Professional Documents
Culture Documents
Analysis of Laboratory Critical Value Reporting at A Large Academic Medical Center
Uploaded by
Levi GasparOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Analysis of Laboratory Critical Value Reporting at A Large Academic Medical Center
Uploaded by
Levi GasparCopyright:
Available Formats
Clinical Chemistry / CRITICAL VALUE REPORTING
Analysis of Laboratory Critical Value Reporting at a Large
Academic Medical Center
Anand S. Dighe, MD, PhD,1 Arjun Rao, MBBS, MBA,2 Amanda B. Coakley, RN, PhD,3
and Kent B. Lewandrowski, MD1
Key Words: Informatics; Clinical pathology; Clinical chemistry; Management; Administration; Hematology; Patient safety; Critical value
reporting
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
DOI: 10.1309/R53XVC2U5CH6TNG8
Abstract Critical value reporting originally was highlighted by
Reporting of laboratory critical values has become Lundberg,1 who defined a critical value as a result suggest-
an issue of national attention as illustrated by recent ing that the patient was in imminent danger unless appropri-
guidelines described in the National Patient Safety ate therapy was initiated promptly. In the 30 years since
Goals of the Joint Commission on Accreditation of Lundberg’s observations, the concept of defining critical val-
Healthcare Organizations. Herein, we report the results ues and systems for reporting have been adopted widely by
of an analysis of 37,503 consecutive laboratory critical laboratories throughout the world.2 In the United States, lab-
values at our institution, a large urban academic oratory accrediting agencies such as the Joint Commission
medical center. We evaluated critical value reporting by on Accreditation of Healthcare Organizations (JCAHO) and
test, laboratory specialty, patient type, clinical care the College of American Pathologists have made critical
area, time of day, and critical value limits. Factors value reporting part of the requirements for accreditation.3,4
leading to delays in critical value reporting are Consequently, critical values are used in virtually all US
identified, and we describe approaches to improving clinical laboratories.
this important operational and patient safety issue. The recent national focus on patient safety has brought
increased attention to the issue of laboratory critical value
reporting. The JCAHO has made improving the process of
critical value reporting a National Patient Safety Goal for the
years 2004 through 2006.3 The JCAHO requires health care
organizations to track and improve the timeliness of report-
ing and receipt of critical test results by the responsible
licensed caregiver. Moreover, the JCAHO has defined criti-
cal test results as not only laboratory tests but also imaging
studies, electrocardiograms, and other diagnostic studies.
Therefore, the process of critical value reporting is of inter-
est across the health care organization.
Critical value reporting parameters may be considered
an important laboratory outcome measurement because they
reflect clinical effectiveness, patient safety, and operational
efficiency. For the critical value reporting process to be
effective, the organization must understand and address the
variables involved in the process. This information is not
readily available in the literature. Most reports have analyzed
758 Am J Clin Pathol 2006;125:758-764 © American Society for Clinical Pathology
758 DOI: 10.1309/R53XVC2U5CH6TNG8
Clinical Chemistry / ORIGINAL ARTICLE
only a few analytes for short periods or have reviewed a the chemistry, hematology, and outpatient health center lab-
small number of critical values in a number of different insti- oratories (chemistry and hematology) was included in our
tutions.5-7 In the present study, we analyzed 12 months of critical value analysis. Microbiology critical values were not
critical value data and more than 37,000 individual critical included in the present study because our microbiology lab-
results to understand the scope of critical value reporting and oratory uses a different documentation process for critical
identify opportunities for process improvement. values.
Critical Callback Procedures
❚Table 1❚ shows the critical callback list for chemistry
Materials and Methods
and hematology that was in use at our institution at the time
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
of the study. The laboratory uses a module in our laboratory
Setting information system (LIS) that automatically flags each test
The Massachusetts General Hospital, Boston, is an 898- result requiring critical callback and organizes it in an appli-
bed tertiary care academic medical center. All major medical cation that aids in the documentation of the phone call
and surgical specialties are supported by the hospital, along placed to the patient’s location (for inpatient and ED
with pediatric and obstetric services and extensive primary patients) or the ordering clinician’s location (for outpa-
care and specialty outpatient practices extending into the tients). Laboratory staff (technologists in the chemistry lab-
greater Boston community. The clinical laboratories include oratory and clinical laboratory assistants in the hematology
chemistry-hematology (core laboratory), microbiology, laboratory) regularly monitor the LIS callback application
blood transfusion services, and various specialty laboratories and perform critical callbacks.
(immunology, diabetes, health center laboratories, neuro-
chemistry). In 2004, the laboratories performed 14 million Data Collection and Analysis
reportable tests, of which 52% were for inpatients, 41% for All data were obtained from reports generated from the
outpatients, and 7% for emergency department (ED) LIS (Misys Healthcare Systems, Tucson, AZ). The data were
patients. Critical values reported from October 1, 2003, to exported to Microsoft Access/Excel (Microsoft, Redmond,
September 30, 2004, were examined. Testing performed in WA) for analysis.
