Professional Documents
Culture Documents
Performance Checklist in Breasts and Axillae Assessment Skill Rationalization
Uploaded by
Trina Joyce HemedezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Performance Checklist in Breasts and Axillae Assessment Skill Rationalization
Uploaded by
Trina Joyce HemedezCopyright:
Available Formats
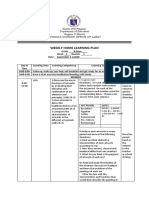
PERFORMANCE CHECKLIST IN BREASTS AND AXILLAE
ASSESSMENT SKILL RATIONALIZATION
1. Gather equipments (centimeter It is easier for the nurses to get the equipments
ruler, small pillow, gloves, needed for the procedure. It will also save time
client handout on breast self- and energy.
examination, and slide for
specimen.
2. Explain procedure to the client. The patient will know what will going t happen in
the procedure. This will reduce the patient’s
anxiety.
3. Ask client to put on a gown. The nurses can easily access the part of
the patient's body being treated.
FEMALE BREASTS
1. Inspect breasts Inspect breast to see if there is infection or
abnormalities.
a. Size and symmetry Breast can be a variety of sizes and are
somewhat round and pendulous. One breast may
normally larger than the other.
b. Color and texture To check if there is redness from local infection or
inflammatory carcinoma.
c. Superficial venous patterns Observe visibility and pattern of breast veins.
d. Retraction and dimpling To inspect for changes or flattening of the normal
convex breast. Ask the patient to raise her arms
over her head, then press her hands against her
hips to contract the pectoral muscles. Inspect the
breast contours carefully in each position.
e. Bilaterally, note color, size, Areolas vary from dark pink to dark brown on the
shape and texture of areolas. patient’s skin tones. They are round and may vary
in size.
f. Bilaterally, note size and Nipples are nearly equal bilaterally in size and are
direction of nipples. in the same location on each breast.
2. Palpate breasts Be sure to palpate every side of the breast, from
nipples, areola to the periphery of the breast
tissue and up into the tail of Spence.
a. Texture and elasticity To know if there is dimples, puckers, bulges or
ridges on the skin of your breast and to know if
there is loss of skin elasticity.
b. Tenderness and temperature To check if there is heaviness, tightness in the
chest, burning in the skin and general soreness.
c. Masses: noting location, size in Palpate carefully for any lumps or mass that is
centimeters, shape , mobility, qualitatively different from or larger than the rest
consistency, and tenderness. of the breast tissue.
d. Palpate nipples by Palpate each nipple, noting its elasticity.
compressing nipple gently Thickening of the nipples and loss of elasticity
between thumb and index suggest an underlying cancer.
finger, observe for discharge.
e. Palpate mastectomy site, if Palpate gently along the scar, these tissues are
applicable, observing the scar may be unusually sensitive. Use a circular motion
and any remaining breast or with two or three fingers.
axillary tissue for redness,
lesions, lumps, swelling or
tenderness
MALE BREASTS
1. Inspect and palpate the Normal male breast has a flat disc of
breasts, areolas, and nipples undeveloped breast tissue beneath the nipple.
for selling nodules or Should be even with no nodules.
ulcerations.
AXILLAE
1. Inspect for rashes or Ask the patient to sit up. Normally there is no
inspection. infection or rashes.
2. Hold the elbow with one hand Use the 3 fingers of your dominant hand and
and use the three fingerpads of reach as high as you can toward the apex of
your other hand to palpate axilla. Warn the patient that this may feel
firmly the axillary lymph nodes. uncomfortable.
3. Palpate high into the axillae, Your fingers should lie directly behind the pectoral
moving downwad against the muscles, pointing toward the midclavicle. Now
ribs to feel for the central press your fingers toward the chest wall of the
nodes. Continue down the axillary nodes, these are the most often palpable.
posterior axillae to feel for the
posterior nodes.
4. Use bimanual palpation to feel To locate if there is any abnormalities or lumps
for the anterior axillary nodes. while doing the procedure.
5. Palpate down the inner aspect To check if there is any lesions or redness
of the upper arm. including bone fractures or joint dislocations
ANALYSIS OF DATA
1. Formulate nursing diagnoses Helps identify nursing priorities and help direct
(wellness, risk, actual) nursing interventions based on identified
priorities. To identify health care needs.
2. Formulate collaborative Collaborative problems using physician-
problems. prescribed and nursing-prescribed interventions.
