Professional Documents
Culture Documents
Tendon Transfers For Radial, Median, and Ulnar Nerve Palsy: Review Article
Uploaded by
DavidBeatonComuladaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tendon Transfers For Radial, Median, and Ulnar Nerve Palsy: Review Article
Uploaded by
DavidBeatonComuladaCopyright:
Available Formats
Review Article
Tendon Transfers for Radial,
Median, and Ulnar Nerve Palsy
Abstract
John G. Seiler III, MD Tendon transfers are used to restore balance and function to a
Mihir J. Desai, MD paralyzed, injured, or absent neuromuscular-motor unit. In general,
tendon transfer is indicated for restoration of muscle function after
S. Houston Payne, MD
peripheral nerve injury, injury to the brachial plexus or spinal cord,
or irreparable injury to tendon or muscle. The goal is to improve
the balance of a neurologically impaired hand. In the upper
extremity, tendon transfers are most commonly used to restore
function following injury to the radial, median, and ulnar nerves. An
understanding of the general principles of tendon transfer is
important to maximize the outcome.
T endon transfers are reconstruc-
tive procedures used to restore
the function of injured or nonfunc-
cial for maximizing outcomes. These
principles are as follows:
1. The functional loss associated
tional neuromuscular units. A with the use of donor tendon should
muscle-tendon unit is strategically be minimized to maximize functional
used to replace a nonfunctional unit. gains following transfer. The donor
From Georgia Hand, Shoulder, and
Many of these procedures were first tendon must be expendable so that
Elbow (Dr. Seiler and Dr. Payne)
and the Department of developed to treat the paralytic se- its removal will not result in unac-
Orthopaedics, Emory University quelae of polio. Many techniques ceptable loss of function, and inner-
School of Medicine (Dr. Desai), were refined during World Wars I vation must be intact.1-3
Atlanta, GA.
and II, with fundamental articles 2. The strength of the proposed mus-
Dr. Seiler or an immediate family published in the immediate postwar
member serves as a board member, cle for transfer must be normal or near
owner, officer, or committee member
years.1-4 normal and under voluntary control of
of the American Board of In general, tendon transfers are in- the patient. Typically, the strength of
Orthopaedic Surgery and has stock dicated to restore function after in- the donor muscle-tendon unit decreases
or stock options held in Orthovita.
Dr. Payne or an immediate family jury to the peripheral nerve, brachial by one grade following transfer; there-
member has stock or stock options plexus, spinal cord, tendons, or mus- fore, only donor muscles with 4/5 or
held in BioMimetic Therapeutics. cles. In the setting of nerve injury, a 5/5 strength should be used for tendon
Neither Dr. Desai nor any immediate
variety of surgical alternatives is transfers.5,6
family member has received
anything of value from or has stock available to improve function. Nerve 3. The tendon excursion of the do-
or stock options held in a repair, nerve reconstruction, capsul- nor unit must be sufficient to restore
commercial company or institution odesis, tenodesis, and arthrodesis
related directly or indirectly to the the lost function of the recipient
subject of this article.
performed alone or in combination unit.4 For example, in wrist exten-
with tendon transfer should be con- sion and flexion, there is 33 mm of
J Am Acad Orthop Surg 2013;21:
675-684
sidered. Here, we describe the ten- tendon excursion. Finger extension
don transfers commonly used for re- and flexion has a tendon excursion
http://dx.doi.org/10.5435/
JAAOS-21-11-675
construction following injury to the of 50 mm and 70 mm, respectively.4
radial, median, and ulnar nerves. Wrist flexion and extension can add
Copyright 2013 by the American
Academy of Orthopaedic Surgeons. An understanding of the general 20 to 30 mm of excursion through a
principles of tendon transfer is cru- tenodesis effect.7
November 2013, Vol 21, No 11 675
Tendon Transfers for Radial, Median, and Ulnar Nerve Palsy
Figure 1 is the Pulvertaft weave8 (Figure 1). The
Preoperative Assessment principal disadvantages of this tech-
nique are difficulty in tensioning the
To develop an effective treatment
transfer, slit propagation, and bulk.
plan, a comprehensive history must
Newer techniques such as spiral link-
be obtained and a physical examina-
ing, loop-tendon suture, and lasso pur-
tion focusing on wrist, hand, and fin-
portedly address drawbacks associated
ger ROM as well as motor function
with the Pulvertaft weave.9-11 Biome-
and sensation must be performed to
chanical studies have suggested that
identify any deficits. The skin should
the pull-out strength of these newer
be examined for injury that may af-
techniques is greater, but they result
fect the planned surgical approach.
in a large cross-sectional area for the
Photograph of a cadaver Examination of the peripheral nerve
demonstrating the Pulvertaft weave repair site and are only suitable if the
of the hand includes evaluation of
technique for joining tendons. The increased size of the transfer juncture
donor tendon has been woven
the motor and sensory function of
is acceptable and does not interfere
through the recipient tendon and the radial, median, and ulnar nerves.
with tendon gliding.9-11
joined with a mattress suture. The Sensory function should be deter-
next slit is made at a 90° angle to mined with two-point discrimina-
the first. A minimum of three
weaves is recommended to create tion.
a strong junction.
Radial Nerve Tendon
Transfers
Decision Making
4. The direction of pull (ie, vector) Deficits resulting from injury to the
of the recipient tendon should be in When evaluating a patient for nerve radial nerve are classified as either
line with that of the donor muscle reconstruction, several variables af- high or low radial nerve palsy. Inju-
and, ideally, the transfer should cross fect decision making and the selec- ries located proximal to the elbow
only one joint.1,2 tion of specific surgical treatment al- result in high radial nerve palsy,
5. A single transferred tendon should ternatives. The surgeon must whereas injuries to the posterior in-
perform one intended function.1-3,5 consider the nature of the primary terosseous nerve (distal to the elbow)
6. The soft-tissue bed for the trans- injury, the time from injury, the ex- result in low radial nerve palsy. High
fer must be stable and allow for ten- pected success of any previous treat- radial nerve palsy is associated with
don gliding with pliable, unscarred ment, and the patient’s goals and ex- loss of function of the brachioradia-
overlying skin. Transfers must not be pectations. Electromyography may lis, extensor carpi radialis brevis
placed through heavily scarred soft- be helpful to determine the severity (ECRB), extensor carpi radialis lon-
tissue planes, which limit excur- of the initial injury because sponta- gus (ECRL), extensor digitorum
sion.1,2 neous motor recovery is unlikely communis (EDC), extensor indicis
7. Preoperatively, the joints con- with abnormal electromyography proprius (EIP), extensor digiti min-
trolled by the transferred tendon findings 3 months from the time of imi, extensor carpi ulnaris (ECU),
must have nearly full passive range injury.1 We find it helpful to con- and extensor pollicis longus (EPL).
