Professional Documents
Culture Documents
GYNE 4.05a Bening Ang Malignant Lesions of The Vulva
Uploaded by
Gray SnellOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GYNE 4.05a Bening Ang Malignant Lesions of The Vulva
Uploaded by
Gray SnellCopyright:
Available Formats
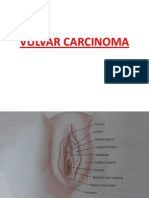
BENIGN AND MALIGNANT LESIONS OF THE VULVA
4.05a
DR. MARIA CRISTINA ESTRELIA-SANTOS 02/22/2017
URETHRAL CARUNCLE
BARTHOLIN’S CYST
Most common large cyst of the vulva
Cystic dilation of an obstructed Bartholin’s gland
Asymptomatic cysts seen in 2% of cases but becomes more
symptomatic as it enlarges
Related to trauma and infection not with STDs
Bartholin’s ducts are lined by transitional epithelium
Small (1-2cm) fleshy outgrowth of the distal edge of the These ducts are easily obstructed, usually near the distal
urethra orifice
Most frequent in postmenopausal women Following obstruction, there is continued secretion of
Initially appears as an eversion of the urethra glandular fluid, which results in the cystic dilation
Aside from ectropion of the posterior urethral wall, it is Usually unilateral, tense and nonpainful
associated with retraction and atrophy of the Treatment:
postmenopausal vagina. o If asymptomatic: no treatment
Growth is secondary to chronic irritation or infection o May become symptomatic due to:
Often secondarily infected, producing ulceration and Size
bleeding When it becomes infected in young
The tissue of the outgrowth is soft, smooth, friable and women less than 40
bright red For acute adenitis without abscess formation: broad
The lesions may be small, single, sessile or pedunculated spectrum antibiotics, frequent hot Sitz baths
Symptoms are variable Treatment of Choice: for a symptomatic cyst or
o Asymptomatic abscess: development of a fistulous tract from the
o Dysuria, frequency, urgency dilated duct to the vestibule (Marsupialization) but if
Point tenderness after contact with undergarments or 40 years old and above do excision biopsy due to
during intercourse risk of Bartholin’s gland carcinoma
Ulcerative lesions produce spotting on contact Simple incision and drainage: has tendency to recur
Differential diagnosis:
o Primary carcinoma of the urethra
o Prolapse of urethral mucosa (mostly in
children)
Diagnosis
o Biopsy under local anesthesia
o Histologically
Transitional and stratified
squamous epithelium with loose
connective tissue
Subdivided into:
o Papillomatous
o Granulomatous
o Angiomatous
Therapy
o Small and asymptomatic lesion:
no treatment needed
o Oral or topical estrogen and avoidance of
irritation: if does not regress or is symptomatic
o Destroy lesion by cryosurgery, laser therapy,
fulguration or operative excision
o After operation, a Foley catheter is left in
place and follow up to prevent urethral
stenosis
URETHRAL PROLAPSE
Seen mostly in children and pre-menarcheal female
Majority asymptomatic but may have dysuria VULVAR CYST
Grossly: Vulvar cysts are either:
o The annular rosette of the friable, edematous, o Epidermal Inclusion Cyst
prolapsed mucosa o Sebaceous Cysts
o It does not have the bright-red color of a Most common small vulvar cysts
caruncle Cannot be differentiated from each other
Therapy:
o Primarily Hot sitz bath and antibiotics
o Estrogen is sometimes effective
o Excision of redundant mucosa may be
needed in some
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 1 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
NEVUS OR MOLE
EPIDERMAL INCLUSION CYST
More frequent than sebaceous cysts
Location:
o Beneath the epidermis Vulvar area
o Commonly on the anterior half of the labia o Makes up only 1% of the skin body surface
majora area
Grossly: o But 5% to 10% of all malignant melanomas
o They are white or yellow cysts arise from this region
o The contents are caseous, thick cheese- like o Estimated that 50% of malignant
o Usually multiple, freely movable, round, slow melanomas arise from a pre-existing
growing, and non-tender, unless infected. nevus
They are firm to shotty in consistency, and contents are Generally asymptomatic
usually under pressure. Most women:
Local scarring of the adjacent skin sometimes occurs o Do not closely inspect their vulvar skin
When rupture of the contents of the cyst produces an o Are unaware of biologic changes in gross
inflammatory reaction in the subcutaneous tissue. appearance of these lesions
Differential Diagnosis for Large epidermal cysts: o Usually recognized when become pigmented
o Fibromas at the time of puberty
o Lipomas Majority of women who develop melanomas are in
o hidradenomas their 50s
May develop following trauma when: Localized nest or cluster of melanocytes
o An infolding of squamous epithelium has Undifferentiated cells that arise from the embryonic
occurred beneath the epidermis neural crest and are present from birth
o In the site of a previous episiotomy or One of the most common benign neoplasms
obstetric laceration Grossly:
o The squamous epithelium which has infolded, o Blue to dark brown to black, but some
continue to produce keratin which is amelanotic
responsible for the caseous, thick cheese-like o Diameter of a few mms to 2 cm
material inside o May either be flat, elevated, or pedunculated
Alternative theories of histogenesis include: Differential diagnosis:
o Embryonic remnants o Hemangiomas
o Occlusion of pilosebaceous ducts of sweat o Endometriosis
glands o Malignant Melanoma
Histology: o Vulvar Intraepithelial Neoplasia
o Characterized by an epithelial lining of o Seborrheic Keratosis
keratinized, stratified squamous Histologically:
epithelium o Lesions are subdivided into: junctional,
o A center of cellular debris that grossly compound, and intradermal nevi
resembles sebaceous material o Junctional activity is common in vulvar nevi
o Most don’t have sebaceous cells or material Many irritants to which vulvar skin is exposed may lead
identified on microscopic examination to malignancy
Treatment: Family history of melanoma is one of the strongest
o Most require no treatment risk factors for the disease.
o However, if the cyst becomes infected Epidemiology
o Treatment consists of local heat application o The lifetime risk of a woman developing
with incision and drainage melanoma from a congenital junctional
o Cysts that become recurrently infected or nevus that measures greater than 2cm in
produce pain should be excised when the diameter is approximately 10%.
acute inflammation has subsided o The lifetime risk of a melanoma forming in
SEBACEOUS CYST women with dysplastic nevi is 15 times that
of the general population.