3. Make necessary referrals. To know if there’s an increased circulation due to
malignancy. An asymmetric venous pattern may
be due to malignancy.
PERFORMANCE CHECKLIST IN HEART & NECK VESSELS
ASSESSMENT SKILL RATIONALIZATION
1. Gather equipment (stethoscope with It is easier for the nurses to get the
bell diaphragm, small pillow, penlight equipments needed for the procedure. It will
or moveable exam light, watch with also save time and energy.
second hand, two centimeter rulers.)
2. Explain the procedure to the patient. The patient will know what will going t
happen in the procedure. This will reduce
the patient’s anxiety.
3. Ask patient to wear gown. The nurses can easily access the part of
the patient's body being treated.
NECK VESSELS
1. Auscultate carotid arteries for bruits. Palpate each carotid artery alternately by
placing the pads of the index and middle
fingers medial to the sternocleidomastoid
muscle on the neck. Note amplitude and
contour of the pulse, elasticity of the artery,
and any thrills.
2. Palpate each carotid artery for This ensures adequate blood flow through
amplitude and contour of the pulse, the other artery to the brain
elasticity of the vessel, and thrills.
3. Inspect for jugular venous pulse. Inspect the jugular venous pulse by
standing on the right side of the client. The
client should be in a supine position with the
torso elevated 30 to 45 degrees. Make sure
the head and torso are on the same plane.
4. Measure jugular venous pressure. Evaluate jugular venous pressure by
watching for distention of the jugular vein. It
is normal for the jugular veins to be visible
when the client is supine; to evaluate jugular
vein distention, position the client in a
supine position with the head of the bed
elevated 30, 45, 60, and 90 degrees.
HEART PRECORDIUM
1. Inspect for visible pulsation (note if With the client in supine position with the
apical or other) head of the bed elevated between 30 and
45 degrees, stand on the client’s right side
and look for the apical impulse and any
abnormal pulsations.
2. Palpate for apical pulse for location, Remain on the client’s right side and ask the
size, strength, and duration of client to remain supine. Use the palmar
pulsation. surfaces of your hand to palpate the apical
impulse in the mitral. After locating the
pulse, use one finger pad for more accurate
palpation
3. Palpate for abnormal pulsation or Use your palmar surfaces to palpate the
vibration at apex, left sternal border apex, left sternal border, and base. No
and base. pulsations or vibrations are palpated in the
areas of the apex, left sternal border, or
base.
4. Auscultate heart sounds for rate and Rate should be 60 to 100 beats per minute
rhythm (apical and radial pulses, with regular rhythm. A regularly irregular
pulse rate deficit, S1 and S2. rhythm, such as sinus arrhythmia when the
heart rate increases with inspiration and
decreases with expiration, may be normal in
young adults. Normally the pulse rate in
females is 5 to 10 beats per minute faster
than in males.
5. Auscultate S1 and S2 heart sounds Auscultate the first heart sound (S1 or “lub”)
for sound locations and with and the second heart sound (S2 or “dubb”).
respiration, splitting of S2. Remember these two sounds make up the
cardiac cycle of systole and diastole. S1
starts systole, and S2 starts diastole. The
space, or systolic pause, between S1 and
S2 is of short duration (thus S1 and S2
occur very close together), whereas the
space, or diastolic pause, between S2 and
the start of another S1 is of longer duration.
6. Auscultate for extra heart sounds Use the diaphragm first then the bell to
(clicks, rubs) and murmurs (systolic auscultate over the entire heart area. Note
or diastolic, intensity grade, pitch, the characteristics of any extra sound heard.
quality, shape, or pattern, location, Auscultate during the systolic pause (space
transmission, effect of ventilation heard between S1 and S2).
and position.
7. Auscultate with the client on the left Ask the client to assume left lateral position.
lateral position and with the client Use the bell of the stethoscope and listen to
stirring up, leaning forward, and the apex of the heart.
exhaling.
ANALYSIS OF DATA
1. Formulate nursing diagnoses Helps identify nursing priorities and help
(wellness, risk, actual) direct nursing interventions based on
identified priorities. To identify health care
needs.
2. Formulate collaborative problems Collaborative problems using physician-
prescribed and nursing-prescribed
interventions.
3. Make necessary referrals. To know if there’s an increased circulation
due to malignancy. An asymmetric venous
pattern may be due to malignancy.