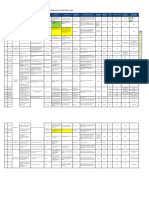
❚Table 1❚
Massachusetts General Hospital Critical Value List
Test Critical Values
Chemistry (blood gas)
Bilirubin, total, 0-3 mo old, mg/dL (µmol/L) >20 (>342)
Calcium, ionized, mg/dL (mmol/L) <3.20 or >6.16 (<0.8 or >1.54)
Hemoglobin, g/dL (g/L) <6.5 (<65)
pCO2, mm Hg <20 or >75
pH <7.10 or >7.59
pO2, mm Hg <40
Chemistry (main laboratory)
Calcium, mg/dL (mmol/L) <6.5 or >14.0 (<1.63 or >3.53)
Carbon dioxide, total, mEq/L (mmol/L) <11 (<11)
Glucose, CSF, mg/dL (mmol/L) <40 (<2.2)
Glucose, plasma, mg/dL (mmol/L) <45 or >500 (<2.5 or >27.8)
Magnesium, mEq/L (mmol/L) <1.0 or >4.9 (<0.50 or >2.45)
Osmolality, plasma or serum, mOsm/kg H2O (mmol/kg H2O) <250 or >335 (<250 or >335)
Phosphorus, mg/dL (mmol/L) <1.1 (<0.36)
Potassium, mEq/L (mmol/L) <2.8 or >6.0 (<2.8 or >6.0)
Sodium, mEq/L (mmol/L) <120 or >160 (<120 or >160)
Hematology
All hematocrit values, % >56% (>0.56)
δ values Various δ checks for platelet and hematocrit values
Differential Presence of blasts on initial smear
Initial hematocrit, % <20 (<0.20)
Initial platelet count, × 103/µL (× 109/L) <50 or >999 (<50 or >999)
Initial WBC count, /µL (× 109/L) <2,000 or >50,000 (<2.0 or >50.0)
Partial thromboplastin time, s >100
Prothrombin time, s >30
CSF, cerebrospinal fluid.
© American Society for Clinical Pathology Am J Clin Pathol 2006;125:758-764 759
759 DOI: 10.1309/R53XVC2U5CH6TNG8 759
Dighe et al / CRITICAL VALUE REPORTING
Results ❚Table 2❚
Critical Values by Laboratory
Critical Value Reporting Laboratory No. (%) of Critical Test Results
Chemistry 25,733 (68.6)
During the period of the study (12 months), the chemistry Hematology 11,770 (31.4)
and hematology laboratories reported 37,503 critical values. Total 37,503 (100)
During the same period, these laboratories reported more than
14 million test results. Therefore, tests with critical values rep-
resented approximately 0.25% of the total test results report-
ed. Examination of only the tests potentially eligible for call- these call volumes correlate with outpatient, inpatient, and ED
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
back (5.1 million tests) demonstrated that 0.74% of these tests specimen throughput (data not shown).
were in the critical range (37,503/5.1 million). The majority of
critical callbacks (68.6%) resulted from testing performed in Inpatient Critical Callbacks
the chemistry laboratory ❚Table 2❚. The hematology laborato- Results for inpatients (which account for 52% of all
ry accounted for 31.4% of critical callbacks. The analytes tests) constituted 74.0% of critical callbacks; for ED patients
most commonly called back were potassium (7,955 results; (7% of all tests), 9.1%; and for outpatients (41% of all tests),
21.2% of critical results) and partial thromboplastin time 16.9%. Thus, on a per test basis, inpatient tests were 3.5 times
(5,467 [14.6%]) ❚Table 3❚. These critical callbacks correspond more likely to result in a critical callback than outpatient
to 1.8% of all potassium levels (7,955/439,104) and 3.0% of tests. As shown in ❚Table 4❚, the intensive care units (ICUs;
all partial thromboplastin times (5,467/183,768) performed. medical, surgical, cardiac, neonatal, transplant, burn, neuro-
Analysis of call volumes vs time ❚Figure 1❚ showed that surgical, and pediatric) were frequent locations for inpatient
inpatient critical value call volumes were high throughout the critical callbacks, together accounting for 50.1% of all criti-
24-hour day, with a range of 830 calls from 12:00 to 1:00 AM cal callbacks, despite representing only 14.1% of the total
to 1,570 calls from 10:00 to 11:00 AM. Outpatient critical inpatient population (127/898 beds). The number of critical
value calls were prominent from 9:00 AM until 11:00 PM, drop- values per year per bed was 109.5 for ICU beds and 18.0 for
ping off to near zero during the late night and early morning. non-ICU beds.
ED critical value calls were highest during the day, but all Owing to the complexity of inpatient care, critical test
times of day had a significant number of calls. As expected, results may not directly reach the responsible caregiver but
❚Table 3❚
Critical Values by Test
Percentage of All Percentage of Test Volume
Test Critical Test Results Critical Test Results* Yearly Test Volume With a Critical Result
Potassium 7,955 21.2 439,104 1.8
Partial thromboplastin time 5,467 14.6 183,768 3.0
Platelet count 3,104 8.3 490,068 0.6
Glucose 2,891 7.7 505,452 0.6
pCO2 (blood gas) 2,346 6.3 140,832 1.7
pO2 1,892 5.0 136,104 1.4
Total CO2 (chemistry) 1,862 5.0 365,004 0.5
Prothrombin time 1,788 4.8 218,100 0.8
Toxicology/TDM drug levels 1,544 4.1 14,280 10.8
Osmolality 1,436 3.8 31,620 4.5
Total calcium 1,325 3.5 338,580 0.4
Hematocrit 1,270 3.4 495,156 0.3
pH 920 2.5 138,936 0.7
Phosphorus 914 2.4 207,840 0.4
Sodium 912 2.4 512,520 0.2
Ionized calcium 698 1.9 90,264 0.8
Magnesium 648 1.7 215,544 0.3
Glucose, CSF 171 0.5 2,796 6.1
Hemoglobin (blood gas) 169 0.5 73,608 0.2
WBC count 151 0.4 496,260 0.03
Total bilirubin (neonates) 40 0.1 9,500 0.4
Total 37,503 100.1 5,105,336 —
CSF, cerebrospinal fluid; TDM, therapeutic drug monitoring.
