and significantly increased bone volume. In a longer, 12-month, open-label and non-placebo-con-
In the pamidronate study, rats were 5/6 nephrectomized, trolled study, 13 patients with persistent severe hyper-
uninephrectomized, or left intact; 14 weeks later, the uni and parathyroidism (PTH >500 pg/mL [normal 12-65 pg/mL]),
5/6 nephrectomized rats received pamidronate 3 mg/kg/ hypercalcemia (>11 mg/dL), normal phosphate, and osteo-
week sc or placebo for eight weeks; the intact rats received penia (T-score <1 SD), received an infusion of pamidronate
placebo (16). Whereas the uninephrectomized rats devel- 60 mg every two months during dialysis (18). Bone density
oped only mild renal failure with no marked bone metabolic increased significantly in both the lumbar spine and femoral
effects, PTH values increased 5-fold in the 5/6 nephrecto- neck. PTH levels were massively increased at three months,
mized rats. Bone histology revealed renal osteopathy with however, only to reverse subsequently in ten of the 13 pa-
osteitis fibrosa and increased bone turnover. Pamidronate tients: by one year, PTH levels in these 10 patients had fallen
therapy markedly decreased bone metabolism in all animals significantly below baseline, while the calcitriol dose had
and attained values below the normal range, while bone been increased from 1 µg/week to 3 µg/week without caus-
density increased significantly. However, no animal devel- ing the hypercalcemia that had previously made such an
oped osteomalacia. increase impossible. Whether the PTH-lowering effect was
directly because of the pamidronate or the increased dose
Clinical studies (Tab. III) of calcitriol remains an open question.
In another open-label study with no placebo arm, 16 patients
The use of bisphosphonates for hyperparathyroid bone dis- with T-score ≤1.0 SD, PTH ≥2 × normal, and no reduction in
ease in dialysis patients has been the subject of varied edi- other bone metabolism parameters (TRAP5b, bone-specific
torials for years. The available animal studies indicate that AP and CrossLaps) received an injection of ibandronate 2 mg
such an approach is highly promising. All the more astonish- after dialysis every four weeks for 1 year; 11 patients were
ing, therefore, that there should still be virtually no data on the eventually fit for assessment (19). The study revealed a sig-
Table II
Bisphosphonate pharmacokinetics in a four-hour dialysis session
Beigel Ala-Houhala Bergner Buttazzoni
et al (7) et al (8) et al (9) et al (10)
Bisphosphonate Clodronate Clodronate Ibandronate Pamidronate
Dose (mg) 300 300 1 1
Treatment dosage 3 × 300-600 mg/d 2-6 mg 60-90 mg
Dialysis clearance (mL/min) 86 ± 10 88 ± 16 92 ± 19 69 ± 17
% administered dose cleared 35 35 37 32
by dialysis
452 © 2012 Società Italiana di Nefrologia - ISSN 1121-8428
JNEPHROL 2013; 26 ( 3 ) : 450-455
Table III
Three long-term bisphosphonate studies in dialysis patients
Wetmore et al (20) Torregrosa et al (18) Bergner et al (19)
Type of study Randomized vs. placebo Open-label Open-label
No. (complete data available) 16/15 (31) 13 (13) 16 (12)
Bisphosphonate Alendronate Pamidronate Ibandronate
Dosage 40 mg/week for 60 mg every 2 mg every
6 weeks 8 weeks 4 weeks
Duration (months) 6 12 12
Route Oral Intravenous during Intravenous after
hemodialysis hemodialysis
Inclusion criteria Age >40 y T-score ≤1 T-score ≤1.5
PTH 100-300 pg/mL PTH > 500 pg/mL PTH >130 pg/mL
Calcium × phosphate Calcium >11 mg/dL TRAP 5b & BAP not
<5.65 Phosphate <6 mg/dL below normal range
Endpoint Bone mineral density Not defined Bone mineral density
Bone density Dual energy X-ray Dual energy X-ray Quantitative computed
measurement absorptiometry absorptiometry tomography
Results Reduced bone density Significantly increased Significantly increased
loss vs. placebo bone density in bone density
lumbar spine & hip in lumbar spine
BAP = bone-specific alkaline phosphatase; PTH = parathyroid hormone; TRAP5b = tartrate-resistant acid phosphatase 5b.