of motion (ROM). Preoperative oc- struct a table that lists the remaining The motor deficit associated with
cupational hand therapy may be nec- intact function postinjury, the func- high radial nerve palsy results in an
essary to improve ROM before ten- tions needed, expendable muscles inability to extend the wrist and fin-
don transfer. In some cases, joint available for transfer, the sequence of gers at the metacarpophalangeal
release may be necessary before the transfers that can achieve the in- (MCP) joints. The ability to extend
transfer is performed.1,2 tended improvement in hand func- and radially abduct the thumb is
8. Tendons with in-phase functions tion, and adjuvant procedures that compromised as well. On examina-
should be used preferentially. The syn- may be performed. tion, decreased sensation manifests
ergistic action of the proposed muscle as an increased two-point discrimi-
for transfer and the recipient muscle nation or complete anesthesia over
(eg, finger flexors acting in concert with Method of Tendon Suture the dorsum of the first web space
wrist extensors and finger extensors with extension onto the dorsum of
with wrist flexors) can facilitate mus- The traditional method of joining the the thumb, index, and middle fin-
cle retraining after transfer.1-3 donor tendon to the recipient tendon gers. Sensory recovery after radial
676 Journal of the American Academy of Orthopaedic Surgeons
John G. Seiler III, MD, et al
Table 1
Tendon Transfers for Radial Nerve Palsy
Restoration of Wrist Restoration of Thumb Restoration of Finger
Tendon Transfer Extension Extension Extension
Brand1 PT to ECRB PL to EPL FCR to EDC
Jones14 PT to ECRB PL to EPL FCR to EDC
Boyes superficialis2,15 PT to ECRB FDS of ring finger to EPL FDS of long finger to EDC
ECRB = extensor carpi radialis brevis, EDC = extensor digitorum communis, EPL = extensor pollicis longus, FCR = flexor carpi radialis,
FDS = flexor digitorum superficialis, PL = palmaris longus, PT = pronator teres
nerve repair is unpredictable and not tients with isolated radial nerve in- backs of these tendon transfers have
as critical as motor improvement af- jury, muscle-tendon units innervated been debated. The FCR tends to be
ter tendon transfer. Patients present by the median and ulnar nerves can easier to harvest and provides ade-
with wrist drop and may present serve as potential donors for tendon quate excursion and strength with-
with decreased grip strength because transfer. Classic tendon transfer tech- out sacrificing wrist flexion and ul-
the wrist cannot be stabilized in a niques for radial nerve palsy include nar deviation.13 The potential
neutral position or extension to max- the Brand,1 Jones,14 and Boyes super- drawback of using the FCU is the
imize flexor tendon excursion for ficialis2,15 transfers (Table 1). sacrifice of coupled wrist flexion and
grip. ulnar deviation, which is critical for
Low radial nerve palsy is associ- Wrist Extension the dart thrower’s motion and power
ated with the loss of muscle function grip.16
distal to the elbow. In patients with To restore wrist extension, the pro- In the FCR transfer, the tendon is
low radial nerve palsy, the ECRL re- nator teres (PT) tendon is transferred divided at the wrist crease and
tains its innervation, and wrist exten- to the ECRB tendon. The ECRB is routed through the interosseous
sion has substantial radial deviation chosen over the ECRL secondary to membrane or radially around the
because the balancing effect of the its more central insertion onto the forearm. The tendon is attached end-
ECU is absent. Typically, no sensory base of the long metacarpal and bal- to-side and en mass to each of the
deficit is associated with low radial anced radioulnar deviation during EDC tendons. The transfer is set
nerve palsy. wrist extension. A radial mid fore- with the wrist in neutral and the
Tendon transfers for radial nerve arm longitudinal incision is made, MCP joints in full extension, with
palsy restore wrist extension, finger and the PT and ECRB tendons are the FCR tendon at <75% of maxi-
extension at the MCP joint, and ex- identified. The PT tendon and a strip mum tension.2 When the FCU trans-
tension with radial abduction of the of periosteum are harvested from the fer is used, the tendon is harvested
thumb. Timing of radial nerve trans- middle third of the radius. The PT through a generous volar forearm in-
fer depends primarily on the initial muscle-tendon unit is freed from fas- cision, released from its insertion to
management of the radial nerve in- cial connections proximally to maxi- the pisiform, and mobilized proxi-
jury and the potential for recovery. mize tendon excursion. The unit is mally. Because the FCU is a unipen-
The more proximal the nerve injury, then routed radially and woven to nate muscle, it must be released suffi-
the less likely it is that muscle rein- the ECRB tendon with the wrist in ciently to allow for tendon excursion
nervation will occur.4,12 If the nerve is 45° of extension. after transfer. The tendon is passed
still intact, 3 months of observation dorsally around the subcutaneous
are advised to allow spontaneous Finger Extension border of the ulna through a gener-
functional recovery to begin. Patients Finger extension can be restored by ous subcutaneous tunnel and is inset
are reevaluated 6 weeks after injury using a flexor carpi radialis (FCR) to into the EDC tendons proximal to
and, if there is no clinical recovery, EDC tendon transfer (Figure 2). the extensor retinaculum. The recipi-
electrodiagnostic studies may reveal Other tendon transfer options in- ent tendons should be mobilized to
evidence of recovery. In the setting of clude flexor carpi ulnaris (FCU) to establish full or near full tendon ex-
extensive soft-tissue injuries or irrep- EDC and flexor digitorum superfi- cursion and then retracted proxi-
arable nerve injury, early tendon cialis (FDS) of the ring or long finger mally to place the MCP joints into
transfer is often appropriate.13 In pa- to EDC. The advantages and draw- extension. The FCU is passed
November 2013, Vol 21, No 11 677
Tendon Transfers for Radial, Median, and Ulnar Nerve Palsy
Figure 2
Photographs of a cadaver demonstrating the flexor carpi radialis (FCR) to extensor digitorum communis (EDC) tendon
transfer for restoration of finger extension. A, A radial incision is made over the FCR tendon for harvest. The FCR
tendon is divided starting at the wrist crease (B), routed dorsoradially around the forearm (C), and attached end-to-side
and en mass to each of the EDC tendons.