* Does not total 100.0% because of rounding.
760 Am J Clin Pathol 2006;125:758-764 © American Society for Clinical Pathology
760 DOI: 10.1309/R53XVC2U5CH6TNG8
Clinical Chemistry / ORIGINAL ARTICLE
2,500
ED
Outpatient
2,000 Inpatient
No. of Critical Values
1,500
1,000
500
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
0
0-1
1-2
2-3
3-4
4-5
5-6
6-7
7-8
8-9
9-10
10-11
11-12
12-13
13-14
14-15
15-16
16-17
17-18
18-19
19-20
20-21
21-22
22-23
23-24
Hour of Day
❚Figure 1❚ Critical values vs time of day. Distribution of critical value calls vs time (24-h clock) for the emergency department
(ED), outpatients, and inpatients.
rather may be communicated to the caregiver via an opera- mean, 0.5 minute; non-ICU settings mean, 2.0 minutes; P =
tions associate (OA; clerical staff members who perform .010). This was likely due to the greater availability of care-
clinical support functions). We therefore wanted to exam- givers in the ICU setting.
ine the communication process from the OA to the respon-
sible caregiver (physician or nurse). To examine the timeli- Critical Value Turnaround Time
ness of reporting, we created a logbook that each inpatient The “in-laboratory” turnaround time for each critical
floor maintained to monitor critical values. The OA docu- value was determined to assess the timeliness of critical value
ments in the logbook the time the call was received from reporting. For the 37,503 critical values, the mean time from
the laboratory, patient identifiers, the test result, and the the value entering the critical callback queue to the time when
time the critical result information was communicated to the critical value information was conveyed to the patient
the responsible caregiver. Critical results communicated location or ordering clinician was 22 minutes, and the median
directly to the licensed caregiver (without involving the time was 9 minutes (data not shown). Delays in critical value
OA) were not documented in the logbook because this reporting correlated with testing performed on outpatients and
information is already captured in the LIS callback appli- testing ordered on requisitions lacking the name of the order-
cation. We examined the logbooks for 29 inpatient care ing clinician or the ordering location. Tests performed in set-
units for 1 month. During this period, 1,477 critical values tings where there is continuous technologist presence (eg,
were documented in the logbook. The mean on-floor com- blood gases) were called back faster than tests performed in
munication time (OA to responsible caregiver) was 1.8 min- other areas. This information was useful as we began to imple-
utes (median, 1.0 minute). Increased communication times ment measures to improve critical value reporting in all areas
were observed on non-ICU floors compared with ICUs (ICU of the laboratory.
❚Table 4❚
Critical Values by Site
Location No. (%) of Critical Test Results No. of Beds Critical Values per Year per Bed
Inpatient 27,744 (74.0)
ICU 13,901 (50.1) 127 109.5
Non-ICU 13,843 (49.9) 771 18.0
Total 27,744 (100.0) 898 30.9
Outpatient 6,330 (16.9) — —
ED 3,429 (9.1) — —
Total 37,503 (100.0) — —
ED, emergency department; ICU, intensive care unit.
© American Society for Clinical Pathology Am J Clin Pathol 2006;125:758-764 761
761 DOI: 10.1309/R53XVC2U5CH6TNG8 761
Dighe et al / CRITICAL VALUE REPORTING
Examination of Critical Value Limits callback policies to reduce the number of critical callbacks.
To better understand our present upper and lower value For example, changing the lower limit callback value for glu-
limits for critical callbacks (eg, the limits for potassium of cose from less than 60 mg/dL (<3.3 mmol/L) to less than 45
<2.8 and >6.0 mEq/L [<2.8 and >6.0 mmol/L]), we plotted the mg/dL (<2.5 mmol/L) has resulted in 2,136 fewer calls per
number of critical callbacks for each analyte vs the result year (an overall reduction of 5.7% of all callbacks) ❚Figure 3❚.
value. This enabled us to examine the potential effect that
changing the limits of critical callback would have on call vol-
umes. Representative graphs of the critical value calls for
Discussion
potassium and glucose are shown in ❚Figure 2❚. This informa-
tion was used in conjunction with published literature and In this report, we provide a comprehensive view of the
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
consultation with clinicians to propose changes to the critical critical value reporting process in a large academic medical
A
120
100
No. of Critical Values
80
60
40
20
0
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
500-520
521-540
541-560
561-580
581-600
601-620
621-640
641-660
661-680
681-700
701-720
721-740
741-760
761-780
781-800
801-900
901-1,000
>1,000
Test Result Value
B
1,600
1,500
1,400
1,300
1,200
No. of Critical Values
1,100
1,000
900
800
700
600
500
400
300
200
100
0
0.2
0.5
1.0
1.1
1.2
1.3
1.4
1.5
1.6
1.7
1.8
1.9
2.0
2.1
2.2
2.3
2.4
2.5
2.6
2.7
6.1
6.2
6.3
6.4
6.5
6.6
6.7
6.8
6.9
7.0
7.1
7.2
7.3
7.4
7.5
7.6
7.7
7.8
7.9
8.0
8.1
8.2
8.3
8.4
8.5
8.6
8.7
8.8
8.9
9.0
9.1
9.2
9.3
9.4
9.5
9.6
9.7
9.8
9.9
10
Test Result Value
❚Figure 2❚ Critical value limit analysis for glucose and potassium. The number of critical value callbacks for glucose (A) and
potassium (B) are plotted vs the test result value. The dotted line indicates the critical value limits for each test (glucose, <45 or
>500 mg/dL [<2.5 or >27.8 mmol/L]; potassium, <2.8 or >6.0 mEq/L [<2.8 or >6.0 mmol/L]).