nificant increase in the primary endpoint, lumbar spine bone
density. At three months, as in the two studies above, PTH Discussion
levels were markedly increased. However, as in the pamidro-
nate study, they had fallen below baseline by the end of the All studies to date have shown the bisphosphonates to be
study. Unlike in the pamidronate study, PTH levels remained readily dialyzable. Despite higher protein binding in some
within the KDOQI guideline range (5) throughout the study. cases, bisphosphonate clearance during a fourhour dialy-
Bone metabolism markers, except for CrossLaps, showed sis session is consistently equivalent to that for normal renal
only a slight non-significant fall. Calcitriol doses underwent function. Thus, a single dialysis session can largely clear a
a slight but non-significant increase during the study. dose of bisphosphonate. For this reason, if the aim is not
The only placebo-controlled study of bisphosphonates in to lose much of the dose immediately, bisphosphonates
the treatment of renal osteopathy was performed with oral should be administered after dialysis. To date, binding to
alendronate 40 mg/week for six weeks in 31 dialysis pa- bone in dialysis patients has only been studied for clodro-
tients over 40 years of age with PTH levels between 100 and nate and ibandronate. The results revealed a marked differ-
300 pg/mL (20). Hip and lumbar spine densities were mea- ence between the aliphatic first-generation bisphosphonate
sured at baseline and six months, and osteocalcin, PTH, clodronate and the aminobisphosphonate ibandronate.
calcium, phosphorus and AP at baseline, one, three, and six Ibandronate showed a very high affinity for bone indepen-
months. Here again PTH levels increased on bisphospho- dently of bone metabolism, whereas with clodronate there
nate therapy. Hip density remained stable in the alendronate was a close correlation with bone turnover. This carries the
group while decreasing significantly in the placebo group. great danger that the near totality of the ibandronate dose
The other parameters did not differ between the groups. binds to bone even if bone metabolism is already low.
© 2012 Società Italiana di Nefrologia - ISSN 1121-8428 453
Bergner: Bisphosphonate therapy in renal osteodystrophy
Several animal studies have clearly shown that bisphos- PTH elevation alone does not exclude low-turnover oste-
phonate therapy reverses both the histologic changes of opathy (26, 27), every dialysis patient would ideally need a
experimental hyperparathyroidism and the changes in bone bone biopsy before commencing bisphosphonate therapy.
metabolism parameters. Osteomalacia was not induced Other unresolved questions concern the duration of bisphos-
despite the substantial reduction in bone remodeling. Bone phonate therapy in high-turnover osteopathy and the most
density increased markedly, as in the osteoporosis studies. appropriate parameters for monitoring treatment.
Yet despite these pharmacokinetic findings and experimen- Special attention should be given to potential side effects
tal renal osteopathy results, clinical study data are meager: of the bisphosphonates, especially the osteonecrosis of the
just three studies in small numbers of dialysis patients re- jaw. This severe side effect is reported mainly in patients
ceiving bisphosphonates. Doubtless all three studies have with high dose bisphosphonate treatment for malignant
substantial weaknesses here and there and are no substi- bone disease who undergo dental surgery (28). Only few
tute for large randomized placebo-controlled clinical trials, case reports of ONJ in dialysis patients are reported (29).