STUDENT'S SIGNATURE: __________________________________
CLINICAL INSTRUCTOR'S SIGNATURE: ______________________
You might also like
- Please Read 1F Simulations Compilations 1Document36 pagesPlease Read 1F Simulations Compilations 1mendozakaceeyNo ratings yet
- Inspection of The Breast: Head-To-Toe Assessment (Q. Breast)Document3 pagesInspection of The Breast: Head-To-Toe Assessment (Q. Breast)emma rose lutellaNo ratings yet
- Rle Week Rationale 1Document4 pagesRle Week Rationale 1julianebauzon14No ratings yet
- Breast Self ExaminationDocument4 pagesBreast Self ExaminationSagar HanamasagarNo ratings yet
- Assessment of The BreastDocument11 pagesAssessment of The BreastSIR ONENo ratings yet
- Module 6 Breast Axilla Assessment-Edited 0 0Document13 pagesModule 6 Breast Axilla Assessment-Edited 0 0Laila PasiganNo ratings yet
- AssesssingDocument20 pagesAssesssingKRISTIAN DRAZEN MIRANDANo ratings yet
- Retdem Checklist: Abdomen Lopez, Marjorie Joy C.: Refer To Picture inDocument4 pagesRetdem Checklist: Abdomen Lopez, Marjorie Joy C.: Refer To Picture inAT4-11 HUMSS 2 CEDRICK ILAONo ratings yet
- LymphaticDocument52 pagesLymphaticlemuel_queNo ratings yet
- Neck Assessment - WPS OfficeDocument20 pagesNeck Assessment - WPS OfficeTricia Denise EstabilloNo ratings yet
- Head and Neck Assessment FindingsDocument4 pagesHead and Neck Assessment FindingsCiara Manguiat100% (1)
- Breast Assessment: Preparing The ClientDocument5 pagesBreast Assessment: Preparing The Clientshannon c. lewisNo ratings yet
- Breast and Axillae AssessmentDocument146 pagesBreast and Axillae AssessmentFaith madayag100% (2)
- Breast Exam: A Systematic ApproachDocument3 pagesBreast Exam: A Systematic ApproachBearaphNo ratings yet
- Head To Toe Physical AssessmentDocument9 pagesHead To Toe Physical Assessmentthe studentNo ratings yet
- Assessment of The Breast: Jonalyn Sotero Esco RN., MANDocument41 pagesAssessment of The Breast: Jonalyn Sotero Esco RN., MANVan MaverickNo ratings yet
- De Veyra Assignment WK 3Document12 pagesDe Veyra Assignment WK 3adrian lozanoNo ratings yet
- Skill - 24-4 Assessing Blood Pressure by AuscultationDocument3 pagesSkill - 24-4 Assessing Blood Pressure by Auscultationshereln.ballNo ratings yet
- Breast Examination: 1. Preparation Health ProviderDocument1 pageBreast Examination: 1. Preparation Health ProviderAufi FillaNo ratings yet
- Assessing The Breasts and Axillae: DelegationDocument4 pagesAssessing The Breasts and Axillae: DelegationVioletteNo ratings yet
- Health Assessment: Tiwonge MunkhondyaDocument27 pagesHealth Assessment: Tiwonge Munkhondyachifunndo charlesNo ratings yet
- Assessing The Thorax and LungsDocument4 pagesAssessing The Thorax and LungsLorenz Jude Cańete100% (2)
- Respiratory Assessment GuideDocument49 pagesRespiratory Assessment GuideArlyn Mendenilla100% (4)
- NCM 112 Skills Lab Cellular AberrationDocument10 pagesNCM 112 Skills Lab Cellular AberrationMeryville JacildoNo ratings yet
- PROCEDURE CHECKLIST FOR BREAST, TESTICULAR AND CERVICAL EXAMSDocument10 pagesPROCEDURE CHECKLIST FOR BREAST, TESTICULAR AND CERVICAL EXAMSjanna mae patriarcaNo ratings yet
- Skills # 8: THE ABDOMEN: Procedure Rationale CXNRDocument3 pagesSkills # 8: THE ABDOMEN: Procedure Rationale CXNRAlyssa Ashley A. ImamNo ratings yet
- MCN Lesson 4Document3 pagesMCN Lesson 4Joeyca Shien PiolNo ratings yet
- Cardiovascular Assessment - RDDocument2 pagesCardiovascular Assessment - RDANGELICA CLAIRE BARECUATRONo ratings yet