Figure 3 Thumb Extension tong splint. After 4 weeks of immo-
A PL to EPL tendon transfer can be bilization, a new splint is applied to
keep the wrist in 15° to 30° of exten-
performed to restore thumb exten-
sion; the thumb and fingers are free,
sion and radial abduction (Figure 3).
and active ROM is encouraged. At 6
Other options include the transfer of
weeks postoperatively, active ROM
the FDS tendon of the long or ring
of the wrist is allowed and additional
finger to the EPL tendon.2 For a PL
retraining is performed with occupa-
to EPL tendon transfer, the EPL ten-
tional therapy. Strengthening exer-
don is mobilized and can be divided cises begin at 8 weeks postopera-
and removed from the third extensor tively and the splint is discontinued.
Photograph of a cadaver compartment and subcutaneously
demonstrating the palmaris longus Excellent results have been reported
(PL) to extensor pollicis longus routed radially to the volar wrist. We with regard to wrist, thumb, and fin-
(EPL) tendon transfer for prefer to harvest the PL tendon as ger ROM following tendon transfers
restoration of thumb extension. The distal as possible and route it around for radial nerve palsy. In a study of
EPL tendon (held with forceps) is
mobilized, divided, and removed the ulna to the EPL. The transfer is 15 patients with radial nerve palsy
from the third extensor set with the EPL tendon sewn into treated with tendon transfers,
compartment. The PL tendon (held the PL tendon and the thumb in full Ropars et al17 reported a high level
with the hemostat) is harvested as
distally as possible and sewn into extension. of patient satisfaction and excellent
the EPL tendon. In this case, the For sequencing purposes, we dis- wrist, thumb, and finger ROM in 11
flexor carpi radialis (FCR) was sect the recipient tendons to ensure patients.
used to restore finger extension, they are appropriate for transfer. The
and the PL tendon was routed
radially through the same donor tendons are transferred to the
subcutaneous tunnel. new location, and the tension of each Median Nerve Tendon
proposed transfer is examined. Transfers
When possible, we inset the wrist
obliquely through the EDC tendons transfer first and then work down- Median nerve palsy is categorized as
and sewn to each finger’s tendon in- stream to insert the tendon transfers either high or low based on the loca-
dividually at approximately 75% of for finger and thumb extension. tion of the nerve injury. Low median
maximum excursion.2 If this method After the tendon transfers are com- nerve palsy usually results in a loss
is selected, the palmaris longus (PL) plete, the wrist and MCP joints are of thumb opposition, which is a
can be transferred through the same immobilized in extension. We prefer composite motion involving prona-
subcutaneous channel that is used to immobilize the wrist in a pronated tion, flexion, and palmar abduction
for the PL to EPL tendon transfer. and dorsiflexed position with a sugar at the trapeziometacarpal joint and
678 Journal of the American Academy of Orthopaedic Surgeons
John G. Seiler III, MD, et al
Table 2 was necessary in only 14%. for restoration of thumb opposition,
High median nerve palsy second- the Thompson pulley, which uses the
Tendon Transfers for Median
Nerve Palsy ary to an injury proximal to the el- distal end of the transverse carpal
bow joint results in loss of thumb ligament and the ulnar border of the
Restoration of Thumb Opposition palmar fascia,26 and the Guyon canal
(Opponensplasty)
opposition, flexion deficits of the dis-
tal interphalangeal (DIP) and proxi- pulley, which uses tendon graft
EIP to APB (ie, Burkhalter)22
mal interphalangeal (PIP) joints in placed through the canal and a sub-
FDS of ring finger to APB (ie, Royle-
Thompson)23 the index and middle fingers, loss of cutaneous palmar tunnel,27 were as-
thumb interphalangeal (IP) flexion, sociated with the least amount of
PL to APB (ie, Camitz)24
and decreased strength of forearm frictional force.28
Restoration of Thumb Interphalan-
geal Flexion In a Bunnell or Royle-Thompson
pronation. In addition, high median
BR to FPL transfer, the FDS of the ring finger is
nerve palsy can cause a sensory defi-
ECRL to FPL transferred to the APB tendon and a
cit that involves the palmar surface
ECU to FPL Bunnell pulley is used23 (Figure 4).
of the thumb and the index and long
Restoration of Index Distal Interpha- The two slips of FDS are transected
fingers and the radial half of the ring
langeal Flexion between the A1 and A2 pulleys and
finger. Wrist flexion typically re-
ECRL to FDP the tendon is retracted into a wrist
mains intact secondary to the ulnar incision. The Bunnell pulley is cre-
APB = abductor pollicis brevis, innervation of the FCU muscle. ated as described previously. Care is
BR = brachioradialis, ECRL = extensor The goals of tendon transfer are
carpi radialis longus, ECU = extensor taken when routing the transfer to
carpi ulnaris, EIP = extensor indicis restoration of thumb IP flexion, avoid ulnar artery and nerve com-
proprius, FDP = flexor digitorum thumb opposition, and flexion of the
profundus, FDS = flexor digitorum pression. A generous subcutaneous
superficialis, FPL = flexor pollicis longus, index and long fingers. Forearm pro- tunnel is made across the palm, and
PL = palmaris longus nation rarely requires reconstruction the tendon is passed through an inci-
because shoulder motion, the flexor- sion on the radial aspect of the
flexion at the MCP joint.18 Several pronator mass, and brachioradialis thumb, centered over the MCP. One
muscles control the position of the can position the arm to overcome slip of the transfer is attached to the
thumb, and innervation patterns most pronation deficits.21 Median distal radial APB tendon and the
vary. Typically, the adductor pollicis nerve transfers are performed when other is attached to the extensor
(AP) and flexor pollicis longus (FPL) motor recovery is no longer expected hood.29 In a biomechanical study,
muscles are still functional in the pa- following nerve repair or irreparable Cooney et al30 reported a 40% resto-
tient with median nerve palsy. The injury (Table 2). ration of thenar strength with this
flexor pollicis brevis (FPB) muscle transfer.