but they do point to a trend. Another point of interest might be the dosage of calcitriol,
In terms of weaknesses, none of the studies incorporated which increased in two studies (18, 19). Rising PTH levels
the gold standard investigation for diagnosing high turnover after starting bisphosphonate treatment lead to a higher
osteopathy, namely bone biopsy, and all patient numbers dosage of calcitriol with the potential risk of higher calcium
were very low. The studies also relied on bone density and and phosphorus levels. On the other hand, several studies
surrogate markers of bone metabolism (21), not the fracture demonstrated a calcium and phosphorus lowering effect
rates used in the pivotal studies of bisphosphonates in the of bisphosphonate treatment (30-33). Therefore, the risk
treatment of osteoporosis. of high calcium and phosphorus levels leading to a diffuse
In the pamidronate study it is also unclear how much of the tissue or vascular calcification would be low. In addition,
drug administered during dialysis was even taken up in bone, bisphosphonates have also shown a direct beneficial effect
since pamidronate is readily dialyzable. The alendronate on tissue and vascular calcification (34-36).
study can be criticized for the ultralow dose used. Neverthe- A case can be made on the basis of the data presented for
less, some observations remain that are consistent across extending bisphosphonate therapy to dialysis patients with
all three studies. Thus, bisphosphonates increase or stabi- certain forms of renal osteopathy. However, in the complete
lize bone density compared to placebo in dialysis patients absence to date of large randomized placebo-controlled tri-
too. They also increase PTH levels, according to a study of als, such therapy can only be recommended at best as an
this phenomenon by Lu et al (22), because of a transient de- individual management decision. In such cases, prior bone
crease in calcium. However, PTH levels subsequently fall to biopsy to confirm high-turnover osteopathy is mandatory.
below baseline, i.e. the effect is only transient.
Many questions remain open – treatment dose, for a start. Financial support: None.
It could be argued that the higher bone metabolism than in
osteoporosis requires a higher dose of bisphosphonate. On Conflict of interest statement: Dr. Bergner received speakers fee from
the other hand, the absence of renal excretion means that no Abbott, Amgen, Bristol-Myers-Squibb, Lilly and Roche Pharma.
bisphosphonate gets lost, with virtually the entire dose being
available to bone. Dose-finding studies are clearly needed. Address for correspondence:
It is also uncertain whether low bone density alone, as in Raoul Bergner, MD
Medizinische Klinik A
osteoporosis, is a sufficient indication for bisphosphonate
Klinikum der Stadt Ludwigshafen GmbH
therapy in dialysis patients (23-25). The danger in low-turn- Bremserstraße 79
over osteopathy is that the bisphosphonate radically inhibits 67063 Ludwigshafen, Germany
residual bone turnover, resulting in adynamic bone. Since bergnerr@klilu.de
ment from Kidney Disease: Improving Global Outcomes
References (KDIGO). Kidney Int. 2006;69(11):1945-1953.
2. Petersen J, Kang MS. In vivo effect of beta 2-microglobulin
1. Moe S, Drüeke T, Cunningham J, et al. Kidney Disease: Im- on bone resorption. Am J Kidney Dis. 1994;23(5):726-730.
proving Global Outcomes (KDIGO). Definition, evaluation, 3. Menaa C, Esser E, Sprague SM. Beta2-microglobulin stimu-
and classification of renal osteodystrophy: a position state- lates osteoclast formation. Kidney Int. 2008;73(11):1275-1281.
454 © 2012 Società Italiana di Nefrologia - ISSN 1121-8428
JNEPHROL 2013; 26 ( 3 ) : 450-455
4. Chowdhury MH, Hamada C, Dempster DW. Effects of heparin 21. Gerakis A, Hutchison AJ, Apostolou T, Freemont AJ, Billis A.
on osteoclast activity. J Bone Miner Res. 1992;7(7):771-777. Biochemical markers for non-invasive diagnosis of hyperpara-
5. KDOQI (Kidney Disease Outcomes Quality Initiative). KDOQI thyroid bone disease and adynamic bone in patients on hae-
Clinical Practice Guidelines for Bone Metabolism and Dis- modialysis. Nephrol Dial Transplant. 1996;11(12):2430-2438.