- Pa2 and Pa3 2Document14 pagesPa2 and Pa3 2Roger ViloNo ratings yet
- Gynaecology Exam GuideDocument15 pagesGynaecology Exam GuidePraveena MoganNo ratings yet
- Care of Patients With Traction TractionDocument5 pagesCare of Patients With Traction TractionMOHAMMAD JABBER M. PAUDACJRNo ratings yet
- Breast ModuleDocument2 pagesBreast ModuleDasha Vee100% (1)
- 7.0 OFFICE ProceduresDocument8 pages7.0 OFFICE ProceduresJennifer Pisco LiracNo ratings yet
- Leopold'S Maneuver: DefinitionDocument3 pagesLeopold'S Maneuver: DefinitionJyra Mae TaganasNo ratings yet
- Return Demonstration: DocumentationDocument27 pagesReturn Demonstration: DocumentationCarlo De VeraNo ratings yet
- Assessment of Breasts and Lymphatic System - Student's ChecklistDocument3 pagesAssessment of Breasts and Lymphatic System - Student's ChecklistRosette Malenab de Asis0% (1)
- MaternalDocument2 pagesMaternalqweyo yhuNo ratings yet
- Approach To Patient With Breast LumpDocument29 pagesApproach To Patient With Breast Lumpfarah fadzilNo ratings yet
- Cardiovascular (CVS) Examination: Procedure StepsDocument15 pagesCardiovascular (CVS) Examination: Procedure StepsGeorich NarcisoNo ratings yet
- Guide to Chest ExamDocument21 pagesGuide to Chest Examhelen joy cuareNo ratings yet
- Pediatric Musculoskeletal Health TeachingDocument14 pagesPediatric Musculoskeletal Health TeachingcorisNo ratings yet
- Pelvic Examination: W - Newton LongDocument3 pagesPelvic Examination: W - Newton LongyuexinchongNo ratings yet
- Assessment of The Head and NeckDocument10 pagesAssessment of The Head and NeckAngela BaldozaNo ratings yet
- HA Procedures Respi Heart and PeripheralDocument10 pagesHA Procedures Respi Heart and Peripheralako at ang exoNo ratings yet
- W2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsDocument6 pagesW2 - MEDSURG Guidelines For Nursing Interventions On Coma PatientsKyla L. Madjad100% (1)
- Skill: Assessing The Thorax and LungsDocument3 pagesSkill: Assessing The Thorax and LungsAlmira GamaoNo ratings yet
- Stagiaire's Guide To General Surgery OSCEsDocument36 pagesStagiaire's Guide To General Surgery OSCEsMawNo ratings yet
- Equipment Needed: General ConsiderationsDocument5 pagesEquipment Needed: General ConsiderationsJamaica Manuel IglesiasNo ratings yet
- Clinical Breast Exam: A Guide to Technique and FindingsDocument40 pagesClinical Breast Exam: A Guide to Technique and Findingsiron100% (1)
- The Gynaecological ExaminationDocument3 pagesThe Gynaecological ExaminationpogimudaNo ratings yet
- Physical Ass 2Document5 pagesPhysical Ass 2andreabreeNo ratings yet
- Thora Procedure 1Document10 pagesThora Procedure 1E PadzNo ratings yet
- LEOPOLD'S MANEUVER RATIONALE&CHECKLISTDocument3 pagesLEOPOLD'S MANEUVER RATIONALE&CHECKLISTNhadzmae Asmadul IsnainNo ratings yet
- Nursing Abdominal AssessmentDocument5 pagesNursing Abdominal AssessmentPatricia G ChiuNo ratings yet
- Head-Toe AssessmentDocument6 pagesHead-Toe AssessmentLamirah ThomasNo ratings yet
- Cardiovascular Assessment GuideDocument9 pagesCardiovascular Assessment GuideMary Joy Anne LucasNo ratings yet
- Nursing Responsibilities in The Care of Casts Traction FixatorsDocument20 pagesNursing Responsibilities in The Care of Casts Traction FixatorsBasmah A. AdompingNo ratings yet
- NeckDocument2 pagesNeckAlmira GamaoNo ratings yet