typically receives dual innervation, Thumb Opposition Burkhalter et al22 first described
with the deep muscle head inner- Several tendon transfers can be used the EIP to APB tendon transfer for
vated by the ulnar nerve. In a study to restore thumb opposition, includ- restoration of thumb opposition.
of the distribution pattern of the me- ing transfer of the EIP, FDS of the The EIP is divided over the index
dian nerve in the palmar region, ring finger, PL, or transfer of the ab- MCP joint and is passed proximally
Olave et al19 found that the median ductor digiti minimi to the APB ten- underneath the extensor retinaculum
nerve innervated the abductor polli- don. In transfers that originate in the (Figure 5). The tendon is routed
cis brevis (APB) muscle, the superfi- forearm, the vector of pull must be around the ulnar side of the wrist,
cial head of the FPB muscle, and the changed to allow opposition. This passed subcutaneously through the
opponens pollicis muscle in 63% of can be achieved by several methods. palm, and attached to the APB inser-
cadaver specimens. The principal The pisiform is optimal for place- tion. The length of this transfer is
motor unit for thumb opposition is ment of a pulley to redirect a tendon usually just sufficient for the purpose
the APB muscle. Because of the ana- for opposition.25 The Bunnell pulley of transfer. In a study of 40 hands
tomic variability in innervation, even uses a half-width thickness of a dis- managed with this technique, Ander-
in the setting of complete low me- tally based portion of FCU tendon son et al31 reported good or excellent
dian nerve injury, patients may retain that is looped and then secured back results in 87.5% of patients, with
thumb opposition. In fact, Jensen20 to itself near the pisiform.23 In a opposition to tip of index or middle
reported that, in 147 cases of injury more recent biomechanical study of finger (“good” result) or to the little
to the median nerve, opponensplasty pulley placement in tendon transfers or ring finger (“excellent” result)
November 2013, Vol 21, No 11 679
Tendon Transfers for Radial, Median, and Ulnar Nerve Palsy
Figure 4 underwent a Camitz transfer, Ter-
rono et al33 reported high patient sat-
isfaction with regard to thumb dex-
terity in 94% of patients.
Following tendon transfer for
thumb opposition, the wrist, thumb,
and MCP joints are immobilized for
4 weeks. The thumb is placed in full
opposition with the wrist slightly
flexed. A fabricated splint is used at
4 weeks postoperatively, and active
ROM begins. Gentle passive ROM
Photographs of a cadaver demonstrating the Bunnell or Royle-Thompson does not begin until 8 weeks postop-
tendon transfer for restoration of thumb opposition. A, The two slips of the eratively.
flexor digitorum superficialis (FDS) of the ring finger are transected between
the A1 and A2 pulleys and the tendon is retracted into a wrist incision. A loop
is made from a half-width thickness of a distally based portion of flexor carpi Thumb and Index Finger
ulnaris (FCU) and is looped and secured to itself near the pisiform. B, A Flexion
generous subcutaneous tunnel is made across the palm, and the tendon is
passed through an incision on the radial aspect of the thumb, centered over In the setting of high median nerve
the metacarpophalangeal joint. One slip of the transfer is attached to the palsy, thumb IP flexion can be re-
distal radial abductor pollicis brevis tendon; the other is attached to the
extensor hood. PL = palmaris longus stored with a transfer of the brachio-
radialis, ECRL, or ECU tendons.27
Using a radial-sided forearm inci-
Figure 5 sion, the brachioradialis tendon is
harvested from its insertion at the ra-
dial styloid process and is woven
into the FPL tendon proximal to the
wrist crease. The transfer is ten-
sioned such that the thumb MCP
and IP joints are in 30° of flexion
with the wrist in a neutral position.
Loss of flexion at the DIP joint of
the index finger adversely affects grip
strength. If ulnar nerve function is
intact, side-to-side tenodesis of the
Photographs of a cadaver demonstrating the extensor indicis proprius (EIP)
to abductor pollicis brevis (APB) tendon transfer for restoration of thumb
flexor digitorum profundus (FDP)
opposition. A, The EIP is divided over the index metacarpophalangeal joint tendons can be performed to restore
and is passed proximally underneath the extensor retinaculum. B, The flexion. This transfer should be set
tendon is routed around the ulnar side of the wrist, passed subcutaneously with the fingers positioned in the
through the palm, and attached to the APB insertion. EDC = extensor
digitorum communis normal flexor cascade. When the
wrist is extended, there is increased
flexion in the digits from radial to ul-
with the IP joint of thumb extended. (Figure 6). An adequate amount of nar. Another option to restore flex-
The Camitz transfer (using the PL palmar fascia must be harvested to ion is an ECRL transfer to the FDP
tendon) was initially described in provide the necessary length for the tendon of the index finger.27 The
1929 and has been traditionally re- transfer. Unlike other transfers for ECRL tendon is tensioned with the
served for patients with long- thumb opposition, the Camitz trans- index finger in full extension and the
standing carpal tunnel syndrome.24 fer only restores palmar abduction of wrist in 30° of flexion.
The PL tendon is harvested with an the thumb secondary to the resultant Following tendon transfers to the
extension of the palmar fascia, vector of pull following surgery.32 In FPL or FDP of the index finger, the
passed subcutaneously to the thumb, a retrospective review of 29 patients wrist, MCP joints, and IP joints are
and attached to the APB insertion with carpal tunnel syndrome who immobilized in 30° of flexion for 4
680 Journal of the American Academy of Orthopaedic Surgeons
John G. Seiler III, MD, et al
weeks. Active ROM is initiated at 4 Figure 6
weeks postoperatively. Strengthening
and passive ROM exercises are be-
gun at 8 weeks postoperatively.
Ulnar Nerve Tendon
Transfers
Ulnar nerve palsy also can be classi-
fied as high or low. Low ulnar nerve
palsy implies injury at the wrist level.