Clinical features of early malignant melanoma: ABCD
o Asymmetry
o Border irregularity
o Color variegation
o Diameter usually > 6 mm
Indication for Excision biopsy:
o Recent changes in growth or color
o Ulceration
o Bleeding
o Pain
Benign cyst o Development of satellite lesions
Closed sac found just under the skin
Found deeper than the epithelial inclusion cyst DYSPLASTIC NEVUS
Contains pasty- or cheesy-looking skin secretions
made up of keratin (usually yellow discharge)
Most often arise from swollen hair follicles, or as a
result of skin trauma
May grow large, become inflamed and tender
Diagnosis:
o Physical appearance or by excision
Treatment:
o Excision
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 2 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
A nevus > 5mm in diameter
o With irregular borders and patches of
variegated pigment
o Treatment
o Proper excisional biopsy
Three-dimensional
Approximately 5-10mm of normal skin around the
nevus should and underlying dermis be included
Done under local anesthesia
Procedure may be elective or during delivery or
gynecologic surgery
HEMANGIOMA
Purple or dark red papules
With irregular verrucoid surface rarely > 2cm
Occur in women between 30-50 years old
Noted for their rapid growth and tendency to
bleed during strenuous exercise
Treatment: Excisional biopsy
Differential diagnosis:
o Kaposi’s sarcoma
o Angiosarcoma
VENOUS MALFORMATIONS AND LYMPHANGIOMAS
Both are rare
Are rare malformations of blood vessels rather than Venous malformations
true neoplasms o May become symptomatic at any age
Vulvar hemangiomas frequently are discovered initially o Relatively prone to thrombosis
during childhood usually single, 1 to 2 cm in diameter, o Differential diagnosis: Vulvar
flat, and soft, and they range in color from brown to red varicosities
or purple o Treatment:
Diagnosis: Sclerotherapy only after
o Usually established by gross inspection of venography and Doppler
the vascular lesions ultrasound has verified the
Types diagnosis
o Strawberry and Cavernous hemangiomas Different from vulvar varicosities which are
o Senile or cherry angoimas exacerbated with pregnancy and tend to regress
o Angiokeratomas postpartum
o Venous malformations Lymphangiomas
o Lymphangiomas o Similar to hemangiomas but they do not
have red blood cells in the vessels
STRAWBERRY AND CAVERNOUS HEMANGIOMA o There is absence of a muscular layer
Congenital defects discovered in 60% of young around the vascular structures
children in the first years of life Grossly:
May increase in size until age 2 o They present as subdermal multiple, white
Spontaneously regress in size by the time the child or gray, vascular nodules with epithelial
goes to school thickening
Cavernous hemangiomas Treatment: Surgical excision if symptoms develop
o Usually purple in color and vary in size
o The larger lesions extending deeply into the TREATMENT FOR HEMANGIOMAS
subcutaneous tissue Rarely require therapy:
Strawberry hemangioma o Asymptomatic hemangiomas
o Usually bright red to dark red and is o Hemangiomas in children
elevated Subtotal resections in adults:
o Rarely increases in size after age 2 o Initial treatment of large symptomatic
hemangioimas
SENILE OR CHERRY ANGIOMAS that are
bleeding or
infected
Cryosurgery or use of an argon laser to destroy
Hemangioma that is associated with troublesome
Common small lesions that arise on the labia majora bleeding
Usually in postmenopausal women Cryosurgical treatment usually involves a single
Most often < 3mm in diameter, multiple, and red- freeze-thaw cycle repeated three times at monthly
brown to dark blue intervals
ANGIOKERATOMA Excisional biopsy
o When the differential diagnosis is
questionable
o Any bleeding vulvar mass
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 3 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
o Performed for the definitive pathologic Mesenchymal origin
diagnosis Mostly in the labia majora, superficial in location
Surgical removal of a large, cavernous Softer and usually larger than fibromas
hemangioma or may be technically quite difficult Grossly:
PYOGENIC GRANULOMA o Majority of lipomas in the vulva are < 3cm
o With the largest reported weight of 44
pounds
o On cut surface, substance is soft, yellow,
lobulated
Histologically
o Lipomas are usually more homogenous than
fibromas
Do not produce symptoms, unless extremely large
Treatment:
Grow under the hormonal influence of pregnancy, o Excision is usually performed to establish the
with similarities to oral lesions diagnosis
Approximately 1cm in diameter o Smaller tumors may be followed
Differential diagnosis, mistaken clinically for: conservatively.
o Malignant Melanomas
o Basal Cell Carcinomas SKENE’S DUCT CYST
o Vulvar Condylomas
o Nevi
Treatment: Wide and deep excision to prevent
recurrence
FIBROMA
Rare and small cysts
Present with symptoms of discomfort, or found on
routine examination
Secondary to infection & scarring of small ducts
(paraurethral glands)
Location: near the urethra (paraurethral)
Most common benign solid tumors of the vulva Differential diagnosis
Mesenchymal in origin o Urethral diverticula
Has low grade potential for being malignant Physical compression of the cyst should not produce
More frequent than lipomas fluid from urethral meatus
Occur in all age groups In Skene’s duct cyst, the cyst produces fluid upon
Commonly found in the labia majora compression
Arise from deeper connective tissue Treatment
o should be considered as dermatofibromas o If the patient is asymptomatic: none
Smaller fibromas o If Symptomatic
o Firm, asymptomatic, discovered as Excision with careful dissection to avoid urethral
subcutaneous nodules injury
o Becomes pedunculated as size and weight
increase HIDRADENOMA
Larger tumors
o Become cystic after undergoing myxomatous
degeneration
May produce chronic pressure symptoms or acute
pain when they degenerate
Vulvar skin over a fibroma may be compromised by
pressure and ulcerates
Grow slowly, size vary from 1-10 cm in diameter
o With a report of one gigantic vulvar fibroma
which weighed more than 250 pounds a
case report
Grossly: Rare, small, benign vulvar tumor
o Have a smooth surface and a distinct Originates from apocrine sweat glands of the inner
contour surface of the labia majora (38%) and nearby
o On cut surface the tissue is gray-white perineum and labia minora (26%)
Microscopically: Occasionally, from eccrine sweat glands
o Has dense collagen fibers with fat or muscle Discovered in white women between the ages of 30-
cells associated with the interlacing 70, most commonly in the fourth decade of life
fibroblasts Not been reported prior to puberty
o Similar to leiomyomas Grossly:
Treatment o May be cystic (55%) or solid.