- The Heart Is Not A Pump - The Blood Moves The Heart, Not Vice VersaDocument14 pagesThe Heart Is Not A Pump - The Blood Moves The Heart, Not Vice VersagiovacaneNo ratings yet
- CBSE Class 10 Science Chapter 6 Life Processes NotesDocument12 pagesCBSE Class 10 Science Chapter 6 Life Processes NotesAVIRUP DASNo ratings yet
- Systemic Circulation NotesDocument4 pagesSystemic Circulation NotesMHAREY C. ARELLANONo ratings yet
- Valvularheart Diseases: PathophysiologyDocument9 pagesValvularheart Diseases: PathophysiologyVoid LessNo ratings yet
- B1 SyncopeDocument84 pagesB1 SyncopeAnonymous HH3c17osNo ratings yet
- Blood pressure checklistDocument1 pageBlood pressure checklistbethuelNo ratings yet
- Congestive Heart FailureDocument43 pagesCongestive Heart FailuresudersonNo ratings yet
- Bab 1 Normal KGBDocument14 pagesBab 1 Normal KGBukhtianitaNo ratings yet
- Hematology & Immune SystemDocument81 pagesHematology & Immune SystemAmanuel Maru100% (1)
- Format Nota RingkasDocument16 pagesFormat Nota Ringkasmyza_zestyNo ratings yet
- SCIENCE YR 5 (2021) HUMAN CIRCULATORY SYSTEM PART 2 - Google Forms ModulDocument7 pagesSCIENCE YR 5 (2021) HUMAN CIRCULATORY SYSTEM PART 2 - Google Forms ModulwidNo ratings yet
- Blood Gas HandbookDocument112 pagesBlood Gas HandbookNuno Silva100% (1)
- 2607 FullDocument94 pages2607 FullanindiawNo ratings yet
- Circulatory System PDFDocument17 pagesCirculatory System PDFNicole EncinaresNo ratings yet
- Weekly Home Learning Plan: Department of EducationDocument19 pagesWeekly Home Learning Plan: Department of EducationMaya CondeNo ratings yet
- Jayden Glomb Autopsy ReportDocument8 pagesJayden Glomb Autopsy ReportKOLD News 13No ratings yet
- Transportation in Plants and AnimalsDocument7 pagesTransportation in Plants and AnimalsDivyansh JhaNo ratings yet
- Tiki Taka CK CardiologyDocument46 pagesTiki Taka CK CardiologyChristian Jara100% (2)
- How Animals SurviveDocument69 pagesHow Animals SurviveMichael Daryl GalsimNo ratings yet
- Acute Coronary Syndromes: Acute MI and Unstable Angina: Tintinalli Chapter 50 September 20, 2005Document62 pagesAcute Coronary Syndromes: Acute MI and Unstable Angina: Tintinalli Chapter 50 September 20, 2005Jibak MajumderNo ratings yet
- Cardiovascular and Hypertensive Disorders in Pregnancy ExamDocument4 pagesCardiovascular and Hypertensive Disorders in Pregnancy ExamReg LagartejaNo ratings yet
- Modern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDDocument21 pagesModern Management of Cardiogenic Pulmonary Edema: Amal Mattu, MD, Joseph P. Martinez, MD, Brian S. Kelly, MDJoni MokodoNo ratings yet
- F3 Chapter 2 - Blood CirculationDocument3 pagesF3 Chapter 2 - Blood CirculationjayweinxNo ratings yet
- 1ST YEAR ENGLISH, PHYSIOLOGY & ANATOMY OBJECTIVESDocument12 pages1ST YEAR ENGLISH, PHYSIOLOGY & ANATOMY OBJECTIVESTajuddin Mohammed100% (1)
- Diafragma en ICCDocument13 pagesDiafragma en ICCMonserrat CruzNo ratings yet
- Sci 9 LM DRAFT 3.31.2014Document394 pagesSci 9 LM DRAFT 3.31.2014URBIZTONDO, GIAN CARLO M.No ratings yet
- HLTAAP001 Student Assessment Booklet (ID 96973)Document72 pagesHLTAAP001 Student Assessment Booklet (ID 96973)Show Ssti0% (5)
- Blood Supply of The HeartDocument5 pagesBlood Supply of The HeartMohammed EljackNo ratings yet
- Pedal EdemaDocument45 pagesPedal Edemafirdaushassan2112No ratings yet
- Pathophysiology of Birth Asphyxia: Fetal Adaptive MechanismsDocument14 pagesPathophysiology of Birth Asphyxia: Fetal Adaptive MechanismsEduardo Rios DuboisNo ratings yet