Physical examination reveals intrin-
sic muscle paralysis and sensory loss
Photographs of a cadaver demonstrating the Camitz tendon transfer for
in the ring and small fingers. Intrin- restoration of thumb opposition. The palmaris longus (PL) tendon (dots) is
sic muscle paralysis results in defor- harvested with an extension of the palmar fascia (A), passed subcutaneously
mity, pinch and grip weakness, and to the thumb (B), and attached to the abductor pollicis brevis (APB) insertion.
loss of radioulnar digital motion. In It is important to harvest enough palmar fascia to provide the necessary
length for the transfer. FCU = flexor carpi ulnaris
patients with high ulnar nerve palsy,
the FDP and FCU of the ring and
small finger are paralyzed. Sensation Table 3
is absent in the palmar and dorsal as-
Ulnar Nerve Tendon Transfers for Management of Clawing and Power
pect of the small and ring fingers and Pinch Weakness
the ulnar third of the palm. Tendon
Indication Transfer Description
transfers for management of injuries
to the ulnar nerve are performed Clawing Zancolli lasso 34
FDS of affected finger
when recovery (either spontaneous Modified Stiles-Bunnell35 FDS of long finger to radial lat-
or after nerve repair) is no longer ex- eral band of small and ring
fingers
pected.
Brand36 FCR or ECRB to radial lateral
bands of small and ring fin-
Clawing gers (ulnar nerve palsy) or
Clawing of the ring and small fingers index, long, ring, and small
fingers (combined ulnar and
after injury to the ulnar nerve is median nerve palsy)
caused by an imbalance in muscles Power pinch weak- Adductorplasty ECRB to AP
that affect resting digital posture. In ness
this setting, the intrinsic flexion Adductorplasty FDS of long finger to AP
forces at the MCP joint are absent
(loss of intrinsic hand function), but AP = adductor pollicis, ECRB = extensor carpi radialis brevis, FCR = flexor carpi ulnaris,
FDS = flexor digitorum superficialis
the EDC function remains intact,
creating hyperextension at the MCP
joint. The typical claw hand posture
is caused by hyperextension at the This can be achieved with both cap- Brand transfer36 (Table 3).
MCP joints and reciprocal flexion at sulodesis and tenodesis. Dynamic The Zancolli lasso uses the FDS of
the PIP and DIP joints. Clawing is tendon transfers also prevent MCP the affected finger to restore MCP
not present in the index or long fin- hyperextension by providing a flex- flexion.34 The FDS slips are tran-
ger because the two most radial lum- ion force to the MCP joint or a cou- sected 2 cm proximal to their inser-
bricals are innervated by the intact pled MCP flexion and IP joint exten- tion and harvested between the A1
median nerve. IP joint extension can sion force. The most commonly used and A2 pulleys (Figure 7). The ten-
be accomplished only with the MCP tendon transfers for management of don ends are passed from between
joints in a neutral or flexed position. clawing of the ring and small fingers the A1 and A2 pulleys and sewn
The goal of corrective procedures is are the Zancolli lasso,34 the modified back on themselves proximal to the
to prevent MCP hyperextension. Stiles-Bunnell transfer,35 and the A1 pulley, creating MCP flexion.
November 2013, Vol 21, No 11 681
Tendon Transfers for Radial, Median, and Ulnar Nerve Palsy
Figure 7 Figure 8
Photograph of a cadaver
demonstrating the Zancolli lasso
transfer for management of Photographs of a cadaver demonstrating the modified Stiles-Bunnell tendon
clawing. In the affected finger, the transfer for management of claw hand deformity. A, The lumbrical canal is
slips of the flexor digitorum exposed, revealing the radial lateral band. The slips of the flexor digitorum
superficialis (FDS) are transected superficialis are transected 2 cm proximal to their insertion, split
2 cm proximal to their insertion and longitudinally, and retracted proximally from the tendon sheath. B, The slips
harvested between the A1 and A2 are then routed distally through the lumbrical canal and inserted into the
pulleys. The tendon ends (held with radial lateral bands of the small and ring fingers.
a hemostat) are passed from
between the A1 and A2 pulleys and
sewn back on themselves proximal
to the A1 pulley, creating metacarpal ligament and palmar to the transfer. Tension is set with the wrist
metacarpophalangeal joint flexion. MCP joint axis of rotation) and in- in extension and fingers in an intrin-
serted into the radial lateral bands of sic plus position.
the small and ring fingers. The trans- Once these transfers are complete,
fer is set with the wrist in neutral and the extremity is immobilized in a
Transfer tension is set with the MCP
the ring and small finger MCP joints in short arm dorsal splint with the wrist
joint in approximately 60° of flex-
ion. This procedure can correct claw- 60° of flexion. Like the Zancolli lasso in 30° of extension and the fingers in
ing by providing an intrinsic plus procedure, the modified Stiles-Bunnell an intrinsic plus position. Wrist and
starting position (MCP joint flexion transfer can result in a swan neck de- digital motion is begun after 3 weeks
and the IP joint extension). In a formity. postoperatively, with strengthening
study of 23 digits with isolated nerve In the setting of low median and exercises beginning at 8 weeks. In a
palsy treated with the Zancolli lasso ulnar nerve palsy with clawing of all recent randomized trial, 50 claw
procedure, Hastings and McCollam37 four fingers, the Brand transfer can hand deformities were managed with
reported correction of claw defor- be used to restore intrinsic function either an immediate active motion
mity in 19 digits at an average 5-year using the FCR or ECRB tendon.36 protocol or immobilization.38 Rath
follow-up. One potential drawback The tendon is split into two or four et al38 reported that the immediate
of this procedure is that removal of tails based on the need to restore in- active motion group had earlier pain
the FDS tendon’s influence on PIP trinsic function to the small and ring relief than did the immobilization
flexion can result in postoperative fingers (ulnar nerve palsy) or to the group, with similar outcomes in both
swan neck deformity. small, ring, long, and index fingers groups at final follow-up.