o Operative removal if symptomatic and if o With well-defined capsules
the lesion is large o Usually sessile, pinkish-gray nodules with
o Occasionally removed for cosmetic reasons white surface epithelium
LIPOMA o Not > 2cm in diameter
o Occasionally, necrosis of a central indented
area occurs, with a protrusion of reddish-
brown granulation tissue
Confused with pyogenic granulomas
Histologically:
o Because of its hyperplastic, adenomatous
pattern a hidradenoma may be mistaken at
first glance for an adenocarcinoma
On close inspection, however, although there is
glandular hyperplasia with numerous tubular
ducts
Second most frequent benign There is paucity of mitotic figures and a lack of
Slow-growing, circumscribed tumors of fat cells from significant cellular and nuclear pleomorphism
the subcutaneous tissue of the vulva
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 4 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
Generally asymptomatic but may cause pruritus or o Vulvar adenosis – occurs after laser therapy
bleeding if the tumor undergoes necrosis of condylomata acuminata
Biopsy is the treatment of choice. GRANULAR CELL MYOBLASTOMA
SYRINGIOMA
A very rare, cystic, asymptomatic, benign adenoma
of the eccrine sweat glands
Grossly: A rare, slow-growing, solid vulvar tumor originates
o Appear as small < 5 mm subcutaneous from neural sheath (Schwann) cells and sometimes
papules called a schwannoma
o Are either skin-colored or yellow These tumors are found in connective tissues
o May coalesce to form cords of firm tissue throughout the body, most commonly in
o Usually located in the labia majora the tongue, and occur in any age group
Differential Diagnosis: Fox-Fordyce disease Approximately 7% are found in the subcutaneous
tissue of the vulva
Twenty percent are located in the vulva usually in the
labia majora and occasionally involves the clitoris
usually 1 to 5 cm in diameter
benign but characteristically infiltrate the surrounding
local tissue
slow growing, painless tumor but as they grow, they
may cause ulcerations in the skin.
The overlying skin often has hyperplastic changes that
may look similar to invasive squamous cell
o The carcinoma.
most common differential diagnosis Grossly
o Multiple retention cysts of apocrine glands o these tumors are not encapsulated
with inflammation of the skin o cut surface of the tumor is yellow
o Produces intense pruritus Histologically
o Treated by oral or topical estrogens and o irregularly arranged bundles of large, round
topical retinoic acid cells with indistinct borders and pink-staining
Treatment: Excisional biopsy or cryosurgery cytoplasm.
Treatment involves wide excision to remove the
ENDOMETRIOSIS filamentous projections into the surrounding tissue.
o If the initial excisional biopsy is not adequate
and aggressive enough, these benign tumors
tend to recur.
o Recurrence occurs in approximately one in
five of these vulvar tumors.
o tumors are not radiosensitive
VON RECKLINGHAUSEN DISEASE
Vulva is involved in 18% with the benign neural sheath
tumors of von Recklinghausen’s disease
Generalized neurofibromatous and café-au-lait spots
Lesions are fleshy, brownish red, polypoid
Rare, only 1 in 500 women with endometriosis will Treatment
present with vulvar lesions o Excision is the treatment of choice for
Most common location: ovaries symptomatic tumors
The firm, small nodules OTHER ABNORMAL TISSUES PRESENTING AS
May be cystic or solid VULVAR MASSES
Vary from a few millimeters to several centimeters in Differential diagnosis of vulvar masses
diameter Leiomyomas
The subcutaneous lesions are: Squamous papillomas
o Blue, red, or purple, depending on their size, Sebaceous adenomas
activity, and closeness to the surface of the Dermoids
skin Mullerian or wolffian duct remnants
The gross and microscopic pathologic picture is Epidermal inclusion cysts
similar to endometriosis of the pelvis Sebaceous cysts
Usually found at the Mucous cysts
o site of an old, healed obstetric laceration Skin diseases such as seborrheic keratosis,
o Episiotomy site condylomata acuminata, and molluscum
o An area of operative removal of a bartholin’s contagiosum
duct cvst,
The pathophysiology of development of vulvar
HEMATOMA
endometriosis may be secondary to:
o Metaplasia
o Retrograde lymphatic spread
o Potential implantation of endometrial tissue
during operation
Most common symptoms:
Pain and introital dyspareunia
Classic history:
o Cyclic discomfort and an enlargement of the
mass associated with menstrual periods.