762 Am J Clin Pathol 2006;125:758-764 © American Society for Clinical Pathology
762 DOI: 10.1309/R53XVC2U5CH6TNG8
Clinical Chemistry / ORIGINAL ARTICLE
center. We provide details regarding the scope, volume, tim- list. In addition to determining which tests are to be included
ing, and operational aspects of critical value reporting. Many in the critical values list, another important strategy is to
of these parameters should be applicable to a variety of set- examine the consequences of changing the boundaries for crit-
tings. This analysis provides a context for comparison and ical value reporting. These boundaries must be defined in con-
process improvement. sultation with clinicians. Small changes in critical value
Increasing workload in the clinical laboratory makes it reporting parameters may result in the addition or loss of thou-
important to achieve efficient use of laboratory resources to sands of phone calls for the laboratory staff.
maximize clinical benefits. Expansion of critical callback lists Outpatient critical values present unique challenges in
to include testing that does not meet the criterion of the timely reporting to clinicians. One of the strongest correlates
“imminent danger” standard may dilute the urgency of a crit- of delayed reporting of critical values was the specimen being
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
ical value call and lead to unnecessary interruptions for clini- obtained from an outpatient. Outpatient critical values are
cians. For example, critical value calls for high creatinine lev- challenging to communicate to the responsible clinician
els will not be of clinical value for patients receiving dialysis because there often are different approaches in various prac-
and in many situations in which the high creatinine value is an tices for determining patient coverage. Unlike inpatients, there
expected finding. In addition, there are many clinical settings is no fixed patient location that can be phoned.
(chemotherapy, malignancy) in which the “critical” test result Another factor we identified as causing delays for outpa-
is expected and reporting of this value may not contribute to tients was illegible or missing ordering provider information. As
improved patient care. By applying this logic to other scenar- a result of this analysis, we have changed our medical policy to
ios, we have not adopted critical callbacks for positive cardiac explicitly state that all requisitions must have an ordering
markers (creatine kinase-MB and troponin T). The marginal provider and an ordering location printed on the requisition.
clinical usefulness vs the marginal resource cost should be We are in the process of communicating this to our caregivers.
considered carefully when the tests and cutoff limits for criti- We also have instituted daily exception reports of critical val-
cal value reporting are determined. National standards have ues called back in times that exceed our threshold limit of
been published concerning critical value ranges.8,9 These stan- acceptability (30 minutes). These reports are distributed to the
dards provide a benchmark against which the laboratory can laboratories and are being used to understand and remedy the
compare and adjust its critical values list accordingly. root causes of delays in critical results reporting. We have noted
Communication by telephone, especially when per- that recent improvements in the critical value communication
formed by technologists, is a costly practice in terms of the times have coincided with increased awareness of critical value
resources required to complete the phone calls and document monitoring. We presently are working with our outpatient
the process. For this reason, it is helpful to try to reduce the practices to improve communication between the laboratories
number of phone calls by careful review of the critical values and the outpatient care centers.
1,000
800
No. of Results
600
400
200
0
0 5 10 15 20 25 30 35 40 45 50 55 60 65 70 75 80 85 90 95 100
Glucose Value (mg/dL)
❚Figure 3❚ Glucose test results and critical value limits. Glucose values are plotted vs the number of results with that value for a
12-month period. The dotted lines indicate the 2,136 results falling between the previous critical value limit (<60 mg/dL [<3.3
mmol/L]) and the current critical value limit (<45 mg/dL [<2.5 mmol/L]). To convert conventional values (mg/dL) to Système
International units (mmol/L), multiply by 0.0551.
© American Society for Clinical Pathology Am J Clin Pathol 2006;125:758-764 763
763 DOI: 10.1309/R53XVC2U5CH6TNG8 763
Dighe et al / CRITICAL VALUE REPORTING
Another contributor to delays in outpatient critical value because many of these “critically low” results will be falsely
reporting is the heterogeneity of the outpatient population, low or no longer relevant. The ability to provide a physician-
with specimens arriving from health centers, clinics, urgent specific critical values list could eliminate a large number of
care centers, dialysis centers, and physicians’ offices. Each of unnecessary critical value calls. These systems, when inter-
these areas is likely to have a different call schedule, answer- faced with automated alerting systems, will have the potential
ing service, and cross-coverage procedure, making reliable to improve patient safety and provide more context-sensitive
communication with the responsible licensed caregiver chal- critical value reporting. At present, practical implementation
lenging. The nature of outpatient specimen transport and pro- of this scenario would be constrained by regulations (partic-
cessing often results in outpatient test results being generated ularly the JCAHO National Patient Safety Goals) that require
in the evening when the outpatient clinic or physician’s office all critical results to be communicated and do not allow for
Downloaded from https://academic.oup.com/ajcp/article-abstract/125/5/758/1759931 by guest on 22 November 2019
is closed. The laboratory must have a mechanism to determine more nuanced approaches.