The modified Stiles-Bunnell transfer (ulnar and median nerve palsy). The
uses the FDS tendon of the long finger tendon tails require extension by free Power Pinch
to provide coupled MCP flexion and IP tendon grafts and are passed palmar Power pinch requires that the AP
joint extension.35 The slips of the to the joint axis of rotation for the muscle, the deep head of the FPB
FDS tendon are transected 2 cm MCP joint. The tendon tails are at- muscle, and the first dorsal interosse-
proximal to their insertion, split lon- tached to the radial lateral bands of ous muscle function properly. In the
gitudinally, and retracted proximally the small, ring, and long fingers and patient with normal pinch function,
from the tendon sheath (Figure 8). to the ulnar lateral band for the in- the thumb MCP joint is flexed and
They are then routed distally through dex finger in a fashion similar to that the IP joint is slightly flexed or ex-
the lumbrical canal (deep to the inter- used in the modified Stiles-Bunnell tended. In the patient with low ulnar
682 Journal of the American Academy of Orthopaedic Surgeons
John G. Seiler III, MD, et al
nerve palsy, impaired power pinch by allowing patients to complete ac- 12. Burkhalter WE: Early tendon transfer in
upper extremity peripheral nerve injury.
results in MCP extension and IP hy- tivities of daily living. Clin Orthop Relat Res 1974;(104):68-
perflexion secondary to compensa- 79.
tion by EPL and FPL tendons (Fro- 13. Bevin AG: Early tendon transfer for
ment sign).39 This can be improved References radial nerve transection. Hand 1976;
with either ECRB or FDS adductor- 8(2):134-136.
plasty (Table 3). Evidence-based Medicine: Levels of 14. Jones A: Tendon fixation in
ECRB adductorplasty is appropri- evidence are described in the table of unrecoverable musculo-spinal paralysis.
J Orthop Surg 1919;1:135-140.
ate for patients with low ulnar nerve contents. In this article, reference 38 is
a level I study. References 13 and 16 15. Chuinard RG, Boyes JH, Stark HH,
palsy and impaired power pinch.39
Ashworth CR: Tendon transfers for
The ECRB insertion is detached from are level III studies. References 2, 6, 8, radial nerve palsy: Use of superficialis
the long finger metacarpal base and 11, 12, 14, 15, 17, 20-22, 24-27, 29, tendons for digital extension. J Hand
Surg Am 1978;3(6):560-570.
withdrawn proximally beneath the 31-33, 35, 36, 39, and 40 are level IV
extensor retinaculum. A free tendon 16. Raskin KB, Wilgis EF: Flexor carpi
studies. Reference 5 is level V expert ulnaris transfer for radial nerve palsy:
graft is used to obtain the appropri- opinion. Functional testing of long-term results.
ate length, and the donor tendon is References printed in bold type are
J Hand Surg Am 1995;20(5):737-742.
routed between the second and third 17. Ropars M, Dréano T, Siret P, Belot N,
those published within the past 5 years. Langlais F: Long-term results of tendon
metacarpals and then attached to the
transfers in radial and posterior
AP tendon insertion. In a study of 18 1. Brand PW: Clinical mechanics of the
interosseous nerve paralysis. J Hand Surg
hand. St. Louis, MO, CV Mosby, 1985,
patients with weakened power pinch pp 127-165.
Br 2006;31(5):502-506.
force treated with ECRB adductor- 18. Boatright JR, Kiebzak GM: The effects
2. Boyes JH: Tendon transfers for radial of low median nerve block on thumb
plasty, Smith39 reported a twofold in- palsy. Bull Hosp Jt Dis 1960;21:97-105. abduction strength. J Hand Surg Am
crease in force postoperatively. 1997;22(5):849-852.
3. Bunnell S: Surgery of the Hand.
Transfer of the FDS tendon of the Philadelphia, PA, JB Lippincott, 1944, 19. Olave E, Prates JC, Del Sol M, Sarmento
long finger to the AP tendon can also pp 295-300. A, Gabrielli C: Distribution patterns of
be used to restore power pinch.40 4. Brand PW, Beach RB, Thompson DE: the muscular branch of the median nerve
Relative tension and potential excursion in the thenar region. J Anat 1995;186(pt
The tendon is harvested in a manner 2):441-446.
of muscles in the forearm and hand.
similar to that used for the Zancolli J Hand Surg Am 1981;6(3):209-219. 20. Jensen EG: Restoration of opposition of
lasso procedure and routed proxi- 5. Curtis RM: Fundamental priciples of the thumb. Hand 1978;10(2):161-167.
mally across the palm to the inser- tendon transfer. Orthop Clin North Am 21. Boswick JA Jr, Stromberg WB Jr:
tion of the AP tendon. The need for 1974;5(2):231-242. Isolated injury to the median nerve
above the elbow: A review of thirteen
a free tendon graft for the ECRB ad- 6. Starr CL: Army experiences with tendon
cases. J Bone Joint Surg Am 1967;49(4):
transfers. J Bone Joint Surg Am 1922;
ductorplasty is the primary draw- 4(1):3-7. 653-658.
back of the procedure. Following ad- 22. Burkhalter W, Christensen RC, Brown P:
7. Smith RJ: Tendon Transfers of the Hand
ductorplasty, the thumb and wrist and Forearm. Boston, MA, Little Brown, Extensor indicis proprius
opponensplasty. J Bone Joint Surg Am
are immobilized for 4 weeks, with 1987.
1973;55(4):725-732.
the wrist in neutral or slight flexion. 8. Pulvertaft RG: Tendon grafts for flexor
tendon injuries in the fingers and thumb: 23. Bunnell S: Opposition of the thumb. J
Active ROM is begun at 6 weeks and Bone Joint Surg Am 1938;20(2):269-
A study of technique and results. J Bone
strengthening exercises are initiated Joint Surg Br 1956;38(1):175-194. 284.
at 8 weeks postoperatively. 24. Camitz H: Surgical treatment of
9. Kulikov YI, Dodd S, Gheduzzi S, Miles
AW, Giddins GE: An in vitro paralysis of opponens muscle of thumbs.
biomechanical study comparing the Acta Chir Scand 1929;65:77-83.
spiral linking technique against the 25. Goldner JL, Irwin CE: An analysis of
Summary pulvertaft weave for tendon repair. paralytic thumb deformities. J Bone Joint
J Hand Surg Eur Vol 2007;32(4):377- Surg Am 1950;32(3):627-639.
381.