Treatment: wide excision or laser vaporization
However, recurrences are common until the woman
reaches menopause
Differential Diagnosis:
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 5 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
Allodynia – pain related to non-painful stimuli
Treatment:
o Topical anesthetics, surgical removal of
skin
CONTACT DERMATITIS
Usually secondary to blunt trauma such as
o A straddle injury from a fall
o An automobile accident
o A physical assault Red, edematous, inflamed skin, weeping eczematoid
Traumatic injuries are reported secondary to a wide vesicles
range of recreational activities Intertriginous areas
o bicycle, motorcycle, skiing, amusement park Treatment
rides o Withdrawal of offending substance
o Spontaneous hematomas are rare o Burrow’s solution
o Usually occur from rupture of a varicose vein o Hydrocortisone
during pregnancy or the postpartum period o Prednisone
Management of non-obstetric vulvar hematomas o Petroleum jelly
o Usually conservative
A pack is placed to promote hemostasis PSORIASIS
o Unless the hematoma is >10cm in diameter
or is rapidly expanding
o Usually venous in origin
o May be controlled by direct pressure
Compression and application of an ice
pack to the area are appropriate therapy
o Operative therapy is indicated
If hematoma continues to expand
In an attempt to identify and ligate the
damaged vessel
Common, generalized, unknown etiology
During the operation careful inspection is performed
Chronic and relapsing
to rule out injury to the urinary bladder and
rectosigmoid Extremely variable and unpredictable course
Marked by spontaneous remissions and
The majority of small hematomas regress with
exacerbations
time
Common areas of involvement are the scalp and
Chronic expanding hematoma has underlying
fingernails
pathophysiology is the repetitive episodes of
Vulvar psoriasis usually affects intertriginous areas
bleeding from capillaries in the granulation tissue of
Manifested by red to red-yellow papules
the hematoma which results in a chronic, slowly
Presence of classic silver scales and bleeding on
expanding vulvar mass
gentle scraping of the plaques may help to
o Treatment is Drainage and Debridement
establish the diagnosis
the scales are less common in the vulva than on other
DERMATOLOGIC DISEASES
areas of the body
Does not involve the vagina
Most common skin diseases involving the vulva May be the first clinical manifestation of HIV
include infection
o contact dermatitis Treatment:
o neurodermatitis o 1% hydrocortisone cream
o psoriasis
o Initial treatment for mild disease
o seborrheic dermatitis
4-week course of a fluorinated
o cutaneous candidiasis
corticosteroid cream ff the patient
o lichen planus
has pain secondary to chronic
Majority of vulvar skin problems are red, scalelike
fissures or a more moderate
rashes
disease
Primary complaint is usually pruritus
If this treatment is not successful, a dermatologist
should be consulted
PRURITUS
Intense itching, desire to scratch, “itch-scratch SEBORRHEIC DERMATITIS
cycle” Rare, etiology unknown
Management Grossly:
Establish diagnosis and treat offending cause o Pale to yellow-red erythematous, edematous
Improve local hygiene lesions with oily scales
Itch-scratch cycle must be interrupted before Treatment: Hydrocortisone cream
condition becomes chronic
Resulting in lichenification (lichen simplex chronicus) LICHEN PLANUS
VULVODYNIA
Chronic vulvar discomfort, burning, stinging, and
rawness
VULVAR VESTIBULITIS
Unknown etiology
Pain and burning at introitus
but not inflammation
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 6 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
VIN III – Severe (CIS)
Paget’s disease
Melanoma in situ
SQUAMOUS CELL HYPERPLASIA
Chronic eruption of shiny, violaceous papules
Involves inner aspects of the vulva
Etiology: Local autoimmune cell mediated response
Symptoms: Pruritus & pain, burning, scarring
Diagnosis: small punch biopsy
Treatment: topical steroid cream
VULVAR CANCER
3-5% of female genital tract malignancies
Fourth in ranking among Female Genital Tract
cancers
Most common is cervix
2nd most common: ovary
3rd most common: uterus Elongation and widening of the rete ridges
o Think, COUV Hyperkeratotic surface layers
90% of vulvar cancers are Squamous cell CA Grossly: whitish or reddish
Disease of older women (60 years)
Increase in vulvar intraepithelial neoplasia (VIN) and LICHEN SCELROSUS
invasive vulvar CA (<50 years)
Prognosis: good if found early
Premalignant & malignant changes arise at
multifocal points on the vulva
o May arise from carcinoma in situ
However, many cases develop in the absence of
premalignant changes
Significant impact on sexuality
Advances in management:
More conservative surgery and improved
psychosexual outcomes Whitish change in vulvar skin
Early detection and biopsy of any abnormal vulvar Epithelium becomes markedly thinned with loss or
lesions are imperative blunting of the rete ridges
Diagnose early stages “cigarette paper” appearance
Improve subsequent morbidity and mortality In some, thickening or hyperkeratosis of the surface
PREDISPOSING FACTOR layer
Well defined predisposing factors are not identified 4.5% risk of developing into vulvar CA (HPV-negative)
Many cases, develop in the absence of premalignant Usually clitoral in location
lesions Some developed malignancies in the cervix, colon,
Occasionally, invasive CA arises from CA-in-situ breast, ovary, and endometrium
PREDISPOSING FACTORS FOR VULVAR CANCERS “Itch-Scratch-Lichen Sclerosus Hypothesis”
o Severe pruritus leads to Squamous cell
o Human Papilloma Virus
hyperplasia progression of SCH leads to
Evidence based link to Vulvar CA
atypia formation
HPV DNA-associated CA were
o Atypia leads to VIN then to invasive
found in younger patients
squamous cell cancer
HPV-positive tumors associated
Aggressive evaluation and treatment has a dramatic
with VIN, warty of basaloid, and
impact on the incidence of vulvar cancer
good prognosis
Treatment with topical steroids would prevent vulvar
HPV-negative is associated with
cancer upon prevention of scratching
keratinized lesion, more like to recur
and lead to death and has poorer
prognosis
o Granulomatous disease of the vulva
o Hypertension
o Diabetes Mellitus
o Obesity – 25% of patients
Recently, pre-malignant lesions have increased in
women in 20-30s Hyperkeratosis of the epithelium
o Multiple sexual contact VULVAR INTRAEPITHELIAL NEOPLASIA
o Venereal diseases (i.e. HPV)
o Immunosuppression
There is also increasing frequency in those treated for
squamous cell CA of the cervix or vagina due to
increased carcinogenesis in the squamous epithelium
of the lower genital tract
Age
>50% 65-75 y.o.
15% <40 y.o.