on-call coverage and work with outpatient practices to
improve the communication processes. From the Departments of 1Pathology, 2Medicine, and 3Nursing,
The potential for technological solutions to improve the Massachusetts General Hospital, Boston.
process of critical value reporting is evident in numerous Address reprint requests to Dr Lewandrowski: Clinical
reports.10,11 The use of information technology to automatical- Chemistry, Bigelow Bldg, Room 510, Massachusetts General
ly communicate with the responsible provider has been Hospital, 55 Fruit St, Boston, MA 02114.
demonstrated to reduce the critical value reporting time in
controlled settings. For implementation of automated critical
value reporting, interfaces from the LIS to technologies that References
facilitate bidirectional communication (such as e-mail or 2-
1. Lundberg GD. When to panic over abnormal values. MLO
way pagers) need to be developed. An important component Med Lab Obs. 1972;4:47-54.
in such a system is the ability of the automatic reporting sys- 2. Lundberg GD. Critical (panic) value notification: an
tem to reliably determine the identity of the responsible established laboratory practice policy (parameter) [editorial].
provider. At larger medical centers, this task can be challeng- JAMA. 1990;263:709.
ing because there may be different coverage lists, tests ordered 3. Joint Commission on the Accreditation of Healthcare
Organizations: National Patient Safety Goals. Available at:
by consultants unknown to the primary caregiver, and patient http://www.jcaho.org/accredited+organizations/patient+safety/
transfers to different locations. An electronic reporting system npsg.htm. Accessed August 22, 2005.
potentially could create dangerous delays in communication if 4. Center for Medicare and Medicaid Services, Department of
not properly implemented. The system needs to have an health and Human Services. Clinical Laboratory
Improvement Amendments of 1988. 68 Federal Register 1047
“acknowledgment” function such that the laboratory can (2003) (codified at 42 CFR §493.1291(g)).
ensure that the responsible caregiver received the result. 5. Lum G. Assessment of a critical limit protocol for point-of-
Electronic systems also require an escalation procedure so that care glucose testing. Am J Clin Pathol. 1996;106:390-395.
lack of acknowledgment of the critical result prompts an alter- 6. Howanitz PJ, Steindel SJ, Heard NV. Laboratory critical values
native approach for communication. policies and procedures: a College of American Pathologists
Q-Probes study in 623 institutions. Arch Pathol Lab Med.
Development of LIS middleware with alert reporting 2002;126:663-669.
software should permit highly nuanced approaches to critical 7. Kuperman GJ, Boyle D, Jha A, et al. How promptly are
value reporting in the near future. Rules-based logic can be inpatients treated for critical laboratory results? J Am Med
applied to laboratory values to build alerts that take into Inform Assoc. 1998;5:112-119.
account not only the result value, but also other related 8. Kost GJ. Table of critical limits. MLO Med Lab Obs.
2004;36:6-7.
results, a change in the current test result from previous
9. Burtis CA, Ashwood ER, Bruns DE. Tietz Textbook of Clinical
results (ie, delta checks), patient demographics, ordering Chemistry and Molecular Diagnosis. Philadelphia, PA: Saunders;
provider, and other parameters to customize the alerting to 2005.
the patient’s condition and the needs of the clinical team for 10. Bates DW, Pappius E, Kuperman GJ, et al. Using information
notification. For example, many oncology physicians do not systems to measure and improve quality. Int J Med Inform.
1999;53:115-124.
want to be notified regarding patients with neutropenia.
11. Tate KE, Gardner RM, Weaver LK. A computerized laboratory
Similarly, there is little usefulness in notifying a diabetologist alerting system. MD Comput. 1990;7:296-301.
of low glucose values for patients seen in an outpatient clinic
764 Am J Clin Pathol 2006;125:758-764 © American Society for Clinical Pathology
764 DOI: 10.1309/R53XVC2U5CH6TNG8
You might also like
- Cl-Molec Cap Assay Check ListDocument74 pagesCl-Molec Cap Assay Check ListAndreína Gabriela Sánchez González0% (1)
- Desirable Biological Variation Database Specifications - WestgardDocument10 pagesDesirable Biological Variation Database Specifications - WestgardElmyLiantika MaranantanNo ratings yet
- GraphicalComparisonsof Interferences in ClinicalChemistryInstrumentationDocument6 pagesGraphicalComparisonsof Interferences in ClinicalChemistryInstrumentationDaniel Huachani CoripunaNo ratings yet
- CLIA Waived Codes ListDocument41 pagesCLIA Waived Codes ListKarunanidhi PalaniveluNo ratings yet