ease in Chronic Kidney Disease. Available at: http://www. 22. Lu KC, Yeung LK, Lin SH, Lin YF, Chu P. Acute effect of pami-
kidney.org/professionals/KDOQI/guidelines_bone/index.htm. dronate on PTH secretion in postmenopausal hemodialysis
Accessed: April 13, 2012. patients with secondary hyperparathyroidism. Am J Kidney
6. Nickolas TL, Leonard MB, Shane E. Chronic kidney disease Dis. 2003;42(6):1221-1227.
and bone fracture: a growing concern. Kidney Int. 2008; 23. Gerakis A, Hadjidakis D, Kokkinakis E, Apostolou T, Raptis
74(6):721-731. S, Billis A. Correlation of bone mineral density with the histo-
7. Beigel AE, Rienhoff E, Olbricht CJ. Removal of clodronate by logical findings of renal osteodystrophy in patients on hemo-
haemodialysis in end-stage renal disease patients. Nephrol dialysis. J Nephrol. 2000;13(6):437-443.
Dial Transplant. 1995;10(12):2266-2268. 24. Fontaine MA, Albert A, Dubois B, Saint-Remy A, Rorive G.
8. Ala-Houhala I, Saha H, Liukko-Sipi S, Ylitalo P, Pasternack A. Fracture and bone mineral density in hemodialysis patients.
Pharmacokinetics of clodronate in haemodialysis patients. Clin Nephrol. 2000;54(3):218-226.
Nephrol Dial Transplant. 1999;14(3):699-705. 25. Ureña P, Bernard-Poenaru O, Ostertag A, et al. Bone mineral
9. Bergner R, Dill K, Boerner D, Uppenkamp M. Elimination of density, biochemical markers and skeletal fractures in haemodi-
intravenously administered ibandronate in patients on hae- alysis patients. Nephrol Dial Transplant. 2003;18(11):2325-2331.
modialysis: a monocentre open study. Nephrol Dial Trans- 26. Coen G, Ballanti P, Bonucci E, et al. Renal osteodystrophy
plant. 2002;17(7):1281-1285. in predialysis and hemodialysis patients: comparison of his-
10. Buttazzoni M, Rosa Diez GJ, Jager V, Crucelegui MS, Algrana- tologic patterns and diagnostic predictivity of intact PTH.
ti SL, Plantalech L. Elimination and clearance of pamidronate Nephron. 2002;91(1):103-111.
by haemodialysis. Nephrology (Carlton). 2006;11(3):197-200. 27. Drüeke TB. Is parathyroid hormone measurement useful for the
11. Saha H, Ala-Houhala I, Ylitalo P, Kleimola T, Pasternack A. diagnosis of renal bone disease? Kidney Int. 2008;73(6):674-676.
Skeletal deposition of clodronate is related to parathyroid 28. Pazianas M, Miller P, Blumentals WA, Bernal M, Kothawala P.
function and bone turnover in dialysis patients. Clin Nephrol. A review of the literature on osteonecrosis of the jaw in pa-
2002;58(1):47-53. tients with osteoporosis treated with oral bisphosphonates:
12. Bergner R, Henrich D, Hoffmann M, et al. High bone-binding prevalence, risk factors, and clinical characteristics. Clin
capacity of ibandronate in hemodialysis patients. Int J Clin Ther. 2007;29(8):1548-1558.
Pharmacol Res. 2005;25(3):123-131. 29. Papagni S, Mongelli N, Cozzolino M, Brancaccio D,
13. Joffe P, Henriksen JH. Aspects of osseous, peritoneal and renal Ciccolella F, Favia G. [Avascular jaw osteonecrosis in a
handling of bisphosphonate during peritoneal dialysis: a meth- hemodialysis patient treated with bisphosphonates.]. G Ital
odological study. Scand J Clin Lab Invest. 1996;56(4):327-337. Nefrol. 2007;24(3):230-234.