2% to 21% < 50 y.o
incidence has increased
from over the past 20
years
40-55 years old: carcinoma in situ
VULVAR ATYPIA
Squamous cell hyperplasia Loss of maturation in squamous epithelium
Lichen sclerosus Microscopic features:
Intraepithelial Neoplasia/ Dysplasia o Multinucleated cells
VIN I – Mild o Abnormal mitoses
VIN II – Moderate o Increased density in cells
o Increase NC ratio
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 7 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
Classification Biopsy
o Mild (VIN I) involve lower third of the o Keyes dermal punch
epithelium o No gross features are diagnostic of
o Moderate (VIN II) ½ to 2/3 of epithelium is vulvar cancer
involved o Done on any suspicious lesions of
o Severe (VIN III) over 2/3 involved the vulva, asymptomatic or
Carcinoma In Situ symptomatic
o Full thickness of epithelium o Full thickness of the skin is incised
VIN is a premalignant finding o For 3-5mm lesions
More than 1/3 of vulvar CA are associated with VIN Done under local anesthesia
VIN tends to be multifocal and regress in majority Rotated downward to obtain a
Risk of progression is higher in old and disk of entire thickness
immunosuppressed Indications for biopsy (PIC-C)
Risk of invasion is higher among raised lesions with Persistent ulceration
irregular surface patterns Itchy area
Increased prevalence in young associated with HPV Confluent, wart-like mass
subtype 16, 18 Change in the color, elevation, or
A study evaluated tissue samples from 48 patients surface of a lesion
Age: 45-88 y.o. MANAGEMENT OF VULVAR ATYPIAS
48% - HPV DNA was detected by PCR Relief of itching
95% - HPV subtypes 16 and 18 o Topical corticosteroids
HPV detection was not associated with age o 1% hydrocortisone
71% - associated with coexisting severe (VIN III) To avoid vulvar contraction due to long-term
corticosteroids
PAGET’S DISEASE o Cotton underclothes
o Avoid strong soaps and detergents
o Burrow’s solution
Lichen Sclerosus
o Topical testosterone OD or BID
o Side effects: clitoral hypertrophy and
increase hair growth
o Local Progesterone
o Surgical excision :severe contracture in
the posterior fourchette
Rare intraepithelial disorder HPV INFECTION
Resemble Paget’s disease of the breast HPV 6, 11 – benign warts
Paget’s Cells HPV 16, 11, 31, 33, 35, 45 – VIN
o Large pale cells that often occur in nests 80% of women 50 years old have acquired HPV at
and infiltrate upward through the some point in their life
epithelium 2/3 had pruritus and dyspareunia
Major importance: Complicated management because:
Associated with invasive adenocarcinoma of the o It is extremely prevalent
vulva, vagina, anus, and distant sites (bladder, cervix, o Risk of progression to VIN is small
colon, stomach, and breast) Best to restrict therapy to individuals with bothersome
Tends to spread occulty symptoms such as warts and VIN
Recurrences are frequent after treatment Asymptomatic (koilocytosis) – no treatment but
Usually seen in post-menopausal women requires follow up
Diffuse erythematous eczematoid lesion VAGINAL INTRAEPITHELIAL NEOPLASIA
Itching is a problem Treating itching and dyspareunia
Frequent association with carcinoma VIN lesions tend to be posterior
o Squamous CA of vulva or cervix o predominantly in the perineal area
o Adenocarcinoma of sweat glands of Wide local excision
vulva Risk of recurrence 50% if margins were involved
o Bartholin’s gland CA 10% risk of recurrence if margins not involved
o Adenocarcinoma of breast and GIT Recurrence may occur even if margins are clean, so
long term follow-up is mandatory
CO2 LASER
CLINICAL PRESENTATION OF VULVAR ATYPIAS
Vulvar condyloma and VIN
Irritation or itching most common Vulvar CIS treated successfully
Whitish change due to thickened keratin layer Mandatory to do colposcopy and biopsy in the
Lichen sclerosus diagnosis of the lesions
o Diffuse lesions VIN lesions require slightly deeper ablation, about 1-3
o Skin appears thin, with scarring and mm deeper for areas with hair
contracture, fissuring, excoriation Washing lesions with 5% acetic acid can aid in
o Cigarette paper appearance identifying the involved areas
Squamous hyperplasia Eradication of abnormal vulvar tissue and healing
o Focal or multifocal without scarring
o Vulva is thickened Vaporization of skin that is too deep causes scarring
VIN Effective in a single treatment in 78.4% of cases
o white, red, or pigmented 96.8% cure with second laser treatment for multiple or
Carcinoma In Situ large lesions and those with recurrent VIN
o 1/3 with CIS present with pigmented lesions Healing is usually complete within 2 weeks
o Lesions are discrete and multifocal Good result if used with other vulvar lesions
o Occur more frequently in those who have o Molluscum Contagiosum
had squamous cell neoplasia of the cervix o Lichen Sclerosis Atrophica
Paget’s disease
o Chronic Vestibulitis
o Reddish eczematoid lesions o Other Dermatologic Lesions
DIAGNOSTICS Postoperative pain following laser treatment can be
Pap smear severe
o Not helpful because vulvar skin is thick o Local treatment with lidocaine gel
and keratinized o Stronger analgesics
o May help if there is ulceration o Local care with sitz baths
Colposcopy
o Not used for routine vulvar examination PAGET’S DISEASE
o Used for those who are being followed
Wide local excision if no malignancy found
for vulvar atypias
Long follow-up
o 3% acetic acid highlights whitish areas
Annual breast exam, Pap smear, screening for GIT
for biopsy
disease
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 8 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
MALIGNANT LESIONS
SYMPTOMS
Long history of pruritus – most common
Vulvar bleeding
Discharge
Dysuria
Pain
SIGNS
Vulvar lump or mass – most common
large, fungating mass – rare
CLINICAL FEATURES
Lesion usually raised, fleshy, ulcerated, leukoplakic,