Tendon transfers are one reconstruc-
26. Thompson TC: A modified operation for
tive option in a ladder of reconstruc- 10. Bidic SM, Varshney A, Ruff MD, opponens paralysis. J Bone Joint Surg
Orenstein HH: Biomechanical Am 1942;24(3):632-640.
tive alternatives that can improve comparison of lasso, Pulvertaft weave,
function after injury to the radial, and side-by-side tendon repairs. Plast 27. Brand PW: Tendon transfers for median
median, or ulnar nerves. By adhering Reconstr Surg 2009;124(2):567-571. and ulnar nerve paralysis. Orthop Clin
North Am 1970;1(2):447-454.
to the general principles of tendon 11. Kim SH, Chung MS, Baek GH, Lee YH,
Lee S, Gong HS: A loop-tendon suture 28. Lee DH, Oakes JE, Ferlic RJ: Tendon
transfers, function can be predictably for tendon transfer or graft surgery. transfers for thumb opposition: A
improved, improving quality of life J Hand Surg Am 2007;32(3):367-372. biomechanical study of pulley location
November 2013, Vol 21, No 11 683
Tendon Transfers for Radial, Median, and Ulnar Nerve Palsy
and two insertion sites. J Hand Surg Am 33. Terrono AL, Rose JH, Mulroy J, transfer in isolated ulnar nerve palsy: A
2003;28(6):1002-1008. Millender LH: Camitz palmaris longus functional evaluation. J Hand Surg Am
abductorplasty for severe thenar atrophy 1994;19(2):275-280.
29. Jacobs B, Thompson TC: Opposition of secondary to carpal tunnel syndrome.
the thumb and its restoration. J Bone J Hand Surg Am 1993;18(2):204-206. 38. Rath S, Selles RW, Schreuders TA, Stam
Joint Surg Am 1960;42(6):1015-1026. HJ, Hovius SE: A randomized clinical
34. Zancolli E: Tendon transfers, in: trial comparing immediate active motion
30. Cooney WP, Linscheid RL, An KN: Structural and Dynamic Bases of Hand with immobilization after tendon
Opposition of the thumb: An anatomic Surgery, ed 2. Philadelphia, PA, JB transfer for claw deformity. J Hand Surg
and biomechanical study of tendon Lippincott Co, 1979, pp 159-206. Am 2009;34(3):488-494,e1-e5.
transfers. J Hand Surg Am 1984;9(6):
777-786. 35. Bunnell S: Tendon transfers in the hand 39. Smith RJ: Extensor carpi radialis brevis
and forearm. Instr Course Lect 1949;6: tendon transfer for thumb adduction: A
31. Anderson GA, Lee V, Sundararaj GD: 106-110. study of power pinch. J Hand Surg Am
Extensor indicis proprius 1983;8(1):4-15.
opponensplasty. J Hand Surg Br 1991; 36. Brand P: Tendon grafting: Illustrated by
16(3):334-338. a new operation for intrinsic paralysis of 40. Tse R, Hentz VR, Yao J: Late
the fingers. J Bone Joint Surg Br 1961; reconstruction for ulnar nerve palsy.
32. Braun RM: Palmaris longus tendon 43:444-453. Hand Clin 2007;23(3):373-392, vii.
transfer for augmentation of the thenar
musculature in low median palsy. J Hand 37. Hastings H II, McCollam SM: Flexor
Surg Am 1978;3(5):488-491. digitorum superficialis lasso tendon
684 Journal of the American Academy of Orthopaedic Surgeons
You might also like
- UE 1 Clavicle FracturesDocument46 pagesUE 1 Clavicle FracturesDavidBeatonComuladaNo ratings yet
- A Proposed Classification of Supracondylar FemurFractures Above Total Knee ArthroplastiesDocument4 pagesA Proposed Classification of Supracondylar FemurFractures Above Total Knee ArthroplastiesDavidBeatonComuladaNo ratings yet
- Matching Nail Angle and Native Neck-Shaft AngleDocument4 pagesMatching Nail Angle and Native Neck-Shaft AngleDavidBeatonComuladaNo ratings yet
- Synergy Hip System-SmallerDocument20 pagesSynergy Hip System-SmallerDavidBeatonComuladaNo ratings yet
- Does Femoral Notching During Total Knee Arthroplasty Influence Periprosthetic Fracture. A Prospective StudyDocument6 pagesDoes Femoral Notching During Total Knee Arthroplasty Influence Periprosthetic Fracture. A Prospective StudyDavidBeatonComuladaNo ratings yet
- Periprosthetic Fractures of The Proximal Femur Beyond The Vancouver ClassificationDocument8 pagesPeriprosthetic Fractures of The Proximal Femur Beyond The Vancouver ClassificationDavidBeatonComuladaNo ratings yet
- The Reliability and Validity of The Vancouver Classification of Femoral Fractures After Hip ReplacementDocument4 pagesThe Reliability and Validity of The Vancouver Classification of Femoral Fractures After Hip ReplacementDavidBeatonComuladaNo ratings yet
- Ankle fractures and syndesmosis injury treatment optionsDocument11 pagesAnkle fractures and syndesmosis injury treatment optionsDavidBeatonComuladaNo ratings yet
- Basic Guitar Chords PDFDocument4 pagesBasic Guitar Chords PDFSamNo ratings yet
- Total Knee Arthroplasty in Osteopetrosis Using Patient-Specific InstrumentationDocument4 pagesTotal Knee Arthroplasty in Osteopetrosis Using Patient-Specific InstrumentationDavidBeatonComuladaNo ratings yet
- Osteoarthritis and Osteopetrosis Treated by Knee ReplacementDocument6 pagesOsteoarthritis and Osteopetrosis Treated by Knee ReplacementDavidBeatonComuladaNo ratings yet
- Osteoarthritis Associated With Osteopetrosis.30Document6 pagesOsteoarthritis Associated With Osteopetrosis.30DavidBeatonComuladaNo ratings yet