14. Geng Z, Monier-Faugere MC, Bauss F, Malluche HH. Short-term 30. Davenport A, Goel S, Mackenzie JC. Treatment of hypercal-
administration of the bisphosphonate ibandronate increases caemia with pamidronate in patients with end stage renal
bone volume and prevents hyperparathyroid bone changes in failure. Scand J Urol Nephrol. 1993;27(4):447-451.
mild experimental renal failure. Clin Nephrol. 2000;54(1):45-53. 31. Trimarchi H, Lombi F, Forrester M, et al. Disodium pamidro-
15. Tomat A, Gamba CA, Mandalunis P, et al. Changes in bone nate for treating severe hypercalcemia in a hemodialysis pa-
volume and bone resorption by olpadronate treatment in an tient. Nat Clin Pract Nephrol. 2006;2(8):459-463, quiz 464.
experimental model of uremic bone disease. J Musculoske- 32. Czosnowski LM, Hudson JQ, Canada RB. Hypercalcemia
let Neuronal Interact. 2005;5(2):174-181. associated with tertiary hyperparathyroidism managed con-
16. Jokihaara J, Pörsti IH, Kööbi P, et al. Treatment of experi- servatively with pamidronate in a hemodialysis patient. Am J
mental renal osteodystrophy with pamidronate. Kidney Int. Med Sci. 2009;337(4):300-301.
2008;74(3):319-327. 33. Musso CG, Guelman R, Varela F, et al. Ibandronate improves
17. Hamdy NA, McCloskey EV, Brown CB, Kanis JA. Effects hyperphosphatemia in dialysis patients with hyperparathy-
of clodronate in severe hyperparathyroid bone disease in roidism. Int Urol Nephrol. 2004;36(4):625-627.
chronic renal failure. Nephron. 1990;56(1):6-12. 34. Tamura K, Hashiba H, Kogo H, Aizawa S, Shigematsu T. [Sup-
18. Torregrosa JV, Moreno A, Mas M, Ybarra J, Fuster D. Useful- pressive effects of bisphosphonates on the vascular calcifica-
ness of pamidronate in severe secondary hyperparathyroid- tion in ESRD patients]. Clin Calcium. 2002;12(8):1129-1135.
ism in patients undergoing hemodialysis. Kidney Int Suppl. 35. Obad D, Larsen NA, Pedersen EB. [Regression of severe peri-
2003;85(85):S88-S90. articular calcifications during treatment with bisphosphonate
19. Bergner R, Henrich D, Hoffmann M, Schmidt-Gayk H, Lenz T, in a dialysis patient]. Ugeskr Laeger. 2010;172(9):719-721.
Upperkamp M. Treatment of reduced bone density with iban- 36. Okada Y, Mori H, Tanaka Y, Hashimoto O. [Positioning of
dronate in dialysis patients. J Nephrol. 2008;21(4):510-516. bisphosphonates for vascular calcification]. Clin Calcium.
20. Wetmore JB, Benet LZ, Kleinstuck D, Frassetto L. Effects of 2010;20(11):1711-1717.
short-term alendronate on bone mineral density in haemo-
dialysis patients. Nephrology (Carlton). 2005;10(4):393-399. Accepted: May 08, 2012
© 2012 Società Italiana di Nefrologia - ISSN 1121-8428 455
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- EmotionalIntelligence TestDocument65 pagesEmotionalIntelligence Testjogutierrez100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Lord of The Rings Real HistoryDocument2 pagesThe Lord of The Rings Real HistoryDUNCAN0420No ratings yet
- Red Sea RoadDocument4 pagesRed Sea RoadEthan Gilmore63% (8)
- In Defense of Something Close To BiblicismDocument19 pagesIn Defense of Something Close To BiblicismLiem Sien LiongNo ratings yet
- TMC451 Sample - Skema JWPDocument2 pagesTMC451 Sample - Skema JWPraihana abdulkarimNo ratings yet