or warty in appearance
Unifocal and occur on the labia majora
5% - multifocal
Labia minora, clitoris, or perineum may be primary
sites
SCREENING
Any vulvar lesion must be thoroughly evaluated to
rule out malignancy
Routine annual visual inspection of the external
genitalia even if the patient is no longer receiving
annual Pap smears
Teaching female patients about vulvar self-
examination
HISTOLOGICAL TYPE
Squamous cell carcinoma -90% Malignant schwannoma
Sarcomas Melanoma -2-9%
o Leiomyosarcoma Bartholin’s gland carcinoma
o Epithelioid sarcoma Adenocarcinoma
o Rhabdomyosarcoma Basal cell carcinoma
Lymphoma Verrucous carcinoma -often
Endodermal sinus tumor misdiagnosed as condyloma TREATMENT
Merkel cell carcinoma acuminata Microinvasive Carcinoma
Dermatofibrosarcoma o Wide excision with 1-2cm margin
protuberans o Hemivulvectomy
o Lymph node dissection may be deferred
Surgical resection -gold standard
CANCER SPREAD Should completely remove the cancer and identify the
extent of disease
Lymphatic embolization Direct extension Determine the stage and the need for additional
o Inguinal lymph nodes Hematogenous spread therapy
o Femoral lymph nodes to distant sites Radical vulvectomy with bilateral dissection of the groin
o Pelvic lymph nodes and pelvic nodes was recommended
o External iliac nodes Presently, more individualized and conservative
approach
Lymph node metastasis – 30% overall
Middle of either labium drain initially to ipsilateral
femoral-inguinal nodes
98% ipsilateral spread
2% contralateral spread
In clitoral or urethral areas spread to either side
Risk increases as the stage of disease, size of the
lesion, and depth of invasion increase Radical vulvectomy or a radical local excision
Pelvic node metastases are uncommon – 2-12% o Aim: to remove the primary lesion with a 2-3
Usually not found in the absence of clinically cm margin
suspicious inguinal and femoral nodes
25% with groin node metastases have positive
pelvic nodes
PROGNOSIS
Related to stage, lesion size, lymph node status
Lymph node involvement and size:
42% if lesion > 2cm
19% if lesion ≤ 2cm
Five-year survival by stage of disease and lymph
node status
Stage I 98% Inguinal-femoral lymphadenectomy
Stage II 85% o Treat deep pelvic nodes with external radiation
Stage III 74% o If >2 groin nodules are positive or there are clinically
Stage IV 31% suspicious groin nodules
Additional predictors of positive nodes: o Do postoperative groin and pelvic radiation therapy
o Tumor de-differentiation Recurrence in the groin
o Suspicious, fixed or ulcerated lymph
o Appears to represent persistent disease
nodes
o Occurring early and near the treated site among
o Capillary-lymphatic space involvement
patients treated conservatively
o Older age
Risk of recurrent disease increases with the number
o Tumor thickness
of positive groin nodes
STAGING Local recurrences
Repeat surgical excision
Radiation therapy with surgery
o To treat groin recurrence
Chemotherapy
o For systemic metastasis
o Poor response rates
o Ineffective in the treatment of recurrent disease
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 9 of 11
GYNECOLOGY
BENIGN AND MALIGNANT LESION OF THE VULVA
BARTHOLIN’S GLAND CARCINOMA o Flat or ulcerated, nodular surrounding the
Adenocarcinoma primary lesions
1-2% of vulvar carcinomas Treatment: Wide Excision
Sign: Prognosis:
o Enlargement of the Bartholin’s gland in a o 5-year survival – 71%
postmenopausal patient o For nodular melanoma – 38%
The American Joint Committee on Cancer (AJCC)
Treatment: TNM classification system and the International
o Radical vulvectomy with bilateral Federation of Gynecology and Obstetrics (FIGO)
inguinal-femoral lymphadenectomy staging system for vulvar cancer
Prognosis is good if nodes are negative
BASAL CELL CARCINOMA REVIEW QUESTIONS
Can arise in the vulva and any skin on the body 1. What is the treatment for Bartholin’s cyst carcinoma?
2% of vulvar carcinomas 2. What is the treatment for microinvasive carcinoma?
Sign: ulcerated lesion 3. What is the classification of VIN if it involves more than
Treatment: wide local excision 2/3 of the epithelium?
If surgical resection margins are free of tumor, the 4. Slow-growing, circumscribed tumors usually larger
disease is cured than fibroma and does not present with pressure
VERRUCOUS CARCINOMA symptoms?
Special variant of squamous cell cancer 5. There is already extension of tumor to the perineal
Sign structures. What is the stage of the tumor?
o Large condylomatous mass on the vulva 6. What is the management for lichen sclerosus if there is
Histopath: already severe contracture in the posterior fourchette?
o Mature squamous cells 7. What are the indications for biopsy of vulvar lesions?
o Extensive keratinization with nests that 8. What is the initial treatment for the cigarette paper
invade the underlying vulvar tissue appearance lesion of the vulva?
Treatment: Wide excision 9. What is the most common symptom of malignant lesion
MELANOMA of the vulva?
10. This tumor originates from the neural sheath.
Most frequent non-squamous cells malignancy of
the vulva
5% of vulvar cancers
Arise from junction or compound nevi
Age: 50 years
Grossly,
o Brown, black or blue-black masses
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 10 of 11
BENIGN AND MALIGNANT LESIONS OF THE VULVA
4.05a
DR. MARIA CRISTINA ESTRELIA-SANTOS 02/22/2017
TRANSCRIBERS: GyneGirls (GG) - AGUIRRE, TAAN Page 11 of 11
You might also like
- GYNE 4.02 - Lower and Upper Genital InfectionDocument12 pagesGYNE 4.02 - Lower and Upper Genital InfectionGray Snell100% (1)
- Benign Gynecologic Lesions FinalDocument11 pagesBenign Gynecologic Lesions Final2012100% (4)
- Gyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesDocument8 pagesGyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesVon HippoNo ratings yet