- SMILE Validation Requirements for Chemistry TEaDocument6 pagesSMILE Validation Requirements for Chemistry TEabenchmark InnovationNo ratings yet
- EP15-A3 Example 2Document4 pagesEP15-A3 Example 2Jenny RosaliNo ratings yet
- Why Be Moral? Philosophical TheoriesDocument7 pagesWhy Be Moral? Philosophical TheoriesRegine CuntapayNo ratings yet
- Icelandic Spells and SigilsDocument16 pagesIcelandic Spells and SigilsSimonida Mona Vulić83% (6)
- Laws of ThermocoupleDocument3 pagesLaws of ThermocoupleMourougapragash SubramanianNo ratings yet
- Oral Medication PharmacologyDocument4 pagesOral Medication PharmacologyElaisa Mae Delos SantosNo ratings yet
- Complete Guide To E-Commerce TechnologyDocument420 pagesComplete Guide To E-Commerce Technologypilatus100% (4)
- Validation QuantitiveDocument13 pagesValidation QuantitiveTrần Thị Thùy NgaNo ratings yet
- Critical Value in HematologyDocument8 pagesCritical Value in HematologySTARK DIAGNOSTICSNo ratings yet
- Free Download CLSI EP26 User Evaluation of Between Reagent Lot VariationDocument20 pagesFree Download CLSI EP26 User Evaluation of Between Reagent Lot VariationDrNikhil choudharyNo ratings yet
- Ep09-A3 (2013) CorrelationDocument98 pagesEp09-A3 (2013) CorrelationSylvain ContiéNo ratings yet
- 10.30-11.15 Mario PlebaniDocument64 pages10.30-11.15 Mario Plebanigsaldadze100% (1)
- EP Evaluator-CLIA EE-CLIA For Evaluating ClinicalDocument3 pagesEP Evaluator-CLIA EE-CLIA For Evaluating ClinicalKamal JaoniNo ratings yet
- Biological Variation Database Structure and Criteria Used For Generation and UpdateDocument7 pagesBiological Variation Database Structure and Criteria Used For Generation and UpdateFede0No ratings yet
- Quality control using pooled serum and retained samplesDocument42 pagesQuality control using pooled serum and retained sampleszahraa aliNo ratings yet
- Flow Cell Wash Kit Exp wsh004 WFC - 9120 - v1 - Revb - 08dec2020 MinionDocument9 pagesFlow Cell Wash Kit Exp wsh004 WFC - 9120 - v1 - Revb - 08dec2020 MinionErikk DangNo ratings yet
- Lab Math Lec (Prelims)Document7 pagesLab Math Lec (Prelims)Merra VenzuelaNo ratings yet
- TE, TEa, Six-SigmaDocument36 pagesTE, TEa, Six-SigmaDr. Pillala KrishnaveniNo ratings yet
- Interferences From Blood Collection Tube Components On Clinical Chemistry Assays - Biochemia MedicaDocument8 pagesInterferences From Blood Collection Tube Components On Clinical Chemistry Assays - Biochemia MedicaBeatThe BeadNo ratings yet
- Clsi Ep18 ADocument59 pagesClsi Ep18 ACristian Gutiérrez VeraNo ratings yet
- Quality Control2Document32 pagesQuality Control2Mustafa KhandgawiNo ratings yet
- Prof. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityDocument91 pagesProf. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityJeLo ReaNdelarNo ratings yet
- Clinical Chemistry Methods Guide 2010: For Labquality Data ProcessingDocument103 pagesClinical Chemistry Methods Guide 2010: For Labquality Data Processingcamilovivi100% (1)
- Water purification systems produce pure waterDocument10 pagesWater purification systems produce pure waterLloid LauretaNo ratings yet
- CAP Presentation On StatisticDocument88 pagesCAP Presentation On StatisticAmirul AriffNo ratings yet
- Adjusting Quality Control Chart Limits For WBC, RBC, HB, and PLT Counts To Reduce Daily Control Risks in Hospital LaboratoryDocument11 pagesAdjusting Quality Control Chart Limits For WBC, RBC, HB, and PLT Counts To Reduce Daily Control Risks in Hospital LaboratoryHerbanu PramonoNo ratings yet
- MANI Quality Control in Hematology AnalysersDocument65 pagesMANI Quality Control in Hematology Analyserscandiddreams100% (1)
- ASVCP Allowable Total ErrorDocument25 pagesASVCP Allowable Total ErrorLaborat.ptj PONDOK TJANDRANo ratings yet
- Quality ControlDocument88 pagesQuality ControlYangnuu TitusNo ratings yet
- Use of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateDocument6 pagesUse of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateTriana AmaliaNo ratings yet
- Clia & Cap Regulatory TrainingDocument23 pagesClia & Cap Regulatory TrainingWilliam David HommelNo ratings yet
- Trace Ability in Laboratory Medicine - References 101029Document2 pagesTrace Ability in Laboratory Medicine - References 101029PittsfordNo ratings yet
- RIQAS General Clinical Chemistry Programme Method QuestionnaireDocument20 pagesRIQAS General Clinical Chemistry Programme Method Questionnairedr_4uNo ratings yet
- Chapitre Validation Diagnostics Assays PDFDocument18 pagesChapitre Validation Diagnostics Assays PDFBuddhi BhaskaraNo ratings yet
- Calibrating and validating analytical methodsDocument32 pagesCalibrating and validating analytical methodsHaziq KhairiNo ratings yet
- TextbookofComputerApplicationsandBiostatistics PDFDocument225 pagesTextbookofComputerApplicationsandBiostatistics PDFMAhabul AlamNo ratings yet