- Vahedi2020 PDFDocument4 pagesVahedi2020 PDFDavidBeatonComuladaNo ratings yet
- Vahedi2020 PDFDocument4 pagesVahedi2020 PDFDavidBeatonComuladaNo ratings yet
- Intramedullary Nailing of Periarticular Fractures.2Document11 pagesIntramedullary Nailing of Periarticular Fractures.2DavidBeatonComuladaNo ratings yet
- Rheumatoid Hand and Wrist Surgery Soft Tissue.99323Document9 pagesRheumatoid Hand and Wrist Surgery Soft Tissue.99323DavidBeatonComuladaNo ratings yet
- Total Joint Arthroplasty in Patients With Osteopetrosis: A Report of 5 Cases and Review of The LiteratureDocument6 pagesTotal Joint Arthroplasty in Patients With Osteopetrosis: A Report of 5 Cases and Review of The LiteratureDavidBeatonComuladaNo ratings yet
- Intramedullary Nailing of Femoral Shaft Fractures .4Document10 pagesIntramedullary Nailing of Femoral Shaft Fractures .4DavidBeatonComuladaNo ratings yet
- Prosthetic Joint InfectionDocument21 pagesProsthetic Joint InfectionDavidBeatonComuladaNo ratings yet
- Hamilton 2014Document1 pageHamilton 2014DavidBeatonComuladaNo ratings yet
- Vanhove2014 PDFDocument5 pagesVanhove2014 PDFDavidBeatonComuladaNo ratings yet
- Vanhove2014 PDFDocument5 pagesVanhove2014 PDFDavidBeatonComuladaNo ratings yet
- Primary TKA TechniqueDocument23 pagesPrimary TKA TechniqueDavidBeatonComuladaNo ratings yet
- Vanhove2014 PDFDocument5 pagesVanhove2014 PDFDavidBeatonComuladaNo ratings yet
- Vanhove2014 PDFDocument5 pagesVanhove2014 PDFDavidBeatonComuladaNo ratings yet
- Limb Length DiscrepancyDocument75 pagesLimb Length DiscrepancyDavidBeatonComuladaNo ratings yet
- Osteoarthritis Associated With Osteopetrosis.30Document6 pagesOsteoarthritis Associated With Osteopetrosis.30DavidBeatonComuladaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Lalpath Shruti ThrroidDocument2 pagesLalpath Shruti ThrroidSatish SrivastavaNo ratings yet
- Assignment 2Document2 pagesAssignment 2Rashida ParveenNo ratings yet
- Vasavi Diagnostic Laboratory: Church Road, Chitradurga - 577501Document2 pagesVasavi Diagnostic Laboratory: Church Road, Chitradurga - 577501Vidya kiranNo ratings yet
- Canvas Lab Exercise 12 Cardiovascular SystemDocument3 pagesCanvas Lab Exercise 12 Cardiovascular SystemJamesanne DemetriaNo ratings yet
- ANATOMY AND BIOMECHANICS OF WRIST JOINT FinalDocument43 pagesANATOMY AND BIOMECHANICS OF WRIST JOINT Finalinas ismailNo ratings yet
- HugeDocument36 pagesHugePupoko100% (2)
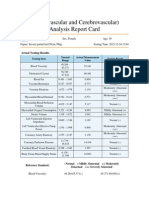
- Cardiovascular and CerebrovascularDocument6 pagesCardiovascular and CerebrovascularJoshelle B. Bancilo0% (1)
- Neuro 2 AnsDocument14 pagesNeuro 2 AnsSantiago AldayNo ratings yet
- How Animals SurviveDocument35 pagesHow Animals SurvivedhonaNo ratings yet
- Copy+of+AM+ +Frog+Dissection+ (Remote)Document21 pagesCopy+of+AM+ +Frog+Dissection+ (Remote)Khosraw HalimiNo ratings yet
- 10th Grade Fitness Assignment Sheet #3 PDFDocument6 pages10th Grade Fitness Assignment Sheet #3 PDFJohn JonesNo ratings yet
- 10 Simple Yoga Poses Height GainDocument11 pages10 Simple Yoga Poses Height GainRajesh GandikotaNo ratings yet
- Planes Systems OrganizationDocument36 pagesPlanes Systems OrganizationR. EssoNo ratings yet
- Activity 1Document3 pagesActivity 1Clarin Perez OrdinarioNo ratings yet
- Spontaneous Regression of Sequestrated Lumbar Disc Herniations - 2014Document6 pagesSpontaneous Regression of Sequestrated Lumbar Disc Herniations - 2014SNNo ratings yet
- Unit 2 Grandrounds Ot ListDocument2 pagesUnit 2 Grandrounds Ot ListBhavvNo ratings yet
- Making Occlusion 2Document7 pagesMaking Occlusion 2Ali QawasNo ratings yet
- Curs 10 MG AN I SEM IDocument34 pagesCurs 10 MG AN I SEM IRusu CristianaNo ratings yet
- Cranial Nerves TableDocument1 pageCranial Nerves TablePIOZRNo ratings yet
- The Slump Test: Examining Spinal Pain and Range of MotionDocument5 pagesThe Slump Test: Examining Spinal Pain and Range of MotionNahu SteinmannNo ratings yet
- Stanford DR Dake MRI MRV Protocol 1.5 TeslaDocument18 pagesStanford DR Dake MRI MRV Protocol 1.5 Teslamarky777100% (1)
- Gait Cycle - Foot & Ankle - OrthobulletsDocument6 pagesGait Cycle - Foot & Ankle - OrthobulletsBOOCOMETRUENo ratings yet
- Neurological Exam of Cats Made SimpleDocument6 pagesNeurological Exam of Cats Made SimplevetthamilNo ratings yet
- MakhaarijDocument18 pagesMakhaarijSalia SoumareNo ratings yet
- 1 The General Plan of PatientDocument7 pages1 The General Plan of PatientcorsairmdNo ratings yet
- Lecture 1 - Development of Respiratory SystemDocument27 pagesLecture 1 - Development of Respiratory SystemRachmad MusyaffaNo ratings yet
- Respiratory System ExplainedDocument6 pagesRespiratory System ExplainedPaulus Villanueva100% (1)
- Head and NeckDocument11 pagesHead and NeckdrsamnNo ratings yet
- Arm Diagram Left - Google Search PDFDocument1 pageArm Diagram Left - Google Search PDFjordanNo ratings yet
- DLL November 21, 2017 - Endocrine GlandsDocument4 pagesDLL November 21, 2017 - Endocrine GlandsHelen Grace Llemos Cabalag100% (2)