- Benign Gynecologic Lesions: Urethral Caruncle, Cyst, Nevus, Hemangioma, Fibroma, Lipoma, Endometriosis, Urethral DiverticulumDocument158 pagesBenign Gynecologic Lesions: Urethral Caruncle, Cyst, Nevus, Hemangioma, Fibroma, Lipoma, Endometriosis, Urethral DiverticulumArianne Joy C. TamarayNo ratings yet
- Benign Gynecologic TumorsDocument57 pagesBenign Gynecologic TumorsDexter IanNo ratings yet
- GYNE 4.01a EndometriosisDocument4 pagesGYNE 4.01a EndometriosisGray SnellNo ratings yet
- GYNE 4.06-Benign and Malignant Lesions of UterusDocument7 pagesGYNE 4.06-Benign and Malignant Lesions of UterusGray SnellNo ratings yet
- Benign and Malignant Cervical LesionsDocument46 pagesBenign and Malignant Cervical LesionsRohitNo ratings yet
- GYNE 4.01b InfertilityDocument4 pagesGYNE 4.01b InfertilityGray SnellNo ratings yet
- GYNE 4.04 Pelvic Organ DisordersDocument7 pagesGYNE 4.04 Pelvic Organ DisordersGray SnellNo ratings yet
- GYNE 4.03 Urinary IncontinenceDocument7 pagesGYNE 4.03 Urinary IncontinenceGray SnellNo ratings yet
- Phyllodes TumorDocument20 pagesPhyllodes TumorManuela KarinaaNo ratings yet
- (Gyne) 2.1 PCOS, Hyperandrogenism & Hyperprolactenemia (OnaCruz) - WiniDocument10 pages(Gyne) 2.1 PCOS, Hyperandrogenism & Hyperprolactenemia (OnaCruz) - WiniDexter IanNo ratings yet
- Internal Medicine - Nephrology Lecture on Cystic Kidney DiseasesDocument3 pagesInternal Medicine - Nephrology Lecture on Cystic Kidney DiseasesVon HippoNo ratings yet
- Pathology 5.05b Vagina and Vulva - DR - Dy (Final Edit)Document11 pagesPathology 5.05b Vagina and Vulva - DR - Dy (Final Edit)Dranreb Berylle MasangkayNo ratings yet
- Benign Gyne LesionsDocument133 pagesBenign Gyne LesionsJulie Ann ValenciaNo ratings yet
- (DERMA) 03 TineasDocument9 pages(DERMA) 03 TineasJolaine ValloNo ratings yet
- Surgical Oncology and Breast BiopsyDocument12 pagesSurgical Oncology and Breast Biopsybo gum parkNo ratings yet
- Breast CancerDocument4 pagesBreast CancerMaikka IlaganNo ratings yet
- 1 GYNE 7 - EndometriosisDocument6 pages1 GYNE 7 - EndometriosisIrene FranzNo ratings yet
- Gyne ReflectionDocument18 pagesGyne ReflectionKC Dela RosaNo ratings yet
- Infertility: Dr. Carolina Paula C. MartinDocument6 pagesInfertility: Dr. Carolina Paula C. MartinMaikka IlaganNo ratings yet
- Malignant Tumors of Uterus: DR Tahira RizwanDocument52 pagesMalignant Tumors of Uterus: DR Tahira RizwanSadia YousafNo ratings yet
- (SURG) 5.4b Management of Soft Tissue SarcomaDocument6 pages(SURG) 5.4b Management of Soft Tissue SarcomaKenneth TorresNo ratings yet
- Clinicopathologic Case Presentation of Uterine MassDocument47 pagesClinicopathologic Case Presentation of Uterine Massvicheryl100% (1)
- GYNE 4.08 Benign and Malignant Lesions of The CervixDocument9 pagesGYNE 4.08 Benign and Malignant Lesions of The CervixGray SnellNo ratings yet
- Medical and Surgical Management: of Uterine LeiomyomasDocument78 pagesMedical and Surgical Management: of Uterine LeiomyomasMarthinKolelupunNo ratings yet
- GYNECOLOGY - 2.8 B&M Lesions of The OvariesDocument6 pagesGYNECOLOGY - 2.8 B&M Lesions of The OvariesAngela CaguitlaNo ratings yet
- Hormone Regulation of the Menstrual CycleDocument8 pagesHormone Regulation of the Menstrual CycleRj PolvorosaNo ratings yet
- EUOGS OSCE Booklet 2020Document26 pagesEUOGS OSCE Booklet 2020Amanda Leow100% (1)
- Gynecology: Recurrent Pregnancy LossDocument6 pagesGynecology: Recurrent Pregnancy LossDawn Marco100% (1)
- Gestational Trophoblastic Disease: (Hydatidiform Mole)Document12 pagesGestational Trophoblastic Disease: (Hydatidiform Mole)Gylle Marie PlazaNo ratings yet
- Pelvic Examination: W - Newton LongDocument3 pagesPelvic Examination: W - Newton LongyuexinchongNo ratings yet
- National Board of Examinations Dated: 19 April 2018: Question Paper For NEET-SSDocument6 pagesNational Board of Examinations Dated: 19 April 2018: Question Paper For NEET-SSrajvolgaNo ratings yet
- Polycystic Kidney DiseaseDocument9 pagesPolycystic Kidney DiseaseCésar Aguilar ContrerasNo ratings yet
- EndometriosisDocument7 pagesEndometriosisIsabel CastilloNo ratings yet
- Female Genital TractDocument5 pagesFemale Genital Tractsarguss14100% (1)
- Gynecology Notes Legal Issues and EthicsDocument19 pagesGynecology Notes Legal Issues and EthicsUsm LeeNo ratings yet
- Uterinefibroids 130120064643 Phpapp02Document73 pagesUterinefibroids 130120064643 Phpapp02Tharun KumarNo ratings yet
- Examination of Breast Lump PDFDocument2 pagesExamination of Breast Lump PDFDanaNo ratings yet
- (Surg2) 5.3 Urology Part 2 - Dr. YusiDocument19 pages(Surg2) 5.3 Urology Part 2 - Dr. YusiAlloiBialbaNo ratings yet
- HerniaDocument5 pagesHerniasarguss14100% (5)
- Breast Cancer PowerpointDocument13 pagesBreast Cancer PowerpointCara DeaNo ratings yet
- Adnexal Masses - Ovarian Cysts (2008)Document23 pagesAdnexal Masses - Ovarian Cysts (2008)Michelle Fynes100% (1)
- Vaginal Delivery Section 8Document86 pagesVaginal Delivery Section 8Justine MembridoNo ratings yet
- FIGO Cancer Report 2018 PDFDocument128 pagesFIGO Cancer Report 2018 PDFAndi Tiara S. AdamNo ratings yet
- Student'S Gynaecology Notes: For Students, by StudentsDocument45 pagesStudent'S Gynaecology Notes: For Students, by StudentsAdli IsmailNo ratings yet
- Management of CA Vulva 2Document33 pagesManagement of CA Vulva 2api-3705046No ratings yet
- Premalignant Lesions of The CervixDocument22 pagesPremalignant Lesions of The Cervixkaren carpioNo ratings yet
- Surgical Anatomy of The Chest Wall, Pleura, and MediastinumDocument8 pagesSurgical Anatomy of The Chest Wall, Pleura, and MediastinumNooneNo ratings yet
- Vulval CaDocument54 pagesVulval CaChethana BhatNo ratings yet
- Medicine 6.1b Approach To Cancer Patients - FernandoDocument7 pagesMedicine 6.1b Approach To Cancer Patients - FernandoAbigail LausNo ratings yet