- Reference Intervals - Direct Priori MethodDocument5 pagesReference Intervals - Direct Priori MethodMWNo ratings yet
- Post-Analytical Best PracticesDocument48 pagesPost-Analytical Best PracticesSaravnan RajendranNo ratings yet
- NABL 112 Effective From 01.06.2019 PDFDocument102 pagesNABL 112 Effective From 01.06.2019 PDFSp PpvNo ratings yet
- Clsi 99% PDFDocument14 pagesClsi 99% PDFstefannyNo ratings yet
- Tests Affected by Haemolysed, Icteric and Lipemic Samples, W5-SOP-1-1-1Document2 pagesTests Affected by Haemolysed, Icteric and Lipemic Samples, W5-SOP-1-1-1Dejan BodetićNo ratings yet
- CorrelationDocument17 pagesCorrelationisabel bautistaNo ratings yet
- Manual For Procurement of Diagnostics-001-June2013Document34 pagesManual For Procurement of Diagnostics-001-June2013Jose MirandaNo ratings yet
- EA-4-10 Acreditarea Laboratoarelor de Microbiologie%Document26 pagesEA-4-10 Acreditarea Laboratoarelor de Microbiologie%dani2703No ratings yet
- Clinical1 Quality Control - 10Document36 pagesClinical1 Quality Control - 10Khansa QureshiNo ratings yet
- Laboratory Turnaround TimeDocument17 pagesLaboratory Turnaround TimeNicole HoNo ratings yet
- Blood Tube Collection GuideDocument365 pagesBlood Tube Collection GuideFeliciadlTNo ratings yet
- Quality Assurance in Hematology Group 11Document51 pagesQuality Assurance in Hematology Group 11Mandy A. DelfinNo ratings yet
- Point-Of-Care Analyzers, Blood Gas - PH - Chemistry - Electrolyte - 050315065814Document3 pagesPoint-Of-Care Analyzers, Blood Gas - PH - Chemistry - Electrolyte - 050315065814Carlos Ferro100% (1)
- Clinical Biochemistry Reference Ranges HandbookDocument18 pagesClinical Biochemistry Reference Ranges HandbookMurali DathanNo ratings yet
- CLIA Requirements For Analytical Quality - WestgardDocument7 pagesCLIA Requirements For Analytical Quality - WestgardApril Woods0% (1)
- IQCPDocument1 pageIQCPPrabhu Selvaraj100% (1)
- 5-Westgard Quality Control 4 SlidesDocument9 pages5-Westgard Quality Control 4 SlidesPaul Avelino CallupeNo ratings yet
- GP33 Manual ClsiDocument3 pagesGP33 Manual ClsiGonzalez ArturoNo ratings yet
- Validation Cell AnalyzersDocument45 pagesValidation Cell AnalyzerscandiddreamsNo ratings yet
- Ep06ed2 Correction Notice Web 20210909Document1 pageEp06ed2 Correction Notice Web 20210909danielNo ratings yet
- Validation and Evaluation of Eight Commercially Available Point of Care CRP MethodsDocument7 pagesValidation and Evaluation of Eight Commercially Available Point of Care CRP MethodsAle AraujoNo ratings yet
- Guide 6 basic toolsDocument30 pagesGuide 6 basic toolsdrs_mdu48No ratings yet
- CLIAbrochure8 PDFDocument12 pagesCLIAbrochure8 PDFAlexandr Chuvakov100% (1)
- IH Hospital Wide QI Master Spreadsheet 2023Document115 pagesIH Hospital Wide QI Master Spreadsheet 2023Uranchimeg MyagmarchimedNo ratings yet
- Histology Respiratory PDFDocument35 pagesHistology Respiratory PDFLevi GasparNo ratings yet
- Philippine Precolonial Literature and its Rich Oral TraditionsDocument37 pagesPhilippine Precolonial Literature and its Rich Oral TraditionsLevi GasparNo ratings yet
- Research ParadigmDocument2 pagesResearch ParadigmLevi GasparNo ratings yet
- Personality Traits For Entrepreneurs Rating WorksheetDocument3 pagesPersonality Traits For Entrepreneurs Rating WorksheetLevi GasparNo ratings yet
- Vector AdditionDocument1 pageVector AdditionLevi GasparNo ratings yet
- ChristineDocument8 pagesChristineLevi GasparNo ratings yet
- Example Letter For College Admission ApplicationDocument1 pageExample Letter For College Admission ApplicationLevi GasparNo ratings yet
- Parasitology Practicals Reviewer COMPLETEDocument39 pagesParasitology Practicals Reviewer COMPLETECarlo Mercado100% (1)
- Checklist For Review of Floor Plans Drug Testing Laboratory 2017 PDFDocument2 pagesChecklist For Review of Floor Plans Drug Testing Laboratory 2017 PDFRitz Bautista Balanay100% (1)
- THE Non-Protein OF The Blood Health and in Hepatic Disease: NitrogenDocument8 pagesTHE Non-Protein OF The Blood Health and in Hepatic Disease: NitrogenLevi GasparNo ratings yet
- Feasibility Study For Automating The Analytical Laboratories of The Chemistry Branch, National Enforcement Investigation Center, Environmental Protection AgencyDocument33 pagesFeasibility Study For Automating The Analytical Laboratories of The Chemistry Branch, National Enforcement Investigation Center, Environmental Protection AgencyLevi GasparNo ratings yet
- 1 s2.0 S0022030253914532 MainDocument6 pages1 s2.0 S0022030253914532 MainLevi GasparNo ratings yet
- Challenging Prejudice and Challenging Prejudice and Discrimination DiscriminationDocument19 pagesChallenging Prejudice and Challenging Prejudice and Discrimination DiscriminationLevi GasparNo ratings yet
- DOH Equipment Clinical LabDocument6 pagesDOH Equipment Clinical Labal gulNo ratings yet