- Johnson & Johnson Tylenol CrisisDocument21 pagesJohnson & Johnson Tylenol CrisisArnab Chatterjee100% (2)
- Malacat V CADocument2 pagesMalacat V CAmmaNo ratings yet
- M1 Questions REV SP23Document2 pagesM1 Questions REV SP23Melia MorrisNo ratings yet
- The Hanle Effect and Level Crossing Spectroscopy in RB Vapour Under Strong Laser ExcitationDocument13 pagesThe Hanle Effect and Level Crossing Spectroscopy in RB Vapour Under Strong Laser Excitationdws2729No ratings yet
- HEF4541B: 1. General DescriptionDocument16 pagesHEF4541B: 1. General DescriptionBoniface AsuvaNo ratings yet
- Adjuvant Icotinib Versus Observation in Patients WDocument11 pagesAdjuvant Icotinib Versus Observation in Patients WVanilson BorgesNo ratings yet
- Adjectives and ComparisonDocument38 pagesAdjectives and ComparisonzulosmandNo ratings yet
- Desilvey S Curated Decay Heritage Beyond SavingDocument197 pagesDesilvey S Curated Decay Heritage Beyond SavingNastassjaSimeNo ratings yet
- MA Thesis - Reinhoudt - Translating and Subtitling Wordplay in Disney SongsDocument102 pagesMA Thesis - Reinhoudt - Translating and Subtitling Wordplay in Disney SongsLaura Alzieu100% (1)
- Lesson 3 Foodways Paper Food SculptureDocument13 pagesLesson 3 Foodways Paper Food Sculptureapi-563955428No ratings yet
- Dicision MakingDocument34 pagesDicision MakingArpita PatelNo ratings yet
- Introduction To Engineering EconomyDocument15 pagesIntroduction To Engineering EconomyKetut PujaNo ratings yet
- Abc Chapter 2Document22 pagesAbc Chapter 2ZNo ratings yet
- Concept and Functions of ManagementDocument55 pagesConcept and Functions of Managementrony_phNo ratings yet
- ECE-1007 - Optoelectronics - Digital AssignmentDocument2 pagesECE-1007 - Optoelectronics - Digital Assignmentsnehal100% (1)
- Present Perfect: Task 1.-Regular VerbDocument3 pagesPresent Perfect: Task 1.-Regular VerbV̶̶̶̶̶̶̶̶̶̶͚̝̪͔̞̳͓a̶̶̻n̶̸̶̶̶̶̶̶̶̟͍͍͖͉ͅe̶̶̶̶͙̹͎g̶̶͈ạ̶̶̶̶̝̪s̶̶̶̶̶̶̶̶̙̩̲̮͉̥͞ Bv100% (1)
- Regalia Sales Order v2.2 October 2017Document1 pageRegalia Sales Order v2.2 October 2017Marcus Vinicius Neves GomesNo ratings yet
- Chapter 4 - Wilhelm Wundt and The Founding of Psychology: Dr. Nancy AlvaradoDocument27 pagesChapter 4 - Wilhelm Wundt and The Founding of Psychology: Dr. Nancy AlvaradoAdalene SalesNo ratings yet
- Principles and Practice of Radiation Therapy 3rd Edition Washington Test BankDocument25 pagesPrinciples and Practice of Radiation Therapy 3rd Edition Washington Test BankEricDanielsyksi100% (57)
- French Revision Guide SampleDocument23 pagesFrench Revision Guide SampleSantha GNo ratings yet
- Coping Mechanism IIDocument7 pagesCoping Mechanism IIEllaNo ratings yet
- Basic Résumé Types: 1. Chronological ResumeDocument9 pagesBasic Résumé Types: 1. Chronological ResumeDegee O. GonzalesNo ratings yet
- CBSE Class 2 EVS Our FestivalsDocument3 pagesCBSE Class 2 EVS Our FestivalsRakesh Agarwal100% (1)
- Breaking Down The Barriers: The Gut Microbiome, Intestinal Permeability and Stress-Related Psychiatric DisordersDocument20 pagesBreaking Down The Barriers: The Gut Microbiome, Intestinal Permeability and Stress-Related Psychiatric DisordersCSilva16No ratings yet
- Unit 5 Student EditionDocument30 pagesUnit 5 Student Editionapi-233507392No ratings yet