- Congenital Anomelies of Reproductive OrgansDocument47 pagesCongenital Anomelies of Reproductive Organsdr_shamimrNo ratings yet
- Uterus NeoDocument11 pagesUterus NeoHester Marie SimpiaNo ratings yet
- Pediatric Surgery Dr. A. IgamaDocument6 pagesPediatric Surgery Dr. A. IgamaMarco Paulo Reyes NaoeNo ratings yet
- Ovarian Tumor: Obstetrics & GynecologyDocument37 pagesOvarian Tumor: Obstetrics & GynecologyFathimathNo ratings yet
- Different Pathologies of The UterusDocument74 pagesDifferent Pathologies of The UterusAmal100% (1)
- Basic Investigation of An Infertile CoupleDocument53 pagesBasic Investigation of An Infertile CoupleRemelou Garchitorena AlfelorNo ratings yet
- GYNE 4.08 Benign and Malignant Lesions of The CervixDocument9 pagesGYNE 4.08 Benign and Malignant Lesions of The CervixGray SnellNo ratings yet
- GYNE 4.07 Benign and Malignant Lesions of The Ovaries and Fallopain Tubes PDFDocument9 pagesGYNE 4.07 Benign and Malignant Lesions of The Ovaries and Fallopain Tubes PDFGray SnellNo ratings yet
- GYNE 4.05b Benign and Malignant Lesions of The VaginaDocument5 pagesGYNE 4.05b Benign and Malignant Lesions of The VaginaGray SnellNo ratings yet
- GYNE 4.01a EndometriosisDocument4 pagesGYNE 4.01a EndometriosisGray SnellNo ratings yet
- GYNE 4.06-Benign and Malignant Lesions of UterusDocument7 pagesGYNE 4.06-Benign and Malignant Lesions of UterusGray SnellNo ratings yet
- GYNE 4.09 RadiotherapyDocument4 pagesGYNE 4.09 RadiotherapyGray SnellNo ratings yet
- GYNE 4.03 Urinary IncontinenceDocument7 pagesGYNE 4.03 Urinary IncontinenceGray SnellNo ratings yet
- Histo 101Document49 pagesHisto 101Gray SnellNo ratings yet
- GYNE 4.04 Pelvic Organ DisordersDocument7 pagesGYNE 4.04 Pelvic Organ DisordersGray SnellNo ratings yet
- Cancer 1Document65 pagesCancer 1Jessa Borre100% (1)
- GYNE 4.01b InfertilityDocument4 pagesGYNE 4.01b InfertilityGray SnellNo ratings yet
- Cancer 1Document65 pagesCancer 1Jessa Borre100% (1)
- 2Nd Shifting Summary.: Non-Spore FormersDocument13 pages2Nd Shifting Summary.: Non-Spore FormersGray SnellNo ratings yet
- MagnesiumDocument10 pagesMagnesiumGray SnellNo ratings yet
- Low Heat Bagged Cement - Safety Data SheetDocument6 pagesLow Heat Bagged Cement - Safety Data SheetLily ShubinaNo ratings yet
- Cystoscopy 508Document6 pagesCystoscopy 508Jayakumar D SwamyNo ratings yet
- Family Health Optima BrochureDocument4 pagesFamily Health Optima BrochureSneha Karan JagtapNo ratings yet
- Awareness On Polycystic Ovarian Syndrome (PCOS) Among College Going GirlsDocument4 pagesAwareness On Polycystic Ovarian Syndrome (PCOS) Among College Going GirlsEditor IJTSRDNo ratings yet
- Mesenchymal Stem Cell Mediated Cancer Therapy CryovidaDocument8 pagesMesenchymal Stem Cell Mediated Cancer Therapy CryovidaJob MonobeNo ratings yet
- The Obstetrics and Gynecology Clerkship: Your Guide To SuccessDocument6 pagesThe Obstetrics and Gynecology Clerkship: Your Guide To SuccessAnnieNo ratings yet
- Case Study: International Journal of Current ResearchDocument2 pagesCase Study: International Journal of Current ResearchUtami MayasariNo ratings yet
- Gene TherapyDocument91 pagesGene Therapytummalapalli venkateswara rao100% (4)
- Vulvar CancerDocument19 pagesVulvar CancerHerbert CanízNo ratings yet
- The DR Royal Rife MachineDocument6 pagesThe DR Royal Rife MachineHayley As Allegedly-Called YendellNo ratings yet
- Effects of A New Progesterone Receptor ModulatorDocument19 pagesEffects of A New Progesterone Receptor ModulatorErka Wahyu KinandaNo ratings yet
- Active Ingredients PomegranateDocument91 pagesActive Ingredients Pomegranatekennitaharyati100% (1)
- Colen 2017Document7 pagesColen 2017yalocim666No ratings yet
- Bombardieri Emilio, John Buscombe, Giovanni Lucignani, Otmar Schober - Advances in Nuclear Oncology - Diagnosis and Therapy-Informa Healthcare (2007)Document546 pagesBombardieri Emilio, John Buscombe, Giovanni Lucignani, Otmar Schober - Advances in Nuclear Oncology - Diagnosis and Therapy-Informa Healthcare (2007)Gh Alexandra ElenaNo ratings yet
- Zhi Bao San Bian Wan Instruction From TcmherbstoreDocument2 pagesZhi Bao San Bian Wan Instruction From TcmherbstoreSiyeNo ratings yet
- 1.an Overview of Functional FoodsDocument55 pages1.an Overview of Functional FoodsNamrathaNo ratings yet
- El PsaDocument2 pagesEl PsaMaherNo ratings yet
- Sleep Quality and Stress: A Literature Review.: June 2015Document10 pagesSleep Quality and Stress: A Literature Review.: June 2015Terry CanzNo ratings yet
- Top 100 Drugs in CanadaDocument25 pagesTop 100 Drugs in CanadaMohamed Omer100% (1)
- Principle of Vaccinology: Elham Ahmadnezhad Farshid Fayyaz JahaniDocument94 pagesPrinciple of Vaccinology: Elham Ahmadnezhad Farshid Fayyaz JahaniPranav NakhateNo ratings yet
- Oncology MCQDocument7 pagesOncology MCQBestoon Saifaddin100% (1)
- GynecologyDocument124 pagesGynecologyrajkumar871992No ratings yet
- REVALIDA EXAM 200 Answers With RationaleDocument17 pagesREVALIDA EXAM 200 Answers With Rationalexaileenx100% (1)
- Food Synergy - The Key To A Healthy DietDocument9 pagesFood Synergy - The Key To A Healthy DietPutri NabillaNo ratings yet
- Dermatofibrosarcoma Protuberans of The Mons Pubis - A Rare Case ReportDocument4 pagesDermatofibrosarcoma Protuberans of The Mons Pubis - A Rare Case ReportIJAR JOURNALNo ratings yet
- 2021 Article 827Document39 pages2021 Article 827Ahmad TaufikNo ratings yet
- Complete Guide To Building An Eating Plan You Can Live With - Muscle & StrengthDocument8 pagesComplete Guide To Building An Eating Plan You Can Live With - Muscle & StrengthAliNo ratings yet
- Acrf CDocument70 pagesAcrf CHussain AzharNo ratings yet
- I Jos 201129Document9 pagesI Jos 201129jklhjNo ratings yet
- Evaluation and Management of Primary Amenorrhea - UpToDateDocument11 pagesEvaluation and Management of Primary Amenorrhea - UpToDateNatasya SugiantoNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)