- Assessment ToolDocument13 pagesAssessment Toolal gulNo ratings yet
- Applied and Environmental Microbiology-1967-Phillips-378.fullDocument12 pagesApplied and Environmental Microbiology-1967-Phillips-378.fullLevi GasparNo ratings yet
- Healthcare Waste Management SystemDocument30 pagesHealthcare Waste Management SystemLevi GasparNo ratings yet
- Phlebotomist Labelling Primary Blood Tubes For Clinical Laboratory Tests An Important Step To Medical Diagnostics 2167 0870.1000e111 PDFDocument2 pagesPhlebotomist Labelling Primary Blood Tubes For Clinical Laboratory Tests An Important Step To Medical Diagnostics 2167 0870.1000e111 PDFLevi GasparNo ratings yet
- Ao2018 0025Document15 pagesAo2018 0025Klayte TayongNo ratings yet
- Ana 5.1 Endocrine System - RiveraDocument10 pagesAna 5.1 Endocrine System - Riveralovelots1234No ratings yet
- Phlebotomist Labelling Primary Blood Tubes For Clinical Laboratory Tests An Important Step To Medical Diagnostics 2167 0870.1000e111 PDFDocument2 pagesPhlebotomist Labelling Primary Blood Tubes For Clinical Laboratory Tests An Important Step To Medical Diagnostics 2167 0870.1000e111 PDFLevi GasparNo ratings yet
- Idm Sec3Document116 pagesIdm Sec3Levi GasparNo ratings yet
- ADDTL NOTES Poor Diet and Physical ActivityDocument1 pageADDTL NOTES Poor Diet and Physical ActivityLevi GasparNo ratings yet
- Health Waste ManagementDocument27 pagesHealth Waste ManagementLevi GasparNo ratings yet
- Instructional Materials 2Document11 pagesInstructional Materials 2Joy Carmen CastilloNo ratings yet
- Healthcare Waste Management HandoutDocument4 pagesHealthcare Waste Management Handoutchicken015No ratings yet
- Purposive CommDocument7 pagesPurposive CommLevi GasparNo ratings yet
- Anova SPSSDocument1 pageAnova SPSSLevi GasparNo ratings yet
- Technology Consulting: Amruta Kulkarni Anu Abraham Rajat JainDocument9 pagesTechnology Consulting: Amruta Kulkarni Anu Abraham Rajat JainRajat JainNo ratings yet
- Business StrategiesDocument2 pagesBusiness Strategiesthristanlexter694No ratings yet
- European Business in China Position Paper 2017 2018 (English Version)Document408 pagesEuropean Business in China Position Paper 2017 2018 (English Version)Prasanth RajuNo ratings yet
- Steel Glossary RBC Capital GoodDocument10 pagesSteel Glossary RBC Capital Goodrajesh pal100% (1)
- Presentation of Urban RegenerationsDocument23 pagesPresentation of Urban RegenerationsRafiuddin RoslanNo ratings yet
- Final - WPS PQR 86Document4 pagesFinal - WPS PQR 86Parag WadekarNo ratings yet
- Drug Study TramadolDocument7 pagesDrug Study TramadolZyrilleNo ratings yet
- Telephone Triggered SwitchesDocument22 pagesTelephone Triggered SwitchesSuresh Shah100% (1)
- Pure and Applied Analysis Problems Solved Step-by-StepDocument8 pagesPure and Applied Analysis Problems Solved Step-by-Stepalpha2122No ratings yet
- Digital Water Monitoring and Turbidity Quality System Using MicrocontrollerDocument8 pagesDigital Water Monitoring and Turbidity Quality System Using MicrocontrollerIrin DwiNo ratings yet
- PrintDocument18 pagesPrintHookandcrookNo ratings yet
- Stellar Structure and EvolutionDocument222 pagesStellar Structure and Evolutionjano71100% (2)
- A ULTIMA ReleaseNotesAxiomV PDFDocument38 pagesA ULTIMA ReleaseNotesAxiomV PDFIVANALTAMARNo ratings yet
- K230F Equipment ManualsDocument166 pagesK230F Equipment ManualsHui ChenNo ratings yet
- Second Quarterly Examination Math 9Document2 pagesSecond Quarterly Examination Math 9Mark Kiven Martinez94% (16)
- Visualization BenchmarkingDocument15 pagesVisualization BenchmarkingRanjith S100% (1)
- LogDocument119 pagesLogcild MonintjaNo ratings yet
- General Biology 2-Week 2-Module 4-Evidence of EvolutionDocument16 pagesGeneral Biology 2-Week 2-Module 4-Evidence of EvolutionFEMALE Dawal LaizaNo ratings yet
- Barelwiyah, Barelvi Chapter 1 (Part 2 of 5)Document31 pagesBarelwiyah, Barelvi Chapter 1 (Part 2 of 5)Dawah ChannelNo ratings yet
- PAPERBOARD QUALITYDocument8 pagesPAPERBOARD QUALITYaurelia carinaNo ratings yet
- INVENTORY MANAGEMENT TechniquesDocument24 pagesINVENTORY MANAGEMENT TechniquesWessal100% (1)
- Kennedy 1945 Bibliography of Indonesian Peoples and CulturesDocument12 pagesKennedy 1945 Bibliography of Indonesian Peoples and CulturesJennifer Williams NourseNo ratings yet
- Athenaze 1 Chapter 7a Jun 18th 2145Document3 pagesAthenaze 1 Chapter 7a Jun 18th 2145maverickpussNo ratings yet
- Design & Construction of Substation 16P Painting System ComplianceDocument103 pagesDesign & Construction of Substation 16P Painting System ComplianceRamil LazNo ratings yet
- SMEs, Trade Finance and New TechnologyDocument34 pagesSMEs, Trade Finance and New TechnologyADBI EventsNo ratings yet
- Serendipity - A Sociological NoteDocument2 pagesSerendipity - A Sociological NoteAmlan BaruahNo ratings yet